Abstract
Background:
Chronic cough (CC; cough that lasts 8 weeks or longer) poses major effective assessment challenges. Assessment of CC may vary considerably among medical specialists.
Objectives:
The aim was to evaluate similarities and consistency of responses across different specialists when performing a basic assessment of CC patients in primary care, and referring patients based on clinical findings or test results.
Methods:
A modified Delphi approach was used. A survey with 74 statements on initial assessment of CC and referral pathways was addressed to a panel of different specialists, who voted the statements in two rounds.
Results:
Seventy-seven physicians [18 primary care physicians (PCPs), 24 pulmonologists, 22 allergists, and 13 ear, nose, and throat specialists] from the National Healthcare System of Spain answered the questionnaire. After two rounds, the panel reached a consensus on 63 out of the 74 proposed items (85.1%). Consensus was not reached among the panelists of at least one specialty on 15 out of these 63 agreed items. The panel agreed on those clinical aspects that should be evaluated by PCPs in all patients with CC including the impact of CC on quality of life. Agreement was reached on initial actions to be taken in primary care, including substitution of drugs that may induce cough, performing a chest X-ray, introduction of anti-reflux measures, initiation of empirical anti-reflux pharmacological therapy in some cases, and performing a spirometry with bronchodilator test and hemogram if an etiological diagnosis was not reached. The panelists agreed on a list of diseases that PCPs should assess before referring CC patients. Algorithms were developed for initial assessment and targeted referral of patients with CC from primary care.
Conclusion:
This study provides the perspective of different medical specialists on how to perform a basic assessment of CC patients in primary care and how and when to refer patients to other specialists.
Keywords: cough, Delphi technique, diagnosis, differential, interdisciplinary communication, primary health care, referral and consultation, symptom assessment
Introduction
Cough is one of the most frequent symptoms for which patients often might seek medical care. 1 Depending on its duration, cough can be classified as acute (less than 3 weeks’ duration), subacute (3 to 8 weeks), or chronic (more than 8 weeks).1,2 Chronic cough (CC) may severely impact patients’ health-related quality of life (HRQoL) and can be highly disruptive not only for the affected individuals, but also for those around them. 1 Patients report numerous physical and/or psychosocial effects associated with CC, including breathlessness, wheezing, fatigue, exhaustion, sleep disturbances, speech impairment, retching, vomiting, and interference with daily activities, as well as urinary incontinence. 3 Moreover, CC is also associated with emotional changes including depression, anxiety, fear, helplessness, or embarrassment, and severe coughing can lead to social isolation. 4
The prevalence of CC varies among different studies depending on the study population and the methodology used. A meta-analysis estimated that CC could affect up to 10% of the adult population. 5 Recent web-based surveys involving panels of adults described a CC prevalence of about 5% in different countries (United States, Japan, Germany and Spain)6–9 and suggested that CC might be underdiagnosed in younger adults. In addition, one-third of individuals with ongoing CC symptoms in primary care may not have any associated comorbidities. 10
Effective diagnosis and treatment of CC pose major challenges. 1 The assessment of an individual patient with CC may range from a complete initial diagnostic evaluation for common associated diseases, to empirical therapy for common conditions known to cause CC with limited diagnostic efforts, and this depends at least in part on the specialist seeing the patients. 11 Besides smoking, clinical conditions classically considered to cause the majority of CC cases are postnasal drip or upper airways cough syndrome, asthma, eosinophilic bronchitis, and gastroesophageal reflux disease. 1 However, two situations are frequent in clinical practice: first, that an underlying disease as an etiology for cough is not identified (named unexplained CC) and second, that the appropriate treatment of the underlying disease and the available antitussive treatments do not alleviate cough (called refractory CC).1,2
The burden of CC for healthcare providers is relevant since many times inappropriate or repetitive diagnostic test are performed. 3 Not surprisingly, treatment can be substantially delayed due to prolonged diagnostic testing, with too many tests and physician visits and poor access to specialist cough centers. 3 Moreover, lack of clear pathways to evaluate and treat patients with CC and difficulties to find an effective solution to CC have led many patients to abandon the healthcare system and look for alternative therapies: in a recent survey, close to 50% Spanish physicians reported that patients with CC are frequently ‘lost to follow-up’ in their clinics. 12
In this context, primary care physicians (PCPs) play a key role in the initial evaluation of patients with CC, by carrying out a rapid but thorough assessment of patients and promptly and appropriately referring them to other specialists, if needed. However, there is a lack of guidance regarding the ideal assessment the PCP must perform to evaluate CC patients and when and to which specialist CC patients must be referred from primary care.
In this study, it was aimed to evaluate the similarities and consistency of responses across PCPs; pulmonologists; allergists; and ear, nose, and throat (ENT) specialists on how to perform a basic assessment of CC patients in primary care and how to refer patients to different specialists based on clinical findings or test results. This work will set the basis for providing guidance and useful tools for CC assessment in primary care and referral recommendations.
Methods
Design
In this project, a qualitative evaluation of the literature was conducted and a consensus method (Delphi method following RAND/UCLA recommendations)13,14 was employed. A scientific committee of five experts (two PCPs, one pulmonologist, one allergist, and one ENT specialist) led the study. After search and review of available literature from different sources, the scientific committee generated 74 debatable statements addressing the assessment of CC in primary care and the referral of CC patients to different specialists. In a second step, these statements were sent to an expert panel of PCPs, pulmonologists, allergists, and ENT specialists for an online evaluation and validation by voting in two rounds.
Literature search
The literature search was focused on guidelines and reviews addressing cough assessment and management, and referral pathways. A search for the identification of guidelines and recommendations was conducted in the following repositories and databases: MEDLINE, via PubMed; The Cochrane Library; U.S. National Guidelines Clearinghouse; Tripdatabase Epistemonikos database; Biblioteca de Guías de Práctica Clínica del Sistema Nacional de Salud (Spanish National Healthcare System Library of Guidelines for Clinical Practice, GuiaSalud). In addition, the websites of the leading American, European, and Spanish scientific societies involved in the management of patients with cough were searched. The search strategy for PubMed included the following terms: Chronic Cough; Refractory Cough; Idiopathic Cough; Continuity of Patient Care; Patient Care Management; Case Management; Comprehensive Health Care; Aftercare; Referral and Consultation; Organization and Administration; Models; Organizational; Secondary Care; Critical Pathways; Health Services Administration; and Interdisciplinary Communication. Literature search was conducted in December 2020. It was restricted to articles published in English and Spanish during the past 10 years.
