Abstract
Background
Spondylodiscitis is a potentially life-threatening infection of the intervertebral disk and adjacent vertebral bodies, with a mortality rate of 2–20%. Given the aging population, the increase in immunosuppression, and intravenous drug use in England, the incidence of spondylodiscitis is postulated to be increasing; however, the exact epidemiological trend in England remains unknown.
Objective
The Hospital Episode Statistics (HES) database contains details of all secondary care admissions across NHS hospitals in England. This study aimed to use HES data to characterise the annual activity and longitudinal change of spondylodiscitis in England.
Methods
The HES database was interrogated for all cases of spondylodiscitis between 2012 and 2019. Data for the length of stay, waiting time, age-stratified admissions, and ‘Finished Consultant Episodes’ (FCEs), which correspond to a patient's hospital care under a lead clinician, were analysed.
Results
In total, 43135 FCEs for spondylodiscitis were identified between 2012 and 2022, of which 97.1% were adults. Overall admissions for spondylodiscitis have risen from 3 per 100,000 population in 2012/13 to 4.4 per 100,000 population in 2020/21. Similarly, FCEs have increased from 5.8 to 10.3 per 100,000 population, in 2012–2013 and 2020/21 respectively. The highest increase in admissions from 2012 to 2021 was recorded for those aged 70–74 (117% increase) and aged 75-59 (133% increase), among those of working age for those aged 60–64 years (91% increase).
Conclusion
Population-adjusted admissions for spondylodiscitis in England have risen by 44% between 2012 and 2021. Healthcare policymakers and providers must acknowledge the increasing burden of spondylodiscitis and make spondylodiscitis a research priority.
Keywords: Spondylodiscitis, Pyogenic, Spine infection, Discitis, Spondylitis, Incidence
Highlights
-
•
Spondylodiscitis is a life-threatening infection of the intervertebral disk and adjacent vertebral bodies with a 2-20% mortality rate.
-
•
Admissions for spondylodiscitis in England have risen by 33% between 2012 and 2021, with the highest increase in those aged 70-74 (117%) and 75-59 (133%).
-
•
Co-morbidities like diabetes, renal failure, and immunosuppression are increasing in prevalence in England, challenging spondylodiscitis eradication.
-
•
Healthcare policymakers and providers must address predisposing factors for spondylodiscitis and improve access to diagnosis and treatment in future service provision plans.
1. Introduction
Spondylodiscitis is the most common form of spinal infection and is estimated to affect between 0.2 and 2.4 per 100.000 population per year in Western countries (Cheung and Luk, 2012; Gouliouris et al., 2010). The term refers to a primary infection of the vertebral disc by a pathogen, with secondary infection of the neighbouring vertebrae, and may involve the posterior elements of the spine and in severe cases culminate in abscess formation, epidural empyema, and bacterial sepsis (Guerado and Cerván, 2012; Hopkinson et al., 2001). Discitis refers to infection of only the intervertebral disc, and osteitis to infection of only the vertebrae. In general, there are three different types of spondylodiscitis: granulomatous (includes tuberculous, brucellar, fungal and aspergillar), parasitic, and pyogenic. In the past, and presently in developing countries, tuberculous spondylodiscitis was the most recorded form of spondylodiscitis (Cheung and Luk, 2012; Yee et al., 2010; Jensen et al., 1997). However, nowadays, pyogenic spondylodiscitis, caused most frequently by Staphylococcus aureus, is the dominant variant of spondylodiscitis in the Western world (Herren et al., 2017; Kehrer et al., 2014).
Although it is a rare pathology, it is a serious one as it can be potentially life-threatening, with a mortality ranging from 2 to 20% (Skaf et al., 2010; Zarghooni et al., 2012). The disease usually presents with non-specific symptoms, accounting for a considerable time period between the onset of symptoms and formal diagnosis, which also is a contributing factor to the high mortality rate (Gouliouris et al., 2010; Fantoni et al., 2012). Recently, increasing numbers of spondylodiscitis have been reported, likely due to a combination of the general aging of the population and the increasing number of patients with compromised immunity, such as caused by immunosuppressive drug therapy, chronic infection and, organ failure, alcohol or drug abuse, diabetes mellitus and AIDS (Cheung and Luk, 2012; Gouliouris et al., 2010; Fantoni et al., 2012; Hadjipavlou et al., 2000). It predominantly affects men with co-morbidities in the age range of 50–70 years old (Gouliouris et al., 2010; Fantoni et al., 2012; Mylona et al., 2009; GRAMMATICO et al., 2008).
Despite spondylodiscitis being a life-threatening pathology, its exact incidence in the United Kingdom has not been studied nor reported (Gouliouris et al., 2010; Skaf et al., 2010; Mylona et al., 2009; GRAMMATICO et al., 2008; Gasbarrini et al., 2005; Malawski and Lukawski, 1991; Sapico and Montgomerie, 1979; Sobottke et al., 2008; Krogsgaard et al., 1998). Knowledge of the true incidence of spondylodiscitis in the United Kingdom would help predict the future economic impact of the condition, and would accelerate awareness about this condition as well as research into therapeutic strategies to prevent it from evolving into reaching life-threatening stages (NHS Digital, 2015; Weir et al., 2019; Weir et al., 2017).
This study aimed to utilize HES data to analyse and describe the incidence of spondylodiscitis in England, including annual admissions, age-stratified incidence, finished consultant episodes, and longitudinal change.
