Abstract
Background:
Although recent studies have identified important risk factors associated with incident carpal tunnel syndrome(CTS), risk factors associated with its severity have not been well explored.
Objective:
To examine the associations between personal, workplace psychosocial and biomechanical factors and incident work disability among workers with carpal tunnel syndrome.
Methods:
Between 2001 and 2010 five research groups conducted coordinated prospective studies of CTS and related work disability among US workers from various industries. Workers with prevalent or incident CTS (N=372) were followed for up to 6.4 years. Incident work disability was measured as: (1)change in work pace or work quality, (2)lost time, or (3)job change following the development of CTS. Psychosocial factors were assessed by questionnaire. Biomechanical exposures were assessed by observation and measurements and included force, repetition, duty cycle and posture. Hazard ratios(HR) were estimated using Cox models.
Results:
Disability incidence rates(IR) per 100 person-years were 33.2 for changes in work pace or quality, 16.3 for lost time, and 20.0 for job change. There was a near doubling of risk for job change among those in the upper tertile of the Hand Activity Level(HAL) Scale (HR=2.17; 95%CI: 1.17–4.01), total repetition rate (HR=1.75; 95% CI:1.02–3.02), %time spent in all hand exertions (HR=2.20; 95%CI:1.21–4.01), and a 6-fold increase for high job strain. Sensitivity analyses indicated attenuation due to inclusion of the prevalent CTS cases.
Conclusion:
Personal, biomechanical and psychosocial job factors predicted CTS–related disability. Results suggest that prevention of severe disability requires a reduction of both biomechanical and organizational work stressors.
Keywords: epidemiology, musculoskeletal disorders, carpal tunnel syndrome, disability, job stress
Introduction
Carpal tunnel syndrome (CTS) is an important occupational health problem due to its considerable incidence rate and associated disability1. Recent large prospective studies with diverse worker risk groups in the US2 (this consortium’s data) and Italy3,4 have reported CTS incidence rates of 2.3 per 100 person years and 5.4 per 100 person years, respectively. Additionally, the median lost work time following CTS is 25 days, making CTS an important driver of overall workers compensation costs1,5. Consequently, a better understanding of CTS-associated disability is key to minimizing the adverse impact of the disorder on workers and employers.
Primary, secondary, and tertiary prevention are commonly defined as: (i)prevention of any physiological change that may lead to injury or disease, (ii)prevention of the occurrence of disease once some pathophysiological change has occurred, and (iii)prevention of disability and recurrence once the injury or disease has occurred. Since it has been shown in other body regions, such as the low back, that etiologic(cause of injury) and prognostic(chance of recovery) factors can be different6, assessing both etiologic and prognostic factors for MSDs like CTS is warranted.
Previously, we pooled six prospective cohort studies with individualized exposure assessments and reported the personal, work psychosocial and biomechanical factors associated with the development of incident cases of CTS7–9. However, no large-scale studies have assessed the risk of work disability among workers with CTS using individual-level biomechanical exposure assessments. Understanding who is at the highest risk for disability once CTS develops is extremely useful for tertiary prevention efforts. Therefore, the goal of these analyses was to explore the personal, biomechanical and work psychosocial factors associated with severity of CTS as measured by three measures of work disability among those with CTS. We hypothesized that the effect estimates of the associations between covariates, physical exposures, psychosocial factors and outcome measures would get higher with increasing severity levels of work disability.
Methods
Study design.
This consortium consists of six research groups which conducted coordinated multi-year, prospective studies of upper extremity musculoskeletal disorders (UEMSDs) among 4,321 US workers from 54 different workplaces across 10 different states between 2001 and 20102,10. Jobs ranged in physical demand; individual-level exposure and health outcome information (including symptoms, physical examination findings, nerve conduction measures and functional outcome assessments) were collected. Similarities in study design allowed pooling of raw study data2,10. Workers meeting the case definition of CTS were assessed through repeated annual or biannual questionnaires for up to 6.4 years (average 2.4 years). This current report had requisite data collected by four research groups that also collected information on work disability representing workers from 9 US states (AL, AR, CA, NV, ME, WA, WI, IL, UT).
Participants.
This study’s analyses relied on the 372 baseline prevalent or incident CTS cases(Figure 1). Electrodiagnostic testing (EDS) of the median and ulnar nerves were performed at baseline and at regular intervals during the follow-up periods. A detailed questionnaire was administered at baseline to assess work history, demographics, psychosocial factors, medical history, musculoskeletal symptoms, and work disability. Periodic surveys were administered to trigger physical exams, electrodiagnostic studies, and assess work related pain and disability.
Figure 1.
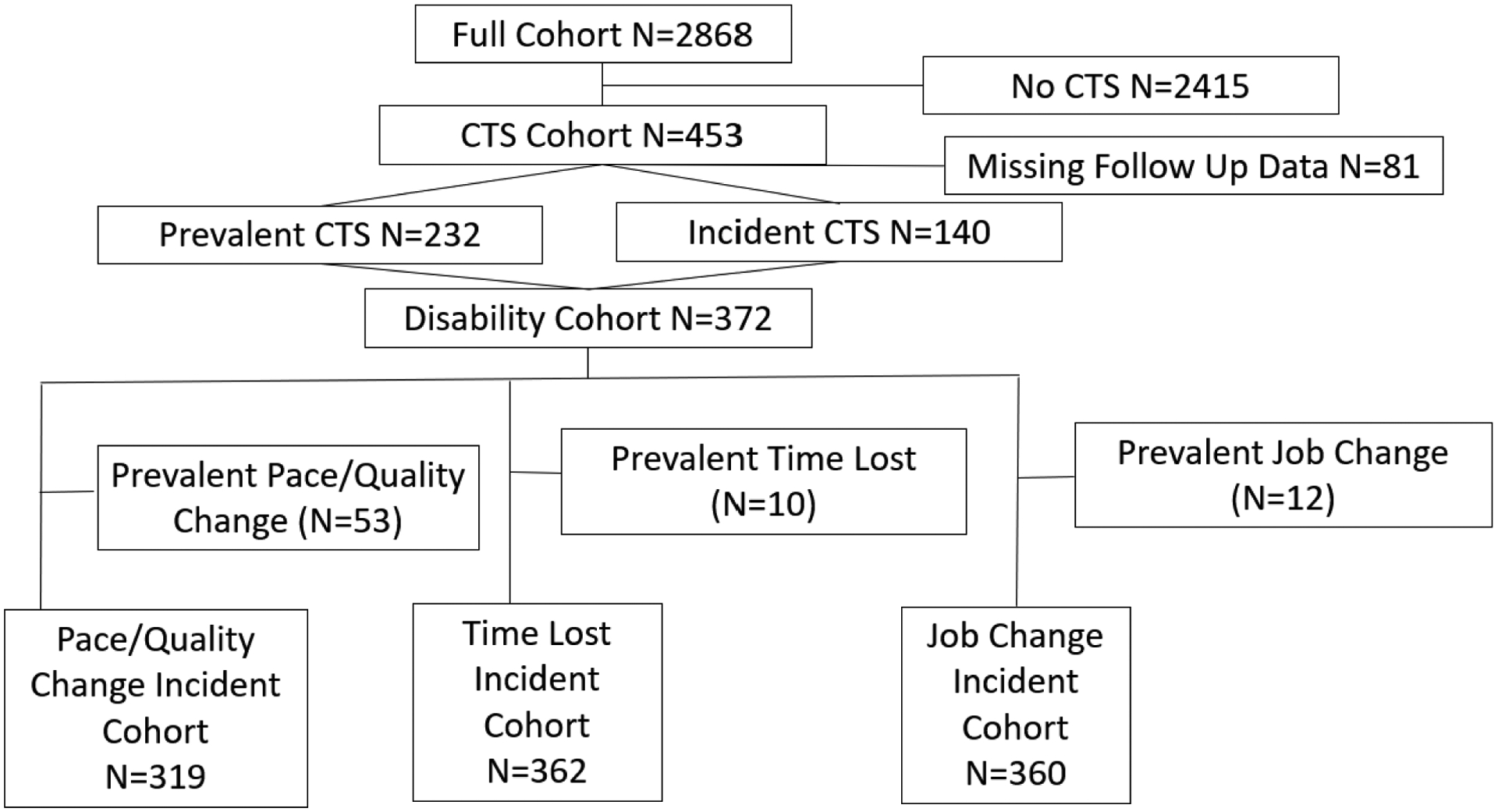
Subject flow chart of the cohort included in the analyses for pace/quality of work change, time lost and job change among those with CTS. Includes both incident and prevalent cases.