Statements development
Literature was reviewed by the scientific committee and, during two virtual meetings, a total of 74 statements were agreed by all the experts. The statements were divided into the following groups: (1) General considerations about CC, (2) Assessment of CC in primary care (comprising initial clinical evaluation, initial medical actions, and initial complementary tests and diagnostic approach, including empirical treatments), and (3) Referral process (including introductory statements, general statements on patients’ referral, specific referral pathways, and additional considerations)
Panelists
Panelists were selected by the scientific committee and their respective scientific societies, taking into account the following selection criteria. They should (1) be PCP, pulmonologist, allergist, or ENT specialist; (2) work for the National Spanish Healthcare System; (3) be affiliated to a Spanish Scientific Society according to their field of expertise; (4) see at least one patient with CC every other week in their clinic. The panel was anonymous to each other through the voting process. The sponsor of the study (MSD Spain) did not participate in the selection of the panel, and the experts of the scientific committee did not participate in the voting process of the statements.
Delphi rounds and analysis
Feedback from panelists was obtained through two rounds of surveys administered through an in-house designed web-based survey. They were given 2 weeks to complete the questionnaire in each round. Participants had the opportunity to add comments or suggestions in case they felt that the statements were not clear enough and to take these comments into account in the discussion of the article. In the first round, all panelists responded to the complete set of 74 statements. Panelists assessed each statement using a single 9-point Likert-type ordinal scale (1: full disagreement; 9: full agreement). Responses were organized into three groups: 1–3 were considered as disagreement, 4–6 as neither agreement nor disagreement, and 7–9 as agreement. Consensus was reached if (1) the median of the responses was in the range 7–9 (agreement) or 1–3 (disagreement), (2) less than one-third of the panelists voted outside these ranges and (3) the interquartile range (IQR) was less than 4.
The results obtained in the first round were analyzed and shared with the participants. The statements that did not reach consensus were subjected to a second round of voting. The scientific committee did not consider it necessary to reformulate or add any statement. Before the second round, the panelists received the personal and global first survey results, as well as individual comments in an anonymous way (i.e. with no identification of the panelist who made each comment), so that they could contrast their personal opinions with those of their fellow panelists and, if necessary, reconsider their initial responses. The results obtained in this second round were analyzed using the same criteria as in the first round.
In addition to the overall analysis, an analysis of responses by specialties was performed to evaluate potential discrepancies among them, but only the global consensus of the entire panel was taken into account to categorize each statement.
Results are shown in tables as median and IQR of the panelists’ responses, and degree of agreement, which was defined as the percentage of panelists who voted within the category that included the median of the answers (1–3, 4–6, or 7–9), and interpretation, including discrepancies among different specialties. Considering the consensus items, the scientific committee developed an algorithm summarizing the conclusions.
Results
The questionnaire was submitted to the panel and responded by 77 experts (18 PCPs, 24 pulmonologists, 22 allergists, and 13 ENT specialists) and all panelists responded to both rounds. After the first round, a consensus on agreement was reached on 62 items. One additional item reached consensus on agreement after the second round of evaluation. Subsequently, after two rounds of evaluation, consensus was reached on 63 out of the 74 proposed items (85.1%) by the panelists overall. In the analysis of the results by specialty, in 15 out of the 63 consensus items, there was divergence among specialties since consensus was not reached among the panelists of at least one specialty.
General considerations about CC
Table 1 shows the outcomes (median with IQR, percentage of agreement, and interpretation) regarding statements on general considerations. The overall panel reached consensus on agreement in all, but one statement. The panel considered that more practical guidelines for the diagnosis and treatment of patients with CC are needed, and emphasis should be given to the initial management in primary care. In addition, they agreed that CC might be, in some patients, a disease in itself and not a symptom of another underlying pathology. There was no consensus on the statement regarding the correct use of CC guidelines in primary care. In addition, although the panel reached consensus on the need to record the diagnosis of CC in medical records, ENT specialists did not.
Table 1.
General considerations about chronic cough.
| Item | Median (IQR) | Percentage of agreement (%) | Result (overall experts panel) | Comments |
|---|---|---|---|---|
| 1. Chronic cough (cough lasting more than 8 weeks) is a frequent reason for consultation in primary care | 8 (7–9) | 88.3 | Agreement in first round | |
| 2. A diagnosis of ‘chronic cough’ needs to be recorded in the medical record of patients with cough of more than 8 weeks’ duration | 9 (8–9) | 88.3 | Agreement in first round | No consensus reached by ENT specialists |
| 3. Current guidelines for the management of chronic cough are correctly used in primary care | 4 (2–5) | 49.4 | No consensus reached | |
| 4. There is a need for the different specialists to be aware of clinical practice guidelines on chronic cough | 9 (8–9) | 94.8 | Agreement in first round | |
| 5. More practical guidelines are needed for the assessment and treatment of patients with chronic cough, focusing on the initial approach in primary care | 9 (7–9) | 97.4 | Agreement in first round | |
| 6. The terms ‘refractory chronic cough’ and ‘unexplained chronic cough’ should be known and used in the diagnosis of patients where appropriate | 8 (7–9) | 83.1 | Agreement in first round | |
| 7. It is necessary to be aware that chronic cough may be, in some patients, a disease in itself and not a symptom of another pathology | 8 (7–9) | 85.7 | Agreement in first round |
ENT, ear, nose, and throat specialist; IQR, interquartile range.
Assessment of CC in primary care: initial clinical assessment and actions
The panel agreed on 12 clinical aspects that should be evaluated by PCPs in all patients with CC, including questions about cough characteristics, accompanying symptoms, warning signs and symptoms (red flags), previous medical history, and cardiopulmonary physical examination. The panel also reached consensus on the importance of assessing the impact of CC on quality of life and on estimating cough intensity using simple tools like a visual analog scale (VAS). PCPs, however, did not reach agreement on this item on the VAS (see ‘Initial clinical assessment’ in Table 2).
Table 2.
Assessment of chronic cough in primary care. Initial clinical assessment and actions.
