Abstract
We demonstrate a highly reliable minimally invasive treatment for removal of residual wire from the mandible. The patient was a 55-year-old Japanese man who was referred to our department for a fistula in his submental area. The patient had undergone open reduction and fixation with wires for mandibular fractures (left parasymphysis, right angle fracture) more than 40 years prior and mandibular tooth extraction and drainage 6 months prior. Minimally invasive endoscopy-assisted wire removal surgery was performed under general anesthesia with good visualization in a narrow surgical field. Bone resection was minimized using an ultrasonic cutting instrument with a wide choice of tip shapes.
The use of endoscopy with ultrasonic cutting tools makes it possible to effectively utilize narrow surgical fields with a small skin incision and minimal bone cutting. The advantages and disadvantages of the newer endoscopic systems in oral and maxillofacial surgical units are discussed.
Key Words: endoscopic-assisted surgery, mandible, minimally invasive surgery, postoperative infection, wire removal
In 1887, Gilmer reported a combination of intermaxillary fixation and wire fixation to treat mandibular fractures.1 Around the same time, in 1886, Hasmann described the use of a screw-and-plate osteosynthesis system to stabilize the jaw.2 Of course, the intraplate fixation systems at that time had many postoperative complications, most involving infection. With large-scale improvements in the concepts of anesthesia and sterility, as well as the 1978 elucidation by Champy et al of the mechanics of the mandible,3 the use of plates for internal fixation of mandibular fractures became more common. Until then, intraosseous wire fixation was the same clinical choice as plate fixation; in this new era intraosseous wires are rarely removed unless complications occur4 and are often left indwelling in the body.
Surgical techniques using endoscopically assisted visual fields have become the standard in many fields; using endoscopes, minimally invasive surgery has become possible in areas where direct vision is difficult. Especially in maxillofacial surgery, where surgical approaches are difficult due to the anatomical complexity and aesthetics are particularly important, endoscopic-assisted surgery is applied to various cases such as tumor resection of the facial area,4,5 cyst removal in the jawbone6,7, and salivary stone removal.8
Here, we report a minimum invasive and highly reliable endoscopically assisted surgery for removal of intraosseous wiring used for open mandible reduction and fixation more than 40 years prior.
CASE PRESENTATION
A 55-year-old Japanese man with dentures had repeated subcutaneous abscesses in the submental area for about half a year, which had worsened several months prior. Antibiotics were prescribed, but lacking improvement, he was referred to the Department of Dermatology of Kagawa University for detailed examination and treatment. On examination, it was revealed that his left mandibular canine tooth had been extracted several months prior due to purulent discharge. Therefore, he was referred to the Department of Oral and Maxillofacial Surgery at the same hospital for the purpose of closer examination related to odontogenic infection.
At the first visit to our department, the patient had a small fistula in the submental area with considerable swelling and pain. There was no source of infection or evidence of infection in the oral cavity. Patient history revealed that open reduction and fixation had been performed at another hospital for fractures of the submental area and right angle of the mandible due to a traffic accident more than 40 years prior. Conservative treatment had been selected for the bilateral mandibular articular process fractures. Subsequent follow-up was terminated. Then, several months before presentation, the left mandibular canine tooth was extracted at the family dentist’s office due to purulent drainage and significant movement, following which the oral symptoms had disappeared (Fig. 1).
FIGURE 1.
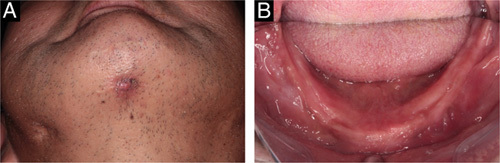
Findings at first visit. (A) The patient had a small fistula in the submental area. (B) There was no obvious source of infection or evidence of infection in the oral cavity.
Panoramic radiographs revealed steel wire ligatures in the parasymphysis and right angle of the mandible. Malformation of the bilateral mandibular condylars was also found (Fig. 2A). Computed tomography (CT) showed that the steel wires passed through the mandible in the midline and right angle of the mandible and ligated the mucosal tissue buccally and labially, respectively. In addition, in the mandibular submental region, non-union of the labial cortical bone was observed from the parasymphysis to symphysis, continuing with the apical portion of the left mandibular canine, but the lingual cortical bone was completely continuous (Fig. 2B–F).