2. Methods
In order to characterise the prevalence of spondylodiscitis, the Hospital Admitted Patient Care Activity reports from the HES (NHS Digital) database between 2012/13 and 2020/21 was analysed. The Hospital Episode Statistics (HES) database contains details of all secondary care (ie inpatient) admissions, accident and emergency attendances, and outpatient appointments across National Health Service (NHS) hospitals in England (NHS Digital, 2015). It offers large-scale big data which can be mined and analysed for trends and patterns in relevant healthcare parameters such as disease occurrence, patient characteristics, and treatment outcomes. The important role of HES data in offering valuable insights into treatment outcomes and cost-effectiveness has for example been shown by multiple studies investigating lumbar surgery (Weir et al., 2017, 2019). The HES database helps NHS care providers to plan resource allocation and planning across NHS England. NHS Digital is the national provider of data and IT technology for health and social care services in NHS England (NHS Digital, 2019). Although the HES data consists of multiple and granular data sets-detailing overall admission, accident and emergency attendance, and outpatient appointments in NHS England, only summary data, reported annually is openly accessible. This includes hospital admission activity stratified by diagnostic (ICD-10) code. Activity measures include the number of Finished Consultant Episodes (FCEs), number of admissions, number of FCEs for males and females, mean time waited for admission in days, mean length of stay in days, median length of stay in days, mean age of patients admitted in years, number of admissions for age groups 0–90+ years old were extracted. One FCE is a continuous period of admitted patient care under one consultant within one healthcare provider. Typically an admission will constitute one FCE. However, one admission can constitute multiple FCEs if there has been a transfer of responsibility within the hospital. This could occur when a different speciality assumes responsibility, and/or a patient is transferred temporarily for intervention under a different consultant (Boyd et al., 2018).
As there is no ICD-10 code specifically for spondylodiscitis, spondylodiscitis cases were identified from three ICD-10 codes: M46.4 (“unspecified discitis”), M46.3 (“Infection of intervertebral disc (pyogenic)”), M46.2 (“Osteomyelitis of vertebra”). These codes were selected due to them being most closely aligned with the definition of spondylodiscitis. To calculate the incidence, the HES data variables for each year were divided by the England population mid-year estimate for the respective year (Office for National Statistics, 2019). Data was collected and compiled by three authors (SGT, RP, HSP).
2.1. Statistical analysis
Descriptive statistics were used to summarize the data on admissions and FCEs for spondylodiscitis between 2012 and 2021. To investigate the incidence of spondylodiscitis over time, the mean number of admissions and FCEs per 100,000 population were calculated for each year between 2012 and 2021. A trend analysis was performed to determine if there was a significant increase or decrease in the incidence over time. The FCE:admissions ratio was also calculated to determine if there were changes in healthcare resource utilization. To examine the age distribution of patients with spondylodiscitis, the mean age and IQR were calculated. The number and percentage of patients in each age group were also calculated. To identify any differences in age distribution between years, the FCE rate per 100,000 population was calculated for each age group and year. To investigate any gender differences in spondylodiscitis incidence, the FCE rate per 100,000 population was calculated for male and female patients for each year between 2012 and 2021. To explore changes in waiting times and length of stay over time, the mean waiting time and length of stay were calculated for each year between 2012 and 2021. A trend analysis was performed to determine if there were significant changes over time. In order to assess for statistical significance, two-way Analysis of Variance (ANOVA) computations was run for: Years & admission-type (admissions vs FCEs), Years & Age (age groups 18–90+), Year & Sex (male vs female), Years (waiting times vs length of stay). Statistical analyses and graph syntheses were conducted using the R software (version 4.0.4). 26A p-value of less than 0.05 was considered statistically significant (p < 0.05). (R Core Team, 2022).
3. Results
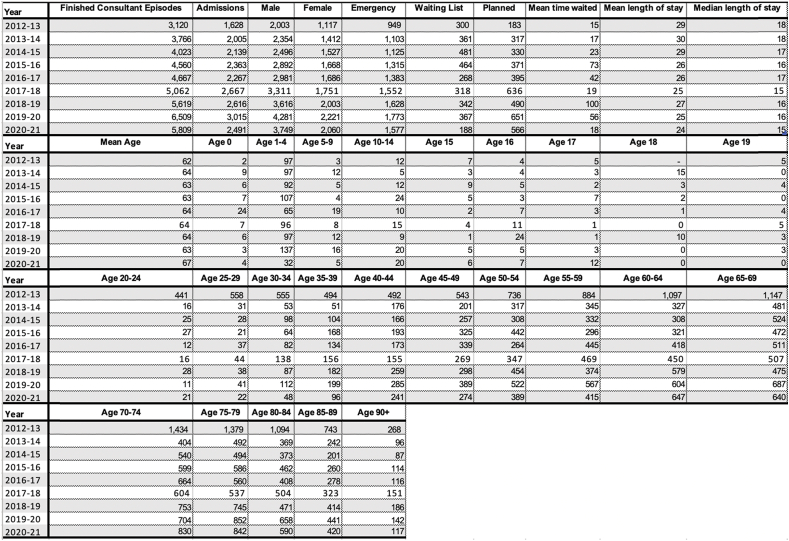
In total, the HES data analysed between 2012 and 2021 revealed 43135 FCEs and 21191 admissions for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) (Table 1).
Table 1.