The case definition of CTS required positive symptoms(numbness, tingling, burning, or pain in one or more of the first three digits) AND positive temperature-adjusted latency criteria for median mononeuropathy at the wrist2,11. Participants with symptoms consistent with CTS and concurrent abnormal median and ulnar nerve EDS were classified as possible polyneuropathy and were censored at the time those criteria were met2.
Work Disability.
We defined three self-reported outcome measures of work disability following the development of CTS reflecting different degrees of severity of disability rank-ordered as follows: (i)a self-reported negative change in work pace or quality of work due to hand/wrist symptoms (level of agreement), (ii) lost time due to hand/wrist symptoms (days unable to work), and/or (iii)a job change due to hand/wrist symptoms within the same company (including light or restricted duty) or to a different one. Each measure of work disability was dichotomous (yes/no). Those reporting work disability at baseline were identified as prevalent disability cases (work pace/quality change, lost time, or job change) and excluded from incident analyses. The outcome for these analyses was one of the measures of incident work disability which occurred at the onset or after the worker met the case definition for CTS.
Individual Factors.
Individual factors such as gender, age, measured body mass index, medical co-morbidities and prior injuries were collected at baseline. Race, education, and work history were also collected at baseline.
Work Psychosocial Factors.
Elements from the Job Content Questionnaire (JCQ) were administered to collect information on work psychosocial factors at baseline. Four job strain “quadrants” were created by using the median split of the JCQ subscales(psychological job demand and decision latitude) to form 4 groups of job strain including high strain(high demand, low control), passive strain(low demand, low control), active strain(high demand, high control) and low strain(low demand, high control)12,13.
Biomechanical Exposure.
Baseline, task-level workplace exposure assessments were obtained for each worker. Exposure assessment typically included: worker interview, task observation by a trained ergonomist, workplace measurements of applied forces and tool and part weights, video recording, and video analyses7 Estimates included the highest hand force requirements for a task using the Borg CR-10 rating scale, a0-to-10-point scale ranging from “nothing at all” to “extremely strong” (Worker Rated Peak Hand Force; Analyst Rated Peak Hand Force). Estimates of the repetitiveness of a task used the HAL scale, a 0-to-10-point scale that has anchors describing the frequency of exertions and recovery. The 2018 ACGIH TLV for Hand Activity is a composite index that combines repetition (HAL scale) and peak hand force to calculate a peak force index(PFI) score for the action limit(PFIAL) and the threshold limit value(PFITLV). Temporal exertion patterns for repetition (Total Hand Repetition Rate; Forceful Hand Repetition Rate), duty cycle (% time All Exertions; % time Forceful Exertions) and posture (% time ≥30°Wrist Extension; % time ≥30°Wrist Flexion) were determined by detailed time studies of task-level videos10,14. Forceful exertions were those requiring ≥9N pinch force or ≥45N of power grip force or a Borg CR-10≥2. Exposure to hand vibration (yes/no) was recorded by the analyst for each. Exposures were measured at the individual task level at all study sites at the time of participant enrollment and measured again if the job changed8. An individual’s job level exposure was calculated as a time-weighted average of task exposures based on self-reported weekly time spent performing each task.
Baseline Covariates.
Covariates known to be likely confounders such as age, gender, and body mass index, were included in every model. The other covariates considered for inclusion in the analyses were medical condition, ethnicity, highest education attained, prior distal UEMSD, time on the job at same company, smoking status, aerobic activity level, and non-aerobic hand intensive activity level.
Statistical Analysis.
Cox proportional hazard models with robust confidence intervals were used to estimate adjusted hazard ratios for personal, biomechanical, and work psychosocial factors and CTS-related incident work disability. Person-time accrued from the time the worker met the case definition of CTS. Mean, median, interquartile range(IQR), incidence rate(IR), hazard ratios(HR) and 95% confidence intervals(95% CI) were calculated. Biomechanical exposures were categorized by tertiles. Models were adjusted for confounding by personal factors (age, gender, BMI), study site and non-overlapping biomechanical exposures8. Confounding by additional covariates that were not mediators on the pathway from exposure to outcome was assessed by successively including and removing each from the model and retaining it if the primary exposure coefficient changed more than 10%.
Results
Among those included in this analysis(Figure 1), compared to the incident CTS cases (N=140 (38%)) those with prevalent CTS (N=232 (62%)) had a slightly higher mean age(2.3years), BMI(1.5kg/m2), and tenure (1.5years); additionally, there were slightly more females(6%) and report of a co-morbidity(7%). Overall, of the 372 workers included in the analysis, two-thirds were 40 years of age or older (50%=44.9 years; IQR: 36.0–52.0) (Table 1). The median year worked at enrollment was 6.5 years(IQR: 3.2–12.0). Table 2 summarizes exposures to biomechanical and psychosocial job factors. There were no significant differences between mean baseline exposure values between the prevalent and incident CTS cases, though the prevalent cases had slightly higher measures of repetition and duty cycle.
Table 1.
