Abstract
Background
Despite the variability in glenoid sizes geographically, most of the currently available commercial glenoid component designs are based on the glenoid parameters of the Caucasian population which may not be suitable for the Indian population due to a mismatch between the prosthesis and native anatomy. The aim of the present study is to systematically review the literature to determine the average glenoid anthropometric parameters in the Indian population.
Methods
A comprehensive literature search was conducted using preferred reporting items for systematic reviews and meta-analyses guidelines in the PubMed, EMBASE, Google Scholar, and Cochrane Library databases from the date of inception to May 2021. Any observational study conducted on the Indian population measuring the glenoid diameters, glenoid index, version, inclination, or any other glenoid measurements were included in the review.
Results
A total of 38 studies were included in this review. The glenoid parameters were assessed on intact cadaveric scapulae in 33 studies, on 3DCT in three studies, and 2DCT in one study. The pooled average of glenoid dimensions are as the following- the superoinferior diameter or height was 34.65 mm, anteroposterior1 diameter or maximum width was 23.72 mm, anteroposterior2 diameter or maximum width of the upper part of the glenoid was 17.05 mm, the glenoid index was 67.88, and the glenoid version was 1.75-degree retroversion. Males were having a mean height of 3.65 mm and maximum width of 2.74 mm larger than the females. A subgroup analysis revealed no significant difference between different parts of India in glenoid parameters.
Conclusion
The glenoid dimensions in the Indian population are smaller compared to the average European and American populations. The average glenoid maximum width of the Indian population is 1.3 mm smaller than the minimum glenoid baseplate size available in reverse shoulder arthroplasty. Glenoid components specific to the Indian market need to be designed to reduce glenoid failure attributable to the above findings.
Level of evidence
III.
Keywords: Glenoid, Anthropometry, Glenoid diameter, Glenoid version, India, Systematic review
Introduction
Shoulder arthroplasty is being increasingly performed to alleviate pain in patients with osteoarthritis of the shoulder and for various other indications. The placement of the glenoid component is one of the cornerstones for a successful total or reverse shoulder arthroplasty. The important factors that should be considered while approaching the glenoid are bone stock, patient-specific anatomy, and restoration of the joint line [1]. The glenoid component in both the total and reverse shoulder arthroplasty are designed based on the anthropometric parameters of the native glenoid. Even a small mismatch of component size to the native anatomy may alter the joint kinematics, and thus the outcome [2]. Anatomic parameters taken into pre-operative consideration include glenoid height, width, inclination, version, articular surface area, and size and shape of the vault. There is considerable variability in the anatomic parameters of the glenoid among different populations [2–5]. This variability may affect the prosthesis design, instrumentation, and implantation techniques [1].
Despite the variability in glenoid sizes geographically, most of the currently available commercial glenoid component designs are based on the glenoid parameters of the Caucasian population [6]. As such, these designs may not be suitable for the Indian population as there may be a mismatch between the prosthesis and native anatomy. A disproportional glenoid component has been shown to cause an early component loosening and failure [7]. There are a few studies describing the glenoid height and width in the Indian population [8–28]. It is thus important to design population and gender-specific implants based on these anthropometric studies. The aim of the present study is to systematically review the literature to determine the average glenoid anthropometric parameters in the Indian population. These data can be used to assist pre-operative planning and may help in designing glenoid components appropriate for the Indian population.
Methods
Literature Search
The search and the study were conducted according to the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines [29]. The search was performed in PubMed, EMBASE, Google Scholar, and Cochrane Library databases for articles from the date of inception to May 2021. Two authors (S.P. and L.D.) independently screened the databases for the eligible articles. The search terms included (“glenoid dimensions” OR “glenoid anthropometry” OR “glenoid CT” OR “glenoid version” OR “glenoid index” OR “glenoid inclination” OR “glenoid morphometry” OR “glenoid diameter” OR “glenoid height” OR “glenoid width” OR “shoulder anthropometry” OR “shoulder dimensions” OR “glenoid” OR “scapula” OR “scapula anthropometry”) AND (Indian OR India OR Indian population). In PubMed ‘the related-articles function’ was used to identify additional studies. All studies were reviewed by their titles, abstracts, and full texts, and the references were cross-checked for other studies eligible for inclusion. Any disagreements between the authors were assessed by another author (M.A.) and a final consensus was made.
Criteria for Selection of Articles and Data Extraction
Any observational study conducted on the Indian population measuring the glenoid diameters, glenoid index, version, inclination, or any other glenoid measurements were included in the review. Both cadaveric observational studies and radiological observational studies were included for assessment. The exclusion criteria included studies in languages other than English, letters to editors, biomechanical studies, reviews, meta-analyses, and studies with insufficient data. All records were exported to EndNote X7 (Thomson and Reuters), and duplicates were removed by the software “duplicates” tool and then checked manually.
Types of Observations
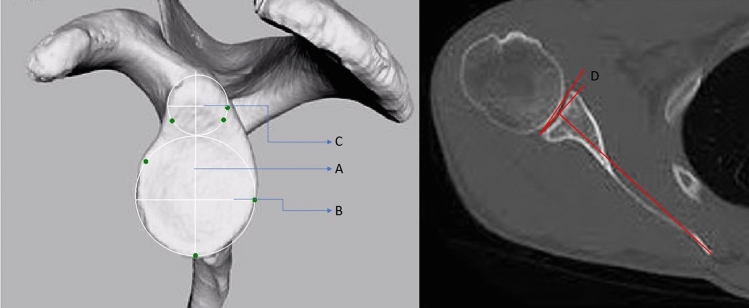
The observed parameters were glenoid supero-inferior diameter or height, anteroposterior diameters or width at any part of the glenoid, glenoid index, glenoid version, and glenoid inclination. The supero-inferior diameter (SI) was the linear measurement of the distance between the most prominent point at the supraglenoid tubercle or the most superior point to the most inferior point of the glenoid margin (Fig. 1). Anterior–posterior diameter 1(AP1) or maximum width was measured as the maximum linear breadth of the glenoid articular margin (Fig. 1). Whereas anterior–posterior diameter 2(AP2) was the maximum width of the upper part of the glenoid, which was drawn at the midpoint between the supraglenoid tubercle and the middle of glenoid cavity or mid-point of the SI diameter (Fig. 1). The glenoid index was the ratio of SI and AP1 diameter multiplied by 100. The glenoid version was mentioned as the transverse plane orientation of scapula by the cadaveric studies. The 3D-CT-based studies measured the angle in a CT slice passing through the center of the glenoid and scapular spine. The angle of version was measured between a line drawn joining the anterior and posterior rim of glenoid and another line drawn perpendicular to a line joining the medial most point of scapular spine and midpoint between anterior and posterior rim of the glenoid [8, 30] (Fig. 1). The glenoid anteversion has been demarcated by the ‘+’ sign and retroversion have been demarcated by the ‘–’ sign.
Fig. 1.
Method of measurement of glenoid height, width, and version (A Glenoid supero-inferior diameter, B Glenoid anteroposterior1 diameter, C Glenoid anteroposterior2 diameter, D: Glenoid version angle)
Two authors (S.P. and L.D.) independently collected the data. The data were extracted on author, Journal, area of study, date of publication, study design, demographics, and glenoid parameters. Any discrepancy present was resolved by another author (M.A.). The means and standard deviations for continuous variables and number (percentage) for categorical variables were noted for all morphological parameters.
