Abstract
Objective:
A better understanding of the impacts of the Coronavirus disease 2019 (COVID-19) pandemic on emergency department (ED) visits for asthma is needed to improve asthma control.
Methods:
Using data from the National Syndromic Surveillance Program (NSSP), we assessed changes in average weekly asthma ED visits in the United States in 3 surveillance periods: (1) March 15, 2020–January 2, 2021; (2) January 3, 2021–January 1, 2022; and (3) January 2–March 5, 2022, relative to pre-pandemic comparison periods between December 30, 2018 and December 28, 2019. For each surveillance period, we assessed changes in asthma ED visits by age group and sex.
Results:
For the surveillance period beginning March 15, 2020, average weekly asthma ED visits declined 31% relative to what was observed during the comparison period – that is, from 45,276 visits/week in 2019 to 31,374 visits/week in 2020. Declines of over 19% and 26% were observed for 2021 and 2022, respectively, relative to the comparison periods. In all surveillance periods, the largest declines occurred among children, especially those ages 0–4 (74%) and 5–11 (66%) years.
Conclusions:
The COVID-19 pandemic impacted asthma ED visits in the United States. The impact was greater among children than adults, as ED visits among children were notably lower during all three pandemic surveillance periods than during the corresponding pre-pandemic periods. Additional information about the roles of behaviors of patients with asthma and changes in asthma care might improve our understanding of the reasons underlying these observed changes.
Keywords: adults, children, epidemiology, pandemic, population-based, surveillance
Introduction
Coronavirus disease 2019 (COVID-19), an illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), emerged in December 2019 and led to a global pandemic (1, 2). Following the declaration of COVID-19 as a national emergency in the United States on March 13, 2020, national and local public health interventions, including stay-at-home orders, physical distancing recommendations, school closures, and reduced business and entertainment activities were implemented to slow SARS-CoV-2 transmission. Healthcare systems also adjusted delivery structures and priorities to prepare for a sharp increase in COVID-19 cases (3). As a result, a drastic decline in emergency care use was reported in 2020 (3, 4) and numerous studies confirmed a decline in emergency department (ED) visits for asthma (5–13). Despite these observations, the impact of the pandemic on ED visits for asthma in the United States and potential differential impacts on sub-populations have not been described.
Approximately 25 million people, 7% of children and 8% of adults, in the United States have current asthma (14). Each year on average, there are 1.6 million ED visits for asthma (15). Asthma symptoms and asthma attacks can be triggered by allergens, ambient air pollution, respiratory viruses, and other exposures (16, 17). Adherence to preventative measures and access to urgent and emergency care for asthma exacerbations are important for managing and improving asthma outcomes. We conducted this study to describe changes in ED visits for asthma in the United States during the COVID-19 pandemic compared to the previous year. We examined changes in asthma ED visits by age and sex.
Materials and Methods
We obtained ED visit data from the National Syndromic Surveillance Program (NSSP), a collaboration among the Centers for Disease Control and Prevention (CDC), state and local health departments, federal, academic, and private sector partners (18). NSSP receives data from approximately 72% of nonfederal EDs from 50 states and the District of Columbia. Healthcare visit data received by NSSP are anonymized and include free-text reason for visit (i.e., chief complaint), discharge diagnoses, patient demographics, and location. For the present analysis, asthma ED visits were defined and identified using a free-text query based on chief complaint terms and discharge diagnosis codes (Supplemental Table 1). This free-text query was developed by CDC, in collaboration with state and local health departments and includes specific negations to limit the inclusion of unrelated visits.
To assess changes in ED visits over time, we used weekly counts of all ED visits (hereafter referred to as all-cause ED visits) and asthma ED visits from December 30, 2018 through March 5, 2022. The 2018–2022 study period was divided into three pandemic surveillance periods (2020, 2021, and 2022) and three corresponding 2018–2019 comparison surveillance periods. For all surveillance periods, weekly all-cause and asthma ED visits were tallied for weeks that began on Sundays, as described elsewhere (19). For each of the comparison surveillance periods, we selected as beginning and ending dates the dates of the calendar weeks of the corresponding pandemic surveillance period (Table 1).
