Abstract
Introduction
N95 respirators, together with eye protection, form vital elements of personal protective equipment (PPE) for healthcare workers (HCW) caring for patients with respiratory infections, such as COVID-19. Duckbill N95 respirators are widely used but have a high failure rate when Fit Tested. The commonest site for inward leaks is the region between the nose and maxilla. Safety goggles with an elastic headband may press the upper rim of the respirator against the face, thereby reducing inward leaks. We hypothesized that the use of safety goggles with an elastic headband will improve the overall fit-factor of a duckbill N95 respirator and increase the proportion of users who pass a quantitative Fit Test.
Methods
About 60 volunteer HCWs, who had previously failed quantitative Fit Testing with a duckbill N95 respirator, participated in this before-and-after intervention study. A PortaCount® 8048 was used for quantitative Fit Testing. The test was first performed with a duckbill N95 respirator only. It was then repeated after participants donned a pair of safety goggles (3M Fahrenheit, ID 70071531621).
Results
Before the intervention, i.e., with the respirator only, 8 (13.3%) participants passed their Fit Test. This increased to 49 (81.7%) after the application of safety goggles (OR 42, 95% CI 7.14–1697.9, p < 0.0001). The adjusted mean overall fit factor, using Tobit regression analysis, increased from 40.3 to 193.0 (t = 12.32, p < 0.001).
Conclusion
The use of safety goggles with an elastic headband significantly increases the proportion of users who pass a quantitative Fit Test and improves the fit-factor of a duckbill N95 respirator.
How to cite this article
Kamal M, Bhatti M, Stewart WC, Johns M, Collins D, Shehabi Y, et al. Safety Goggles with Elastic Headband to Improve N95 Fit Following Failed Quantitative Fit Test. Indian J Crit Care Med 2023;27(6):386–391.
Keywords: COVID-19, Eye protection, Fit Test, Goggles, N95 respirators, Personal protective equipment
Highlights
Ill-fitting N95 respirators are health risk for healthcare workers caring for patients with respiratory illness like COVID-19. The gap between the skin and respirator near the nasolabial fold commonly allows air leak. Safety goggles with an elastic wrap-around headband that presses the superior margin of the respirator against the face may improve N95 respirator seal.
Introduction
N95 respirators are crucial items of personal protective equipment (PPE) for healthcare workers (HCWs) looking after patients with coronavirus disease of 2019 (COVID-19) or other respiratory infections for which droplet or airborne precautions are required. Their use is recommended by the World Health Organization (WHO) and the Australian Department of Health (ADH).1,2 The respirators are so-called because they are certified to block at least 95% of particles larger than 0.3 μM in non-oily conditions. N95 respirators are available in different designs and sizes. Facial morphology varies with race, body habitus, weight, age, and sex. Therefore, it is recommended that the N95 respirator be Fit Tested prior to use.1–3
Healthcare workers caring for patients with COVID-19 are at risk of contracting SARS-CoV-2, the virus responsible for the disease. There is evidence to suggest that compared to the general community, frontline HCWs have a higher risk of testing positive for COVID-19.4–6 Therefore, ensuring HCW protection from the contraction of SARS-CoV-2 is paramount.
Quantitative Fit Testing (QnFT) using a particle counter is a recognized, accurate method of ensuring that a respirator fits a person's face with a good seal and has been shown to be superior in the detection of leaks compared with qualitative Fit Testing.7–10 A PortaCount® Respirator Fit Tester (Fig. 1) can be used to perform a QnFT. It counts the particles inside and outside of the respirator and calculates a ratio, termed the fit-factor. The HCW undergoing Fit Testing then performs several physical maneuvers designed to mimic bedside behaviors that may alter the seal offered by the respirator. Fit-factor is calculated during each such exercise. An overall fit-factor score of ≥100, accommodating for all exercises in a Fit Test, is considered a “pass” and recognized as an adequate level of protection from infectious agents such as SARS-CoV-2.3,11
Fig. 1.
PortaCount Respirator Fit Tester 8048 | TSI
Duckbill N95 respirators (Fig. 2) are widely used around the world. The ADH and New South Wales Clinical Excellence Commission recommend that all HCWs using N95 respirators be Fit Tested prior to their use.2,3 Healthcare workers who fail a Fit Test with a duckbill respirator must use an alternative. These may include a different model of N95 respirator or a Powered Air Purifying Respirator (PAPR). The latter does not rely on fitting but is expensive, complicated to donn, and not commonly available.
