Gilbert’s syndrome (GS) is a mild liver condition, characterized by impaired ability to process bilirubin.1 Its prevalence ranges from 0.5% to 10%, depending on the population.2 Studies have shown that individuals with GS have a lower risk of atherosclerotic cardiovascular disease (ASCVD).3–5 However, no systematic comparison across different subgroups has been conducted. Using a large electronic health record (EHR), we measured the effect of GS on incident ASCVD events by age, race, and sex subgroups. Our findings highlight protection effect of GS varies among different subgroups.
We used Explorys, an EHR dataset of over 21 million individuals.6 We formed a cohort of individuals who received care between 1 January 1999 and 8 June 2022 and defined the baseline as previously described.6 We extracted comorbidities and incident ASCVD events using previously published diagnosis codes.7 We excluded individuals with prevalent ASCVD, liver disease, diabetes, pregnancy status, or low-density lipoprotein ≥190 mg/dL before baseline, resulting in 1 192 515 individuals followed for a median of 4.2 years (quartile 1: 1.9, quartile 3: 7.0). Our primary outcome was 10-year incident ASCVD expressed per 1000 patient-years (1 K PY).6 Individuals were censored at the last follow-up or end of the prediction window (note that it was infeasible to record if medical care was received elsewhere). Consistent with ASCVD guidelines, we analysed all individuals aged 40–79 years and stratified them into 10-year age strata to account for the upper limit at each age decade.7
Individuals with a consistent mild elevation of serum bilirubin (median total bilirubin >1.2 mg/dL) were classified as GS (n = 44 230; 3.7%).2 To create a comparison group, 44 230 non-GS individuals were matched using six variables including components of the Pooled Cohort Equations (sex, age, race), the PCE score, body mass index, and total number of office visits in the 2 years before baseline (as a surrogate for utilization).7 A search-based match adjusting for these variables in a generalized linear model was applied to each subgroup.8 A calliper value of 0.1 was applied for each variable to account for derivation of each variable. A 1:1 matching was applied due to subgroup limitation to match multiple non-GS individuals in smaller groups (e.g. Black individuals) and Poisson test was used to compare incidence rates. The matching was performed from a pool of 1 148 285 non-GS individuals.
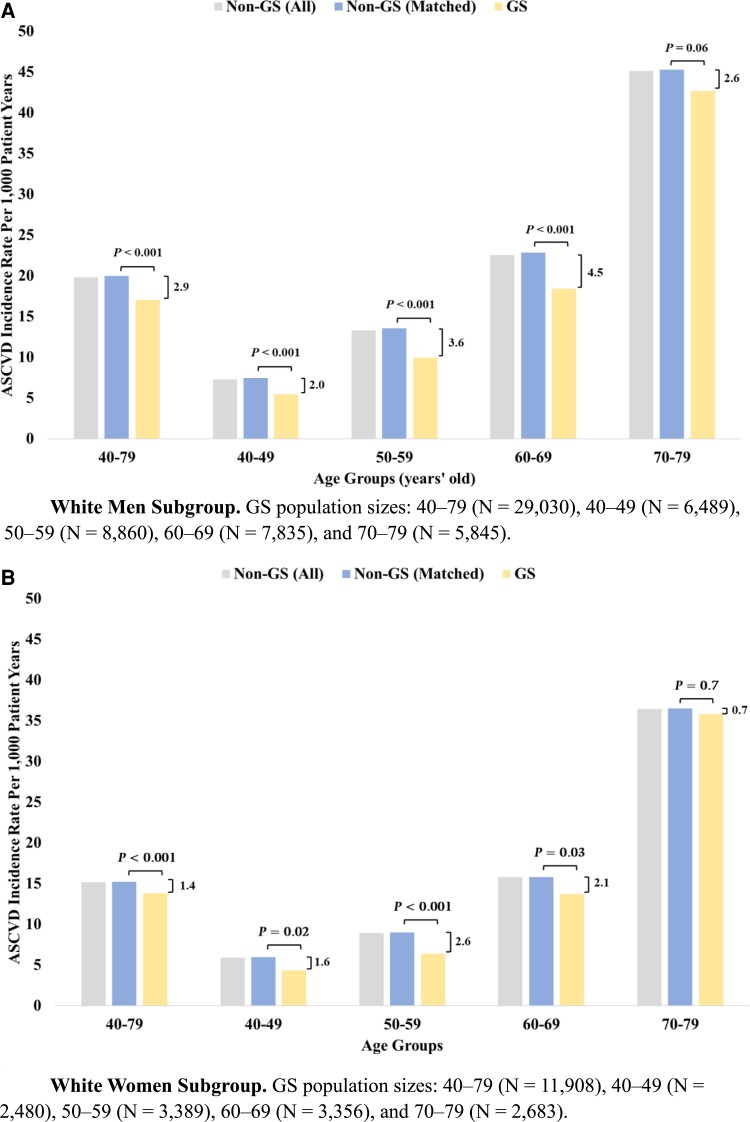
Mean total bilirubin at baseline remained constant across all age subgroups for both GS (1.6 mg/dL) and non-GS (0.6 mg/dL) individuals except for the 70–79 of age (0.7 mg/dL), and the difference in mean total bilirubin was significant in all subgroups (P < 0.001). As shown in Figure 1A, GS White men had lower ASCVD incidence rates compared to non-GS individuals (17.1 vs. 20.0 per 1 K PY, P < 0.001). Additionally, the 40–49, 50–59, and 60–69 of age subgroups had lower ASCVD rates in GS compared to non-GS (5.5 vs. 7.5, 10.0 vs. 13.5, and 18.4 vs. 22.8 per 1 K PY, P < 0.001 for all). As expected, ASCVD incidence rates increased with age for both GS and non-GS groups. As shown in Figure 1B, among White women (n = 11 908), protective effect was significant for 40–69 age group, to a lesser extent when compared to White men.
