The Authors Reply We would like to thank the editor and Mugikura et al. for the letter that included many constructive insights for our case report (1). As Mugikura et al. proposed, this case likely involves the compensatory development of so-called choroidal anastomosis, with progressive posterior cerebral artery (PCA) involvement (2). Occlusion at the bilateral internal carotid artery terminus was already present in this case, and the progressive PCA involvement was thought to have led to the onset of an ischemic event. The infarction started from the right parietal lobe at the border region of the right middle cerebral artery and right posterior cerebral artery, and it expanded into the superior parietal lobule, which corresponds to the vascular territory of the parieto-occipital artery, a terminal artery of the PCA.
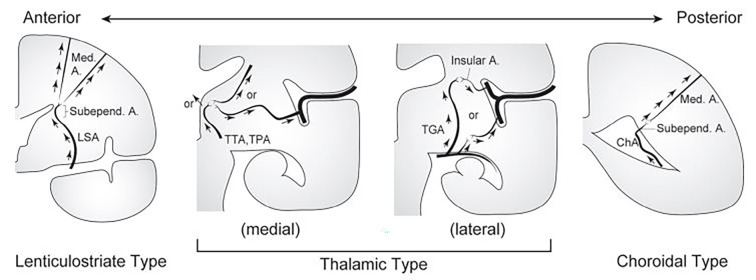
On single-photon emission computed tomography, the area perfused by the right pericallosal artery was relatively well-maintained in the present case; this, as shown in a report by Mugikura et al. (2), is thought to be due to the functioning of deep collateral circulation. Based on a report by Funaki et al. (3), there are a few potential routes, such as a route from the anterior or posterior choroidal artery via the subependymal artery or medullary artery, as well as a route from the thalamoperforating artery, thalamotuberal artery (a perforating branch of the posterior communicating artery), or the thalamogeniculate artery (a perforating branch of the P2 segment) via the medullary artery (Figure). Furthermore, in the present case, we were able to confirm anastomosis from the ophthalmic artery to the anterior cerebral artery via ethmoidal moyamoya on cerebral angiography, and we believe this also contributed to the CBF maintenance. To identify these blood vessels, a comparison with coronal images obtained via magnetic resonance angiography time-of-flight imaging was extremely useful.
Figure.
Schematic illustration showing the coronal plane of the left cerebral hemisphere and three subtypes of collateral anastomoses: lenticulostriate, thalamic, and choroidal anastomoses. A: artery, Med: medullary, Subepend: subependymal, TGA: thalamogeniculate artery, TPA: thalamoperforating artery, TTA: thalamotuberal artery. Reprinted with permission from Funaki et al. (3).
While infarction of a portion of the PCA region (e.g., the calcarine artery region) was avoided in the present case, this, as explained by Mugikura et al., appears to be the effect of the pial network that formed before the PCA involvement progressed. The ivy sign was observed in the calcarine sulcus and parieto-occipital sulcus in the present case, suggesting the presence of hypervascularity at the superficial occipital lobe in the background. Recently, various methods of visualizing the collateral circulation path and the ischemic changes in moyamoya disease have become available, and we look forward to the further development of imaging studies.
We thank Mugikura et al. for their constructive suggestions.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Mugikura S, Mori N. Development of ivy sign and infarction in the lateral part of the hemisphere or the middle cerebral artery territory in association with steno-occlusive involvement of the posterior cerebral artery in moyamoya disease. Intern Med 62: 1701, 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mugikura S, Takahashi S, Higano S, et al. The relationship between cerebral infarction and angiographic characteristics in childhood moyamoya disease. AJNR Am J Neuroradiol 20: 336-343, 1999. [PMC free article] [PubMed] [Google Scholar]
- 3. Funaki T, Fushimi Y, Takahashi JC, et al. Visualization of periventricular collaterals in moyamoya disease with flow-sensitive blackblood magnetic resonance angiography: preliminary experience. Neurol Med Chir (Tokyo) 55: 204-209, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]