Abstract
Monteggia injuries are rare, but severe injuries of the elbow including various injury patterns. Treatment of these injuries is still topic of debate and strategies differ widely. In this systematic review on Monteggia injuries in adults, we aimed to clarify the incidence of different injury patterns within Monteggia injuries, investigate the main reasons leading to revision surgery and explore which surgical treatments should be favored to achieve satisfactory clinical results.
We initially identified 182 publications and ultimately included 17 retrospective studies comprising 651 cases. All patients were classified using the Bado classification, leading to 30.5% Bado type I fractures, 60.4% type II fractures, 5.1% type III and 3.1% type IV fractures. Mean revision rate was 23%. Ulna non-union (28%) and limited range-of-motion (22%) are the main reasons for revision surgery. Meta-analysis shows a trend toward the use of locking plates for ulna fixation which may lead to less revision surgery and fewer ulna non-unions. Further biomechanical and clinical research is necessary to clarify the role of radial head surgery.
Keywords: Monteggia injury, Elbow trauma, Olecranon fracture, Suture, Radial head fracture, Coronoid fracture, Elbow dislocation, Ulna non-union
Introduction
In 1814, Giovanni Battista Monteggia first described a Monteggia fracture as a fracture of the proximal ulna combined with a dislocation of the radial head [1]. Overall, Monteggia injuries are rare and account for only 1–5% of all fractures around the elbow [2]. Today, the eponym of Monteggia fracture, Monteggia-like-lesion or Monteggia-lesion includes multiple patterns of injury of the proximal ulna and the radial head [3]. Bado classified Monteggia fractures by defining four subtypes depending on the direction of radial head dislocation [4]. Jupiter subclassified the Bado type II fracture with regard to the location of the ulna fracture and included radial head fractures [5]. Giannicola identified six injury patterns in Monteggia lesions: (1) ulna fracture, (2) radio-humeral dislocation, (3) ulno-humeral dislocation, (4) proximal radio-ulnar dislocation, (5) radial fracture and (6) distal radio-ulnar joint lesion [3]. Today, treatment of these injuries is still a topic of debate resulting in widely different treatment strategies. Also, definition of the various injury patterns is inconsistent throughout the literature. Therefore, due to the rarity of these injuries, it is difficult to compare and evaluate different treatment strategies for these injuries.
Our goal with this systematic review was to clarify the incidence of different injuries within Monteggia injuries such as ulna fractures, coronoid fractures and radial head fractures. Furthermore, we aimed to investigate the main reasons leading to revision surgery and explore whether certain surgical treatments should be favored to achieve satisfactory clinical results.
Materials and methods
We applied the “Preffered Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) guidelines to guarantee methodical transparency. We included all studies published in English or German language since 1990 that used the Bado/Jupiter classification for Monteggia fractures and Monteggia-like-lesions. The research excluded studies without Bado classification, biomechanical studies, or anatomically studies. We also excluded review articles, case reports and studies which lack basic information such as mean follow-up or mean age of patients.
The MEDLINE database using the PubMed interface was investigated using the search terms “Monteggia fracture “OR” Monteggia-like-lesion “OR” Monteggia injury” NOT child NOT pediatric. The research was completed on 15.12.2021.
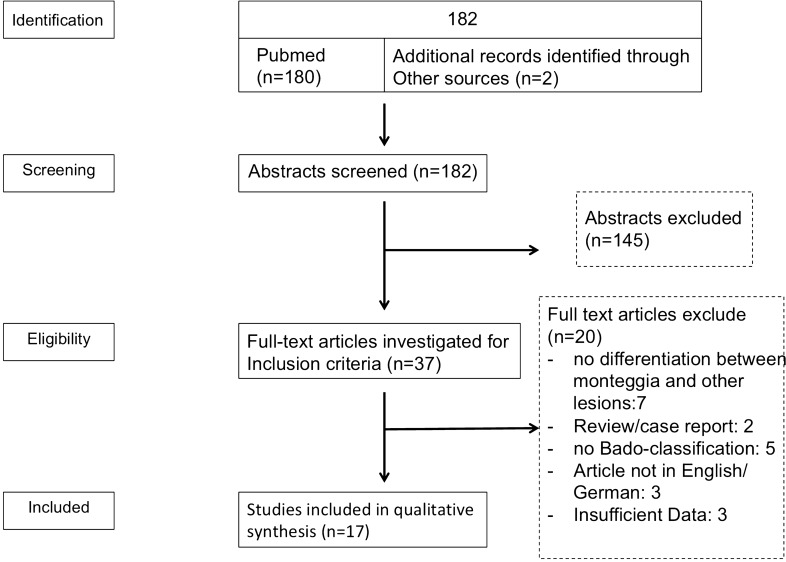
The studies identified were examined by two independent reviewers (MMW and VR). First, title and abstracts were checked for exclusion criteria. Subsequently, the full text was evaluated wether inclusion criteria were met by the study. In case of borderline decisions, a third reviewer was consulted to reach a consensus decision (MK). All borderline cases could be resolved by a consensus decision. The process of decision-making is depicted in the PRISMA-adapted flow diagram (Fig. 1).
