Abstract
Topic:
Understanding approaches to sustainability in cataract surgery and their risks and benefits
Clinical Relevance:
In the United States, healthcare is responsible for approximately 8.5% of greenhouse gas (GHG), and cataract surgery is one of the most commonly performed surgical procedures. Ophthalmologists can contribute to reducing GHG emissions, which lead to a steadily increasing list of health concerns ranging from trauma to food instability.
Methods:
We conducted a literature review to identify the benefits and risks of sustainability interventions. We then organized these interventions into a decision tree for use by individual surgeons.
Results:
Identified sustainability interventions fall into the domains of advocacy and education, pharmaceuticals, process, and supplies and waste. Existing literature shows certain interventions may be safe, cost-effective, and environmentally friendly. These include dispensing medications home to patients after surgery, multi-dosing appropriate medications, training staff to properly sort medical waste, reducing the number of supplies used during surgery, and implementing immediate sequential bilateral cataract surgery where clinically appropriate. The literature was lacking on the benefits or risks for some interventions, such as switching specific single use supplies to reusables or implementing a hub-and-spoke style theatre setup. Many of the advocacy and education interventions have inadequate literature specific to ophthalmology but are likely to have minimal risks.
Conclusions:
Ophthalmologists can engage in a variety of safe and effective approaches to reduce or eliminate dangerous GHG emissions associated with cataract surgery.
Keywords: Sustainability, carbon emissions, life cycle assessment, quality, value, surgery, cataracts, healthcare delivery, climate change, greenhouse gases, efficiency
Précis
Ophthalmologists have a variety of options for engaging in sustainability at work. Many interventions may also reduce costs while maintaining safety in surgery.
Introduction
Environmental issues are of increasing concern to the general public and to healthcare professionals. Climate change is causing an increase in immediate health threats from drought and fire, flooding and storms, and tick- and mosquito-borne diseases.1–3 For eye care, climate change will likely increase ocular trauma (from extreme weather events), vector-borne diseases such as trachoma4–6 and onchocerciasis,7,8 and diseases affected by exposure to heat, ultraviolet radiation, ozone, and other environmental pollutants.9–17 Without prompt efforts to address climate change, the severity of these impacts is expected to increase drastically.
Unfortunately, the health care systems charged with maintaining and improving peoples’ health are among the largest contributors to climate changing greenhouse gas emissions. Globally, healthcare emits about 5% of greenhouse gases.18 The proportion is higher in the United States, where approximately 8.5% of the US’ total greenhouse gas emissions come from the health sector.19–21 Unintentionally, healthcare is also responsible for other emissions adversely impacting health, including 9% of the US’ toxic air pollutants.21
Sustainability efforts within the health care sector have been expanding.22 Hospitals and health systems have been joining organizations like Practice Greenhealth and Health Care Without Harm or, most recently, voluntarily pledging to reduce greenhouse gas (GHG) emissions through the Health Sector Climate Pledge created by the Department of Health and Human Services’ Office of Climate Change and Health Equity (OCCHE).23 ESG (environmental, social and governance) concerns are now becoming a focus of governing boards and health system leaders as they recognize both the immediate and long term negative consequences of failure to create more resilience in operations and lead efforts toward decarbonization. Medical societies and colleges are also engaging in climate action, through action statements or by joining groups such as the Medical Society Consortium for Climate and Health.24,25 The American Academy of Ophthalmology (AAO) and American Society of Cataract & Refractive Surgery (ASCRS) joined the Consortium in 2020, giving their members access to educational and advocacy resources.26
Sustainability, Climate, and Eye Health
Though procedures in ophthalmology may use fewer resources and generate less waste than other specialties, the need for eye care is expansive. Cataract surgery, for example, is one of the most commonly performed operations worldwide, and the global need will continue to increase with a growing and aging population. Though there is a dearth of research on the environmental footprint from medical care,27 a small body of literature exists for cataract care and some other eye conditions.28–37 For high income countries, a majority of emissions originate in the manufacturing and distribution of single use surgical supplies.38 There is substantial variability in waste generation and emissions from cataract surgery in different countries, suggesting improvements are possible.29,33,39,40 Historically, there has been a tension between reusable and single-use items because of the fear of infection, but the notion that single-use items are safer for patients is not always supported by evidence.41–43 Advancements in infection control practices such as improved OR ventilation, sterilization methods, surgical technique, and availability of antimicrobial prophylaxis have significantly reduced the risks associated with reusable items.43–45 Endophthalmitis studies at Aravind Eye Care System raise the possibility that many of the costly and wasteful infection control protocols utilized by operating rooms in the United States could be unnecessary.40 A pre-pandemic survey of ophthalmic surgeons and nurses showed overwhelming support for sustainability interventions such as the reuse of supplies and multi-dosing of medications,46 with those in Ambulatory Surgical Centers more likely to state that they are already engaged in these practices.40,47
What Can a Clinician Do?
Despite increasing knowledge and a growing desire for action, many clinicians are unsure how to begin acting on climate change, especially within the clinical space. Interventions must be carefully selected, as sustainability might conflict with other important concerns, such as: infection control and prevention, excellent clinical outcomes (such as postoperative visual acuity), regulatory and other legal requirements, protocols enforced by accrediting bodies, cost containment, and employee stress and burnout. Here, we describe a variety of potential interventions for cataract surgeries, summarize existing literature on the broader impacts of each intervention, and offer guidance for ophthalmic clinicians on actions they can take to make eye care more sustainable.
Methods
Selecting Interventions
A list of potential interventions to improve environmental sustainability in cataract surgery was generated based on previous literature described above 28,39,43,48–51 and field observations. The ‘rethink, reduce, reuse, recycle’ framework was used to develop and organize potential interventions.22 All interventions were sorted into topic domains, including advocacy, education, pharmaceuticals, process changes, supplies, and waste. For this study, our team focused on potential environmental sustainability interventions that could be enacted by clinical personnel such as surgeons, nurses, surgical technicians, and pharmacists. As such, some items were moved into the domain of ‘advocacy’ in anticipation that the clinician could only advocate for those changes rather than directly implementing them (ex: sourcing renewable electricity, encouraging green building design for any new construction or renovations, etc.). For each intervention, the academic literature was reviewed to assess any known impacts to emissions, costs, safety, and outcomes. Gaps in the literature were noted.
Literature Review
A literature search was conducted in the electronic databases PUBMed, SCOPUS, and Cochrane Library to identify articles related to a specific sustainability intervention in the medical space. The article titles and abstracts were screened, and potentially relevant articles were retrieved for evaluation of the full text. The literature for each intervention was summarized and outcomes were compared for effectiveness. In addition to academic databases, we attempted to capture any hospital or health system websites or reports that might specify some of the benefits or challenges associated with adopting a particular intervention.
The study team also qualitatively assessed each intervention in the areas of 1) likely impact on environmental sustainability, specifically greenhouse gas emissions, 2) likely amount of effort for a hospital or health facility to enact, and 3) likely financial impact to the healthcare facility. A simple three-point ranking scale was used to evaluate these effects as either generally positive, neutral, or generally negative.
Decision Chart Development
Focusing specifically on the supply and pharmaceutical interventions, our team developed decision support charts to help navigate the overwhelming array of potential sustainability options for the individual clinician. The charts were developed by assessing the various end points for supply and drug interventions, eg. Reduce, reuse, or recycle, and organizing in a way that optimizes for reduction of supply and drug use first. Reducing supply items typically results in the largest GHG emissions savings.52
Results
Literature about Sustainability Interventions
Table 1 lists the interventions and an assessment of their impact, according to domain type.