Data Management, Quality Analysis, and Evidence Synthesis
Due to the availability of solely cross-sectional studies on this topic, a standard meta-analysis is not possible; hence, the methods and results of this review were written qualitatively. A narrative summary of the evidence was produced and where appropriate tables reported the study design, patient population, and observed measurements of included papers. An overall pooled comparison will be undertaken. The quality analysis was performed with the help of the Anatomical Quality Assessment (AQUA) tool for the assessment of cadaveric studies [31] and the NIH (National Institutes of Health) tool for assessing the cross-sectional studies performed on CT scans of patients [32]. The NIH tool comprises 14 criteria based on which it helps in assessing the quality of the studies. While the AQUA tool comprises five categories based on which the level of bias risk can be judged as “low risk”, “high risk”, and “moderate risk”. Any discrepancy present was resolved by another author (M.A). The studies were also divided according to the area of origin in India to assess the regional distribution of glenoid anatomy. North Indian studies were demarcated by any study conducted in Jammu and Kashmir, Himachal Pradesh, Punjab, Haryana, Uttarakhand, Uttar Pradesh, or New Delhi and National Capital Region (NCR). East Indian studies were demarcated by all studies conducted from states eastern to and including Bihar, Jharkhand, Chhattisgarh, and Odisha. Whereas West Indian studies were demarcated by any studies conducted from Madhya Pradesh, Rajasthan, Gujarat, or Maharashtra, and South Indian studies were demarcated by all studies from states southern to and including Telangana, Karnataka, and Andhra Pradesh.
Statistical Analysis
Descriptive statistics were used to summarize all collected information from the studies. The data was analysed by Kolmogorov–Smirnov test for normality. The normally distributed data were compared by ANOVA test between groups and if the data was not normally distributed Kruskal Wallis test was used for comparison between groups. Statistical analyses were performed with SPSS v23 (SPSS Inc., Chicago, IL, USA). A pooled analysis of average means across studies using the following formula was also performed for all observed parameters:
n = study population (study 1, study 2 etc.) mean = overall mean of the study population
Results
Search Results
The search strategy initially yielded 398 articles from PubMed, 12 articles from Embase, 77 articles from Cochrane Library, and 1040 articles from Google Scholar search. Among them, 36 studies were included for analysis after excluding 746 articles in total according to inclusion criteria. A detailed PRISMA flow diagram of the search is provided in Fig. 2. There were CT (computed tomography) and digital photograph-based measurements as well as cadaveric measurements mentioned in two studies by Uma et al. [27] and Raaj et al. [16]. These different methods of measurement in the same study were counted as different studies while assessing. Thus, there were 38 studies included in this systematic review.
Fig. 2.
The PRISMA flow diagram of the search
Study Characteristics
All of these studies were cross-sectional studies performed on the adult human scapula. The glenoid parameters were assessed on intact cadaveric scapulae in 33 studies, on 3DCT in three studies[8, 16, 30], on 2DCT in one study[17], and digital photographs taken from cadaveric scapulae in one study[27] (Table 1). Digital vernier calipers were used for measurements in all of the cadaveric studies. Whereas, commercially available computer programs were used for measurements in studies that used CT scan-based measurements. The study by Uma et al. used Image J software for measurements of all parameters on digital photographs [27]. Most of the cadaveric studies have performed the measurements on right or left scapulae of unknown gender. However, four studies had mentioned the gender but not the side of the scapulae [8, 17, 33, 34]. A total of 4266 scapulae were assessed by these 38 studies (Table 1).
Table 1.
Glenoid dimensions across different studies
| Author name | Type of study | Number of scapulae | Glenoid SI diameter or Height | Glenoid AP1 diameter or maximum width | Glenoid AP2 diameter or Upper half maximum width | Glenoid index | Glenoid version | Glenoid inclination |
|---|---|---|---|---|---|---|---|---|
| Akhtar et al. [57] | C | 228 | 35.80 ± 3.14 | 23.63 ± 2.50 | 16.17 ± 2.24 | 66.40 ± 8.14 | ||
| Ankushrao et al. [5] | C | 107 | 36.71 ± 4.14 | 24.85 ± 3.50 | 16.27 ± 3.24 | 65.40 ± 8.14 | ||
| Bamne et al. [20] | C | 33 R | − 3.30 ± 3.63 | |||||
| 34 L | − 1.00 ± 4.06 | |||||||
| Bodanki et al. [30] | 3D CT | 100 | 32.9 ± 3.2 | 23.4 ± 2.62 | 0.07 ± 5.38 | 6.68 ± 5.49 | ||
| Chavan et al. [58] | C | 50 | 36.83 ± 3.18 | 25.08 ± 2.53 | ||||
| Chhabra et al. [28] | C | 126 | 38.78 ± 3.03 | 24.93 ± 2.55 | 18.66 ± 2.13 | 64.29 ± 9.79 | ||
| Deepali et al. [9] | C | 67 | 34.07 ± 3.79 | 24.44 ± 2.98 |
R (− 3.30 ± 3.63) L (− 1.00 ± 4.06) |
|||
| Dhindsa et al. [59] | C | 41 R | 34.13 ± 3.16 | 24.05 ± 2.86 | 70.37 ± 4.08 | |||
| 39 L | 34.11 ± 2.57 | 23.36 ± 2.22 | 68.59 ± 4.36 | |||||
| Gupta et al. [60] | C | 60 | 34 ± 3.85 | 21.9 ± 3.05 | ||||
| Jagiasi et al. [18] | C | 20 | 35.4 ± 1.3 | 25.3 ± 2.1 | ||||
| Kalra S et al. [61] | C | 69 | 34.09 ± 3.66 | 23.96 ± 3.22 | ||||
| Kavita et al. [62] | C | 67 R | 35.2 ± 3.0 | 25.0 ± 2.7 | 16.6 | |||
| 62 L | 34.7 ± 2.8 | 24.9 ± 2.4 | ||||||
| Khalkar et al. [26] | C | 111 R | 33.20 ± 2.72 | 23.33 ± 2.04 | 16.14 ± 2.0 | |||
| 111 L | 32.73 ± 2.83 | 22.82 ± 2.3 | 15.90 ± 1.96 | |||||
| Lingamdenne et al. [35] | C | 50 | 36.85 ± 3.17 | 25.07 ± 2.55 | 11.58 ± 2.02 | |||
| Mahto et al. [56] | C | 40 R | 36.2 ± 1.7 | 24.2 ± 1.3 | ||||
| 40 L | 33.2 ± 1.8 | 22.5 ± 1.4 | ||||||
| Mamatha et al. [12] | C | 98 R | 33.67 ± 2.82 | 23.35 ± 2.04 | 16.27 ± 2.01 | |||
| 104 L | 33.92 ± 2.87 | 23.02 ± 2.3 | 15.77 ± 1.9 | |||||
| Meshram et al. [8] | 3D CT | 200 | 33.9 ± 3.1 | 24.2 ± 2.1 | 22.4 ± 2.4 | − 3.47 ± 4.7 | ||
| Pal et al. [13] | C | 100 | 33.9 ± 2.1 | 23.5 ± 2.4 | 14.0 ± 2.1 | |||
| Patel et al. [33] | C | 40 M | 34.63 ± 3.59 | 23.89 ± 2.29 | ||||
| 22 F | 31.28 ± 1.64 | 22.22 ± 2.72 | ||||||
| Patil et al. [21] | C | 104 R | 33.68 ± 4.32 | 23.29 ± 2.34 | 15.74 ± 1.75 | |||
| 120 L | 32.09 ± 4.11 | 24.90 ± 2.95 | 16.81 ± 1.74 | |||||
| Raaj et al. [16] | C | 50 R | 33.1 ± 4.1 | 21.4 ± 4.4 | 15.6 ± 3.2 | |||