Fig. 1.
PRISMA-adapted flowchart illustrating study selection and exclusion criteria
All data of the 17 included studies regarding number of patients, mean age, gender, mean follow-up, trauma mechanism, fracture classification (Bado/Jupiter, Mason, O’Driscoll, Regan&Morrey), range-of-motion, surgical procedures, outcome scores (Disability of the arm and shoulder (DASH); Mayo Elbow Performance Score (MEPS); Mayo Modified Wrist Score (MMWS); Broberg and Morrey), complications and revision rates were extracted and transferred into tables.
Microsoft® Excel® 2011 for Mac and GraphPad PRISM 6 (Graphpad Software, Inc) were used for data collection, data visualization and statistical analyses.
Results
We identified 182 studies in relation to our search terms. After exclusion of 145 abstracts that failed to meet the inclusion criteria, 37 full-text articles were assessed for eligibility. As demonstrated in Fig. 1, we excluded 20 articles that did not fulfill the inclusion criteria. Seventeen articles were finally included in qualitative synthesis.
Characteristics of the included publications are depicted in Table 1. In total, 651 patients with a mean age of 48.4 years were included. Gender ratio was nearly balanced with 343 male (53%) and 304 female (47%) reported patients. The mean follow-up was 52.9 months (10–234.5 months). Eleven publications reported the mechanism leading to the Monteggia injury. We identified traffic accidents (35%), low-energy falls (defined as a fall from less than 2 m; 32%) and high-energy falls (14%) as the main reasons for Monteggia injuries. In 52 cases (13%), the height of the fall was not further described. Work-related accidents (4%) and other trauma mechanisms (2%) like gun shots are rare injury causes (Table 2).
Table 1.
Overview of the publications included, depicting number of patients, mean patient age, gender and mean follow-up in months
| First author | Number of patients | Mean age | Male | Female | Mean follow-up (months) |
|---|---|---|---|---|---|
| Calderazzi et al. 2020 | 12 | 59.25 | 5 | 7 | 17.5 |
| Eden et al. 2019 | 40 | 49 | 23 | 17 | 36 |
| Egol et al. 2005 | 20 | 52.6 | 7 | 13 | 28.8 |
| Guiton et al. 2009 | 11 | 54.6 | 6 | 5 | 234.55 |
| Hamaker et al. 2017 | 119 | 37 | 77 | 42 | 10 |
| Jung et al. 2020 | 27 | 56 | 11 | 16 | 69 |
| Jungbluth et al. 2017 | 46 | 57.7 | 19 | 27 | 65.3 |
| Jupiter et al. 1991 | 13 | 56.1 | 4 | 9 | 39.6 |
| Klug et al. 2019 | 78 | 54.7 | 34 | 44 | 55.2 |
| Konrad et al. 2007 | 63 | 42.1 | 41 | 22 | 100.8 |
| Korner et al. 2004 | 49 | 38 (Median) | 31 | 18 | 83 (Median) |
| Laun et al. 2015 | 10 | 52.4 | 4 | 6 | 12.3 |
| Perez et al. 2002 | 54 | 41 | 37 | 17 | 24 |
| Ring et al. 1998 | 48 | 52 | 23 | 25 | 78 |
| Schmalzl et al. 2019 | 14 | 63 | 2 | 14 | 21,9 |
| Simpson et al. 1996 | 24 | 51 | 14 | 10 | 24 |
| Strauß et al. 2006 | 23 | 52.9 | 5 | 12 | 29 |
| 651 | 48.38 | 343 | 304 | 52.87 | |
| 53% | 47% |
Table 2.