A table showing the data extracted from the Health Episode Statistics (HES) for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) between 2012/13 and 2020/21. The following variables were extracted: Number of Finished Consultant Episodes (FCEs), number of admissions, number of FCEs for males and females, mean time waited for admission in days, mean length of stay in days, median length of stay in days, mean age of patients admitted in years, number of admissions for age groups 0–90+ years old. Median length of stay is only provided for ICD 46.4.
4. Incidence
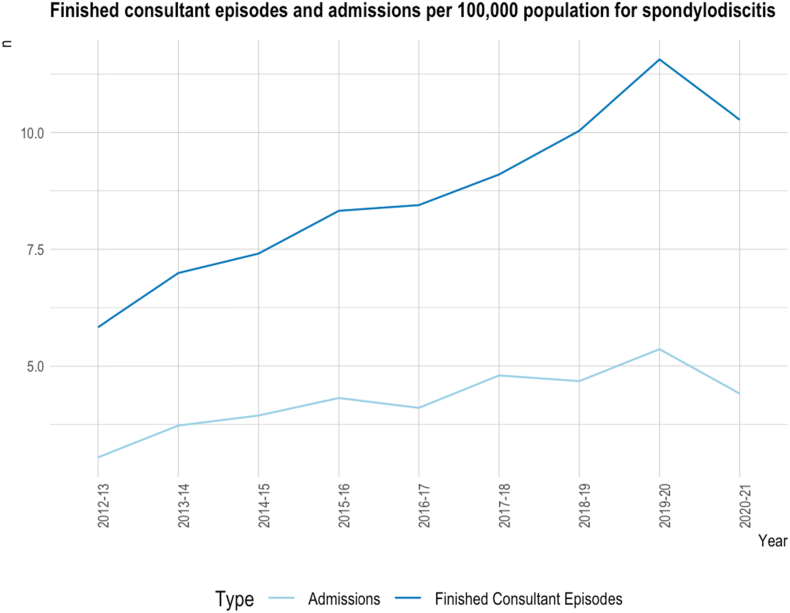
The mean number of admissions from 2012 to 2021 for spondylodiscitis was 6.5 (IQR: 4.6) per 100,000 population. Overall admissions for spondylodiscitis increased from 3.04 per 100,000 in 2012/13 to 4.40 per 100,000 population in 2020/21 (Table 1, Fig. 1), which is an approximately 44% increase. The highest number of admissions was recorded in 2019/20, namely 5.4 per 100,000 population. FCEs similarly increased from 5.8 per 100,000 population in 2012/13 to 10.3 per 100,000 population in 2020/21 (Fig. 1), which constitutes a 77% increase. The highest recording of FCEs was also in 2019/20, namely 11.6 per 100,000 population (Fig. 1). Interestingly, the FCE:admissions ratio increased from 2012/13 to 2020/21 from 1.9 to 2.3, which constitutes a 21% increase ( Table 1).
Fig. 1.
A line graph showing finished consultant episodes (FCEs) and admissions per 100,000 population for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) from 2012/13 to 2020/21. One FCE is a continuous period of admitted patient care under one consultant within one healthcare provider, and multiple FCEs may be counted for a single patient. At the bottom, a legend signified the assigned meaning of the line colours: dark blue is assigned for FCEs, and light blue for admissions. The x-axis shows the years from 2012/13 to 2020/21, and the y-axis shows the number (“n”) of admissions or FCEs, respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The ANOVA analysis showed that the epidemiological trend or difference, in terms of between FCEs and admissions, was statistically significant in terms of yearly change and difference between FCEs: admissions (p < 0.001 and p < 0.05, respectively) (Table 2).
Table 2.
A table showing the results of the Analysis of Variance (ANOVA) for age-specific, episode type (FCE & admission)-adjusted incidence for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) between 2012/13 and 2020/21, computing an ANOVA analysis for type-specific trend analysis. The following variables are shown as a result of a two-way ANOVA: Data frames (Df), sum of squares (Sum Sq), mean squares (Mean Sq), F statistic (F value), probability (Pr), and p-value (p). Significance is indicated in the significance code legend at the bottom of the table.
