Abstract
Context:
Sleep plays a vital role in cognitive and physical performance. Teenage athletes (ages 13-19 years) are considered especially at risk for disordered sleep and associated negative cognitive, physical, and psychosomatic effects. However, there is a paucity of evidence-based recommendations to promote sleep quality and quantity in athletes who fall within this age range. We performed a review of the literature to reveal evidence-based findings and recommendations to help sports instructors, athletic trainers, physical therapists, physicians, and other team members caring for young athletes provide guidance on sleep optimization for peak sports performance and injury risk reduction.
Methods:
PubMed, Scopus, and Cochrane CENTRAL were searched on May 11, 2016, and then again on September 1, 2020, for relevant articles published to date.
Study Design:
Narrative review.
Level of Evidence:
Level 4.
Results:
Few studies exist on the effects disordered sleep may have on teenage athletes. By optimizing sleep patterns in young athletes during training and competitions, physical and mental performance, and overall well-being, may be optimized. Adequate sleep has been shown to improve the performance of athletes, although further studies are needed.
Conclusion:
Twenty-five percent of total sleep time should be deep sleep, with a recommended sleep time of 8 to 9 hours for most young athletes. Screen and television use during athletes’ bedtime should be minimized to improve sleep quality and quantity. For young athletes who travel, jet lag can be minimized by allowing 1 day per time zone crossed for adjustment, limiting caffeine intake, planning meals and onboard sleeping to coincide with destination schedules, timing arrivals in the morning whenever possible, and using noise-canceling headphones and eyeshades.
Strength-of-Recommendation Taxonomy (SORT):
B.
Keywords: adolescents, competition, sports, teen, teenagers
Sleep plays a vital role in sports performance in children and adolescents. There are many factors that affect sleep quality and duration that bear consideration in athletes, especially in teenagers. For example, younger athletes may be more affected by travel and timing of scheduled training and competition than their adult counterparts. Altitude has adverse effects on sleep; therefore, it is beneficial for athletes to undergo acclimation before competitions, particularly adolescents. Improper diet and nutrition choices may also negatively influence sleep. 30 Sleep deprivation in teenagers is associated with poor athletic performance, 18 increased risk of injuries, 62 increased pain scores, 51 persistent pain, 12 and overall health. 17 This review explores factors affecting sleep duration and quality and discusses evidence-based recommendations that support healthy sleep habits in young athletes.
Methods
We conducted a review of medical literature to identify articles on sleep and sports. PubMed, Scopus, and Cochrane CENTRAL were first searched on May 11, 2016, with English-language limits, resulting in 2509 citations after eliminating duplicates. The search included subject headings and keywords such as “sleep,” “sports,” “injuries,” “athletes,” “teenager,” “performance,” and “sleep deprivation.” The search results were updated on September 1, 2020, resulting in an additional 243 citations after removing duplicates, for a total of 2752 articles. Further articles were identified by searching the reference lists of relevant publications. Four authors reviewed the abstracts identified through this process to determine eligibility for study inclusion. The narrative review included articles related to sleep in athletes of any age as there were not a lot of articles focused on children and adolescents. Articles focused on sleep in pediatric athletes and active youth were examined thoroughly. Articles unrelated to sleep in athletes or active individuals were excluded.
General Characteristics of Sleep
The basic structural organization of normal sleep includes 2 distinct phases: nonrapid eye movement, which usually comes first, followed by rapid eye movement. Nonrapid eye movement sleep is then subdivided into 4 stages: N1, N2, N3, and N4. 55 The length of time it takes to transition from full wakefulness to the lightest of these stages, N1, is referred to as sleep-onset latency, 55 which varies widely from person to person. An average of 40 minutes after falling asleep, humans enter N3 stage, which should comprise 25% of their total sleep time. During N3, the brain produces slow, long waves, called δ waves, corresponding to deep sleep. This stage is considered the most restful portion of the entire sleep cycle, as it plays a major role in helping clear the brain for learning the following day, and reverts the accumulated need for sleep that builds over a normal day of being awake. 55
The recommended minimum amount of sleep for individuals between the ages of 7 and 19 years is 8 to 9 hours per night; 10 hours is the recommendation minimum for children 6 years old and younger. It has been suggested that a significant number of pediatric athletes do not meet this recommended minimum due to a variety of factors, such as having to train, compete, and travel, in addition to maintaining a regular academic load.
One study, evaluating 196 competitive athletes between the ages of 14.4 and 17 years, found that 14.8% of them slept 6 hours 59 minutes or less, 33.2% slept between 7 hours and 7 hours 59 minutes, and only 52% of the athletes slept 8 hours or more. 92 Research has demonstrated that sleep is paramount for athletes to be healthy in mind and body, and this is especially true in pediatric athletes whose minds and bodies are in the process of physically developing while trying to succeed with academic and athletic performance in school. 92 Normal sleep physiology and chronotypes in children and adolescents include later bedtimes and later morning wakening patterns than adults. 91 A child’s sleep patterns can be affected by their parents’ sleep habits, as well as their daily activity and behaviors, sleep environment, and psychosocial conditions. 15
Factors Affecting Sleep
Many factors affect a person’s sleep, and some are especially relevant to young athletes. Low quality or quantity of sleep can affect a person’s overall performance and even increase the chance of injury, 69 so taking these factors into account may improve an athlete’s performance during training and competitions. Perhaps this becomes most evident when young athletes travel to a far location for competitions, where jet lag and changes in time zones, altitudes, oxygen levels, bed type, and environmental conditions (eg, noise, amount of light, distractions) are involved. The following are some factors that may affect sleep quantity and quality, which if taken into careful consideration, may help maximize the performance of young athletes.
Exercise
Exercise in general tends to have a positive effect on sleep in individuals compared with sedentary counterparts. Different types of exercise may influence participants in different ways. Elite individual-sport athletes, for example, tend to go to bed earlier and wake up earlier, yet obtain less sleep overall than those who participate in team sports. 48 In a study comparing sedentary adolescent girls who began a physical activity program versus those who remained inactive, sleep quality only improved in the active group. 36 Another study exploring how daily training load impacted the sleep-wake cycle of adolescent female basketball players during a 14-day training camp found that sleep onset and offset times were delayed and total sleep times were prolonged during rest days compared with training days. 49 Gerber et al, 31 studying the effects of vigorous exercise in 42 late adolescent and collegiate students, demonstrated similar favorable effects on sleep quantity and quality (ie, increased total sleep time, more stage N4 and rapid eye movement sleep, more slow-wave sleep, and a lower percentage of light sleep). Furthermore, they found that vigorous exercise was associated with less stress, pain, subjective sleep complaints, and depressive symptoms. 31
A study evaluating quality of sleep in adolescent runners and football players compared with nonathlete controls showed favorable sleep patterns in the adolescent athletes, specifically, shortened sleep-onset latency, fewer awakenings after sleep onset, more N4 sleep, and less rapid eye movement sleep. 40 Interestingly, these favorable sleeping patterns were sustained even on days without exercise. 11 Conversely, a study comparing high-school swimmers who overreached (a term loosely defined as regularly training before your muscles have had time to recover from the previous workout) with those who did not overreach showed that overreaching was associated with decreased sleep efficiency. 99 Thus, we can observe a trend suggesting that exercise is beneficial to sleep quantity and quality, so long as the person is not overreaching in their training.
