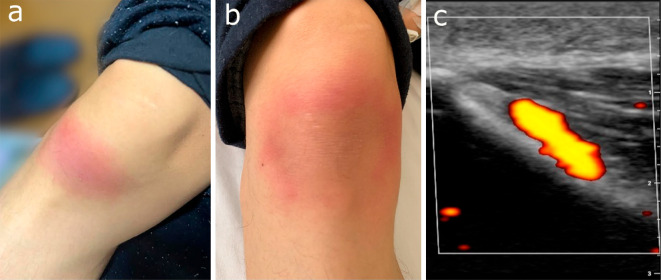
A 25-year-old man presented with right knee pain that developed 1 week after the onset of acute tonsillitis. In the previous two months, he had experienced tonsillitis twice. At the second instance of tonsilitis, the findings of a rapid streptococcal test were positive and he also complained of right knee pain 10 days after the onset of tonsillitis. The knee pain improved with oral non-steroidal anti-inflammatory drugs (NSAIDs) administered as needed; however, the third attack was severe. Despite receiving antibiotics for eight days, he became unable to walk. He supplied a snapshot taken via mobile phone at home two days before admission, which showed erythema along the right patellar tendon (Picture a). A physical examination showed extended erythema over the knee (Picture b). Ultrasonography of the right knee detected enthesitis on the medial and lateral collateral tendons and patellae tendons (Picture c). The latency period between the tonsillitis and the onset was less than 10 days, and the response to NSAIDs was poor; therefore, a diagnosis of post-streptococcal reactive arthritis (PSRA) was made (1). Three weeks' treatment with NSAIDs combined with corticosteroid injection into the ligaments alleviated his symptoms. PSRA is broadly defined as reactive arthritis, and 19% of patients with PSRA have polytendonitis, tenosynovitis, or enthesitis (2). Distinguishing enthesitis from joint symptoms may be a clinical clue to prompt physicians to diagnose PSRA.
Picture.
Data are available upon reasonable request by any qualified researchers who engage in rigorous, independent scientific research and will be provided following review and approval of a research proposal and Statistical Analysis Plan (SAP) and execution of a Data Sharing Agreement (DSA). All data relevant to the study are included in the article.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Maness DL, Martin M, Mitchell G. Poststreptococcal illness: recognition and management. Am Fam Physician 97: 517-522, 2018. [PubMed] [Google Scholar]
- 2. Sarakbi HA, Hammoudeh M, Kanjar I, Al-Emadi S, Mahdy S, Siam A. Poststreptococcal reactive arthritis and the association with tendonitis, tenosynovitis, and enthesitis. J Clin Rheumatol 16: 3-6, 2010. [DOI] [PubMed] [Google Scholar]