Table 1:
Intervention strategies, by topic domain, and their likely impact on environmental footprint, hospital effort, and hospital finances
| Topic Domains | Topic Sub-domain | R Category | Intervention Type | GHG (or sustainability) Impact | Effort (from hospital) | Likely Financial Impacts |
|---|---|---|---|---|---|---|
| Advocacy | Health System | Reduce | Encourage sourcing renewable energy (solar, wind, etc.) | high | high | neutral |
| Advocacy | Health System | Reduce | Encourage sustainability in any capital projects (ex: build new construction or renovations to existing green building standards) | medium | medium | savings |
| Advocacy | Health System | Rethink | Purchase carbon offsets (for energy emissions from surgery, supply purchases, patient or staff commuting, conference travel, etc.) | high | medium | cost |
| Advocacy | Health System | Reuse | Contract with a third party single use device reprocessor | high | medium | savings |
| Advocacy | Manufacturers | Recycle | Inquire or enroll in take-back programs (for expired supplies, etc.) | low | low | savings |
| Advocacy | Manufacturers | Reduce | Encourage suppliers to reduce/optimize product packaging | medium | low | neutral |
| Advocacy | Manufacturers | Reduce | Encourage suppliers to switch to virtual Directions for Use (ex: intraocular lens or IOL directions, etc.) | medium | low | neutral |
| Advocacy | Manufacturers | Reduce | Inquire about the carbon emissions associated with manufacturing their product(s) | high | high | neutral |
| Advocacy | Manufacturers | Reuse | Ask suppliers about reusable alternatives (ex: reusable IOL loader, etc.) | medium | medium | savings |
| Advocacy | Manufacturers | Reuse | Encourage suppliers to manufacture single use devices that can be reprocessed | high | low | savings |
| Education | Patients | Rethink | Educate patients on the dangers of climate change and emissions from medical practice (provides an opportunity to highlight the health system’s accomplishments; can be done passively with posters, etc.) | low | low | neutral |
| Education | Professional Training | Rethink | Create and/or promote formal educational content on climate and health in medical education, residency training, and ongoing credentialling for ophthalmologists and other health professionals | medium | medium | neutral |
| Education | Staff | Recycle | Re-educate staff of recycling and other sorting protocols | low | low | savings |
| Pharmaceuticals | Anesthesia | Reduce | Do not pre-emptively draw up drugs for emergency-use (ex: epinephrine, propofol) | medium | medium | savings |
| Pharmaceuticals | Dispensing | Reuse | Dispense intra/pre-operative drugs home with patient when appropriate | medium | medium | neutral |
| Pharmaceuticals | Multi-dosing | Reuse | Multi-dose topical drugs in the pre-operative area (ex: dilating drops) | medium | medium | savings |
| Pharmaceuticals | Multi-dosing | Reuse | Multi-dose topical drugs in the OR (ex: tropicamide) | medium | medium | savings |
| Pharmaceuticals | Sizing | Reduce | Reduce/optimize the vial or bottle size of single-use drugs | medium | low | savings |
| Process | Care Pathway | Reduce | Eliminate pre-operative antibiotics, where clinically indicated, as department policy | medium | medium | savings |
| Process | Care Pathway | Reduce | Patient uses street clothes (no disposable patient gown) | medium | low | savings |
| Process | Operations | Rethink | Enact a hub and spoke operating model for high-volume surgeons | low | high | neutral |
| Process | Operations | Rethink | Enact same-day, sequential bilateral surgeries, where clinically appropriate | medium | medium | neutral |
| Supplies | Custom Pack | Reduce | Reduce the number of unused items in the custom pack by removing them, and perhaps relocating some things as pick items in individual peel packs (including: gauze, OR towels, single use cups and basins, syringes, pens, bottles, sharps holders, etc.) | medium | low | savings |
| Supplies | Custom Pack | Rethink | Standardize surgical supplies across surgeons (preference cards, custom packs, and pick items) | low | high | savings |
| Supplies | Custom Pack | Reuse | Replace single-use plastic basins and cups with reusables (ex: metal or reusable plastic) | medium | medium | savings |
| Supplies | Draping | Reduce | Face drape only (eliminate full body patient drape) | medium | medium | neutral |
| Supplies | Draping | Reduce | Eliminate disposable cover on the chair/bed | medium | medium | savings |
| Supplies | Draping | Reduce | Eliminate draping on other surfaces in the OR (instead clean all surfaces with a sterilizing wipe) | medium | medium | savings |
| Supplies | Expiration | Reduce | Narrow the expiration window on drugs/supplies in the room (the dates when they would need to be removed) | low | medium | savings |
| Supplies | Patient | Reuse | Switch to reusable med/surgical supplies (ex: patient restraints, stethoscopes, BP cuffs, etc.) | low | low | savings |
| Supplies | Preference Card | Reduce | Develop a ‘minimal’ baseline preference card for new employees | medium | low | savings |
| Supplies | Preference Card | Reduce | Review/optimize all physician preference cards | low | medium | savings |
| Supplies | Reusable Tray | Reduce | Remove unused instruments from trays and consolidate sets | low | medium | savings |
| Supplies | Reusable Tray | Reduce | Remove the sterile scope covers | low | high | neutral |
| Supplies | Reusable Tray | Reuse | Replace all single use plastic bluewrap with reusable hard containers | medium | high | savings |
| Supplies | Scrub | Reuse | Alternative for disposable, single use BD EZ Scrub | medium | medium | neutral |
| Supplies | Staff | Reuse | Switch to reusable sterile gowns for surgical team | medium | medium | savings |
| Supplies | Staff | Reuse | Switch to reusable caps or multiple uses per day | low | low | savings |
| Supplies | Staff | Reuse | Switch to reusable gowns for non-clinical staff | medium | medium | savings |
| Waste | Recycling | Recycle | Recycle hard plastic bins and trays | low | medium | neutral |
| Waste | Recycling | Recycle | Recycle paper packaging (prior to patient entering OR) | low | medium | neutral |
Advocacy & Education
Recognizing the limits of an individual in tackling a problem as large as climate change, the categories of advocacy and education are meant to illustrate ways in which clinicians can leverage their authority and respected position to achieve climate action reach. According to an annual Gallup poll, the American public typically ranks clinicians (doctors and nurses) as the most trusted professions.53 Doctors often hold substantial power at their medical facilities when it comes to decision-making and planning, and this can apply to cataract surgery as well as many other procedures and specialties.
Within their institution, clinicians can engage in educational activities, such as grand rounds or training sessions with their peers and colleagues, to discuss sustainability, climate change, and proper waste sorting. Though virtually no academic literature exists studying the impact of inter-collegial discussions in the medical space, climate communication is seen as an essential step in addressing the crisis.54–57 Clinicians can also advocate to add formal coursework on climate and health to medical and nursing school curriculums and continuing education programs, to better prepare clinicians for their future work. A few studies have monitored changes to medical education, but it may be too early to determine whether approaches are effective for preparing these students for the climatic changes they will experience in their practices.58–66
Waste training in medicine has a larger literature base. Recycling is an important component of dealing with operating room waste. Proper waste sorting and recycling in operating rooms can have a positive environmental and financial impact, but several barriers to operating room recycling exist. Operating room staff should be trained on proper waste sorting and recycling protocols, and clinicians can both advocate and educate on this topic. A survey of clinicians at Mayo Clinic found that 57% of respondents were unclear on which items in operating room are recyclable. After the implementation of a recycling education program, cost savings of 10.3% were achieved in sharps waste disposal.67 Another study created a 409% increase in recycling participation following distribution of an informational email, posting of recyclable materials guides in each room, and convenient placement of recycling receptacles.68 A recycling improvement program, consisting of staff training sessions and educational materials, could have a substantial impact on environmental emissions.
Clinicians might also leverage their relative local influence by advocating for changes such as investing in renewable energy sources, green building design, and carbon offsets. These are all well-tested methods of reducing GHGs and other emissions; however, they often require consensus-building from many stakeholders. Carbon offsetting, the practice of paying a third party to “absorb” GHG emissions, is a common but debatable practice.69,70 Some approaches can provide combined community benefit, and monetizing GHG emissions provides some financial incentives for their reduction. However, offset programs should be carefully vetted. In general, it is better to prevent emissions than to rely on these absorption schemes.71,72 That said, many health systems and other businesses rely on carbon offsetting to reach their carbon reduction or elimination goals, and use carbon offsetting while they explore options for direct GHG reductions.73
This advocacy could extend beyond health system practices and policies, to local and federal governments. Groups such as the Medical Society Consortium for Climate and Health support clinicians in writing editorials and contacting legislators.74 Manufacturers will also respond to the clinician voice. Clinicians can use their individual and collective power to talk to suppliers, manufacturers, drug developers, and product representatives about developing more sustainable products. Sustainability for manufacturers could take the form of new product design using more sustainable materials and decreased packaging, products that create less waste, or optimizing aspects of manufacturing, such as energy and water use or distribution routes.75,76 Because the production and manufacturing of medical products results in at least 15% of the industry’s GHGs, this is an important group to engage and mobilize.
Pharmaceuticals
While new drug formulations and packaging decisions have a role in clinical sustainability, ophthalmologists have direct control over the use and waste of pharmaceuticals in cataract surgery. With 3.8 million cataract procedures performed every year in the United States, medications potentially totaling $560 million are needlessly discarded.77,78 Single dose eye drops in preoperative and postoperative settings have been found to create substantial physical and financial waste and environmental pollution.31 There is a consensus within ophthalmology that excessive surgical drug waste unnecessarily increases the carbon footprint and costs of cataract surgery.77 An obvious approach, relatively unstudied in ophthalmology,79 would be to resize single-dose vials to volumes more appropriate for a single surgery. Unfortunately, this intervention may not always be cost effective.
Allowing patients to use topical medications after discharge, rather than discarding the unused medication can address some drug waste issues.80 A recent position paper endorsed by ASCRS, AAO, AGS (American Glaucoma Society), and OOSS (Outpatient Ophthalmic Surgery Society) supports sending drugs home with patients that must be continued postoperatively, stating that “It is wasteful and unnecessarily burdensome to discard the newly opened multi-use bottle and instead require the patient to purchase the same medication through an outpatient pharmacy.”77 Despite this, there is wide regional variation in pharmaceutical dispensing regulations. Recent legislative efforts at the state level have been successful in reducing regulatory obstacles to allow medication to be sent home with patients. In 2021, legislation in Illinois was signed into law stipulating that topical medications ordered at least 24 hours preoperatively and used in the OR must be properly labeled before the unused portion can be given to patients for post-discharge care.
