Abstract
Introduction:
Few instruments measure knowledge, attitudes, and beliefs (KAB) related to bladder health. Existing questionnaires have predominantly focused on KAB related to specific conditions such as urinary incontinence, overactive bladder, and other pelvic floor disorders. To address this literature gap, The Prevention of Lower Urinary Tract Symptoms Research Consortium (PLUS) developed an instrument that is being administered in the baseline assessment of the PLUS RISE FOR HEALTH longitudinal study.
Methods:
The Bladder Health Knowledge, Attitudes, and Beliefs (BH-KAB) instrument development process consisted of two phases, item development and evaluation. Item development was guided by a conceptual framework, review of existing KAB instruments, and a review of qualitative data from the PLUS Consortium Study of Habits, Attitudes, Realities, and Experiences (SHARE). Evaluation comprised three methods to assess content validity and reduce and refine items: q-sort, e-panel survey, and cognitive interviews.
Results:
The final 18-item BH-KAB instrument assesses self-reported bladder knowledge; perceptions of bladder function, anatomy, and related medical conditions; attitudes towards different patterns of fluid intake, voiding, and nocturia; the potential to prevent or treat urinary tract infections and incontinence; and the impact of pregnancy and pelvic muscle exercises on bladder health.
Conclusion:
The PLUS BH-KAB instrument may be used independently or in conjunction with other KAB instruments for a more comprehensive assessment of women’s KAB related to bladder health. The BH-KAB instrument can inform clinical conversations, health education programming, and research examining potential determinants of bladder health, LUTS, and related behavioral habits (e.g., toileting, fluid intake, pelvic muscle exercises).Key words: Bladder Health, Survey Methodology, Women’s Health, Lower Urinary Tract Symptoms, Primary Prevention
INTRODUCTION
The Prevention of Lower Urinary Tract Symptoms Research Consortium (PLUS) was established to create the evidence base for bladder health promotion and lower urinary tract symptoms (LUTS) prevention in girls and women.1 The PLUS Consortium defines bladder health as “a complete state of physical, mental, and social well-being related to bladder function and not merely the absence of LUTS,” with bladder function that “permits daily activities, adapts to short-term physical or environmental stressors, and allows optimal well-being (e.g., travel, exercise, social, occupational, or other activities).”2
Theory and evidence across decades of research support the importance of knowledge, attitudes, and beliefs (KAB) in shaping a variety of health behaviors, including eating, physical activity, sexual health behaviors, refraining from substance use or using substances in moderation, and injury-prevention behaviors.3,4 Thus one hypothesizes that an individual’s KAB around bladder health and lower urinary tract function may influence daily choices about toileting, activities, diet, and fluid intake, and therefore have significant impact on long-term bladder health. KAB may also shape perceptions of what is normal and influence when and how one changes behaviors such as self-management and treatment-seeking for early LUTS. A small body of literature suggests that knowledge deficits exist with respect to bladder health, as well as attitudes and beliefs that may lead to less than optimal bladder health behaviors (e.g., thinking it is normal to leak urine and not seeking treatment for symptoms).5–8 Among its research aims, PLUS prioritized the assessment of women’s bladder health and related KAB in planning their RISE FOR HEALTH (RISE) longitudinal study.9,10 Understanding what women from varied backgrounds at different ages know, think, and believe about overall bladder health and not only LUTS will inform the development of bladder health promotion strategies and LUTS prevention interventions.
There are a limited number of validated instruments that measure KAB related to bladder health. Existing tools have predominantly focused on KAB related to LUTS such as urinary incontinence (UI) and overactive bladder, as well as other pelvic floor disorders. These instruments include the Urinary Incontinence Knowledge Scale (UIKS),11 the Incontinence Quiz,12 the Prolapse and Incontinence Knowledge Questionnaire (PIKQ),13 and the Adolescent Bladder and Pelvic Health Questionnaire (ABPHQ).8 Other KAB instruments were designed by researchers to meet specific study objectives and did not undergo a rigorous development process.14–18 Collectively, these KAB instruments are limited by their focus on UI (e.g., etiology, relationship to aging, symptoms, impacts, prevention, treatment, and management); perceived bladder function norms and attitudes towards UI and treatment-seeking for urinary symptoms; toileting behaviors; and KAB and/or practices of pelvic muscle exercises in women with UI or who are pregnant or postpartum.5, 12–19 Few instruments measure knowledge of pelvic anatomy and function,5 or KAB about factors that influence overall bladder health such as dietary, hygiene, and voiding behaviors as opposed to only symptoms. Current KAB instruments are also limited by their focus on UI, populations studied, lack of a conceptual framework and operational definition of bladder health guiding instrument design, and limited items measuring beliefs related to bladder health and factors that may influence bladder health.
To address limitations of prior instruments, PLUS developed an instrument that assessed KAB related to bladder health and function among women. This paper describes the process used to develop the KAB instrument and assess its face and content validity in women from varied backgrounds.
METHODS
2.1. Overview
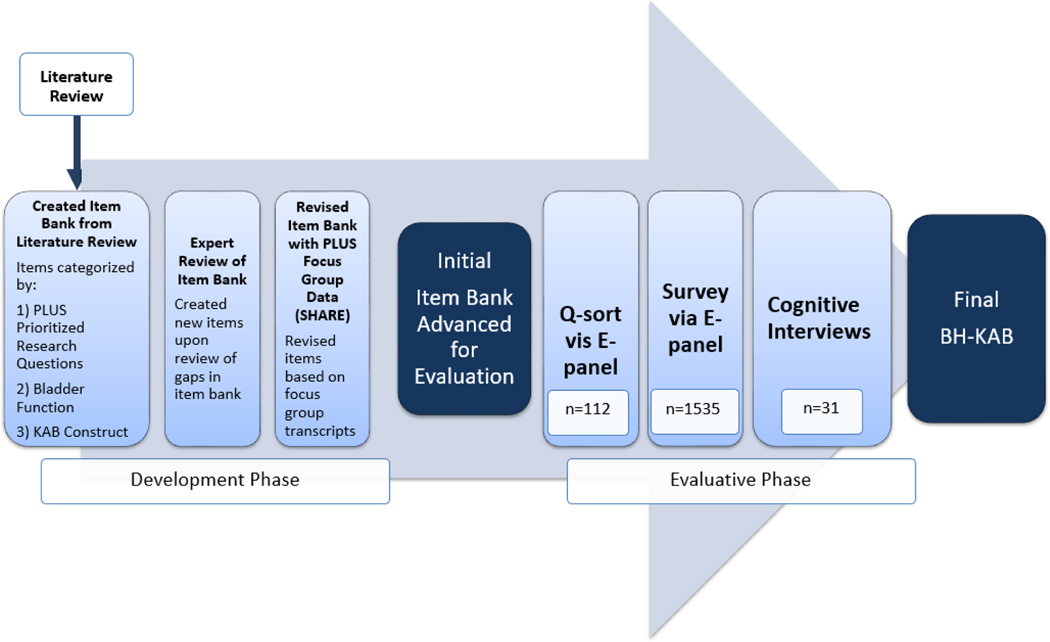
The Bladder Health Knowledge, Attitudes, and Beliefs (BH-KAB) instrument development process consisted of two phases, item development and evaluation (Figure 1). The item development phase was guided by a review of existing bladder- or pelvic floor-related KAB instruments, a review of qualitative data from the PLUS Consortium Study of Habits, Attitudes, Realities, and Experiences (SHARE), 20 and expert opinion. The evaluative phase comprised three methods to establish face and content validity and refine and reduce items: q-sort, 21,22 e-panel survey,23 and cognitive interviews.24 The transdisciplinary KAB workgroup conducting the development process contained members from medicine, nursing, midwifery, public health, psychology, women’s studies, and psychometrics. , including clinicians with expertise in LUTS care.