FIGURE 2.
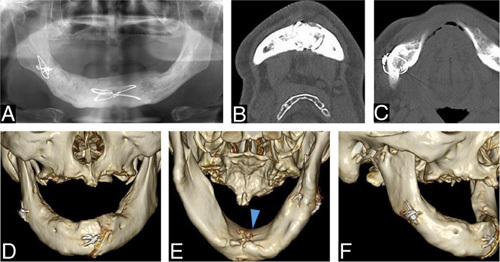
Radiological finding. (A) Panoramic radiographs revealed steel wire ligatures in the parasymphysis and right angle of the mandible. (B, C) Computed tomography axial view showing the wire penetrating the buccal to lingual aspects of the mandible. (B) Parasymphysis; (C) angle of the mandible. (D, E) Computed tomography three-dimensional view showing an intraosseous wire with a labial wire knot. Some parts are completely embedded in the bone. (Arrowhead: Complete embedment of the wire in the mandible).
In order to completely resolve the fistula, it was necessary to remove the intraosseous wire in his mandible that had caused the infection. Since the patient strongly desired minimally invasive surgery, we planned to surgically remove the intraosseous wire through a small incision using an endoscopically assisted visual field.
Endoscope-assisted Surgery Procedure
Surgery was performed on the patient with nasotracheal intubation under general anesthesia. The approach to the wire was based on the past incision line. The fistula in the submental area was removed by making a spindle-shaped skin incision around the fistula. After reaching the mandible, a 4-mm Karl Storz endoscope with a light source at a 70-degree angle was inserted intraorally to confirm wire position. Under the guidance of a rigid endoscope, the visual field was expanded sufficiently to determine the deep position of the tongue. An ultrasonic cutting instrument was used to cut the bone around the wire. Ultrasonic cutting instruments have bone-cutting tips of various angles,9 so that even with a small entry point, the target site can be easily reached with minimal cutting. The narrower, less invasive surgical field of endoscopic-assisted surgery was highly compatible with use of ultrasonic cutting instruments for minimal bone dissection. (Fig. 3, supplemental Video, Supplemental Digital Content 1, http://links.lww.com/SCS/E968)
FIGURE 3.
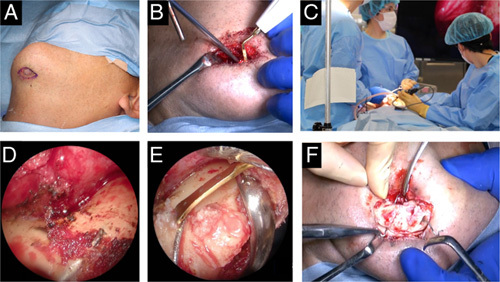
Intraoperative views. (A) Fistula removal. (B) Excess bone removal using ultrasonic cutting instruments. (C) Situations using endoscopes. It is possible for surgeons and assistants to share a narrow surgical field of view. (D) Endoscopic image on the lingual side. The expanded field of view enables clear confirmation of the condition of bones and wires. (E) Surrounding bone cutting using an ultrasonic cutting instrument in an endoscopic view. (F) Labial wire removal was finally accomplished after lingual bone removal.
No facial nerve injury, dysphagia, or facial subcutaneous hematoma was observed in the postoperative clinical course. From the 2nd day after surgery, it was possible for the patient to wear his dentures without any problems. The postoperative scar was minimal, and a good postoperative course was obtained.
DISCUSSION
In this case, we performed intraosseous wire removal from the mandible using an endoscopically assisted approach. The endoscope provided a sufficient field of view with minimal invasiveness. Conventionally for such surgeries, it has been necessary to make a larger incision to obtain the surgical field of view. However, this technology allows us to perform a safe, effective surgery that preserves the integrity of the surrounding tissue.