Another approach to combatting drug waste in cataract surgery is multi-dosing bottles. Single use eye drops have been associated with increased cost, up to three times as much, compared with multi-dose bottles.81 A 2022 study found multi-dose preoperative and pre-injection eyedrop protocols saved approximately $240,000 per institution over a 5 year period and led to a 97% reduction in the number of bottles disposed.82 On a per mL basis, Rahemtulla et al. (2021) found that single use dilating eye drops are four times more expensive than multi-dose bottles.81 Other studies have reported similar cost reductions, one of them focusing specifically on topical anesthetics and fluorescein dye.81,83,84 The negative environmental impact is attributed to the waste accumulation from extra packaging and unused drug.81 Additionally, minimally used bottles are often disposed with regular trash, and the chemicals may contaminate drinking water. In 2013, the AAO published recommendations supporting the use of multi-dose eye drops to minimize waste, cost, and environmental impact.35 In 2015, ASCRS announced their position supporting the use of multi-dose eye drops on multiple patients as long as proper protocols are followed.85
The primary concern with multi-dose eye drops is risk of infection.86 Some multi-dose bottles contain preservatives, but these only inhibit the growth of bacteria and do not prevent contamination. Multiple studies have assessed microbial contamination of multi-dose eye drop containers, finding bacteria or other microbes in 0.7% to 40% of bottles or bottle tips, depending on the type of drug, the length of use, and use setting (e.g. inpatient, outpatient, or surgical).80,87–89 Improper use appears to be the main cause of contamination, with increased risks when the application time period is increased, untrained staff handle the drops, and the eye drops are used on a larger number of patients.86 One study found a contamination rate of 2.5%, which would result in a 1:400 risk of cross-contamination with coagulase-negative staphylococcus if the bottle was reused once and 1:80 if reused 6 times.90 This study suggested that reducing this particular infectious risk to zero costs the UK National Health Service between £2.75–4.6 million per year and generates over 6.85 tons of paper waste and 12.69 tons of plastic waste.90
Contamination of the dropper and, furthermore, contamination of the solution is the biggest concern in extended use of multi-dose eye drops. A variety of guidelines governing pharmacies and organizations exist to ensure quality of eye drops and reduced risk of contamination and infection. The US Pharmacopeia 797 provides guidelines for the use of sterile preparations and multi-dose vials to ensure patient safety and quality of care.91 Policies and procedures for the successful use of multi-dose eye drops include guidelines for handling the dropper bottle, expiration dating, training of the medical staff who administer eye drops, and clearly identifying when dropper bottles should be discarded due to contamination.92 To handle the dropper, staff should wash their hands before and after administering eye drops to patients, the tamper-proof seal should be unopened before using the dropper and completely removed before using, and when the cap is removed to use the medication, it should be placed inside up on a clean surface to avoid contamination. After use, the cap should be placed in a sterile manner and screwed down tightly to avoid leaking and contamination.92 According to these guidelines, if a multi-dose vial has been opened or accessed, the vial should be dated and discarded within 28 days unless otherwise specified by the manufacturer. However, each center can set their own criteria; some discard bottles after 24 hours35 and some after 28 days.92 A 28 day expiration date, once opened, is based on a flawed 2015 CMS Surveyor Infection Control Working Group checklist. In June, 2022, CMS clarified that only injectable vials are subject to this expiration date, unless otherwise noted by the manufacturer, and that eyedrops can be used multidose on multiple patients with aseptic application techniques, proper storage, and manufacturer multi-dose labeling.93 Surveyors nationally were educated about this change. Regular training of new and existing staff on handling and administration policies is vital for patient safety and quality of care.
Despite the evidence, many practices continue to require single-dose eye drops for cataract surgery because of fear of cross-contamination between subjects. Most studies that encourage single dose eye drops over multi-dose eye drops do not mention the training of technicians administering and handling the drops.86 Wu et al. (2021) showed through video recordings and bacterial cultures the efficacy and safety of multi-dose preoperative eye drops administered by properly trained ophthalmic technicians.35,86 At the end of each day, they sent all used bottles to the microbiology laboratory and cultured samples obtained from bottle tips. None of the bottle tips revealed positive bacterial cultures.35 Virani et al (2016) collected multi-dose eyedrops used long term (37 days to 54 days) and the eye drop solution was cultured for assessment of microbial contamination.94 They showed that none of the eye drop solutions had any growth on any culture media after 14 days. Based in their results they stated that the contamination of drops is not a rule, even after a month of being open. Several authors emphasized that the protocol and training of personal for multi-dose drops instillation is vital to avoid contamination.35,94,95
The presence, type, and concentration of preservatives has been shown to affect the incidence of contamination.95 It’s been reported that most of the medications contaminated had thimerosal or benzalkonium chloride as preservatives.96 It’s also been suggested that the role of preservatives is not sufficient to ensure the sterility of multi-dose eye drops.96 Aside from the risk of infection, bacterial contamination alters the solution’s pH and reduces the efficacy of the medication.96
Tsegaw et al (2017) reported a contamination rate of 11%, all of it being from the dropper’s tip and none from the residual solution of the dropper.96 The prevalence of contamination of single use drops was 3.2% and of multi-dose eyedrops was 24.3% and contamination levels increased in both as the duration of used increased from 1 week to greater than 1 week. However, this literature comes from other international settings and may not be representative of a US case.
Jensen et al. (2014) created a protocol that states a multi-dose dropper is contaminated when: the tip is touched by any structure or surface of the eye; the tip is touched by the administering staff member; a seal-open dropper has no expiration date; a seal-open dropper has an expiration date greater than 28 days; and/or there is an open, uncapped bottle, regardless of expiration date.92 Following each of the variations in process identified, they demonstrated that the postoperative infection rates in patients undergoing cataract surgery were similar using single-dose or multi-dose eye drops. As such, while the various processes do not follow current FDA guidelines, one could view the study outcome as a risk assessment to provide justification for use within an accredited facility. Cost advantages to using multi-dose eye drops were significant for both the patient and the healthcare facility preoperatively, intraoperatively, and postoperatively.92
Anesthesia is another aspect of care that can generate unnecessary waste and environmental emissions. We were unable to find literature specifically focused on environmental emissions associated with ophthalmic anesthesia, but generically, there are guidelines for “greening” anesthetic practice which should be utilized.50,97 Importantly, lower-impact anesthesia options should be prioritized, and in the case of ophthalmology, general anesthesia is used infrequently and anesthetic gases such as desflurane and sevoflurane are potent greenhouse gases whose emissions should be avoided if possible.98–100
In summary, the evidence shows that limited durations of use, proper handling of multi-dose droppers, and regular training of administering staff can minimize the risk of contamination, decrease waste, and decrease environmental and financial costs before, during, and after cataract surgery.35,81,92 However, this practice should be implemented with rigorous policies and staff training, and may not be appropriate for every ophthalmic setting.
Process
Interventions to the process for ophthalmic surgery include optimizing a standard preference card, having the patient wear street clothes, changing to a hub and spoke model of surgery, and conducting same-day, simultaneous bilateral cataract surgeries. Optimizing surgical preference cards to a standard minimum represents a particularly attractive intervention in terms of financial savings and environmental impact. A universal preference card in other surgical specialties has been shown to reduce costs drastically, especially if it reduces unused supplies.101–103 In studies where it has succeeded, preference card standardization relies on surgeon buy-in and engagement, through open communication and incentive. Additionally, major US health systems such as Banner Health and University of Missouri Health Care have reported cost savings due to preference card standardization.103,104 While the financial benefit of preference card standardization has been clearly demonstrated, the environmental impact remains more nebulous. Studies on the sterilization of tools, amount of requested supplies a la carte, and operating room time would clarify how standardizing preference cards improves the footprint of cataract surgery.
While the conventional viewpoint that patient gowning reduces unnecessary contamination merits consideration,105 there has been a lack of evidence demonstrating that patient gowning results in a significant decrease in adverse ophthalmic outcomes. Patients at Aravind Eye Hospital wear their own clothes for cataract surgery with no significant difference in rates of endophthalmitis,106 and the lack of gowning is practiced already in some US facilities.47 Additionally, wearing gowns has been shown to increase stress and anxiety for patients due to exposing their bodies.107 Ophthalmic surgery seems to present a unique opportunity for this intervention, since these operations typically only need to access the eye. Nevertheless, a study involving the different practical considerations of gowns, including contamination, access for intravenous lines, comfort, warmth, and soiling is needed.
For surgeons in higher volume settings, a hub and spoke model of surgery could improve operational efficiency and reduce emissions associated with energy consumption. In this model, the surgeon is the hub that does the operation while the midlevel ophthalmic personnel are the spokes that do the preoperative and postoperative preparations. Aravind has patients within the same operating room on two separate tables but regulations in the United States would require multiple operating rooms for different patients.106 One of the main benefits of improved efficiency lies in reduced energy usage of the operating room. While this would still apply, the benefit might be mitigated by the ratio of operating rooms to patients, and number of operating room personnel, staying the same. Additionally, efficiency alone is not always a financial benefit as Roberts et. al. found in their evaluation of a hub and spokes model for femtosecond laser-assisted cataract surgery compared to traditional phacoemulsification surgery.108 Although financial and environmental considerations can have mutual goals, a life cycle assessment (LCA) of a surgical hub and spokes model would identify the different variables affected by a model change.
Immediate sequential bilateral cataract surgery (ISBCS) involves performing phacoemulsification with intraocular lens placement in both eyes of the patient on the same visit in the same operative setting. Though this practice has been widely debated, literature increasingly supports the use of ISBCS for its benefits in providing faster patient rehabilitation, and cost and time savings.109 Environmental emissions are reduced from limiting the duplication of pre- and post-operative visits and travel time for the patient. According to data from the Bureau of Labor Statistics’ American Time Use Survey, the average time spent traveling to access healthcare services is 34 minutes, so reducing the number of visits required could significantly reduce travel related environmental emissions.110 However, there is typically limited reduction in supplies used as, in the US, both surgeries are treated as separate cases for infection control purposes. The infection risks of ISBCS are now recognized to be low with the advent of intracameral antibiotics. Numerous studies have proven ISBCS to be more cost-effective and efficient.109,111,112
ISBCS also offers the ability to improve OR efficiency in terms of reduced patient transfer and preparation times, which could allow more surgeries to be performed within a given time. O’Bart et al. (2020) demonstrated that with ISBCS it is possible to achieve an average 16% reduction in the time taken to perform two cataract surgeries.113 Additionally, there is potential room to reduce waste by optimizing staff schedules to align with case schedules.