Socio-demographic characteristics and baseline health of the Carpal Tunnel Syndrome (CTS) Disability Cohort including those having CTS at baseline and those developing an Incident Case of CTS (n=372).*
| Demographics (n(%)) | Total N=372 |
|---|---|
| Gender | |
| Male | 126 (34%) |
| Female | 246 (66%) |
| Age (years) | |
| < 30 years of age | 45 (12%) |
| ≥ 30 & <40 years of age | 79 (21%) |
| ≥ 40 & <50 years of age | 138 (37%) |
| ≥ 50 years of age | 110 (30%) |
| Race/Ethnicity | |
| Caucasian | 213 (57%) |
| Hispanic/Latino | 44 (12%) |
| Black/African American | 37 (10%) |
| Asian | 17 (5%) |
| Other | 15 (4%) |
| Education | |
| Some high school or less | 52 (14%) |
| High school graduate or above | 315 (85%) |
| Handedness | |
| Left-handed | 35 (9%) |
| Right-handed | 337(91%) |
| Body Mass Index (kg/m 2 ) | |
| <25 | 71 (19%) |
| ≥25 & <30 (Overweight) | 115 (31%) |
| ≥30 (Obese) | 184 (50%) |
| General Health | |
| Very good or excellent | 142 (38%) |
| Good | 161 (43%) |
| Fair or poor | 53(14%) |
| Medical Condition | |
| No medical condition | 309 (83%) |
| Current medical condition | 63 (17%) |
| Diabetes mellitus | 24 (7%) |
| Rheumatoid arthritis | 17 (5%) |
| Thyroid disease (hyper/hypo) | 31 (8%) |
| Pregnancy | 0 (0%) |
| Previous Distal Upper Extremity Musculoskeletal Disorder (UEMSD) | |
| No previous Distal UEMSD | 204 (55%) |
| Previous Distal UEMSD | 77 (21%) |
| Smoking Status | |
| Never smoked | 188(51%) |
| Currently smokes | 96 (26%) |
| Previously smoked | 85 (23%) |
| Non-Occupational Weekly Aerobic Non-Hand Activity | |
| ≤3hr/wk | 91 (25%) |
| >3hr/wk | 114 (31%) |
| Non-Occupational Weekly Hand Intensive Activity | |
| ≤3hr/wk | 74 (20%) |
| >3hr/wk | 206 (55%) |
| Summary of Workplace Factors | |
| Years Worked at Enrollment | |
| ≤ 1year | 35 (10%) |
| >1 year & ≤ 3 years | 53 (15%) |
| >3 years & ≤ 7 years | 95 (26%) |
| >7years & ≤12 years | 104(29%) |
| >12 years | 73 (20%) |
| Job Satisfaction | |
| Very satisfied | 106 (29%) |
| Satisfied | 187 (50%) |
| Not satisfied (includes Neutral, Dissatisfied, Very Dissatisfied) | 67 (18%) |
remaining percentages represent missing data
Table 2.
Summary of baseline biomechanical and work psychosocial exposures.
| N | Mean (SD) | |
|---|---|---|
| FORCE MEASURES | ||
| Peak Borg CR-10: Worker’s rating (0 to 10 scale) | 346 | 3.9 (2.2) |
| Peak Borg CR-10: Analyst’s rating (0 to 10 scale) | 365 | 3.0 (1.7) |
| REPETITION MEASURES | ||
| Hand Activity Level (HAL) Scale: Analyst’s rating (0 to 10 scale) | 367 | 4.9 (1.7) |
| Total Repetition Rate* (reps/min) | 363 | 21.6 (15.7) |
| Forceful Repetition Rate* (reps/min) | 363 | 7.7 (10.1) |
| DUTY CYCLE | ||
| % Duration All Exertions* (0% to 100%) | 363 | 67.1 (18.4) |
| % Duration Forceful Exertions* (0% to 100%) | 363 | 22.4 (19.4) |
| POSTURE MEASURES | ||
| % Time ≥30°Wrist Flexion* (0% to 100%) | 360 | 4.2 (9.1) |
| % Time≥30°Wrist Extension* (0% to 100%) | 360 | 13.8 (20.6) |
| WORK PSYCHOSOCIAL MEASURES | ||
| Psychological DemandƗ | 182 | 31.9 (4.9) |
| Decision LatitudeƗ | 180 | 60.0 (8.5) |
| OTHER MEASURES | N | % |
| Vibration | ||
| None | 190 | 54.6 |
| Some | 158 | 45.4 |
| 2018 ACGIH TLV for Hand Activity | ||
| Lower Tertile (< PFIAL) | 72 | 19.8 |
| Middle Tertile (≥ PFIAL & < PFITLV) | 86 | 23.7 |
| Upper Tertile (≥ PFITLV) | 205 | 56.5 |
Direct measurements and/or from videotape analyses.
Domain of the Karasek Job Strain Index
Disability prevalence, incidence and time to disability onset after CTS.
Participants who met the criteria for a work disability at the time they met the CTS case definition were considered prevalent work disability cases (Figure 1); incident rates by disability varied(Table 3). The median time to onset of disability differed among those meeting the criteria for CTS at baseline (prevalent CTS cases) compared to those who developed incident CTS. Specifically, a change in work pace/quality was reported after a median interval of 521 days (IQR: 239–722) by prevalent CTS cases (n=114) compared to 155 days (IQR: 60 – 414) by incident CTS cases (n=43), lost work time was experienced after a median period of 459 days (IQR: 314–711) by prevalent CTS cases (n=72) compared to 227 days (IQR: 78–435) by incident CTS cases (n=25), and job change occurred after a median interval of 570 days (IQR: 244–729) among prevalent CTS cases (n=88) compared to 231 days (IQR: 116–535) among incident CTS cases (n=24).
Table 3.
Personal factors and risk of CTS-related work disability, hazard ratios and 95% confidence intervals adjusted for age, gender, BMI and consortium research site.
