Abstract
The PTSD Checklist for DSM-5 (PCL-5) is a widely used self-rated measure of DSM-5 PTSD symptoms. The goal of this systematic review was to synthesize research on the psychometric properties of the PCL-5 to guide clinical and research applications. We focused on reliability, validity, factor structure, optimal cutoff scores, and sensitivity to clinical change indices. A systematic review of the literature following PRISMA guidelines was conducted using PubMed, PsycINFO, CINAHL, and PTSDpubs with search terms capturing selected psychometric indices of the PCL-5. The inclusion criteria were: peer-reviewed publication in English; primary focus on the PCL-5 psychometrics; empirical study; and study with adult samples. The search yielded 265 studies; 56 papers (amounting to 64 studies) met inclusion criteria and were reviewed. Findings generally indicated evidence for: acceptable internal consistency and test-retest reliability; construct validity; a 7-factor Hybrid Model; recommended cutoff scores between 31–33; and ability to index sensitivity to clinical change. To further advance knowledge and applications of the PCL-5, we need more research on abbreviated versions of the PCL-5, bifactor modeling as applied to the PCL-5, as well as on PCL-5 item difficulty estimates, discrimination parameters, and clinical change score estimates.
Keywords: Posttraumatic stress disorder, PTSD Checklist for DSM-5, psychometric indices, systematic review
Introduction
Posttraumatic stress disorder (PTSD) is a serious and potentially disabling psychiatric disorder that can emerge following exposure to actual or threatened death, serious injury, and/or sexual violence (American Psychiatric Association [APA], 2013), with a lifetime prevalence of 8.3% in the United States population (Kilpatrick et al., 2013). PTSD is associated with negative physical health outcomes (e.g., cardiovascular diseases; Pacella et al., 2013; Ryder et al., 2018); mood disorders, substance use, and suicidal behaviors (Jacobson et al., 2001; Pietrzak et al., 2011; Rytwinski et al., 2013); and impairments in social and interpersonal functioning (Alonso et al., 2011; Birkley et al., 2016; Smith et al., 2005; Wald & Taylor, 2009). PTSD is also linked with greater healthcare service utilization (Kartha et al., 2008; Klassen et al., 2013), and lower levels of income, educational attainment, and occupational success (Sareen et al., 2011; Wald & Taylor, 2009; Vilaplana-Pérez et al., 2020). Indeed, PTSD imposes substantial medical and economic burden on individuals and society. Unsurprisingly, effective and timely treatment of PTSD is imperative; hence, an accurate assessment of PTSD symptoms is critical in this regard.
The PTSD Checklist (PCL; Weathers et al., 1993; Weathers et al., 2013) is a widely used self-rated measure of PTSD symptoms. The PCL has been used to estimate provisional PTSD, quantify symptom severity, and monitor symptom change across time and in response to interventions (Weathers et al., 1993; Weathers et al., 2013). The PCL for Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) – PCL-5 – was developed to reflect changes to the DSM-5 PTSD criteria (APA, 2013). Revisions to the PCL-5 from the PCL for DSM-IV included: (1) adding three items to capture newly added PTSD symptoms (blame, negative emotions, reckless/self-destructive behaviors); (2) revising the language of certain items; and (3) changing the response scale from 1–5 to 0–4 (Blevins et al., 2015).
The PCL-5 is a 20-item self-rated scale that assesses symptoms across the four DSM-5 clusters: intrusions (Criterion B), avoidance of trauma reminders (Criterion C), negative alterations in cognitions and mood (NACM; Criterion D), and alterations in arousal and reactivity (AAR; Criterion E; APA, 2013). The PCL-5 can be used as a measure of symptom severity by summing the 20 items, or a measure of provisional PTSD by using an appropriate cutoff score or by following the DSM-5 diagnostic rules (i.e., endorsement of at least 1 B item, 1 C item, 2 D items, and 2 E items at a rating of 2 or above; Blevins et al., 2015; Wortmann et al., 2016). The PCL-5 has three formats for administration based on whether and how a Criterion A trauma is examined: without the Criterion A trauma component, with a brief Criterion A trauma assessment, and with the Life Events Checklist for DSM-5 (LEC-5) and extended Criterion A trauma assessment (Blevins et al., 2015).
The PCL-5 has undergone extensive psychometric investigations since its development and has been examined across several different languages and settings. In this systematic review, we aimed to synthesize findings from these psychometric investigations to inform strategic and appropriate uses of the PCL-5 tailored to different contexts and goals. Specifically, we synthesized data on the following psychometric properties across different PCL-5 formats (including abbreviated versions): (1) reliability (internal consistency, test-retest), (2) validity (convergent, discriminant, concurrent, predictive), (3) factor structure (i.e., structural models), (4) optimal cutoff score to determine probable PTSD diagnosis (i.e., diagnostic utility statistics), and (5) sensitivity to clinical change indices that reference clinically meaningful symptom improvement or exacerbation over time. Clinicians and researchers can use the synthesized information to gain an enhanced understanding of the strengths, weaknesses, and discriminative use of the PCL-5; to determine if and when the PCL-5 provides reliable and valid information; and to guide clinical and research decisions involving the PCL-5 (Rust & Golombok, 2014).
Method
Comprehensive Search Strategy and Article Selection
We conducted a systematic review following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021).
Eligibility information.
Inclusion criteria for studies were: (1) peer-reviewed publication in English, irrespective of the language and version of PCL-5; (2) empirical study vs. theoretical/conceptual/review paper; and (3) study with adult samples. For the current review, we synthesized literature on psychometric properties of reliability, validity, structural models, diagnostic utility statistics, and sensitivity to clinical change indices. Notably, there has been a recent review on invariance of the PTSD construct examined by different PTSD measures (Contractor et al., 2019) and on network analyses of the PTSD construct (Birkeland et al., 2020); hence we did not focus on these psychometric properties in the current review. Lastly, although we aimed to examine item difficulty and discrimination parameters of the PCL-5, we found only one study that matched pre-determined study inclusion criteria for this review; hence, we did not discuss this particular psychometric property in detail.
Information Sources and Search Strategy.
The following databases were searched: PubMed, PsycINFO, Cumulative Index of Nursing and Allied Health Literature (CINAHL), and PTSDpubs (formerly PILOTS). The following combination of terms was used to identify articles by searching the abstract, title, and key term fields: (“PTSD Checklist for DSM-5” or “PCL-5” or “PTSD Checklist 5” OR “PTSD Checklist-5” OR “Posttraumatic Stress Disorder Checklist for DSM-5” OR “PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition” OR “Posttraumatic Stress Disorder Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition” OR “DSM-5 Posttraumatic Stress Disorder Symptom*” OR “DSM-5 PTSD Symptom*” OR “DSM-5 PTSD”) AND (“psychometric*” OR “internal consistenc*” OR “reliabilit*” OR “test-retest” OR” temporal stabilit*” OR “validit*” OR “convergent validit*” OR “discriminant validit*” OR “construct validit*” OR “criterion validit*” OR “factor structure*” OR “factor analys*” OR “structural validit*” OR “confirmatory factor analys*” OR “exploratory factor analys*” OR “sensitivity to clinical change*” OR “clinical change*” OR “item response theor*” OR “diagnostic utilit*” OR “cut-off score*” OR “differential item analys*” OR “latent response theor*” OR “measurement validity” OR “structural model*”). The timeframe for the search was not constrained.
Selection Process.
See Figure 1 for a detailed description of the process. Abstracts produced by the initial search were screened independently by authors SRF and AMR. Then, for each abstract identified as potentially meeting inclusion criteria, the full-text articles were independently reviewed by SRF and HR, with author AAC cross-checking a random 20% of the articles to ascertain the reliability of the extracted information. Discussions with senior authors AAC and NHW occurred in cases of discrepancies or if questions arose regarding inclusion criteria.
Figure 1.
