Abstract
Context:
Despite the well-known positive effects of exercise in hypertensive patients, the best mode of exercise is still under discussion.
Objective:
A systematic review of the literature, synthesizing data on the effects of high-intensity interval training (HIIT) on peak oxygen consumption (VO2 peak), blood pressure (BP), cardiac autonomic modulation, and resting heart rate (HR) in patients with hypertension.
Data Sources:
MEDLINE (via PubMed), CENTRAL, PEDro database, and SciELO (from the earliest date available to December 31, 2020).
Study Selection:
Randomized controlled trials (RCTs) that evaluated the effects of HIIT in hypertensive patients.
Study Design:
Systematic review and meta-analysis.
Level of Evidence:
Level 2.
Data Extraction:
Mean differences (MDs) with a 95% CI were calculated, and heterogeneity was assessed using the I2 test.
Results:
Nine RCTs encompassing 569 patients met the eligibility criteria and were included in the systematic review. Five trials compared supervised HIIT with moderate-intensity continuous training (MICT) and a control; 1 trial compared HIIT with MICT, and 3 compared HIIT with a control. In comparison with MICT, HIIT improved VO2 peak MD (3.3 mL.kg-1.min-1; 95% CI, 1.4-5.3; N = 130). In comparison with controls, HIIT improved VO2 peak MD (4.4 mL.kg-1.min-1; 95% CI, 2.5-6.2; N = 162).
Conclusion:
Despite the low quality of the evidence, HIIT is superior to MICT in improving VO2 peak in patients with hypertension. HIIT effectively improved VO2 peak, BP, and resting HR when compared with controls. HIIT appears to be safe only when performed in a supervised manner for stage 1 hypertension patients without associated risk factors.
Keywords: blood pressure, exercise, hypertension, rehabilitation
Hypertension is the most common, costly, and preventable cardiovascular disease risk factor. 35 Although progress has been observed in therapeutic approaches to hypertension, the prevalence of hypertension remains high and is a leading cause of cardiovascular disease.35,29
Because hypertension is a chronic condition needing long-term treatment, strategies with few side effects requiring less-invasive procedures should be developed. 38 The positive effects of various exercise protocols on the blood pressure (BP) of adults with and without hypertension have already been demonstrated.7,11,12,37
Hence, moderate-intensity continuous training (MICT: exercise with unchanged intensity [moderate intensity]) and high-intensity interval training (HIIT: exercise that alternates between high-intensity stimuli and recovery intervals [low intensity]) stand out among the different aerobic exercise training methods used for BP control.8,17,25,28
In addition, Leal et al, 28 in an elegant systematic review and meta-analysis, compared the effects of MICT and HIIT on the BP of hypertensive patients. They concluded that HIIT and MICT reduce the systolic blood pressure (SBP) in adults with hypertension, and HIIT reduced diastolic blood pressure (DBP) even further. However, they included studies on patients with other cardiovascular diseases. 28 Seemingly, no meta-analysis on the effects of HIIT in hypertensive subjects without other underlying cardiovascular diseases has been published.
According to Franklin, 10 for patients who are sedentary and/or not used to high-intensity exercises, HIIT can sharply increase the risk of sudden cardiac death and/or acute myocardial infarction with a known or hidden cardiovascular disease. Thus, safe HIIT practice should begin under supervision, involving patients at low cardiovascular risk (stage 1 hypertension without additional risk factors), with adequate physical fitness (basic functional and structural adaptation, arising from a low- to moderate-intensity physical exercise program).4,27 In this sense, hypertension (stage 1 with 3 or more risk factors; stage 2 with 1 or 2 risk factors; stage 3, regardless of any other risk factors) can characterize patients as at high risk of cardiovascular mortality. 4 Therefore, this study can provide further scientific input to professionals in the field regarding the benefits and safety of supervised HIIT with this population. The present systematic review and meta-analysis aimed to analyze published randomized controlled trials (RCTs) investigating the effects of HIIT on peak oxygen consumption (VO2 peak), BP, cardiac autonomic modulation, and resting heart rate (HR) in patients with hypertension without other underlying cardiovascular diseases.