Timing of Exercise
Recent studies have reported that vigorous exercise a few hours before bedtime does not disturb sleep quantity or quality. Vigorous or moderate late-night (ie, 2-3 hours before bedtime) exercise in teenagers did not negatively affect sleep-onset latency or wake time after sleep onset, but instead seemed to improve sleep-onset latency without disturbing sleep quality.25,65 In addition, 1 study showed that early evening high-intensity training did not impact subsequent sleep quality or quantity in elite male youth soccer players. 74 However, in the adult population, other studies concluded that sleep quality and quantity were impaired in elite soccer players (25.9 [SD 7.5] years of age) after night matches and in elite swimmers (22.5 [SD 1.7] years of age) who trained early in the morning.28,78,79 However, in these cases, sleep disturbance may have been related to an overall decrease in available time to sleep due to sports scheduling.28,78,79 Therefore, in general, contrary to popular belief, it is not detrimental to sleep quality for people to train 2 to 3 hours before bedtime.
Competition
Factors related to competition, such as anxiety, may result in altered sleep patterns and adversely affect performance.26,47,81 Despite young athletes reporting increased nervousness and poorer sleep on nights before competition, sleep efficiency was paradoxically improved and sleep duration was increased from baseline by about 45 minutes on average during competition periods.73,75 It is important to take these factors into consideration during competition seasons.
Travel and Jet Lag
Teenage athletes may be more affected by travel, timing of scheduled training, and competition than adult athletes. 13 Research suggests that different age groups perform best at different times of the day; for example, prepubescent children and preadolescents tend to perform best in the early morning, whereas pubescent and postpubescent adolescents appear to perform best in the afternoons. 13
Disturbances in the sleep-wake cycle following travel may cause sleep fragmentation, premature awakenings, difficulty initiating sleep, and overall sleep loss. 7 East-to-west air travel seems to have less effect on both sleep and jet lag compared with west-to-east flights.7
Recommendations to help minimize jet lag include (1) allowing 1 day per time zone crossed for adjustment, (2) limiting caffeine intake, (3) planning meals and onboard sleeping to coincide with the destination schedule, (4) timing arrivals in the morning whenever possible, (5) using noise-canceling headphones and eyeshades. 7 Light is thought to influence sleep by suppressing melatonin 67 ; however, studies evaluating the effects of light on sleep in young athletes are limited.
Diet and Nutrition
A number of nutritional factors may affect sleep, including supplements (eg, valerian, melatonin, and tryptophan), composition of food ingested, and timing of meals. 33 There are some general concerns in the pediatric population regarding nutrition and supplements, such as consumption of caffeine, sugars, and high calories from ingesting sports and energy drinks. 16 A large cross-sectional study involving 1032 adolescents aged 13 to 17 years reported that nearly two-thirds had consumed energy drinks at least once, and about 41% recently (within the past 3 months); so one can infer that consumption of energy drinks among adolescents is widespread despite current recommendations against use. 63
Medications and Supplements
Imbalance of serotonin (5-hydroxytryptamine) affects sleep. Ingestion of tryptophan, melatonin, and high-glycemic-index foods affect serotonin balance, which in turn have different effects on the regulation of sleep. Tryptophan intake may improve sleep-onset latency and subjective sleep quality. 33
Evidence of melatonin’s positive effects on sleep duration and quality is limited in healthy athletic populations. A double-blind study showed 5 mg of melatonin versus placebo did not have a statistically significant difference in subjective sleep quality or physical performance, and resulted in less than 1% difference in time to complete 4 km of cycling between both groups. 2 Another study similarly suggested that standard doses of melatonin taken at bedtime have limited or no significant effect on quality and quantity of sleep or athletic performance in adult athletes. 57 In children and adolescents, there is concern that exogenous intake of this pineal hormone may affect pubertal reproductive hormones, and it is therefore not recommended. 13
Caffeine is commonly used by adult athletes as a performance enhancement supplement. Although it can increase feelings of energy after its consumption, it may also negatively affect sleep.10,76 Caffeine consumed within 2 hours of bedtime increases sleep-onset latency and decreases slow-wave sleep and total sleep time.10,76 Consumption of any amount of caffeine is not recommended for pediatric athletes. 16
Performance-Enhancing Substances
Performance-enhancing substances, such as anabolic androgenic steroids, are not recommended for healthy adult or pediatric athletes for a myriad of reasons which fall outside the scope of this paper. In adult athletes, however, anabolic androgenic steroids have been associated with reduced sleep efficiency and alteration of sleep architecture. 95
Meal Composition and Timing
There are few data regarding the relationship between the composition of meals and sleep quality in teenage athletes. However, a pediatric study comparing ingestion of high- and low-glycemic-index drinks 1 hour before bedtime demonstrated increased arousals in the high-glycemic-index group. 37 The form of carbohydrate intake (ie, solid meal vs drink with high, normal, and low carbohydrate content) may also have effects on sleep quality. For example, a study comparing these different forms of intake demonstrated decreased sleep-onset latency up to 3 hours after ingestion of solid meals without effect on sleep quality or duration as compared with a liquid meal. 68 They hypothesized that solid meals have a vagal afferent stimulation which contributes to the observed decrease in sleep-onset latency, which liquid meals do not. Another study, involving 18-year-old Brazilian basketball players, noted that as the total energy intake for the day increased, the quality of sleep decreased (lower sleep efficiency and wake after sleep onset) regardless of the last meal’s glycemic index; however, conclusions may be limited due to the number of study subjects involved (N = 9). Further research exploring the relationship between nutrition and sleep in teenage athletes is necessary.