Fig. 2.
Proshield® duckbill N95 respirator | BSN Medical
In addition to a respirator, it is now increasingly recognized that eye protection with safety goggles or a face shield should be used when caring for patients with respiratory infections like COVID-1912—a recommendation echoed by the WHO and the ADH.
Duckbill N95 respirators are widely used but have a high failure rate when Fit Tested.13 It has been found that the commonest site for a poor seal is the upper rim of the respirator between the nasal and maxillary region, as illustrated in panel “A”, Figure 3.14,15 Safety goggles with a wraparound elastic headband, as shown in Figure 4, are widely available. When worn with a duckbill N95 respirator, the lower margin of the safety goggles presses the upper rim of the respirator against the face, which may improve the seal, in addition to providing eye protection.
Fig. 3.
(A) Demonstrates the common site of inward leak for an N95 respirator; (B) Shows the modified N95 respirator and safety goggles pressing the gap between the nose and the cheeks
Fig. 4.

Fahrenheit antifog safety goggles | 3M
We have previously shown that in a group of unselected participants, the proportion of participants who passed a Fit Test with a duckbill N95 respirator was 27%.16,17 This number rose to 73% when safety goggles with a wraparound elastic headband were worn with the respirator. That study was an unpowered pilot investigation in an unselected group using two types of duckbill N95.
Here, we performed a follow-up, prospective, powered study to determine the impact of the use of safety goggles with an elastic headband on Proshield® duckbill N95 respirator fit in HCWs who have previously failed QnFT. For this study, we used 3M Fahrenheit googles (Fig. 4). We hypothesized that the use of these safety goggles will improve the fit-factor of the N95 respirator, and a significant proportion of participants would then pass their Fit Test.
Methods
The study was approved by the South Eastern Sydney Local Health District Human Research and Ethics Committee (2021/ETH11680). All participants received a Participant Information Sheet and written informed consent was obtained prior to testing. We performed a prospective before-and-after study. Quantitative Fit Testing was performed with an N95 respirator only and again with the respirator and goggles.
Participants
All participants worked at the Prince of Wales Hospital, Sydney, Australia. Participation in the study was voluntary. The participants were HCWs that had previously failed a quantitative Fit Test with the Proshield® duckbill N95 respirator. Data were collected between November and December 2021. Male participants shaved their facial hair on the day of their participation. Any HCW who previously had an adverse reaction to isopropyl alcohol was excluded.
Testing Process
Testing was carried out in accordance with the manufacturer guidelines.18 The testing process for this study is outlined in Figure 5. All participants were tested with a Proshield® duckbill N95 respirator shown in Figure 2 (BSN Medical Australia, model number TN01-11, CDC approval number 84A-3348). The participants had a choice of small or medium sizes and selected the appropriate respirator for their faces.
Fig. 5.

Testing sequence
We used antifog safety goggles as shown in Figure 4 (3M Fahrenheit ID 70071531621; Product code 40170-00000). These goggles were chosen for several reasons: (i) they are large enough to be worn over prescription eyeglasses and have side cut-outs for temples to fit through, (ii) they have antifog properties, (iii) they are indirectly vented, (iv) the wide elasticated headband was detachable and adjustable, and (v) they are easily cleaned and disinfected.
Quantitative Fit Testing was performed using a PortaCount® Respirator Fit Tester 8048 (as shown in Fig. 1) and its accompanying software (TSI Incorporated, Shoreview, Minnesota, USA 55126). A particle generator was used throughout the study and an ambient particle count was recorded prior to each test. This particle generator was used to ensure the number of particles in the ambient air was always greater than 100 particles per cm3. Fit Testing was carried out with the participant in a seated position and by a trained fit tester.
On the date of testing, the participants’ age, sex, height, and weight were documented. For testing, the respirator was modified with a hollow probe inserted into the front of it and connected to a 1.5-m sample tube. One end of the sample tube is attached to the sample port on the PortaCount®, and the other end is attached to the probe on the front of the respirator. Another tube, called the ambient tube, sampled room air, as shown in Figure 6. This meant the PortaCount® could simultaneously sample particles from inside the respirator and the room to determine a fit-factor using Equation 1.