Table 1.
Calendar weeks and dates of three pandemic surveillance and three corresponding comparison surveillance periods
| Pandemic surveillance periods |
Comparison surveillance periods |
|||
|---|---|---|---|---|
| Comparison | Calendar weeks | Dates | Calendar weeks | Dates |
| 2020 vs. 2019 | Weeks 12–53 | March 15, 2020–January 2, 2021 | Weeks 11–52 | March 10, 2019–December 28, 2019 |
| 2021 vs. 2019 | Weeks 1–52 | January 3, 2021–January 1, 2022 | Weeks 1–52 | December 30, 2018–December 28, 2019 |
| 2022 vs. 2019 | Weeks 1–9 | January 2, 2022–March 5, 2022 | Weeks 1–9 | December 30, 2018–March 2, 2019 |
Weekly counts of asthma ED visits were used to generate average weekly asthma ED visits and percentage change in average weekly asthma ED visits for each pandemic and comparison surveillance period. Weekly counts of all-cause ED visits were used to calculate the average weekly proportions of all-cause ED visits that were asthma ED visits. Average weekly proportions were calculated as the average of the weekly quotients of asthma ED visits by all-cause ED visits, multiplied by 1000. All measures were calculated within categories of age (0–4, 5–17, 18–64, and 65+ years) and by sex. We excluded from sex-specific measures all ED visits reported to NSSP with missing patient sex information. All analyses were conducted using R 4.1.2 (R Core Team, 2022).
To account for changes over time in the numbers of EDs sharing data with NSSP, we restricted our analyses to include only those EDs that consistently shared data with NSSP and that reported at least one asthma ED visit during the entire study period. Overall, 2233 (70%) met the data quality criteria and thus were included in our analyses. Among these, the number of EDs that reported asthma ED visits each week varied because some EDs did not receive asthma ED visits each week during the study period. In this analysis, the average weekly numbers of EDs with asthma ED visits were 2163 in 2019, 2174 in 2020, 2172 in 2021, and 2175 in 2022.
The analytic plan for the present study was reviewed and determined to be exempt from full Institutional Review Board review at the Centers for Disease Control and Prevention.
Results
Average weekly counts of all-cause and asthma ED visits were lower during each of the three pandemic surveillance periods than during the corresponding pre-pandemic comparison surveillance periods (Table 2). For example, during the 2020 pandemic surveillance period, there were an average of 1.1 million weekly all-cause ED visits and 31 374 weekly asthma ED visits, compared to 1.5 million weekly all-cause and 45 276 weekly asthma ED visits each week during the corresponding pre-pandemic comparison surveillance period, reflecting a 23.8% reduction in weekly all-cause ED visits and a 30.7% reduction in weekly asthma ED visits (Table 3). Percentage declines were larger for asthma ED visits than for all-cause ED visits during all three pandemic surveillance periods. Declines in average weekly asthma ED visits were largest in 2020 and smallest in 2021 among children 0–17 years and adults 65+ years for both female and male patients. Among adults 18–64 years of age, the largest percentage declines occurred in 2022, relative to comparable weeks in 2019; this was observed for both female and male patients (Supplemental Table 2). In all three surveillance periods, declines in average weekly asthma ED visits were notably larger among children than among adults.
Table 2.