| 50 L | 31.6 ± 3.4 | 20.5 ± 2.8 | 14.8 ± 1.7 | |||||
| Raaj et al. [16] | 3D CT | 50 R | 35.86 | 24.04 | 19.92 | |||
| 50 L | 30.6 | 21.52 | 15.84 | |||||
| Rajput et al. [11] | C | 43 R | 34.76 ± 3 | 23.31 ± 3 | 15.1 ± 2.54 | |||
| 57 L | 34.43 ± 3.21 | 22.92 ± 2.8 | 13.83 ± 2.45 | |||||
| SN Gosavi et al. [14] | C | 62 R | 35.03 ± 5.25 | 24.17 ± 2.57 | 14.56 ± 2.03 | |||
| 80 L | 35.3 ± 3.41 | 23.9 ± 2.66 | 14.6 ± 1.85 | |||||
| SV Uma et al. [27] | C | 100 R | 34.34 ± 3.11 | 23.91 ± 2.48 | 66.89 ± 9.7 | |||
| 100 L | 34.62 ± 3.21 | 24.59 ± 2.49 | 67.99 ± 8.03 | |||||
| SV Uma et al. [27] | S | 100 R | 35.5 ± 5.2 | 23 ± 2.2 | 66.89 ± 9.7 | − 5.985 | ||
| 100 L | 35.9 ± 7.7 | 24.1 ± 4.5 | 67.99 ± 8.03 | |||||
| Sahu et al. [17] | 2D CT | 100 | 31.3 ± 2.2 | 24.0 ± 2 | − 1.8 ± 3.8 | 78.7 ± 4.8 | ||
| Shalom PE et al. [55] | C | 100 | 35.18 ± 3.39 | 24.05 ± 2.79 | 18.31 ± 2.36 | 68.05 ± 4.87 | ||
| Shewale et al. [34] | C | 102 M | 35.95 ± 2.3 | 23.6 ± 1.5 | 17.46 ± 2.52 | |||
| 40 F | 31 ± 2.5 | 20.3 ± 2.25 | 14.8 ± 1.91 | |||||
| Singh A et al. [54] | C | 100 | 34.24 ± 3.27 | 23.93 ± 2.67 | 12.96 ± 1.84 | 70.12 ± 7.13 | ||
| Singh R et al. [23] | C | 172 | 33.6 ± 3.2 | 23.6 ± 3.1 | 15.3 ± 2.1 | |||
| Sinha et al. [10] | C | 53 | 34.12 ± 3.16 | 23.28 ± 2.99 | 18.04 ± 2.57 | |||
| Thute et al. [22] | C | 62 R | 36.09 ± 2.52 | 24.40 ± 3.67 | 16.02 ± 2.94 | |||
| 60 L | 36.4 ± 1.86 | 23.57 ± 3.41 | 16.37 ± 3.35 | |||||
| Vaishnani et al. [53] | C | 36 R | 38.49 ± 3.17 | 24.76 ± 2.49 | 18.83 ± 2.19 | |||
| 38 L | 38.06 ± 3.34 | 24.23 ± 2.14 | 17.97 ± 2.08 | |||||
| Vardhan et al. [52] | C | 60 | 36.78 ± 3.02 | 22.93 ± 2.54 | 20.62 ± 2.13 | 66.29 ± 9.79 | ||
| Varghese et al. [51] | C | 25 R | 36.92 ± 1.81 | 23.91 ± 2.91 | 16.52 ± 2.48 | |||
| 25 L | 34.92 ± 2.14 | 22.19 ± 1.52 | 16.27 ± 2.51 | |||||
| Vinay et al. [19] | C | 182 | 32.83 ± 2.9 | 24.76 ± 2.1 | ||||
| 32.46 ± 2.7 | 24.25 ± 2.4 | |||||||
| Yadav et al. [24] | C | 30 R | 33.71 ± 3.26 | 24.19 ± 2.56 | 71.76 ± 4.08 | |||
| 36 L | 33.33 ± 2.77 | 23.11 ± 2.31 | 69.34 ± 4.36 |
C Cadaveric, S Software based cadaveric measurements, 2D CT 2-Dimensional Computed Tomography, 3D CT 3-Dimensional Computed Tomography, R Right, L Left, SI Supero-inferior, AP Anteroposterior
In case of Glenoid version, “–” sign demarcates retroversion and ‘+’ sign demarcates anteversion
Quality Assessment
The quality analysis was performed with the help of the AQUA tool for the assessment of cadaveric studies [31] and most of the studies were having low risk of bias as per all of the criteria except for methodology characterization. The NIH tool was used for assessing the cross-sectional studies performed on CT scans of patients which showed equivocal results [32]. The results have been summarized in Tables 2 and 3.
Table 2.
Assessment of bias by AQUA tool
| Author name | Objective(s) and subject characteristics | Study design | Methodology characterization | Descriptive anatomy | Reporting of results |
|---|---|---|---|---|---|
| Akhtar et al. [57] | Moderate | Moderate | High | Low | Moderate |
| Ankushrao et al. [5] | Moderate | Low | High | Moderate | Low |
| Bamne et al. [20] | Low | Moderate | High | Moderate | Moderate |
| Bodanki et al. [30] | Low | Low | High | Moderate | Low |
| Chavan et al. [58] | Low | Moderate | High | Low | Low |
| Chhabra et al. [28] | Low | Low | High | Low | Low |
| Deepali et al. [9] | Moderate | Low | High | Low | Low |
| Dhindsa et al. [59] | Moderate | Low | Moderate | Low | Moderate |
| Gupta et al. [60] | Moderate | Low | High | High | Low |
| Jagiasi et al. [18] | Moderate | Low | High | Low | Low |
| Kalra et al. [61] | Low | Low | Moderate | Low | Low |
| Kavita et al. [62] | Low | Low | High | Low | Low |
| Khalkar et al. [26] | Low | Low | High | Moderate | Low |
| Lingamdenne et al. [35] | Low | Low | Moderate | Low | Low |
| Mahto et al. [56] | Moderate | Moderate | High | Low | Moderate |
| Mamatha et al. [12] | Low | Low | High | Low | Low |
| Meshram et al. [8] | Low | Low | High | Low | Low |
| Pal et al. [13] | Moderate | Low | High | Moderate | Low |
| Patel et al. [33] | High | Low | High | Low | Low |
| Patil et al. [21] | Low | Low | Moderate | Low | Low |
| Raaj et al. Cadaveric [16] | Moderate | Moderate | High | Low | Low |
| Raaj et al. CT [16] | Moderate | Moderate | High | Low | Low |
| Rajput et al. [11] | Moderate | Low | Moderate | Low | Low |
| SN gosavi et al. [14] | Low | Low | Moderate | Low | Low |
| SV uma et al. cadaveric [27] | Low | Low | High | Low | Low |
| SV uma et al. Image J software [27] | Low | Low | High | Low | Low |
| Sahu et al. [17] | Moderate | Low | Moderate | Moderate | Low |
| Shalom et al. [55] | Low | Low | High | Low | Low |
| Shewale et al. [34] | Moderate | Low | High | Moderate | Low |
| Singh et al. [54] | Moderate | Low | High | Low | Low |
| Singh et al. [23] | Moderate | Low | High | Low | Low |
| Sinha et al. [10] | Moderate | Low | Moderate | Low | Low |
| Thute et al. [22] | Low | Low | High | Moderate | Low |
| Vaishnani et al. [53] | Moderate | Low | High | Low | Low |
| Vardhan et al. [52] | Moderate | Low | High | Moderate | Moderate |
| Varghese et al. [51] | Moderate | Moderate | High | Low | Low |
| Vinay et al. [19] | Low | Low | High | Moderate | low |
| Yadav et al. [24] | High | Moderate | High | Low | Low |
Table 3.
NIH quality assessment tool for assessing the cross-sectional studies
| Author name | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bodanki et al. [30] | No | Yes | NA | No | No | NA | NA | NA | NA | NA | Yes | NA | NA | NA |
| Meshram et al. [8] | Yes | Yes | NA | No | Yes | NA | NA | NA | NA | NA | Yes | NA | NA | NA |
| Raaj et al. [16] | Yes | Yes | NA | Yes | No | NA | NA | NA | NA | NA | Yes | NA | NA | NA |
| Sahu et al. [17] | Yes | Yes | NA | Yes | No | NA | NA | NA | NA | NA | Yes | NA | NA | NA |
NA Not Applicable
Numbers in the top row are representative of the 14 criteria of NIH assessment tool as described below:
1. Was the research question or objective in this paper clearly stated?
2. Was the study population clearly specified and defined?
3. Was the participation rate of eligible persons at least 50%?
4. Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants?
5. Was a sample size justification, power description, or variance and effect estimates provided?
6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured?
7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed?