| Column1 |
Analysis of Variance (ANOVA): Episode type & Year |
|||||
|---|---|---|---|---|---|---|
|
Response: |
Population-adjusted spondylodiscitis incidence per 100,000 population |
|||||
| Df | Sum Sq | Mean Sq | F value | Pr (>F) | p (∗) | |
| Year | 2 | 838.94 | 419.47 | 596.2613 | 1.97E-09 | ∗∗∗ |
| Episode type | 8 | 23.59 | 2.95 | 4.1914 | 0.02929 | ∗ |
| Residuals | 128 | 1.692 | 0.01322 | |||
| Signif. codes: | ‘∗∗∗’ | 0.001 | ‘∗∗’ | 0.01 | ‘∗’ | 0.05 |
4.1. Age
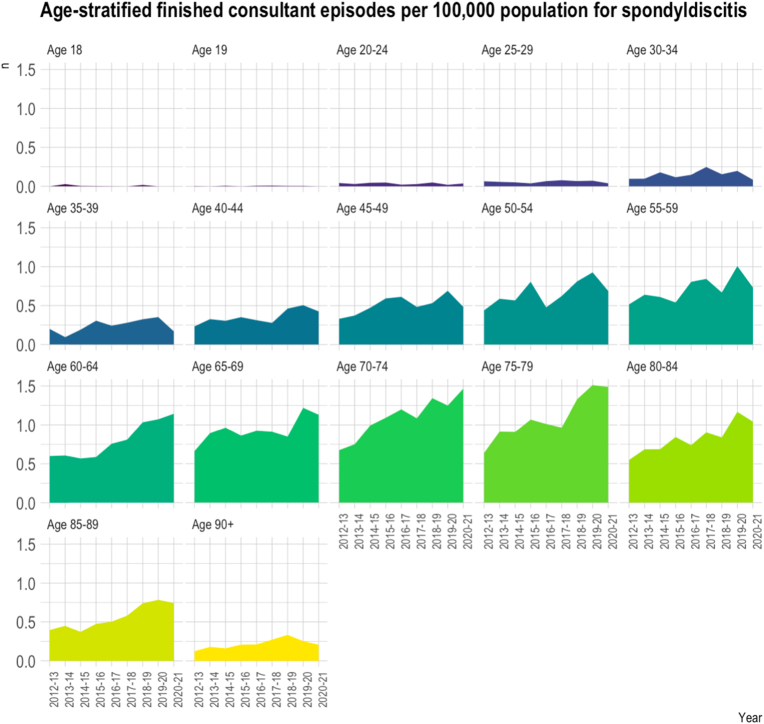
Overall, the mean age of the 43,135 FCEs for spondylodiscitis was 63.5 years (IQR: 1.1). per 100,000 population (Table 1, Fig. 2). Of all FCEs, 2.9% (n = 1248) were <18 years old; and 64.9% (n = 27,991) were aged >65 years. The remaining 25.1% (n = 15,144) were of working age, between 18 and 64 years. For patients of working age, the highest number of FCEs were recorded for those ages 60–64, with 4751 admissions between 2012 and 2021. The highest overall recorded FCEs were for those aged 70–74 years, namely 6532 FCEs (Fig. 2). The highest overall FCE rate in 2020/2021 was recorded for those aged 70–74 years (1.47 per 100,000 population) and 75–79 years (1.49 per 100,000 population), and for those between 18 and 64 years old for the age group 60–64 years (1.14 per 100,000 population) and age 65–69 years (1.13 per 100,000 population). The highest rate of increase in FCEs was for the age group 65–69 years old between the years 2018/19 and 2019/20, with an increase of 0.37 FCEs per 100,000 population, which is approximately an increase of 44%. The highest increase in FCEs from 2012/13 to 2020/21 was for those aged 75-59 years (+0.85 FCEs per 100,000 population, 133% increase), secondly age group 70–74 years (+0.79 FCEs per 100,000 population, 118% increase), among those of working age for those aged 60–64 years (+0.54 FCEs per 100,000 population, 91% increase). The ANOVA-analysis showed that the epidemiological trend or difference, in terms of between years and each age group, was statistically significant (p < 0.001 and p < 0.05, respectively) (Table 3).
Fig. 2.
An area chart showing age-stratified admissions for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) per 100,000 population from 2012/13 to 2020/21 for the following age groups: age 18, 19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65-59, 70–74, 75–79, 80–84, 85–89, 90+ years. On the x-axis is the time in years from 2012/13 to 2020/21, and on the y-axis is the number of admissions per 100,000 population for spondylodiscitis in the respective year for the respective age group. The colours are categorically chosen to represent and differentiate between the different age groups. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Table 3.
A table showing the results of the Analysis of Variance (ANOVA) for age-specific, population-adjusted incidence for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) between 2012/13 and 2020/21, computing an ANOVA analysis for age-specific trend analysis. The following variables are shown as a result of a two-way ANOVA: Data frames (Df), sum of squares (Sum Sq), mean squares (Mean Sq), F statistic (F value), probability (Pr), and p-value (p). Significance is indicated in the significance code legend at the bottom of the table.
| Column1 |
Analysis of Variance (ANOVA): Age & Year |
|||||
|---|---|---|---|---|---|---|
|
Response: |
Population-adjusted spondylodiscitis incidence per 100,000 population |
|||||
| Df | Sum Sq | Mean Sq | F value | Pr (>F) | p (∗) | |
| Year | 9 | 37.424 | 4.1582 | 314.57 | <2.20E-16 | ∗∗∗ |
| Age | 16 | 21.1825 | 1.3239 | 100.155 | <2.20E-16 | ∗∗∗ |
| Residuals | 128 | 1.692 | 0.01322 | |||
| Signif. codes: | ‘∗∗∗’ | 0.001 | ‘∗∗’ | 0.01 | ‘∗’ | 0.05 |
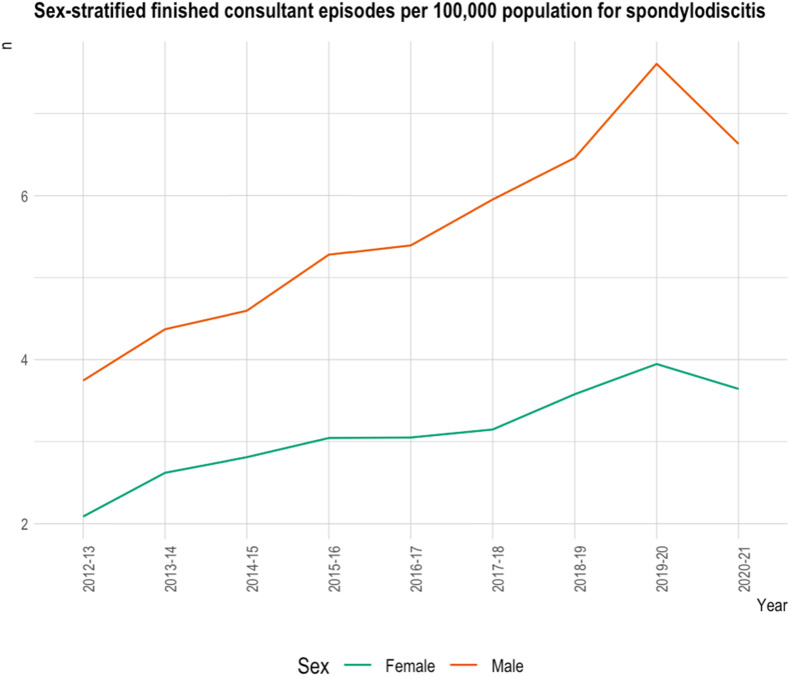
4.2. Sex
The number of FCEs per 100,000 population for male spondylodiscitis patients was higher than those for female patients every year from 2012 to 2021 (Table 1, Fig. 3). The median male number of FCEs per year for all years between 2012 and 2021 was 2981 (IQR: 1257). The median female number of FCEs per number per year was 1686 (IQR: 562). Notably, the male:female ratio for the total number of FCEs for spondylodiscitis per year has been steadily increasing since 2012, consistently year on year. The male: female ratio was 1.79 in 2012, and increased to 1.82 in 2021, indicating that the incidence gap between males and females for spondylodiscitis is slowly widening. The ANOVA-analysis showed that the epidemiological trend or difference, in terms of between years and each sex, was highly significant (p < 0.01 and p < 0.001, respectively) (Table 4).