Average weekly asthma emergency department (ED) visits, with standard deviations (SD), during three pandemic surveillance periods and three corresponding comparison surveillance periods using data from the National Syndromic Surveillance Program, December 2018–March 2022
| 2020 pandemic surveillance period vs. comparison surveillance period | 2021 pandemic surveillance period vs. comparison surveillance period | 2022 pandemic surveillance period vs. comparison surveillance period | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Pandemic surveillance period | Comparison surveillance period | Pandemic surveillance period | Comparison surveillance period | Pandemic surveillance period | Comparison surveillance period | |
|
|
||||||
| Average (SD) weekly visits | Average (SD) weekly visits | Average (SD) weekly visits | Average (SD) weekly visits | Average (SD) weekly visits | Average (SD) weekly visits | |
| All-cause ED visits | ||||||
| Total | 1 144 071 (37 440) | 1 501 237 (140 926) | 1 387 502 (123 327) | 1 497 834 (39 392) | 1 307 838 (109 090) | 1 482 785 (48 844) |
| Asthma ED visits | ||||||
| Total | 31 374 (4534) | 45 276 (4409) | 36 021 (3023) | 44 826 (4403) | 31 497 (2830) | 42 616 (3400) |
| Age, in years | ||||||
| 0–4 | 926 (984) | 3584 (485) | 2414 (892) | 3520 (900) | 2077 (598) | 3230 (283) |
| 5–11 | 1643 (1334) | 4859 (564) | 3073 (1044) | 4843 (1265) | 2775 (667) | 4706 (1011) |
| 12–17 | 1638 (632) | 3106 (369) | 2245 (448) | 3083 (605) | 2002 (230) | 2947 (498) |
| 18–44 | 15 417 (1124) | 18 980 (2036) | 15 929 (939) | 18 677 (1277) | 13 577 (2020) | 17 309 (1146) |
| 45–64 | 7789 (545) | 9774 (822) | 8015 (361) | 9762 (556) | 7124 (908) | 9642 (625) |
| 65+ | 3961 (363) | 4973 (416) | 4345 (171) | 4942 (362) | 3942 (298) | 4782 (355) |
| Sexa | ||||||
| Female | 19 742 (2374) | 27 447 (2766) | 22 017 (1471) | 27 223 (2326) | 19 328 (2202) | 26 095 (1960) |
| Male | 11 593 (2186) | 17 770 (1661) | 13 952 (1643) | 17 542 (2107) | 12 114 (830) | 16 454 (1487) |
For all surveillance periods, the sums of the sex-specific values do not equal the asthma ED visit total values because ED visits reported with missing patient sex information are excluded from the sex-specific averages, but included in the total averages.
Table 3.
Estimated differences in average weekly all-cause emergency department (ED) visits and asthma ED visits during three pandemic surveillance periods and three corresponding comparison surveillance periods using data from the National Syndromic Surveillance Program, December 2018–March 2022
| 2020 pandemic surveillance period vs. comparison surveillance period | 2021 pandemic surveillance period vs. comparison surveillance period | 2022 pandemic surveillance period vs. comparison surveillance period | |
|---|---|---|---|
|
|
|||
| No. (% change) | No. (% change) | No. (% change) | |
| All-cause ED visits | |||
| Total | 357 166 (−23.8) | 110 332 (−7.4) | 174 947 (−11.8) |
| Asthma ED visits | |||
| Total | 13 902 (−30.7) | 8 805 (−19.6) | 11 119 (−26.1) |
| Age, in years | |||
| 0–4 | 2658 (−74.2) | 1106 (−31.4) | 1152 (−35.7) |
| 5–11 | 3216 (−66.2) | 1770 (−36.5) | 1931 (−41.0) |
| 12–17 | 1468 (−47.3) | 838 (−27.2) | 945 (−32.1) |
| 18–44 | 3564 (−18.8) | 2748 (−14.7) | 3732 (−21.6) |
| 45–64 | 1985 (−20.3) | 1747 (−18.0) | 2518 (−26.1) |
| 65+ | 1012 (−20.4) | 596 (−12.1) | 841 (−17.6) |
| Sexa | |||
| Female | 7706 (−28.1) | 5206 (−19.1) | 6767 (−25.9) |
| Male | 6177 (−34.8) | 3589 (−20.5) | 4340 (−26.4) |
For each of the surveillance period comparisons, the sums of the sex-specific values do not equal the asthma ED visit total values because ED visits reported with missing patient sex information are excluded from the sex-specific averages, but included in the total averages.
Overall, asthma ED visits accounted for, on average, 27 of every 1000 ED visits each week during the 2020 pandemic surveillance period, 26 of every 1000 ED visits each week during the 2021 pandemic surveillance period, and 24 of every 1000 ED visits each week during the 2022 pandemic surveillance period (Figure 1). When stratified by age group, a similar pattern of declining average weekly proportions of all-cause ED visits that were asthma ED visits was observed among patients aged 12 years and older, whereas among children ages 0–4 years and 5–11 years, asthma ED visits accounted for smaller proportions in 2020 than in 2021 and 2022 (Figure 2). When stratified by sex, increasingly lower proportions were observed each year among women; among men, the proportion declined during the 2020 pandemic surveillance period and remained stable thereafter (Figure 3).