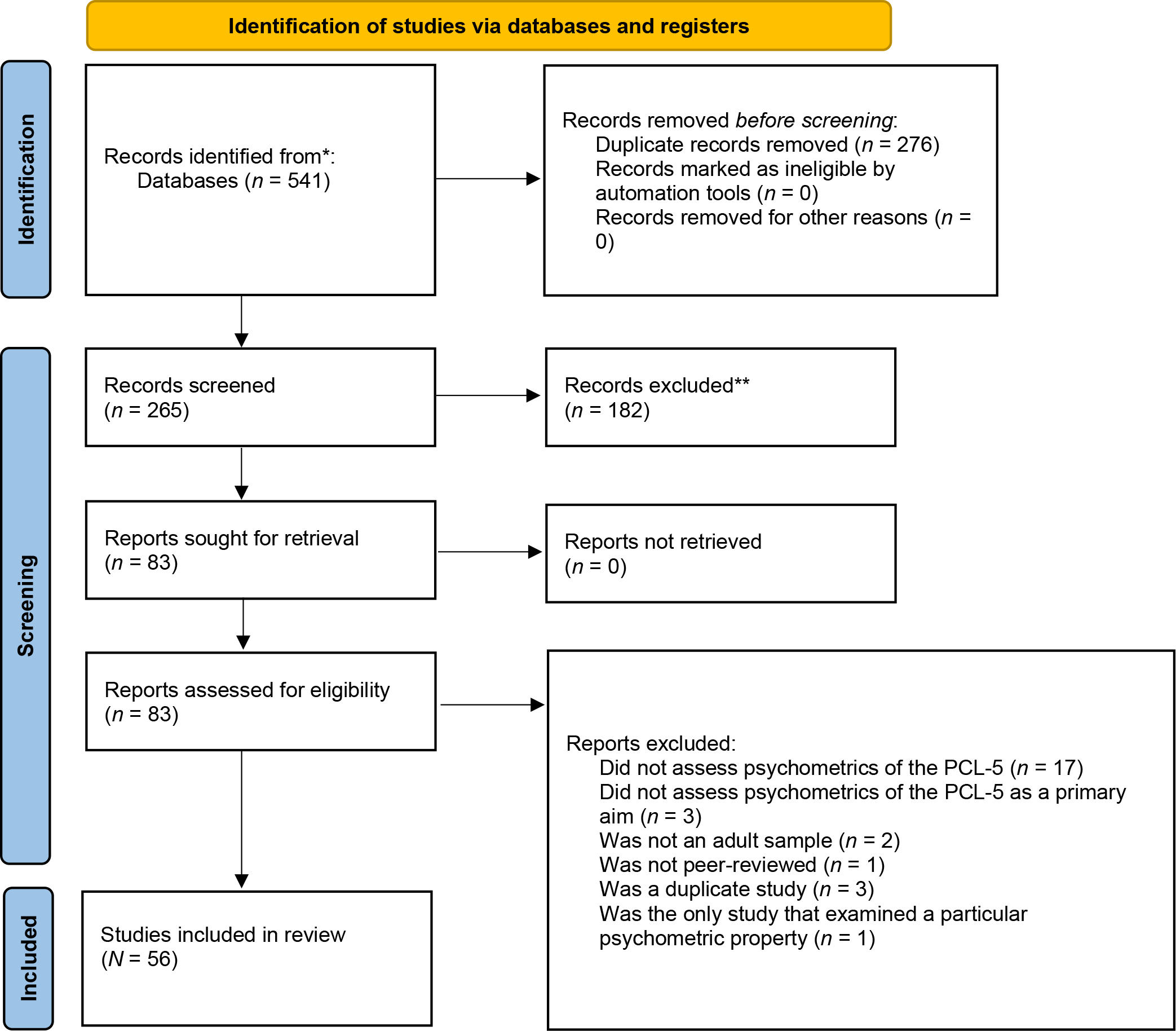
Flow diagram of review process
Data Collection Process.
Using standardized forms, the following descriptive information was extracted from each study: sample size, sample type, demographic information (age, gender, race/ethnicity), index trauma measure, and PCL-5 information (version, language, mode of administration, mean score with the standard deviation). Finally, information referencing the psychometric results from each study was extracted: reliability (internal consistency, test-retest), validity (convergent, discriminant, concurrent, predictive), structural models (information on the optimal model [fit indices, range of factor loadings, items with highest and lowest factor loadings, range of factor correlations]), diagnostic utility statistics (recommended cutoff scores, diagnostic utility estimates [sensitivity, specificity, utility, positive predictive power, negative predictive power]), and sensitivity to clinical change (kappa estimates, Pearson correlations, concordance correlations).
Data items
Reliability.
Relevant estimates of reliability for the current review included internal consistency and test-retest reliability of the PCL-5 scores (total and DSM-5 subscales). Internal consistency refers to the homogeneity of the items within an instrument and the degree to which each item reliably reflects the measured construct (Cronbach, 1951). Internal consistency is frequently measured by Cronbach’s alpha, with values ranging from 0 to 1. Recommended values indicate: ≥.90 is excellent, .80-.90 is good, .70-.80 is acceptance, .60-.70 is questionable, .50-.60 is poor, and <.50 is unacceptable (Nunally & Bernstein, 1994). Test-retest reliability evaluates the consistency of responses on a measure across multiple administrations. Test-retest reliability is often measured by the strength of the correlation between the two administrations, with recommended values ≥.60 (Cicchetti, 1994).
Validity.
Relevant estimates of validity for the current review included construct (i.e., convergent and discriminant) and criterion (i.e., concurrent and predictive) validity of the observed PCL-5 scores (total and DSM-5 subscales). Construct validity refers to the extent that a measure is accurately capturing the construct it is purported to measure. Construct validity is typically established by examining the pattern of correlations between the score on the measure of interest and scores on a series of other measures that assess constructs that would theoretically be similar (convergent validity) or dissimilar (discriminant validity) to the measured construct (Cronbach & Meehl, 1955). Criterion validity captures the extent to which a score on the measure of interest relates to a specific and independent criterion that is identified as relevant to the measured construct (Cohen et al., 1996). Criterion validity can be evaluated by examining associations between scores on measures administered simultaneously (concurrent validity) or at different timepoints (predictive validity; Engellant et al., 2016).
Evidence for construct and criterion validity is indicated by correlation patterns (i.e., direction and magnitude of relationships) that are consistent with theoretical expectations. Correlation coefficients between .10 and .30 are considered weak effects, between .30 and .50 are considered moderate effects, and >.50 are considered strong effects (Cohen, 1988). Stronger correlations (>.50) are recommended as evidence of convergent, concurrent, and predictive validity. Evidence for discriminant validity would be indicated by lower correlations (weak to moderate) with measures of unrelated constructs and by negative correlations with measures of opposite constructs (Nunally & Bernstein, 1994; Terwee et al., 2007). Construct validity is also examined using effect size estimates (ralerting-CV and rcontrast-CV) that quantify the degree of convergence between theoretically-predicted and observed correlations across measured constructs; higher values represent a greater degree of match between observed and predicted correlation patterns (Westen & Rosenthal, 2003). Lastly, group difference statistics are also used to examine validity; investigators determine whether scores differ in expected ways across groups.
Structural Models.
The factor structure is assessed to determine whether the underlying structure of the measure is consistent with the conceptual understanding of the measured construct. The factor structure is examined through the use of confirmatory factor analysis (CFA) or exploratory factor analysis (EFA). The adequacy of the model can be evaluated by examining several fit indices, such as Tucker Lewis index (TLI; Tucker & Lewis, 1973), root mean square error of approximation (RMSEA; Steiger, 1990), standardized root mean square residual (SRMR; Hu & Bentler, 1999), and comparative fit index (CFI; Bentler, 1990). A well-fitting (adequate) model has CFI and TLI values ≥.95 (.90-.94), a SRMR value of ≤.05 (.06-.08), and an RMSEA value ≤.06 (.07-.08; Hu & Bentler, 1999). Chi-square difference tests are conducted to compare the nested models (Kline, 2011). Non-nested models are compared using the Bayesian Information Criterion (BIC) and Akaike Information Criterion (AIC) values, with lower values indicating better fit (Kass & Raftery, 1995; Kline, 2011).
Diagnostic Utility Estimates.
Diagnostic utility estimates are used to evaluate the appropriateness of a measure in accurately determining the presence or absence of a specific condition (Cicchetti, 1994). This is examined by comparing the level of diagnostic agreement between a measure (e.g., PCL-5) and a reference test (e.g., gold standard assessment). Several indicators, such as sensitivity (proportion of individuals correctly identified as having the condition; true positives), specificity (proportion of individuals correctly identified as not having the condition, true negatives), positive predictive power (probability that individuals screening positive truly have the condition), and negative predictive power (probability that individuals screening negative truly do not have the condition) are examined. These metrics can be used to identify the optimal cutoff score for identifying the presence of a condition (i.e., probable PTSD).
Sensitivity to Clinical Change Index.
Sensitivity to clinical change refers to the ability of a measure to detect meaningful change in symptom severity over time (Husted et al., 2000). The PCL-5’s sensitivity to change is critical for demonstrating its practical use in capturing symptom change (e.g., improvement) following an intervention.
Results
Study Selection
The initial search resulted in 541 articles. After removing duplicates, the initial database search resulted in 265 articles. Authors SRF and AMR reviewed abstracts and excluded 182 articles based on abstract review. Next, 83 full-text articles were reviewed independently by Authors SFR and HR and 56 articles (amounting to 64 unique samples) were identified as meeting inclusion criteria. For the rest of the review, we will reference the 64 unique studies (i.e., samples) hereon for all reported estimates (e.g., frequencies) to capture more nuanced data. Samples that were studied longitudinally were counted as one sample and only baseline data are reported in results. Similarly, studies that divided one sample into multiple subsamples were counted as one sample, and only data for the full sample are reported in results. Similarly, studies that divided one sample into multiple subsamples were counted as one sample, and only data for the full sample is reported in text.
Study Characteristics
Supplemental Table 1 outlines sample characteristics and methodological information. Sample sizes ranged from 56 to 11,728. Primarily, the samples included military personnel (current duty or veteran; n = 17; 26.6%), university students (n = 16; 25.0%), treatment-seeking individuals (mental health outpatient or inpatient; n = 9; 14.1%), and community participants (recruited online and in-person; n = 8; 12.5%). The mean age ranged from 18 to 60. More than half of the studies (n = 35; 54.7%) reported information on race and ethnicity; most of these studies (n = 30; 85.7%) reported having a primarily white sample (>50%). The index trauma was primarily assessed using the Life Events Checklist for DSM-5 (LEC-5, n = 24; 37.5%; Gray et al., 2004) and the Stressful Life Events Screening Questionnaire (SLESQ, n = 8; 12.5%; Goodman et al., 1998). The PCL-5 version most commonly administered was the PCL-5 without Criterion A (n = 55; 85.9%). The PCL-5 in English was administered across most studies (n = 39; 60.9%). The PCL-5 was most frequently administered through the computer and as a self-rated measure (n = 31; 48.4%). Mean PCL-5 scores ranged from 5.5 to 55.4 across studies.