Figure 1.
Development and Evaluative Phases of Item Development for the Bladder Knowledge, Attitudes, and Beliefs (BH-KAB) instrument.
2.2. Item Development Phase
PLUS developed a conceptual framework to guide the development of items related to women’s bladder health. This framework places individuals within an ecosystem of risk and protective factors, including interpersonal relationships (e.g., family influence), institutions (e.g., school and workplace environments), community (e.g., cultural norms), and societal structures that facilitate or constrain health. Within this framework, KAB are conceptualized as key individual-level determinants of health behaviors.25–27 The KAB workgroup focused on KAB that may influence general knowledge about the bladder and related behaviors. The KAB instrument described in this article is intended to measure variation in KAB across women and inform future bladder health education efforts. It contains items to assess general knowledge about the bladder and selected KAB in relation to toileting behaviors, fluid intake, pregnancy, childbirth, and the pelvic floor.
2.2.1. Literature Review and Expert Review of Initial Item Bank
Initially, the KAB working group conducted a literature review to identify an existing bladder health KAB instrument or items that addressed four PLUS prioritized research topics (Table 1). This review identified 268 unique items from questionnaires derived from 32 papers on bladder related KAB. Most items focused on urinary incontinence and not bladder health. Existing questions from the literature were categorized based on the Consortium’s research topics and questions relevant to KAB (Table 1) and KAB relative to bladder health function domains (storage, emptying, bioregulatory).2,28 Among the items identified through the literature review, almost half were related to the prioritized research questions (n=131, 45%). Overall, nearly half assessed knowledge/beliefs (n=164, 49%), some described attitudes (n=27, 10%), and the majority assessed one of the three bladder function domains (n=208, 78%). Once the items were compiled and categorized, non-KAB items and redundancies were eliminated and gaps in the item bank were identified. The KAB workgroup used an iterative process to develop new items and subsequently prioritized a revised set (n=133).
Table 1.
PLUS Research Topics and Questions Relevant to BH-KAB
| PLUS Topic | KAB-Related Question |
|---|---|
|
| |
| Influence of one’s own and others’ bladder-related KAB on behavior | How are women’s bladder-related behaviors influenced by their own bladder-related KAB, |
| Pelvic floor muscles | When and how do women learn about their pelvic floor muscles? |
| Pregnancy | How do KAB about pregnancy and postpartum influence bladder health? |
2.2.2. Review of Codes from PLUS Focus Groups (SHARE)
As foundational work for measuring bladder health and bladder health-related KAB, PLUS previously conducted the SHARE study.20,29 Forty-four focus groups were held with 360 adolescent and adult women ages 11–93 years who were diverse with respect to age, race, ethnicity, geography, and socio-economic status. SHARE study methods are detailed elsewhere.20,30 The review of SHARE codes aimed to identify common terminology and topics that were not previously captured by the literature review or working group augmentation of the item bank. Working group members who participated in the SHARE study, reviewed and identified codes related to KAB. Assessment of the following SHARE codes were conducted by two-person teams for each code: “Bladder Knowledge Acquisition,” “Bladder Knowledge,” “Bladder Assumptions and Beliefs,” “Fluid Intake,” and “I don’t know.” Review by each team prompted changes to language of existing KAB items and development of new items. After addition of items based on SHARE transcript review, the KAB item bank contained 154 unique items. The workgroup advanced items that were present in SHARE focus groups, had evidence for association with LUTS (e.g., weight gain or loss) based on working group knowledge of the literature, and/or were deemed a priority by expert clinician review. A resulting 112 items were forwarded to the evaluative phase.
2.3. Evaluative Phase
A three-stage approach assessed the relevance and content validity of the KAB items: q--sort, e-panel survey, and cognitive interviews. Institutional Review Board (IRB) approval for the q-sort and e-panel survey was obtained by the Scientific and Data Coordinating Center. Approval for the cognitive interviews was obtained from the IRBs at all four participating sites. The following sections detail the methodology for each approach.
2.3.1. Q-sort Method via E-panel
Q-methodology is way of extracting subjective opinions.31 The primary technique of q-methodology is the q-sort, which involves rank-ordering a set of items from very strongly agree to very strongly disagree.32 The item bank was quite large at the conclusion of the item development phase. Thus, the goal of the KAB q-sort was to narrow the large array of items to those bladder related topics that most resonated with participants, while also being judged to be meaningful by clinicians in the working group. Q-sort participants were recruited by Dynata (Shelton, CT), a marketing data service firm. Dynata invites potential respondents from an enrolled panel of members to complete a survey using a private and secure portal. We aimed to include respondents in each of four age groups: 18–25 years, 26–45 years, 46–64 years and >65 years. Respondents received a small incentive for completing e-panel surveys. One hundred and twelve participants formed this e-panel and completed the q-sort survey online using a specialized sorting program, QSorTouch (www.qsortouch.com).33 Informed consent was obtained through Dynata, and demographic data of participants were collected. The q-sort technique was performed in two steps. First, participants followed a survey link where they were asked to provide their level of agreement with items in a set of statements. Then, they sorted these statements into a grid based on level of agreement with the item according to specific prompts (e.g., Do you disagree or agree with the following statements about your bladder?). Although the number of grid boxes can vary in the q-sort technique, 9 grid boxes were chosen due to the number of items being sorted. In a q-sort, it is ideal to have only a small number of items in each grid box and to have approximately the same number of items in each box. Participants could not put more than 4 or 5 statements into any one of 9 grid boxes ranging from −4 (Very strongly disagree) to +4 (Very strongly agree) with respect to overall level of agreement. If participants neither agreed nor disagreed, they could sort items into a “Neutral or Unsure” box. In addition to the q-sort items, participants completed a small subset of e-panel survey questions that would be tested more fully during the survey stage.