8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome
9. Were the exposure measures clearly defined, valid, reliable, and implemented consistently across all study participants?
10. Was the exposure(s) assessed more than once over time?
11. Were the outcome measures clearly defined, valid, reliable, and implemented consistently across all study participants?
12. Were the outcome assessors blinded to the exposure status of participants?
13. Was loss to follow-up after baseline 20% or less?
14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?
Outcome Analysis
Glenoid Dimensions
All of the glenoid morphometric parameters were found to be not normally distributed. So non-parametric tests were used for analysis. Glenoid supero-inferior diameter and AP1 diameter were mentioned by all 38 studies except one (Table 1). However, only 22 studies had mentioned AP2 diameter. The pooled average glenoid supero-inferior diameter was 34.65 mm (95% CI 34.13–35.18) (Table 4). The pooled average glenoid AP1 diameter was 23.72 mm (95% CI 23.41–24.03) (Table 4). Whereas the pooled average glenoid AP2 diameter was 17.05 mm (95% CI 15.82–18.28) (Table 5). The glenoid index was mentioned by 7 studies and the pooled average was 67.88 (95% CI 65.73–10.02). The glenoid version was mentioned in 5 studies and the pooled average was -1.75 degrees (95% CI − 5.79 to 2.28). The glenoid inclination was measured in only two studies. It was measured as an angle between the glenoid surface line (line joining superior and inferior rim) and a line drawn along the floor of the supraspinatus fossa in the study by Sahu et al. [17]. However, the glenoid inclination was defined as the angle between a line drawn perpendicular to the glenoid surface line (line joining superior and inferior rim) and another line perpendicular to the tangent along medial border of scapula by Lingamdenne et al. [35]. The mean glenoid inclination was mentioned to be 78.7 ± 4.8 degrees (Range: 70.7–95.9) in the study by Sahu et al. [17]. However, it was measured as 11.58 ± 2.02 (Range: 9–18) in the study by Lingamdenne et al. [35]. None of the other studies had measured glenoid inclination.
Table 4.
Morphometric values of glenoid cavity across studies
| Parameters | Pooled average | Median | 95% confidence interval | Range |
|---|---|---|---|---|
| Glenoid SI diameter (mm) | 34.65 | 34.16 | 34.13–35.18 | 32.64–38.78 |
| Glenoid AP1 diameter (mm) | 23.72 | 23.65 | 23.41–24.03 | 20.95–25.3 |
| Glenoid AP2 diameter (mm) | 17.05 | 16.22 | 15.82–18.28 | 12.9–24.9 |
| Glenoid index | 67.88 | 68.05 | 65.73–70.02 | 64.3–70.55 |
| Glenoid version (degrees) | − 1.75 | − 2.13 | (− 5.79)–(2.08) | (− 5.98)–(2.15) |
SI Supero-inferior, AP Anteroposterior
In case of Glenoid version, “–” sign demarcates retroversion and ‘ + ’ sign demarcates anteversion
Table 5.
Distribution of glenoid morphometric parameters across different regions of India
| Parameters | Eastern India | Western India | Northern India | Southern India | P value | |
|---|---|---|---|---|---|---|
| Glenoid SI diameter (mm) | Pooled average | 35.11 | 35.05 | 34.61 | 34.24 | 0.48 |
| Median | 34.7 | 34.87 | 34.09 | 34.13 | ||
| Range | 33.9–36.78 | 32.96–38.27 | 33.52–38.78 | 32.64–36.85 | ||
| Glenoid AP1 diameter (mm) | Pooled average | 23.33 | 23.98 | 23.8 | 23.65 | 0.43 |
| Median | 23.35 | 24.1 | 23.7 | 23.8 | ||
| Range | 22.93–23.63 | 22.45–25.3 | 21.9–24.93 | 20.95–25.07 | ||
| Glenoid AP2 diameter (mm) | Pooled average | 17.21 | 16.8 | 15.64 | 17.85 | 0.73 |
| Median | 17.1 | 16.16 | 15.3 | 16.39 | ||
| Range | 14.01–20.62 | 14.46–22.4 | 12.96–18.66 | 15.2–24.9 | ||
| Glenoid index | Pooled average | 65.66 | 70.05 | 68.05 | 0.07 | |
| Median | 65.29 | 70.12 | 68.05 | |||
| Range | 64.3–66.4 | 69.48–70.55 | 68.05 | |||
| Glenoid version (degrees) | Pooled average | − 1.1 | − 2.64 | 0.56 | ||
| Median | − 2.15 | − 2.64 | ||||
| Range | − 3.5 to 2.15 | − 5.98 to 0.7 |
SI Supero-inferior, AP Anteroposterior
In case of Glenoid version, “–” sign demarcates retroversion and ‘ + ’ sign demarcates anteversion
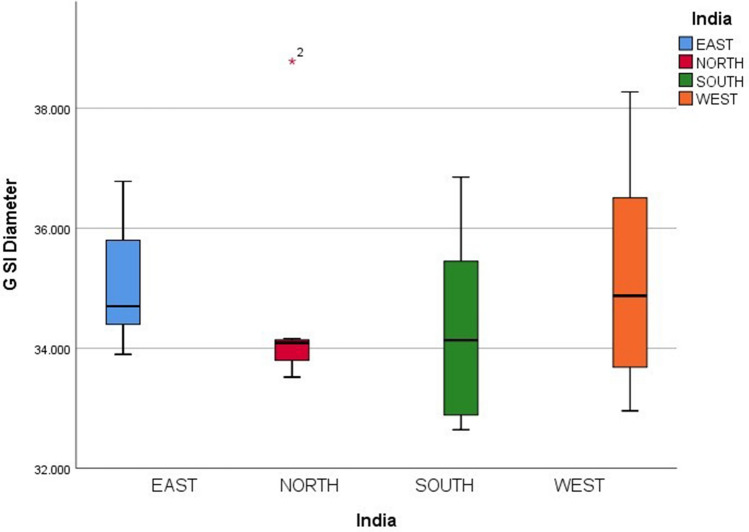
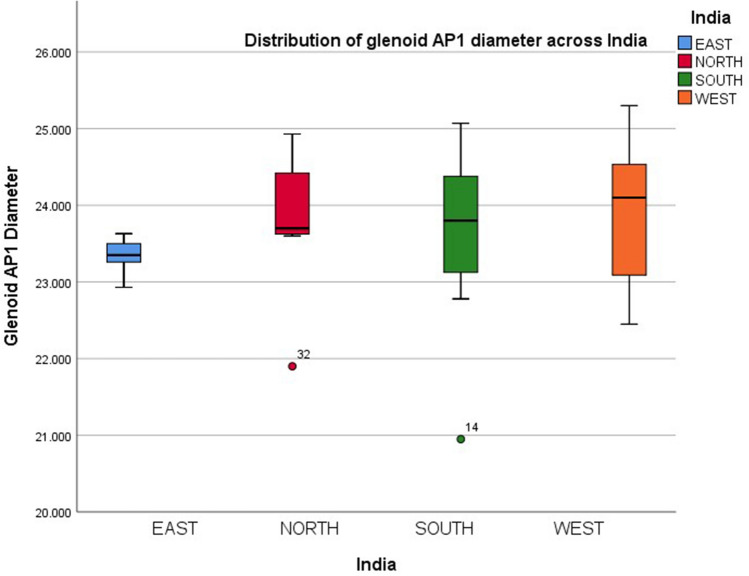
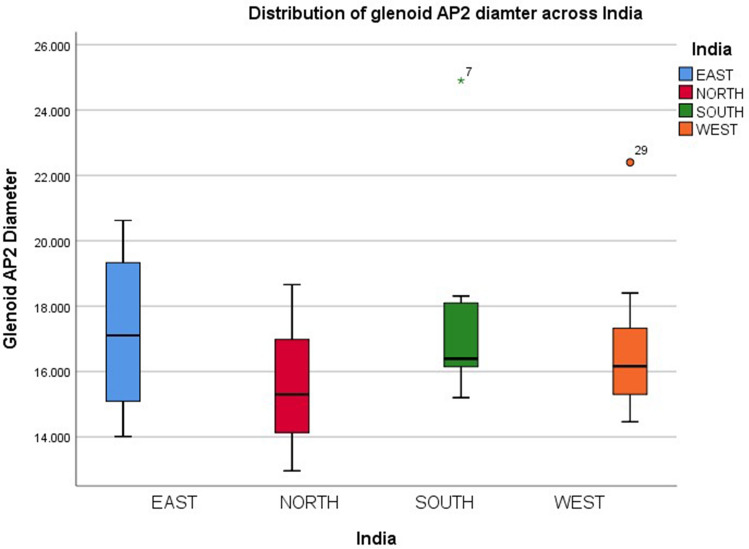
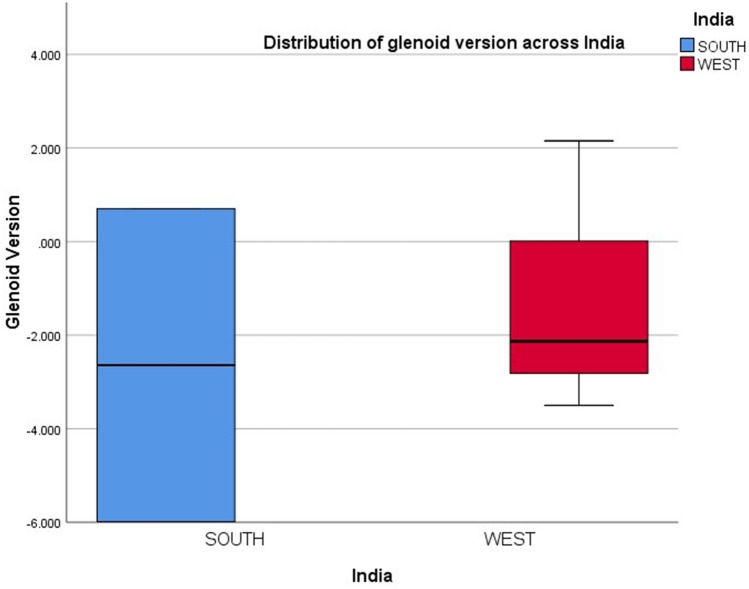
Geographical Variation of Glenoid Parameters Across India
The studies included in this systematic review originated from all over India. A total of 5 studies were from East India, 13 from West India, 7 from North India, and 12 from South India. There was one study by Sahu et al. [17]. which included 39 patients from Central and North India, 10 patients from South India, and one patient from West Bengal. Thus, this study was not taken into account while performing a subgroup analysis of glenoid parameters of different parts of India. The analysis reveals no significant difference between different parts of India in glenoid parameters. Western India had the highest median SI diameter (34.87 mm) and median AP1 diameter (24.1 mm). Whereas northern India had the lowest median SI diameter (34.09 mm) and eastern India had the lowest median AP1 diameter (23.35 mm). Northern India had the lowest median AP2 diameter (15.3 mm) but the highest median glenoid Index (70.12). The glenoid index was not mentioned in any western Indian study and the Glenoid version was not mentioned in any of the eastern or northern Indian studies. The distribution of glenoid parameters across India has been summarized in Table 5 and Figs. 3, 4, 5, and 6.