Fig. 3.
A line chart showing sex-stratified finished consultant episodes for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) from 2012/13 to 2020/21 for males and females per 100,000 population. One FCE is a continuous period of admitted patient care under one consultant within one healthcare provider, and multiple FCEs may be counted for a single patient. At the bottom, a legend signified the assigned meaning of the line colours: green is assigned for FCEs for female patients, and orange for FCEs for male patients. The x-axis shows the years from 2012/13 to 2020/21, and the y-axis shows the number (“n”) of FCEs, respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Table 4.
A table showing the results of the Analysis of Variance (ANOVA) for sex-specific, population-adjusted incidence for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) between 2012/13 and 2020/21, computing an ANOVA analysis for sex-specific trend analysis. The following variables are shown as a result of a two-way ANOVA: Data frames (Df), sum of squares (Sum Sq), mean squares (Mean Sq), F statistic (F value), probability (Pr), and p-value (p). Significance is indicated in the significance code legend at the bottom of the table.
| Column1 |
Analysis of Variance (ANOVA): Sex & Year |
|||||
|---|---|---|---|---|---|---|
|
Response: |
Duration in days |
|||||
| Df | Sum Sq | Mean Sq | F value | Pr (>F) | p (∗) | |
| Year | 8 | 12.78 | 1.598 | 6.9338 | 6.43E-03 | ∗∗ |
| Sex | 2 | 364.79 | 182.397 | 791.5564 | 6.39E-10 | ∗∗∗ |
| Residuals | 128 | 1.692 | 0.01322 | |||
| Signif. codes: | ‘∗∗∗’ | 0.001 | ‘∗∗’ | 0.01 | ‘∗’ | 0.05 |
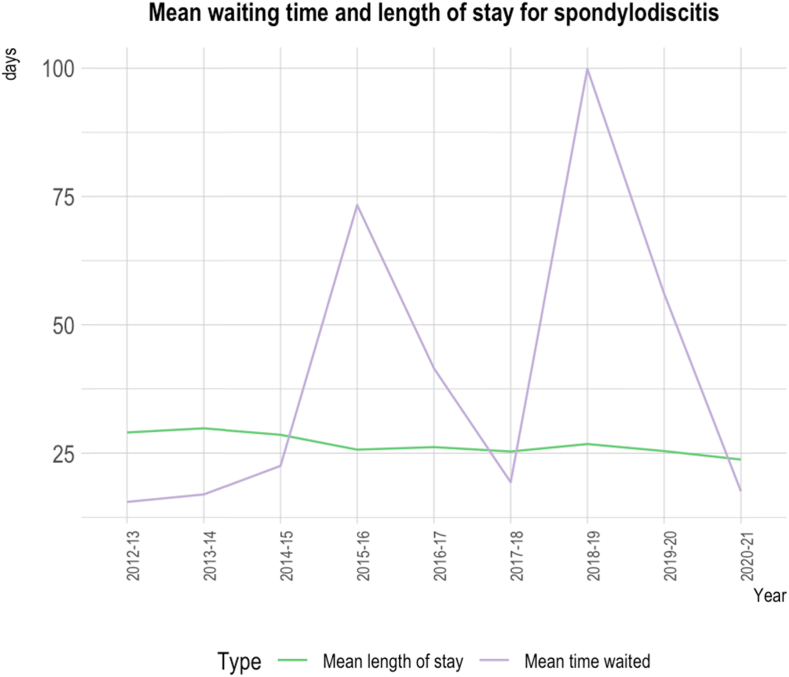
4.3. Waiting times & length of stay
Mean waiting times between primary care referral and special review have fluctuated between 2012 and 2021 (Table 1, Fig. 4). The mean waiting time was 5 days in 2012/2013 and 18 days in 2020/2021. The highest mean waiting times were recorded in 2015/2016 and 2018/2019 with 73 and 100 days, respectively (Table 1). The mean length of stay was 29 days in 2012/13 and decreased to 24 days in 2020/21 (Fig. 4). The mean length of stay reached the maximum in 2013/14 at 30 days and the minimum in 2020/21 at 24. Overall, the trend is decreasing, albeit fluctuating. The ANOVA analysis showed that the epidemiological trend or difference, in terms of between waiting times and length of stay, was highly significant (p < 0.001), however, change over years was found to be not significant (Table 5).