Psychometric Properties
Reliability.
A total of 51 studies (79.7%) assessed internal consistency (Cronbach’s alpha coefficients) for the PCL-5 total scale score and 18 studies (28.1%) assessed internal consistency for the PCL-5 subscale scores. Internal consistency coefficients ranged from .83 to .97 for the PCL-5 total scale score, and .57-.93, .69-.91, .74-.94, and .71-.90 across the intrusions, avoidance, NACM, and AAR subscale scores, respectively. For studies using the abbreviated versions (n = 4; 6.3%), the internal consistency coefficients ranged from .82 to .87 for the 4-item and .90 to .93 for the 8-item total scale scores. Internal consistency was also assessed using Omega coefficients in two of these studies (Hurlocker et al., 2018; Moring et al., 2019); the coefficient for the PCL-total score was .94, and the PCL-5 subscale scores had the following ranges: intrusions (.54-.94), avoidance (.38-.83), NACM (.58-.83), and AAR (.67-.77). Test-retest reliability was examined in 9 studies (17.6%) for the PCL-5 total scale score and in 4 studies (7.8%) for the PCL-5 subscale scores; time intervals ranged from one to six weeks. Several different time intervals were used: 1 week (Blevins et al., 2015), 10 days (Hall et al., 2019), 15 days (Boysan et al., 2017), an interval with a mean of 20.95 days (Ashbaugh et al., 2016), an interval with a median of 16 days (Pereira-Lima et al., 2019), 3 weeks (Carvalho et al., 2020; Krüger-Gottschalk et al., 2017), 1 month (Bovin et al., 2016), and 6 weeks (Sveen et al., 2016). Coefficients ranged from .58 to .91 for the PCL-5 total scale score and .58-.91, .49-.88, .63-.92, and .76-.89 across the intrusions, avoidance, NACM, and AAR subscale scores, respectively. For the abbreviated versions, one study found a test-retest reliability of .84 for both the 4- and 8-item scale scores. See Supplemental Table 1 for a detailed summary of reliability estimates.
Validity.
A total of 21 studies assessed validity (32.8%). Of these, 20 studies examined construct validity (i.e., construct validity broadly, convergent, and/or discriminant validity) and 4 studies examined criterion validity (i.e., criterion validity broadly, concurrent and/or predictive validity). Findings are grouped by validity type as indicated in the study, with the exception of studies that did not specify validity type; these studies were grouped under the broader construct of convergent validity. See Supplemental Table 2 for a detailed summary of validity estimates. Notably, no studies assessed predictive validity.
Construct validity.
A total of 20 studies examined construct validity (convergent/discriminant validity) of the PCL-5 scores. Of those, 17 studies (85.0%) examined convergent validity. For the complete measure, the PCL-5 total score showed moderate to strong correlations with other measures of PTSD (n=16; .44-.89). In reference to the PCL-5 subscale scores, there were also moderate to strong correlations with other measures of PTSD (intrusions [n=2; .48-.67], avoidance [n=2; .57-.57], NACM [.73], AAR [n=2; .50-.69]). The PCL-5 total score also correlated with measures of trauma/stressors (n=10; .12-.46), depression (n=12; .54-.81), anxiety (n=9; .56-.74), general mental (n=6; .32-.75) and physical (n=2; .09-.29) health, functional impairment (n=3; .59-.68), stress (n=2; .56-.62), suicidal ideation (n=3; .54-.57), substance use (n=3; .12-.26), somatic symptoms (n=3; .50-.61), sleep (n=2; .51-.62), negative cognitions (n=4; .47-.61), and dissociation (n=4; .53-.72). Although examined less frequently, the PCL-5 total score also correlated with constructs of panic (.50), sexual problems (.33), borderline personality symptoms (.68), rumination (.68), anger (.55), mania (.47), psychosis (.46), memory problems (.51), repetitive thoughts and behaviors (.70), and personality functioning (.66).
The PCL-5 intrusion subscale score correlated with other measures of the total PTSD score (.55), PTSD symptom clusters (intrusions [n=4; .53-.76], avoidance [.52], AAR [.44]), depression (n=2; .47-.62), anxiety (.60), general mental health (n=2; .61 −.66), trauma (n=4; .14-.22), dissociation (.58), stress (.47), sexual problems (.28), and sleep (.57). The PCL-5 avoidance subscale score correlated with other measures of the total PTSD score (.46), PTSD symptom clusters (intrusions [.37], avoidance [n=4, .55-.68], AAR [.34]), depression (n=2; .47-.53), anxiety (.54), general mental health (n=2; .51-.57), trauma (n=4; .01-.17), dissociation (.50), stress (.41), sexual problems (.19), and sleep (.46). The PCL-5 NACM subscale score correlated with other measures of the total PTSD score (.54), PTSD symptom clusters (intrusions [.48], avoidance [.51], NACM [.68], AAR [.41]), depression (n=2; .60-.64), anxiety (.62), general mental health (n=2; .60-.69), trauma (n=4; .10-.27), dissociation (.61), stress (.51), sexual problems (.29), and sleep (.62). The PCL-5 AAR subscale score correlated with other measures of the total PTSD score (.53), PTSD symptom clusters [intrusions [.39], avoidance [.47], AAR [n=4; .62-.81]), depression (n=2; .52 - .65), anxiety (.58), general mental health (n=2; .60 −.68), trauma (n=4; .09-.16), dissociation (.61), stress (.61), sexual problems (.33), and sleep (.51).
Construct validity was further assessed using group difference tests. Individuals with PTSD (vs. without PTSD) had a significantly higher PCL-5 total score (Fung et al., 2019). Individuals with probable PTSD (determined using recommended cutoff scores on the 4-item abbreviated PCL-5, and 8-item abbreviated PCL-5, separately) had significantly greater physical and mental functional impairment compared to those without probable PTSD. Individuals with probable PTSD (determined using recommended cutoff scores for the 20-item PCL-5) had significantly greater mental functional impairment compared to those without probable PTSD (Geier et al., 2020). As expected, demographics (higher levels of education and being married) and psychological symptoms (dissociation and depression) predicted probable PTSD on the PCL-5 among individuals who were incarcerated (Öğülmüş et al., 2020). Construct validity of a 4-item abbreviated version of the PCL-5 (B3, C2, D6, and E1) was assessed by comparing odds ratios between the abbreviated and full versions of the PCL-5 with measures of depression, generalized anxiety disorder, panic disorder, and intermittent explosive disorder; there was a high degree of similarity between the odds ratios for the abbreviated and full versions of the PCL-5.
A total of 5 studies (7.8%) explicitly examined discriminant validity. The PCL-5 total score correlated with measures of trauma (n=3; .12-.30), traumatic stress symptoms (.74), depression (n=4; .60-.64), anxiety (n=2; .40-.61), somatic symptoms (n=2; .49-.51), substance use (alcohol [n=3; .10-.40], drug [.39]), personality disorders (antisocial [.39], borderline [.58], psychopathy [.08]), schizophrenia (.49), paranoia (.43), mania (.31), social support (−.11), pain (.33), guilt (n=3; .03-.32), anger (.33), sleep (.48), and resilience (−.22). Discriminant validity was further tested by examining the statistical difference between correlations: Ashbaugh et al. (2016) found that the correlation between the PCL-5 total score and a measure of depression was lower than the correlation between the PCL-5 total score and another measure of PTSD.
Construct validity of the PCL-5 was further supported by effect size statistics that found strong matches between the observed and predicted patterns of correlations (ralerting-CV ranged from .86 to .94 and rcontrast-CV ranged from .86 to .92). This suggests a strong degree of convergence between the predicted and observed correlations between the PCL-5 total score and (1) Personality Assessment Inventory subscales (i.e., traumatic stress, depression, anxiety, borderline personality features, schizophrenia, paranoia, somatic complaints, alcohol, drug, antisocial features, and mania; Blevins et al., 2015); (2) measures of PTSD, depression, anxiety, suicidal ideation, substance use, and distress/functioning (Ito et al., 2017); and (3) measures of PTSD, trauma, anxiety, depression, guilt, anger, sleep disturbances, alcohol use, somatic symptoms, and resilience (Wortmann et al., 2016).
Criterion validity.
A total of 4 studies (19.0%) examined concurrent validity, which was tested by examining both correlations and group difference tests. Individuals with PTSD (vs. depression and healthy controls) scored higher on the PCL-5 total score and measures of dissociation, depression, and anxiety (Boysan et al., 2017a); and on measures of psychological symptoms and trauma cognitions, with two exceptions: the PCL-5 avoidance subscale and depression measure scores were not statistically different between individuals with PTSD vs. depression (Boysan et al., 2017b). Additional support for concurrent validity was found by examining associations between the PCL-5 and other measures of PTSD, including the Clinician Administered PTSD Scale for DSM-5 (CAPS-5) total severity score (.90), the Posttraumatic Symptoms Scale-10 total score (.82), and the Posttraumatic Symptoms Scale-14 total score (.85; Rosendahl et al., 2019). Similarly, the PCL-5 demonstrated strong correlations with measures of depression (.72) and anxiety (.71; Van praag et al., 2020).