Fig. 3.
Distribution of glenoid superoinferior diameter across India
Fig. 4.
Distribution of glenoid anteroposterior1 diameter across India
Fig. 5.
Distribution of glenoid anteroposterior2 diameter across India
Fig. 6.
Distribution of glenoid version diameter across India
Gender Variation of Glenoid Parameters
There were only four studies that measured the glenoid parameters of known gender and compared them. Among these 2 studies were cadaveric [33, 34] and 2 studies were CT based [8, 17]. These studies assessed a total of 200 male and 174 female scapulae. The median SI and AP1 diameters were higher in males compared to females (Table 6). The difference in glenoid SI and AP1 diameter between males and females was statistically significant (p: 0.029), with males having a mean SI diameter 3.65 mm and AP1 diameter 2.74 mm larger than the females.
Table 6.
Distribution of glenoid morphometric parameters across genders
| Parameters | Male | Female | P value | |
|---|---|---|---|---|
| Glenoid SI diameter (mm) | Pooled average | 34.62 | 30.97 | 0.029 |
| Median | 35.29 | 31.14 | ||
| Range | 31.8–36.1 | 29.9–31.7 | ||
| Glenoid AP1 diameter (mm) | Pooled average | 24.22 | 21.48 | 0.029 |
| Median | 24.2 | 21.5 | ||
| Range | 23.89–24.6 | 20.3–22.5 |
SI Supero-inferior, AP Anteroposterior
Discussion
With the increasing numbers of shoulder arthroplasty across India, an idea about population-specific glenoid dimensions is paramount for pre-operative planning and glenoid component designs specific to our market should be available in the armamentarium. Accordingly, the single most important finding of this systematic review is the maximum glenoid width (AP1 diameter) is smaller compared to the available baseplate dimensions at present. The average AP1 diameter (maximum width) was 23.72 mm with the lowest mean maximum width of 20.95 mm in a study by Raaj et al. [16]. Whereas the commonly used baseplate sizes in reverse shoulder arthroplasty (RSA) are between 27 and 29 mm and 27 mm is the smallest size available for the Delta Xtend system (DePuy Synthes), 25 mm for the Comprehensive reverse shoulder system (Zimmer, USA), 24 mm for Univers revers (Arthrex) and 26 mm for Unic Reverse (Evolutis) [36].
The fixation of the baseplate is one of the cornerstones for success in RSA. The oversized base plate has been shown to cause difficulty in putting the screws, scapula fracture, and suboptimal fixation [36]. Thus, it is of utmost importance that the correct size of baseplate should be chosen. However, there have been multiple studies showing variations between glenoid dimensions according to ethnicity. Coskun et al. had shown the mean SI diameter and AP1 diameter of the Turkish population to be 36.3 mm and 24.6 mm [37]. Churchill et al. performed an anthropometric study on 172 scapulae belonging to the population of the United states of America to note a mean SI diameter of 37.5 mm in males and 32.6 mm in females [38]. The AP1 diameter in the same population was noted to be 27.8 mm in males and 23.6 mm in females. A cadaveric study performed on the Egyptian population showed the mean SI diameter and AP1 diameter to be 33.1 mm (right side), 28.7 mm (left side) and 23.35 mm (right side), 23.02 mm (left side) respectively [39]. Similarly, another study performed on the Nigerian population revealed the mean SI diameter to be 37.71 mm on the right side and 36.22 mm on the left side [40]. Whereas they noted a mean AP1 diameter to be 26.2 mm on the right side and 24.35 mm on the left side. In the Chinese population the mean SI diameter and mean AP1 diameter were shown to be 34.5 mm and 25.1 mm respectively by Wang et al. [41]. Mizuno et al. compared the glenoid dimensions between100 Japanese and 100 French shoulders in 3DCT to note a mean SI diameter of 33.3 mm, mean glenoid AP1 diameter of 25.5 mm in the Japanese population and mean SI diameter of 35.4 mm, mean glenoid AP1 diameter of 26.7 mm in French population [42]. This systematic review highlighted an Indian glenoid to have an average SI diameter of 34.65 mm and an average AP1 diameter of 23.72 mm. Thus, we can note high variations in glenoid dimensions between Caucasian and Asian populations which necessitates the use of a suitable glenoid baseplate in the Asian population [3, 5, 7, 14, 28, 34, 39–41, 43–62] (Table 7).
Table 7.