Figure 1.
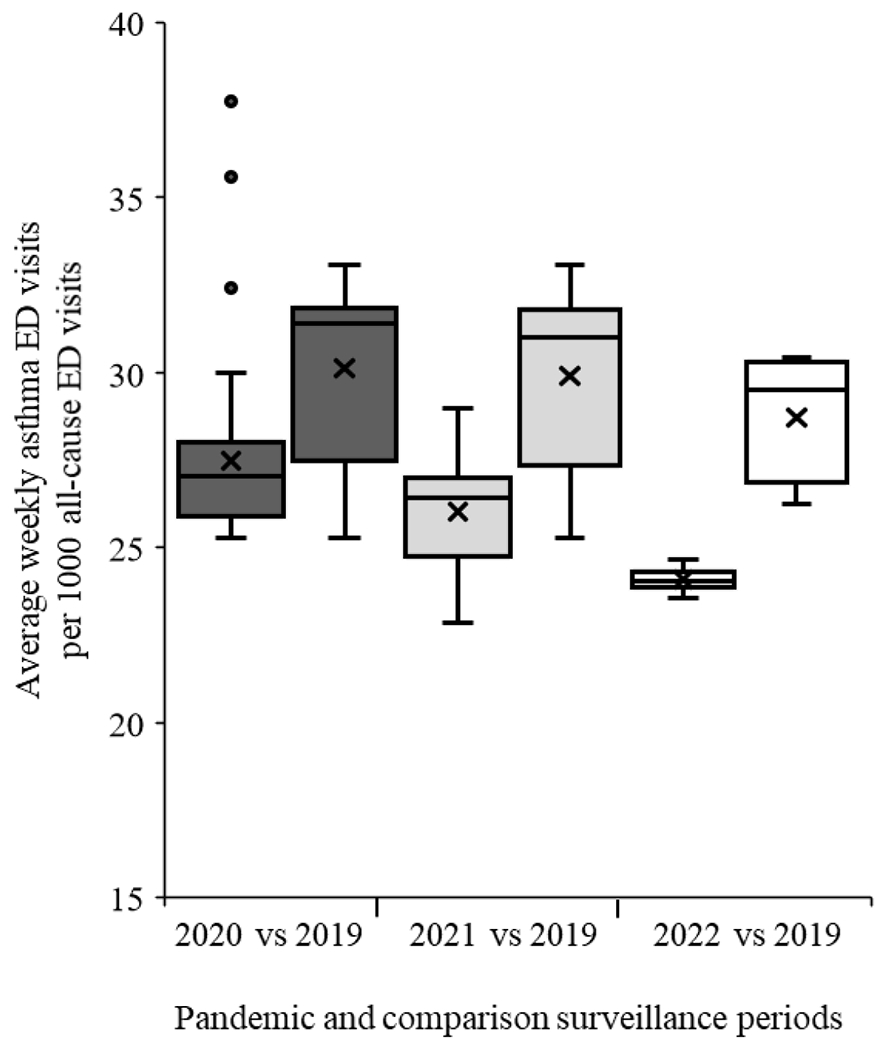
Box and whisker plot of average weekly asthma emergency department (ED) visits per 1000 all-cause ED visits for the 2020 (■), 2021 (■), and 2022 (□) pandemic surveillance periods and the corresponding 2019 comparison surveillance periods
Figure 2.