Most common trauma causes leading to Monteggia injuries
| First author | Number of patients | High-energy fall | Low-energy fall | Traffic accident | Not specified fall | Work related | Other reasons |
|---|---|---|---|---|---|---|---|
| Egol et al. 2005 | 20 | 3 | 17 | ||||
| Jungbluth et al. 2017 | 46 | 13 | 14 | 19 | |||
| Jupiter et al. 1991 | 13 | 3 | 10 | 0 | 0 | ||
| Klug et al. 2019 | 78 | 20 | 44 | 14 | 0 | ||
| Konrad et al. 2007 | 63 | 32 | 19 | 12 | |||
| Korner et al. 2004 | 49 | 28 | 16 | 5 | |||
| Laun et al. 2015 | 10 | 3 | 3 | 4 | |||
| Perez et al. 2002 | 54 | 0 | 21 | 32 | 1 | ||
| Ring et al. 1998 | 48 | 8 | 29 | 5 | 6 | ||
| Simpson et al. 1996 | 24 | 6 | 12 | 5 | 1 | ||
| Strauß et al. 2006 | 6 | 4 | 2 | ||||
| 411 | 57.00 | 133.00 | 144.00 | 52.00 | 17.00 | 8.00 | |
| 14% | 32% | 35% | 13% | 4% | 2% |
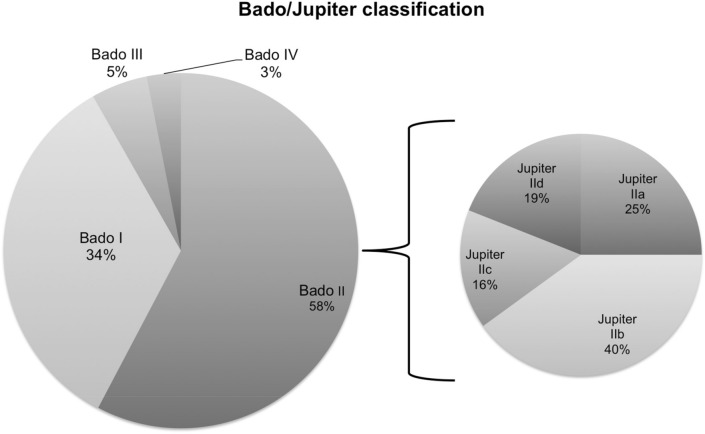
All patients were classified using the Bado classification for Monteggia fractures [4]. 31.5% were Bado type I fractures, 60.4% were Bado type II fractures. Bado type III and IV fractures are rare and represented only 5 and 3% of all Monteggia injuries, respectively. Thirteen of the 17 studies also provided information about the subclassification of Bado II fractures according to Jupiter [5]. There were 79 type IIa, 132 type IIb, 47 type IIc and 61 type IId injuries (Fig. 2).
Fig. 2.
Bado classification of 651 patients and subclassification of 370 Bado type II fractures according to Jupiter
290 radial head fractures were reported in 14 of the 17 publications. According to the Mason classification, 28% were classified as Mason type II fractures, 55% were classified as Mason type III fractures. Mason type I and IV constituted only 11 and 3% of all reported radial head fractures, respectively [6].
Seven publications additionally classified coronoid fractures. Jungbluth et al., Klug et al., Korner et al., Laun et al., Jung et al., and Strauss et al. used the Regan and Morrey classification [7–13]. Schmalzl and colleagues applied the O’Driscoll classification of coronoid process fractures [14, 15]. Altogether, there were 162 coronoid fractures reported.
There were 148 reported revisions, leading to a mean revision rate of 23% (0 to 63%). Main complications leading to additional surgery were ulna non-union (28%), limited range-of-motion, including elbow stiffness (22%), failed osteo-synthesis of ulna or radial head (13% and 11%), persistent instability (12%) and infection (9%). In 5% of the cases, revision was necessary due to other reasons that were not declared further (Table 3).
Table 3.