Ninety-four statements were generated for the q-sort from the 112 items advanced to the evaluative phase. Several of the items were excluded because they did not convert well to statement form or were merged with another item. Three separate q-sets and corresponding prompts were constructed: (1) Do you agree or disagree with the following statements about your bladder? (52 items) (2) Which of the following things are good for your bladder and which are bad for your bladder? (25 items) (3) Which of the following are signs that your bladder is working well and which are signs your bladder is not working well? (17 items). Collectively, sets included topics on bladder function, medical conditions associated with bladder health, pelvic muscle function, pregnancy and bladder health, fluid consumption, voiding with urge, delayed voiding, and characteristics of urine. To decrease participant burden, q-sorting was divided between two groups of participants (n=60 and n=52); each group completed a subset of q-sort questions. Data from the sorting program were exported as a .csv file and analyzed using Ken-Q Analysis v. 1.0.6. 34
2.3.2. Survey Method via e-panel
Items were reviewed by the working group after the q-sort. Thirty-eight prioritized items were advanced to a second evaluation method, a survey via e-panel that aimed to assure sufficient variation in responses. In addition, items assessing pelvic anatomy were introduced. Another Dynata e-panel with 1535 participants was recruited to receive a separate set of survey items that assessed variation in item response when using varying stems (i.e., questions) and response options. The workgroup recognized that the number of q-sort participants in the 18–25 year old group was insufficient. Sampling targets of equal distribution of all four age categories was set for the Survey e-panel. Additionally, we aimed to have half of the participants completing high school or less. Informed consent was obtained through Dynata, and demographic data of participants were collected. The e-panel process allowed for randomization of alternative stem and response options and efficient presentation of items. The distribution of responses was evaluated. The KAB working group selected items to advance to the cognitive interviewing stage for further assessment of language and concept understanding.
2.3.3. Cognitive Interview Method
Lastly, cognitive interviewing, an iterative process aimed to evaluate the survey items using a think-aloud method and verbal probing, was conducted to assure participants interpreted remaining items in the pool as intended.35–37 The working group reviewed the e-panel survey items and prioritized those that were advanced to interviews. Thirty-one women aged 18 and above were recruited from the four PLUS sites where IRB approval was obtained. Individuals were included who had female sex assigned at birth, fluent in written and spoken English (may be bilingual), age ≥18 years old, available for a virtual 2 hour interview and questionnaire completion, able to read and provide verbal or written consent, and access to a computer with internet, audio and video capabilities for participants completing their interviews virtually. Those who had physical or mental conditions that would impede participation in interviews or completion of questionnaires were excluded. Each site recruited women primarily from the community, but also from clinical settings. Throughout recruitment, strategies were adjusted to ensure a sample with a range of LUTS experiences and variation in age, race, ethnicity, and education.
Consent was obtained prior to one-on-one interviews, which were conducted using a secure virtual meeting platform. Interviewers presented items individually to participants and followed a standardized interview structure, including common probes to assess understanding of each item and unique probes to elicit feedback on specific items. Cognitive interviews were conducted using multiple rounds over 6 weeks to assess 69 items. The KAB working group reviewed item performance and each interviewee’s comments weekly. This review informed edits and subsequent sets of items advanced to the following week’s interviews. Saturation was reached on the 6th round after 31 interviews.
RESULTS
As a result of the evaluative phase, the BH-KAB instrument was developed. The number of items considered at different stages of the process were as follows: q-sort (94 items), survey (38 items), and cognitive interview (69 items). Below, key findings from each stage of the evaluative phase are presented. Selective findings describe how specific items of the final Bladder Health Knowledge, Attitudes, and Beliefs (BH-KAB) instrument were influenced by evaluation data.
Table 2 contains distributions of sociodemographic variables across different stages of evaluation. The two older age groups (46–64, 65+) were overrepresented in q-sort samples. Age groups were more evenly distributed in survey and cognitive interview samples. Roughly 20% of q-sort and cognitive interview samples and 45% of the survey sample were comprised of women whose highest level of education was a high school degree or less. Remaining women were predominantly distributed across the associate’s degree, bachelor’s degree, or master’s degree categories, with fewer women reporting a doctoral or professional degree or vocational or technical degree. While samples were predominantly White across all evaluation stages (58%−92%), greater racial/ethnic diversity was observed for the survey and cognitive interview samples. Twelve percent of the survey sample reported being Black or African American, and 13% reported being Hispanic. Thirteen percent of the cognitive interview sample reported being Asian, and 22% reported being Black or African American. Table 3 demonstrates that our participants represent the spectrum of LUTS.
Table 2.
Demographic Characteristics of Q-sort, e-panel survey, and cognitive interview participants.