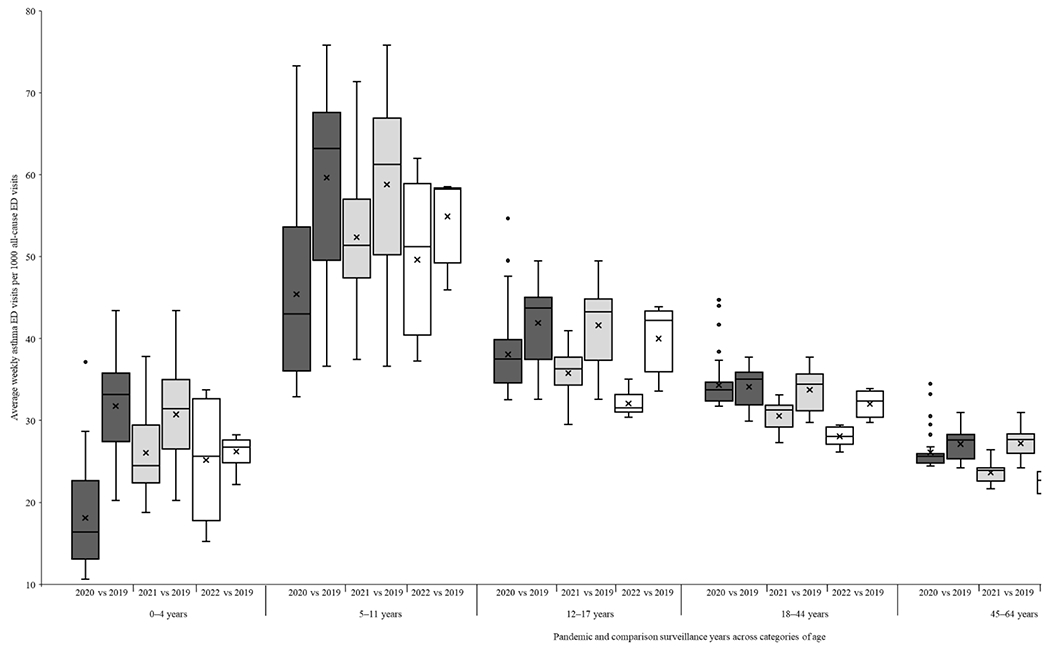
Box and whisker plot of average weekly asthma emergency department (ED) visits per 1000 all-cause ED visits for the 2020 (■), 2021 (■), and 2022 (□) pandemic surveillance periods and the corresponding 2019 comparison surveillance periods, across categories of age
Figure 3.
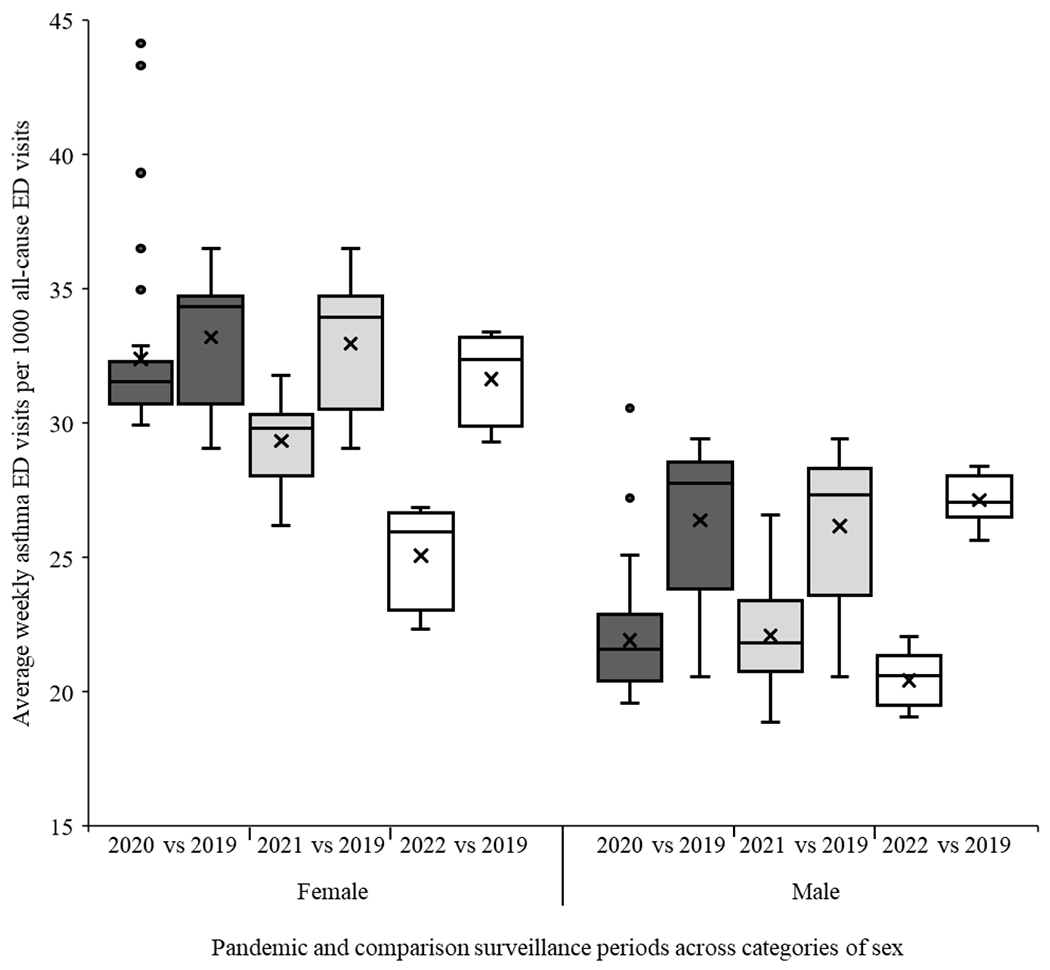
Box and whisker plot of weekly asthma emergency department (ED) visits per 1000 all-cause ED visits for the 2020 (■), 2021 (■), and 2022 (□) pandemic surveillance periods and the corresponding 2019 comparison surveillance periods, across categories of sex
Discussion
To investigate the impact of the COVID-19 pandemic on asthma ED visits in the United States, we compared time trends in asthma ED visits during the March 15, 2020–March 5, 2022 pandemic period to a those of the same weeks during the December 30, 2018–December 28, 2019 comparison period. Overall, relative to the average weekly asthma ED visits in 2019, we observed notably lower weekly averages in 2020, 2021, and early 2022, with the largest declines observed in 2020 and among children.
The decrease in asthma ED visits in 2020 coincided with the first wave of COVID-19 cases in the United States. Although our data do not provide insights into the reasons for the decline in asthma ED visits, the observed decline could be due, in part, to changes in care-seeking behaviors to avoid healthcare facilities for non-COVID-19-related medical needs or fear of contracting COVID-19 in medical facilities. In addition, changes in healthcare systems, including delivery structures, priorities, behaviors of providers, availabilities for non-COVID-19 patients, and diagnosis coding related to billing for COVID-19 treatment and in patients with both COVID-19 and asthma could also have had an impact on reported asthma ED visits. Nationally, declines