| Item | Median (IQR) | Percentage of agreement (%) | Result | Comments |
|---|---|---|---|---|
| Initial clinical assessment | ||||
| The initial clinical assessment of patients with chronic cough by the primary care physician should include: | ||||
| 8. Patients clinical background | 9 (9–9) | 100.0 | Agreement in first round | |
| 9. The characteristics of cough (dry or productive, characteristics of expectoration, and so on) | 9 (9–9) | 98.7 | Agreement in first round | |
| 10. If the patient has a feeling of ‘urge to cough’ | 8 (7–9) | 84.4 | Agreement in first round | |
| 11. Whether there are factors that trigger cough or facilitate the onset of diseases producing cough (environmental factors, exposures at home or at work, and so on) | 9 (9–9) | 100.0 | Agreement in first round | |
| 12. Concomitant systemic symptoms (fever, asthenia, and so on) | 9 (9–9) | 98.7 | Agreement in first round | |
| 13. If there are associated upper respiratory symptoms (rhinorrhea, changes in voice characteristics, and so on) | 9 (9–9) | 98.7 | Agreement in first round | |
| 14. If there are associated lower respiratory symptoms (wheezing, dyspnea, or other) | 9 (9–9) | 100.0 | Agreement in first round | |
| 15. The presence of symptoms suggestive of gastroesophageal reflux or digestive disease (dysphagia, dyspepsia, and so on) | 9 (9–9) | 100.0 | Agreement in first round | |
| 16. The presence of red flags suggesting serious underlying disease requiring urgent diagnostic work-up a | 9 (9–9) | 100.0 | Agreement in first round | |
| 17. An estimate of cough intensity using a simple index (e.g. a visual analog scale or a numerical scale) | 8 (6.5–9) | 75.3 | Agreement in first round | No consensus reached by PCPs |
| 18. An assessment of the impact of cough on quality of life | 8 (7–9) | 81.8 | Agreement in first round | |
| 19. Cardiopulmonary physical examination | 9 (9–9) | 96.1 | Agreement in first round | |
| Initial diagnostic tests and actions | ||||
| In all patients with chronic cough, the primary care physician must: | ||||
| 20. Assess oxygen saturation with a pulse oximeter | 8 (6–9) | 71.4 | Agreement in first round | No consensus reached by PCPs |
| 21. Perform a posteroanterior and lateral chest X-ray, unless contraindicated | 9 (8–9) | 88.3 | Agreement in first round | |
| 22. Encourage smokers to stop smoking | 9 (9–9) | 100.0 | Agreement in first round | |
| 23. Substitute, if the patient’s comorbidities permit, drugs that may induce cough (angiotensin-converting enzyme inhibitors, beta-blockers, or others) | 9 (9–9) | 98.7 | Agreement in first round | |
| 24. Introduce general and dietary anti-reflux measures | 9 (7–9) | 87.0 | Agreement in first round | |
| 25. Reasonably rule out infectious diseases, including tuberculosis, as the cause of cough | 9 (8–9) | 97.4 | Agreement in first round | |
| 26. In patients with chronic cough who have peptic or reflux symptoms, empirical anti-reflux pharmacological treatment is recommended | 9 (8–9) | 89.6 | Agreement in first round | |
| 27. In patients with chronic cough who report wheezing, or when wheezing is detected on physical examination, empirical treatment with bronchodilators is recommended | 7 (5–8) | 64.9 | No consensus reached | Agreement in second round reached by allergists and by ENT specialists |
ENT, ear, nose, and throat specialist; IQR, interquartile range; PCP, primary care physician.
Warning signs or ‘red flags’ include: hemoptysis; smoker >45 years of age with a new cough, change in cough, or coexisting voice disturbance; adults aged 55–80 years who have a 30-pack-year smoking history and currently smoke or who have quit within the past 15 years; prominent dyspnea, especially at rest or at night; hoarseness; systemic symptoms (fever, weight loss, peripheral edema with weight gain); trouble swallowing when eating or drinking; vomiting; recurrent pneumonia; abnormal respiratory exam and/or abnormal chest radiograph coinciding with duration of cough (taken from the study by Irwin et al. 10 ).
In addition, the panel reached agreement on seven initial actions to be adopted in primary care (see ‘Initial diagnostic tests and actions’ in Table 2), including performing a posteroanterior and lateral chest X-ray, unless contraindicated, substitution of drugs that may induce cough (when this is feasible), introduction of general and dietary anti-reflux measures and, in patients with CC who have peptic or reflux symptoms, initiation of empirical anti-reflux pharmacological therapy. PCPs did not reach consensus on the need to assess oxygen saturation with pulse oximeter.
Assessment of CC in primary care: complementary diagnostic tests, diagnostic approach, and empirical treatments
Regarding initial complementary tests and diagnostic approach in primary care, the panelists agreed that spirometry with bronchodilator test and hemogram should be performed if an etiological diagnosis of CC was not reached by clinical history and chest X-ray, but did not agree in performing a computed tomography (CT) scan in patients with no pathological findings in the chest X-ray (see ‘Complementary diagnostic tests’ in Table 3).
Table 3.
Assessment of chronic cough in primary care: complementary tests, diagnostic approach, and empirical treatments.
| Item | Median (IQR) | Percentage of agreement (%) | Result | Comments |
|---|---|---|---|---|
| Complementary diagnostic tests | ||||
| If the etiology of chronic cough has not been diagnosed by the clinical history and chest X-ray in the primary care clinic: | ||||
| 28. Spirometry with bronchodilator testing should be performed | 9 (8–9) | 84.4 | Agreement in first round | No consensus reached by ENT specialists |
| 29. A hemogram should be performed | 8 (6–9) | 71.4 | Agreement in first round | No consensus reached by PCPs and by ENT specialists |
| 30. Chest CT should not be performed in the study of chronic cough if the patient has no abnormalities on chest X-ray | 5 (2–8) | 23.4 | No consensus reached | |
| The diseases that primary care physicians should assess, within their possibilities, before referring a patient with chronic cough include: | ||||
| 31. Asthma | 9 (9–9) | 100.0 | Agreement in first round | |
| 32. Cough as asthmatic equivalent (cough as asthma variant) | 9 (8–9) | 94.8 | Agreement in first round | |
| 33. Eosinophilic bronchitis | 6 (2–8) | 15.6 | No consensus reached | |
| 34. Laryngopharyngeal reflux. | 9 (6–9) | 70.1 | Agreement in first round | |
| 35. Gastroesophageal reflux | 9 (8–9) | 92.2 | Agreement in first round | |
| 36. Allergic rhinitis | 9 (7–9) | 81.8 | Agreement in first round | |
| 37. Chronic rhinosinusitis | 9 (7–9) | 85.7 | Agreement in first round | |
| 38. Obstructive sleep apnea | 7 (4.5–8) | 61.0 | No consensus reached | |
| 39. Vocal cord dysfunction | 6 (3–8) | 27.3 | No consensus reached | |
| 40. Chronic obstructive pulmonary disease (COPD) | 9 (8–9) | 87.0 | Agreement in first round | |
| 41. Chronic post-infectious cough | 9 (8–9) | 89.6 | Agreement in first round | |
| 42. Foreign body aspiration | 8 (6–9) | 68.8 | Agreement in first round | No consensus reached by pulmonologists |
| 43. Somatic cough syndrome (formerly called psychogenic chronic cough) | 7 (4–9) | 64.9 | No consensus reached | Agreement in second round reached by allergists and by pulmonologists |
| Empirical treatments | ||||
| Before referring a patient with chronic cough without any diagnostic suspicion based on the clinical history or the complementary tests performed in primary care, it is advisable to carry out: | ||||
| 44. An empirical anti-reflux treatment | 8 (6–9) | 72.7 | Agreement in first round | No consensus reached by PCPs and by pulmonologists |
| 45. An empirical treatment of asthma | 7 (3–8) | 53.2 | No consensus reached | |
| 46. An empirical treatment of allergic rhinitis | 7 (3.5–8) | 66.2 | No consensus reached | Agreement in first round reached by allergists Agreement in second round reached by ENT specialists |
| 47. An empirical treatment of eosinophilic bronchitis | 5 (2–7) | 32.5 | No consensus reached | |
| 48. Several empirical treatments can be carried out at the same time if there are no diseases suspected over others | 4 (1–7) | 22.1 | No consensus reached | |
CT, computed tomography; ENT, ear, nose, and throat specialist; IQ, interquartile range; PCP, primary care physician.