Structural Models.
Extensive factor-analytical research has been conducted with the PCL versions (Armour et al., 2016). The four-factor DSM-5 Model comprising of intrusions, avoidance, NACM, AAR closely resembles the DSM-IV Emotional Numbing (EN) Model (Friedman et al., 2011); the EN Model (King et al., 1998) split PTSD’s avoidance and numbing into separate factors (Asmundson et al., 2004). Additionally, a DSM-5 Dysphoria Model (Miller et al., 2013) and a DSM-5 Dysphoric Arousal (DA) Model similar to their DSM-IV counterparts were proposed. The Dysphoria Model (Simms et al., 2002) retains the EN Model’s intrusion and avoidance factors, and combines some AAR and numbing symptoms to create PTSD’s dysphoria factor, which potentially accounts for PTSD’s comorbidity with distress-based disorders (Contractor et al., 2014; Watson, 2009). The DA Model (Elhai et al., 2011) retains the three EN Model factors, while separating the AAR cluster into dysphoric arousal and anxious arousal symptoms. Further, the six-factor Anhedonia (AN) Model (Liu et al., 2014) differentiates Criterion D symptoms of negative from positive affect (Watson, 2005, 2009), while the six-factor Externalizing Behavior (EB) Model (Tsai et al., 2015) proposes an additional externalizing behaviors factor (E1-E2) representing emotion regulation difficulties. Lastly, the Hybrid Model integrates the components of other DSM-5 models resulting in seven factors (Armour et al., 2015). See Supplemental Table 3 for PCL-5 structural models.
Among the studies examined, 47 studies (73.4%) assessed PCL-5 structural models. Of those, the Hybrid Model was tested across 34 studies (72.3%) and was found to be optimal across 28 studies (82.3%) compared to the examined alternate models. The Anhedonia Model was found to perform equally well as the Hybrid Model across 6 of these studies. Using a different approach, support was also found for a two- and four-factor bifactor model (Schmitt et al., 2018). The following are the ranges for the most commonly reported fit indices for the CFA models: RMSEA (0.0-.12), CFI (.89–1.00), TLI (.86–1.00), and SRMR (.03-.05). The factor loadings were reported by 30 studies (63.8%); 22 studies (46.8%) reported factor correlations. Item factor loadings ranged from .01 to .97 across studies; item 8 (memory impairment) had the lowest factor loading across most studies (n = 16; 53.3%) and item 7 (avoidance of trauma reminders) had the highest factor loading across most studies (n = 7; 23.3%). Factor correlations ranged from .21 to .996. See Supplemental Table 4 for detailed information on PCL-5 structural models.
Diagnostic Utility Statistics.
Notably, we report conclusive results on optimal cutoff scores as provided by authors of included studies; in the event that the authors have concluded that there is no diagnostic cutoff score, we report that as such to keep the scope of this review feasible and meaningful. Overall, 21 studies (32.3%) examined the optimal cutoff score to determine a probable PTSD diagnosis using the PCL-5; they produced a total of 30 potential cutoff scores for the full PCL-5, 3 for the 4-item abbreviated PCL-5, and 4 for the 8-item abbreviated PCL-5. These cutoff scores were most commonly examined among military personnel, university students, and treatment-seeking samples.
For the 20-item PCL-5, recommended cutoff scores ranged from 22 to 49. Recommended cutoff scores most frequently ranged between 31 and 33 (n = 11; 36.7%). Across these studies, the diagnostic utility estimates for the identified optimal scores had the following ranges: sensitivity (.50–1.00), specificity (.35-.97), diagnostic utility (.52-.95), positive predictive power (.38-.97), and negative predictive power (.63–1.00). For the 4-item abbreviated PCL-5, cutoff scores ranged from 4 to 10 (sensitivity [.76–1.00], specificity [.52-.83], diagnostic utility [.77-.87], positive predictive power [.42-.63], and negative predictive power [.83–1.0]). For the 4-item abbreviated PCL-5, Zuromski et al. (2019) did not conclusively provide an optimal cutoff score; looking at provided data, cutoff scores in the range of 6–7 seem to have an optimal combination of specificity and sensitivity broadly across the different full PCL-5 threshold values. For the 8-item abbreviated PCL-5, cutoff scores ranged from 13 to 21 (sensitivity [.79-.96], specificity [.39-.90], diagnostic utility [.77-.92], positive predictive power [.38-.71], and negative predictive power [.84-.99]). See Supplemental Table 5 for a summary of cutoff scores and diagnostic utility statistics.
Sensitivity to clinical change.
One study examined sensitivity to clinical change for the PCL-5. Wortmann et al. (2016) found that the PCL-5 showed agreement with a clinical interview for current DSM-IV PTSD symptoms (PTSD Symptom Scale–Interview [PSS-I]; Foa et al., 1993) in terms of pre- to post-treatment changes (i.e., highly correlated and of nearly equal magnitude). Specifically, kappa estimates ranged from .28 to .55, the Pearson correlation coefficient was .72, and the concordance correlation coefficient was .68.
Discussion
In this systematic review, we summarized findings on the following psychometric properties of the PCL-5: reliability, validity, structural models, diagnostic utility, and sensitivity to clinical change indices. To begin with, we note certain sample and methodological characteristics across reviewed studies. There was significant variation in the size of the samples used, with most sample sizes between 200 and 500. Indicative of less diversity across examined studies, most studies utilized data from military or university samples, and used samples that identified as predominantly white and female. Also, most studies used the LEC-5 as the index measure, the English version of the PCL-5, the PCL-5 version without Criterion A trauma assessment, and a computer-administered self-rated measure of the PCL-5.
Broadly, the PCL-5 scores (total and subscale) demonstrated acceptable internal consistency and test-retest reliability, including scores from abbreviated versions. Notably, the studies demonstrated good to excellent internal consistency for the PCL-5 total score (coefficient > .80). Internal consistency estimates of the subscale scores ranged between acceptable and excellent. Differently, the study by Sveen et al., 2016 found that the intrusion subscale score had poor internal consistency (.57); this may be due to the overall low levels of PTSD symptom severity in the sample or translation differences related to the Swedish version of the PCL-5. Scores derived from the 4-item abbreviated PCL-5 had good internal consistency and scores derived from the 8-item abbreviated PCL-5 had excellent internal consistency. Lower internal consistency coefficients for the subscale scores and for the scores of the 4-item abbreviated PCL-5 is consistent with evidence suggesting that Cronbach’s alpha estimates are influenced by the number of items in a scale (range of 2–5 items per subscale; Streiner, 2003). In these cases, omega coefficients may be a better alternative to assessing internal consistency as it appears to overcome these limitations of Cronbach’s alpha (Trizano-Hermosilla & Alvardao, 2016). Further, for the most part, the PCL-5 total and subscale scores had acceptable temporal stability across multiple administrations of the full scale and abbreviated versions (coefficients >.60), with two exceptions: poor reliability was found for the PCL-5 total score using the Filipino (Tagalog) version of the PCL-5 in a sample of migrant workers (.58; Hall et al., 2019) and for two subscale scores (intrusions [.58] and avoidance [.49]) derived from the Swedish version of the PCL-5 in a sample of parents with children with burn injuries (Sveen et al., 2016). Findings may speak to important characteristics of the sample or the version of the PCL-5. Overall, the PCL-5 appears to be a reliable measure across various populations, settings, and translations.
In support of convergent validity, and as expected, the strongest correlations were found between the PCL-5 and other measures of PTSD (with the exception of one study by Fung et al., 2019 that found a moderate correlation between the total score of the Chinese version of the PCL-5 and another measure of PTSD). Further, PCL-5 scores had moderate to strong correlations with related constructs, such as measures of functional impairment, mental health, and other disorders/symptoms (e.g., depression, anxiety, borderline personality disorder symptoms, panic, dissociation, rumination, negative cognitions, sleep disturbances, somatic complaints, repetitive thoughts/behaviors, traumatic stress symptoms, stress, memory problems, suicidal ideation). Additionally, findings supported the discriminant validity of the PCL-5 through weak to moderate (at times negative) correlations between the PCL-5 and less strongly related constructs, such as substance use, guilt, health, pain, resilience, sexual problems, social support, psychosis, schizophrenia, paranoia, mania, and personality disorders (except borderline personality disorder symptoms). Further support for construct validity of the PCL-5 was found through a strong match between observed correlations and correlations predicted by past research across measures of PTSD, psychopathology, functioning, and distress (Blevins et al., 2015; Ito et al., 2017; Wortmann et al., 2016). Relatedly, concurrent validity was demonstrated via associations between the PCL-5 scores and measures of PTSD, anxiety, and depression, as well as via results that individuals with vs. without PTSD scored higher on the PCL-5 and related measures of mental health and functioning (Boysan et al., 2017a; Boysan et al., 2017b; Rosendahl et al., 2019; Van praag et al., 2020).