Relaxation Training
A study involving young dancers (8-19 years old) in Australia found that implementation of a progressive muscle relaxation intervention led to a statistically significant decrease in sleep-onset latency. 53 In addition, a systematic review of the efficacy of cognitive behavioral sleep interventions on 357 adolescents (mean age, 14 years) found that the interventions improved sleep-onset latency by 16.15 minutes (95% CI −26.13 to −6.17) and sleep efficacy by 2.82% (95% CI 0.58% to 5.07%), both measured by actigraphy. Furthermore, subjective global sleep quality, daytime sleepiness, depression, and anxiety also improved. 8
Altitude
Altitude is associated with more frequent sleep arousals, reduction in N4 sleep, decreased slow-wave sleep, decreased oxygen saturation, and increased periodic breathing (including increased central apneas and hypopneas), giving an overall feeling of poor sleep quality.4,35,39
Adolescents competing at high altitude without adequate time for acclimation may be more sensitive to experiencing symptoms of overtraining and poor performance, including general fatigue, headaches, diminished appetite, and impaired sleep quality or quantity. 7 In the absence of jet lag, the more time athletes spend at high altitude, the less they experience sleep disturbances. 80 On returning to low altitude, sleep behaviors return to baseline after 5 to 6 days. 45 Acclimation at high altitude may improve sleep in young athletes. Fourteen days at a new time zone and altitude provided a suitable adaptation period for teen Australian football players.45,80
Temperature
Current evidence suggests that as body temperature decreases, it becomes easier to fall asleep 83 ; however, there are few studies of this in young athletes and findings are conflicting.
Electronic Media
Sleep behavior is influenced by use of electronic media, including televisions, computers, smartphones, and tablets. A study of 4th to 7th graders showed that shorter sleep duration and perceived insufficient rest were associated with increased screen use during bedtime and sleeping with a television in the room. 24
Taking a Sleep History
The Pittsburgh Sleep Quality Index, a validated questionnaire inventory tool, is the most widely used psychometric sleep quality screening instrument successfully applied to adolescents and young adult athletes. 93 This index includes questions regarding bedtime, sleep-onset latency, wake time, total sleep time, night-time awakenings and disturbances, sleep quality, sleep medication use, and daytime functioning. Samuels et al 77 published the Athlete Sleep Screening Questionnaire, a novel, subjective, self-reported sleep-screening questionnaire for elite athletes. Common questions that reflect sleep disorder risk factors are listed in Table 1.
Table 1.
Key discussion topics when taking a thorough sleep history
| 1 | Current sleep habits |
| 2 | Changes from baseline sleep habits (encourage the use of a sleep diary) |
| 3 | Past medical or family history of sleep disorders (eg, narcolepsy, insomnia, sleep apnea), psychiatric conditions (eg, depression, anxiety, attention-deficit/hyperactivity disorder), and other relevant health issues |
| 4 | Medication use (past and current), both prescription and over the counter |
| 5 | Sleep aid use and frequency |
| 6 | Caffeine or other stimulant substance intake |
| 7 | Recreational drug use history |
| 8 | Sleep habits (eg, bed times, time of awakening, nap history) |
| 9 | Subjective assessment of sleep quality (eg, average, better, worse than average, feel rested, presence of fatigue, daytime somnolence) |
Sleep and Injury
Sleep deprivation in teenagers is associated with an increased risk of musculoskeletal injury, a situation which can be especially detrimental to young athletes. A systematic review evaluating a possible relationship between chronic lack of sleep and increased risk of sports and musculoskeletal injury found a statistically significant association.18,29 Lack of sleep is not only associated with increased risk of musculoskeletal injuries but may also be linked to other forms of injury and injury-prone behaviors. 69 Another study found that employed adolescent students who slept 5 hours or less per school night were 2.9 times more likely to experience an occupational injury than adolescents who slept at least 8 hours per night. 32 Likewise, drivers aged 17 to 19 years getting 6 hours of sleep or less per night demonstrated an increased risk of motor vehicle accidents compared with those getting more than 6 hours of sleep each night. 58 Interestingly, high-school students who slept 7 hours or less per school night also displayed a significant increase in injury-related risk behaviors (eg, infrequent use of seat belt or bicycle helmet and driving under the influence of alcohol) compared with students who slept at least 9 hours per school night. 101 Sleep-deprived adolescents were more likely to experience a bicycle accident,41,69 with the greatest risk noted in adolescents sleeping fewer than 5.5 hours per night. 87
Milewski et al 62 found that adolescent athletes who slept less than 8 hours per night were 1.7 times more likely to sustain a sport-related injury than their peers who slept at least 8 hours. The increased injury rate is thought to be correlated with an association between sleep deprivation and decreased psychomotor performance, mood, motor, and cognitive function. 62 Similarly, Luke et al 52 found a relationship between sleeping 6 or fewer hours per night and fatigue-related injury in pediatric athletes. An increased risk of injury was also seen in elite adolescent athletes with suboptimal nutrition who slept fewer than 8 hours on weekdays and those with simultaneously increased training load and intensity and decreased sleep time. 97 So, the importance of proper rest schedules that allow for ideal quality and quantity of sleep extend beyond optimizing athletic performance and will indeed decrease the overall risk of injury in athletes. Furthermore, lack of sleep has been associated with increased pain scores, increased perceived symptoms, and persistent pain in pediatric patients. 23 The evidence suggesting that lack of adequate sleep places children and adolescents at increased risk of falls, accidents, and injuries, sport-related or otherwise, is overwhelming.
Obesity, Illness, Stress, Mood, and Disease
Poor sleep quality and quantity have been implicated as risk factors for morbidity in children, including obesity, mental illness, asthma, and other health problems. 21 Although we could not find studies evaluating the effects of sleep deprivation on illness in pediatric athletes, college freshmen and active adults with poor sleep quality and quantity (<7 hours per night) had elevated body mass index and lower performance in physical fitness tests.14,50 A 1-year study had 65 female soccer players (age range, 13-18 years) recording their sleep duration in hours and rated their stress, mood, fatigue, and soreness. Findings suggested that increased sleep was significantly associated with improved fatigue, mood, and stress. 100
Sleep and Mental Health
A study comparing sleep electroencephalogram patterns, sleep logs, and psychologic functioning in adolescents before and after a 3-week exercise program involving daily 30-minute runs concluded that the intervention group demonstrated improvements in objective sleep, subjective sleep quality, mood, concentration, and daytime sleepiness compared with controls. 40
The implementation of a treatment algorithm enables a strategic approach to evaluate sleep hygiene (Table 2). In an interesting case study, a 14-year-old boy suffering from multiple academic and personal challenges was originally diagnosed with depression, schizotypal personality disorder, and learning disabilities. 102 However, further sleep evaluation revealed a non-24-hour sleep-wake pattern and melatonin rhythm dissociations. Despite that, routine melatonin use in healthy adolescents is discouraged. In this specific case in which a hormonal imbalance was present, treatment with oral melatonin restored a normal sleep-wake schedule, and subsequent psychiatric evaluations failed to substantiate any of the 3 previous diagnoses. 102 Thus, awareness and screening of sleep disorders may prevent psychiatric misdiagnoses and enable accurate diagnosis and treatment of sleep-wake schedule disorders (Table 3).2,20,24,27,32,44,58,67,79,82,95,101 Sleep problems are also connected with overall suicidality in adolescents, although aggressive behavior has not been concurrently associated. 102
Table 2.