Fig. 6.

Tube connecting PortaCount® to participant's respirator
Equation 1.
The formula used to calculate the overall fit-factor. Fit-factor is represented as “ff” in the equation
The participant checked that the respirator was properly placed over the chin and the nose bridge. A mirror was provided for them to check the position of the respirator.
Once the participant was satisfied with respirator placement, the PortaCount® sampling tube was attached to the respirator probe and was manually supported by the participant throughout the test so as not to drag the respirator away from the face.
The OSHA 29 CFR 1910.134 protocol was used for QnFT (BTextbox 1). This comprises of seven exercises each carried out by the participant for 60 seconds. The PortaCount® would calculate a fit-factor for each exercise which was recorded. The fit-factor for each exercise is the ratio of the number of particles in the ambient air to the number of particles inside the respirator, as sampled by the ambient tube and the sampling tube, respectively. An overall fit-factor was calculated after testing using the formula shown in Equation 1.
Box 1: OSHA 29 CFR 1910.134 protocol
OHSA 29 CFR 1910.134 Quantitative Fit Test protocol
ff1: Normal breathing 60 s
ff2: Deep breathing 60 s
ff3: Move head from side-to-side 60 s
ff4: Move head up and down 60 s
ff5: Read the ‘rainbow passage’ 60 s
ff6: Bend forwards 60 s
ff7: Normal breathing 60 s
An overall fit-factor of ≥100 is considered a “pass” and a score <100 is considered a “fail”.3,11 The PortaCount® truncated results greater than 200 and assigned them a value of “200+”.
Once the overall fit-factor with the respirator alone was calculated, the participant was asked to fit the safety goggles with the elastic headband. The aim was to ensure that the lower rim of the goggles pushed the upper rim of the respirator onto the face. When the user was satisfied with goggle placement, QnFT was repeated, and a post-intervention fit-factor calculated. After their use, the goggles were cleaned using hospital-grade disinfectant wipes (Clinell universal wipes, containing benzalkonium chloride, polyhexamethylene biguanide, and didecyl dimethyl ammonium chloride, GAMA Healthcare, Victoria, Australia, 3168).
Statistical Analysis
We conducted the study only on HCWs who had previously failed a Fit Test with a Proshield® duckbill N95 respirator. We assumed that facial features of the participants may have changed since their last test, and up to 20% may pass quantitative fit testing in this study. Based on our pilot study,16 we estimated that 40% of the participants may progress from fail to pass with the use of safety goggles. We calculated that a dependent sample size of 54 participants would be required for a two-sample paired proportions test, with a two-tail α of 0.05 and power of 0.8. Our null hypothesis was that the use of safety goggles will not improve the proportion of participants who pass the quantitative Fit Test (i.e., achieved an overall fit-factor ≥100).
The PortaCount® truncated fit-factor scores greater than 200; therefore, a Tobit regression model with an upper-bound correction (upper limit = 200) was used for the analysis. Tobit regression analysis performs a comparison of two samples, in this case, the pre-intervention and post-intervention fit-factors, and controls for the clustering effect of the truncated fit-factor scores. Summary statistics (mean and standard errors) for the overall fit-factor are reported as unadjusted (raw) and adjusted (using Tobit analysis). Categorical data (“pass” or “fail” overall Fit Test) were analyzed using McNemar's test with Edwards correction. Statistical analysis was performed using STATA V16 (Texas 77845-4512, USA).
Results
We enrolled 60 participants to account for possible dropouts. However, there were no dropouts, and data collected from all 60 participants were analyzed.
Data on cohort demographics are presented in Table 1. The mean age of the participants was 39 years (SD 11.5). About 85% of participants were female, and the median BMI was 23.9 (IQR 21.1–27.6).
Table 1.
Participant demographic data
| Cohort demographics | |
|---|---|
| Parameter | Value |
| Age – Mean (SD) | 39 (11.5) |
| Sex | Female 85% |
| BMI – Median (IQR) | 23.9 (21.1–27.6) |
We have reported the unadjusted mean overall fit-factor and the adjusted mean overall fit-factor using Tobit regression modeling. The adjusted mean overall fit-factor and the proportion of participants who passed/failed are presented in Figures 7 and 8. The number of participants who passed their Fit Test without goggles (i.e., pre-intervention) was 8/60 (13.3%). After the application of safety goggles, the number of participants who passed increased to 49/60 (81.7%). About 42 participants who failed without the goggles passed with its application. One participant converted from a “pass” to a “fail”.