Supplies & Waste
Unused surgical supplies are routinely discarded in operating rooms, which significantly contributes to waste and the overall carbon footprint. Consistently unused items should be removed from surgical custom packs and surgeon preference cards wherever possible, to save on costs, waste generation, and embodied emissions. Some single-use items could be replaced with a smaller product. For example, in the US many ophthalmic facilities use a full-body drape during eye surgeries where a smaller face drape may be sufficient. Additionally, many single-use items could be substituted with reusable alternatives without compromising clinical outcomes.
Disposable custom procedure packs minimize surgical preparation time and reduce touch-points on products, leading to lower risk of contamination. However, custom packs often contain items that are infrequently used, contributing to unnecessary expense and waste. Once a custom pack is opened, every item in the pack must be discarded, even if it has not been used. Clinicians often add items to the packs yet find it difficult to remove unnecessary items. In terms of both environmental impact and financial savings, optimizing custom procedure packs can be significantly beneficial, and several facilities have reported positive results. By streamlining their packs to remove infrequently used items, Marysville Surgical Center has saved $32,000 annually without increasing room turnover times.114 Items should be made available as needed (sometimes called ‘pick items’) to avoid unnecessarily opening a custom pack or kit to access a single item. Despite the potential for reducing cost and waste, there are few studies available on the topic.
While a single-use, disposable drape covering the face is necessary for cataract surgery, some facilities instead use a large, full body drape. We were unable to find literature identifying pros and cons of either approach, but are aware of eye surgery centers using both approaches.47
Studies have found that the use of reusable surgical gowns reduces GHG emissions and solid waste generation while also providing superior protection and durability compared to single-use gowns.115 Vozzola, et al. (2018) compared the environmental impacts of market-representative reusable and disposable gowns using standard lifecycle assessment procedures. Compared to the disposable gown system, the reusable gown system showed a 28% reduction in energy consumption, a 30% reduction in greenhouse gas emissions, a 41% reduction in blue water consumption, and a 93% reduction in solid waste generation.116 Aravind Eye Hospital uses reusable surgical gowns and other linens along with numerous other sustainable practices with surgical outcomes that are equivalent to Western countries.47 However, there is a lack of prospective, randomized studies comparing the clinical impact of reusable vs single-use surgical gowns. There are also limited studies on the impacts of reusable draping on infections.117–121
Manufacturers may have some solutions to reducing supply waste, though a clinician may need to advocate for their health facility to participate. Examples include vendors that can assist with single-stream recycling (such as Stericycle),122 or single-use device reprocessors who have US Food and Drug Administration approval to clean, sterilize, and resell single use medical and surgical products.123,124 Such initiatives can increase the circularity of medical products and materials, leading to a reduction in resource extraction from producing items new each time.44
Decision Tree for Prioritizing Sustainability Strategies in Ophthalmology
The multitude of options available to an individual can be overwhelming. Though there are many frameworks to decide what activities might be most fulfilling for an individual or most impactful in reducing GHGs, we have put together a decision tree to aid in making changes to clinical practice, focusing specifically on supplies (Figure 1) and pharmaceuticals (Figure 2).
Figure 1:
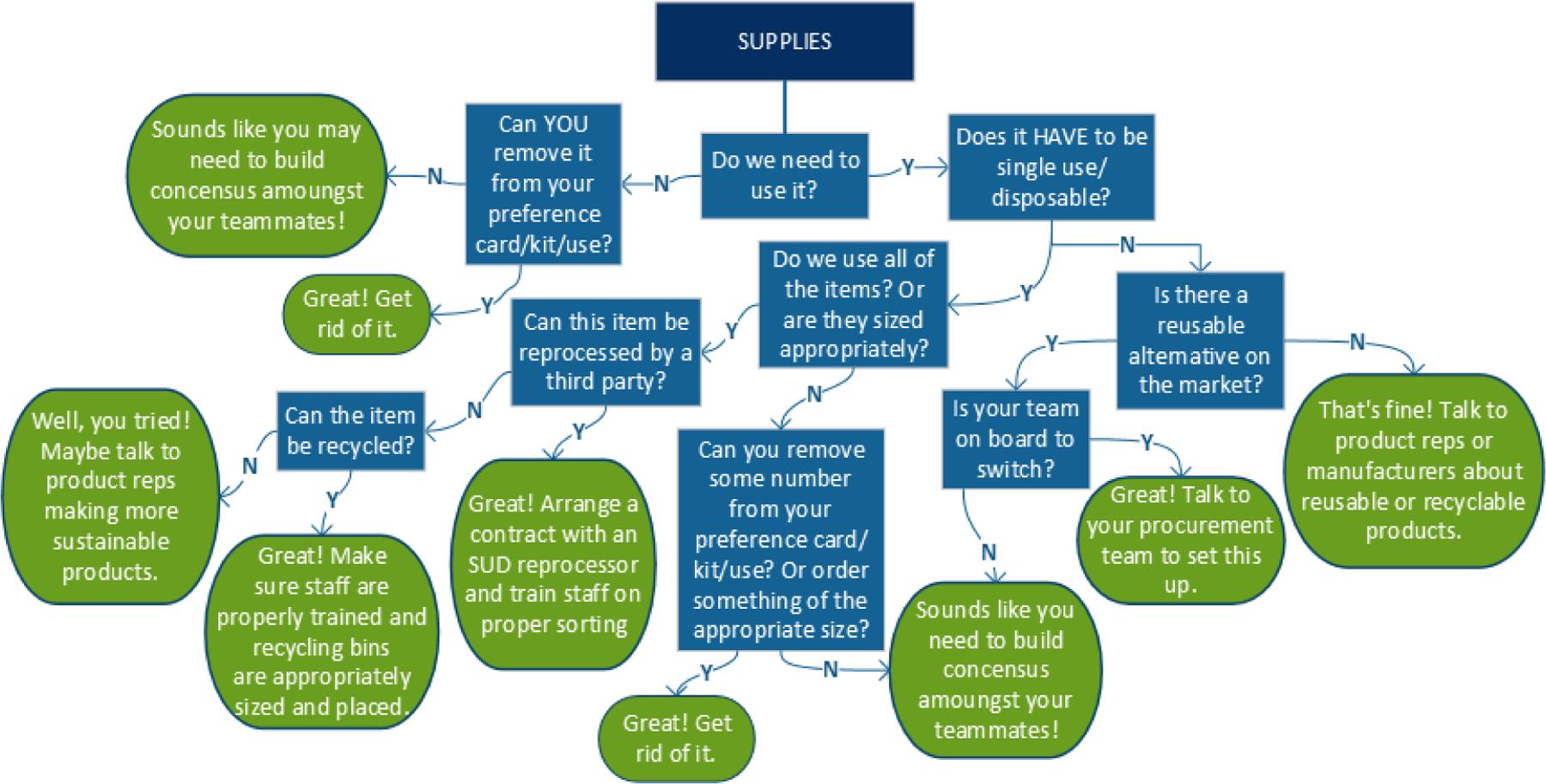
Decision Flow Chart for Selecting Sustainability Interventions related to Supplies in Cataract Surgery (in the US)
Figure 2:
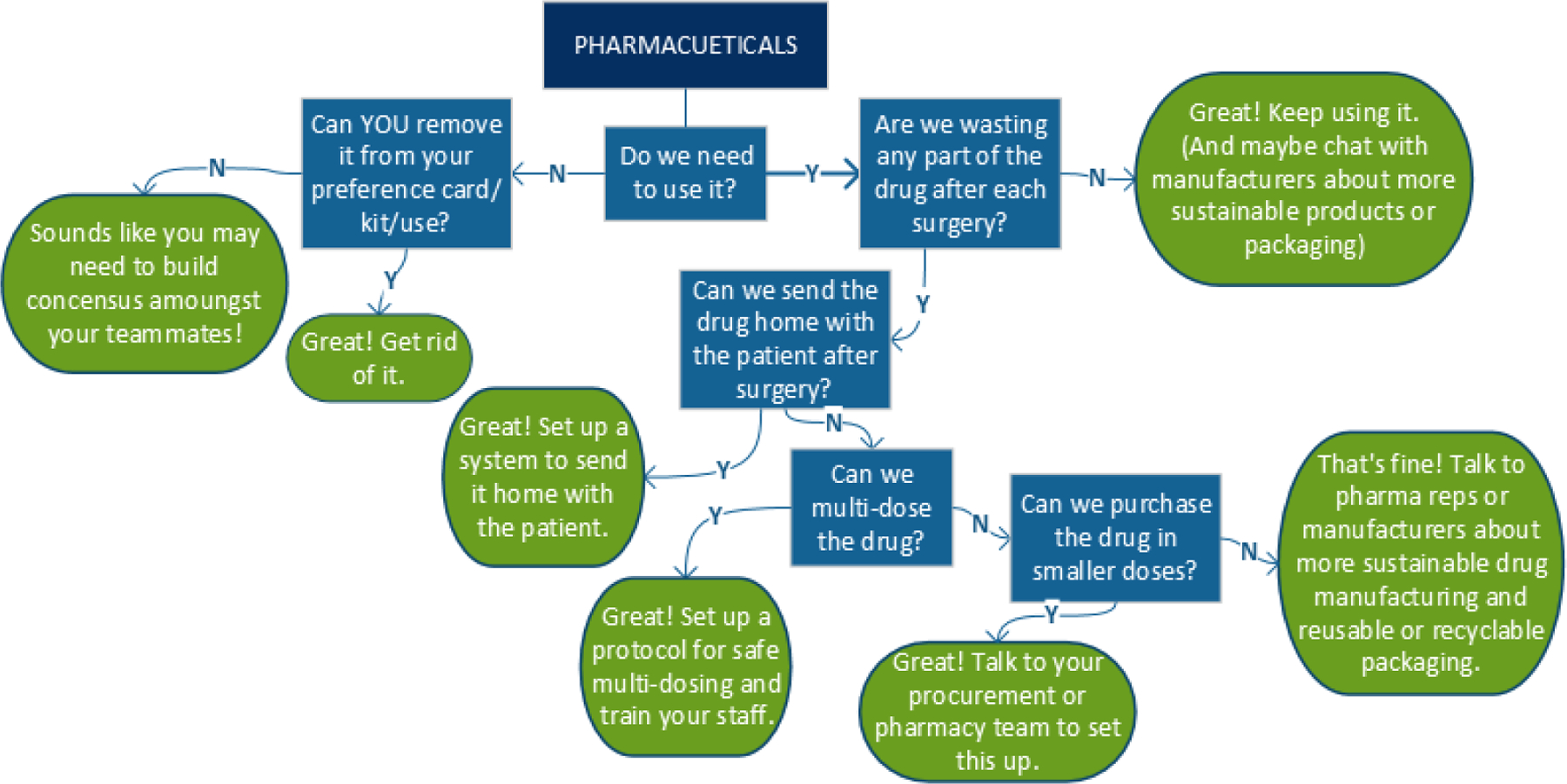
Decision Flow Chart for Selecting Sustainability Interventions related to Pharmaceuticals in Cataract Surgery (in the US)
Considerations for Clinics and Other Healthcare Spaces
Though we focus primarily on an operating room setting, other spaces for healthcare delivery can substantial environmental impacts as well. Some of the strategies here can be applied to other clinical spaces and other surgical disciplines, but there may be strategies unique to these areas. For example, outpatient departments screening patients may use other types of disposable supplies and have other, unique forms of waste (ex: energy use, travel needs of patients, etc.).125
Conclusions
There are many ways to improve the efficiency and sustainability of cataract surgery and eye care. Not every intervention has been well studied; for example, there are likely contextual factors that will determine whether reusable supplies or multi-dosing of drugs is appropriate for a specific facility. Which interventions will work best must be determined by the individual stakeholders at each hospital or health system. Despite the limitations of existing literature, there is sufficient evidence that reducing environmental emissions in the operating room is achievable and cost efficient.
Though addressing the climate crisis may still feel overwhelming for the individual clinician, research suggests that climate action and activism builds resilience, helping to stave off climate-related anxiety and depression.126–128 We hope this article provides clinicians with some guidance and literary tools to support climate action within their professional institutions, and we recommend clinicians peruse https://eyesustain.org/ for updated information on sustainability, climate, and health for ophthalmology.
Acknowledgements
This work was supported by the The Patrick and Catherine Weldon Donaghue Medical Research Foundation’s Greater Value Portfolio and the National Eye Institute of the National Institutes of Health under Award Number R56EY033779. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pachauri RK, Allen M, Barros V, et al. Climate Change 2014: Synthesis Report. Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change 2014. 9291691437. http://epic.awi.de/37530/ [Google Scholar]
- 2.IPCC. Global Warming of 1.5°C: IPCC Special Report on Impacts of Global Warming of 1.5°C above Pre-industrial Levels in Context of Strengthening Response to Climate Change, Sustainable Development, and Efforts to Eradicate Poverty Cambridge University Press; 2022. [Google Scholar]
- 3.Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. The Lancet 2021;397(10269):129–170. doi: 10.1016/S0140-6736(20)32290-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramesh A, Bristow J, Kovats S, et al. The impact of climate on the abundance of Musca sorbens, the vector of trachoma. Parasites & Vectors 2016/January/27 2016;9(1):48. doi: 10.1186/s13071-016-1330-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramesh A, Kovats S, Haslam D, Schmidt E, Gilbert CE. The Impact of Climatic Risk Factors on the Prevalence, Distribution, and Severity of Acute and Chronic Trachoma. PLOS Neglected Tropical Diseases 2013;7(11):e2513. doi: 10.1371/journal.pntd.0002513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prost A, Négrel AD. Water, trachoma and conjunctivitis. Bull World Health Organ 1989;67(1):9–18. [PMC free article] [PubMed] [Google Scholar]