Distribution of glenoid morphometric parameters across world
| Studies | Region of origin | Method of measurement | No of shoulders studied | Mean glenoid SI diameter or Height | Mean glenoid AP1 diameter or Maximum width | Glenoid version | Glenoid inclination (+ up) |
|---|---|---|---|---|---|---|---|
| Coskun et al. [37] | Turkey | C | 90 | 36.3 | 24.6 | ||
| Rosales-Rosales et al. [43] | Spain | CT | 154 | 28.78 | 20.27 | ||
| Mathews et al.[7] | Switzerland | CT | 18 | 36.6 | 27.8 | − 1 | + 13 |
| Polguj et al. [44] | Poland | C | 86 | 38.32 | 27.67 | ||
| Mizuno et al.[42] | French | CT | 100 | 35.4 | 26.7 | − 2.3 | + 11.6 |
| Japanese | CT | 100 | 33.3 | 25.5 | − 6 | + 10.4 | |
| Churchill et al. [6] | USA | C | 344 | 35.1 | 25.7 | − 1.2 | |
| Piponov et al. [3] | USA | CT | 108 | 31.7 | 24.7 | 0.5 | |
| Iannotti et al. [45] | USA | C & MRI | 140 | 39 | 29 | ||
| Lombardo et al. [46] | USA | CT | 39 | 34.9 | 25.7 | ||
| Australia | 37 | 34.6 | 24.7 | ||||
| Cabezas et al.[47] | USA | CT | 92 | 35.8 | |||
| Korea | 58 | 33.4 | |||||
| Aigbogun et al. [40] | Nigeria | C | 200 | 36.9 | 25.3 | ||
| Ei-din et al. [48] | Egypt | C | 160 | 38.9 | 28.2 | ||
| Gamal hameed et al. [39] | Egypt | C | 38 right | 33.1 | 24.4 | ||
| 30 left | 28.7 | 22.1 | |||||
| Chaijaroonkhanarak et al. [49] | Thailand | C | 166 males | 37.1 | 27.4 | ||
| 98 females | 33.2 | 23.7 | |||||
| Wang et al. [41] | China | CT | 90 | 34.5 | 25.1 | − 0.03 | |
| Jung et al. [51] | Korea | CT | 38 | 37.7 | 26.9 | ||
| Present study | India | C & CT | 4266 | 34.65 | 23.72 | − 1.75 |
SI Supero-inferior, AP Anteroposterior, C Cadaveric study, CT Computed Tomography
In case of glenoid version, “–” sign demarcates retroversion and ‘ + ’ sign demarcates anteversion
The glenoid version can also dictate the fate of the glenoid component in anatomic or reverse shoulder arthroplasty. Nyffeler et al. [63] has shown the eccentric loading of the glenoid to increase even in 4 degrees of increased anteversion or retroversion from a neutral position. Although the glenoid version can be changed during shoulder arthroplasty, the native version should be evaluated carefully during the preoperative period. Glenoid version has also shown variations across different countries and ethnicities (Table 7). Churchill et al. [38] found the average glenoid version for black and white patients in the United States of America to be 0.20° and 2.65° of retroversion, respectively. Whereas, Mizuno et al. [42] noted a mean of 2.3 degrees of retroversion in the French population and 6 degrees of retroversion in the Japanese population. The Indian data presented in this systematic review was suggestive of an average of 1.75 degrees of retroversion which is comparable to other ethnicities except for the Japanese population showing excessive mean retroversion. Probably further Asian studies would be needed to understand the difference in the glenoid version between these two Asian populations. The glenoid inclination was measured by different methods in the Indian studies compared to the studies conducted on other ethnic populations. Thus, no inter-study comparisons can be drawn between the glenoid inclination of these studies.
Another important finding from this review was the similarity between the glenoid dimensions all over India. This study includes a unique comparison between glenoid diameters, version, and glenoid index between eastern, western, northern, and southern parts of India which has never been performed before. Although the glenoid dimensions of India have shown to differ from other countries, the similarity of glenoid parameters between the different regions of India highlights the need for uniform measurements of prostheses all over the country. India is a country with vast genetic diversities [64]. This is further important considering the preconceived notion that in a country as large and populated as India there are bound to be geographical variations of anatomical parameters. The present review refutes that notion with no findings of statistical significance across geographical domains.
The subgroup analysis based on genders reveals that there is a significant difference in glenoid dimensions between genders. The glenoid SI and AP1 diameters were both significantly higher in males. Thus, the median width (AP1 diameter) of 24.2 mm in males and 21.5 mm can guide the proposed approximate width for the glenoid baseplate in a gender-based Indian RSA glenoid baseplate. The glenoid dimension in Indian females and males is significantly lower than in other ethnic populations. A few Indian authors have already reported difficulty in placing the central peg of glenoid baseplate due to the small size of the Indian glenoid [65]. This mismatch between the available sizes of glenoid components and the average glenoid maximum width points out the urgent need for smaller sizes of glenoid baseplates in the inventory of RSA. Of note, only four studies included in gender-specific comparisons represent an underpowered sub-group analysis.
The stability of the baseplate is one of the principles determining factors for the long-term outcome of reverse shoulder arthroplasty and the same holds even for the glenoid component of the anatomic shoulder arthroplasty [66, 67]. Even the smallest available glenoid baseplates available in the market can cause an overhanging and poor fixation to the glenoid if it has a maximum diameter lesser than 25 mm. The overhanging prosthesis has been already shown to affect the stability and limit the impingement-free range of motion in clinical studies [68]. Thus, it's high time to make the custom-made smaller glenoid baseplates (< 25 mm) available to the Indian population.
The review has its limitations. First, the quality of most of the studies was poor. In addition to that, the measurements of glenoid parameters were performed by different methods like manual measurement, software-based, or CT-based measurements across studies. However, there were only 5 studies that didn’t perform the measurements on cadavers. The pooled average between different measurements didn’t differ much (Table 8). Thus, cadaveric or CT-based measurements may be used interchangeably. Another limitation of this review is that we have not calculated state-specific variations, but used four large geographical domains for comparison of glenoid dimensions. To the best of our knowledge, this was the first systematic review performed on Indian glenoid dimensions including 36 studies.
Table 8.
Comparison of glenoid dimensions measured by manual measurements in cadavers, software-based measurements in cadavers, 2D CT and 3D CT
| Type of study | Number of scapulae | Glenoid SI diameter or Height | Glenoid AP1 diameter or maximum width | Glenoid AP2 diameter or Upper half maximum width | Glenoid index | Glenoid version |
|---|---|---|---|---|---|---|
| Cadaveric | 3025 | 34.8 | 23.8 | 16.7 | 67.8 | − 1.98 |
| Software based Cadaveric [27] | 200 | 35.5 | 23 | 66.89 | − 5.985 | |
| 35.9 | 24.1 | 67.99 | ||||
| 2D CT [17] | 100 | 31.3 | 24.0 | − 1.8 | ||
| 3D CT [8, 16, 30] | 400 | 33.3 | 23.5 | 20.1 | − 1.4 |
SI Supero-inferior, AP Anteroposterior, CT Computed Tomography
Conclusion
The glenoid dimensions in the Indian population are smaller compared to the average European and American populations. The average glenoid maximum width of the Indian population is 1.3 mm smaller than the minimum glenoid baseplate size available in RSA. The morphometric parameters of the glenoid cavity don’t differ between different regions of India. However, males have a higher glenoid dimension compared to females. Glenoid components specific to the Indian market need to be designed to reduce glenoid failure attributable to the above findings.
Author contributions
SP: Writing of manuscript, manuscript preparation, Data abstraction and analysis. MA: Planning of study, writing of manuscript, Data abstraction and analysis. LD: Data abstraction. BSR: Quality analysis. RBK: Data abstraction and analysis, proofing of manuscript.
Funding
There is no funding source.
Data availability
All data supporting the findings of this study are available within the paper and its Supplementary Information. Additional data can be made available on request to corresponding author.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was exempted from any ethical clearance.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Souvik Paul, Email: 1990.souvik@gmail.com.
Manit Arora, Email: manit_arora@hotmail.com.
Lakhsmana Das, Email: sekarldas@gmail.com.
Balgovind S. Raja, Email: balgovindsraja@gmail.com
Roop Bhusan Kalia, Email: roopkalia2003@yahoo.com.