Fig. 7.
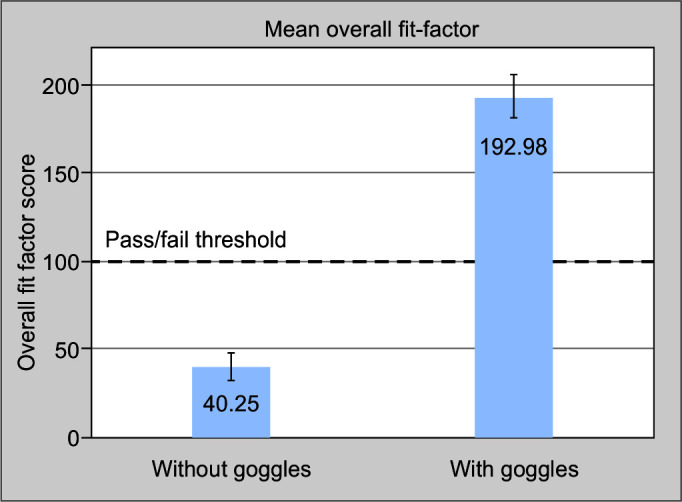
Adjusted mean overall fit-factor calculated using Tobit regression analysis. The horizonal dashed line represents the pass/fail threshold
Fig. 8.
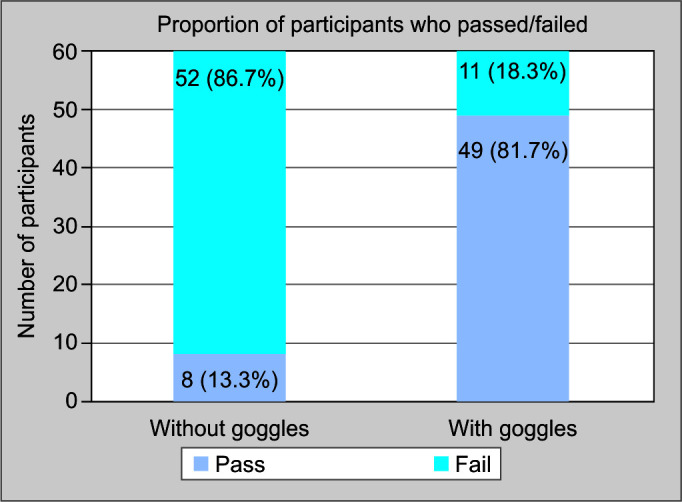
Proportion of participants who passed (ff ≥ 100) and failed (ff < 100) the overall Fit Test before and after the use of the safety goggle
Before the application of safety goggles, the unadjusted mean overall fit-factor for participants was 39.39 (SE 7.45; 95% CI 24.49–53.57). The Tobit-adjusted mean overall fit-factor was 40.25 (SE 7.91; 95% CI 24.59–55.92) – significantly lower than the pass threshold of 100. After the application of the safety goggles, the unadjusted mean overall fit-factor for participants was 163.97 (SE 7.56; 95% CI 148.85–179.09). The adjusted mean overall fit-factor was 192.98 (SE 12.15; 95% CI 168.91–217.05). Therefore, the overall fit-factor increased in 57/60 (95%) participants by an adjusted mean of 152.73 (t = 12.32; p-value < 0.001). Interestingly, three participants had a decrease in their overall fit-factor after donning the safety goggles.
A 2 × 2 contingency table for the analysis of categorical data is presented in Table 2. Using McNemar's test, we found that there was a significantly increased proportion of participants who passed QnFT (i.e., had an overall fit-factor ≥100) after the application of safety goggles. Compared with baseline use of a N95 respirator alone, the odds ratio for passing the QnFT with the addition of safety goggles was 42 (95% CI 7.14–1697.9, p-value = < 0.0001).
Table 2.
2 × 2 contingency table for analysis of categorical pass/fail data for all participants
| Postintervention (with goggles) | ||||
|---|---|---|---|---|
| Pass | Fail | Column total | ||
| Preintervention (without goggles) |
Pass Fail Row total |
7 42 49 |
1 10 11 |
8 52 60 |
These results reject our null hypothesis that the use of safety goggles does not improve the proportion of participants who pass the quantitative Fit Test.