- 7.Cheke RA, Basáñez M-G, Perry M, et al. Potential effects of warmer worms and vectors on onchocerciasis transmission in West Africa. Philosophical Transactions of the Royal Society B: Biological Sciences 2015;370(1665):20130559. doi:doi: 10.1098/rstb.2013.0559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalkstein LS, Smoyer KE. The impact of climate change on human health: Some international implications. Experientia 1993/November/01 1993;49(11):969–979. doi: 10.1007/BF02125644 [DOI] [PubMed] [Google Scholar]
- 9.Auger N, Rhéaume M-A, Bilodeau-Bertrand M, Tang T, Kosatsky T. Climate and the eye: Case-crossover analysis of retinal detachment after exposure to ambient heat. Environmental research 2017;157:103–109. [DOI] [PubMed] [Google Scholar]
- 10.Echevarría-Lucas L, Senciales-González JM, Medialdea-Hurtado ME, Rodrigo-Comino J. Impact of Climate Change on Eye Diseases and Associated Economical Costs. International Journal of Environmental Research and Public Health 2021;18(13). doi: 10.3390/ijerph18137197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim SH, Yu MH, Lee JH, Yoon JS, Rah SH, Choi M. Seasonal variation in acute post-cataract surgery endophthalmitis incidences in South Korea. Journal of Cataract & Refractive Surgery 2019;45(12):1711–1716. doi: 10.1016/j.jcrs.2019.07.022 [DOI] [PubMed] [Google Scholar]
- 12.Hong J, Zhong T, Li H, et al. Ambient air pollution, weather changes and outpatient visits for allergic conjunctivitis: A retrospective registry study. Scientific Reports 2016/April/01 2016;6(1):23858. doi: 10.1038/srep23858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mandell JT, Idarraga M, Kumar N, Galor A. Impact of Air Pollution and Weather on Dry Eye. J Clin Med Nov 20 2020;9(11)doi: 10.3390/jcm9113740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang C-J, Yang H-H, Chang C-A, Tsai H-Y. Relationship between Air Pollution and Outpatient Visits for Nonspecific Conjunctivitis. Investigative Ophthalmology & Visual Science 2012;53(1):429–433. doi: 10.1167/iovs.11-8253 [DOI] [PubMed] [Google Scholar]
- 15.Chua SYL, Khawaja AP, Morgan J, et al. The Relationship Between Ambient Atmospheric Fine Particulate Matter (PM2.5) and Glaucoma in a Large Community Cohort. Invest Ophthalmol Vis Sci Nov 1 2019;60(14):4915–4923. doi: 10.1167/iovs.19-28346 [DOI] [PubMed] [Google Scholar]
- 16.Chua SYL, Warwick A, Peto T, et al. Association of ambient air pollution with age-related macular degeneration and retinal thickness in UK Biobank. British Journal of Ophthalmology 2022;106(5):705. doi: 10.1136/bjophthalmol-2020-316218 [DOI] [PubMed] [Google Scholar]
- 17.Lin CC, Chiu CC, Lee PY, et al. The Adverse Effects of Air Pollution on the Eye: A Review. Int J Environ Res Public Health Jan 21 2022;19(3)doi: 10.3390/ijerph19031186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karliner J, Slotterback S, Boyd R, Ashby B, Steele K. Health Care’s Climate Footprint: How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action 2019:48. September, 2019. https://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf [Google Scholar]
- 19.Eckelman MJ, Huang K, Lagasse R, Senay E, Dubrow R, Sherman JD. Health Care Pollution And Public Health Damage In The United States: An Update: Study examines health care pollution and public health damage in the United States. Health Affairs 2020;39(12):2071–2079. [DOI] [PubMed] [Google Scholar]
- 20.Eckelman MJ, Sherman JD. Estimated Global Disease Burden From US Health Care Sector Greenhouse Gas Emissions. Am J Public Health Apr 2018;108(S2):S120–s122. doi: 10.2105/ajph.2017.303846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eckelman MJ, Sherman J. Environmental Impacts of the U.S. Health Care System and Effects on Public Health. PLoS ONE 2016;11(6):e0157014. doi: 10.1371/journal.pone.0157014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sullivan GA, Petit HJ, Reiter AJ, et al. Environmental Impact and Cost Savings of Operating Room Quality Improvement Initiatives: A Scoping Review. J Am Coll Surg 2023;236(2):411–423. [DOI] [PubMed] [Google Scholar]
- 23.Assistant Secretary for Health (ASH). Health Care Sector Commitments to Emissions Reduction and Resilience Accessed 9/26/2022, https://www.hhs.gov/climate-change-health-equity-environmental-justice/climate-change-health-equity/actions/health-care-sector-pledge/index.html
- 24.Climate Change and Health: A Position Paper of the American College of Physicians. Annals of Internal Medicine 2016;164(9):608–610. doi: 10.7326/m15-2766/27089232 [DOI] [PubMed] [Google Scholar]
- 25.The Medical Society Consortium on Climate and Health. Medical Society Policy Statements Accessed 1/19/2020, 2020. https://medsocietiesforclimatehealth.org/category/medical-society-policy-statements/
- 26.ASCRS joins the Medical Society Consortium on Climate & Health. ASCRS EyeWorld; 2020. https://www.eyeworld.org/ascrs-joins-medical-society-consortium-climate-health
- 27.Drew J, Christie SD, Tyedmers P, Smith-Forrester J, Rainham D. Operating in a Climate Crisis: A State-of-the-Science Review of Life Cycle Assessment within Surgical and Anesthetic Care. Environmental Health Perspectives 2021;129(7):076001. doi:doi: 10.1289/EHP8666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buchan JC, Thiel CL, Steyn A, et al. Addressing the environmental sustainability of eye health-care delivery: a scoping review. The Lancet Planetary Health 2022/June/01/ 2022;6(6):e524–e534. doi: 10.1016/S2542-5196(22)00074-2 [DOI] [PubMed] [Google Scholar]
- 29.Goel H, Wemyss TA, Harris T, et al. Improving productivity, costs and environmental impact in International Eye Health Services: using the ‘Eyefficiency’ cataract surgical services auditing tool to assess the value of cataract surgical services. BMJ Open Ophthalmology 2021;6(1):e000642. doi: 10.1136/bmjophth-2020-000642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steyn A, Cassels-Brown A, Chang D, et al. Frugal innovation for global surgery: leveraging lessons from low- and middle-income countries to optimise resource use and promote value-based care. The Bulletin of the Royal College of Surgeons of England 2020;102(5):198–200. doi: 10.1308/rcsbull.2020.150 [DOI] [Google Scholar]
- 31.Tauber J, Chinwuba I, Kleyn D, Rothschild M, Kahn J, Thiel CL. Quantification of the Cost and Potential Environmental Effects of Unused Pharmaceutical Products in Cataract Surgery. JAMA Ophthalmology 2019;137(10):1156–1163. doi: 10.1001/jamaophthalmol.2019.2901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thiel CL, Schehlein E, Ravilla T, Ravindran RD, Robin AL, Saeedi OJ, … Venkatesh R. Cataract Surgery and Environmental Sustainability: Waste and Lifecycle Assessment of Phacoemulsification at a Private Healthcare Facility. Journal of Cataract and Refractive Surgery,. 2017;11(43):1391–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Venkatesh R, van Landingham SW, Khodifad AM, et al. Carbon footprint and cost–effectiveness of cataract surgery. Current Opinion in Ophthalmology 2016;27(1):82–88. [DOI] [PubMed] [Google Scholar]