In this case, the wire used for open reduction and fixation several decades ago had been the source of infection and required removal. In the era when wires were generally used in tandem with plates, wire infections were less common than plate infections. Also, complications usually occur in the early postoperative period, making cases of delayed infection such as this quite rare.10 Nonetheless, there have been reported cases in which a more modern plate system required removal 10 years or more after installation due to infection or foreign body sensation.11,12 In the present case, it seems that the infection of the left mandibular canine may have spread to the osseous tissue surrounding the wire. With foreign bodies left in the maxilla or mandible, even after some years, inflammation can spread from new oral infections. In such cases it is necessary to confirm the patient’s history of open reduction and fixation, make an appropriate diagnosis, and select a treatment that resolves the route of infection.
The biggest problem when removing wires completely embedded in the mandible is the lingual procedure.13 This site requires a very large bone resection to be performed from the normal labial approach. Even when approaching from both the labial and lingual sides using open-field surgery, the visibility is very poor due to the presence of the mental spine. Therefore, a very large incision and exfoliation are required for proper and safe removal. That is why we considered the larger field of view offered by endoscopy the best surgical option for intraosseous wire removal in this case.
The use of endoscopy provides a magnified field of view. This effect not only enables efficient wire removal, but is also useful for other non-invasive, minimally bone-removing surgical procedures in the mandible. In recent years, the introduction of 4K resolution monitors has made it possible to clearly see greater detail during surgery.14 Moreover, the introduction of 4K monitors does not require a learning curve as it shares the same landmarks as the 2D devices predominantly used today.15 Therefore, further introduction in the field of oral and maxillofacial surgery is expected in the future. Using an endoscope intraoperatively offers additional advantages. Since multiple people can check the operative field at the same time, communication between operators becomes smoother. It is especially useful for rapid technical development in surgeries with very narrow fields of view like this case. Postoperative feedback and/or instruction/ training can also be provided using this method.16
A final advantage of endoscopy involves the bone-cutting device. With a narrow surgical field, rotary cutting instruments pose the risk of soft tissue damage. With a variety of angled tips to choose from, ultrasonic cutting instruments can reach narrow surgical sites while minimizing invasiveness to soft tissues.17,18 The combined use of endoscopy and ultrasonic bone-cutting equipment is highly effective in narrow-field-of-view surgeries like this one.
Endoscopic technology has its limitations: not only the operator but also the assistant must be familiar with the new techniques and perspectives. Maturity as a team is required; hence, it may be difficult to introduce endoscopy to all maxillofacial and oral surgery facilities immediately. In addition, repeated changes of gaze between the monitor and surgical field are required during surgery. This can be physically stressful for both the surgeon and the assistant.6 Utilization of a head-mounted display or a glasses-type device could lead to easier adoption of this technique.
CONCLUSION
Intraosseous wire removal from the mandible was performed using an endoscopically assisted approach. The endoscope was able to secure a sufficient field of view with minimal invasiveness. Especially when combined with ultrasonic surgical instruments, this technology allows safe oral and maxillofacial surgery that reliable preserves the integrity of the surrounding tissue.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by JSPS KAKENHI Grant Numbers JP19K19158.
Footnotes
Written patient consent was obtained to publish clinical photographs.
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's website, www.jcraniofacialsurgery.com.
Contributor Information
Shintaro Sukegawa, Email: gouwan19@gmail.com.
Ryo Miyazaki, Email: miyazaki.ryo@kagawa-u.ac.jp.
Yusuke Matsuki, Email: matsuki.yusuke@kagawa-u.ac.jp.
Masashi Iwata, Email: iwata.masashi@kagawa-u.ac.jp.
Fumi Nakai, Email: nakai.fumi.kq@kagawa-u.ac.jp.
Yasuhiro Nakai, Email: nakai.yasuhiro.wf@kagawa-u.ac.jp.
Minoru Miyake, Email: miyake.minoru@kagawa-u.ac.jp.