Causes for revision surgery in Monteggia injuries
| Number of patients | Number of revisions | Revision rate | Ulna non-union | Infection | Failed osteo-synthesis ulna | Failed osteo-synthesis radial head | Limited ROM | Instability | Other reasons | |
|---|---|---|---|---|---|---|---|---|---|---|
| Calderazzi et al. 2020 | 12 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Eden et al. 2019 | 40 | 6 | 0.15 | 1 | 0 | 2 | 2 | 0 | 0 | 1 |
| Egol et al. 2005 | 20 | 11 | 0.55 | 6 | 0 | 0 | 1 | 0 | 3 | 1 |
| Guiton et al. 2009 | 11 | 2 | 0.18 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hamaker et al. 2017 | 119 | 23 | 0.19 | 4 | 5 | 0 | 0 | 3 | 1 | 1 |
| Jung et al. 2020 | 27 | 17 | 0.63 | 0 | 0 | 0 | 5 | 5 | 0 | 0 |
| Jungbluth et al. 2017 | 46 | 6 | 0.13 | 4 | 2 | 0 | 0 | 0 | 0 | 0 |
| Jupiter et al. 1991 | 13 | 2 | 0.15 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
| Klug et al. 2019 | 78 | 23 | 0.29 | 5 | 3 | 0 | 2 | 7 | 4 | 2 |
| Konrad et al. 2007 | 63 | 10 | 0.16 | 6 | 0 | 0 | 2 | 2 | 0 | 0 |
| Korner et al. 2004 | 49 | 14 | 0.29 | 4 | 1 | 0 | 1 | 5 | 3 | 0 |
| Laun et al. 2015 | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Perez et al. 2002 | 54 | 14 | 0.26 | 4 | 1 | 0 | 0 | 4 | 4 | 0 |
| Ring et al. 1998 | 48 | 12 | 0.25 | 1 | 0 | 6 | 3 | 1 | 1 | 0 |
| Schmalzl et al. 2019 | 14 | 3 | 0.21 | 0 | 0 | 1 | 1 | 0 | 0 | 1 |
| Simpson et al. 1996 | 24 | 5 | 0.21 | 0 | 0 | 3 | 0 | 2 | 0 | 0 |
| Straus et al. 2006 | 6 | 2 | 0.33 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 634 | 148.00 | 23% | 37.00 | 12.00 | 14.00 | 17.00 | 29.00 | 16.00 | 6.00 |
| percentage | 105% | 23% | 28% | 9% | 11% | 13% | 22% | 12% | 5% |
Ulna fractures were mainly treated using locking compression plates (LCP) or dynamic compression plates (including low contact dynamic compression plates, DCP or LCDCP), but ulna reconstruction plates, 1/3 tubular plates and tension wire were also used for internal fixation. In nine cases, external fixation was applied, and in one case, the surgeon decided to use a 6.5 mm cancellous bone screw (Table 4). Seven studies nearly exclusively used LCPs (222 LCPs in 227 cases), whereas nine studies mainly used LCDCPs or DCPs for Ulna reconstruction. Egol and colleagues utilized LCDCPs in 12 patients, LCDCP/DCPs in five patients and ulna reconstruction plates in three cases.
Table 4.