This being said, we note that there were some unexpected findings such as lower-than-expected correlations between the PCL-5 scores and some measures of trauma, substance use, health (Fung et al., 2019; Hall et al., 2019; Ibrahim et al., 2018; Moodliar et al., 2020; Rosendahl et al., 2019); higher-than-expected correlations between the PCL-5 scores and unrelated constructs such as psychosis-based symptoms/disorders (Blevins et al., 2015; Ito et al., 2019); and mixed findings for the magnitude of associations between the PCL-5 scores and constructs such as anger and mania. These unexpected findings may be due to sample specific characteristics and/or selected measures. Further, moderate correlations between the PCL-5 and unrelated constructs may speak to overlapping symptomology and high rates of comorbidities between PTSD and other mental health symptoms more broadly (Brady et al., 2000). In summary, review findings generally support the convergent, discriminant, and concurrent validity of the PCL-5 scores (total and subscale), indicated by a theoretically-consistent pattern of correlations between the PCL-5 scores and examined constructs. Predictive validity was not examined among the reviewed studies; more research is needed to examine the utility of the PCL-5 in predicting theoretically-determined distal outcomes such as substance use (Jacobsen et al., 2001) and functional impairment (Byers et al., 2014).
The factor structure of PTSD informs diagnostic algorithms used in research and clinical settings, which can translate to treatment referrals and approaches (e.g., symptoms targeted in treatment); this highlights the need to examine the structural validity/models of the PCL-5. In this regard, our review primarily indicated that the Hybrid Model is optimal compared to alternate factor-analytical models (including the DSM-5 Model). Despite such strong empirical support from the factor-analytical literature, the Hybrid Model has been the topic of ongoing debate. Researchers caution against reconfiguring PTSD symptom clusters based on fit indices alone, as fit indices may be distorted by the complexity of the model (i.e., more complex models may account for more variance resulting in better fit statistics) and under-identified factors (i.e., factors defined by only two indicators; Rasmussen et al., 2019). Additionally, the clinical utility of these complex models may be compromised (Silverstein et al., 2018). In this regard, while the current review indicates that the current DSM-5 Model may not optimally represent PTSD’s latent structure, we need to acknowledge the feasibility/utility of its clinical applications and its parsimony when making decisions about what diagnostic structure to use. Complicating this issue, our review findings identified the Anhedonia Model as an equally well-performing model across multiple studies (Blevins et al., 2015; Bovin et al., 2016; Morderno et al., 2020; Shevlin et al., 2017; Van Praag et al., 2020); this model may be optimal due to parsimony and having fewer latent factors identified by a small number of items. Beyond the need for future research on PCL-5’s optimal latent structure, studies may also benefit from considering bifactor modeling to examine the factor structure of the PCL-5; bifactor modeling is a multilevel approach that includes a general factor to represent the shared variance and separate unique factors to represent the variance unexplained by the general factor.
Recommended cutoff scores for the PCL-5 varied significantly across each study, ranging from 23–49 for the full PCL-5. Broadly, across the reviewed studies, recommended cutoff scores that maximized diagnostic utility most frequently ranged between 31 and 33. For the abbreviated PCL-5 versions, the optimal cutoff scores ranged between 4 and 10 for the 4-item scale and 13 and 21 for the 8-item scale. Consistent with findings for the PCL for DSM-IV (McDonald & Calhoun, 2010), our review results suggest that a universal cutoff score applicable across diverse samples and settings does not exist for the PCL-5. Variations in the cutoff scores may be due to methodological and contextual factors, such as sample/demographic characteristics, severity and prevalence estimates for PTSD and disorders, comorbidities, and the type of reference standards (McDonald & Calhoun, 2010; Whiting et al., 2004). Importantly, identifying an appropriate cutoff score will vary based on the user’s priority and goals. Specifically, there is an important trade-off between sensitivity and specificity (i.e., higher sensitivity results in lower specificity and vice versa); thus, a cutoff score with greater sensitivity may be chosen if there is a more critical need to confirm tentative diagnoses (i.e., minimize false negatives), whereas greater specificity may be more beneficial in cases where it would be of greater value to rule out potential diagnoses (i.e., minimize false positives). Also, cut-off score considerations are contextually dependent; for instance, false positives could lead to costly and unnecessary treatments and false negatives could lead to failures in treatment (Trevethan, 2017). Our review provides a summary of cutoff scores (with associated diagnostic estimates) that can be used as a guide to identify the most appropriate cutoff score based on goals and priorities. Notably, and an important area for future research, only one study examined PCL-5’s sensitivity to clinical change (Wortmann et al., 2016). Findings indicated that the PCL-5 was able to detect meaningful symptom changes across a treatment-seeking military sample.
We need to consider some caveats and limitations when interpreting findings from this review. First, psychometric investigations of the PCL-5 are limited by the data reported by each study and specific to the particular population and setting of that study. Second, studies differed on their conceptualization of what serves as evidence of the different types of validity. For instance, similar constructs were used as evidence for both convergent and discriminant validity (e.g., mania and anger). Third, there are limited investigations on predictive validity, sensitivity to clinical change, and item difficulty/discrimination parameters. Fourth, the primary mode of administering the PCL-5 in the reviewed studies was via an online format. Research is needed to examine any potential differences in the psychometric properties of the PCL-5 by mode of administration, considering that research and clinical settings may vary in their method of administering the PCL-5 and that the mode of administration can influence data quality, as responses may vary due to specific factors related to the method of administration (Bowling, 2005).
In summary, the current systematic review indicated that the PCL-5 is a psychometrically strong measure of PTSD symptoms across contextually-distinct and demographically-varied samples. As a comprehensive guide, this review can be used to inform both clinical and research applications of the PCL-5, as well as future research on PCL-5 psychometrics. Specifically, based on data from most studies, our review findings suggest (1) good to excellent internal consistency for the PCL-5 total score, (2) acceptable to excellent internal consistency for the PCL-5 subscale scores, (3) strong support for construct validity, (4) strongest evidence for a 7 factor structure of PTSD symptoms (Hybrid Model), (5) recommended cutoff scores between 31 and 33 for the 20-item PCL-5 total score, and (6) promising evidence of sensitivity to clinical change. Further, promising evidence for strong psychometrics for the PCL-5 abbreviated versions supports their meaningful use in intensive longitudinal study designs to minimize participant burden and maximize the richness of collected data. Findings also highlight important avenues of future work on the psychometric properties of the PCL-5, including examining how the mode of administration may impact psychometric properties, utilizing bifactor models, estimating item difficulty and discrimination parameters, and capturing clinical change scores across different contexts. Such an enhanced understanding of the psychometric properties of the PCL-5 can facilitate appropriate and valid applications of this measure across different clinical and research contexts, and help to outline relative strengths and weaknesses of the PCL-5.
Supplementary Material
Public Health Statement.
This study reviewed the literature on the PTSD Checklist for DSM-5 (PCL-5) and found that it is an accurate and reliable measure for assessing PTSD symptom severity and diagnosis across a wide range of populations. This study can be used to inform appropriate and strategic use of the PCL-5. Accurate and reliable measurements of PTSD are necessary for detecting, intervening, and monitoring PTSD.
Funding:
This work was supported, in part, by grants from the National Institutes of Health awarded to NHW (K23DA039327 and P20GM125507) and to SRF (F31DA051167). Compliance with Ethical Standards: The current study is in compliance with all ethical standards.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Ethical approval: The current study is a systematic review and thus exempt from IRB approval.