- 34.Morris DS WT, Somner JEA, Connor A. The Carbon Footprint of Cataract Surgery. Eye 2013:495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu AM, Kumar P, Stein JD, Venkatesh R, Zhou Y, Robin AL. A Videographic Evaluation of Eyedrop Administration by Ophthalmic Technicians. Ophthalmology May 2021;128(5):796–798. doi: 10.1016/j.ophtha.2020.09.029 [DOI] [PubMed] [Google Scholar]
- 36.Allen M Drug Companies Make Eyedrops Too Big — And You Pay for the Waste. ProPublica October/18/2017. https://www.propublica.org/article/drug-companies-make-eyedrops-too-big-and-you-pay-for-the-waste [Google Scholar]
- 37.Namburar S, Pillai M, Varghese G, Thiel C, Robin AL. Waste generated during glaucoma surgery: A comparison of two global facilities. American Journal of Ophthalmology Case Reports 2018/December/01/ 2018;12:87–90. doi: 10.1016/j.ajoc.2018.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morris DS, Wright T, Somner JEA, Connor A. The carbon footprint of cataract surgery. Eye 2013;(27):495–501. doi:10.1038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thiel CL, Schehlein E, Ravilla T, et al. Cataract surgery and environmental sustainability: Waste and lifecycle assessment of phacoemulsification at a private healthcare facility. Journal of Cataract & Refractive Surgery 11// 2017;43(11):1391–1398. doi: 10.1016/j.jcrs.2017.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Haripriya A, Chang DF, Ravindran RD. Endophthalmitis Reduction with Intracameral Moxifloxacin Prophylaxis: Analysis of 600 000 Surgeries. Ophthalmology 2017/June/01/ 2017;124(6):768–775. doi: 10.1016/j.ophtha.2017.01.026 [DOI] [PubMed] [Google Scholar]
- 41.Bhutta M Our over-reliance on single-use equipment in the operating theatre is misguided, irrational and harming our planet. Annals of the Royal College of Surgeons of England November/01 2021;103:709–712. doi: 10.1308/rcsann.2021.0297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hii J, Sharples M, Anstey M, McGain F. When we truly need single-use equipment, will we have enough? Single-use versus reusable anaesthesia equipment: a qualitative analysis of Western Australian hospitals. Australian Health Review 2020; [DOI] [PubMed] [Google Scholar]
- 43.Sherman JD, Thiel C, MacNeill A, et al. The Green Print: Advancement of Environmental Sustainability in Healthcare. Resources, Conservation and Recycling 2020/October/01/ 2020;161:104882. doi: 10.1016/j.resconrec.2020.104882 [DOI] [Google Scholar]
- 44.MacNeill AJ, Hopf H, Khanuja A, et al. Transforming The Medical Device Industry: Road Map To A Circular Economy: Study examines a medical device industry transformation. Health Affairs 2020;39(12):2088–2097. [DOI] [PubMed] [Google Scholar]
- 45.Huncke TK, Ryan S, Hopf HW, Axelrod D, Bell C. Greening the Operating Room: Reduce, Reuse, Recycle, and Redesign Schaumburg, IL: American Society of Anesthesiologists. 2012; [Google Scholar]
- 46.Chang DF, Thiel CL, for the Ophthalmic Instrument Cleaning Sterilization Task Force. Survey of cataract surgeons’ and nurses’ attitudes toward operating room waste. Journal of Cataract & Refractive Surgery 2020;46(7):933–940. doi: 10.1097/j.jcrs.0000000000000267 [DOI] [PubMed] [Google Scholar]
- 47.Thiel CL, Zhang J, Chang DF. Differences in reuse of cataract surgical supplies and pharmaceuticals based on type of surgical facility. J Cataract Refract Surg 2022:1092–1094. vol. 9. [DOI] [PubMed] [Google Scholar]
- 48.Sherman J, McGain F, Lem M, Mortimer F, Jonas W, MacNeill A. Net zero healthcare: a call for clinician action. BMJ September/20 2021;374:n1323. doi: 10.1136/bmj.n1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Buchan J, Thiel C, Thomas P. Carbon and Cataracts: How to Make Your Service Sustainable. In: Liu C, Shalaby Bardan A, eds. Cataract Surgery: Pearls and Techniques. Springer International Publishing; 2021:227–240. [Google Scholar]
- 50.Pradere B, Mallet R, de La Taille A, et al. Climate-smart Actions in the Operating Theatre for Improving Sustainability Practices: A Systematic Review. Eur Urol 2022/February/10/ 2022;doi: 10.1016/j.eururo.2022.01.027 [DOI] [PubMed] [Google Scholar]
- 51.Wong YL, Noor M, James KL, Aslam TM. Ophthalmology Going Greener: A Narrative Review. Ophthalmology and Therapy 2021/December/01 2021;10(4):845–857. doi: 10.1007/s40123-021-00404-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thiel CL, Woods NC, Bilec MM. Strategies to Reduce Greenhouse Gas Emissions from Laparoscopic Surgery. American Journal of Public Health 2018;108(S2):S158–S164. doi: 10.2105/ajph.2018.304397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saad L Military Brass, Judges Among Professions at New Image Lows Gallup. https://news.gallup.com/poll/388649/military-brass-judges-among-professions-new-image-lows.aspx [Google Scholar]
- 54.Hayhoe K Saving us: A climate scientist’s case for hope and healing in a divided world Simon and Schuster; 2021. [Google Scholar]
- 55.Yates EF, Bowder AN, Roa L, et al. Empowering Surgeons, Anesthesiologists, and Obstetricians to Incorporate Environmental Sustainability in the Operating Room. Ann Surg Jun 1 2021;273(6):1108–1114. doi: 10.1097/sla.0000000000004755 [DOI] [PubMed] [Google Scholar]
- 56.den Boer ACL, Teherani A, de Hoop E. Discussing climate change and other forms of global environmental change during the clinical encounter: Exploring US physicians’ perspectives. The Journal of Climate Change and Health 2021/October/01/ 2021;4:100058. doi: 10.1016/j.joclim.2021.100058 [DOI] [Google Scholar]
- 57.McKimm J, Redvers N, El Omrani O, Parkes MW, Elf M, Woollard R. Education for sustainable healthcare: Leadership to get from here to there. Medical Teacher 2020:1–5. doi: 10.1080/0142159X.2020.1795104 [DOI] [PubMed] [Google Scholar]
- 58.Rublee C, Bills C, Theron E, et al. Outcomes of a Climate Change Workshop at the 2020 African Conference on Emergency Medicine. African Journal of Emergency Medicine 2021/September/01/ 2021;11(3):372–377. doi: 10.1016/j.afjem.2021.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kligler SK, Clark L, Cayon C, Prescott N, Gregory JK, Sheffield PE. Climate change curriculum infusion project: An educational initiative at one U.S. medical school. The Journal of Climate Change and Health 2021/October/01/ 2021;4:100065. doi: 10.1016/j.joclim.2021.100065 [DOI] [Google Scholar]
- 60.Hampshire K, Ndovu A, Bhambhvani H, Iverson N. Perspectives on climate change in medical school curricula—A survey of U.S. medical students. The Journal of Climate Change and Health 2021/October/01/ 2021;4:100033. doi: 10.1016/j.joclim.2021.100033 [DOI] [Google Scholar]
- 61.Luo OD, Carson JJK, Sanderson V, Vincent R. Training future healthcare sustainability leaders: Lessons learned from a Canadian-wide medical student community of practice. The Journal of Climate Change and Health 2021/October/01/ 2021;4:100066. doi: 10.1016/j.joclim.2021.100066 [DOI] [Google Scholar]
- 62.Burch H, Watson B, Simpson G, Beaton LJ, Maxwell J, Winkel KD. Mapping climate change and health into the medical curriculum: co-development of a” planetary health-organ system map” for graduate medical education. medRxiv 2021; [Google Scholar]
- 63.Shaw E, Walpole S, McLean M, et al. AMEE Consensus Statement: Planetary health and education for sustainable healthcare. Medical Teacher 2021/March/04 2021;43(3):272–286. doi: 10.1080/0142159X.2020.1860207 [DOI] [PubMed] [Google Scholar]