Different treatment strategies and fixation devices for fixation of the Ulna in Monteggia injuries
| Number of patients | Ulna locking compression plate | Ulna LCDCP/DCP | Ulna reconstruction plate | 1/3 tubular Plate | Ulna tension wire | 6.5 mm cancellous bone screw | External fixation | |
|---|---|---|---|---|---|---|---|---|
| Calderazzi et al. 2020 | 12 | 11 | 0 | 1 | 0 | 0 | 0 | 0 |
| Eden et al. 2019 | 40 | 40 | 0 | 0 | 0 | 0 | 0 | 0 |
| Egol et al. 2005 | 20 | 12 | 5 | 3 | 0 | 0 | 0 | 0 |
| Guiton et al. 2009 | 11 | 0 | 10 | 0 | 0 | 0 | 0 | 1 |
| Hamaker et al. 2017 | 119 | 0 | 119 | 0 | 0 | 0 | 0 | 0 |
| Jung et al. 2020 | 27 | 24 | 0 | 0 | 0 | 3 | 0 | 0 |
| Jungbluth et al. 2017 | 46 | 46 | 0 | 0 | 0 | 0 | 0 | 0 |
| Jupiter et al. 1991 | 13 | 0 | 9 | 1 | 3 | 0 | 0 | 0 |
| Klug et al. 2019 | 78 | 78 | 0 | 0 | 0 | 0 | 0 | 4 |
| Konrad et al. 2007 | 63 | 0 | 52 | 0 | 0 | 11 | 0 | 0 |
| Korner et al. 2004 | 49 | 0 | 15 | 21 | 3 | 8 | 0 | 2 |
| Laun et al. 2015 | 10 | 10 | 0 | 0 | 0 | 0 | 0 | 0 |
| Perez et al. 2002 | 54 | 0 | 35 | 11 | 3 | 3 | 1 | 1 |
| Ring et al. 1998 | 48 | 0 | 37 | 2 | 0 | 3 | 0 | 0 |
| Schmalzl et al. 2019 | 14 | 13 | 0 | 0 | 0 | 1 | 0 | 0 |
| Simpson et al. 1996 | 24 | 0 | 24 | 0 | 0 | 0 | 0 | 0 |
| Strauss et al. 2006 | 6 | 0 | 3 | 3 | 0 | 0 | 0 | 1 |
| Total | 634 | 234 | 309 | 42 | 9 | 29 | 1 | 9 |
| Percentage | 100% | 37% | 49% | 7% | 1% | 5% | 0% | 1% |
There was limited information about the approach used to treat the ulna fracture and, if present, the radial head fracture. Six studies used the posterior approach to reduce and fix the ulna fracture. To address radial head fractures, Schmalzl et al. and Simpson et al. used the Boyd approach, and Calderazzi et al., Hamaker et al. and Klug et al. used a lateral approach. Eleven studies did not provide any information regarding the approach they used.
In six studies, reconstruction of the lateral collateral ligament with suture anchors was performed if necessary [7, 8, 11, 12, 14, 16]. The other 11 studies did not provide any information whether they performed ligament reconstruction.
In 14 studies, a total of 255 radial head fractures were surgically treated. Open reduction and internal fixation were applied in 117 cases. Partial resection of radial head was performed in eight patients. Ninety-one radial head prostheses were implanted and 39 patients underwent total radial head resection (Table 5).
Table 5.
Different treatment strategies and procedures addressing radial head fractures in Monteggia injuries
| ORIF | Partial resection | Prostheses | Resection | |
|---|---|---|---|---|
| Calderazzi et al. 2020 | 2 | 2 | 5 | 1 |
| Eden et al. 2019 | 19 | 0 | 1 | 1 |
| Egol et al. 2005 | 3 | 0 | 4 | 0 |
| Guiton et al. 2009 | 0 | 0 | 0 | 0 |
| Hamaker et al. 2017 | 0 | 0 | 0 | 0 |
| Jung et al. 2020 | 0 | 0 | 27 | 0 |
| Jungbluth et al. 2017 | 15 | 0 | 22 | 0 |
| Jupiter et al. 1991 | 3 | 0 | 1 | 6 |
| Klug et al. 2019 | 26 | 0 | 19 | 7 |
| Konrad et al. 2007 | 12 | 0 | 0 | 4 |
| Korner et al. 2004 | 9 | 0 | 4 | 3 |
| Laun et al. 2015 | 3 | 0 | 5 | 0 |
| Perez et al. 2002 | 10 | 0 | 0 | 3 |
| Ring et al. 1998 | 10 | 2 | 0 | 10 |
| Schmalzl et al. 2019 | ||||
| Simpson et al. 1996 | 2 | 4 | 0 | 4 |
| Strauss et al. 2006 | 3 | 0 | 3 | 0 |
| Total | 117 | 8 | 91 | 39 |
| Percentage | 46% | 3% | 36% | 15% |
All but one publication reported about the range-of-motion (ROM) for extension-flexion and pronation-supination. Korner and colleagues reported the median ROM, and the other 15 studies reported mean range-of-motion. Disability of arm, shoulder and hand (DASH) score was used to asses clinical and functional outcome in 11 publications, Mayo elbow performance score (MEPS) was used in seven and Broberg and Morrey Score (BMS) in nine studies [17]. Mayo modified wrist score (MMWS) was reported in three publications. All publications report that revision surgery was associated with a worse outcome (Table 6).
Table 6.