| Q-sort 1 a (N=60) | Q-sort 2 a (N=52) | E-Panel Survey (N=1535) | Cognitive Interviews (N=31) | |
|---|---|---|---|---|
|
| ||||
| n (%) | n (%) | n (%) | n (%) | |
| Age Group | ||||
| 18–25 | 1 (1.7%) | 0 (0%) | 256 (16.7%) | 8 (25.8%) |
| 26–45 | 14 (23.3%) | 1 (1.9%) | 314 (20.5%) | 5 (16.1%) |
| 46–64 | 24 (40.0%) | 22 (42.3%) | 417 (27.2%) | 11 (35.5%) |
| 65+ | 19 (31.7%) | 26 (50.0%) | 469 (30.6%) | 4 (12.9%) |
| Missing | 2 (3.3%) | 3 (5.8%) | 79 (5.1%) | 3 (9.7%) |
| Education | ||||
| Completed HS or less | 14 (23.3%) | 11 (21.2%) | 691 (45.0%) | 6 (19.4%) |
| Associate’s degree or some college | 13 (21.7%) | 13 (25.0%) | 322 (21.0%) | 4 (12.9%) |
| Bachelor’s degree | 19 (31.7%) | 17 (32.7%) | 297 (19.3%) | 14 (45.2%) |
| Master’s degree | 9 (15.0%) | 11 (21.2%) | 150 (9.8%) | 6 (19.4%) |
| Doctoral or Professional degree | 3 (5.0%) | 0 (0%) | 33 (2.1%) | 0 (0%) |
| Vocational or technical degree | 2 (3.3%) | 0 (0%) | 42 (2.7%) | 0 (0%) |
| Missing | 0 (0%) | 0 (0%) | 0 (0%) | 1 (3.2%) |
| Race and Ethnicity | ||||
| Asian | 4 (6.7%) | 3 (5.8%) | 73 (4.8%) | 4 (12.9%) |
| Black or African American | 4 (6.7%) | 0 (0%) | 190 (12.4%) | 7 (22.6%) |
| Top Eastern or North African | 0 (0%) | 0 (0%) | 0 (0%) | 1 (3.2%) |
| Hispanic | 4 (6.7%) | 0 (0%) | 199 (13.0%) | 0 (0%) |
| White or Caucasian | 47 (78.3%) | 48 (92.3%) | 1029 (67.0%) | 18 (58.1%) |
| Another Race, Ethnicity, or Origin | 1 (1.7%) | 1 (1.9%) | 43 (2.8%) | 1 (3.2%) |
| Missing | 0 (0%) | 0 (0%) | 3 (0.2%) | 0 (0%) |
In addition to completing the q-sort, participants in Q-Sort 1 and Q-Sort 2 completed a small subset of e-panel survey questions. To avoid “double-counting” participants in terms of considering the diversity of all participants, they are excluded from the demographic variable distributions for the e-panel survey column.
Table 3.
LUTS Characteristics of E-Panel Survey and Cognitive Interview Participants.
| E-Panel Survey (N=1535) | Cognitive Interviews (N=31) | |
|---|---|---|
|
| ||
| In the past year have you been told by a health care provider that you had a urinary tract infection (UTI)? | ||
| I have never had a UTI in my life | 506 (33.0%) | 9 (29.0%) |
| No, I haven’t had a UTI in the past year | 783 (51.0%) | 17 (54.8%) |
| Yes | 245 (16.0%) | 5 (16.1%) |
| Missing | 1 (0.1%) | 0 (0%) |
| In the past year, have you ever accidentally leaked urine, even just a drop or two? | ||
| No, not even once in the past year | 447 (29.1%) | 7 (22.6%) |
| Only once or twice over the entire year | 373 (24.3%) | 5 (16.1%) |
| Up to six times over the entire year | 225 (14.7%) | 10 (32.3%) |
| At least once a month every month | 180 (11.7%) | 4 (12.9%) |
| More often than that | 305 (19.9%) | 5 (16.1%) |
| Missing | 5 (0.3%) | 0 (0%) |
| In the past year, have you experienced any of the following? Please do NOT count or consider times when this was a result of having a UTI. | ||
| Trouble or difficulty starting to pee | ||
| Yes | 247 (16.1%) | 3 (9.7%) |
| No | 1280 (83.4%) | 28 (90.3%) |
| Missing | 8 (0.5%) | 0 (0%) |
| Feel you like are not completely emptying your bladder | ||
| Yes | 398 (25.9%) | 12 (38.7%) |
| No | 1125 (73.3%) | 19 (61.3%) |
| Missing | 12 (0.8%) | 0 (0%) |
| Dribbling at least a few drops after you think you have finished peeing | ||
| Yes | 711 (46.3%) | 13 (41.9%) |
| No | 820 (53.4%) | 18 (58.1%) |
| Missing | 4 (0.3%) | 0 (0%) |
3.1. Q-sort Key Findings
Examples of highest ranked factors included “Kegel exercises make your pelvic muscles stronger,” “My bladder holds urine,” and “My bladder releases urine.” In contrast, lowest ranked factors included “Pelvic muscles have no effect on sex,” “Having a baby can improve bladder control,” and “My bladder digests food.”
The q-sort informed response options for different questions on the BH-KAB, including the bladder function question, “From what you understand, which of the following things does the bladder do?” (Appendix, Item 2). To assess variance in knowledge about bladder function, q-sort participants were asked, “Do you agree or disagree with the following statements about your bladder?” Responses were included in Item 2 if they elicited very high agreement (e.g., my bladder holds urine) or very low agreement (e.g., my bladder digests food.) These rankings assisted the workgroup in identifying items that were clearly correct and incorrect to many participants.
Q-sort results assisted in excluding response options for specific BH-KAB questions. For example, participants were asked, “Which of the following things are good for your bladder and which are bad for your bladder?” Lowest ranked items for practices considered “good” or “bad” were excluded from a BH-KAB question assessing knowledge about prevention of UTIs (Appendix, Item 9), including wiping the genital region prior to sex and wiping the genital region from back to front after voiding. Highly ranked items were retained, including “peeing after sex” and “wiping from front to back.” Additionally, entire items were excluded upon review of the Q-sort results. Items assessing characteristics of urine (e.g., color of urine, force of urine stream) were not viewed as salient by q-sort participants with respect to whether the bladder was working and were subsequently excluded from the item pool.
3.2. Survey via E-panel Key Findings
A survey via e-panel assessed three characteristics of female pelvic anatomic diagrams. The distribution of responses was compared across front versus side views, color versus black and white images, and inclusion versus exclusion of pelvic muscles. Greater variation in responses (utilization of all response options) and accuracy of responses was elicited when the front view was provided. Less variation and accuracy were noted when pelvic muscles were included. The KAB workgroup selected a front-facing anatomic diagram without pelvic muscles as the final BH-KAB item. There was no difference between the color and black and white images; as such, the color diagram was not selected given the associated expense.
Additionally, e-panel findings assisted in the selection of terminology. Disparate results were elicited when the phrase, “pelvic muscle exercises” was compared to “Kegel exercise.” There was lower endorsement of items using the terminology “Kegel,” suggesting that many women were less aware of the term “Kegel” than “pelvic muscle” in relation to pelvic muscle exercises. Separate items using the terminology “pelvic muscle exercise” and “Kegel exercise” were advanced to cognitive interviewing for additional item refinement.
