Abstract
Purpose
Relative femoral neck lengthening (RNL) is a newer technique to correct coxa breva and coxa vara to relieve a femoro-acetabular impingement and improve hip abductor function without changing the position of the head on the shaft. Proximal femoral osteotomy (PFO) changes the position of the femoral head relative to the shaft. We studied the short-term complications of procedures that combined RNL with PFO.
Methods
All hips that underwent RNL and PFO using a surgical dislocation and extended retinacular flap development were included. Hips that were treated only with intra-articular femoral osteotomies (IAFO) were excluded. Hips that underwent RNL and PFO, with IAFO and/or acetabular procedures were included. Intra-operative evaluation of the femoral head blood flow was performed with the drill hole technique. Clinical evaluation and hip radiographs were obtained at 1 week, 6 weeks, 3 months, 6 months, 12 months and 24 months.
Results
Seventy two patients (31 males, 41 females, 6–52 years of age) underwent 79 combined RNL and PFO. 22 hips underwent additional procedures like head reduction osteotomy, femoral neck osteotomy, and acetabular osteotomies. There were 6 major and 5 minor complications noted. Two hips developed non-unions, both with basicervical varus-producing osteotomies. Four hips developed femoral head ischemia. Two of these hips avoided collapse with early intervention. One hip had persistent abductor weakness requiring hardware removal and three hips, all in boys developed symptomatic widening of the hip on the operated side from varus-producing osteotomy. One hip had asymptomatic trochanteric non-union.
Conclusion
RNL is routinely performed by releasing the short external rotator muscle tendon insertion from the proximal femur to raise the posterior retinacular flap. Though this technique protects the blood supply from direct injury, it seems to stretch the vessels with major corrections in the proximal femur. We recommend evaluating the blood flow intraoperatively and postoperatively and taking necessary steps early to decrease the stretch on the flap. It may be safer to avoid raising the flap for major extra-articular proximal femur corrections.
Significance
The results of this study suggest ways to improve the safety of procedures that combine RNL and PFO.
Keywords: Coxa vara, Coxa breva, Relative neck lengthening, Avascular necrosis, Nonunion, Hip widening, Proximal femur osteotomy
Introduction
Hip preservation surgery is evolving with advanced surgical procedures to optimize hip function. Relative femoral neck lengthening (RNL) is one such procedure designed to move the greater trochanter(GT) laterally and distally after removing the upper part of the neck effectively to relieve impingement of the neck and GT, and to improve abductor function in coxa breva [1, 2]. It is an alternative to valgus osteotomy for coxa vara when changing the head to acetabulum relation is not required. However, it is technically more difficult requiring surgical dislocation of the hip joint and elevation of retinacular flaps off the femoral neck [3, 4]. This adds iatrogenic risk to the femoral head blood supply and hip joint stability [5]. Complex deformities require an additional proximal femoral osteotomy (PFO) to change the orientation of the femoral head relative to the shaft. These can be done in the same setting through the same surgical approach. Sparse literature exists on the safety and complication rate of combined safe surgical dislocation (SSD) and PFO. However, in most studies PFO was combined with head-neck osteochondroplasty, which doesn’t need complete elevation of the extended retinacular flap [6–8]. We aimed to study the short-term complications of such combined procedures which included SSD, RNL and PFO.
Materials and Methods
All hips that underwent RNL and extra-articular PFO using surgical dislocation and extended retinacular flap development were studied from an IRB-approved database from 2005 to 2021. Hips that were treated by RNL and intra-articular femoral osteotomies (IAFO) without extra-articular PFO were excluded. Hips that underwent RNL and PFO with additional IAFO and/or acetabular procedures were included.