References
- 1.Matsen FA, Clinton J, Lynch J, et al. Glenoid component failure in total shoulder arthroplasty. The Journal of Bone and Joint Surgery-American Volume. 2008;90:885–896. doi: 10.2106/JBJS.G.01263. [DOI] [PubMed] [Google Scholar]
- 2.Dillon MT, Chan PH, Prentice HA, et al. The association between glenoid component design and revision risk in anatomic total shoulder arthroplasty. Journal of Shoulder and Elbow Surgery. 2020;29:2089–2096. doi: 10.1016/j.jse.2020.02.024. [DOI] [PubMed] [Google Scholar]
- 3.Piponov HI, Savin D, Shah N, et al. Glenoid version and size: Does gender, ethnicity, or body size play a role? International Orthopaedics. 2016;40:2347–2353. doi: 10.1007/s00264-016-3201-8. [DOI] [PubMed] [Google Scholar]
- 4.Matsumura N, Oki S, Ogawa K, et al. Three-dimensional anthropometric analysis of the glenohumeral joint in a normal Japanese population. Journal of Shoulder and Elbow Surgery. 2016;25:493–501. doi: 10.1016/j.jse.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Ankushrao DS, Dombe DD. Morphological and morphometrical study of scapulae in western Indian population. Indian Journal of Clinical Anatomy and Physiology. 2017;4:298–303. [Google Scholar]
- 6.Sheth U, Saltzman M. Reverse total shoulder arthroplasty: Implant design considerations. Current Reviews in Musculoskeletal Medicine. 2019;12:554–561. doi: 10.1007/s12178-019-09585-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mathews S, Burkhard M, Serrano N, et al. Glenoid morphology in light of anatomical and reverse total shoulder arthroplasty: A dissection and 3D-CT-based study in male and female body donors. BMC Musculoskeletal Disorders. 2017 doi: 10.1186/s12891-016-1373-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meshram P, Pawaskar A, Kekatpure A. 3D CT scan-based study of glenoid morphology in Indian population: Clinical relevance in design of reverse total shoulder arthroplasty. Journal of Clinical Orthopaedics and Trauma. 2020;11:S604–S609. doi: 10.1016/j.jcot.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deepali RK, Ashutosh A, Ajay C, et al. Osseous anatomy of glenoid: Cadaveric study. International Journal of Anatomy and Research. 2016;4:2473–2479. [Google Scholar]
- 10.Sinha P, Bhutia KL, Kumar TB, Sarda RK. Morphometric study of glenoid cavity of dry human scapula. International Journal of Medical Research Professionals. 2016 doi: 10.21276/ijmrp.2016.2.3.020. [DOI] [Google Scholar]
- 11.Rajput HB, Vyas KK, Shroff BD. A study of morphological patterns of glenoid cavity of scapula. National Journal of Medical Research. 2012;2:504–507. [Google Scholar]
- 12.Mamatha T, Pai SR, Murlimanju BV, et al. Morphometry of glenoid cavity. The Online Journal of Health and Allied Sciences. 2011;10:1–4. [Google Scholar]
- 13.Pal M, Sarma HP, Guha I. Glenoid cavity of scapula in Indian population: A morphometric analysis. Journal of Anatomical Society of India. 2018;67:S71–S72. [Google Scholar]
- 14.Gosavi S, Jadhav S, Garud R. Morphometric study of scapular glenoid cavity in Indian population. IOSR Journal of Dental and Medical Sciences. 2014;13:67–69. [Google Scholar]
- 15.Sahu D, Jagiasi JD, Valavi AS, Ubale T. The distance between the pectoralis major tendon insertion and the top of the humeral head is a reliable landmark: An anatomic study. Joints. 2019;7:37–40. doi: 10.1055/s-0039-3401818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raaj MS, Felicia C, Sundarapandian S, Ashma KA. Morphologic and morphometric analysis of glenoid cavity of human scapula. International Journal of Research in Medical Sciences. 2018;7:52. [Google Scholar]
- 17.Sahu D, Joshi M, Rathod V, et al. Geometric analysis of the humeral head and glenoid in the Indian population and its clinical significance. JSES International. 2020;4(4):992–1001. doi: 10.1016/j.jseint.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jagiasi JD, Valavi AS, Ubale TV, Sahu D. Humeral head and glenoid dimensions in the Indian population: A cadaveric study. International Journal of Anatomy and Research. 2018;6:5760–5764. [Google Scholar]
- 19.Vinay G. A morphometric study of scapular glenoid cavity. Journal of Anatomical Society of India. 2016;65:S2. [Google Scholar]
- 20.Bamne A. Determination of the native angles of glenoid and humerus head version of adult skeletons At Karad, Maharashtra, India. International Journal of Anatomy and Research. 2017;5:4707–4710. [Google Scholar]
- 21.Patil GV. Morphometrical study of scapular glenoid cavities. Journal of Anatomical Society of India. 2015;64:S3. [Google Scholar]
- 22.Thute PP, Keche HA, Fulmali DG. Morphometric study of glenoid cavity of human scapula in Central India. Journal of Evolution of Medical and Dental Sciences. 2020;9:2340–2344. [Google Scholar]
- 23.Singh R. Surgical anatomy of the glenoid cavity and its use in shoulder arthroplasty among the north indian population. Cureus. 2020 doi: 10.7759/cureus.11940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yadav Y, Potdar P, Dhakar J. Morphometric study of glenoid cavity of scapulae in north Indian population with clinical significance. Santosh University Journal of Health Sciences. 2020;5:78–81. doi: 10.18231/j.sujhs.2019.016. [DOI] [Google Scholar]
- 25.Morelli KM, Martin BR, Charakla FH, et al. Acromion morphology and prevalence of rotator cuff tear: a systematic review and meta-analysis. Clinical Anatomy. 2019;32:122–130. doi: 10.1002/ca.23309. [DOI] [PubMed] [Google Scholar]
- 26.Khalkar A, Jadhav S. Morphology and morphometry of glenoid cavity and it’s clinical significance. Indian Journal of Applied Research. 2020;6(10):49–51. [Google Scholar]
- 27.Uma S, Balasubramanyam V. Morphometry of glenoid using digital photographs and image processing software. International Journal of Anatomy and Research. 2016;4:2720–2724. [Google Scholar]
- 28.Chhabra N, Prakash S, Mishra BK. An anatomical study of glenoid cavity: its importance in shoulder prosthesis. International Journal of Anatomy and Research. 2015;3:1419–1424. [Google Scholar]
- 29.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bodanki C, Yadoji HK, Maryada VR, Annapareddy Venkata GR. Three Dimensional anthropometric analysis of glenoid anatomy in normal Indian population. Indian Journal of Orthopaedics. 2021;55:861–868. doi: 10.1007/s43465-020-00321-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henry BM, Tomaszewski KA, Ramakrishnan PK, et al. Development of the anatomical quality assessment (AQUA) tool for the quality assessment of anatomical studies included in meta-analyses and systematic reviews. Clinical Anatomy. 2017;30:6–13. doi: 10.1002/ca.22799. [DOI] [PubMed] [Google Scholar]
- 32.Study Quality Assessment Tools. (2021). NHLBI, NIH. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 19 Jun 2021
- 33.Patel S, Shah M, Vora R, et al. Morphometric analysis of scapula to determine sexual dimorphism. International Journal of Medicine and Public Health. 2013;3:207. [Google Scholar]
- 34.Shewale SN, Laeeque M, Sukre SB, Patil SC. Morphometric study of glenoid cavities of scapulae in Marathwada population. International Journal of Anatomy and Research. 2017;5:3759–3765. [Google Scholar]
- 35.Lingamdenne PE, Marapaka P. Measurement and analysis of anthropometric measurements of the human scapula in Telangana region, India. International Journal of Anatomy and Research. 2016;4:2677–2683. [Google Scholar]