Discussion
This study found that a significant proportion of participants, who had previously failed a quantitative Fit Test with the tested duckbill respirator, passed with the application of 3M Fahrenheit antifog safety goggles. Moreover, the overall fit-factor of the duckbill respirator significantly increased with the application of the goggles.
N95 respirators are a valuable resource, particularly during the COVID-19 pandemic.19,20 However, it has been found that they have a high failure rate.21 Ideally, a broad range of respirators should fit all users. However, most hospitals only stock a limited variety of respirators. Any intervention that enhances the fit of a respirator may improve the safety of HCWs. For example, Wardhan et al. trialled using double-sided adhesive tape around a respirator to optimize its seal.22 However, this group used qualitative fit testing, which is inferior to quantitative fit testing.8–10 Guidelines have been clear in advising those looking after COVID-19 patients to wear eye protection.1–3 Therefore, we chose to use the eye-protective element as our intervention that enhances the respirator fit so as not to add another element to PPE.
We used N95 respirators and goggles that are widely available internationally, which is a strength of this study. The goggles are nondisposable and easily disinfected. They are antifog, accommodate for eyeglasses, and their indirect venting system protects from splashes when compared with a direct venting system. Another strength is that by using recommended eye protection as the element that optimizes the N95 respirator fit, there is no additional element to PPE for HCWs. Last, we chose to perform quantitative Fit Testing with a particle counter, which is considered the superior method of detecting leaks when compared with qualitative fit testing. It eliminates participant reporting bias and objectively quantifies the testing process.
This study has several limitations. We tested only one form of N95 respirator, and therefore these results can only be applied to the Proshield® duckbill N95 respirator. Additionally, the trial was conducted in a single center in Australia, which limits external validity. Moreover, the order of before-and-after testing was not randomized; all participants were tested with the respirator only followed by testing with the respirator and the goggles. Lastly, a large proportion of the participants were female, due to the lack of randomization in the study and the opportunistic sampling method used.
Our study may have far-reaching implications, better protection, use of one respirator, less waste, and cost-saving. Another strength is that by using recommended eye protection as the element that optimizes the N95 respirator fit, there is no additional element to PPE for HCWs.
Conclusion
We conclude that the use of safety goggles significantly increases the proportion of users who pass a quantitative Fit Test and significantly improves the fit-factor of a duckbill N95 respirator. It is recommended that similar studies on other N95 respirators be carried out.
Orcid
Mohamed Kamal https://orcid.org/0000-0002-0803-5190
Mominah Bhatti https://orcid.org/0000-0002-7477-6923
Warren Christopher Stewart https://orcid.org/0000-0003-3048-9516
Moira Johns https://orcid.org/0000-0001-5532-1723
David Collins https://orcid.org/0000-0002-9522-7501
Yahya Shehabi https://orcid.org/0000-0003-4707-7462
Solomon Rajesh Thambiraj https://orcid.org/0000-0001-5107-9060
Sumesh Arora https://orcid.org/0000-0002-2065-3522
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.WHO. Infection Prevention and Control during Healthcare when Coronavirus Disease (COVID-19) is Suspected or Confirmed; 2021 [Google Scholar]
- 2.Australian Department of Health. Guidance on the Use of Personal Protective Equipment (PPE) in Hospitals during the COVID-19 Outbreak; 2020 [Google Scholar]
- 3.NSW Clinical Excellence Commission. Respiratory Protection Program Manual. 2020 1st edition; [Google Scholar]