Surgical dislocation and retinacular flap development followed descriptions by Ganz et al. [3, 4]. Intra-operative evaluation of the femoral head blood flow was performed by documenting brisk bleeding through a 2 mm drill hole made in the femoral head[9]. PFO was done routinely with the opening wedge technique and fixed with a plate, Femoral head and neck osteotomies were fixed with screws or threaded pins. The greater trochanter was fixed separately with screws or tension band wires. Anterior hip precautions and weight-bearing restrictions were recommended for 4 weeks. Bone scintigraphy was obtained only for femoral neck osteotomies in the first postoperative week. Metal suppressed MRI was performed for vascular concerns that arose after a month. Weight-bearing was advanced gradually after 4 weeks based on radiographic healing of the osteotomies. Clinical evaluation and hip radiographs were obtained at 1 week, 6 weeks, 3 months, 6 months, 12 months and 24 months. Infection, avascular necrosis and non-union were considered as major complications. Limp, abductor weakness, dissatisfaction of appearance were considered as minor complications.
Results
Seventy two patients (31 males, 41 females, 6–52 years of age) underwent 79 combined RNL and PFO from 2005 to 2021. Twenty two hips underwent additional procedures like head reduction osteotomy, femoral neck osteotomy, and acetabular osteotomies. Femoral neck osteoplasty was performed routinely. Follow-up was 5 months to 60 months. All hips had at least 12 months of follow-up or a complication before 12 months. There were 6 major and 5 minor complications in 11 hips of 11 patients. All happened in the first 12 months. There were no anesthetic complications, nerve injuries, deep infections, or any other complications.
Avascular Necrosis
Four hips developed femoral head ischemia, all with PFO at or below the level of the lesser trochanter. Three of them required multiplane correction. None of the simple varus and valgus osteotomies developed vascular issues. None of the hips with additional acetabular side procedures had avascular necrosis. The first patient underwent surgical dislocation for Dunn osteotomy for a severe stable slip. After full elevation of anterior and posterior retinacular flaps, the physis was noted to be fused. The surgery was changed to femoral neck osteoplasty and flexion, valgus, internal rotation osteotomy below the lesser trochanter. Decreased bleeding after femoral head reduction into the acetabulum was ignored and blood flow was not evaluated with any postoperative imaging. The femoral head collapsed three months after surgery.
The second hip underwent an additional subtrochanteric internal rotation osteotomy under the same anesthetic after a modified Dunn osteotomy for a severe stable slip resulting in inadequate internal rotation of the hip. Brisk bleeding from the femoral head stopped after the head was reduced into the acetabulum and a postoperative bone scan did not show any uptake in the femoral head. This patient underwent a decrease in femoral internal rotation at the PFO level and that restored bleeding from the head immediately and she was doing well at the last follow-up of 49 months (Fig. 1).
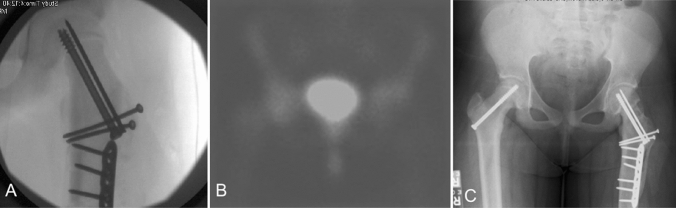
Fig. 1.
Case illustration of femoral head ischemia following RNL and PFO. A The subtrochanteric internal rotation osteotomy following modified Dunn osteotomy at the same setting to improve the internal rotation of the hip for a severe stable slip. Brisk bleeding from the femoral head stopped after the head was reduced into the acetabulum. B Postoperative bone scan did not show any uptake in the left femoral head. C This patient underwent a decrease in femoral internal rotation at the PFO level and that restored bleeding from the head immediately and she was doing well at the last follow-up of 49 months
The third hip underwent true neck lengthening (RNL plus lateral translation of intertrochanteric osteotomy) and Colonna capsular interposition arthroplasty for the absent acetabulum, recurrent dislocation, coxa breva, and coxa vara. This hip developed progressive collapse with subluxation at 9 months after the procedure with sudden onset of pain and underwent implant removal. Patient was pain-free with a functional range of motion at the last follow-up.
The fourth hip developed pain three months after varus flexion osteotomy to unload an osteochondral defect along with correction of caput valgum with lateral subluxation. MRI scan with metal suppression sequence showed avascular necrosis. This hip was treated with zoledronic acid injection into the femoral head and it remained spherical at the follow-up for 15 months.