- 64.Gandhi V, Al-Hadithy N, Göpfert A, Knight K, van Hove M, Hockey P. Integrating sustainability into postgraduate medical education. Future Healthc J 2020;7(2):102–104. doi: 10.7861/fhj.2020-0042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ryan EC, Dubrow R, Sherman JD. Medical, nursing, and physician assistant student knowledge and attitudes toward climate change, pollution, and resource conservation in health care. BMC Medical Education 2020/June/23 2020;20(1):200. doi: 10.1186/s12909-020-02099-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Madden DL, McLean M, Brennan M, Moore A. Why use indicators to measure and monitor the inclusion of climate change and environmental sustainability in health professions’ education? Medical Teacher 2020:1–4. doi: 10.1080/0142159X.2020.1795106 [DOI] [PubMed] [Google Scholar]
- 67.Azouz S, Boyll P, Swanson M, Castel N, Maffi T, Rebecca AM. Managing barriers to recycling in the operating room. Am J Surg Apr 2019;217(4):634–638. doi: 10.1016/j.amjsurg.2018.06.020 [DOI] [PubMed] [Google Scholar]
- 68.B S. Effect of Convenience on Participation in Recycling by Anesthesia Providers in the Operating Room: A Pilot Study Depaul University; 2016. [Google Scholar]
- 69.Larsson C, Orvehed M. Carbon Offsetting, a new form of CO2lonialism? : Local implications of tree-planting projects in East Africa. Student thesis 2021. Accessed 2021–06-11t14:18:21.989+02:00. http://urn.kb.se/resolve?urn=urn:nbn:se:sh:diva-45657 [Google Scholar]
- 70.Streck C How voluntary carbon markets can drive climate ambition. Journal of Energy & Natural Resources Law 2021/July/03 2021;39(3):367–374. doi: 10.1080/02646811.2021.1881275 [DOI] [Google Scholar]
- 71.González-Ramírez J, Kling CL, Valcu A. An overview of carbon offsets from agriculture. Annual review of resource economics 2012;4(1):145–160. [Google Scholar]
- 72.De Cian E, Tavoni M. The role of international carbon offsets in a second-best climate policy: A numerical evaluation 2010; [Google Scholar]
- 73.Bebinger M Inside A Boston OR, Surgery Shows Hospital’s Steps To Reduce Its Carbon Footprint. WBUR December/19/2019. https://www.wbur.org/news/2019/12/19/boston-medical-center-operating-room-climate-friendly [Google Scholar]
- 74.Charles J, Lois AN, Mukhopadhyay C, Maibach E, Patz JA. Health professionals as advocates for climate solutions: A case study from Wisconsin. The Journal of Climate Change and Health 2021/October/01/ 2021;4:100052. doi: [Google Scholar]
- 75.Weaver E, O’Hagan C, Lamprou DA. The sustainability of emerging technologies for use in pharmaceutical manufacturing. Expert Opinion on Drug Delivery 2022/July/03 2022;19(7):861–872. doi: 10.1080/17425247.2022.2093857 [DOI] [PubMed] [Google Scholar]
- 76.Moultrie J, Sutcliffe L, Maier A. Exploratory study of the state of environmentally conscious design in the medical device industry. J Cleaner Prod 2015/December/01/ 2015;108:363–376. doi: 10.1016/j.jclepro.2015.06.014 [DOI] [Google Scholar]
- 77.Reducing Topical Drug Waste in Ophthalmic Surgery Multi-society Position Paper 2022. [Google Scholar]
- 78.Kauh CY, Blachley TS, Lichter PR, Lee PP, Stein JD. Geographic Variation in the Rate and Timing of Cataract Surgery Among US Communities. JAMA Ophthalmol Mar 2016;134(3):267–76. doi: 10.1001/jamaophthalmol.2015.5322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bach PB, Conti RM, Muller RJ, Schnorr GC, Saltz LB. Overspending driven by oversized single dose vials of cancer drugs. Bmj 2016;352:i788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Stevens J, Matheson M. Survey of the contamination of eyedrops of hospital inpatients and recommendations for the changing of current practice in eyedrop dispensing. British journal of ophthalmology 1992;76(1):36–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rahemtulla KA, Cheema MK, Nickonchuk T, Guirguis M, Al Hamarneh YN, Damji KF. Quantifying the cost of single-use minims and multidose bottles for eye drops in routine ophthalmic practice: a multicentre study. Can J Ophthalmol Jul 17 2021;doi: 10.1016/j.jcjo.2021.06.005 [DOI] [PubMed] [Google Scholar]
- 82.Berkowitz ST, Finn A, Sternberg P, Jr., Patel S. Potential Cost Savings Associated with a Multiuse Preoperative and Preinjection Eyedrop Protocol. Ophthalmology 2022;129(11):1305–1312. doi: 10.1016/j.ophtha.2022.06.023 [DOI] [PubMed] [Google Scholar]
- 83.Somner JE, Cavanagh DJ, Wong KK, Whitelaw M, Thomson T, Mansfield D. The precautionary principle: what is the risk of reusing disposable drops in routine ophthalmology consultations and what are the costs of reducing this risk to zero? Eye (Lond) Feb 2010;24(2):361–3. doi: 10.1038/eye.2009.129 [DOI] [PubMed] [Google Scholar]
- 84.Rautenbach P, Wilson A, Gouws P. The reuse of opthalmic Minims: an unacceptable cross-infection risk? Eye (Lond) Jan 2010;24(1):50–2. doi: 10.1038/eye.2009.39 [DOI] [PubMed] [Google Scholar]
- 85.ASCRS Releases Position Statement on Two Established Ophthalmic Practices 2015. https://ascrs.org/clinical-education/clinical-reports [Google Scholar]
- 86.Daehn T, Schneider A, Knobloch J, Hellwinkel OJC, Spitzer MS, Kromer R. Contamination of multi dose eyedrops in the intra and perioperative context. Sci Rep Oct 13 2021;11(1):20364. doi: 10.1038/s41598-021-99892-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nentwich MM, Kollmann K, Meshack J, Ilako DR, Schaller UC. Microbial contamination of multi-use ophthalmic solutions in Kenya. British journal of ophthalmology 2007;91(10):1265–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Clark PJ, Ong B, Stanley CB. Contamination of diagnostic ophthalmic solutions in primary eye care settings. Military medicine 1997;162(7):501–506. [PubMed] [Google Scholar]
- 89.Daehn T, Schneider A, Knobloch J, Hellwinkel OJ, Spitzer MS, Kromer R. Contamination of multi dose eyedrops in the intra and perioperative context. Scientific Reports 2021;11(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Somner J, Cavanagh D, Wong K, Whitelaw M, Thomson T, Mansfield D. The precautionary principle: what is the risk of reusing disposable drops in routine ophthalmology consultations and what are the costs of reducing this risk to zero? Eye 2010;24(2):361–363. [DOI] [PubMed] [Google Scholar]
- 91.United States Pharmacopeial Convention. USP 797: Guidebook to Pharmaceutical Compounding: Sterile Preparations Rockville, MD: 2008. [Google Scholar]
- 92.Jensen MK, Nahoopii R, Johnson B. Using multidose eyedrops in a health care setting: a policy and procedural approach to safe and effective treatment of patients. JAMA Ophthalmol Dec 2014;132(12):1476–9. doi: 10.1001/jamaophthalmol.2014.3248 [DOI] [PubMed] [Google Scholar]
- 93.Updated Guidance for Ambulatory Surgical Centers - Appendix L of the State Operations Manual (SOM) 89 (2022). [Google Scholar]
- 94.Virani S, Rewri P, Vyas A. Microbiological Safety of Using Eye Drops after One Month: Contamination Is a Rule or Mere Regulation? Delhi J Ophthalmol 2016;26(3):176–179. [Google Scholar]
- 95.Nentwich MM, Kollmann KHM, Meshack J, Ilako DR, Schaller UC. Microbial contamination of multi-use ophthalmic solutions in Kenya. British Journal of Ophthalmology 2007;91(10):1265–1268. doi: 10.1136/bjo.2007.116897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tsegaw A, Tsegaw A, Abula T, Assefa Y. Bacterial contamination of multi-dose eye drops at ophthalmology department, University of Gondar, Northwest Ethiopia. Middle East African Journal of Ophthalmology 2017;24(2):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability within anaesthesia and critical care. British Journal of Anaesthesia 2020/August/12/ 2020;doi: 10.1016/j.bja.2020.06.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.McGain F, Sheridan N, Wickramarachchi K, Yates S, Chan B, McAlister S. Carbon Footprint of General, Regional, and Combined Anesthesia for Total Knee Replacements. Anesthesiology 2021;135(6):976–991. doi: 10.1097/aln.0000000000003967 [DOI] [PubMed] [Google Scholar]