3.3. Cognitive Interview Key Findings
While most participants understood and interpreted the items as intended, cognitive interviewing revealed issues with some items that required alterations across multiple rounds. Two key examples were pelvic muscle exercise terminology and the concepts of LUTS prevention, treatment, and cure.
Whereas the e-panel was designed to elicit the distribution of responses when the terms “Kegel” and “pelvic muscle” exercise were varied, cognitive interviews were designed to determine if women understood items when either term was used. The terminology of “pelvic muscle exercises” compared to “Kegel exercises” was probed. Some women thought each term referred to distinctly different activities. This feedback prompted a redesign and retesting of items through cognitive interviews. Participants were first asked whether they were familiar with each term and then asked a set of questions using the term(s) with which they were familiar. Subsequent interviewees endorsed excellent understanding of questions after this modification. In the final BH-KAB instrument, KAB related to “pelvic muscle exercises” and “Kegel exercises” are assessed separately for familiarity with terms, perceived benefits of exercises, and the timing and source of learning about exercises.
The concepts of prevention, treatment, and cure were deemed problematic by participants. Some described prevention and treatment as the same concept. Others distinguished between the public health concepts of primary and secondary prevention, noting that prevention meant that a disease never happens, or that a disease or symptom ever happens “again.” One participant stated she had “no idea what prevention means.” Others noted that treatment and cure were the same if the treatment was successful. One participant interpreted cure to imply “world-wide” cure. These comments highlighted the ambiguous wording of our items. Revised items were assessed in a subsequent cognitive interviewing round. Feedback resulted in inclusion of only the terms “prevent” and “treat” (Appendix, items 12 and 13).
3.4. Final BH-KAB Items
The final BH-KAB instrument contains 18 items (Appendix). By design, all items are related to PLUS research topics and questions relevant to KAB (Table 1). The items assess self-reported bladder knowledge; perceptions of bladder function, anatomy, and related medical conditions; attitudes towards different patterns of fluid intake, voiding, and nocturia; the potential to prevent or treat urinary tract infections (UTI) and incontinence; and the impact of pregnancy and pelvic muscle exercises on bladder health (Table 4). Questions were written to be understood by women with varying degrees of educational attainment. The Flesch-Kinkaid Reading Grade Level for the final items was 6.7.
Table 4.
Topics in the Bladder Knowledge, Attitudes, and Beliefs (BH-KAB) Instrument by Item.
| Item | Topic |
|---|---|
|
| |
| 1 | Bladder knowledge self-assessment |
| 2 | Bladder function |
| 3 | Bladder anatomy |
| 4 | Related medical conditions |
| 5 | Water consumption and bladder health |
| 6 | Perception of fluid types |
| 7 | Voiding with urge |
| 8 | Nocturia |
| 9 | Prevention of UTIs |
| 10 | Aging and incontinence |
| 11 | Incontinence treatment |
| 12 | Prevention and treatment – provider |
| 13 | Prevention and treatment - woman |
| 14 | Pregnancy’s impact on bladder function |
| 15 | Duration of pregnancy’s impact on incontinence |
| 16 | Pelvic muscle exercises – function, knowledge acquisition |
| 17 | Kegel exercises – function, knowledge acquisition |
| 18 | Pelvic muscle exercises and pregnancy |
DISCUSSION
The PLUS Consortium conceptualized KAB as important individual-level determinants of bladder health behaviors in women. This paper focuses on the development and face and content validation of questions to assess bladder health-related KAB in women. In contrast to established KAB instruments,5, 11–13 which focus on specific urinary symptoms, the PLUS Bladder Health Knowledge, Attitudes, and Beliefs (BH-KAB) instrument concisely assesses multiple domains that participants and investigators determined were of the greatest importance to inform strategies to promote bladder health among women. Unique topics assessed in the B-KAB compared to prior instruments used in adult women include knowledge about urinary tract anatomy, healthy bladder function, and medical conditions that affect bladder health, as well as perceived effects of different types of fluid intake, including water consumption, on bladder health, and perceived effects of different voiding patterns in response to urge. Our instrument may be used by practitioners and researchers to identify gaps in knowledge and health-compromising attitudes and beliefs that should be addressed through prevention and intervention strategies tailored to individuals and communities.
A variety of methods were employed in the development of the BH-KAB and evaluation of its face and content validity, including published literature, expert opinion, qualitative data review, surveys, and cognitive interviews of women from varied communities. In contrast to the majority of prior research,11–19 our methodology incorporated women with and without LUTS from various age, education, racial, and ethnic groups, which allowed for a range of lived experiences to guide refinement of the BH-KAB. This approach was necessary to develop an instrument that is likely to be relevant and valid for the assessment of bladder-related KAB across the lifespan of adult women. The three evaluation techniques provided varying levels of information. Data from the cognitive interviews seemed to more strongly inform the content and edits of items ultimately included in the instrument. Our experience aligns with literature highlighting the utility of cognitive interviews.38 The e-panel survey did, however, identify variations in responses; this led to greater confidence that items would elicit adequate variability when administered in future research. The least informative method was the e-panel q-sort, although it had good utility in directing the BH-KAB working group toward items that were salient to participants.
Administration of the BH-KAB instrument in the RISE study, a large national longitudinal study, will enable PLUS investigators to determine how KAB factors align with other assessed constructs, including self-reported behaviors and social determinants of health (SDOH), to broadly inform future strategies to promote bladder health in women. PLUS investigators will examine individual BH-KAB items in relation to self-reported behaviors and SDOH. The RISE study will poise investigators to examine how individual-level factors interact with social and systemic factors to inform prevention approaches that can be tailored to the needs of individuals and communities. In addition, the large sample planned in RISE will allow examination of how individual items are distributed, with consideration of creating a scoring algorithm for specific subscales that can then undergo psychometric evaluation.