Nonunion
Two hips developed non-unions, both with basicervical varus-producing osteotomies fixed with locking plates and without bone grafting. Both had implant failure with screw breakage. One healed with varus malunion and Trendelenburg gait, which was revised with a valgus osteotomy at 13 months from the index procedure. The other non-union was treated with repair and revision of plate fixation at 9 months from the index procedure (Fig. 2). That has healed within 5 months.
Fig. 2.
Case illustration of basicervical varus osteotomy complicated by nonunion. A Anteroposterior pelvis radiograph with left hip caput valgum, fovea alta and focal chondral lesion in the weight-bearing surface of the femoral head. B Immediate post-operative radiograph following left hip RNL and basicervical varus-producing osteotomy. Note the correction of the fovea alta and good coverage of the femoral head. C Nine months following the index procedure with implant failure and nonunion of the osteotomy site with healed trochanter. D Following revision fixation with pediatric hip plate and bone grafting
One hip had asymptomatic trochanteric non-union, treated with revision fixation and bone grafting at the time of contralateral hip optimization (Fig. 3).
Fig. 3.

One year after RNL done for poste septic sequel of the hip, showing the trochanteric nonunion with screw loosening
Abductor Weakness and Dissatisfaction with Appearance
One hip had persistent abductor weakness at six months requiring hardware removal including the stainless-steel wires used for GT fixation. Three hips, all in boys, developed symptomatic widening of the hip on the operated side from varus-producing osteotomy. None of them were treated for the deformity.
Discussion
Coxa breva was historically treated with true neck lengthening as described by Morscher or GT transfer as described by Lascombes [10, 11]. Both were described without dislocation of the hip joint and without elevation of the posterior retinacular flap. Complete correction of impingement and direct protection of the lateral retinaculum was not the focus of those procedures. RNL is a newer procedure using surgical dislocation approach and posterior retinacular flap elevation to clear impinging bone while protecting the blood supply [4]. In coxa vara, RNL can produce apparent valgus of the neck without any osteotomy between the neck and the shaft, and GT advancement improves functional neck length superiorly. It is routinely performed by releasing the short external rotator muscle tendon insertion from the proximal femur to raise the posterior retinacular flap and trim the bone from the top of the neck and the base of the GT.
Short external rotators especially the obturator externus insertion is shown to protect the femoral head blood supply from any stretch injury with surgical dislocation [12]. Isolated PFO or RNL do not cause any stretching of the flap and are at low risk of avascular necrosis as it protects all sources of blood supply to the head [13, 14]. Though the proper technique of posterior retinaculum flap elevation protects the blood supply from direct injury, it seems to allow stretching of the flap with additional osteotomies and major corrections in the proximal femur compromising the femoral head blood supply. Most times, once intraarticular optimization (osteoplasty, capital realignment, head reduction or neck osteotomy) was done, additional PFO may be needed either to improve the stability or to relieve the impingement or to move the damaged cartilage away from the weight-bearing area. Surgeons need to be aware of this potential risk with the combination of RNL and PFO. We recommend evaluation of the blood flow intraoperatively and postoperatively and taking necessary steps early to decrease the stretch on the retinacular flap. It is safer to avoid raising the posterior flap fully for major extra-articular proximal femur corrections. We observed that stretch on the retinacular flap was more significant with valgus, flexion and internal rotation osteotomy, commonly done for healed slipped capital femoral epiphysis. If the retinacular flap has been elevated and intraoperative decision needs a major derotation osteotomy, stretch on the flap can be avoided by making a more distal osteotomy or by staging the procedure. We recommend a low threshold to take post-operative bone scan to evaluate femoral head blood supply in RNL procedures involving PFO corrections in more than one plane. In patients with no uptake in the immediate post-operative bone scan, close follow-up was recommended to look for early radiographic changes and intervene with bisphosphonate injection before collapse.