in ED visits were noted for numerous health conditions during this period (3, 4). Czeisler et al. reported that over 40% of adults in the United States avoided medical care, including 12% who avoided urgent or emergency care, due to concerns related to COVID-19 during the pandemic (3).
Factors other than healthcare system avoidance might also have contributed to the observed decline. The declaration of a national emergency on March 13, 2020, followed by stay-at-home orders across the country, impacted daily routines and social interactions and might have reduced exposures to respiratory pathogens and other asthma triggers. If exposure to asthma triggers were, in fact, reduced during the pandemic, such a reduction could have led to a decline in asthma exacerbations. Changes in daily routines such as staying at home might have also allowed parents to better observe and manage symptoms in children with existing asthma. For pediatric populations (aged <18 years), closures of schools and childcare facilities as well as other mitigation efforts and behavior changes likely reduced transmission of respiratory pathogens. Taquechel et al. (2020) reported a reduction in rhinovirus infections, a common asthma trigger, in the greater Philadelphia area after March 2020 and a decline in pediatric asthma emergency and inpatient encounters (6). Ullmann et al. found in a cohort of 85 pre-school children with wheezing in Rome, Italy that self-reported wheezing episodes declined after the March–June 2020 lockdown period (20). For adult populations, Salciccioli et al. (2021) assessed asthma exacerbations in a cohort of African American and Hispanic individuals with moderate-to-severe asthma in the United States during the first and second quarters of 2019 and 2020 and found a 41% reduction in asthma exacerbations in 2020, compared to 2019 (21).