Compared to other bladder-related KAB instruments that also used a multimethod approach in establishing content validity (e.g., literature review, expert opinion, cognitive interviews, and/or pilot testing), 5, 11–13 our development process involved multiple evaluation stages (q-sort, survey, cognitive interviewing) with a total of 1678 women. The present validation included a larger number of women in comparison to other KAB instrument validation studies. Attempts were made to recruit a sample that varied with respect to race, ethnicity, and education. Within the e-panel sample, which involved over 1,500 women, over 12% of women identified as Black or African American, and 13% identified as Hispanic. Roughly 20% or more of participants at each stage of evaluation reported that their highest level of education was a high school degree or less; this assisted our team in developing questions that are likely to be understood by women with different levels of education. Limitations must also be acknowledged. While BH-KAB development and evaluation phases attempted to engage a diverse sample of women, samples were predominantly White. Future research should examine whether KAB varies across women of different racial and ethnic groups, and whether associations between KAB and bladder behaviors vary across groups. Such research would inform culturally tailored prevention and intervention approaches. Another limitation was the use of online panels, which limited participation in this portion of the process to women with internet access. It is also important to note that the PLUS BH-KAB instrument was developed for adult women aged 18 years and over. Central to the PLUS Consortium research agenda is the concept that bladder health KAB should be evaluated across the lifespan. The development of a similar instrument for adolescent girls is planned in the future.
1. CONCLUSION
The PLUS BH-KAB instrument can inform clinical conversations, health education programming, and research examining potential determinants of bladder health, LUTS, and related behavioral habits (e.g., toileting, fluid intake, pelvic muscle exercises). The BH-KAB instrument will also be useful for research examining how variations in social and community context and systemic factors such as racism, economic privilege, and deprivation can influence KAB about bladder health. Inclusion of the BH-KAB instrument in the RISE study provides a unique opportunity to inform the future of women’s bladder health promotion and LUTS prevention interventions.
Supplementary Material
Acknowledgements:
We gratefully acknowledge the collegial work of the Prevention of Lower Urinary Tract Symptoms (PLUS) Research Consortium members, listed below.
Loyola University Chicago - Maywood, IL (U01DK106898)
Multi-Principal Investigators: Linda Brubaker, MD; Elizabeth R. Mueller, MD, MSME
Investigators: Marian Acevedo-Alvarez, MD; Colleen M. Fitzgerald, MD, MS; Cecilia T. Hardacker, MSN, RN, CNL; Jeni Hebert-Beirne, PhD, MPH; Missy Lavender, MBA.
Northwestern University - Chicago IL (U01DK126045)
Multi-Principal Investigators: James W. Griffith, PhD; Kimberly Sue Kenton, MD; Melissa Simon, MD,MPH; Investigators: Julia Geynisman-Tan, MD; Oluwateniola Brown, MD; Margaret Mueller, MD
University of Alabama at Birmingham - Birmingham, AL (U01DK106858)
Principal Investigator: Alayne D. Markland, DO, MSc
Investigators: Tamera Coyne-Beasley, MD, MPH, FAAP, FSAHM; Kathryn L. Burgio, PhD; Cora E. Lewis, MD, MSPH; Gerald McGwin, Jr., MS, PhD; Camille P. Vaughan, MD, MS; Beverly Rosa Williams, PhD.
University of California San Diego - La Jolla, CA (U01DK106827)
Principal Investigator: Emily S. Lukacz, MD
Investigators: Sheila Gahagan, MD, MPH; D. Yvette LaCoursiere, MD, MPH; Jesse Nodora, DrPH.
University of Michigan - Ann Arbor, MI (U01DK106893)
Principal Investigator: Janis M. Miller, PhD, APRN, FAAN
Investigators: Lisa Kane Low, PhD, CNM, FACNM, FAAN, Abigail Smith PhD
University of Minnesota (Scientific and Data Coordinating Center) - Minneapolis MN (U24DK106786)
Multi-Principal Investigators: Kyle D. Rudser, PhD; Jerry McGwin
Investigators: Sonya S. Brady, PhD; Haitao Chu, MD, PhD; Cynthia S. Fok, MD, MPH; Peter Scal, PhD; Todd Rockwood, PhD.
University of Pennsylvania - Philadelphia, PA (U01DK106892)
Principal Investigator: Multi-Principal Investigators: Diane K. Newman, DNP FAAN; Ariana L. Smith, MD
Investigators: Amanda Berry, MSN, CRNP; Andrea Bilger, MPH; Heather Klusaritz, PhD, MSW; Terri Lipman, PhD, CRNP; Ann E. Stapleton, MD; Jean F. Wyman, PhD.
Washington University in St. Louis - Saint Louis, MO (U01DK106853)
Principal Investigator: Siobhan Sutcliffe, PhD, ScM, MHS
Investigators: Aimee S. James, PhD, MPH; Jerry L. Lowder, MD, MSc; Melanie R. Meister, MD, MSCI.
Yale University - New Haven, CT (U01DK106908)
Principal Investigator: Leslie M. Rickey, MD, MPH
Investigators: Marie A. Brault, PhD (Dec. 2020-); Deepa R. Camenga, MD, MHS; Shayna D. Cunningham, PhD.
Steering Committee Chair: Linda Brubaker, MD. UCSD, San Diego. (January 2021-)
NIH Program Office: National Institute of Diabetes and Digestive and Kidney Diseases, Division of Kidney, Urologic, and Hematologic Diseases, Bethesda, MD.
NIH Project Scientist: Julia Barthold, M.D.
Funding for this work was provided through the following NIH awards:
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) at the National Institutes of Health (NIH) by cooperative agreements [U24 DK106786, U01 DK106853, U01 DK126045, U01 DK106858, U01 DK106898, U01 DK106893, U01 DK106827, U01 DK106908, U01 DK106892]. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
For the Prevention of Lower Urinary Tract Symptoms (PLUS) Research Consortium, National Institutes of Health (NIH), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
Footnotes
Data Availability Statement: no data
The authors affirm that all required disclosures are included here:
All authors receive support from the NICH PLUS Research Consortium. Additional disclosures are as follows:
D. Yvette LaCoursiere, MD, MPH: received CalMed Grant funding and served on SASGOG Board of Directors
Lisa Kane Low, PhD, CNM: received grants from NIDDK, Consulting fees from the American College of Nurse-Midwives, received honoraria for speaking engagements Mississippi Perinatal Quality Collaborative, Brown University, University of California, San Diego and grant funding from Greenwall Foundation, Regional Perinatal Quality Collaborative; received travel support from ACOG as a Liaison to CREOG, served as a board member for Growing Futures Together and Birth Detroit
Sara Putnam, MS: no disclosures
Jean F. Wyman, PhD: received consulting fees from the University of Pennsylvania, Department of Obstetrics and Gynecology, served on SUNA publications committee,
Diane K. Newman, DNP: Received grant from Hollister and SUNA for survey research, received royalties from Springer Nature, served as an advisor for Coloplast, Convatec and Urovant Sciences, received faculty honoraria from the American Urological Association for an APP course and editorial honoraria from Digital Science Press
Shayna Cunningham, PhD, MHS: no disclosures
Leslie Rickey, MD, MPH: Author royalties from UptoDate, served on Renovia Advisory Board, Urocure LLC Quality and Safety Oversight Committee
Amanda Berry, PhD, MSN, CRNP: no disclosures
Sheila Gahagan, MD, MPH: no disclosures
Camille P. Vaughan, MD, MS: Received grants/contracts from US Department of Veteran’s Affairs, Agency for Healthcare Research and Quality, NIH; received consulting fees from Becton, Dickinson & Company
Oluwateniola Brown, MD: no disclosures
Sonya S. Brady, PhD, LP: received travel reimbursement and honorarium for speaking engagement from NIH
Information excluded from drafts to anonymize the manuscript:
University of Minnesota Institutional Review Board (IRB) approval for the q-sort and e-panel survey was obtained by the PLUS Scientific and Data Coordinating Center. Approval for the cognitive interviews was obtained from the IRBs at all four participating PLUS sites: University of Alabama at Birmingham, University of Michigan, University of Pennsylvania, and University of Minnesota.