Fig. 4.
A line chart comparing mean waiting time for admission and length of stay during admission, both in days, for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) from 2012/13 to 2020/21. At the bottom, a legend signified the assigned meaning of the line colours: purple is assigned for mean time waited in days, and green for mean length of stay in days. The x-axis shows the years from 2012/13 to 2020/21, and the y-axis shows the days for mean length of stay and mean time waited for admission, respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Table 5.
A table showing the results of the Analysis of Variance (ANOVA) for age-specific, population-adjusted incidence for spondylodiscitis (ICD-10: M46.4 + M46.3+ M46.2) between 2012/13 and 2020/21, computing an ANOVA analysis for waiting time (WT) and length of stay (LOS)-specific trend analysis. The following variables are shown as a result of a two-way ANOVA: Data frames (Df), sum of squares (Sum Sq), mean squares (Mean Sq), F statistic (F value), probability (Pr), and p-value (p). Significance is indicated in the significance code legend at the bottom of the table.
| Column1 |
Analysis of Variance (ANOVA): Waiting time, Length of stay & Years |
|||||
|---|---|---|---|---|---|---|
|
Response: |
Duration in days |
|||||
| Df | Sum Sq | Mean Sq | F value | Pr (>F) | p (∗) | |
| Type (WT & LOS) | 2 | 838.94 | 419.47 | 596.2613 | 1.97E-09 | ∗∗∗ |
| Year | 8 | 3558.3 | 444.8 | 0.9381 | 0.534921 | |
| Residuals | 128 | 1.692 | 0.01322 | |||
| Signif. codes: | ‘∗∗∗’ | 0.001 | ‘∗∗’ | 0.01 | ‘∗’ | 0.05 |
5. Discussion
Spondylodiscitis is a rare but life-threatening infection of the spine, and the current incidence in England was unknown. Given the poor outcomes and the high mortality rate (2–20%), it is pivotal to know the approximate prevalence and the healthcare burden of spondylodiscitis, in order for healthcare providers and governance to allocate funds to improve the management and prevention of spondylodiscitis (Skaf et al., 2010; Zarghooni et al., 2012). This is the first study to utilize HES data to analyse spondylodiscitis activity within England, and we found that admissions for spondylodiscitis in England have risen by 68% between 2012 and 2021, particularly affecting those patients aged between 60 and 75 years.
Using admission activity to represent incidence in this manner has its limitations. Notably, patients discharged from emergency departments with oral antibiotics or seen via outpatient services will not have been captured. Further inter-hospital transfers will be represented as multiple admissions, as would re-admissions. Whilst this may account for the differences between previous estimates in the literature for the Western World, namely between 0.2 and 2.4 per 100,000 population per year this is a sizeable margin (Cheung and Luk, 2012; Gouliouris et al., 2010). Further it would not explain trends in admission activity or indicators of care complexity (Hopkinson et al., 2001).
FCEs are a different metric of activity. Defined as “a continuous period of admitted patient care under one consultant within one healthcare provider”, typically one hospital admission is one FCE. However within this spondylodiscitis population, FCEs were much higher than admissions, a difference that is also widening; the mean FCE:admissions ratio was found to have increased by 21% between 2012/13 to 2020/21, despite the overall length of admission remaining stable. Spondylodiscitis is typically initially diagnosed and triaged by general medical physicians. This disparity could therefore arise from demands for multidisciplinary management such as specialist input from infectious disease, spinal surgeons, geriatricians and/or intensive care. It could also reflect the requirement for repeat procedures, such as surgery or radiological guided aspiration or biopsy. This suggests spondylodiscitis cases increasingly require more interdisciplinary care, which would present a different complexity and burden to healthcare systems, than simply the number of patients encountered.
Potential explanations for this include an aging and increasingly co-morbid population in England. The number of hospital admissions in NHS England has been rising steadily for the last 10 years. In fact, admissions peaked in 2019/20, and, notably, have risen faster than the population growth: A report by NHS Digital found that the number of people between 65 and 69 years of age has increased by 34% in the last decade, however hospital admissions growing by almost 57% (NHS Digital, 2016). The age-stratified analysis employed in this study also indicated that for the sub-group of patients of working age (18–64 years old), the highest number of admissions were recorded for those aged 60–64 years, as well as having the sharpest increase in the incidence of spondylodiscitis, which is in line with the ageing of the population and the findings by NHS Digital on it. Alongside age, notably, co-morbidities such as diabetes mellitus, renal failure and immunosuppression, recognised to challenge spondylodiscitis eradication are also increasing in prevalence in England (Diabetes; Kerr, 2017). Their increased prevalence in men may also explain the gender differences in spondylodiscitis incidence.
Further trends in the data were noted, but are more difficult to contextualise within the constraints of this dataset. For example, admissions dropped between 2019/2020 and 2020/2021. This correlates with the COVID-19 pandemic. This could both be a true observation, e.g. reduced rates of infection in the context of strict public health measures, but also related to decreased hospital attendance and delayed data collection. Waiting times for primary care referral and special review for spondylodiscitis also fluctuated over the study period, with the highest waiting times recorded in 2015/16 and 2018/19. In the absence of policy change or recognised system pressures, this is most likely an aberration of data reporting.