References
- *Acquaye HE (2018). Assessing the factor structure of models for posttraumatic stress disorder symptoms in a war-related civilian sample. Counseling Outcome Research and Evaluation, 9(2), 90–101. 10.1080/21501378.2018.1461532 [DOI] [Google Scholar]
- Alonso J, Petukhova M, Vilagut G, Chatterji S, Heeringa S, Üstün TB, ... & Kessler RC. (2011). Days out of role due to common physical and mental conditions: results from the WHO World Mental Health surveys. Molecular psychiatry, 16(12), 1234–1246. 10.1038/mp.2010.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Armour C, Contractor A, Shea T, Elhai JD, & Pietrzak RH (2016). Factor structure of the PTSD checklist for DSM-5: relationships among symptom clusters, anger, and impulsivity. The Journal of Nervous and Mental Disease, 204(2), 108–115. 10.1097/NMD.0000000000000430 [DOI] [PubMed] [Google Scholar]
- Armour C, Mullerova J, & Elhai JD (2016). A systematic literature review of PTSD’s latent structure in the Diagnostic and Statistical Manual of Mental Disorders: DSM-IV to DSM-5. Clinical Psychology Review, 44, 60–74. 10.1016/j.cpr.2015.12.003 [DOI] [PubMed] [Google Scholar]
- *Armour C, Tsai J, Durham TA, Charak R, Biehn TL, Elhai JD, & Pietrzak RH (2015). Dimensional structure of DSM-5 posttraumatic stress symptoms: Support for a hybrid Anhedonia and Externalizing Behaviors model. Journal of Psychiatric Research, 61, 106–113. 10.1016/j.jpsychires.2014.10.012 [DOI] [PubMed] [Google Scholar]
- Armour C, Tsai J, Durham TA, Charak R, Biehn TL, Elhai JD, & Pietrzak RH (2015). Dimensional structure of DSM-5 posttraumatic stress symptoms: Support for a hybrid Anhedonia and Externalizing behaviors model. Journal of Psychiatric Research, 61, 106–113. 10.1016/j.jpsychires.2014.10.012 [DOI] [PubMed] [Google Scholar]
- *Ashbaugh AR, Houle-Johnson S, Herbert C, El-Hage W, & Brunet A (2016). Psychometric validation of the English and French versions of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). PloS One, 11(10), e0161645. 10.1371/journal.pone.0161645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson GJG, Stapleton JA, & Taylor S (2004). Are avoidance and numbing distinct PTSD symptom clusters? Journal of Traumatic Stress, 17, 467–475. 10.1007/Sl0960-004-5795 [DOI] [PubMed] [Google Scholar]
- *Barbieri A, Visco-Comandini F, Alunni Fegatelli D, Schepisi C, Russo V, Calò F, ... & Stellacci A. (2019). Complex trauma, PTSD and complex PTSD in African refugees. European Journal of Psychotraumatology, 10(1), 1700621. 10.1080/20008198.2019.1700621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- *Biehn TL, Elhai JD, Seligman LD, Tamburrino M, Armour C, & Forbes D (2013). Underlying dimensions of DSM-5 posttraumatic stress disorder and major depressive disorder symptoms. Psychological Injury and Law, 6(4), 290–298. 10.1007/s12207-013-9177-4 [DOI] [Google Scholar]
- Birkeland MS, Greene T, & Spiller TR (2020). The network approach to posttraumatic stress disorder: A systematic review. European Journal of Psychotraumatology, 11(1), 1700614. 10.1080/20008198.2019.1700614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birkley EL, Eckhardt CI, & Dykstra RE (2016). Posttraumatic stress disorder symptoms, intimate partner violence, and relationship functioning: A meta-analytic review. Journal of Traumatic Stress, 29(5), 397–405. 10.1002/jts.22129 [DOI] [PubMed] [Google Scholar]
- *Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- *Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Bowling A (2005). Mode of questionnaire administration can have serious effects on data quality. Journal of Public Health, 27(3), 281–291. 10.1093/pubmed/fdi031 [DOI] [PubMed] [Google Scholar]
- *Boysan M, Guzel Ozdemir P, Ozdemir O, Selvi Y, Yilmaz E, & Kaya N (2017). Psychometric properties of the Turkish version of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, (PCL-5). Psychiatry and Clinical Psychopharmacology, 27(3), 300–310. 10.1080/24750573.2017.1342769 [DOI] [Google Scholar]
- *Boysan M, Guzel Ozdemir P, Yilmaz E, Selvi Y, Özdemir O, & Celal Kefeli M (2017). Psychometric properties of the Turkish version of the Clinician-Administered PTSD scale for diagnostic and statistical manual of mental disorders, (Turkish CAPS-5). Psychiatry and Clinical Psychopharmacology, 27(2), 173–184. 10.1080/24750573.2017.1326746 [DOI] [Google Scholar]
- Brady KT, Killeen TK, Brewerton T, & Lucerini S (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. Journal of Clinical Psychiatry, 61, 22–32. [PubMed] [Google Scholar]
- Byers AL, Covinsky KE, Neylan TC, & Yaffe K (2014). Chronicity of posttraumatic stress disorder and risk of disability in older persons. JAMA Psychiatry, 71(5), 540–546. 10.1001/jamapsychiatry.2014.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Caldas SV, Contractor AA, Koh S, & Wang L (2020). Factor Structure and Multi-Group Measurement Invariance of Posttraumatic Stress Disorder Symptoms Assessed by the PCL-5. Journal of Psychopathology and Behavioral Assessment, 42(2), 364–376. 10.1007/s10862-020-09800-z [DOI] [Google Scholar]
- *Carvalho T, da Motta C, & Pinto-Gouveia J (2020). Portuguese version of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Comparison of latent models and other psychometric analyses. Journal of Clinical Psychology, 76(7), 1267–1282. 10.1002/jclp.22930 [DOI] [PubMed] [Google Scholar]
- *Cheng P, Xu LZ, Zheng WH, Ng RM, Zhang L, Li LJ, & Li WH (2020). Psychometric property study of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) in Chinese healthcare workers during the outbreak of corona virus disease 2019. Journal of Affective Disorders, 277, 368–374. 10.1016/j.jad.2020.08.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti DV (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment, 6(4), 284–290. 10.1037/1040-3590.6.4.284 [DOI] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences, 2nd ed. Hillsdale, NJ: Erlbaum [Google Scholar]
- Cohen RJ, Swerdlik ME, & Phillips SM (1996). Psychological testing and assessment: An introduction to tests and measurement (3rd ed.). Mayfield Publishing Co. [Google Scholar]
- *Contractor AA, Caldas SV, Dolan M, Lagdon S, & Armour C (2018). PTSD’s factor structure and measurement invariance across subgroups with differing count of trauma types. Psychiatry Research, 264, 76–84. 10.1016/j.psychres.2018.03.065 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Caldas SV, Dolan M, Natesan P, & Weiss NH (2019). Invariance of the construct of posttraumatic stress disorder: A systematic review. Journal of Traumatic Stress, 32(2), 287–298. 10.1002/jts.22389 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Durham TA, Brennan JA, Armour C, Wutrick HR, Frueh CB, & Elhai JD (2014). DSM-5 PTSD’s symptom dimensions and relations with major depression’s symptom dimensions in a primary care sample. Psychiatry Research, 215, 146–153. 10.1016/j.psychres.2013.10.015 [DOI] [PubMed] [Google Scholar]
- *Contractor AA, Weiss NH, Dolan M, & Mota N (2020). Examination of the structural relations between posttraumatic stress disorder symptoms and reckless/self-destructive behaviors. International Journal of Stress Management, 27(1), 35–44. 10.1037/str0000133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronbach LJ (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16(3), 297–334. [Google Scholar]
- Cronbach LJ, & Meehl PE (1955). Construct validity in psychological tests. Psychological Bulletin, 52(4), 281–302. 10.1037/h0040957 [DOI] [PubMed] [Google Scholar]
- *Drake-Brooks MM, Hinkson KD Jr, Osteen P, & Bryan CJ (2020). Examining the DSM-5 latent structures of posttraumatic stress disorder in a national sample of student veterans. Journal of Anxiety Disorders, 74, 102262. 10.1016/j.janxdis.2020.102262 [DOI] [PubMed] [Google Scholar]
- *Durham TA, Byllesby BM, Lv X, Elhai JD, & Wang L (2018). Anger as an underlying dimension of posttraumatic stress disorder. Psychiatry Research, 267, 535–540. 10.1016/j.psychres.2018.06.011 [DOI] [PubMed] [Google Scholar]
- *Eddinger JR, & McDevitt-Murphy ME (2017). A confirmatory factor analysis of the PTSD checklist 5 in veteran and college student samples. Psychiatry Research, 255, 219–224. 10.1016/j.psychres.2017.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Biehn TL, Armour C, Klopper JL, Frueh BC, & Palmieri PA (2011). Evidence for a unique PTSD construct represented by PTSD’s D1–D3 symptoms. Journal of Anxiety Disorders, 25, 340–345. 10.1016/j.janxdis.2010.10.007 [DOI] [PubMed] [Google Scholar]
- Engellant KA, Holland DD, & Piper RT (2016). Assessing convergent and discriminant validity of the motivation construct for the technology integration education (TIE) model. Journal of Higher Education Theory & Practice, 16(1). [Google Scholar]
- *Erwin MC, Charak R, Durham TA, Armour C, Lv X, Southwick SM, ... & Pietrzak RH. (2017). The 7-factor hybrid model of DSM-5 PTSD symptoms and alcohol consumption and consequences in a national sample of trauma-exposed veterans. Journal of Anxiety Disorders, 51, 14–21. 10.1016/j.janxdis.2017.08.001 [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, & Rothbaum BO (1993). Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress, 6(4), 459–473. 10.1002/jts.2490060405 [DOI] [Google Scholar]