In addition, the panelists agreed on a list of diseases that family physicians should assess, within their possibilities, when facing CC patients before referring them (see ‘Complementary diagnostic tests’ in Table 3), but consensus was not reached on empirical treatments, except for empirical anti-reflux treatment (although for the panel overall, but not for PCPs and pulmonologists; see ‘Empirical treatments’ in Table 3).
Referral of patients with CC from primary care
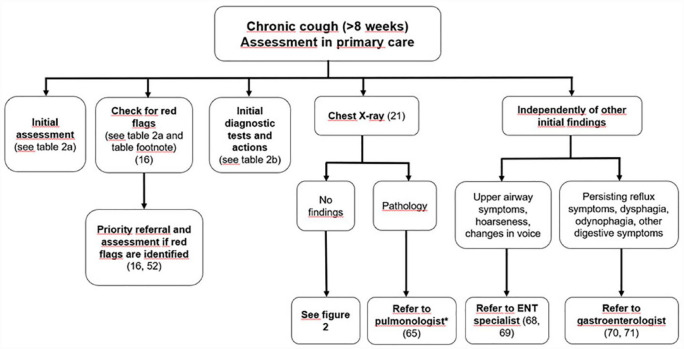
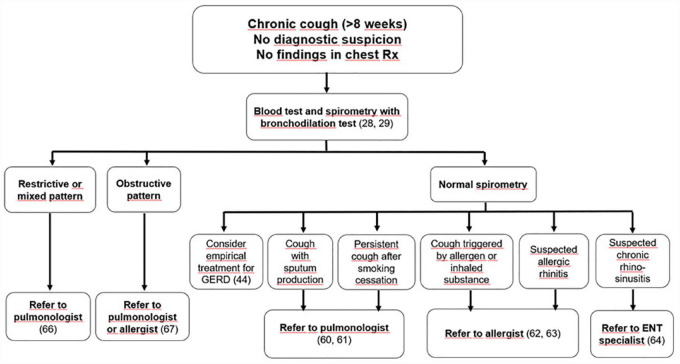
The panelists agreed that in primary care 11 general aspects should be considered when referring patients with CC (see ‘General considerations on patients’ referral’ in Table 4). Notably, the panel showed a high percentage of agreement (96%) in undergoing a complete diagnostic work-up until a diagnosis is made, whether it is CC caused by underlying pathology, or refractory CC or unexplained CC. Referral should be performed promptly when a serious warning sign or symptom (red flags) is identified that needs to be investigated as a matter of priority and without delay (100% agreement). In addition, consensus was reached on other circumstances that need patients’ referral (see ‘General considerations on patients’ referral’ in Table 4). Regarding referral to specific specialists, consensus was reached during the first round on the different referral pathways proposed, with minor discrepancies among specialists on some of the statements (see ‘Selective referral to specific specialists of patients without diagnosis reached in primary care’ in Table 4). Figures 1 and 2 depict an algorithm that summarizes consensus items regarding initial assessment and targeted referral of patients with CC from primary care. Table 5 shows additional considerations regarding the use of appropriate diagnostic terminology.
Table 4.
Referral of patients with chronic cough from primary care to other specialists.
| Item | Median (IQR) | Percentage of agreement (%) | Result | Comments |
|---|---|---|---|---|
| General considerations on patients’ referral | ||||
| 49. The diagnosis of chronic cough often requires the participation of different specialists | 9 (8–9) | 94.8 | Agreement in first round | |
| 50. Patients with chronic cough should be explained that the study of chronic cough is sometimes difficult and time-consuming, and that they should be patient | 9 (8–9) | 90.9 | Agreement in first round | |
| 51. All patients with chronic cough should undergo a complete diagnostic work-up, based on the best available evidence, until a diagnosis is made, whether it is chronic cough caused by an underlying disease, refractory chronic cough or unexplained chronic cough | 9 (8–9) | 96.1 | Agreement in first round | |
| In the primary care setting, the primary care physician should refer patients with chronic cough to another specialist: | ||||
| 52. In the event that there is a serious warning sign (red flags) a that needs to be investigated as a matter of priority and without delay | 9 (9–9) | 100.0 | Agreement in first round | |
| 53. To confirm a suspected diagnosis, when complementary tests needed are not available in the primary care setting | 9 (9–9) | 98.7 | Agreement in first round | |
| 54. When no diagnosis has been found that account for chronic cough after the diagnostic work-up in primary care | 9 (8–9) | 96.1 | Agreement in first round | |
| 55. To prescribe a treatment or to perform a diagnostic intervention that is not available in primary care | 9 (8–9) | 100.0 | Agreement in first round | |
| 56. In case of suspected cough hypersensitivity syndrome or cough reflex hyper-reactivity | 9 (7–9) | 87.0 | Agreement in first round | No consensus reached by ENT specialists |
| 57. In case of refractory chronic cough (when an etiological diagnosis has been found in primary care and the underlying cause has been correctly treated, but cough persists) | 9 (8–9) | 93.5 | Agreement in first round | |
| 58. Patients with chronic cough in the above-mentioned situations should be referred to a specific chronic cough clinic or to a specialist with expertise in chronic cough, where such a clinic or specialist exists | 9 (7–9) | 90.9 | Agreement in first round | |
| 59. In the absence of referral to a specialized chronic cough unit, the primary care physician should act as case manager of patients with chronic cough | 7 (6–9) | 72.7 | Agreement in second round | No consensus reached by PCPs |
| Selective referral to specific specialists of patients without diagnosis reached in primary care | ||||
| Patients with chronic cough, chest X-ray and spirometry with bronchodilator test with no pathological findings: | ||||
| 60. Should be preferably referred to the pulmonologist if cough is productive | 8 (7–9) | 77.9 | Agreement in first round | |
| 61. Should be preferably referred to the pulmonologist if cough does not improve after stopping smoking | 8 (7–9) | 77.9 | Agreement in first round | No consensus reached by PCPs |
| 62. Should be preferably referred to the allergist if cough appears to be triggered by an allergen, exposure, or inhaled substance | 8 (6.5–9) | 75.3 | Agreement in first round | No consensus reached by pulmonologists |
| 63. Should be preferably referred to the allergist if allergic rhinitis is suspected | 8 (6.5–9) | 75.3 | Agreement in first round | No consensus reached by pulmonologists and by ENT specialists |
| 64. Should be preferably referred to the ENT specialist if chronic rhinosinusitis is suspected | 8 (7–9) | 79.2 | Agreement in first round | No consensus reached by pulmonologists |
| Patients with chronic cough and pathological findings in the chest X-ray and/or the spirometry with bronchodilator test: | ||||
| 65. Patients with a pathological chest X-ray (e.g. space-occupying lesion, infiltrates, interstitial disease) should preferably be referred to the pulmonologist unless the diagnosis is treatable by the primary care physician (e.g. pneumonia without severity criteria or other cause treatable at the time) | 9 (9–9) | 98.7 | Agreement in first round | |
| 66. Patients with normal chest X-ray and spirometry showing a restrictive or mixed pattern should be referred to the pulmonologist | 9 (7–9) | 89.6 | Agreement in first round | |
| 67. Patients with normal chest X-ray and spirometry showing an obstructive pattern should be referred to the pulmonologist or the allergist depending on the judgment of the primary care physician and additional findings | 9 (7–9) | 81.8 | Agreement in first round | No consensus reached by PCPs |
| Regardless of the results of the chest X-ray and the spirometry with bronchodilator test: | ||||
| 68. Patients should be referred to the ENT specialist when upper airway symptoms requiring specialized upper airway examination are present | 9 (8–9) | 93.5 | Agreement in first round | |
| 69. Patients should be referred to the ENT specialist if they present hoarseness or voice changes | 9 (8–9) | 92.2 | Agreement in first round | |
| 70. Patients should be referred to the gastroenterologist if they present accompanying reflux symptoms that persist after empirical treatment | 9 (8–9) | 90.9 | Agreement in first round | |
| 71. Patients should be referred to the gastroenterologist if they present dysphagia, odynophagia, or other persistent digestive symptoms | 9 (8–9) | 93.5 | Agreement in first round | |
ENT, ear, nose, and throat specialist; IQR, interquartile range; PCP, primary care physician.