In short, only activity data from 2012/13 to 2020/21 is available. This, therefore, does not include further patient details such as co-morbidities or treatment outcomes, and as aforementioned does not allow a patient's care to be linked across episodes. Spondylodiscitis does not have a unique ICD code and in such contexts hospital coding often differs across centres. It is also noted that during this period, efforts to improve hospital coding have occurred, for example, supported in some centres by the adoption of electronic health records. Together this may have affected case ascertainment and the identification of true trends, and does limit the identification of causality.
However, overall the data presented follows methodology utilised in other health settings to summarize activity across all hospitals across a population. Moreover, the changes in demography and indicators of increasing care complexity are justifiable. Together the authors believe this indicates addressing spondylodiscitis should be an increasing research priority.
This is highly relevant to the spinal surgery community as a topical area is the role of surgery, where some countries are advocating early surgical debridement to reduce mortality, length of treatment and disability. This contrasts current practice in England which is commonly non-operative, and would be one example of a knowledge gap that needs to be addressed (Sur et al., 2015; BASS. Management).
6. Conclusion
Our study found that population-adjusted admissions for spondylodiscitis in England have increased by 44% between 2012 and 2021, with patients aged between 60 and 75 being particularly affected. The rise in spondylodiscitis is linked to several risk factors, including diabetes, immunosuppression, intravenous drug use, and spinal surgery, all of which have increased simultaneously in incidence. The increasing FCE:admissions ratio is a notable finding, suggesting that the burden of caring for patients with spondylodiscitis is becoming more complex and resource-intensiveConservative therapy with antimicrobials is the mainstay of treatment for spondylodiscitis in the UK, but the increasing FCEs may suggest increased recurrence of spondylodiscitis. Further studies are necessary to compare outcomes of early surgical versus conservative treatment to identify the most effective treatment option. The findings have important implications for healthcare providers and governance to allocate funds to improve the management and prevention of spondylodiscitis.
Previous presentation
None.
Funding
There were no sources of funding for this study.
Declaration of competing interest
There are no conflicts of interests to be declared.
Handling Editor: Prof F Kandziora
Abbreviations
- FCE
Finished Consultant Episodes
- HES
Hospital Episode Statistics
- NHS
National Healtcare Service
References
- BASS. Management Update for pyogenic spinal infections background. https://spinesurgeons.ac.uk/resources/Documents/News/Knowledge_Update_in_the_Management_of_Spondylodiscitis_v05.pdf
- Boyd A., Cornish R., Johnson L., Simmonds S., Syddall H., Westbury L., et al. Understanding hospital episode statistics (HES) resource report. 2018. https://www.closer.ac.uk/wp-content/uploads/CLOSER-resource-understanding-hospital-episode-statistics-2018.pdf
- Cheung W.Y., Luk K.D.K. Pyogenic spondylitis. Int. Orthop. 2012;36(2):397–404. doi: 10.1007/s00264-011-1384-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diabetes U.K. Diabetes statistics. https://www.diabetes.org.uk/professionals/position-statements-reports/statistics
- Fantoni M., Trecarichi E.M., Rossi B., Mazzotta V., di Giacomo G., Nasto L.A., et al. Epidemiological and clinical features of pyogenic spondylodiscitis. Eur. Rev. Med. Pharmacol. Sci. 2012;16(Suppl. 2):2–7. https://www.ncbi.nlm.nih.gov/pubmed/22655478 [PubMed] [Google Scholar]
- Gasbarrini A.L., Bertoldi E., Mazzetti M., Fini L., Terzi S., Gonella F., et al. Clinical features, diagnostic and therapeutic approaches to haematogenous vertebral osteomyelitis. Eur. Rev. Med. Pharmacol. Sci. 2005;9(1):53–66. https://www.ncbi.nlm.nih.gov/pubmed/15852519 [PubMed] [Google Scholar]
- Gouliouris T., Aliyu S.H., Brown N.M. Spondylodiscitis: update on diagnosis and management. J. Antimicrob. Chemother. 2010;65(3) doi: 10.1093/jac/dkq303. iii11–iii24. [DOI] [PubMed] [Google Scholar]
- Grammatico L., Baron S., Rusch E., Lepage B., Surer N., Desenclos J.C., et al. Epidemiology of vertebral osteomyelitis (VO) in France: analysis of hospital-discharge data 2002–2003. Epidemiol. Infect. 2008;136(5):653–660. doi: 10.1017/S0950268807008850. 2007/06/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerado E., Cerván A.M. Surgical treatment of spondylodiscitis. An update. Int. Orthop. 2012;36(2):413–420. doi: 10.1007/s00264-011-1441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadjipavlou A.G., Mader J.T., Necessary J.T., Muffoletto A.J. Hematogenous pyogenic spinal infections and Their surgical management. Spine. 2000;25(13) doi: 10.1097/00007632-200007010-00010. https://journals.lww.com/spinejournal/Fulltext/2000/07010/Hematogenous_Pyogenic_Spinal_Infections_and_Their.10.aspx [DOI] [PubMed] [Google Scholar]