Among the cohort of 48 hips in 47 patients with various pathologies (developmental dysplasia of hip, SCFE, post traumatic AVN, Perthes and FAI) that underwent SSD with PFO, Frank W. Parilla et al. reported a major complication rate of 4.2% (2 complications). Both were non-union of the intertrochanteric osteotomy which need revision fixation. Minor complications include segmental AVN in one, heterotrophic ossification in two and delayed unions in two [15]. Similarly, there were no instances of AVN among 23 slips that underwent combined safe surgical dislocation and PFO (all underwent osteochondroplasty) in a report by Baraka et al. at mean follow-up of 3.8 years. The only reported major complication was one loss of fixation and instrumentation failure at 2 post-operative weeks [8]. Among a cohort of 19 slips that underwent SSD and PFO (all underwent osteochondroplasty) at 5.1-year mean follow-up, Erickson et al. reported two major complications, one non-union of the intertrochanteric osteotomy and one instrumentation failure within two post-operative weeks that required revision surgery. There were no instances of post-operative AVN or chondrolysis and no other complications were reported [7]. The results of the above studies show that the risk of AVN was very less with combined SSD and PFO, wherein only osteochondroplasty was performed which does not require the complete elevation of the retinacular flap. Our results show a higher incidence of femoral head ischemia when PFO was performed in the setting of complete elevation of the retinacular flap for RNL.
RNL with basicervical varus osteotomies seems to be the risk factor in both non-unions. This could be from the limited contact area of the bone ends from the opening wedge technique we used without bone grafting. The stripping of the retinaculum decreases blood flow to the neck of the femur and this might have decreased the healing potential further. Increased bone contact by shaping a closing wedge at the osteotomy site, bone grafting, and compressive fixation should decrease the non-union risk.
The current study’s 7.59% major complication rate was within the 4.0–10.8% summed literature major complication rate for isolated SSD and isolated PFO [3, 4, 13, 14]. This rate was also consistent with the major complication rates reported across the few studies of combined SSD and PFO (0–10.6%) [6–8]. Although these observations support an acceptability of the complication profile associated with combined RNL and PFO, authors feel that the AVN rate was higher with this combined procedure. This devastating complication of the hip preservation surgery can be avoided or at least can be identified early to prevent the collapse of the femoral head with careful intraoperative and postoperative monitoring of the femoral head blood supply.
Varus PFO increases ipsilateral pelvic width especially when the osteotomy is performed at a distal level. RNL allows more varus correction without causing impingement and abductor dysfunction. Basicervical level was chosen to decrease this problem when the neck length was not short to begin with. Varus-producing locking plates and GT fragment fixation over the plate made the hips look even wider. Plate removal after adequate healing helps to decrease lateral prominence. We still continue to place the GT fragment over the plate because GT fixation under the plate takes away our ability to look inside the joint, limits advancement of GT, and requires the release of vastus lateralis origin from the GT fragment. GT fixation with screws is faster with less hardware prominence compared to wire fixation. We chose wire fixation only when screw fixation could not be accomplished, usually because of the lack of space for screw fixation around the plate.
Limitations
It is a single-surgeon retrospective case series of RNL and PFO. There were several different diagnoses, deformities, and procedures performed without a control group in a wide range of age group. We did not attempt to subgroup the hips and compare the complication rates. However, it is a large series of uncommon procedures with clinically important observations.
Significance
The findings of this study suggest risk factors for iatrogenic complications and ways to improve safety and satisfaction with combined RNL and PFO procedures.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Data availability
Authors declare that required data will be provided if required.
Declarations
Conflict of Interest
None declared.
Informed Consent
Written consent for publication of patient details was obtained from the patient/parent/guardian.
Ethical approval
Ethical approval was waived by the local Ethics Committee of University A in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Prasad V. Gourineni, Email: pgourineni@gmail.com
Durga prasad Valleri, Email: durga.valleri@gmail.com.
Prakash Chauhan, Email: drpcortho30@gmail.com.
Summer Watkins, Email: kidrn456@gmail.com.