Red flags include: hemoptysis; smoker >45 years of age with a new cough, change in cough, or coexisting voice disturbance; adults aged 55–80 years who have a 30-pack-year smoking history and currently smoke or who have quit within the past 15 years; prominent dyspnea, especially at rest or at night; hoarseness; systemic symptoms (fever, weight loss, peripheral edema with weight gain); trouble swallowing when eating or drinking; vomiting; recurrent pneumonia; abnormal respiratory exam and/or abnormal chest radiograph coinciding with duration of cough (taken from the study by Irwin et al. 10 ).
Figure 1.
Summary algorithm resulting from the statements where agreement was reached.
The number between brackets refers to the statements from which the algorithm was built. Referral to a specific specialist must not preclude referral to other specialists if different pathologies co-exist or are suspected in the same patient. Referral pathways are subjected to accessibility to each specialist in the different healthcare systems. ENT, ear, nose, and throat specialist; PCP, primary care physician.
*Unless a diagnosis is achieved, and the patient can be treated by the PCP at the primary care clinic.
Figure 2.
Summary algorithm resulting from the statements where agreement was reached.
The number between brackets refers to the statements from which the algorithm was built. Referral to a specific specialist must not preclude referral to other specialists if different pathologies co-exist or are suspected in the same patient. Referral pathways are subjected to accessibility to each specialist in the different healthcare systems. ENT, ear, nose, and throat specialist; GERD, gastroesophageal reflux disease.
Table 5.
Final considerations.
| Item | Median (IQR) | Percentage of agreement (%) | Result | Comments |
|---|---|---|---|---|
| 72. When after an appropriate diagnostic work-up, an underlying disease as a cause of cough has not been found, patients should be diagnosed with ‘unexplained chronic cough’ | 8 (8–9) | 87.0 | Agreement in first round | |
| 73. When an underlying disease as a cause of cough has been found, and has been treated correctly but cough persists, patients should be diagnosed with ‘refractory chronic cough’ | 8 (7–9) | 84.4 | Agreement in first round | |
| 74. Patients who return to primary care after diagnostic work-up of cough and have unexplained chronic cough (no underlying cause) or refractory chronic cough (underlying cause correctly treated but cough persists) should be referred again for specific cough therapy if cough has not been controlled with conventional treatments | 8 (7–9) | 76.6 | Agreement in first round | No consensus reached by PCPs and by ENT specialists |
ENT, ear, nose, and throat specialist; IQR, interquartile range; PCP, primary care physician.
Discussion
This work aimed to evaluate the similarities and consistency of responses across PCPs, pulmonologists, allergists, and ENT specialists regarding the basic assessment of CC patients in primary care and referral pathways based on clinical findings or test results. A panel of PCPs, pulmonologist, allergists, and ENT specialists with experience in the management of CC expressed their degree of agreement on statements elaborated based on literature search and expert advice. The panel reached consensus in most of the items, and the results can be helpful for the elaboration of future recommendations and guidelines aiming to standardize the diagnostic approach to CC.
Several respiratory societies have published guidelines regarding the diagnosis and management of CC.1,15–20 However, these guidelines are not intended for PCPs and, in general, they do not elaborate in how this first approach or first steps to reach a diagnosis should be carried out in the primary care setting. In this context, the approach of this Delphi project can complement the recommendations of guidelines. 21
The first step in diagnosing adult patients complaining of CC is the clinical evaluation. The panel reached consensus on the initial clinical assessment of CC in primary care (see Tables 1 and 2), including questions to rule out factors that may trigger cough or facilitate the onset of cough-associated diseases, and the assessment of accompanying symptoms that may provide a clue to the cause of coughing. The initial assessment must always include an evaluation of red flags, which are symptoms or signs suggesting serious underlying pathology that requires an urgent diagnosis. 15
Regarding the impact of CC, guidelines recommend that the impact of cough should be assessed either by recording simple measures, such as a cough score out of 10 on a VAS, or by more detailed, validated measures of quality of life, such as the Leicester Cough Questionnaire (LCQ) 22 or the Cough-specific Quality of Life Questionnaire (CQLQ). 23 The panel agreed on the importance of estimating cough intensity using a simple index (e.g. VAS or equivalent numerical scale), and assessing the impact of cough on quality of life, but no recommendations on specific tool were made. Agreement by PCPs was not reached for assessing cough intensity with VAS or an equivalent alternative; inclusion of VAS in protocols, recommendations, and/or electronic health records might help using this simple tool. The ERS guidelines recommend to consider the use of validated questionnaires that may help to detect features of airway reflux,24–26 but they are time-consuming and their implementation in primary care might be complex.
The panel agreed on most of the initial actions to be taken by the PCPs in all patients with CC (see Table 3). In line with other guidelines, 1 the panel agreed that risk factors should be eliminated, such as stopping smoking and discontinuing the use of angiotensin-converting enzyme (ACE) inhibitors of other drugs that can induce cough, if possible. Although ACE inhibitors can easily be replaced by angiotensin-receptor blockers, other therapies such as beta-blockers can be more difficult to be discontinued, especially in patients with concomitant heart disease. Independent of the actions taken, the panel agreed that a chest X-ray should be performed as part of the routine evaluation of CC patients, as well as a spirometry with bronchodilator test in those with no diagnosis after chest X-ray. On the contrary, and in alignment with current guidelines, 1 there was no consensus on performing a chest scan in patients with non-pathological chest X-ray.