- 99.Sherman J, Le C, Lamers V, Eckelman M. Life Cycle Greenhouse Gas Emissions of Anesthetic Drugs. Anesthesia & Analgesia May. 2012;114(5):1086–1090. [DOI] [PubMed] [Google Scholar]
- 100.Sulbaek Andersen MP, Sander SP, Nielsen OJ, Wagner DS, Sanford TJ, Wallington TJ. Inhalation anaesthetics and climate change. British Journal of Anaesthesia 2010;105(6):760–766. [DOI] [PubMed] [Google Scholar]
- 101.Embick E, Bieri M, Koehler TJ, Yang A. Cost containment: an experience with surgeon education and universal preference cards at two institutions. Surg Endosc Nov 2020;34(11):5148–5152. doi: 10.1007/s00464-019-07305-9 [DOI] [PubMed] [Google Scholar]
- 102.Avansino JR, Goldin AB, Risley R, Waldhausen JH, Sawin RS. Standardization of operative equipment reduces cost. J Pediatr Surg Sep 2013;48(9):1843–9. doi: 10.1016/j.jpedsurg.2012.11.045 [DOI] [PubMed] [Google Scholar]
- 103.Cerno O Standardized surgery preference cards reduce surgery costs at MU Health Care Standardized surgery preference cards reduce surgery costs at MU Health Care 2020. [Google Scholar]
- 104.Catalyst H Analytics Driven Improvement Efforts Reduces Surgical Supply Costs by $3.2M Analytics Driven Improvement Efforts Reduces Surgical Supply Costs by $3.2M 2020. [Google Scholar]
- 105.Fitzgerald RH Jr. Microbiologic environment of the conventional operating room. Arch Surg Jul 1979;114(7):772–5. doi: 10.1001/archsurg.1979.01370310014003 [DOI] [PubMed] [Google Scholar]
- 106.Thiel CL, Schehlein E, Ravilla T, et al. Cataract surgery and environmental sustainability: Waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg Nov 2017;43(11):1391–1398. doi: 10.1016/j.jcrs.2017.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jacofsky MC, Auran RL, Williams A, Mauro S, Sietsema D. Exposure-Related Anxiety and Improving Patient Satisfaction with Medical Undergarments During Surgery: A Randomized Controlled Trial. J Bone Joint Surg Am 2022/August// 2022;104(15):1380–1385. doi: 10.2106/jbjs.22.00126 [DOI] [PubMed] [Google Scholar]
- 108.Roberts HW, Wagh VK, Mullens IJM, Borsci S, Ni MZ, O’Brart DPS. Evaluation of a hub-and-spoke model for the delivery of femtosecond laser-assisted cataract surgery within the context of a large randomised controlled trial. Br J Ophthalmol Nov 2018;102(11):1556–1563. doi: 10.1136/bjophthalmol-2017-311319 [DOI] [PubMed] [Google Scholar]
- 109.Bhalla JS, Zakai MU, Mehtani A. Immediate sequential bilateral cataract surgery and its relevance in COVID-19 era. Indian Journal of Ophthalmology 2021;69(6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Travel and Wait Times are Longest for Health Care Services and Result in an Annual Opportunity Cost of $89 Billion 2022. [Google Scholar]
- 111.Leivo T, Sarikkola A-U, Uusitalo RJ, Hellstedt T, Ess S-L, Kivelä T. Simultaneous bilateral cataract surgery: Economic analysis; Helsinki Simultaneous Bilateral Cataract Surgery Study Report 2. Journal of Cataract & Refractive Surgery 2011/June/01/ 2011;37(6):1003–1008. doi: 10.1016/j.jcrs.2010.12.050 [DOI] [PubMed] [Google Scholar]
- 112.Alio JL, Gessa-Sorroche M, Nowrouzi A, Maldonado MJ. Immediate bilateral sequential cataract surgery. Archivos de la Sociedad Española de Oftalmología (English Edition) 2022/July/01/ 2022;97(7):402–408. doi: 10.1016/j.oftale.2022.02.010 [DOI] [PubMed] [Google Scholar]
- 113.Shah V, Naderi K, Maubon L, et al. Acceptability of immediate sequential bilateral cataract surgery (ISBCS) in a public health care setting before and after COVID-19: a prospective patient questionnaire survey. BMJ Open Ophthalmol 2020;5(1):e000554. doi: 10.1136/bmjophth-2020-000554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ross N Are You Overpacking? : Association of periOperative Registered Nurses; 2007. [Google Scholar]
- 115.Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives – the old, the new, and the way forward: A narrative review. Waste Management & Research 2019;37(1):3–19. doi:10.1177/0734242×18793937 [DOI] [PubMed] [Google Scholar]
- 116.Vozzola E, Overcash M, Griffing E. Environmental considerations in the selection of isolation gowns: A life cycle assessment of reusable and disposable alternatives. American Journal of Infection Control 2018/August/01/ 2018;46(8):881–886. doi: 10.1016/j.ajic.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 117.Yu J, Ji TA, Craig M, McKee D, Lalonde DH. Evidence-based Sterility: The Evolving Role of Field Sterility in Skin and Minor Hand Surgery. Plast Reconstr Surg Glob Open 2019;7(11):e2481–e2481. doi: 10.1097/GOX.0000000000002481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Overcash M A Comparison of Reusable and Disposable Perioperative Textiles: Sustainability State-of-the-Art 2012. Anesthesia & Analgesia May. 2012;114(5):1055–1066. [DOI] [PubMed] [Google Scholar]
- 119.Balestrazzi A, Malandrini A, Montagnani F, et al. Phacoemulsificator and Sterile Drapes Contamination during Cataract Surgery: A Microbiological Study. European Journal of Ophthalmology 2012/March/01 2011;22(2):188–194. doi: 10.5301/EJO.2011.8434 [DOI] [PubMed] [Google Scholar]
- 120.Baykasoğlu A, Dereli T, Yılankırkan N. Application of cost/benefit analysis for surgical gown and drape selection: A case study. American Journal of Infection Control 2009;37(3):215–226. doi: [DOI] [PubMed] [Google Scholar]
- 121.Rutala WAP, Weber DJMD. A Review of Single‐Use and Reusable Gowns and Drapes in Health Care • Infection Control and Hospital Epidemiology 2001;22(4):248–257. [DOI] [PubMed] [Google Scholar]
- 122.Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plastic Surgery 2015/December/01 2015;23(4):235–238. doi: 10.1177/229255031502300409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Grantcharov P, Ahmed S, Wac K, Rivas H. Reprocessing and reuse of single-use medical devices: perceptions and concerns of relevant stakeholders toward current practices. JBI Evidence Implementation 2019;17(1):53–57. doi: 10.1097/xeb.0000000000000146 [DOI] [PubMed] [Google Scholar]
- 124.Unger S, Landis A. Assessing the Environmental, Human Health, and Economic Impacts of Reprocessed Medical Devices in a Phoenix Hospital’s Supply Chain. Journal of Cleaner Production 2016;112(3)doi: 10.1016/j.jclepro.2015.07.144 [DOI] [Google Scholar]
- 125.My Green Doctor Foundation. My Green Doctor Foundation 2023. https://mygreendoctor.org/
- 126.Ojala M How do children cope with global climate change? Coping strategies, engagement, and well-being. Journal of Environmental Psychology 2012;32(3):225–233. [Google Scholar]
- 127.Geiger N, Swim JK, Gasper K, Fraser J, Flinner K. How do I feel when I think about taking action? Hope and boredom, not anxiety and helplessness, predict intentions to take climate action. Journal of Environmental Psychology 2021/August/01/ 2021;76:101649. doi: 10.1016/j.jenvp.2021.101649 [DOI] [Google Scholar]
- 128.Godden NJ, Farrant BM, Yallup Farrant J, et al. Climate change, activism, and supporting the mental health of children and young people: Perspectives from Western Australia. Journal of Paediatrics and Child Health 2021;57(11):1759–1764. doi: 10.1111/jpc.15649 [DOI] [PMC free article] [PubMed] [Google Scholar]