Overview of ROM and different outcome scores after Monteggia injuries
| Number of patients | ROM ex-flex | ROM pro-sup | MEPS | DASH | Broberg&Morrey | Mayo modified wrist score (MMWS) | |
|---|---|---|---|---|---|---|---|
| Calderazzi et al. 2020 | 12 | 106.9 | 131.7 | 84.9 | 18.8 | ||
| Eden et al. 2019 | 40 | 117 | 136 | 84.0 | 28 | ||
| Egol et al. 2005 | 20 | 95 | 105 | 64.1 | 79.1 | ||
| Guiton et al. 2009 | 11 | 120.0 | 136.4 | 94.5 | 7.6 | 94.2 | |
| Hamaker et al. 2017 | 119 | 121.36 | 138.40 | ||||
| Jung et al. 2022 | 27 | 100.00 | 131.00 | 77.0 | 30.00 | ||
| Jungbluth et al. 2017 | 46 | 125.2 | 168.5 | 90.7 | 15.1 | 86.6 | 88.4 |
| Jupiter et al. 1991 | 13 | 115.0 | 128.5 | 82.3 | |||
| Klug et al. 2019 | 78 | 114 | 155 | 88.9 | 14.7 | 88.1 | |
| Konrad et al. 2007 | 47 | 109.7 | 134.212766 | 17.4 | 87.2 | ||
| Korner et al. 2004 | 49 | 115 (Median) | 130 (Median) | ||||
| Laun et al. 2015 | 10 | 121 | 160 | 89.2 | 20.1 | 86.5 | 86.5 |
| Perez et al. 2002 | 54 | ||||||
| Ring et al. 1998 | 48 | 112 | 128 | 86 | |||
| Schmalzl et al. 2019 | 14 | 116 | 138 | 82.0 | 23.6 | 79 | |
| Simpson et al. 1996 | 24 | 109.3 | 125.4 | ||||
| Strauß et al. 2006 | 23 | 116.0 | 122.0 | 26.0 | 80.0 | ||
| Mean | 114.90 | 140.24 | 87.99 | 18.02 | 85.50 | 88,08 |
We hypothesized that surgical management of the ulna is crucial for preventing ulnar non-union and revision surgery in general. We compared seven studies mainly using locking compression plates (LCP in 222 of 227 cases) with nine studies mainly using non-locking fixation techniques. Mean revision rate of the LCP group was 0.2 (STD ± 0.08172; n = 7) compared to 0.22 (STD ± 002056; n = 9) in the non-LCP group. Mean rate of ulna non-union was 0.0257 (STD ± 0.01378; n = 7) in the LCP group and 0.09 (STD ± 0.0355; n = 9) in the non-LCP group. No significant difference with p < 0.05 was found using unpaired t test with Welch’s correction (Fig. 3).
Fig. 3.
A Comparison of mean revision rates between publications using locking compression plates (LCP) for ulna fixation (n = 7) with publications not using locking compression plates (non-LCP; n = 9) rates. B overview of revision rates in 17 publications treating Monteggia injuries. C Comparison of ulna non-union rates between publications using locking compression plates (LCP) for ulna fixation (n = 7) with publications not using locking compression plates (non-LCP; n = 9). D Overview of ulna non-union rates in 17 publications treating Monteggia injuries
Discussion
In this systematic review on Monteggia injuries, we aimed to clarify the incidence of different injury patterns within Monteggia injuries, investigate the main reasons leading to revision surgery and explore which surgical treatments should be favored to achieve satisfactory clinical results. Ulna non-union (28%) and limited range-of-motion (22%) are the main reasons for revision surgery. The use of locking compression plates for ulna fixation might help reducing those complications.
The term “Monteggia fracture” or “Monteggia-like-lesion” does not clearly define injuries which makes it difficult to compare different publications regarding these subjects. Giannicola and colleagues [18] proposed a different approach to classify and determine Monteggia injuries, but the Bado/Jupiter classification remains the most common classification systems. The epidemiology within these classifications was not well investigated. Bado based his classification on a cohort of 22 adults and 18 children leading to a statistical distribution of 25% type I, 70% injuries [4]. Evans reported a distribution of 15% type I, 80% [19]. In our meta-analysis, Bado type II injuries remain the most common type (60.5%), but with a less frequent occurrence than previously reported. According to Jupiter et al., type IIc and IId injuries only account for 8% of the Bado type II injuries. Following our research, subtype IIb and IIa are the most common subtypes, but subtype IIc and IId seem to be more common than previously expected. Our meta-analysis provides more precise data about the epidemiology and incidents of different subtypes of Monteggia injuries than previous studies.