- Herren C., Jung N., Pishnamaz M., Breuninger M., Siewe J., Sobottke R. Spondylodiscitis: diagnosis and treatment options. Dtsch. Arztebl. Int. 2017;114(51–52):875–882. doi: 10.3238/arztebl.2017.0875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkinson N., Stevenson J., Benjamin S. A case ascertainment study of septic discitis: clinical, microbiological and radiological features. QJM: Int. J. Med. 2001;94(9):465–470. doi: 10.1093/qjmed/94.9.465. [DOI] [PubMed] [Google Scholar]
- Jensen A.G., Espersen F., Skinhøj P., Rosdahl V.T., Frimodt-Møller N. Increasing frequency of vertebral osteomyelitis following Staphylococcus aureus bacteraemia in Denmark 1980–1990. J. Infect. 1997;34(2):113–118. doi: 10.1016/S0163-4453(97)92395-1. [DOI] [PubMed] [Google Scholar]
- Kehrer M., Pedersen C., Jensen T.G., Lassen A.T. Increasing incidence of pyogenic spondylodiscitis: a 14-year population-based study. J. Infect. 2014;68(4):313–320. doi: 10.1016/j.jinf.2013.11.011. [DOI] [PubMed] [Google Scholar]
- Kerr M. 2017. Chronic Kidney Disease in England: the Human and Financial Cost.https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/Chronic-Kidney-Disease-in-England-The-Human-and-Financial-Cost.pdf [Google Scholar]
- Krogsgaard M.R., Wagn P., Bengtsson J. Epidemiology of acute vertebral osteomyelitis in Denmark: 137 cases in Denmark 1978–1982, compared to cases reported to the National Patient Register 1991–1993. Acta Orthop. Scand. 1998;69(5):513–517. doi: 10.3109/17453679808997789. [DOI] [PubMed] [Google Scholar]
- Malawski S.K., Lukawski S. Pyogenic infection of the spine. Clin. Orthop. Relat. Res. 1991;272(272):58–66. doi: 10.1097/00003086-199111000-00009. [DOI] [PubMed] [Google Scholar]
- Mylona E., Samarkos M., Kakalou E., Fanourgiakis P., Skoutelis A. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin. Arthritis Rheum. 2009;39(1):10–17. doi: 10.1016/j.semarthrit.2008.03.002. [DOI] [PubMed] [Google Scholar]
- NHS Digital . 2015. Hospital Episode Statistics (HES) - NHS Digital.https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics [Google Scholar]
- NHS Digital Hospital admissions hit record high as population ages. https://digital.nhs.uk/news/news-archive/2016-news-archive/hospital-admissions-hit-record-high-as-population-ages
- NHS Digital. Home - NHS Digital; 2019. https://digital.nhs.uk [Google Scholar]
- Office for National Statistics . 2019. England Population Mid-year Estimate - Office for National Statistics.https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/timeseries/enpop/pop [Google Scholar]
- R Core Team . 2022. R: A Language and Environment for Statistical Computing. [Google Scholar]
- Sapico F.L., Montgomerie J.Z. Pyogenic vertebral osteomyelitis: report of nine cases and review of the literature. Rev. Infect. Dis. 1979;1(5):754–776. doi: 10.1093/clinids/1.5.754. [DOI] [PubMed] [Google Scholar]
- Skaf G.S., Domloj N.T., Fehlings M.G., Bouclaous C.H., Sabbagh A.S., Kanafani Z.A., et al. Pyogenic spondylodiscitis: an overview. J. Infect. Pub. Health. 2010;3(1):5–16. doi: 10.1016/j.jiph.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Sobottke R., Seifert H., Fätkenheuer G., Schmidt M., Gossmann A., Eysel P. Current diagnosis and treatment of spondylodiscitis. Dtsch. Arztebl. Int. 2008;105(10):181–187. doi: 10.3238/arztebl.2008.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sur A., Tsang K., Brown M., Tzerakis N. Management of adult spontaneous spondylodiscitis and its rising incidence. Ann. R. Coll. Surg. Engl. 2015;97(6):451–455. doi: 10.1308/rcsann.2015.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir S., Samnaliev M., Kuo T.-C., Ni Choitir C., Tierney T.S., Cumming D., et al. The incidence and healthcare costs of persistent postoperative pain following lumbar spine surgery in the UK: a cohort study using the Clinical Practice Research Datalink (CPRD) and Hospital Episode Statistics (HES) BMJ Open. 2017;7(9) doi: 10.1136/bmjopen-2017-017585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir S., Kuo T.-C., Samnaliev M., Tierney T.S., Manca A., Taylor R.S., et al. Reoperation following lumbar spinal surgery: costs and outcomes in a UK population cohort study using the Clinical Practice Research Datalink (CPRD) and Hospital Episode Statistics (HES) Eur. Spine J. 2019;28(4):863–871. doi: 10.1007/s00586-018-05871-5. [DOI] [PubMed] [Google Scholar]
- Yee D.K.H., Samartzis D., Wong Y.-W., Luk K.D.K., Cheung K.M.C. Infective spondylitis in southern Chinese: a descriptive and comparative study of ninety-one cases. Spine. 2010;35(6) doi: 10.1097/BRS.0b013e3181cff4f6. https://journals.lww.com/spinejournal/Fulltext/2010/03150/Infective_Spondylitis_in_Southern_Chinese__A.7.aspx [DOI] [PubMed] [Google Scholar]
- Zarghooni K., Röllinghoff M., Sobottke R., Eysel P. Treatment of spondylodiscitis. Int. Orthop. 2012;36(2):405–411. doi: 10.1007/s00264-011-1425-1. [DOI] [PMC free article] [PubMed] [Google Scholar]