| PACE/QUALITY CHANGE (N=319; n=157; IR=33.2 per 100PYs) |
LOST TIME (N=362; n=97; IR=16.3 per 100 PYs) |
JOB CHANGE (N=360; n=112; IR=20.0 per 100 PYs;) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Cases(n) | HR | 95% CI | N | Cases(n) | HR | 95% CI | N | Cases(n) | HR | 95% CI | |
| Gender * | 317 | 155 | 360 | 97 | 358 | 110 | ||||||
| Male | 36 | 1.00 | 19 | 1.00 | 20 | 1.00 | ||||||
| Female | 119 | 1.27 | 0.85–1.89 | 78 | 1.13 | 0.67–1.92 | 90 | 1.47 | 0.9–2.39 | |||
| Age (years) ** | 317 | 155 | 360 | 97 | 358 | 110 | ||||||
| < 30 years of age | 18 | 1.00 | 8 | 1.00 | 12 | 1.00 | ||||||
| ≥30 & <40 years of age≥ | 34 | 0.79 | 0.42–1.46 | 20 | 1.02 | 0.45–2.31 | 26 | 0.94 | 0.43–2.05 | |||
| ≥40 & <50 years of age | 58 | 0.48 | 0.26–0.88 | 34 | 0.84 | 0.38–1.84 | 42 | 0.51 | 0.23–1.11 | |||
| ≥50 years of age | 45 | 0.54 | 0.29–0.99 | 35 | 1.18 | 0.55–2.52 | 30 | 0.49 | 0.22–1.08 | |||
| Ethnicity | 274 | 130 | 314 | 82 | 312 | 94 | ||||||
| Caucasian | 89 | 1.00 | 59 | 1.00 | 72 | 1.00 | ||||||
| Hispanic/Latino | 37 | 1.92 | 1.24–2.97 | 15 | 1.64 | 0.85–3.17 | 15 | 1.54 | 0.84–2.83 | |||
| Black/African American | 30 | 0.86 | 0.38–1.94 | -- | 0.00 | 0–0 | -- | 0.00 | 0–0 | |||
| Asian | 13 | 0.99 | 0.29–3.39 | -- | 0.00 | 0–0 | -- | 0.00 | 0–0 | |||
| Other | 13 | 0.98 | 0.39–2.49 | 8 | 0.65 | 0.31–1.38 | 7 | 0.52 | 0.22–1.25 | |||
| Education | 312 | 150 | 355 | 96 | 353 | 109 | ||||||
| Some high school or less | 17 | 1.00 | 13 | 1.00 | 8 | 1.00 | ||||||
| High school graduate or above | 133 | 0.89 | 0.55–1.45 | 83 | 0.68 | 0.37–1.25 | 101 | 1.54 | 0.79–3.01 | |||
| Handedness | 317 | 155 | 360 | 97 | 358 | 110 | ||||||
| Left handed | 13 | 1.00 | 10 | 1.00 | 8 | 1.00 | ||||||
| Right handed | 142 | 1.78 | 1.06–2.99 | 87 | 1.17 | 0.66–2.06 | 110 | 2.11 | 1.12–3.98 | |||
| Body Mass Index (kg/m 2 ) | 317 | 155 | 360 | 97 | 358 | 110 | ||||||
| <25 | 24 | 1.00 | 11 | 1.00 | 22 | 1.00 | ||||||
| ≥25 & <30 (Overweight) | 54 | 1.30 | 0.83–2.03 | 29 | 1.88 | 0.88–4.0 | 33 | 0.80 | 0.46–1.39 | |||
| ≥30 (Obese) | 77 | 1.11 | 0.58–2.13 | 57 | 3.40 | 1.31–8.8 | 55 | 0.60 | 0.27–1.31 | |||
| General Health | 305 | 145 | 346 | 93 | 343 | 106 | ||||||
| Very good or excellent | 57 | 1.00 | 40 | 1.00 | 47 | 1.00 | ||||||
| Good | 63 | 1.25 | 0.86–1.82 | 40 | 1.09 | 0.70–1.72 | 43 | 1.02 | 0.66–1.6 | |||
| Fair or poor | 25 | 1.80 | 1.12–2.88 | 13 | 1.37 | 0.64–2.91 | 16 | 1.69 | 1.00–2.86 | |||
| Comorbidity | 317 | 155 | 360 | 97 | 358 | 110 | ||||||
| No medical condition | 124 | 1.00 | 74 | 1.00 | 85 | 1.00 | ||||||
| Current medical condition | 31 | 0.91 | 0.61–1.36 | 23 | 1.01 | 0.62–1.64 | 25 | 1.01 | 0.65–1.58 | |||
| Diabetes mellitus | 9 | 0.70 | 0.31–1.58 | 8 | 1.12 | 0.55–2.29 | 7 | 0.71 | 0.31–1.63 | |||
| Rheumatoid arthritis | 12 | 1.50 | 0.79–2.85 | 9 | 1.40 | 0.71–2.74 | 7 | 0.92 | 0.41–2.05 | |||
| Thyroid disease | 14 | 0.70 | 0.43–1.14 | 12 | 1.01 | 0.54–1.9 | 15 | 1.13 | 0.7–1.83 | |||
| Previous Distal UEMSD | 252 | 137 | 272 | 87 | 271 | 100 | ||||||
| No previous Distal UEMSD | 94 | 1.00 | 54 | 1.00 | 72 | 1.00 | ||||||
| Previous Distal UEMSD | 43 | 1.20 | 0.82–1.75 | 33 | 1.29 | 0.82–2.01 | 28 | 0.90 | 0.57–1.42 | |||
| Smoking Status | 315 | 154 | 357 | 97 | 355 | 110 | ||||||
| Never smoked | 77 | 1.00 | 52 | 1.00 | 56 | 1.00 | ||||||
| Currently smokes | 40 | 1.17 | 0.78–1.77 | 20 | 0.82 | 0.46–1.45 | 29 | 1.32 | 0.80–2.18 | |||
| Previously smoked | 37 | 1.10 | 0.74–1.66 | 25 | 0.97 | 0.60–1.56 | 25 | 1.01 | 0.62–1.64 | |||
| Non-occupational weekly Aerobic Non-Hand Activity | 189 | 123 | 202 | 85 | 197 | 95 | ||||||
| ≤3hr/wk | 56 | 1.00 | 25 | 1.00 | 43 | 1.00 | ||||||
| >3hr/wk | 67 | 0.70 | 0.49–1.00 | 60 | 1.88 | 1.18–3.00 | 52 | 0.73 | 0.48–1.11 | |||
| Non-occupational weekly Hand Intensive Activity | 250 | 136 | 271 | 87 | 270 | 100 | ||||||
| ≤3hr/wk | 28 | 1.00 | 10 | 1.00 | 14 | 1.00 | ||||||
| >3hr/wk | 108 | 0.92 | 0.60–1.41 | 77 | 2.09 | 1.06–4.13 | 86 | 1.57 | 0.90–2.75 | |||
| Summary of Workplace Factors | ||||||||||||
| Years Worked at Enrollment | 312 | 150 | 355 | 96 | 353 | 108 | ||||||
| ≤1year | 9 | 1.00 | 7 | 1.00 | 6 | 1.00 | ||||||
| >1 year & ≤3 years | 13 | 1.73 | 0.65–4.60 | 7 | 0.63 | 0.23–1.73 | 12 | 3.98 | 1.38–11.44 | |||
| >3 years & ≤7 years | 56 | 2.33 | 1.06–5.09 | 38 | 1.20 | 0.53–2.71 | 34 | 2.26 | 0.83–6.18 | |||
| >7years & ≤12 years | 40 | 2.00 | 0.88–4.53 | 28 | 0.74 | 0.31–1.76 | 31 | 3.03 | 1.08–8.53 | |||
| >12 years | 32 | 2.21 | 0.93–5.24 | 16 | 0.42 | 0.16–1.08 | 25 | 3.17 | 1.05–9.56 | |||
| Job Satisfaction | 308 | 147 | 350 | 95 | 347 | 108 | ||||||
| Very satisfied | 27 | 1.00 | 19 | 1.00 | 19 | 1.00 | ||||||
| Satisfied | 82 | 1.69 | 1.09–2.62 | 50 | 0.89 | 0.50–1.58 | 61 | 1.57 | 0.94–2.63 | |||
| Not satisfied | 38 | 2.02 | 1.21–3.37 | 26 | 1.24 | 0.67–2.29 | 28 | 1.60 | 0.86–3.00 | |||
adjusted only for age, BMI and consortium research site
adjusted only for gender, BMI and consortium research site
Socio-demographic factors, baseline health status, and disability incidence.