The mean revision rate in our meta-analysis was 23%, indicating that Monteggia injuries are still difficult to treat. By analyzing reasons for revision, we could point out that ulna non-union (28%) and failed osteo-synthesis of ulna (11%) were common reasons for revision surgery. These findings suggest a lack of stability of the ulna fixation and therefore raise the question for the best treatment strategy for theses fractures. Biomechanical investigations show that fixation locking compression plates show less axial displacement than reconstruction plates and 1/3 tubular plates and therefore suggest that locking compression plates are favorable in complex ulna fractures [20]. Eden and colleagues used different types of locking compression plates including variable-angle locking double mini-plates, straight and pre-contoured plates with overall good results [21]. Comparing the LCP with the non-LCP group in our meta-analysis, we could see a lower revision rate (20% vs. 22%) and a lower rate of ulna non-unions in the LCP group (2.6% vs. 9%). Nevertheless, no significant differences could be found, presumably due to the underpowered t test. Considering the current biomechanical investigations and the favorable tendencies in our meta-analysis, we recommend using locking compression plates for the fixation of Monteggia injuries.
Complications in radial head osteo-synthesis (13%) and persistent instability (12%) are also common reasons for revision surgery in Monteggia injuries. Since postero-lateral instability of the radial head is one of the main reasons for persistent instability, the management of radial head fractures seems crucial to avoid instability and failed osteo-synthesis [9, 21, 22]. Especially, Mason III fractures raise the question whether they should be treated via ORIF, prostheses or radial head resection. Klug et al. showed that reconstruction of Mason III fractures in Monteggia injuries leads to better clinical results than resection or arthroplasty. There was no significant difference between radial head resection and radial head arthroplasty. Thus, more research is needed to clarify whether radial head arthroplasty or radial head resection leads to significant differences for the overall outcome after Monteggia injuries.
Conclusion
In conclusion, we could present new insights regarding the epidemiology of Monteggia injuries regarding the Bado/Jupiter classification, could show that revisions in Monteggia injuries are still frequent and highlight the main complications leading to revision surgery. There are hints that using locking compression plates for ulna fixation could lead to less revision surgery and prevent ulna non-union, but more research is necessary to support these tendencies. Coronoid fractures and reconstructable radial head fractures should be addressed with open reduction and internal fixation. Whether radial head arthroplasty shows significant advantages over radial head resection remains debatable.
Acknowledgements
The authors have no competing interests to declare that are relevant to the content of this article.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Declarations
Conflicts of interest
No conflicts of interest or financial funding are declared by the authors.
Compliance with ethical standards
All included articles state that procedures involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants involved in the included articles.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rehim SA, Maynard MA, Sebastin SJ, Chung KC. Monteggia fracture dislocations: a historical review. J Hand Surg. 2014;39(7):1384–1394. doi: 10.1016/j.jhsa.2014.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Josten C, Freitag S. Monteggia and monteggia-like-lesions: classification, indication, and techniques in operative treatment. Eur J Trauma Emerg Surg. 2009;35(3):296–304. doi: 10.1007/s00068-008-8028-6. [DOI] [PubMed] [Google Scholar]
- 3.Giannicola G, Sacchetti FM, Greco A, Cinotti G, Postacchini F. Management of complex elbow instability. Musculoskelet Surg. 2010;94(Suppl 1):S25–36. doi: 10.1007/s12306-010-0065-8. [DOI] [PubMed] [Google Scholar]