Regarding empirical treatments, the panel agreed that in patients with CC and peptic or reflux symptoms, an empirical anti-reflux pharmacological treatment is recommended. In line, the 2020 ESR guidelines recommend the initiation of proton-pump inhibitors (PPIs) only when peptic symptoms or evidence of acid reflux are present. 1 Other guidelines recommend anti-acid drugs with lifestyle changes such as dietary changes and weight loss in patients with CC when a reflux-cough syndrome is suspected.16,17,21,27 Evidence suggests that anti-acid drugs are unlikely to improve cough outcomes, unless patients have peptic symptoms or evidence of acid reflux, although the level of evidence is low. 1 A systematic review found only modest benefit of PPIs in patients with acid reflux and no significant benefits in patients without acid reflux. 28 Although the panel agreed on trying an empirical anti-reflux treatment, this statement did not reach consensus among PCPs or among pulmonologists, and is open to further discussion. Agreement was not reached on other empirical treatments. Empirical treatments can delay the diagnostic process, especially if they are ineffective.
The American College of Chest Physicians (CHEST) Expert Cough Panel considers empirical treatment for the most common causes of CC such as asthma, upper airway cough syndrome, or non-asthmatic eosinophilic bronchitis,15,21 while the ERS guidelines recommend considering empirical treatment of asthmatic cough (cough variant asthma and eosinophilic bronchitis), particularly when exhaled nitric oxide fraction (FeNO) or blood eosinophils levels are high. 1 In this study, statements of empirical treatment of these potential causes of CC did not reach consensus: it was considered that this could delay patients’ referral and diagnostic study. However, allergists and ENT specialists agreed on trying an empiric treatment of allergic rhinitis; the reason might be that this is one of the most frequent causes of CC seen in their respective clinics and the accompanying symptoms usually are illustrative.
Finally, based on the initial findings, the panel assessed the proposed referral pathways and reached overall consensus on all of them, although for several, consensus was not reached among some specialists (see Table 4) maybe reflecting differences in clinical practice. Besides these minor discrepancies, authors built a practical algorithm that summarizes the primary care approach and the referral pathways upon which consensus was reached (see Figures 1 and 2), which can be useful not only for PCPs but also for other specialists managing patients with CC. It is important to point out that referral to a specific specialist must not preclude referral to other specialists as well if different pathologies co-exist or are suspected in the same patient.
The diagnostic process and management of CC can be challenging for doctors and patients and proper diagnosis and treatments are often delayed even for years.3,29 In this regard, the authors would like to emphasize three consensus items: (1) all patients with CC should undergo a complete diagnostic work-up, using the best available evidence, until a diagnosis is made, whether it is CC caused by underlying pathology, refractory CC or unexplained CC; (2) patients with CC should be told that the evaluation of CC can often be difficult and time-consuming and that they should have ‘patience’; and (3) it is necessary to be aware that CC may be, in some patients, a disease in itself and not a symptom of another pathology. These three statements (7, 50, and 51) were agreed in the first round and provide additional insights to both doctors and patients preparing them to deal effectively with the CC diagnostic process. In addition, the terms ‘refractory chronic cough’ and ‘unexplained chronic cough’ do not usually appear in electronic health records. The panel reached consensus on using these terms to diagnose patients with cough that persists after the underlying disease is correctly treated and otherwise controlled, or cough without a final diagnosis after a complete diagnostic work-up, respectively.
This study has the inherent limitations of the Delphi methodology: it is not possible to include the individual opinions of the panelists, or discuss the items in depth, and some issues may be overlooked. In addition, there could be subjectivity linked to personal evaluations or preferences. The study was performed in the context of the Spanish public national health system, and panelists were selected taking into account their experience in the field of CC. Thus, two limitations arise: the findings could not apply to health systems with different structures or functioning, and the opinions of other physicians, with less knowledge of CC, could have been different. Since the sample of the panel was not homogeneous among the different specialists (with higher number of pulmonologists and lower of ENT specialists), some groups of specialists may have influenced the consensus in their favor. Not only was the overall assessment detailed, but also if a specific group of specialists did/did not reach consensus in all the statements. Finally, it needs to acknowledge that experts’ opinions contribute with a low degree of evidence to the formulation of recommendations but are important when no other evidence is available. It was not the authors’ aim to establish recommendations, but to explore consistency or opinions regarding the different addressed topics, which can be useful for future consensus guidelines.
In summary, this study provides the perspective of different medical specialists on the initial assessment of CC patients in primary care and on how and when to refer patients to other specialists. Gathering consensus items, the scientific committee developed tables and a practical algorithm that might be useful tools for PCPs in clinical practice to optimize the decision-making process during the assessment and referral of patients with CC.
Acknowledgments
This study was reviewed and endorsed by the following scientific societies (in alphabetical order): Grupo de Respiratorio en Atención Primaria (GRAP, Spanish Respiratory Group of Primary Care), Sociedad Española de Alergología e Inmunología Clínica (SEAIC, Spanish Society of Allergology and Clinical Immunology), Sociedad Española de Neumología y Cirugía Torácica (SEPAR, Spanish Society of Pulmonology and Thoracic Surgery), and Sociedad Española de Otorrinolaringología (SEORL, Spanish Society of Otorhinolaryngology).