Figure 1.
Atherosclerotic cardiovascular disease incidence rate comparing Gilbert’s syndrome with matched and unmatched non-Gilbert’s syndrome individuals. P and absolute difference values are presented. (A) White men subgroup. Gilbert’s syndrome population sizes: 40–79 (n = 29 030), 40–49 (n = 6489), 50–59 (n = 8860), 60–69 (n = 7835), and 70–79 (n = 5845). (B) White women subgroup. Gilbert’s syndrome population sizes: 40–79 (n = 11 908), 40–49 (n = 2480), 50–59 (n = 3389), 60–69 (n = 3356), and 70–79 (n = 2683).
We report significant findings: (i) White individuals with GS consistently exhibited protective effect as they aged, and furthermore its magnitude increased with age (due to small sample sizes, we could not determine this effect in Black subgroups); and (ii) mean total bilirubin remained constant despite increase in protective effect magnitude with age.
Our study has some limitations: as majority in our cohort are White, analysis is limited in precision for Black individuals, lack of death data may miss fatal ASCVD events, and our observational findings should not be used to infer casual effects. Further, we acknowledge that categorization was based on race alone, and it may be beneficial to include ethnicity in future studies. Lastly, correction of confounders (e.g. comorbidities, medications) considering the outcome9 in addition to the adjustment that we applied to match GS and non-GS individuals8 may provide an additional robustness to our conclusions.
Our study extends previous research3,10 and may inform drug safety and clinical trial design. Furthermore, in addition to well-established risk factors (e.g. hypertension, high cholesterol),7 clinical decisions regarding ASCVD prevention may be improved by consideration of the potential protective effects of GS on incident ASCVD.
Ethical statement
The institutional review board of IBM approved this study and its methods, including the EHR cohort assembly using Explorys, data extraction, and analyses.
Contributor Information
Uri Kartoun, Center for Computational Health, IBM Research, 314 Main St., Cambridge, MA 02142, USA.
Akl C Fahed, Cardiovascular Disease Initiative, Broad Institute of MIT and Harvard, Cambridge, MA, USA; Division of Cardiology, Massachusetts General Hospital, Boston, MA, USA.
Shinwan Kany, Cardiovascular Disease Initiative, Broad Institute of MIT and Harvard, Cambridge, MA, USA.
Pulkit Singh, Data Sciences Platform, Broad Institute of MIT and Harvard, Cambridge, MA, USA.
Shaan Khurshid, Cardiovascular Disease Initiative, Broad Institute of MIT and Harvard, Cambridge, MA, USA; Demoulas Center for Cardiac Arrhythmias, Massachusetts General Hospital, Boston, MA, USA.
Aniruddh P Patel, Cardiovascular Disease Initiative, Broad Institute of MIT and Harvard, Cambridge, MA, USA; Division of Cardiology, Massachusetts General Hospital, Boston, MA, USA.
Puneet Batra, Data Sciences Platform, Broad Institute of MIT and Harvard, Cambridge, MA, USA.
Anthony Philippakis, Cardiovascular Disease Initiative, Broad Institute of MIT and Harvard, Cambridge, MA, USA.
Amit V Khera, Cardiovascular Disease Initiative, Broad Institute of MIT and Harvard, Cambridge, MA, USA; Division of Cardiology, Massachusetts General Hospital, Boston, MA, USA; Verve Therapeutics, Boston, MA, USA.