Recommendations for patients with PPCS symptoms related to mental health
| 1 | All patients with PPCS should be screened for mental health disorders, including depression, anxiety, PTSD, personality disorders, substance abuse, and somatoform disorders |
| 2 | All patients with PPCS should be screened for sleep disorders |
| 3 | For severe or complex PCS, PPCS, or failed treatments, referral to a mental health specialist or team should be encouraged |
| 4 | Compensatory strategies, restorative approaches, and cognitive rehabilitation should be included in a goal-oriented, comprehensive treatment plan |
| 5 | Consider use of electronic external memory devices, such as computers, smart phones, or portable voice prompt devices, to promote daily functioning |
PCS, postconcussion syndrome; PPCS, persistent postconcussion symptoms; PTSD, posttraumatic stress disorder.
Table 3.
Recommendations for practitioners to address postconcussion syndrome sleep disturbances
| 1 | Educate on the importance of sleep hygiene.27,67 |
| 2 | Advise that the primary goal of treatment is to improve the restorative quality and continuity of sleep rather than focus on the total duration of sleep, although sleep duration within age-appropriate recommendations is encouraged.24,32,58,79,101 |
| 3 | Pharmacotherapy (eg, melatonin, zolpidem) may be prescribed for short-term or long-term sleep impairments but should only be used for a short duration and at the lowest effective dose.2,95 Concussed athletes presenting with sleep difficulties may be treated safely with melatonin.44,82 |
Sleep and Concussion
In general, studies have shown conflicting evidence regarding the effect of concussion on sleep.60,70,88 In 1 study, patients with mild traumatic brain injuries reported more sleep disturbances including insomnia, difficulty falling asleep, and greater sleep impairment. However, sleep quantity, timing, and daytime sleepiness did not differ between these patients and close matched controls. 88 In another study evaluating surveys of 158 people with a history of mild traumatic brain injury, 92% of the individuals reported poor subjective sleep quality. 93
Recovery from concussions and neural remodeling has been shown to be hindered by sleep disruption.70,82,88 High-school and college athletes who experienced low quality sleep the night before baseline neurocognitive ImPACT testing reported a greater number of symptoms on the Postconcussion Symptom Scale.54,61,82 Ensuring that student athletes obtain at least 8 hours of sleep the night before taking the postinjury ImPACT test may reduce the likelihood that reported symptoms are due to sleep deprivation rather than concussion. 54
Sleep and Performance
Cognitive Performance
Sleep deprivation has been associated with impaired emotional function, short-term memory, working memory, and attention in children; and improving sleep hygiene has been shown to improve cognitive performance.13,98 A study of adolescents aged 8 to 12 years with weekly bedtime adjustments to either 1 hour earlier (sleep optimization) or 1 hour later (sleep deprivation) found that when sleep was restricted, children showed poorer performance on memory tasks, supporting the ubiquitous need to promote healthy sleep habits in children. 98
In a group of college-aged female soccer players, higher levels of global sleep dysfunction were significantly related to decreased vigor and increased tension, depression, anger, fatigue, somatic anxiety, worry, and concentration disruption. 6 In another study, a population of adolescents, who reported reduced sleep duration and other sleep-related symptoms on the Postconcussion Symptom Scale, scored lower results on the neurocognitive ImPACT testing (ImPACT Applications Inc.) when compared with asymptomatic optimally rested individuals. This difference was most pronounced in high-school girls.82,87 Other studies of ultra-endurance and extreme sport athletes have shown that prolonged exercise and its associated lack of sleep may negatively affect cognitive performance; however, the subjects studied in these investigations were adult athletes.22,36
Athletic Performance
In teenage athletes, numerous studies have consistently implicated sleep deprivation in delayed reaction time, mood disturbance, reduced time to exhaustion, increased perceived effort, fatigue, and reduced time to task failure without impacting physiologic markers of anaerobic, aerobic, or power output.9,38,90,94 Interestingly, even the type of bed in which athletes sleep may affect their performance. One study compared 74 young athletes aged 10 to 19 years who slept on either a high-rebound or a low-rebound mattress topper, or a spring mattress with no topper for 6 to 8 weeks. 59 The authors found that sleeping on high-rebound mattress toppers resulted in statistically significant improvements on some athletic performance measures (eg, 40-meter sprint) compared with sleeping on low-rebound toppers or spring mattresses without a topper. 59 Another study carried out in Italy with 12 karate athletes between 16 and 18 years of age showed that after a single night of sleep deprivation, selective attention, maximal force, and maximal force time (isometric strength) of brachial biceps was decreased, which highlights the importance of a proper sleep regimen for athletes in combat sport. 5
Psychomotor Performance
High-school student athletes often experience diminished sleep duration during the school week compared with weekends. Psychomotor vigilance test performance, a standard measure of reaction time, was found progressively to decrease throughout the week, with the worst results on Fridays. 89 Improving sleep duration in a small sample of collegiate basketball players was shown significantly to improve psychomotor vigilance test reaction times and performance in sport-specific tasks, such as shooting accuracy and sprint times. 56 A cross-sectional study assessing a connection between quality of sleep and quality of life in 272 healthy adolescent athletes between the ages of 13 and 18 years found a significant association between poor sleep quality and worse physical function/mobility, greater self-reported anxiety, depressive symptoms, fatigue, and pain interference. 72 These findings suggest that teaching otherwise healthy adolescent athletes ways to improve sleep quality through proper sleep hygiene may have great potential to improve these measured outcomes.
Cardiopulmonary Function
In a study that examined sleep deprivation in younger athletes, 17- to 18-year-old male volleyball players and runners in the sleep-deprived cohort demonstrated shorter time to exhaustion and decreased exercise ventilation, but no cardiac function changes compared with controls. 3 Other studies, performed using adult athletes as samples, suggest that sleep deprivation associated with endurance events increases athletes’ perceived exertion and impairs cognitive performance, mood, and general wellbeing, but does not alter physiologic performance.22,36,46
Recovery
There is little information in the literature regarding the biochemical and physiologic processes of recovery in the pediatric population; however, within the adult medical literature, sleep is known to play a critical role in the regenerative process during recovery. 96 Without adequate sleep after exertion, athletes may experience impaired muscle recovery, decreased glycogen storage, decreased power and endurance, and increased soreness.23,66,84 Interestingly, sleep deprivation secondary to early morning rising may cause greater detriment to anaerobic performance than late bedtime.85,86 In addition, a positive association was found between subjective recovery and total sleep time, sleep-wake patterns, and time off from exercise. 43
Interventions
Napping
One study reported that positive performance gains were found in simple gross motor skill acquisition after napping. 64 However, napping has not been found to be advantageous in offsetting the performance effects of jet lag or in endurance racing, running economy, or complex gross motor skill acquisition.34,42,71 Data regarding napping as an intervention for sleep deprived teenage athletes are scarce.