- Friedman MJ, Resick PA, Bryant RA, & Brewin CR (2011). Considering PTSD for DSM-5. Depression and Anxiety, 28, 750–769. 10.1002/da.20767 [DOI] [PubMed] [Google Scholar]
- *Fung HW, Chan C, Lee CY, & Ross CA (2019). Using the post-traumatic stress disorder (PTSD) checklist for DSM-5 to screen for PTSD in the Chinese context: a pilot study in a psychiatric sample. Journal of Evidence-Based Social Work, 16(6), 643–651. 10.1080/26408066.2019.1676858 [DOI] [PubMed] [Google Scholar]
- *Geier TJ, Hunt JC, Hanson JL, Heyrman K, Larsen SE, Brasel KJ, & deRoon-Cassini TA (2020). Validation of Abbreviated Four-and Eight-Item Versions of the PTSD Checklist for DSM-5 in a Traumatically Injured Sample. Journal of Traumatic Stress, 33(3), 218–226. 10.1002/jts.22478 [DOI] [PubMed] [Google Scholar]
- *Geier TJ, Hunt JC, Nelson LD, Brasel KJ, & deRoon-Cassini TA (2019). Detecting PTSD in a traumatically injured population: The diagnostic utility of the PTSD Checklist for DSM-5. Depression and Anxiety, 36(2), 170–178. 10.1002/da.22873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman LA, Corcoran C, Turner K, Yuan N, & Green BL (1998). Assessing traumatic event exposure: General issues and preliminary findings for the Stressful Life Events Screening Questionnaire. Journal of Traumatic Stress,11(3), 521–542. 10.1023/A:1024456713321 [DOI] [PubMed] [Google Scholar]
- *Grau P, Garnier-Villarreal M, & Wetterneck C (2019). An analysis of the latent factor structure of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) in a PTSD partial hospitalization program. Traumatology, 25(4), 269–274. 10.1037/trm0000200 [DOI] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric properties of the life events checklist. Assessment, 11(4), 330–341. 10.1177/1073191104269954 [DOI] [PubMed] [Google Scholar]
- *Hall BJ, Yip PS, Garabiles MR, Lao CK, Chan EW, & Marx BP (2019). Psychometric validation of the PTSD Checklist-5 among female Filipino migrant workers. European Journal of Psychotraumatology, 10(1), 1571378. 10.1080/20008198.2019.1571378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- *Hurlocker MC, Vidaurri DN, Cuccurullo LAJ, Maieritsch K, & Franklin CL (2018). Examining the latent structure mechanisms for comorbid posttraumatic stress disorder and major depressive disorder. Journal of Affective Disorders, 229, 477–482. 10.1016/j.jad.2017.12.076 [DOI] [PubMed] [Google Scholar]
- Husted JA, Cook RJ, Farewell VT, & Gladman DD (2000). Methods for assessing responsiveness: a critical review and recommendations. Journal of Clinical Epidemiology, 53(5), 459–468. 10.1016/S0895-4356(99)00206-1 [DOI] [PubMed] [Google Scholar]
- *Ibrahim H, Ertl V, Catani C, Ismail AA, & Neuner F (2018). The validity of Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq. BMC Psychiatry, 18(1), 1–8. 10.1186/s12888-018-1839-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ito M, Takebayashi Y, Suzuki Y, & Horikoshi M (2019). Posttraumatic stress disorder checklist for DSM-5: Psychometric properties in a Japanese population. Journal of Affective Disorders, 247, 11–19. 10.1016/j.jad.2018.12.086 [DOI] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, & Kosten TR (2001). Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. American Journal of Psychiatry, 158(8), 1184–1190. 10.1176/appi.ajp.158.8.1184 [DOI] [PubMed] [Google Scholar]
- Kartha A, Brower V, Saitz R, Samet JH, Keane TM, & Liebschutz J (2008). The impact of trauma exposure and post-traumatic stress disorder on healthcare utilization among primary care patients. Medical Care, 46(4), 388. 10.1097/MLR.0b013e31815dc5d2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kass RE, & Raftery AE (1995). Bayes factors. Journal of the American Statistical Association, 90(430), 773–795. [Google Scholar]
- *Keane TM, Rubin A, Lachowicz M, Brief D, Enggasser JL, Roy M, Hermos J, Helmuth E, & Rosenbloom D (2014). Temporal stability of DSM–5 posttraumatic stress disorder criteria in a problem-drinking sample. Psychological Assessment, 26(4), 1138–1145. 10.1037/a0037133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy CE, Fonner VA, Armstrong KA, Denison JA, Yeh PT, O’Reilly KR, & Sweat MD (2019). The Evidence Project risk of bias tool: assessing study rigor for both randomized and non-randomized intervention studies. Systematic reviews, 8(1), 1–10. 10.1186/s13643-018-0925-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DW, Leskin GA, King LA, & Weathers FW (1998). Confirmatory factor analysis of the Clinician-Administered PTSD scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment, 10(2), 90–96. 10.1037/1040-3590.10.2.90 [DOI] [Google Scholar]
- Klassen BJ, Porcerelli JH, & Markova T (2013). The effects of PTSD symptoms on health care resource utilization in a low-income, urban primary care setting. Journal of Traumatic Stress, 26(5), 636–639. 10.1002/jts.21838 [DOI] [PubMed] [Google Scholar]
- Kline RB (2011). Principles and practice of structural equation modeling. (3rd ed.). New York, NY.: The Guilford Press. [Google Scholar]
- *Krüger-Gottschalk A, Knaevelsrud C, Rau H, Dyer A, Schäfer I, Schellong J, & Ehring T (2017). The German version of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): psychometric properties and diagnostic utility. BMC Psychiatry, 17(1), 1–9. 10.1186/s12888-017-1541-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Levitt EE, Syan SK, Sousa S, Costello MJ, Rush B, Samokhvalov AV, ... & MacKillop J. (2021). Optimizing screening for depression, anxiety disorders, and posttraumatic stress disorder in inpatient addiction treatment: A preliminary investigation. Addictive Behaviors, 112, 106649. 10.1016/j.addbeh.2020.106649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Liu P, Wang L, Cao C, Wang R, Zhang J, Zhang B, ... & Elhai JD. (2014). The underlying dimensions of DSM-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivors. Journal of Anxiety Disorders, 28(4), 345–351. 10.1016/j.janxdis.2014.03.008 [DOI] [PubMed] [Google Scholar]
- Liu P, Wang L, Cao C, Wang R, Zhang J, Zhang B, Wu Q, Zhang H, Zhao Z, Fan G, & Elhai JD (2014). The underlying dimensions of DSM-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivours. Journal of Anxiety Disorders, 28, 345–351. 10.1016/j.janxdis.2014.03.008 [DOI] [PubMed] [Google Scholar]
- *Makhubela M (2018). Latent structure of the Post-Traumatic Stress Disorder (PTSD) Checklist for DSM-5 (PCL-5) in South African mortuary workers. Journal of Psychology in Africa, 28(3), 206–211. 10.1080/14330237.2018.1475909 [DOI] [Google Scholar]
- McDonald SD, & Calhoun PS (2010). The diagnostic accuracy of the PTSD checklist: a critical review. Clinical Psychology Review, 30(8), 976–987. 10.1016/j.cpr.2010.06.012 [DOI] [PubMed] [Google Scholar]
- *McSweeney LB, Koch EI, Saules KK, & Jefferson S (2016). Exploratory factor analysis of Diagnostic and Statistical Manual, criteria for posttraumatic stress disorder. The Journal of Nervous and Mental Disease, 204(1), 9–14. 10.1097/NMD.0000000000000390 [DOI] [PubMed] [Google Scholar]
- *Moodliar R, Russo J, Bedard-Gilligan M, Moloney K, Johnson P, Seo S, ... & Zatzick D. (2020). A Pragmatic Approach to Psychometric Comparisons between the DSM-IV and DSM-5 Posttraumatic Stress Disorder (PTSD) Checklists in Acutely Injured Trauma Patients. Psychiatry, 1–12. 10.1080/00332747.2020.1762396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mordeno IG, & Hall BJ (2017). DSM-5-based latent PTSD models: assessing structural relations with GAD in Filipino post-relocatees. Psychiatry Research, 258, 1–8. 10.1016/j.psychres.2017.09.057 [DOI] [PubMed] [Google Scholar]
- *Mordeno IG, Carpio JGE, Nalipay MJN, & Saavedra RLJ (2017). PTSD’s underlying dimensions in typhoon Haiyan survivors: Assessing DSM-5 symptomatology-based PTSD models and their relation to posttraumatic cognition. Psychiatric Quarterly, 88(1), 9–23. 10.1007/s11126-016-9429-z [DOI] [PubMed] [Google Scholar]
- *Mordeno IG, Luzano JGC, Mordeno ER, & Ferolino MAL (2020). Investigating the latent dimensions of posttraumatic stress disorder and the role of anxiety sensitivity in combat-exposed Filipino soldiers. Military Psychology, 32(3), 223–236. 10.1080/08995605.2020.1724594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mordeno IG, Nalipay MJN, Sy DJS, & Luzano JGC (2016). PTSD factor structure and relationship with self-construal among internally displaced persons. Journal of Anxiety Disorders, 44, 102–110. 10.1016/j.janxdis.2016.10.013 [DOI] [PubMed] [Google Scholar]
- *Moring JC, Nason E, Hale WJ, Wachen JS, Dondanville KA, Straud C, ... & STRONG STAR Consortium. (2019). Conceptualizing comorbid PTSD and depression among treatment-seeking, active duty military service members. Journal of Affective Disorders, 256, 541–549. 10.1016/j.jad.2019.06.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Murphy D, Ross J, Ashwick R, Armour C, & Busuttil W (2017). Exploring optimum cut-off scores to screen for probable posttraumatic stress disorder within a sample of UK treatment-seeking veterans. European Journal of Psychotraumatology, 8(1), 1398001. 10.1080/20008198.2017.1398001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnally JC, & Bernstein IH (1994). Psychometric Theory (3rd ed.). New York: McGraw-Hill. [Google Scholar]