Our findings extend those of previous studies that reported declines of all-cause ED and asthma ED visits during the first half of 2020 and that are, in general, consistent with our findings (4–8, 21). Hartnett et al. examined ED visits in the United States from March 29 through April 25 of 2020 and 2019 and reported a 42% decrease in average weekly all-cause ED visits and an 84% decrease in average weekly asthma ED visits nationwide (4). Ulrich et al. investigated asthma ED visits of children aged 2–18 years enrolled in Medicaid and found that visits during January–June in 2020 were 50% lower than the 2017–2019 average (13). Our results extend these findings by reporting on differences in asthma ED visits across a three-year pandemic period, as well as by age and sex.
Declines in asthma ED visits in 2020 and 2021 have also been reported in single-hospital and regional studies in the United States and worldwide (5–11, 22, 23). Kenyon et al. examined the pediatric asthma ED visits in Children’s Hospitals of Philadelphia (Pennsylvania, USA) and reported that mean daily visits were 76% lower in the March–April 2020 “COVID-era” compared to the January–March 2020 “pre-COVID era” (5). Chavasse et al. (2020) described pediatric asthma presentations at St. Georges University Hospital (London, England) and reported a 90% decrease in mean daily pediatric hospital admissions for acute asthma after the lockdown (7). Taquechel et al. examined pediatric asthma healthcare use in the Greater Philadelphia area and reported an 84% decrease in emergency or inpatient asthma encounters comparing a 60-day period after versus before March 17, 2020 (6).
A few limitations should be considered when interpreting our findings. First, NSSP data are not nationally representative. However, the changes reported do represent the actual, observed changes in ED visits that occurred in nearly three-fourths of EDs across the United States. Therefore, the reported changes likely reflect ED visit patterns before and during the COVID-19 pandemic in the United States. Second, NSSP coverage has increased over time and varies by geographic region. For example, percentages of nonfederal EDs sending data to NSSP varies considerably by state, with <50% of EDs in California, Hawaii, Iowa, Maryland, Minnesota, and Oklahoma currently participating. To account for these differences, we restricted our analyses to data from facilities that reported consistently throughout the period of study, and numbers of these ED facilities stayed relatively constant over time. Third, counts of asthma ED visits returned by the syndrome definition are subject to differences in coding practices across facilities. Also, our analytic approach averaged weekly ED counts within surveillance periods and compared averages in 2020, 2021, and 2022 to the comparable averages in 2019. Because of this approach, our results do not account for trends in behaviors, exposures, or other factors within each surveillance period. Lastly, we note that our study was not designed to assign a causal link between any COVID-19 prevention measures and declines in asthma ED visits.
Despite these limitations, syndromic surveillance has strengths, such as access to anonymized health records with the potential for rich demographic data at the national and more granular geographic levels. The timely nature of syndromic surveillance makes it a valuable and actionable data source to evaluate the health impacts on ED visit trends in near real-time. Because of the long-term health implications of asthma, early detection, particularly in school-age children, can enhance the effectiveness of prevention programs.
Conclusions
Overall, our study characterized changes in asthma ED visits during three pandemic years (2020–2022), compared to those in the pre-pandemic year (2019). We found declines in average weekly asthma ED visits in 2020, 2021, and 2022, with the largest declines in 2020 and among children. Additional information about the reasons underlying changes in asthma ED visits in 2020–2022, including the impacts of mitigation efforts on population exposures to asthma triggers, the influence of the pandemic on behaviors of patients, and changes in healthcare systems delivery structures, priorities, behaviors of providers, and resources for non-COVID patients during the pandemic might provide insights for reducing the burden of asthma hospitalizations and ED visits.
Supplementary Material
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Interest Statement: The authors report there are no competing interests to declare.