Sleep Extension
Extending sleep hours above habitual baseline levels may improve athletic motor performance and decrease perceived sleepines.56,84 Sleep extension may counter the effects of sleep deprivation if used either before the deprivation event or after to facilitate recovery. 1 Nevertheless, tapering exertion before a competition may decrease sleep quality (slow-wave sleep) and have a negative effect on an athlete’s mood, which may affect overall performance; therefore, conclusions should be carefully drawn.
Summary and Future Directions in Sleep Research
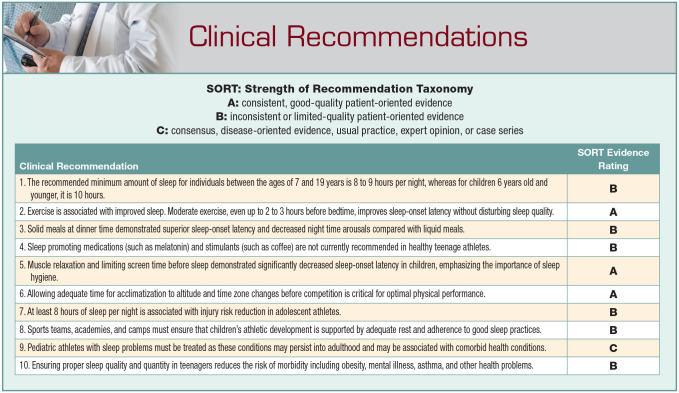
Exercise is associated with improved sleep by altering many factors; for example, by shortening sleep-onset latency. Interestingly, recent studies have demonstrated moderate exercise 2 to 3 hours before bedtime in teenagers seemed to improve sleep-onset latency without disturbing quality of sleep.25,65 Solid meals at dinner time demonstrated superior sleep-onset latency compared with liquids with equivalent carbohydrate content, with low-glycemic-index content showing fewer night time arousals than high-glycemic-index consumption.37,68 Sleep-promoting medications, such as standard doses of melatonin, compared with placebo, had no statistically significant effect on quality or quantity of sleep or physical performance 2 ; however, this has only been demonstrated in adults. Regular use of melatonin, or stimulants such as coffee, is not currently recommended in healthy teenagers. Muscle relaxation and limiting screen time demonstrated a statistically significant decrease in sleep-onset latency in children, 53 emphasizing the importance of sleep hygiene over pharmaceutical agents. Allowing adequate time for acclimation to altitude and time zone changes before competition is also important for optimal performance. At least 8 hours of sleep per night is associated with injury risk reduction in teenage athletes. 62 It is important for healthcare providers to take an adequate sleep history (Tables 1 and 2) and provide education on healthy sleep guidelines. If a sleep disorder is suspected or identified in a pediatric patient, referral to a sleep specialist for further evaluation and treatment may be warranted (Table 3).
Educators, trainers, physical therapists, parents, and clinicians must be a part of the effort to optimize sleep in teenage athletes. Sports camps, traveling teams, and academies must ensure that children’s academic and athletic development are supported by adequate rest. Monitoring mechanisms should be in place to help implement and ensure athlete adherence to good sleep practices. Teenage athletes with sleep problems must be identified and treated as these conditions may persist into adulthood and are associated with a variety of comorbid physical and mental health conditions. 19
Limitations
Part of the available data and conclusions regarding athletes and sleep are drawn from adult studies. Furthermore, there is a general lack of rigor in available pediatric studies, as most were nonrandomized, lacked control groups, were case studies, or had small sample sizes, and were therefore difficult to generalize to children and adolescents, let alone teenage athletes. Many subjects surrounding lack of sleep and sleep improvement in teenage athletes have not been thoroughly studied and, therefore leave room for future research.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1.Arnal PJ, Lapole T, Erblang M, et al. Sleep extension before sleep loss: effects on performance and neuromuscular function. Med Sci Sports Exerc. 2016;48:1595-1603. [DOI] [PubMed] [Google Scholar]
- 2.Atkinson G, Buckley P, Edwards B, et al. Are there hangover-effects on physical performance when melatonin is ingested by athletes before nocturnal sleep? Int J Sports Med. 2001;22:232-234. [DOI] [PubMed] [Google Scholar]
- 3.Azboy O, Kaygisiz Z. Effects of sleep deprivation on cardiorespiratory functions of the runners and volleyball players during rest and exercise. Acta Physiol Hung. 2009;96:29-36. [DOI] [PubMed] [Google Scholar]
- 4.Beaumont M, Batejat D, Pierard C, et al. Zaleplon and zolpidem objectively alleviate sleep disturbances in mountaineers at a 3,613 meter altitude. Sleep. 2007;30:1527-1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ben Cheikh R, Latiri I, Dogui M, et al. Effects of one-night sleep deprivation on selective attention and isometric force in adolescent karate athletes. J Sports Med Phys Fitness. 2017;57:752-759. [DOI] [PubMed] [Google Scholar]
- 6.Benjamin CL, Curtis RM, Huggins RA, et al. sleep dysfunction and mood in collegiate soccer athletes. Sports Health. 2020;12:234-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benjamin HJ, Boniquit NT, Hastings ES. The traveling athlete. Adolesc Med State Art Rev. 2015;26:189-207. [PubMed] [Google Scholar]
- 8.Blake MJ, Sheeber LB, Youssef GJ, et al. Systematic review and meta-analysis of adolescent cognitive-behavioral sleep interventions. Clin Child Fam Psychol Rev. 2017;20:227-249. [DOI] [PubMed] [Google Scholar]
- 9.Blumert PA, Crum AJ, Ernsting M, et al. The acute effects of twenty-four hours of sleep loss on the performance of national-caliber male collegiate weightlifters.J Strength Cond Res. 2007;21:1146-1154. [DOI] [PubMed] [Google Scholar]
- 10.Bonnet MH, Arand DL. Caffeine use as a model of acute and chronic insomnia. Sleep. 1992;15:526-536. [PubMed] [Google Scholar]
- 11.Brand S, Beck J, Gerber M, et al. Evidence of favorable sleep-EEG patterns in adolescent male vigorous football players compared to controls. World J Biol Psychiatry. 2010;11:465-475. [DOI] [PubMed] [Google Scholar]
- 12.Bruce ES, Lunt L, McDonagh JE. Sleep in adolescents and young adults. Clin Med (Lond). 2017;17:424-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carskadon MA. Sleep and circadian rhythms in children and adolescents: relevance for athletic performance of young people. Clin Sports Med. 2005;24:319-328, x. [DOI] [PubMed] [Google Scholar]