Regardless of outcome measure, females had non-significant, modestly higher rates of work disability than males(Table 3), and older age was associated with lower rates of work disability. Hispanics experienced higher disability rates than other ethnic groups and having a high BMI more than tripled the rate of lost time following CTS.
Work history, biomechanical exposures, psychosocial job factors and disability incidence.
Measures of hand repetition, such as a HAL of more than 4 or a total hand repetition rate of more than 13.6 reps/minute or spending more than 76% of time in any hand exertion, or spending more than 29% of time in forceful hand exertion increased the rate of a job change (Table 4).
Table 4.
Biomechanical and psychosocial job factors and risk of CTS-related work disability, hazard ratios and 95% confidence intervals adjusted for age, gender, BMI and consortium research site.
| PACE/QUALITY CHANGE | LOST TIME | JOB CHANGE | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cutoffs | Cohort (N) | Cases (n) | HR | 95%CI | Cohort (N) | Cases (n) | HR | 95%CI | Cohort (N) | Cases (n) | HR | 95%CI | |
| FORCE MEASURES (adj. for total repetition rate, % duration all exertions, % Time ≥30°WristFlexion) | |||||||||||||
| Peak Borg CR-10: Worker (0 to 10 scale) | 276 | 142 | 309 | 89 | 305 | 105 | |||||||
| Lower Tertile | ≤3 | 48 | 1.00 | 31 | 1.00 | 35 | 1.00 | ||||||
| Middle Tertile | >3 & ≤4.5 | 46 | 1.24 | 0.81–1.92 | 27 | 1.07 | 0.62–1.85 | 36 | 1.17 | 0.71–1.93 | |||
| Upper Tertile | >4.5 | 48 | 1.09 | 0.72–1.65 | 31 | 1.15 | 0.67–1.99 | 34 | 1.14 | 0.69–1.91 | |||
| Peak Borg CR-10: Analyst (0 to 10 scale) | 287 | 144 | 323 | 89 | 320 | 105 | |||||||
| Lower Tertile | ≤2.3 | 46 | 1.00 | 26 | 1.00 | 35 | 1.00 | ||||||
| Middle Tertile | >2.3 & ≤3.8 | 58 | 1.17 | 0.74–1.84 | 36 | 1.14 | 0.66–1.97 | 39 | 0.91 | 0.54–1.56 | |||
| Upper Tertile | >3.8 | 40 | 0.99 | 0.62–1.59 | 27 | 1.43 | 0.81–2.56 | 31 | 1.25 | 0.70–2.25 | |||
| REPETITION MEASURES (adj. for Analyst Rated Peak CR-10, % Time ≥30°WristFlexion) | |||||||||||||
| Hand Activity Level (HAL Scale: Analyst (0 to 10 scale) | 287 | 145 | 323 | 89 | 320 | 105 | |||||||
| Lower Tertile | ≤4 | 41 | 1.00 | 24 | 1.00 | 18 | 1.00 | ||||||
| Middle Tertile | >4 & ≤6 | 71 | 1.45 | 1.00–2.13 | 37 | 0.84 | 0.48–1.48 | 56 | 2.37 | 1.34–4.21 | |||
| Upper Tertile | >6 | 33 | 1.09 | 0.68–1.77 | 28 | 1.17 | 0.67–2.06 | 31 | 2.17 | 1.18–4.02 | |||
| Total Repetition Rate (reps/min) | 287 | 144 | 323 | 89 | 320 | 105 | |||||||
| Lower Tertile | ≤13.6 | 40 | 1.00 | 20 | 1.00 | 21 | 1.00 | ||||||
| Middle Tertile | >13.6 & ≤24.0 | 50 | 1.36 | 0.90–2.09 | 37 | 1.43 | 0.81–2.54 | 40 | 1.87 | 1.09–3.23 | |||
| Upper Tertile | >24.0 | 54 | 1.20 | 0.79–1.85 | 32 | 1.45 | 0.82–2.58 | 44 | 1.75 | 1.02–3.02 | |||
| Forceful Repetition Rate* (reps/min) | 293 | 145 | 329 | 89 | 326 | 105 | |||||||
| Lower Tertile | ≤2.3 | 41 | 1.00 | 25 | 1.00 | 26 | |||||||
| Middle Tertile | >2.3& ≤8.1 | 49 | 1.09 | 0.70–1.72 | 30 | 1.44 | 0.82–2.55 | 33 | 1.14 | 0.66–2.00 | |||
| Upper Tertile | >8.1 | 55 | 1.28 | 0.79–2.09 | 34 | 1.36 | 0.81–2.30 | 46 | 1.62 | 0.94–2.80 | |||
| DUTY CYCLE (adj. for Analyst Rated CR-10, % Time ≥30°Wrist Flexion) | |||||||||||||
| % Duration All Exertions (0 to 100%) | 287 | 144 | 323 | 89 | 320 | 105 | |||||||
| Lower Tertile | ≤58.6 | 44 | 1.00 | 29 | 1.00 | 27 | 1.00 | ||||||
| Middle Tertile | >58.6 & ≤75.8 | 46 | 0.90 | 0.61–1.36 | 30 | 0.96 | 0.56–1.65 | 43 | 1.82 | 1.09–3.06 | |||
| Upper Tertile | >75.8 | 54 | 1.62 | 1.03–2.56 | 30 | 1.15 | 0.69–1.93 | 35 | 2.20 | 1.22–4.01 | |||
| % Duration Forceful Exertions* (0 to 100%) | 293 | 145 | 329 | 89 | 326 | 105 | |||||||
| Lower Tertile | ≤11.0 | 39 | 1.00 | 27 | 1.00 | 28 | 1.00 | ||||||
| Middle Tertile | >11.0 & ≤28.6 | 52 | 1.29 | 0.83–2.02 | 27 | 1.17 | 0.68–2.06 | 33 | 1.12 | 0.65–1.96 | |||
| Upper Tertile | >28.6 | 54 | 1.51 | 0.95–2.41 | 35 | 1.38 | 0.83–2.33 | 44 | 1.74 | 1.02–2.98 | |||
| POSTURE MEASURES (adj. for Analyst Rated CR-10, total repetition rate, % duration all exertions) | |||||||||||||
| % Time ≥30°Wrist Extension (0 to 100%) | 287 | 144 | 323 | 89 | 320 | 105 | |||||||
| Lower Half | ≤3.3 | 66 | 1.00 | 45 | 1.00 | 45 | 1.00 | ||||||
| Upper Half | >3.3 | 78 | 1.04 | 0.72–1.50 | 44 | 0.84 | 0.52–1.35 | 60 | 1.11 | 0.72–1.73 | |||
| % Time ≥30° Wrist Flexion (0 to 100%) | 287 | 144 | 323 | 89 | 320 | 105 | |||||||
| Lower Half | ≤0.8 | 76 | 1.00 | 42 | 1.00 | 48 | 1.00 | ||||||
| Upper Half | >0.8 | 68 | 0.93 | 0.66–1.33 | 47 | 1.00 | 0.65–1.57 | 57 | 1.26 | 0.83–1.91 | |||
| OTHER (adj. for Analyst Rated Peak CR-10, total repetition rate, % duration all exertions, % Time ≥30°Wrist Flexion) | |||||||||||||
| Vibration | 276 | 139 | 306 | 88 | 303 | 104 | |||||||
| None | ≤0 | 61 | 1.00 | 32 | 1.00 | 43 | 1.00 | ||||||
| Some | >0 | 78 | 0.84 | 0.57–1.24 | 56 | 1.05 | 0.67–1.66 | 61 | 0.88 | 0.57–1.38 | |||
| 2018 ACGIH TLV for Hand Activity | 287 | 145 | 323 | 89 | 320 | 105 | |||||||
| Lower Tertile | < PFIAL | 20 | 1.00 | 14 | 1.00 | 13 | 1.00 | ||||||
| Middle Tertile | ≥ PFIAL & < PFITLV | 43 | 1.24 | 0.70–2.22 | 20 | 0.79 | 0.40–1.56 | 28 | 1.02 | 0.50–2.07 | |||
| Upper Tertile | ≥ PFITLV | 82 | 1.37 | 0.79–2.39 | 55 | 1.27 | 0.72–2.25 | 64 | 1.56 | 0.80–3.04 | |||
| WORK PSYCHOSOCIAL EXPOSURES | |||||||||||||
| Psychological Job Demands** | 142 | 38 | 175 | 12 | 176 | 16 | |||||||
| Low Demands | <32 | 15 | 1.00 | 4 | 1.00 | 4 | 1.00 | ||||||