- *Öğülmüş S, Boysan M, Fidan-Acar Ö, & Koca H (2020). The underlying dimensions of DSM-5 posttraumatic stress disorder (PTSD) and their relationships with mental and somatoform dissociation, depression and anxiety among jail inmates. British Journal of Guidance & Counselling, 48(3), 374–393. 10.1080/03069885.2020.1738338 [DOI] [Google Scholar]
- Pacella ML, Hruska B, & Delahanty D (2013). The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. Journal of Anxiety Disorders, 27, 33–46. 10.1016/j.janxdis.2012.08.004 [DOI] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, ... & Moher D. (2021). Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. Journal of Clinical Epidemiology, 134, 103–112. 10.1016/j.jclinepi.2021.02.003 [DOI] [PubMed] [Google Scholar]
- *Pereira-Lima K, Loureiro SR, Bolsoni LM, Apolinario da Silva TD, & Osório FL (2019). Psychometric properties and diagnostic utility of a Brazilian version of the PCL-5 (complete and abbreviated versions). European Journal of Psychotraumatology, 10(1), 1581020. 10.1080/20008198.2019.1581020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25(3), 456–465. 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Pietrzak RH, Tsai J, Armour C, Mota N, Harpaz-Rotem I, & Southwick SM (2015). Functional significance of a novel 7-factor model of DSM-5 PTSD symptoms: Results from the National Health and Resilience in Veterans Study. Journal of Affective Disorders, 174, 522–526. 10.1016/j.jad.2014.12.007 [DOI] [PubMed] [Google Scholar]
- *Price M, Szafranski DD, van Stolk-Cooke K, & Gros DF (2016). Investigation of abbreviated 4 and 8 item versions of the PTSD Checklist 5. Psychiatry Research, 239, 124–130. 10.1016/j.psychres.2016.03.014 [DOI] [PubMed] [Google Scholar]
- *Rosendahl J, Kisyova H, Gawlytta R, & Scherag A (2019). Comparative validation of three screening instruments for posttraumatic stress disorder after intensive care. Journal of Critical Care, 53, 149–154. 10.1016/j.jcrc.2019.06.016 [DOI] [PubMed] [Google Scholar]
- *Ross J, Kaliská L, Halama P, Lajčiaková P, & Armour C (2018). Examination of the latent structure of DSM-5 posttraumatic stress disorder symptoms in Slovakia. Psychiatry Research, 267, 232–239. 10.1016/j.psychres.2018.06.028 [DOI] [PubMed] [Google Scholar]
- Rust J, & Golombok S (2014). Modern psychometrics: The science of psychological assessment. (3rd ed.). Routledge. [Google Scholar]
- Rytwinski NK, Scur MD, Feeny NC, & Youngstrom EA (2013). The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 26, 299–309. 10.1002/jts.21814 [DOI] [PubMed] [Google Scholar]
- Sareen J, Afifi TO, McMillan KA, & Asmundson GJ (2011). Relationship between household income and mental disorders: findings from a population-based longitudinal study. Archives of General Psychiatry, 68(4), 419–427. 10.1001/archgenpsychiatry.2011.15 [DOI] [PubMed] [Google Scholar]
- *Schmitt TA, Sass DA, Chappelle W, & Thompson W (2018). Selecting the “best” factor structure and moving measurement validation forward: An illustration. Journal of Personality Assessment, 100(4), 345–362. 10.1080/00223891.2018.1449116 [DOI] [PubMed] [Google Scholar]
- *Seligowski AV, & Orcutt HK (2016). Support for the 7-factor hybrid model of PTSD in a community sample. Psychological Trauma: Theory, Research, Practice, and Policy, 8(2), 218–221. 10.1037/tra0000104 [DOI] [PubMed] [Google Scholar]
- *Shevlin M, Hyland P, Karatzias T, Bisson JI, & Roberts NP (2017). Examining the disconnect between psychometric models and clinical reality of posttraumatic stress disorder. Journal of Anxiety Disorders, 47, 54–59. 10.1016/j.janxdis.2017.02.006 [DOI] [PubMed] [Google Scholar]
- Silverstein MW, Dieujuste N, Kramer LB, Lee DJ, & Weathers FW (2018). Construct validation of the hybrid model of posttraumatic stress disorder: Distinctiveness of the new symptom clusters. Journal of Anxiety Disorders, 54, 17–23 10.1016/j.janxdis.2017.12.003 [DOI] [PubMed] [Google Scholar]
- Simms LJ, Watson D, & Doebbeling BN (2002). Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf war. Journal of Abnormal Psychology, 111(4), 637–647. 10.1037//0021-843X.111.4.637 [DOI] [PubMed] [Google Scholar]
- Smith MW, Schnurr PP, & Rosenheck RA (2005). Employment outcomes and PTSD symptom severity. Mental Health Services Research, 7, 89–101. 10.1007/s11020-005-3780-2 [DOI] [PubMed] [Google Scholar]
- Steiger JH (1990). Structural model evaluation and modification: An interval estimation approach. Multivariate behavioral research, 25(2), 173–180. 10.1207/s15327906mbr2502_4 [DOI] [PubMed] [Google Scholar]
- Streiner DL (2003). Starting at the beginning: an introduction to coefficient alpha and internal consistency. Journal of Personality Assessment, 80(1), 99–103. surveys. 10.1207/S15327752JPA8001_18 [DOI] [PubMed] [Google Scholar]
- *Sveen J, Bondjers K, & Willebrand M (2016). Psychometric properties of the PTSD Checklist for DSM-5: a pilot study. European Journal of Psychotraumatology, 7(1), 30165. 10.3402/ejpt.v7.30165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, ... & de [Google Scholar]
- *Tiamiyu MF, Gan Y, Kwiatkowski D, Foreman KC, Dietrich A, Elliott K, & Elhai JD (2016). Relationships between latent factors of posttraumatic stress disorder and posttraumatic growth. The Journal of Nervous and Mental Disease, 204(5), 344–348. 10.1097/NMD.0000000000000490 [DOI] [PubMed] [Google Scholar]
- Trevethan R (2017). Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Frontiers in public health, 5, 307. 10.3389/fpubh.2017.00307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Tsai J, Harpaz-Rotem I, Armour C, Southwick SM, Krystal JH, & Pietrzak RH (2014). Dimensional structure of DSM-5 posttraumatic stress disorder symptoms: Results from the National Health and Resilience in Veterans Study. The Journal of Clinical Psychiatry, 76(5), 546–553. 10.4088/JCP.14m09091 [DOI] [PubMed] [Google Scholar]
- Tucker L, & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38, 1–10. 10.1007/BF02291170 [DOI] [Google Scholar]
- *van der Meer CA, Bakker A, Schrieken BA, Hoofwijk MC, & Olff M (2017). Screening for trauma-related symptoms via a smartphone app: The validity of Smart Assessment on your Mobile in referred police officers. International Journal of Methods in Psychiatric Research, 26(3), e1579. 10.1002/mpr.1579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Van Praag DL, Fardzadeh HE, Covic A, Maas AI, & von Steinbüchel N (2020). Preliminary validation of the Dutch version of the Posttraumatic stress disorder checklist for DSM-5 (PCL-5) after traumatic brain injury in a civilian population. PloS One, 15(4), e0231857. 10.1371/journal.pone.0231857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Verhey R, Chibanda D, Gibson L, Brakarsh J, & Seedat S (2018). Validation of the posttraumatic stress disorder checklist–5 (PCL-5) in a primary care population with high HIV prevalence in Zimbabwe. BMC Psychiatry, 18(1), 1–8. 10.1186/s12888-018-1688-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vet HC (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology, 60(1), 34–42. 10.1016/j.jclinepi.2006.03.012 [DOI] [PubMed] [Google Scholar]
- Vilaplana-Pérez A, Sidorchuk A, Pérez-Vigil A, Brander G, Isoumura K, Hesselmark E, ... & de la Cruz LF (2020). Assessment of Posttraumatic Stress Disorder and Educational Achievement in Sweden. JAMA Network Open, 3(12), e2028477–e2028477. 10.1001/jamanetworkopen.2020.28477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wald J, & Taylor S (2009). Work impairment and disability in posttraumatic stress disorder: A review and recommendations for psychological injury research and practice. Psychological Injury and Law, 2(3), 254–262. 10.1007/s12207-009-9059-y [DOI] [Google Scholar]
- Watson D (2005). Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology, 114, 522–536. 10.1037/0021-843X.114.4.522 [DOI] [PubMed] [Google Scholar]
- Watson D (2009). Differentiating the mood and anxiety disorders: A quadripartite model. The Annual Review of Clinical Psychology, 5, 221–247. 10.1146/annurev.climpsy.032408.153510 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov.
- Westen D, & Rosenthal R (2003). Quantifying construct validity: Two simple measures. Journal of Personality and Social Psychology, 84(3), 608–618. 10.1037/0022-3514.84.3.608 [DOI] [PubMed] [Google Scholar]
- Whiting P, Rutjes AW, Reitsma JB, Glas AS, Bossuyt PM, & Kleijnen J (2004). Sources of variation and bias in studies of diagnostic accuracy: a systematic review. Annals of Internal Medicine, 140(3), 189–202. 10.7326/0003-4819-140-3-200402030-00010 [DOI] [PubMed] [Google Scholar]
- *Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, Foa EB, Young-McCaughan S, Yarvis JS, Hembree EA, Mintz J, Peterson AL, & Litz BT (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28(11), 1392–1403. 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]
- *Zuromski KL, Ustun B, Hwang I, Keane TM, Marx BP, Stein MB, ... & Kessler RC (2019). Developing an optimal short-form of the PTSD Checklist for DSM-5 (PCL-5). Depression and Anxiety, 36(9), 790–800. 10.1002/da.22942 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