- 14.Chang SP, Chen YH. Relationships between sleep quality, physical fitness and body mass index in college freshmen. J Sports Med Phys Fitness. 2015;55:1234-1241. [PubMed] [Google Scholar]
- 15.Chen T, Wu Z, Shen Z, et al. Sleep duration in Chinese adolescents: biological, environmental, and behavioral predictors. Sleep Med. 2014;15:1345-1353. [DOI] [PubMed] [Google Scholar]
- 16.Committee on Nutrition and the Council on Sports Medicine Fitness. Sports drinks and energy drinks for children and adolescents: are they appropriate? Pediatrics. 2011;127:1182-1189. [DOI] [PubMed] [Google Scholar]
- 17.Conklin AI, Yao CA, Richardson CG. Chronic sleep disturbance, not chronic sleep deprivation, is associated with self-rated health in adolescents. Prev Med. 2019;124:11-16. [DOI] [PubMed] [Google Scholar]
- 18.Copenhaver EA, Diamond AB. The value of sleep on athletic performance, injury, and recovery in the young athlete. Pediatr Ann. 2017;46:e106-e111. [DOI] [PubMed] [Google Scholar]
- 19.Covassin T, Elbin RJ, III, Larson E, et al. Sex and age differences in depression and baseline sport-related concussion neurocognitive performance and symptoms. Clin J Sport Med. 2012;22:98-104. [DOI] [PubMed] [Google Scholar]
- 20.Dagan Y, Ayalon L. Case study: psychiatric misdiagnosis of non-24-hours sleep-wake schedule disorder resolved by melatonin. J Am Acad Child Adolesc Psychiatry. 2005;44:1271-1275. [DOI] [PubMed] [Google Scholar]
- 21.Daniel LC, Boergers J, Kopel SJ, et al. Missed sleep and asthma morbidity in urban children. Ann Allergy Asthma Immunol. 2012;109:41-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis GR, Etheredge CE, Marcus L, et al. Prolonged sleep deprivation and continuous exercise: effects on melatonin, tympanic temperature, and cognitive function. Biomed Res Int. 2014;2014:781863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duffield R, Murphy A, Kellett A, et al. Recovery from repeated on-court tennis sessions: combining cold-water immersion, compression, and sleep recovery interventions. Int J Sports Physiol Perform. 2014;9:273-282. [DOI] [PubMed] [Google Scholar]
- 24.Falbe J, Davison KK, Franckle RL, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics. 2015;135:e367-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flausino NH, Da Silva Prado JM, de Queiroz SS, et al. Physical exercise performed before bedtime improves the sleep pattern of healthy young good sleepers. Psychophysiology. 2012;49:186-192. [DOI] [PubMed] [Google Scholar]
- 26.Fullagar HH, Duffield R, Skorski S, et al. Sleep, travel, and recovery responses of national footballers during and after long-haul international air travel. Int J Sports Physiol Perform. 2016;11:86-95. [DOI] [PubMed] [Google Scholar]
- 27.Fullagar H, Skorski S, Duffield R, et al. The effect of an acute sleep hygiene strategy following a late-night soccer match on recovery of players. Chronobiol Int. 2016;33:490-505. [DOI] [PubMed] [Google Scholar]
- 28.Fullagar HH, Skorski S, Duffield R, et al. Impaired sleep and recovery after night matches in elite football players. J Sports Sci. 2016;34:1333-1339. [DOI] [PubMed] [Google Scholar]
- 29.Gao B, Dwivedi S, Milewski MD, et al. Lack of sleep and sports injuries in adolescents: a systematic review and meta-analysis. J Pediatr Orthop. 2019;39:e324-e333. [DOI] [PubMed] [Google Scholar]
- 30.Geiker NRW, Astrup A, Hjorth MF, et al. Does stress influence sleep patterns, food intake, weight gain, abdominal obesity and weight loss interventions and vice versa? Obes Rev. 2018;19:81-97. [DOI] [PubMed] [Google Scholar]
- 31.Gerber M, Brand S, Herrmann C, et al. Increased objectively assessed vigorous-intensity exercise is associated with reduced stress, increased mental health and good objective and subjective sleep in young adults. Physiol Behav. 2014;135:17-24. [DOI] [PubMed] [Google Scholar]
- 32.Graves JM, Miller ME. Reduced sleep duration and history of work-related injuries among Washington State adolescents with a history of working. Am J Ind Med. 2015;58:464-471. [DOI] [PubMed] [Google Scholar]
- 33.Halson SL. Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med. 2014;44 (Suppl. 1):S13-S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoedlmoser K, Birklbauer J, Schabus M, et al. The impact of diurnal sleep on the consolidation of a complex gross motor adaptation task. J Sleep Res. 2015;24:100-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoshikawa M, Uchida S, Sugo T, et al. Changes in sleep quality of athletes under normobaric hypoxia equivalent to 2,000-m altitude: a polysomnographic study.J Appl Physiol (1985). 2007;103:2005-2011. [DOI] [PubMed] [Google Scholar]
- 36.Hurdiel R, Peze T, Daugherty J, et al. Combined effects of sleep deprivation and strenuous exercise on cognitive performances during The North Face(R) Ultra Trail du Mont Blanc(R) (UTMB(R)). J Sports Sci. 2015;33:670-674. [DOI] [PubMed] [Google Scholar]
- 37.Jalilolghadr S, Afaghi A, O’Connor H, et al. Effect of low and high glycaemic index drink on sleep pattern in children. J Pak Med Assoc. 2011;61:533-536. [PubMed] [Google Scholar]
- 38.Jarraya S, Jarraya M, Chtourou H, et al. Effect of time of day and partial sleep deprivation on the reaction time and the attentional capacities of the handball goalkeeper. Biol Rhythm Res. 2014;45:183-191. [Google Scholar]
- 39.Johnson PL, Edwards N, Burgess KR, et al. Sleep architecture changes during a trek from 1400 to 5000 m in the Nepal Himalaya. J Sleep Res. 2010;19:148-156. [DOI] [PubMed] [Google Scholar]
- 40.Kalak N, Gerber M, Kirov R, et al. Daily morning running for 3 weeks improved sleep and psychological functioning in healthy adolescents compared with controls. J Adolesc Health. 2012;51:615-622. [DOI] [PubMed] [Google Scholar]
- 41.Kim SY, Sim S, Kim SG, et al. Sleep deprivation is associated with bicycle accidents and slip and fall injuries in Korean adolescents. PLoS One. 2015;10:e0135753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Knechtle B, Wirth A, Knechtle P, et al. A comparison of ultra-endurance cyclists in a qualifying ultra-cycling race for Paris-Brest-Paris and Race Across America-Swiss cycling marathon. Percept Mot Skills. 2012;114:96-110. [DOI] [PubMed] [Google Scholar]