The authors are grateful to all the participating panelists, who voted the statements following the Delphi methodology:
Julio Delgado Romero (Hospital Universitario Virgen Macarena, Sevilla), Santiago Quirce (Hospital Universitario La Paz, Madrid), Manuel Rial Prado (Complejo Hospitalario Universitario A Coruña, A Coruña), Paula Méndez Brea (Complejo Hospitalario Universitario de Santiago, Santiago de Compostela, A Coruña), Diana Betancor Pérez (Hospital Universitario Fundación Jiménez Díaz, Madrid), Aythamy Henríquez Santana (Hospital Universitario Infanta Elena, Valdemoro, Madrid) María Álvarez Puebla (Hospital Universitario de Navarra, Pamplona), Ignacio Antepara Ercoreca (Hospital Universitario de Basurto, Bilbao), Jose María Vega Chicote (Hospital Civil HRU, Málaga), Itxaso Orue Rivero (Santutxu-Solokoetxe, Bilbao), Mar Fernández Nieto (Hospital Universitario Fundación Jiménez Díaz, Madrid), Javier Domínguez Ortega (Hospital Universitario La Paz, Madrid), Ignacio Esteban Gorgojo (Hospital Universitario General de Villalba, Villalba, Madrid), Lorena Soto Retes (Hospital de la Santa Creu i Sant Pau, Barcelona), Remedios Cárdenas Contreras (Hospital Universitario Juan Ramón Jiménez, Huelva), Irina Bobolea Popa (Hospital Clìnic de Barcelona, Barcelona), Ismael García Moguel (Hospital Universitario 12 de Octubre, Madrid), Mar Gandolfo Cano (Hospital Universitario de Fuenlabrada, Fuenlabrada, Madrid), Blanca Barroso García (Hospital Universitario Fundación Jiménez Díaz, Madrid), Marcela Valverde Monge (Hospital Universitario Fundación Jiménez Díaz, Madrid), Francisco Javier Contreras Porta (Hospital Universitario La Paz, Madrid). Carlos Moral Paredes (Centro Salud Chandrexa de Queixa, Chandrexa De Queixa, Ourense), Diego Murillo Garcia (Centro de Salud Fregenal de la Sierra, Frenegal de la Sierra, Badajoz), José Luis Martínez Carrasco (Centro de Salud Fuencarral, Madrid), María Concepción Rodríguez Gallego (Centro de Salud Aravaca, Madrid), Mari Carmen Antón Sanz (Centro de Salud Alpedrete, Alpedrete, Madrid), Enrique Mascarós Balaguer (Centro de Salud Arquitecto Tolsá, Valencia), Daniel Ocaña Rodríguez (Centro de Salud Norte, Algeciras, Cádiz), Miguel Domínguez Santaella (Centro de Salud Victoria, Málaga), Inés López Fernández (Servicio Urgencias Hospital Universitario Lucus Augusti, Lugo), Leovigildo Ginel Mendoza (Centro de Salud Ciudad Jardín, Málaga), Pere Josep Simonet Aineto (CAP M Bernades-EAP Viladecans-2, Viladecans, Barcelona), María Luisa López Díaz-Ufano (Centro de Salud Reyes Católicos, San Sebastián de los Reyes, Madrid), Silvia María González Carranza (Centro de Salud Eibar, Eibar, Guipúzcoa), Milagros González Béjar (Centro de Salud Montesa, Madrid), Sara Núñez Palomo (Centro de Salud Torrelaguna, Torrelaguna, Madrid), Araceli Fernández Revuelta (Delicias Sur, Zaragoza), Juan Antonio Trigueros Carrero (Centro de Salud Menasalbas, Menasalbas, Toledo), Anna Mª Pedro Pijoan (ABS Gaudí, Barcelona). José Gregorio Soto Campos (Hospital Universitario de Jerez, Jerez de la Frontera, Cádiz), Antonio Pereira Vega (Hospital Universitario Juan Ramón Jiménez, Huelva), Xavier Aguilar Bargalló (Hospital Universitario Joan XXIII, Tarragona), Eusebi Chiner Vives (Hospital Universitario San Juan de Alicante, Alicante), M Auxiliadora Romero Falcón (Hospital Universitario Virgen del Rocío, Sevilla), Alfredo de Diego Damia (Hospital Universitario y Politécnico La Fe, Valencia), Jacinto Ramos González (Hospital Universitario de Salamanca, Salamanca), Eva Martínez Moragón (Hospital Universitario Dr. Peset, Valencia), Francisco Casas Maldonado (Hospital Universitario San Cecilio de Granada, Huetor Vega, Granada), Luis Manuel Entrenas Costa (Hospital Universitario Reina Sofía, Córdoba), Alicia Padilla Galo (Hospital Regional de Málaga, Málaga), Luis Puente Maestu (Hospital General Universitario Gregorio Marañón, Madrid), Marina Blanco Aparicio (Hospital Universitario A Coruña, A Coruña), Francisco-Javier González Barcala (Hospital Clínico Universitario, Santiago de Compostela, A Coruña), Aurelio Arnedillo Muñoz (Hospital Universitario Puerta del Mar, Cádiz), Gerardo Pérez Chica (Hospital Universitario de Jaén, Jaén), María Dolores Martínez Pitarch (Hospital Lluis Alcanys Xàtiva, Alboraya, Valencia), Ana Pueyo Bastida (Hospital Universitario de Burgos, Burgos), Bernardino Alcázar Navarrete (Hospital Universitario Virgen de las Nieves, Granada), Ana Gómez-Bastero Fernández (Hospital Universitario Virgen Macarena, Sevilla), Carlos Almonacid Sánchez (Hospital Universitario de Toledo, Toledo), Isabel Urrutia Landa (Hospital de Galdakao, Bilbao), Laura Vigil Giménez (Hospital Universitario Parc Tauli, Sabadell, Barcelona); Ebymar Arismendi Núñez (Hospital Clìnic de Barcelona, Barcelona). Ana Ruiz Fornells Noreña (Hospital Universitario Severo Ochoa, Leganés, Madrid), Jesús Gimeno Hernández (Hospital Clínico San Carlos, Madrid), Álvaro Sánchez Barrueco (Hospital Universitario General de Villalba y Hospital Universitario Fundación Jiménez Díaz, Madrid), Elena Mora Rivas (Hospital Universitario Ramón y Cajal, Madrid), Mayte Pinilla Urraca (Hospital Universitario Puerta de Hierro, Madrid), Desirée Méndez Brenderbache (Hospital Universitario Severo Ochoa, Leganés, Madrid), Concepción Pescador Mesonero (Hospital Universitario Severo Ochoa, Leganés, Madrid), Paloma Pinacho Martínez (Hospital Universitario de Torrejón, Torrejón de Ardoz, Madrid), María Gil Melcón (Complejo Asistencial Universitario de Salamanca, Salamanca), Luz López Flórez (Hospital Universitario La Paz, Madrid), Paula Martínez Pascual (Hospital Universitario Severo Ochoa, Leganés, Madrid), Carles Heredia Llinas (Hospital Universitario Severo Ochoa, Leganés, Madrid), Raimundo Gómez-Blasi Camacho (Hospital Universitario de Torrejón, Torrejón de Ardoz, Madrid).
Writing and editorial assistance was provided by Dr. Pablo Rivas on behalf of Content Ed Net.
Contributor Information
Christian Domingo, Pulmonology Department, Consorci Corporació Sanitària Parc Taulí, Parc Taulí, 1, 08208 Sabadell, Barcelona, Spain; Department of Medicine, Universitat Autònoma de Barcelona (UAB), Barcelona, Spain.
Jaime Gonzálvez, Primary Care, Centro de Salud Teis, Vigo, Spain.
Ignacio Dávila, Allergy Department, Hospital Clínico de Salamanca, Salamanca, Spain; Department of Biomedical and Diagnosis Sciences, Faculty of Medicine, University of Salamanca, Salamanca, Spain.
Alfonso del Cuvillo, Rhinology and Asthma Unit, UGC ORL Department, Hospital Universitario de Jerez, Jerez de la Frontera, Spain.
Marta Sánchez-Jareño, Medical Affairs, MSD, Madrid, Spain.
Luis Cea-Calvo, Medical Affairs, MSD, Madrid, Spain.
Karlos Naberán, Primary Care, Respiratory Diseases Working Group of Primary Care (GRAP), Zaragoza, Spain.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Author contributions: Christian Domingo: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing.
Jaime Gonzálvez: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing.
Ignacio Dávila: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing.
Alfonso del Cuvillo: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing.
Marta Sánchez-Jareño: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing.