- 4.Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel MP, Kute VB, Goswami J, Balwani MR. Hospitals may become “Disease Hotspots” for COVID-19 amid shortage of personal protective equipment. Indian J Crit Care Med. 2020;24(11):1145–1146. doi: 10.5005/jp-journals-10071-23645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramasubban S. COVID collateral: “Don't forget the diligent healthcare worker”. Indian J Crit Care Med. 2020;24(8):613–614. doi: 10.5005/jp-journals-10071-23542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duling MG, Lawrence RB, Slaven JE, Coffey CC. Simulated workplace protection factors for half-facepiece respiratory protective devices. J Occup Environ Hyg. 2007;4(6):420–431. doi: 10.1080/15459620701346925. [DOI] [PubMed] [Google Scholar]
- 8.Danyluk Q, Hon CY, Neudorf M, Yassi A, Bryce E, Janssen B, et al. Health care workers and respiratory protection: Is the user seal check a surrogate for respirator Fit Testing? J Occup Environ Hyg. 2011;8(5):267–270. doi: 10.1080/15459624.2011.566016. [DOI] [PubMed] [Google Scholar]
- 9.Hon CY, Danyluk Q, Bryce E, Janssen B, Neudorf M, Yassi A, et al. Comparison of qualitative and quantitative Fit Testing results for three commonly used respirators in the healthcare sector. J Occup Environ Hyg. 2017;14(3):175–179. doi: 10.1080/15459624.2016.1237030. [DOI] [PubMed] [Google Scholar]
- 10.Lawrence RB, Duling MG, Calvert CA, Coffey CC. Comparison of performance of three different types of respiratory protection devices. J Occup Environ Hyg. 2006;3(9):465–474. doi: 10.1080/15459620600829211. [DOI] [PubMed] [Google Scholar]
- 11.Occupational Safety and Health Administration. Fit Testing Procedures; Part I. OSHA-Accepted Fit Test Protocols. USA Department of Labor; 2004 [Google Scholar]
- 12.Chu DK, Akl PEA, Duda S, Solo K, Yaacoub S, Schunemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/j.jvs.2020.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Milosevic M, Kishore Biswas R, Innes L, Ng M, Mehmet Darendeliler A, Wong A, et al. P2/N95 filtering facepiece respirators: Results of a large-scale quantitative mask fit testing program in Australian health care workers. Am J Infect Control. 2022;50(5):509–515. doi: 10.1016/j.ajic.2021.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harber P, Su J, Badilla AD, Rahimian R, Lansey KR. Potential role of infrared imaging for detecting facial seal leaks in filtering facepiece respirator users. J Occup Environ Hyg. 2015;12(6):369–375. doi: 10.1080/15459624.2015.1006636. [DOI] [PubMed] [Google Scholar]
- 15.Roberge RJ, Monaghan WD, Palmiero AJ, Shaffer R, Bergman MS. Infrared imaging for leak detection of N95 filtering facepiece respirators: A pilot study. Am J Ind Med. 2011;54(8):628–636. doi: 10.1002/ajim.20970. [DOI] [PubMed] [Google Scholar]
- 16.Johns M, Kyaw S, Lim R, Stewart WC, Thambiraj SR, Shehabi Y, et al. Fit factor change on quantitative fit testing of Duckbill N95 respirators with the use of safety goggles. Indian J Crit Care Med. 2021;25(9):981–986. doi: 10.5005/jp-journals-10071-23972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Todi S. Clearing the fog on the use of N95 mask. Indian J Crit Care Med. 2021;25(9):961–962. doi: 10.5005/jp-journals-10071-23976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.TSI. PortaCount Respirator Fit Tester – User Manual. 2021 P/N 6010633, Revision P; [Google Scholar]
- 19.Haji JY, Subramaniam A, Kumar P, Ramanathan K, Rajamani A. State of personal protective equipment practice in Indian Intensive Care Units amidst COVID-19 pandemic: A nationwide survey. Indian J Crit Care Med. 2020;24(9):809–816. doi: 10.5005/jp-journals-10071-23550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chawla G, Abrol N, Kakkar K. Personal protective equipment: A Pandora's box. Indian J Crit Care Med. 2020;24(5):371–372. doi: 10.5005/jp-journals-10071-23443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Degesys NF, Wang RC, Kwan E, Fahimi J, Noble JA, Raven MC. Correlation between N95 extended use and reuse and fit failure in an Emergency Department. JAMA. 2020;324(1):94–96. doi: 10.1001/jama.2020.9843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wardhan R, Brennan MM, Brown HL, Creech TB. Does a modified adhesive respirator improve the face seal for health care workers who previously failed a fit test?: A pilot study during the Coronavirus Disease 2019 pandemic. A A Pract. 2020;14(8):e01264. doi: 10.1213/XAA.0000000000001264. [DOI] [PMC free article] [PubMed] [Google Scholar]