References
- 1.Patel A, Jernigan DB. Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak - United States, December 31, 2019–February 4, 2020. MMWR Morb Mortal Wkly Rep 2020;69(5):140–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed 2020;91(1):157–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Czeisler M, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep 2020;69(36):1250–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69(23):699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kenyon CC, Hill DA, Henrickson SE, Bryant-Stephens TC, Zorc JJ. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract 2020;8(8):2774–6.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taquechel K, Diwadkar AR, Sayed S, Dudley JW, Grundmeier RW, Kenyon CC, et al. Pediatric asthma health care utilization, viral testing, and air pollution changes during the COVID-19 pandemic. J Allergy Clin Immunol Pract 2020;8(10):3378–87.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chavasse RJ. Covid-19: reduced asthma presentations in children. BMJ 2020;370:m2806. [DOI] [PubMed] [Google Scholar]
- 8.Krivec U, Kofol Seliger A, Tursic J. COVID-19 lockdown dropped the rate of paediatric asthma admissions. Arch Dis Child 2020;105(8):809–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guijon OL, Morphew T, Ehwerhemuepha L, Galant SP. Evaluating the impact of coronavirus disease 2019 on asthma morbidity: A comprehensive analysis of potential influencing factors. Ann Allergy Asthma Immunol 2021;127(1):91–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levene R, Fein DM, Silver EJ, Joels JR, Khine H. The ongoing impact of COVID-19 on asthma and pediatric emergency health-seeking behavior in the Bronx, an epicenter. Am J Emerg Med 2021;43:109–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheehan WJ, Patel SJ, Margolis RHF, Fox ER, Shelef DQ, Kachroo N, et al. Pediatric asthma exacerbations during the COVID-19 pandemic: Absence of the typical fall seasonal spike in Washington, DC. J Allergy Clin Immunol Pract 2021;9(5):2073–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simoneau T, Greco KF, Hammond A, Nelson K, Gaffin JM. Impact of the COVID-19 pandemic on pediatric emergency department use for asthma. Ann Am Thorac Soc 2021;18(4):717–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ulrich L, Macias C, George A, Bai S, Allen E. Unexpected decline in pediatric asthma morbidity during the coronavirus pandemic. Pediatr Pulmonol 2021;56(7):1951–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Asthma surveillance data. Available at https://www.cdc.gov/asthma/asthmadata.htm. Accessed 21 July 2021.
- 15.Centers for Disease Control and Prevention. Asthma emergency department visits 2010-2018. Available at https://www.cdc.gov/asthma/asthma_stats/asthma-ed-visits_2010-2018.html. Accessed 30 July 2021.
- 16.Chau-Etchepare F, Hoerger JL, Kuhn BT, Zeki AA, Haczku A, Louie S, et al. Viruses and non-allergen environmental triggers in asthma. J Investig Med 2019;67(7): 1029–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schatz M, Rosenwasser L. The allergic asthma phenotype. J Allergy Clin Immunol Pract 2014;2(6):645–8. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. National Syndromic Surveillance Program (NSSP). Available at https://www.cdc.gov/nssp/index.html. Acccessed on 2 August 2022.
- 19.Centers for Disease Control and Prevention. MMWR Weeks. Available at https://ndc.services.cdc.gov/wp-content/uploads/MMWR_Week_overview.pdf. Accessed 8 September 2022.
- 20.Ullmann N, Allegorico A, Bush A, Porcaro F, Negro V, Onofri A, et al. Effects of the COVID-19 pandemic and lockdown on symptom control in preschool children with recurrent wheezing. Pediatr Pulmonol 2021;56(7):1946–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salciccioli JD, She L, Tulchinsky A, Rockhold F, Cardet JC, Israel E. Effect of COVID-19 on asthma exacerbation. J Allergy Clin Immunol Pract 2021;9(7):2896–9.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan KF, Kwok WC, Ma TF, Hui CH, Tam TC, Wang JK, et al. Territory-wide study on hospital admissions for asthma exacerbations in the COVID-19 pandemic. Ann Am Thorac Soc 2021;18(10):1624–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Papadopoulos NG, Mathioudakis AG, Custovic A, Deschildre A, Phipatanakul W, Wong G, et al. Childhood asthma outcomes during the COVID-19 pandemic: Findings from the PeARL multi-national cohort. Allergy 2021;76(6):1765–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