In June 2007 the ICMJE adopted the WHO’s definition of clinical trial: “any research study that prospectively assigns human participants or groups of humans to one or more health-related interventions to evaluate the effects on health outcomes.” No components of this work contained interventions and we did not assess any intervention’s impact on health outcomes. Participant were included to assess the salience of items, question stems and responses during the survey development process. As such this was not a clinical trial and did not require registering as such.
Contributor Information
D. Yvette LaCoursiere, Department of Obstetrics, Gynecology and Reproductive Sciences, University of California, San Diego, La Jolla CA.
Lisa Kane Low, University of Michigan, School of Nursing, Ann Arbor MI.
Sara Putnam, University of Minnesota School of Public Health, Division of Biostatistics, Minneapolis MN.
Jean F. Wyman, University of Minnesota, School of Nursing, Minneapolis MN.
Diane K. Newman, University of Pennsylvania, Perelman School of Medicine, Philadelphia PA.
Shayna Cunningham, Department of Public Health Sciences, University of Connecticut School of Medicine, Farmington CT.
Leslie Rickey, Yale School of Medicine, New Haven CT.
Amanda Berry, Children’s Hospital of Philadelphia, Philadelphia PA.
Sheila Gahagan, University of California, San Diego CA.
Camille P. Vaughan, Division of Geriatrics & Gerontology, Department of Medicine, Emory University and Department of Veterans Affairs Birmingham/Atlanta Geriatric Research, Education, and Clinical Center, Atlanta GA.
Oluwateniola Brown, Division of Female Pelvic Medicine and Reconstructive Surgery, Northwestern University Feinberg School of Medicine, Chicago IL..
Sonya S. Brady, Division of Epidemiology & Community Health, University of Minnesota School of Public Health, Minneapolis MN.
References
- 1.Harlow BL, Bavendam TG, Palmer MH, et al. The Prevention of Lower Urinary Tract Symptoms (PLUS) Research Consortium: A Transdisciplinary Approach Toward Promoting Bladder Health and Preventing Lower Urinary Tract Symptoms in Women Across the Life Course. J Womens Health (Larchmt). 2018;27(3):283–289. doi: 10.1089/jwh.2017.6566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lukacz ES, Bavendam TG, Berry A, et al. A Novel Research Definition of Bladder Health in Women and Girls: Implications for Research and Public Health Promotion. J Womens Health (Larchmt). 2018;27(8):974–981. doi: 10.1089/jwh.2017.6786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Montano D, Kasprzyk D. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz K, Rimer B, Viswanath K, eds. Health Behavior: Theory, Research, and Practice. 5th ed. Josey-Bass; 2015:95–124. [Google Scholar]
- 4.Skinner C, Tiro J, Champion V. The Health Belief Model. In: Glanz K, Rimer B, Viswanath K, eds. Health Behavior: Theory, Research, and Practice. Josey-Bass; 2005:79–94. [Google Scholar]
- 5.Hebert-Beirne JM, O’Conor R, Ihm JD, Parlier MK, Lavender MD, Brubaker L. A Pelvic Health Curriculum in School Settings: The Effect on Adolescent Females’ Knowledge. J Pediatr Adolesc Gynecol. 2017. Apr;30(2):188–192. doi: 10.1016/j.jpag.2015.09.006. Epub 2015 Sep 25. PMID: 26409155. [DOI] [PubMed] [Google Scholar]
- 6.Parden AM et al. (2016) Prevalence, Awareness, and Understanding of Pelvic Floor Disorders in Adolescent and Young Women Female Pelvic Med Reconstr Surg. 2016. ; 22(5): 346–354. doi: 10.1097/SPV.0000000000000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen CCG, Cox JT, Yuan C. et al. Knowledge of pelvic floor disorders in women seeking primary care: a cross-sectional study. BMC Fam Pract 20, 70 (2019). 10.1186/s12875-019-0958-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liebergall-Wischnitzer M, Cnaan T, Hochner H, Paltiel O. Self-reported prevalence of and knowledge about urinary incontinence among community-dwelling Israeli women of child-bearing age. J Wound Ostomy Continence Nurs. 2015;42(4):401–6. [DOI] [PubMed] [Google Scholar]
- 9.Smith AL, Rickey LM, Brady SS, et al. Laying the Foundation for Bladder Health Promotion in Women and Girls. Urology. 2021;150:227–233. doi: 10.1016/j.urology.2020.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brady SS, Bavendam TG, Berry A, et al. The Prevention of Lower Urinary Tract Symptoms (PLUS) in girls and women: Developing a conceptual framework for a prevention research agenda. Neurourol Urodyn. 2018;37(8):2951–2964. doi: 10.1002/nau.23787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuan H, Williams BA. Knowledge of urinary incontinence among Chinese community nurses and community-dwelling older people. Health Soc Care Community. 2010;18(1):82–90. doi: 10.1111/j.1365-2524.2009.00876.x [DOI] [PubMed] [Google Scholar]
- 12.Branch LG, Walker LA, Wetle TT, DuBeau CE, Resnick NM. Urinary Incontinence Knowledge Among Community-Dwelling People 65 Years of Age and Older. J Am Geriatr Soc. 1994;42(12):1257–1261. doi: 10.1111/j.1532-5415.1994.tb06507.x [DOI] [PubMed] [Google Scholar]
- 13.Shah AD, Massagli MP, Kohli N, Rajan SS, Braaten KP, Hoyte L. A reliable, valid instrument to assess patient knowledge about urinary incontinence and pelvic organ prolapse. Int Urogynecol J. 2008;19(9):1283–1289. doi: 10.1007/s00192-008-0631-x [DOI] [PubMed] [Google Scholar]