REFERENCES
- 1.Gilmer TL. A case of fracture of the lower jaw with remarks on treat- ment. Arch Dent 1887;4:388 [Google Scholar]
- 2.Pham Dang N, Barthélémy I, Bekara F. From rigid bone plate fixation to stable dynamic osteosynthesis in mandibular and craniomaxillo-facial surgery: Historical evolution of concepts and technical developments. J Stomatol Oral Maxillofac Surg 2019;120:229–233 [DOI] [PubMed] [Google Scholar]
- 3.Champy M, Loddé JP, Schmitt R, et al. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg 1978;6(C):14–21 [DOI] [PubMed] [Google Scholar]
- 4.Hasegawa K, Sukegawa S, Ono S, et al. Endoscopic-assisted resection of pleomorphic adenoma in the accessory parotid gland. J Med Invest 2021;68:376–380 [DOI] [PubMed] [Google Scholar]
- 5.Kishimoto T, Sukegawa S, Katase N, et al. Endoscope-assisted resection of intramuscular cavernous hemangioma within the temporal muscle. J Craniofac Surg 2019;30:193–195 [DOI] [PubMed] [Google Scholar]
- 6.Sukegawa S, Kanno T, Matsuo A, et al. Surgical strategy of endoscopically assisted periradicular surgery using novel head-mounted display system. Ann Maxillofac Surg 2020;10:186–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sukegawa S, Shimizu R, Sukegawa Y, et al. Prognostic Factors in Endodontic Surgery Using an Endoscope: A 1 Year Retrospective Cohort Study. Materials 2022;15:3353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chow A, Peters K, Schrepfer T. A novel approach to treat pediatric sialorrhea using sialendoscopy for salivary gland directed sclerotherapy. Am J Otolaryngol 2022;43:103489. [DOI] [PubMed] [Google Scholar]
- 9.Sukegawa S, Kanno T, Kawakami K, et al. Use of a piezosurgery technique to remove a deeply impacted supernumerary tooth in the anterior maxilla. Case Rep Dent 2015;2015:1–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.el-Degwi A, Mathog RH. Mandible fractures—Medical and economic considerations. Otolaryngol Head Neck Surg 1993;108:213–219 [DOI] [PubMed] [Google Scholar]
- 11.Sukegawa S, Masui M, Sukegawa-Takahashi Y, et al. Maxillofacial trauma surgery patients with titanium osteosynthesis miniplates: remove or not? J Craniofac Surg 2020;31:1338–1342 [DOI] [PubMed] [Google Scholar]
- 12.Sukegawa S, Kanno T, Manabe Y, et al. Is the removal of osteosynthesis plates after orthognathic surgery necessary? Retrospective long-term follow-up study. Int J Oral Maxillofac Surg 2018;47:1581–1586 [DOI] [PubMed] [Google Scholar]
- 13.Hickman DM, Beck R. A technical aid in transoral wiring of mandibular fractures. Ann Plast Surg 1984;12:90–91 [DOI] [PubMed] [Google Scholar]
- 14.Zwimpfer TA, Wismer C, Fellmann-Fischer B, et al. Comparison of 2D 4K vs. 3D HD laparoscopic imaging systems using a pelvitrainer model: a randomized controlled study. Updates Surg 2022;74:1137–1147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rigante M, la Rocca G, Lauretti L, et al. Preliminary experience with 4K ultra-high definition endoscope: analysis of pros and cons in skull base surgery. Acta Otorhinolaryngol Ital 2017;37:237–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Godden DRP, Robertson JM. The value of patient feedback in the audit of TMJ arthroscopy. Br Dent J 2000;188:37–39 [DOI] [PubMed] [Google Scholar]
- 17.Bilge S, Kaba YN, Demirbas AE, et al. Evaluation of the pterygomaxillary separation pattern in Le Fort I osteotomy using different cutting instruments. J Oral Maxillofac Surg 2020;78:1820–1831 [DOI] [PubMed] [Google Scholar]
- 18.Sukegawa S, Yamamoto N, Matsuyama T, et al. Factors of successful treatment using the bone lid technique in maxillofacial surgery: a pilot study. J Hard Tissue Biol 2021;30:193–198 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