- 43.Kolling S, Steinacker JM, Endler S, et al. The longer the better: sleep-wake patterns during preparation of the World Rowing Junior Championships. Chronobiol Int. 2016;33:73-84. [DOI] [PubMed] [Google Scholar]
- 44.Kostyun RO, Milewski MD, Hafeez I. Sleep disturbance and neurocognitive function during the recovery from a sport-related concussion in adolescents. Am J Sports Med. 2015;43:633-640. [DOI] [PubMed] [Google Scholar]
- 45.Lastella M, Roach GD, Halson SL, et al. The effects of transmeridian travel and altitude on sleep: preparation for football competition. J Sports Sci Med. 2014;13:718-720. [PMC free article] [PubMed] [Google Scholar]
- 46.Lastella M, Roach GD, Halson SL, et al. The impact of a simulated grand tour on sleep, mood, and well-being of competitive cyclists. J Sports Med Phys Fitness. 2015;55:1555-1564. [PubMed] [Google Scholar]
- 47.Lastella M, Roach GD, Halson SL, et al. Sleep/wake behaviour of endurance cyclists before and during competition. J Sports Sci. 2015;33:293-299. [DOI] [PubMed] [Google Scholar]
- 48.Lastella M, Roach GD, Halson SL, et al. Sleep/wake behaviours of elite athletes from individual and team sports. Eur J Sport Sci. 2015;15:94-100. [DOI] [PubMed] [Google Scholar]
- 49.Lastella M, Roach GD, Vincent GE, et al. The impact of training load on sleep during a 14-day training camp in elite, adolescent, female basketball players. Int J Sports Physiol Perform. 2020;15:724-730. [DOI] [PubMed] [Google Scholar]
- 50.Lentino CV, Purvis DL, Murphy KJ, et al. Sleep as a component of the performance triad: the importance of sleep in a military population. US Army Med Dep J. 2013:98-108. [PubMed] [Google Scholar]
- 51.Lewandowski AS, Palermo TM, De la Motte S, et al. Temporal daily associations between pain and sleep in adolescents with chronic pain versus healthy adolescents. Pain. 2010;151:220-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Luke A, Lazaro RM, Bergeron MF, et al. Sports-related injuries in youth athletes: is overscheduling a risk factor? Clin J Sport Med. 2011;21:307-314. [DOI] [PubMed] [Google Scholar]
- 53.McCloughan LJ, Hanrahan SJ, Anderson R, et al. Psychological recovery: Progressive muscle relaxation (PMR), anxiety, and sleep in dancers. Perform Enhanc Health. 2016;4:12-17. [Google Scholar]
- 54.McClure DJ, Zuckerman SL, Kutscher SJ, et al. Baseline neurocognitive testing in sports-related concussions: the importance of a prior night’s sleep. Am J Sports Med. 2014;42:472-478. [DOI] [PubMed] [Google Scholar]
- 55.McLaughlin Crabtree V, Williams NA. Normal sleep in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2009;18:799-811. [DOI] [PubMed] [Google Scholar]
- 56.Mah CD, Mah KE, Kezirian EJ, et al. The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep. 2011;34:943-950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Manfredini R, Manfredini F, Conconi F. Standard melatonin intake and circadian rhythms of elite athletes after a transmeridian flight. J Int Med Res. 2000;28:182-186. [DOI] [PubMed] [Google Scholar]
- 58.Martiniuk AL, Senserrick T, Lo S, et al. Sleep-deprived young drivers and the risk for crash: the DRIVE prospective cohort study. JAMA Pediatr. 2013;167:647-655. [DOI] [PubMed] [Google Scholar]
- 59.Maruyama T, Sato S, Matsumura M, et al. Evaluations of effects of sleep surfaces on athletic performance in youth. Sci Rep. 2020;10:11805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mathias JL, Alvaro PK. Prevalence of sleep disturbances, disorders, and problems following traumatic brain injury: a meta-analysis. Sleep Med. 2012;13:898-905. [DOI] [PubMed] [Google Scholar]
- 61.Mihalik JP, Lengas E, Register-Mihalik JK, et al. The effects of sleep quality and sleep quantity on concussion baseline assessment. Clin J Sport Med. 2013;23:343-348. [DOI] [PubMed] [Google Scholar]
- 62.Milewski MD, Skaggs DL, Bishop GA, et al. Chronic lack of sleep is associated with increased sports injuries in adolescent athletes. J Pediatr Orthop. 2014;34:129-133. [DOI] [PubMed] [Google Scholar]
- 63.Miller KE, Dermen KH, Lucke JF. Caffeinated energy drink use by U.S. adolescents aged 13-17: a national profile. Psychol Addict Behav. 2018;32:647-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Morita Y, Ogawa K, Uchida S. The effect of a daytime 2-hour nap on complex motor skill learning. Sleep Biol Rhythms. 2012;10:302-309. [Google Scholar]
- 65.Myllymaki T, Kyrolainen H, Savolainen K, et al. Effects of vigorous late-night exercise on sleep quality and cardiac autonomic activity. J Sleep Res. 2011;20:146-153. [DOI] [PubMed] [Google Scholar]
- 66.Nedelec M, Halson S, Abaidia AE, et al. Stress, sleep and recovery in elite soccer: a critical review of the literature. Sports Med. 2015;45:1387-1400. [DOI] [PubMed] [Google Scholar]
- 67.Nedelec M, Halson S, Delecroix B, et al. Sleep hygiene and recovery strategies in elite soccer players. Sports Med. 2015;45:1547-1559. [DOI] [PubMed] [Google Scholar]
- 68.Orr WC, Shadid G, Harnish MJ, et al. Meal composition and its effect on postprandial sleepiness. Physiol Behav. 1997;62:709-712. [DOI] [PubMed] [Google Scholar]
- 69.Owens JA, Fernando S, Mc Guinn M. Sleep disturbance and injury risk in young children. Behav Sleep Med. 2005;3:18-31. [DOI] [PubMed] [Google Scholar]
- 70.Parcell DL, Ponsford JL, Redman JR, et al. Poor sleep quality and changes in objectively recorded sleep after traumatic brain injury: a preliminary study. Arch Phys Med Rehabil. 2008;89:843-850. [DOI] [PubMed] [Google Scholar]
- 71.Petit E, Mougin F, Bourdin H, et al. A 20-min nap in athletes changes subsequent sleep architecture but does not alter physical performances after normal sleep or 5-h phase-advance conditions. Eur J Appl Physiol. 2014;114:305-315. [DOI] [PubMed] [Google Scholar]
- 72.Potter MN, Howell DR, Dahab KS, et al. Sleep quality and quality of life among healthy high school athletes. Clin Pediatr (Phila). 2020;59:170-177. [DOI] [PubMed] [Google Scholar]