- 4.Bado JL. The Monteggia lesion. Clin Orthop. 1967;50:71–86. doi: 10.1097/00003086-196701000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Jupiter JB, Leibovic SJ, Ribbans W, Wilk RM. The posterior Monteggia lesion. J Orthop Trauma. 1991;5(4):395–402. doi: 10.1097/00005131-199112000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42(172):123–132. doi: 10.1002/bjs.18004217203. [DOI] [PubMed] [Google Scholar]
- 7.Jungbluth P. The challenge of Monteggia-like lesions of the elbow: mid-term results of 46 cases. Bone Jt J. 2018;100-B(2):212–218. doi: 10.1302/0301-620X.100B2.BJJ-2017-0398.R2. [DOI] [PubMed] [Google Scholar]
- 8.Klug A, Konrad F, Gramlich Y, Hoffmann R, Schmidt-Horlohé K. Surgical treatment of the radial head is critical to the outcome of Monteggia-like lesions. Bone Jt J. 2019;101-B(12):1512–1519. doi: 10.1302/0301-620X.101B12.BJJ-2019-0547.R1. [DOI] [PubMed] [Google Scholar]
- 9.Korner J. Monteggia injuries in adults: critical analysis of injury pattern, management, and results. Unfallchirurg. 2004;107(11):1026–1040. doi: 10.1007/s00113-004-0825-8. [DOI] [PubMed] [Google Scholar]
- 10.Laun R, Wild M, Brosius L, Hakimi M. Monteggia-like lesions—treatment strategies and one-year results. GMS Interdiscip Plast Reconstr Surg DGPW. 2015;4:13. doi: 10.3205/iprs000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jung M, Groetzner-Schmidt C, Porschke F, Grützner PA, Guehring T, Schnetzke M. Monteggia-like lesions in adults treated with radial head arthroplasty-mid-term follow-up of 27 cases. J Orthop Surg. 2020;15(1):5. doi: 10.1186/s13018-019-1540-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Strauss EJ, Tejwani NC, Preston CF, Egol KA. The posterior Monteggia lesion with associated ulnohumeral instability. J Bone Joint Surg Br. 2006;88(1):84–89. doi: 10.1302/0301-620X.88B1.16704. [DOI] [PubMed] [Google Scholar]
- 13.Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989;71(9):1348–1354. doi: 10.2106/00004623-198971090-00011. [DOI] [PubMed] [Google Scholar]
- 14.Schmalzl J, Sadler N, Feucht M, Gerhardt C, Lehmann LJ. Monteggia-like lesions. Obere Extrem. 2019;14(1):53–59. doi: 10.1007/s11678-018-0485-x. [DOI] [Google Scholar]
- 15.O’Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–134. [PubMed] [Google Scholar]
- 16.Calderazzi F. Monteggia-like lesions: preliminary reports and mid-term results of a single center. Acta Bio-Medica Atenei Parm. 2020;91(4):e2020134. doi: 10.23750/abm.v91i4.9864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 18.Giannicola G, Scacchi M, Sacchetti FM, Cinotti G. Clinical usefulness of proximal ulnar and radial fracture-dislocation comprehensive classification system (PURCCS): prospective study of 39 cases. J Shoulder Elbow Surg. 2013;22(12):1729–1736. doi: 10.1016/j.jse.2013.07.050. [DOI] [PubMed] [Google Scholar]
- 19.Evans EM. Pronation injuries of the forearm, with special reference to the anterior Monteggia fracture. J Bone Joint Surg Br. 1949;31B(4):578–588. doi: 10.1302/0301-620X.31B4.578. [DOI] [PubMed] [Google Scholar]
- 20.Wegmann K. Reconstruction of Monteggia-like proximal ulna fractures using different fixation devices: a biomechanical study. Injury. 2016;47(8):1636–1641. doi: 10.1016/j.injury.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 21.Eden L, Frey SP, Gilbert F, Jordan MC, Fenwick A, Meffert RH. Anatomically shaped locking plates for radial head and olecranon fracture fixation in Monteggia-like lesions. Technol Health Care. 2020;28(2):193–201. doi: 10.3233/THC-191812. [DOI] [PubMed] [Google Scholar]
- 22.Llusà Perez M, Lamas C, Martínez I, Pidemunt G, Mir X. Monteggia fractures in adults. Review of 54 cases. Chir Main. 2002;21(5):293–297. doi: 10.1016/s1297-3203(02)00126-9. [DOI] [PubMed] [Google Scholar]
- 23.Egol KA, Tejwani NC, Bazzi J, Susarla A, Koval KJ. Does a monteggia variant lesion result in a poor functional outcome?: a retrospective study. Clin Orthop. 2005;438:233–238. doi: 10.1097/01.blo.0000168806.79845.8b. [DOI] [PubMed] [Google Scholar]