| High Demands | ≥32 | 23 | 1.53 | 0.82–2.89 | 8 | 2.15 | 0.60–7.73 | 12 | 3.39 | 1.04–11.08 | |||
| Decision Latitude | 141 | 38 | 173 | 12 | 174 | 16 | |||||||
| Low Latitude | <60 | 20 | 1.00 | 8 | 1.00 | 9 | 1.00 | ||||||
| High Latitude | ≥60 | 18 | 0.64 | 0.33–1.28 | 4 | 0.32 | 0.11–1.01 | 7 | 0.45 | 0.16–1.28 | |||
| Job Strain | 141 | 38 | 173 | 12 | 174 | 16 | |||||||
| Low Strain | 9 | 1.00 | 2 | 1.00 | 2 | 1.00 | |||||||
| Passive Strain | 9 | 1.12 | 0.45–2.81 | 2 | 1.75 | 0.27–11.39 | 5 | 3.18 | 0.64–15.98 | ||||
| Active Strain | 6 | 1.09 | 0.41–2.95 | 2 | 2.83 | 0.45–18.2 | 2 | 2.09 | 0.33–13.29 | ||||
| High Strain | 14 | 2.15 | 0.95–4.91 | 6 | 4.82 | 1.04–22.54 | 7 | 6.58 | 1.27–34.25 | ||||
only adjusted for posture (% Time ≥30°WristFlexion)
Not all research sites in the consortium had compatible psychosocial data and thus the cohort having both biomechanical exposure and work psychosocial data was smaller than the main cohort. Nevertheless, among those with lost time or job change, 6 out of 12 (50%) and 7 out of 16 (44%) cases had high job strain, respectively, yet only 2 individuals in each model had low job strain (Table 4).
A sensitivity analysis indicates that the incident CTS cases had consistently higher effect estimates than the prevalent CTS cases, despite wide confidence intervals due to a limited number of incident disability cases. For example, those with middle and high percent time in forceful exertion had a 2.37(95%CI:0.62–9.05) and 3.04(95%CI:0.94–9.84) increased in the rate of a job change compared to the prevalent CTS who had rates of 0.92(95%CI:0.49–1.72) and 1.51(95%CI:0.82–2.79).
Discussion
This prospective cohort study of workers with CTS found that the incidence of those with CTS experiencing new changes in work pace/quality was much higher (33.2/100-pyrs) than the incidence of those who experienced lost time (16.3/100-pyrs) or job changes (20.0/100-pyrs) due to CTS. Changes in pace and quality of work are likely to precede lost time or job changes, and these self-reported difficulties in performing job tasks might continue for some time before a change in job duties or the inability to perform the job occurred. Another potential explanation for these findings is that the inconveniences and financial and other penalties associated with lost time resulted in that measure being lowest.
An important finding of this research was how non-occupational risk factors differed considerably for the three measures of disability. In contrast to prior studies15,16, being older was not associated with increased risk of CTS-related disability. In fact, workers older than 40 years reported a reduced rate of changes in work pace or quality or job changes. However, consistent with prior studies, women and workers with self-reported rheumatoid arthritis did have trends in increased rates of CTS-related disability7,17. Workers who reported their health as ‘fair’ or ‘poor’ had a 70–80% increased rate in changes in work pace/quality or job change and obese workers had a higher rate of lost time due to CTS, but not pace/quality change or job change.
In a prior paper, we found that greater time in non-occupational hand intensive activity was associated with a lower risk of developing CTS7. In the current analyses, baseline hand intensive exposures outside of and during work were associated with a higher incidence of subsequent disability. There are various possible explanations for these seemingly disparate findings beyond a potentially spurious result. One explanation is that the risks for the development of CTS are not the same as those that produce disability. Another explanation is that, regardless of disease or symptoms, there is a minimal level of hand intensive activities that cannot be reduced, particularly among women caring for dependents in the home since activities of daily living were included as non-occupational hand intensive activity. Perhaps those caring for dependents may not have any alternatives to performing offhand intensive activities in the home, thus leading to lost time at work.
Workers with longer tenure at baseline tended to have reduced rates of CTS-related disability than those who worked for shorter durations. In fact, individuals who worked more than 12 years had a 58% reduction in the rate of lost time following CTS. Perhaps these workers had a greater ability to influence their work given their tenure. Alternatively, perhaps these workers represented a healthier population and were able to continue working despite their condition either due to greater ability to adapt to symptoms over time and/or potentially having milder symptoms.
Consistent with prior analyses on CTS incidence17, work psychosocial factors such as job dissatisfaction and job strain were independently associated with disability following CTS. However, associations with disability were much stronger; in fact, high job strain was the strongest predictor of severe disability outcomes, with a 4-fold increased rate of lost time and a 6.5-fold increased rate of job change. High psychological job demands increased disability independent from biomechanical factors and high decision latitude on the job appeared to protect workers though confidence intervals were wide. Similar to studies of low back pain6, increased job strain may increase the rate of disability following CTS, suggesting that reducing job strain may be an early intervention strategy to prevent costly work disability.