- 73.Richmond LK, Dawson B, Stewart G, et al. The effect of interstate travel on the sleep patterns and performance of elite Australian Rules footballers. J Sci Med Sport. 2007;10:252-258. [DOI] [PubMed] [Google Scholar]
- 74.Robey E, Dawson B, Halson S, et al. Sleep quantity and quality in elite youth soccer players: a pilot study. Eur J Sport Sci. 2014;14:410-417. [DOI] [PubMed] [Google Scholar]
- 75.Romyn G, Robey E, Dimmock JA, et al. Sleep, anxiety and electronic device use by athletes in the training and competition environments. Eur J Sport Sci. 2016;16:301-308. [DOI] [PubMed] [Google Scholar]
- 76.Salinero JJ, Lara B, Abian-Vicen J, et al. The use of energy drinks in sport: perceived ergogenicity and side effects in male and female athletes. Br J Nutr. 2014;112:1494-1502. [DOI] [PubMed] [Google Scholar]
- 77.Samuels C, James L, Lawson D, et al. The Athlete Sleep Screening Questionnaire: a new tool for assessing and managing sleep in elite athletes. Br J Sports Med. 2016;50:418-422. [DOI] [PubMed] [Google Scholar]
- 78.Sargent C, Halson S, Roach GD. Sleep or swim? Early-morning training severely restricts the amount of sleep obtained by elite swimmers. Eur J Sport Sci. 2014;14 (Suppl. 1):S310-S315. [DOI] [PubMed] [Google Scholar]
- 79.Sargent C, Roach GD. Sleep duration is reduced in elite athletes following night-time competition. Chronobiol Int. 2016;33:667-670. [DOI] [PubMed] [Google Scholar]
- 80.Sargent C, Schmidt WF, Aughey RJ, et al. The impact of altitude on the sleep of young elite soccer players (ISA3600). Br J Sports Med. 2013;47 (Suppl. 1):i86-i92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shearer DA, Jones RM, Kilduff LP, et al. Effects of competition on the sleep patterns of elite rugby union players. Eur J Sport Sci. 2015;15:681-686. [DOI] [PubMed] [Google Scholar]
- 82.Silverberg ND, Berkner PD, Atkins JE, et al. relationship between short sleep duration and preseason concussion testing. Clin J Sport Med. 2016;26:226-231. [DOI] [PubMed] [Google Scholar]
- 83.Simmons E, McGrane O, Wedmore I. Jet lag modification. Curr Sports Med Rep. 2015;14:123-128. [DOI] [PubMed] [Google Scholar]
- 84.Skein M, Duffield R, Minett GM, et al. The effect of overnight sleep deprivation after competitive rugby league matches on postmatch physiological and perceptual recovery. Int J Sports Physiol Perform. 2013;8:556-564. [DOI] [PubMed] [Google Scholar]
- 85.Souissi N, Chtourou H, Aloui A, et al. Effects of time-of-day and partial sleep deprivation on short-term maximal performances of judo competitors. J Strength Cond Res. 2013;27:2473-2480. [DOI] [PubMed] [Google Scholar]
- 86.Souissi N, Souissi M, Souissi H, et al. Effect of time of day and partial sleep deprivation on short-term, high-power output. Chronobiol Int. 2008;25:1062-1076. [DOI] [PubMed] [Google Scholar]
- 87.Sufrinko A, Johnson EW, Henry LC. The influence of sleep duration and sleep-related symptoms on baseline neurocognitive performance among male and female high school athletes. Neuropsychology. 2016;30:484-491. [DOI] [PubMed] [Google Scholar]
- 88.Sullivan KA, Edmed SL, Allan AC, et al. Characterizing self-reported sleep disturbance after mild traumatic brain injury. J Neurotrauma. 2015;32:474-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Suppiah HT, Low CY, Chia M. Effects of sport-specific training intensity on sleep patterns and psychomotor performance in adolescent athletes. Pediatr Exerc Sci. 2016;28:588-595. [DOI] [PubMed] [Google Scholar]
- 90.Taheri M, Arabameri E. The effect of sleep deprivation on choice reaction time and anaerobic power of college student athletes. Asian J Sports Med. 2012;3:15-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tarokh L, Raffray T, Van Reen E, et al. Physiology of normal sleep in adolescents. Adolesc Med State Art Rev. 2010;21:401-417, vii. [PubMed] [Google Scholar]
- 92.Taylor L, Chrismas BC, Dascombe B, et al. The importance of monitoring sleep within adolescent athletes: athletic, academic, and health considerations. Front Physiol. 2016;7:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Towns SJ, Silva MA, Belanger HG. Subjective sleep quality and postconcussion symptoms following mild traumatic brain injury. Brain Inj. 2015;29:1337-1341. [DOI] [PubMed] [Google Scholar]
- 94.Vardar SA, Ozturk L, Kurt C, et al. Sleep deprivation induced anxiety and anaerobic performance. J Sports Sci Med. 2007;6:532-537. [PMC free article] [PubMed] [Google Scholar]
- 95.Venancio DP, Tufik S, Garbuio SA, et al. Effects of anabolic androgenic steroids on sleep patterns of individuals practicing resistance exercise. Eur J Appl Physiol. 2008;102:555-560. [DOI] [PubMed] [Google Scholar]
- 96.Venter RE. Perceptions of team athletes on the importance of recovery modalities. Eur J Sport Sci. 2014;14 (Suppl. 1):S69-S76. [DOI] [PubMed] [Google Scholar]
- 97.von Rosen P, Frohm A, Kottorp A, et al. Too little sleep and an unhealthy diet could increase the risk of sustaining a new injury in adolescent elite athletes. Scand J Med Sci Sports. 2017;27:1364-1371. [DOI] [PubMed] [Google Scholar]
- 98.Vriend JL, Davidson FD, Corkum PV, et al. Manipulating sleep duration alters emotional functioning and cognitive performance in children. J Pediatr Psychol. 2013;38:1058-1069. [DOI] [PubMed] [Google Scholar]
- 99.Wall SP, Mattacola CG, Swanik CB, et al. Sleep efficiency and overreaching in swimmers. J Sport Rehabil. 2003;12:1-12. [Google Scholar]
- 100.Watson A, Brickson S. Impaired sleep mediates the negative effects of training load on subjective well-being in female youth athletes. Sports Health. 2018;10:244-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wheaton AG, Olsen EO, Miller GF, et al. Sleep duration and injury-related risk behaviors among high school students - United States, 2007-2013. MMWR Morb Mortal Wkly Rep. 2016;65:337-341. [DOI] [PubMed] [Google Scholar]
- 102.Zschoche M, Schlarb AA. Is there an association between insomnia symptoms, aggressive behavior, and suicidality in adolescents? Adolesc Health Med Ther. 2015;6:29-36. [DOI] [PMC free article] [PubMed] [Google Scholar]