- 14.Zhang N, He Y, Wang J, Zhang Y, Ding J, Hua K. Effects of a new community-based reproductive health intervention on knowledge of and attitudes and behaviors toward stress urinary incontinence among young women in Shanghai: a cluster-randomized controlled trial. Int Urogynecol J. 2016;27(4):545–553. doi: 10.1007/s00192-015-2851-1 [DOI] [PubMed] [Google Scholar]
- 15.Temtanakitpaisan T, Bunyavejchevin S, Buppasiri P, Chongsomchai C. Knowledge, Attitude, and Practices (KAP) Survey Towards Pelvic Floor Muscle Training (PFMT) Among Pregnant Women. Int J Womens Health. 2020;12:295–299. doi: 10.2147/IJWH.S242432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tantisiriwat N, Manchana T. Knowledge and acceptance of Thai women toward the pelvic floor muscle training. J Med Assoc Thai. 2014;97(1):7–11. [PubMed] [Google Scholar]
- 17.Dessie SG, Adams SR, Modest AM, Hacker MR, Elkadry EA. Bladder Symptoms and Attitudes in an Ethnically Diverse Population. Female Pelvic Med Reconstr Surg. 2016;22(1):37–42. doi: 10.1097/SPV.0000000000000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Neill AT, Hockey J, O’Brien P, et al. Knowledge of pelvic floor problems: a study of third trimester, primiparous women. Int Urogynecol J. 2017;28(1):125–129. doi: 10.1007/s00192-016-3087-4 [DOI] [PubMed] [Google Scholar]
- 19.Liao Y-M, Dougherty MC, Liou Y-S, Tseng I-J. Pelvic floor muscle training effect on urinary incontinence knowledge, attitudes, and severity: an experimental study. Int J Nurs Stud. 2006;43(1):29–37. doi: 10.1016/j.ijnurstu.2005.01.004 [DOI] [PubMed] [Google Scholar]
- 20.Low LK, Williams BR, Camenga DR, et al. Prevention of Lower Urinary Tract Symptoms Research Consortium Focus Group Study of Habits, Attitudes, Realities, and Experiences of Bladder Health. J Adv Nurs. July 2019. doi: 10.1111/jan.14148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cross RM. Exploring attitudes: the case for Q methodology. Health Educ Res. 2005;20(2):206–213. doi: 10.1093/her/cyg121 [DOI] [PubMed] [Google Scholar]
- 22.Brown R. Q Methodology and Qualitative Research. Qual Health Res. 1996;6(4):561–567. doi: 10.1177/104973239600600408 [DOI] [Google Scholar]
- 23.Baker R, Blumberg S, Brick J, et al. AAPOR Report On Online Panels. Public Opin Q. 2010;74(4):711–781. [Google Scholar]
- 24.Beatty PC, Willis GB. Research Synthesis: The Practice of Cognitive Interviewing. Public Opin Q. 2007;71(2):287–311. doi: 10.1093/poq/nfm006 [DOI] [Google Scholar]
- 25.Kelder S, Hoelscher D, Perry C. How individuals, environments, and health behaviors interact: Social Cognitive Theory. In: Glanz K, Rimer B, Viswanath K, eds. Health Behavior: Theory, Research, and Practice. Jossey-Bass/Wiley; 2015:159–181. [Google Scholar]
- 26.Skinner C, Tiro J, Champion V. The Health Belief Model. In: Glanz K, Rimer B, Viswanath K, eds. Health Behavior: Theory, Research, and Practice. Josey-Bass; 2005:79–94. [Google Scholar]
- 27.Lowder JL, Bavendam TG, Berry A, et al. Terminology for bladder health research in women and girls: Prevention of Lower Urinary Tract Symptoms transdisciplinary consortium definitions. Neurourol Urodyn. 2019;38(5):1339–1352. doi: 10.1002/nau.23985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Newman DK, Burgio KL, Cain C, Hebert-Beirne J, Low LK, Palmer MH, Smith AL, Rickey L, Rudser K, Gahagan S, Harlow BL, James AS, LaCoursiere DY, Hardacker CT, Wyman JF (2021). Toileting behaviors and lower urinary tract symptoms: A cross-sectional study of diverse women in the United States. International Journal of Nursing Studies Advances 3. 100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams BR, Nodora J, Newman DK, et al. I never knew anyone who peed on themselves on purpose: Exploring adolescent and adult women’s lay language and discourse about bladder health and function. Neurourol Urodyn. 2020;39(1):225–236. doi: 10.1002/nau.24174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cross RM. Exploring attitudes: the case for Q methodology. Health Educ Res. 2005;20(2):206–213. doi: 10.1093/her/cyg121 [DOI] [PubMed] [Google Scholar]
- 31.Brown SR. Q Methodology and Qualitative Research. Qual Health Res. 1996;6(4):561–567. doi: 10.1177/104973239600600408 [DOI] [Google Scholar]
- 32.Pruneddu A. Q-SorTouch: User Manual; 2016 [Google Scholar]
- 33.Banasick S. KADE: A desktop application for Q methodology. J open source Softw. 2019;4(36):1360. doi: 10.21105/joss.01360 [DOI] [Google Scholar]
- 34.Beatty PC, Willis GB. Research Synthesis: The Practice of Cognitive Interviewing. Public Opin Q. 2007;71(2):287–311. doi: 10.1093/poq/nfm006 [DOI] [Google Scholar]
- 35.Tourangeau R, Rips LC, & Rasinski K. The psychology of survey response. Cambridge: Cambridge University Press, 2000. [Google Scholar]
- 36.Ericsson KA, Simon HA. Verbal reports as data. Psychol Rev. 1980;87:215–251 [Google Scholar]
- 37.Ryan K, Gannon-Slater N, & Culbertson MJ (2012). Improving Survey Methods With Cognitive Interviews in Small- and Medium-Scale Evaluations. American Journal of Evaluation, 33(3), 414–430. 10.1177/1098214012441499 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.