In stark contrast to prior analyses on CTS incidence, peak force estimates showed weak positive associations with disability8. This suggests that while peak force contributes to the development of CTS, once a person has CTS, other factors become relatively more important contributors to disability. This is in line with the phase model of disability18,19 and previous research demonstrating that risk factors for MSD incidence may differ from those for work disability and specific durations or phases of work disability6. It is also consistent with a substantial body of research suggesting disability is strongly related to psychosocial issues, although that literature is mostly related to spine pain20–22, and with the pyramid model of disability where different risk factors influence the transition between different states of injury and disability23.
In this regard, perhaps a more important finding from this study was the association between measures of total repetition rate, the % time spent in any hand exertion and some of the measures of disability. These measures were not strongly associated with incident CTS in our prior analyses8, yet they were associated with disability following CTS. This suggests that once a person meets a CTS case definition, stay-at-work and return-to-work strategies that reduce total repetition and the % time spent in any hand exertion(light or heavy) may reduce some of the measures of future disability. Regardless, it should be noted that these findings suggest that force is still an important predictor of CTS disability when it also includes a measure of duration. The TLV for Hand Activity has performed well as a predictor of incident CTS and may be useful as a surveillance tool3,9. These findings suggest that separately tracking hand activity levels as a part of surveillance efforts may be useful in building proactive strategies for preventing disability following CTS among workers in high-risk groups.
Study results regarding disability from CTS are similar to what is seen in clinical practice. Our study used a clinically-relevant case definition for CTS that requires both symptoms of median neuropathy and electrodiagnostic studies showing slowing of conduction in the median nerve at the wrist11. Our study found a greater chance of disability among workers with CTS who had more hand intensive activities at work. This finding has been seen in other studies24, is commonly seen in clinical practice, and is reflected in clinical guidelines that recommend modifying work to decrease hand intensive activities among patients with CTS. Our study found that workers with CTS reported decreased pace or quality of work, a finding seen in other studies, where CTS patient reported decreased functional abilities25 including symptoms that interfered with production rates and/or quality of work26. Clinically, loss of work capacity is commonly seen before the outcomes of lost work or change in jobs.
Strengths and Limitations.
The pooling of data from four cohort studies that included workers from different industries provides one of the largest and most diverse prospective cohort studies ever assembled for examining risk factors for work disability due to CTS and allows for greater generalizability than any single study sample. The large cohort increases precision of point-estimates and allows for exploration of exposure-outcome relationships and thresholds of risk while adjusting for important covariates.
Despite the large size of the pooled cohort, there were not enough incident CTS cases to restrict these analyses to only those workers with incident CTS. Thus, individuals who had CTS at the inception of the cohort(and who subsequently developed CTS-related work disability) were also included. These prevalent CTS workers were likely to be either: (i)at a later stage of disease progression, (ii)be chronic cases, and/or (iii)survivors somehow able to maintain work ability despite having CTS. However, a sensitivity analysis that included only the incident CTS cases showed the same patterns of association and with larger effect estimates indicating attenuation of the rates reported in this analysis of combined CTS incident and prevalent cases. Psychosocial job factors were not assessed at all workplaces and this reduced the number of individuals who had information on both biomechanical and psychosocial measures. Additionally, some studies only assessed psychosocial stress at baseline; thus, only baseline measurements are included in this analysis. Despite this limitation, strong independent effects of low job satisfaction on changes in work pace or quality and of job strain on lost time and job change were found. A much larger sample size would have been needed to determine interaction effects between biomechanical and work psychosocial exposures.
Reliance on self-reported measures of disability and varying intervals of assessment across study sites may have introduced varying amounts of recall or reporting bias; however, this limitation probably applies only to changes in work quality or pace and less to lost work time or job change. Further, the inclusion of prevalent CTS cases at baseline may have led to increased recall bias for those individuals and/or may have contributed to bias from the healthy worker survivor effect. In essence, those with CTS at baseline may have been a healthier cohort that could sustain work despite progressing disease than those who may have already left the workplace thereby leading to an underestimation of effect estimates. Additionally, we did not collect information related to workers compensation claim status or treatment. Therefore, we cannot make any inferences about how CTS management influences CTS-related work disability. Finally, while all three outcomes are plausible, if not likely consequences of CTS, they were not necessarily collected for studying CTS-related disability per se. Thus, the non-specific nature of the work disability questionnaire items which related the incidence of disability to any hand/wrist discomfort and not CTS specifically may have led to inclusion of disability related to concurrent hand/wrist tendinitis with CTS. alone.
Future Research.
Our results indicate that effective strategies to prevent CTS-related disability need to include both ergonomic and organizational job redesign. Development of rapid and low-cost alternative technology that reliably and accurately measures biomechanical exposures may improve feasibility and expand the impact of such interventions.
Conclusion
To our knowledge, this is the first large prospective cohort study to estimate associations between biomechanical, work psychosocial, and personal factors and subsequent CTS-related work-disability based on rigorous case criteria and individualized exposure assessment. Understanding the risk factors associated with work disability among those with CTS is necessary to design comprehensive intervention strategies for those most likely to develop subsequent work disability. The results of the current study show that reducing total repetition rate and the % time spent in any (light & heavy) hand exertion may reduce the risk of some measures of subsequent disability among those with CTS. The inclusion of prevalent CTS cases in this analysis attenuated the effect estimates reported. The results also suggest that increasing job satisfaction as well as lowering job strain by increasing decision latitude at work and reducing psychological job demands may be important organizational strategies to reduce risk of subsequent work disability.
KEY MESSAGES.
What is already known about this subject?
Although studies have shown the associations between risk factors and incident carpal tunnel syndrome (CTS), few large prospective studies using rigorous case criteria, individual-level exposure data, and appropriate controls for confounding have examined associations between various types of risk factors and disability due to CTS.
What are the new findings?
Although prior analyses found that various measures of force but not repetition, per se, were strongly associated with incident CTS, measures of repetitive hand activity and duration of all (light and heavy) hand exertions were associated with increased work disability following CTS.
Furthermore, low job satisfaction and high job strain increased the rate of work disability following CTS.
How might this impact on policy or clinical practice in the foreseeable future?
Understanding risk factors associated with work disability is important to developing effective intervention strategies for preventing disability once someone develops CTS. These observations suggest that tertiary prevention strategies may be most effective when they reduce both biomechanical exposures and work psychosocial stress.
Acknowledgements:
The authors would like to acknowledge Dr. Arun Garg, Dr. Barbara Silverstein, and Dr. Susan Burt and Linda Merlino who were previously part of the ULMSD Consortium. Additionally, we would like to thank the numerous students and researchers who collaborated on various aspects of the Consortial studies, the numerous employers who provided access to the workplace and the thousands of workers for their time and participation.