Steven A Lubitz, Cardiovascular Disease Initiative, Broad Institute of MIT and Harvard, Cambridge, MA, USA; Demoulas Center for Cardiac Arrhythmias, Massachusetts General Hospital, Boston, MA, USA.
Patrick T Ellinor, Cardiovascular Disease Initiative, Broad Institute of MIT and Harvard, Cambridge, MA, USA; Demoulas Center for Cardiac Arrhythmias, Massachusetts General Hospital, Boston, MA, USA.
Vibha Anand, Center for Computational Health, IBM Research, 314 Main St., Cambridge, MA 02142, USA.
Kenney Ng, Center for Computational Health, IBM Research, 314 Main St., Cambridge, MA 02142, USA.
Lead author biography
 Dr Kartoun is a Staff Research Scientist and an IBM Master Inventor, co-developer of technologies such as MELD-Plus, EMRBots, Memory-memory (M2) Authentication, and Subpopulation-based Feature Selection. Prior to joining IBM Research in 2016 Dr Kartoun worked at Microsoft Health Solutions Group and at Massachusetts General Hospital.
Dr Kartoun is a Staff Research Scientist and an IBM Master Inventor, co-developer of technologies such as MELD-Plus, EMRBots, Memory-memory (M2) Authentication, and Subpopulation-based Feature Selection. Prior to joining IBM Research in 2016 Dr Kartoun worked at Microsoft Health Solutions Group and at Massachusetts General Hospital.
Funding
None declared.
Data availability
Due to data retention policies and limitations, the original data used in this study cannot be accessed or shared.
References
- 1. Schmid R. Gilbert’s syndrome – a legitimate genetic anomaly? N Engl J Med 1995;333:1217–1218. [DOI] [PubMed] [Google Scholar]
- 2. Bosma PJ, Chowdhury JR, Bakker C, Gantla S, de Boer A, Oostra BA, Lindhout D, Tytgat GNJ, Jansen PLM, Elferink RPJO, Chowdhury NR. The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilbert’s syndrome. N Engl J Med 1995;333:1171–1175. [DOI] [PubMed] [Google Scholar]
- 3. Bulmer AC, Bakrania B, Du Toit EF, Boon AC, Clark PJ, Powell LW, Wagner KH, Headrick JP. Bilirubin acts as a multipotent guardian of cardiovascular integrity: more than just a radical idea. Am J Physiol Heart Circ Physiol 2018;315:H429–H447. [DOI] [PubMed] [Google Scholar]
- 4. Tanaka M, Fukui M, Tomiyasu K, Akabame S, Nakano K, Hasegawa G, Oda Y, Nakamura N. Low serum bilirubin concentration is associated with coronary artery calcification (CAC). Atherosclerosis 2009;206:287–291. [DOI] [PubMed] [Google Scholar]
- 5. Marconi VC, Duncan MS, So-Armah K, Re VL, Lim JK, Butt AA, Goetz MB, Rodriguez-Barradas MC, Alcorn CW, Lennox J, Beckman JA, Justice A, Freiberg M. Bilirubin is inversely associated with cardiovascular disease among HIV-positive and HIV-negative individuals in VACS (Veterans Aging Cohort Study). J Am Heart Assoc 2018;7:e007792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kartoun U, Khurshid S, Kwon BC, Patel AP, Batra P, Philippakis A, Khera AV, Ellinor PT, Lubitz SA, Ng K. Prediction performance and fairness heterogeneity in cardiovascular risk models. Sci Rep 2022;12:12542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC Jr, Sorlie P, Stone NJ, Wilson PW, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S49–S73. [DOI] [PubMed] [Google Scholar]
- 8. Sekhon JS. Multivariate and propensity score matching software with automated balance optimization: the matching package for R. J Stat Softw 2011;42:1–52. [Google Scholar]
- 9. Elze MC, Gregson J, Baber U, Williamson E, Sartori S, Mehran R, Nichols M, Stone GW, Pocock SJ. Comparison of propensity score methods and covariate adjustment: evaluation in 4 cardiovascular studies. J Am Coll Cardiol 2017;69:345–357. [DOI] [PubMed] [Google Scholar]
- 10. Vítek L, Jirsa M, Brodanová M, Kalab M, Marecek Z, Danzig V, Novotný L, Kotal P. Gilbert syndrome and ischemic heart disease: a protective effect of elevated bilirubin levels. Atherosclerosis 2002;160:449–456. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to data retention policies and limitations, the original data used in this study cannot be accessed or shared.