Luis Cea-Calvo: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing.
Karlos Naberan: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by MSD, Spain.
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Christian Domingo: Board member and consulting fees from Sanofi, Novartis, GSK, MSD, AstraZeneca. Lectures for Sanofi, Novartis, GSK, MSD, AstraZeneca. Educational presentations for AstraZeneca, Sanofi, GSK, MSD.
Jaime Gonzálvez: Consulting fees from MSD. Lectures for Sanofi, AstraZeneca, GSK, Gebro, Menarini, Boehringer Ingelheim, Ferrer, Chiesi, MSD. Payments for article’s preparation: GSK, Boehringer Ingelheim, Menarini.
Ignacio Dávila: Consulting fees from Sanofi, AstraZeneca, GSK, Sanofi, MSD, Allergy Therapeutics, FAES. Lectures for Sanofi, AstraZeneca, GSK, Sanofi, Allergy Therapeutics, Diater, Chiesi, Alk, Leti, Teva, Thermo Fisher. Grants to institution from Thermo Fisher.
Alfonso del Cuvillo: Consulting fees from Sanofi, AstraZeneca, GSK, Alk, Menarini. Lectures for Sanofi; AstraZeneca, GSK, Alk, Menarini.
Marta Sánchez-Jareño: Full-time employee at MSD Spain.
Luis Cea-Calvo: Full-time employee at MSD Spain.
Karlos Naberán: No conflict of interest declared.
Availability of data and materials: The data sets used and analyzed during this study are available from the corresponding author on reasonable request.
References
- 1.Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 2020; 55: 1901136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGarvey L, Gibson PG.What is chronic cough? Terminology. J Allergy Clin Immunol Pract 2019; 7: 1711–1714. [DOI] [PubMed] [Google Scholar]
- 3.Morice A, Dicpinigaitis P, McGarvey L, et al. Chronic cough: new insights and future prospects. Eur Respir Rev 2021; 30: 210127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Won HK, Song WJ.Impact and disease burden of chronic cough. Asia Pac Allergy 2021; 11: e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Song WJ, Chang YS, Faruqi S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J 2015; 45: 1479–1481. [DOI] [PubMed] [Google Scholar]
- 6.Meltzer EO, Zeiger RS, Dicpinigaitis P, et al. Prevalence and burden of chronic cough in the United States. J Allergy Clin Immunol Pract 2021; 9: 4037–4044. [DOI] [PubMed] [Google Scholar]
- 7.Tobe K, Kubo T, Okuyama K, et al. Web-based survey to evaluate the prevalence of chronic and subacute cough and patient characteristics in Japan. BMJ Open Respir Res 2021; 8: e000832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Virchow JC, Li VW, Fonseca E, et al. Chronic cough in Germany: results from a general-population survey. ERJ Open Res 2022; 8: 420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Domínguez-Ortega J, Plaza V, Li VW, et al. Prevalence of chronic cough and patient characteristics in adults in Spain: a population-based cross-sectional survey. Chron Respir Dis 2022; 19: 14799731221098722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hull JH, Langerman H, Ul-Haq Z, et al. Burden and impact of chronic cough in UK primary care: a dataset analysis. BMJ Open 2021; 11: e054832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuzniar TJ.Assessment of chronic cough. BMJ Best Practice. https://bestpractice.bmj.com/topics/es-es/69 (2022, accessed 16 Jan 2022). [Google Scholar]
- 12.Molina-París J, Trigueros JA, Gómez-Sáenz JT, et al. Percepciones de médicos de familia, neumólogos y alergólogos sobre el abordaje de los pacientes con tos crónica. Resultados de una Encuesta Anónima. Semergen 2021; 47: 376–384. [DOI] [PubMed] [Google Scholar]
- 13.Jones J, Hunter D.Consensus methods for medical and health services research. BMJ 1995; 311: 376–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. The RAND/UCLA appropriateness method user’s manual . RAND, http://www.rand.org/pubs/monograph_reports/MR1269.html (2001, accessed 13 May 2020). [Google Scholar]
- 15.Irwin RS, French CL, Chang AB, et al. Classification of cough as a symptom in adults and management algorithms. Chest 2018; 153: 196–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mukae H, Kaneko T, Obase Y, et al. The Japanese respiratory society guidelines for the management of cough and sputum (digest edition). Respir Investig 2021; 59: 270–290. [DOI] [PubMed] [Google Scholar]
- 17.Kardos P, Dinh QT, Fuchs KH, et al. German Respiratory Society guidelines for diagnosis and treatment of adults suffering from acute, subacute and chronic cough. Respir Med 2020; 170: 105939. [DOI] [PubMed] [Google Scholar]
- 18.Shankar PS, Korukonda K, Bendre S, et al. Diagnoses and management of adult cough: an Indian Environmental Medical Association (EMA) position paper. Respir Med 2020; 168: 105949. [DOI] [PubMed] [Google Scholar]
- 19.Song WJ, Choi M, Lee DH, et al. The KAAACI/KDA evidence-based practice guidelines for chronic spontaneous Urticaria in Korean adults and children: part 1. Allergy Asthma Immunol Res 2020; 12: 563–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pacheco A, de Diego A, Domingo C, et al. Tos crónica. Arch Bronconeumol 2015; 51: 579–589. [DOI] [PubMed] [Google Scholar]
- 21.Michaudet C, Malaty J.Chronic cough: evaluation and management. Am Fam Physician 2017; 96: 575–580. [PubMed] [Google Scholar]
- 22.Birring SS, Prudon B, Carr AJ, et al. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax 2003; 58: 339–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.French CT, Irwin RS, Fletcher KE, et al. Evaluation of a cough-specific quality-of-life questionnaire. Chest 2002; 121: 1123–1131. [DOI] [PubMed] [Google Scholar]
- 24.Morice AH, Faruqi S, Wright CE, et al. Cough hypersensitivity syndrome: a distinct clinical entity. Lung 2011; 189: 73–79. [DOI] [PubMed] [Google Scholar]
- 25.Belafsky PC, Postma GN, Koufman JA.Validity and reliability of the reflux symptom index (RSI). J Voice 2002; 16: 274–277. [DOI] [PubMed] [Google Scholar]
- 26.Wen S, Wang S, Niu S, et al. Sensitivity and specificity of combination of Hull airway reflux questionnaire and gastroesophageal reflux disease questionnaire in identifying patients with gastroesophageal reflux-induced chronic cough. Ann Transl Med 2020; 8: 1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kahrilas PJ, Altman KW, Chang AB, et al. Chronic cough due to gastroesophageal reflux in adults. Chest 2016; 150: 1341–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kahrilas PJ, Howden CW, Hughes N, et al. Response of chronic cough to acid-suppressive therapy in patients with gastroesophageal reflux disease. Chest 2013; 143: 605–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perotin JM, Launois C, Dewolf M, et al. Managing patients with chronic cough: challenges and solutions. Ther Clin Risk Manag 2018; 14: 1041–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]