Funding Acknowledgement:
These consortial data were collected at multiple consortial sites and used many sources of support that include research grants, training grants and other funding sources. These include 1U01OH007917-01, 1R01OH07914-01, 1R01OH009712-01, 1R01OH010474-01, UL1RR-24992, T42/CCT810426-10, 3TC42OH008414, and T42OH008429. Additionally, the data collection, data abstraction, data reduction, analyses and other activities required major support beyond usual funding mechanisms including state funds, donations, and extensive In-kind support.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
References
- 1.Foley M; Silverstein B; Polissar N The Economic Burdens of Carpal Tunnel Syndrome: Long-Term Earnings of CTS Claimants in Washington State. Am J Ind Med. 2007;50:155–172. doi: 10.1002/ajim.20430. [DOI] [PubMed] [Google Scholar]
- 2.Dale AM, Harris-Adamson C, Rempel D, et al. Prevalence and incidence of carpal tunnel syndrome in US working populations: Pooled analysis of six prospective studies. Scand J Work Environ Health. 2013;39(5). doi: 10.5271/sjweh.3351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonfiglioli R, Mattioli S, Armstrong TJ, et al. Validation of the ACGIH TLV for hand activity level in the OCTOPUS cohort: A two-year longitudinal study of carpal tunnel syndrome. Scand J Work Environ Health. 2013;39(2):155–163. doi: 10.5271/sjweh.3312 [DOI] [PubMed] [Google Scholar]
- 4.Violante FS, Farioli A, Graziosi F, et al. Carpal tunnel syndrome and manual work: the OCTOPUS cohort, results of a ten-year longitudinal study. Scand J Work Environ Health. 2016;42(4):280–290. doi: 10.5271/sjweh.3566 [DOI] [PubMed] [Google Scholar]
- 5.Bureau of Labor Statistics. Nonfatal Occupational Injuries and Illnesses Requiring Days Away from Work. Published online 2018.
- 6.Krause N, Dasinger LK, Deegan LJ, Rudolph L, Brand RJ. Psychosocial job factors and return-to-work after compensated low back injury: A disability phase-specific analysis. Am J Ind Med. 2001;40(4):374–392. doi: 10.1002/ajim.1112 [DOI] [PubMed] [Google Scholar]
- 7.Harris-Adamson C, Eisen EA, Dale AM, et al. Personal and Workplace psychosocial risk factors for carpal tunnel syndrome: A pooled study cohort. Occup Environ Med. 2013;70(8). doi: 10.1136/oemed-2013-101365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris-Adamson C, Eisen EA, Kapellusch J, et al. Biomechanical risk factors for carpal tunnel syndrome: A pooled study of 2474 workers. Occup Environ Med. 2015;72(1). doi: 10.1136/oemed-2014-102378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kapellusch JM, Gerr FE, Malloy EJ, et al. Exposure-response relationships for the ACGIH threshold limit value for handactivity level: Results from a pooled data study of carpal tunnel syndrome. Scand J Work Environ Health. 2014;40(6). doi: 10.5271/sjweh.3456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kapellusch JM, Garg A, Bao SS, et al. Pooling job physical exposure data from multiple independent studies in a consortium study of carpal tunnel syndrome. Ergonomics. 2013;56(6):1021–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rempel D, Evanoff B, Amadio PC, et al. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am J Public Health. 1998;88(10):1447–1451. doi: 10.2105/AJPH.88.10.1447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karasek RA. Job Demands, Job Decision Latitude, and Mental Strain: Implications for Job Redesign. Adm Sci Q. 1979;24(2):285–308. doi: 10.2307/2392498 [DOI] [Google Scholar]
- 13.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. - PsycNET. J Od Occup Health Psychol. 3(4):322–355. [DOI] [PubMed] [Google Scholar]
- 14.Bao SS, Kapellusch JM, Garg A, et al. Developing a pooled job physical exposure data set from multiple independent studies: An example of a consortium study of carpal tunnel syndrome. Occup Environ Med. 2015;72(2):130–137. doi: 10.1136/oemed-2014-102396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abásolo L, Lajas C, León L, et al. Prognostic factors for long-term work disability due to musculoskeletal disorders. Rheumatol Int. 2012;32(12):3831–3839. doi: 10.1007/s00296-011-2264-5 [DOI] [PubMed] [Google Scholar]
- 16.Abásolo L, Carmona L, Lajas C, et al. Prognostic factors in short-term disability due to musculoskeletal disorders. Arthritis Care Res. 2008;59(4):489–496. doi: 10.1002/art.23537 [DOI] [PubMed] [Google Scholar]
- 17.Harris-Adamson C, Eisen EA, Neophytou A, et al. Biomechanical and psychosocial exposures are independent risk factors for carpal tunnel syndrome: Assessment of confounding using causal diagrams. Occup Environ Med. Published online 2016. doi: 10.1136/oemed-2016-103634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krause N, Frank JW, Dasinger LK, Sullivan TJ, Sinclair SJ. Determinants of duration of disability and return to work after work related injury and illness: Challenges for future research. Am J Ind Med. 2001;40(4):464–484. [DOI] [PubMed] [Google Scholar]
- 19.Krause N, Ragland DR. Occupational Disability Due to Low Back Pain: A New Interdisciplinary Classification Based on a Phase Model of Disability. Spine. 1994;19(9):1011–1020. [DOI] [PubMed] [Google Scholar]
- 20.Feuerstein M, Berkowitz SM, Haufler AJ, Lopez MS, Huang GD. Working with low back pain: Workplace and individual psychosocial determinants of limited duty and lost time¶*. Am J Ind Med. 2001;40(6):627–638. doi: 10.1002/ajim.10000 [DOI] [PubMed] [Google Scholar]
- 21.Carragee EJ, Alamin TF, Miller JL, Carragee JM. Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain. Spine J. 2005;5(1):24–35. doi: 10.1016/j.spinee.2004.05.250 [DOI] [PubMed] [Google Scholar]
- 22.Vargas-Prada S, Coggon D. Psychological and psychosocial determinants of musculoskeletal pain and associated disability. Best Pract Res Clin Rheumatol. 2015;29(3):374–390. doi: 10.1016/j.berh.2015.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Evanoff B, Dale AM, Descatha A. A conceptual model of musculoskeletal disorders for occupational health practitioners. Int J Occup Med Environ Health. 2014;27(1):145–148. doi: 10.2478/s13382-014-0232-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blanc PD, Faucett J, Kennedy JJ, Cisternas M, Yelin E. Self-reported carpal tunnel syndrome: Predictors of work disability from the National Health Interview Survey Occupational Health Supplement. Am J Ind Med. 1996;30(3):362–368. doi: [DOI] [PubMed] [Google Scholar]
- 25.Foley M, Silverstein B. The long-term burden of work-related carpal tunnel syndrome relative to upper-extremity fractures and dermatitis in Washington State. Am J Ind Med. 2015;58(12):1255–1269. doi: 10.1002/ajim.22540 [DOI] [PubMed] [Google Scholar]
- 26.Evanoff B, Gardner BT, Strickland JR, Buckner-Petty S, Franzblau A, Dale AM. Long term symptomatic, functional, and work outcomes of carpal tunnel syndrome among construction workers. Am J Ind Med. 2016;368:357–368. doi: 10.1002/ajim.22564 [DOI] [PMC free article] [PubMed] [Google Scholar]