References
- 1.Albers CE, Steppacher SD, Schwab JM, Tannast M, Siebenrock KA. Relative femoral neck lengthening improves pain and hip function in proximal femoral deformities with a high-riding trochanter. Clinical Orthopaedics. 2015;473(4):1378–1387. doi: 10.1007/s11999-014-4032-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson LA, Erickson JA, Severson EP, Peters CL. Sequelae of Perthes disease: treatment with surgical hip dislocation and relative femoral neck lengthening. Journal Pediatr Orthop. 2010;30(8):758–766. doi: 10.1097/BPO.0b013e3181fcbaaf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. Journal Bone Joint Surg Br. 2001;83-B(8):1119–1124. doi: 10.1302/0301-620X.83B8.0831119. [DOI] [PubMed] [Google Scholar]
- 4.Ganz R, Huff TW, Leunig M. Extended retinacular soft-tissue flap for intra-articular hip surgery: surgical technique, indications, and results of application. Instructional Course Lectures. 2009;58:241–255. [PubMed] [Google Scholar]
- 5.Leibold CS, Vuillemin N, Büchler L, Siebenrock KA, Steppacher SD. Surgical hip dislocation with relative femoral neck lengthening and retinacular soft-tissue flap for sequela of Legg–Calve–Perthes disease. Operative Orthopädie und Traumatologie. 2022;34(5):352–360. doi: 10.1007/s00064-022-00780-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rebello G, Spencer S, Millis MB, Kim YJ. Surgical dislocation in the management of pediatric and adolescent hip deformity. Clinical Orthopaedics. 2009;467(3):724–731. doi: 10.1007/s11999-008-0591-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erickson JB, Samora WP, Klingele KE. Treatment of chronic, stable slipped capital femoral epiphysis via surgical hip dislocation with combined osteochondroplasty and Imhauser osteotomy. Journal of Children's Orthopaedics. 2017;11(4):284–288. doi: 10.1302/1863-2548.11.160259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baraka MM, Hefny HM, Thakeb MF, Fayyad TA, Abdelazim H, Hefny MH, et al. Combined Imhauser osteotomy and osteochondroplasty in slipped capital femoral epiphysis through surgical hip dislocation approach. Journal of Children's Orthopaedics. 2020;14(3):190–200. doi: 10.1302/1863-2548.14.200021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gill TJ, Sledge JB, Ekkernkamp A, Ganz R. Intraoperative assessment of femoral head vascularity after femoral neck fracture. Journal Orthopaedics Trauma. 1998;12(7):474–478. doi: 10.1097/00005131-199809000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Hasler CC, Morscher EW. Femoral neck lengthening osteotomy after growth disturbance of the proximal femur. Journal Pediatric Orthopaedics Part B. 1999;8(4):271–275. [PubMed] [Google Scholar]
- 11.Lascombes P, Prevot J, Allouche A, Ligier JN, Metaizeau JP. Lengthening osteotomy of the femoral neck with transposition of the greater trochanter in acquired coxa vara. Revue de Chirurgie Orthopedique et Reparatrice de l'Appareil Moteur. 1985;71(8):599–601. [PubMed] [Google Scholar]
- 12.Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. Journal Bone Joint Surg Br. 2000;82-B(5):679–683. doi: 10.1302/0301-620X.82B5.0820679. [DOI] [PubMed] [Google Scholar]
- 13.Schai PA, Exner GU. Die intertrochantäre Korrekturosteotomie nach Imhäuser. Operative Orthopädie und Traumatologie. 2007;19(4):368–388. doi: 10.1007/s00064-007-1212-8. [DOI] [PubMed] [Google Scholar]
- 14.Kartenbender K, Cordier W, Katthagen BD. Long-term follow-up study after corrective imhäuser osteotomy for severe slipped capital femoral epiphysis. Journal of Pediatric Orthopaedics. 2000;20:749–756. doi: 10.1097/01241398-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Parilla FW, Nepple JJ, Pashos GE, Schoenecker PL, Clohisy JC. Is combined surgical dislocation and proximal femoral osteotomy a safe procedure for correction of complex hip deformities? Journal of Hip Preservation Surgery. 2022;9(2):126–133. doi: 10.1093/jhps/hnac011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Authors declare that required data will be provided if required.