- 36.Mourad W, Wiater JM, Wiater BP, Martusiewicz A. Baseplate options for reverse total shoulder arthroplasty. Current Reviews in Musculoskeletal Medicine. 2020;13:769–775. doi: 10.1007/s12178-020-09677-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coskun N, Karaali K, Cevikol C, et al. Anatomical basics and variations of the scapula in Turkish adults. Saudi Medical Journal. 2006;27:1320–1325. [PubMed] [Google Scholar]
- 38.Churchill RS, Brems JJ, Kotschi H. Glenoid size, inclination, and version: An anatomic study. Journal of Shoulder and Elbow Surgery. 2001;10:327–332. doi: 10.1067/mse.2001.115269. [DOI] [PubMed] [Google Scholar]
- 39.Hassanein GHE-S. Morphometry of glenoid fossa in adult Egyptian scapulae. International Journal of Anatomy and Research. 2015;3:1138–1142. [Google Scholar]
- 40.Aigbogun EO, Oladipo GS, Oyakhire MO, Ibeachu CP. Morphometry of the glenoid cavity and its correlation with selected geometric measurements of the scapula. Bangladesh Journal of Medical Science. 2017;16:572–579. [Google Scholar]
- 41.Wang H, Tang K, Gong J, et al. Measurement and analysis of glenoid bony anatomy by use of three-dimensional computed tomography. Chinese Journal of Reparative and Reconstructive Surgery. 2009;23:822–826. [PubMed] [Google Scholar]
- 42.Mizuno N, Nonaka S, Ozaki R, et al. Three-dimensional assessment of the normal Japanese glenoid and comparison with the normal French glenoid. Orthopaedics & Traumatology, Surgery & Research. 2017;103:1271–1275. doi: 10.1016/j.otsr.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 43.Rosales-Rosales L, Rosales-Varo AP, García-Espona MA, et al. Anthropometrical study of the human glenoid in a normal Spanish population. Revista Española de Cirugía Ortopédica y Traumatología. 2019;63:327–335. doi: 10.1016/j.recot.2019.04.005. [DOI] [PubMed] [Google Scholar]
- 44.Polguj M, Jȩdrzejewski KS, Podgórski M, Topol M. Correlation between morphometry of the suprascapular notch and anthropometric measurements of the scapula. Folia Morphol (Warsz) 2011;70:109–115. [PubMed] [Google Scholar]
- 45.Iannotti JP, Gabriel JP, Schneck SL, et al. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. Journal of Bone and Joint Surgery. American Volume. 1992;74:491–500. [PubMed] [Google Scholar]
- 46.Lombardo D, Kolk S, Frank C, Sabesan V. Computational assessment of glenoid morphology in us and Australian patients. Orthopaedic Proceedings. 2016;98-B:6. [Google Scholar]
- 47.Cabezas AF, Krebes K, Hussey MM, et al. Morphologic variability of the shoulder between the populations of North American and East Asian. CiOS Clinics in Orthopedic Surgery. 2016;8:280–287. doi: 10.4055/cios.2016.8.3.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.El-Din WAN, Ali MHM. A morphometric study of the patterns and variations of the acromion and glenoid cavity of the scapulae in Egyptian population. Journal of Clinical and Diagnostic Research. 2015;9:AC08–AC11. doi: 10.7860/JCDR/2015/14362.6386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chaijaroonkhanarak W, Amarttayakong P, Ratanasuwan S, et al. Predetermining glenoid dimensions using the scapular dimensions. European Journal of Orthopaedic Surgery & Traumatology. 2019;29:559–565. doi: 10.1007/s00590-018-2313-9. [DOI] [PubMed] [Google Scholar]
- 50.Jung HJ, Jeon IH, Ahn TS, et al. Penetration depth and size of the nonarthritic glenoid: Implications for glenoid replacement. Clinical Anatomy. 2012;25:1043–1050. doi: 10.1002/ca.22045. [DOI] [PubMed] [Google Scholar]
- 51.Varghese S, Madhavan Chandramathi Amma M. Morphometric study of dry human scapulae. Journal of Evolution of Medical and Dental Sciences. 2017;6:5365–5371. [Google Scholar]
- 52.Vardhan, H., Chuhan, S. K., Modi, S. (2019). Study of morphology of glenoid cavity of scapula : Done on dry bone specimen in the department of anatomy of MGM medical college Jamshedpur. International Journal of Medical and Health Research, 2, 91–94
- 53.Vaishnani H, Jethva K, Rathwa A, Sharma P. Morphometry and Morphology of Glenoid Cavity of Scapula. International Journal of Anatomy and Research. 2018;6:4798–4802. [Google Scholar]
- 54.Singh A, Singh A, Agarwal P, Gupta R. A morphological and morphometric study of glenoid fossa of scapula and its implication in shoulder arthroplasty. International Journal of Anatomy Radiology and Surgery. 2019;8:10–13. [Google Scholar]
- 55.Shalom PE, Dakshayani K. A morphometric study of glenoid cavity and its implication in shoulder arthroplasty and prosthetic designs. National Journal of Clinical Anatomy. 2018;7:190–194. [Google Scholar]
- 56.Mahto AK, Omar S. Dimensions of glenoid fossa of scapula: implications in the biomechanics of an implant design. International Journal of Scientific Study. 2015;3:146–148. [Google Scholar]
- 57.Akhtar M, Kumar B, Fatima N, Kumar V. Morphometric analysis of glenoid cavity of dry scapulae and its role in shoulder prosthesis. International Journal of Research in Medical Sciences. 2016;4:2770–2776. [Google Scholar]
- 58.Chavan SR, Bhoir M, Verma S, Professor A. A study of anthropometric measurements of the human scapula in Maharashtra, India. International Journal of Anatomy. 2017;1:23–26. [Google Scholar]
- 59.Dhindsa GS, Singh Z. A study of morphology of the glenoid cavity. Journal of Evolution of Medical and Dental Sciences. 2014;3:7036–7044. [Google Scholar]
- 60.Gupta S, Magotra R, Kour M. Morphometric analysis of glenoid fossa of scapula. Journal of Evolution of Medical and Dental Sciences. 2015;4:7761–7766. [Google Scholar]
- 61.Kalra S, Thamke S, Khandelwal A, Khorwal G. Morphometric analysis and surgical anatomy of coracoid process and glenoid cavity. Journal of Anatomical Society of India. 2016;65:114–117. [Google Scholar]
- 62.Kavita P, Jaskaran S. Morphology of coracoid process and glenoid cavity in adult human scapulae. International Journal Of Pharmaceutical And Bio-Medical Science. 2013;2(2):62–65. [Google Scholar]
- 63.Nyffeler RW, Sheikh R, Atkinson TS, et al. Effects of glenoid component version on humeral head displacement and joint reaction forces: An experimental study. Journal of Shoulder and Elbow Surgery. 2006;15:625–629. doi: 10.1016/j.jse.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 64.Reich D, Thangaraj K, Patterson N, et al. Reconstructing Indian population history. Nature. 2009;461:489–494. doi: 10.1038/nature08365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Thati B, Bodanki C, Badam VK, et al. Custom 3D printed jigs in salvage reverse shoulder arthroplasty for failed four-part proximal humerus fracture fixation: A case report. Journal of Orthopaedic Case Reports. 2020;10:25–28. doi: 10.13107/jocr.2020.v10.i02.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kim MS, Rhee YG, Oh JH, et al. Clinical and radiologic outcomes of small glenoid baseplate in reverse total shoulder arthroplasty: A prospective multicenter study. Clinics in Orthopedic Surgery. 2022;14:119. doi: 10.4055/cios20301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hasler A, Meyer DC, Tondelli T, et al. Radiographic performance depends on the radial glenohumeral mismatch in total shoulder arthroplasty. BMC Musculoskeletal Disorders. 2020;21:1–9. doi: 10.1186/s12891-020-03219-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chae SW, Kim SY, Lee H, et al. Effect of baseplate size on primary glenoid stability and impingement-free range of motion in reverse shoulder arthroplasty. BMC Musculoskeletal Disorders. 2014;15:1–7. doi: 10.1186/1471-2474-15-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data supporting the findings of this study are available within the paper and its Supplementary Information. Additional data can be made available on request to corresponding author.