Methods
Eligibility Criteria
This systematic review was completed following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 32
The review included RCTs that studied the effects of HIIT compared with MICT or control (no exercise) in patients with hypertension. Studies were considered eligible for this systematic review if they (1) included adult patients (aged ≥18 years) with hypertension (SBP >130 and/or DBP >80 mmHg) and without other underlying cardiovascular diseases; (2) used a randomized controlled clinical trial design; (3) compared HIIT with either MICT or a control (no exercise); (4) performed interventions for at least 4 weeks. Studies that recruited patients with other cardiac or respiratory diseases were excluded. The outcomes of interest were the peak oxygen consumption (VO2 peak [in mL.kg-1.min-1]), cardiac autonomic modulation, BP, and HR.
Search Strategy for Identification of Studies
References were searched for in MEDLINE (via PubMed), Cochrane Central Register of Controlled Trials (CENTRAL), Physiotherapy Evidence Database (PEDro), and Scientific Electronic Library Online (SciELO) up to December 2020 without language restrictions. This systematic search used a standard protocol and, whenever possible, a controlled vocabulary (MeSH terms for PubMed and Cochrane). The search strategy employed 3 groups of keywords and their synonyms: study research design, patients, and interventions. The strategy developed by Higgins et al 22 was used to identify RCTs in PubMed, as shown in Appendix Table A1 (available in the online version of this article). RCTs in other databases were identified using a search strategy involving similar MeSH terms. The bibliographies of the studies included in the present systematic review were checked to identify other potentially eligible studies.
Data Collection and Analysis
Two reviewers independently checked titles and abstracts. If ≥1 reviewer considered a study eligible, the full text was obtained for a complete assessment. Then, 2 reviewers independently assessed the full text of selected studies to ascertain whether they met the eligibility criteria, and 2 authors independently extracted data from the published reports using standard data extraction forms adapted from Higgins et al. 22 The following aspects were reviewed in the studies: hypertensive population, intervention (HIIT vs MICT), outcome measures, and results.
Quality of Meta-analysis Evidence
The quality of the studies was scored by 2 authors using the PEDro scale, which is based on important criteria, such as concealed allocation, intention-to-treat analysis, blinding, and adequacy of follow-up. 30
Summary of Findings Table
The quality of evidence for VO2 peak, BP, and resting HR was assessed with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE). 18 GRADEpro GDT 2015 was used to import data from the Review Manager and to create a Summary of Findings table. 19 We used the 5 GRADE items (study limitations, consistency of effect, imprecision, indirectness, and publication bias) used to assess the quality of a body of evidence provided by studies that contribute with data to a meta-analysis. 22 Decisions to downgrade the quality of studies were justified in footnotes, and comments were made to help readers understand the review when necessary.22,19
Statistical Assessment
Pooled-effect estimates were obtained by comparing the changes in least-square means from baseline to endpoint for each group and were expressed as the weighted mean difference (MD) between groups. For continuous variables, results were expressed as the MD of change in the variables between randomized groups. Conversion of nonparametric data to means and SD was based on recently established methods. 42 When the CI but not the SD of change was available, the CI was converted into an SD, as recommended by Higgins et al, 22 and calculations were made using fixed- and random-effects models. Data from multiarm RCTs were extracted regarding all relevant experimental intervention groups (HIIT vs MICT) and the control group. In follow-up reports with multiple endpoints, only data closest to the end of the exercise program were included. In crossover trials, effect sizes were extracted only at the first crossover point.
Two comparisons were made: (1) HIIT versus MICT; and (2) HIIT versus control (no exercise). Significance was set at α < 0.05. Heterogeneity among studies was examined using Cochran’s Q test and I2, with values greater than 40% considered indicative of a high degree of heterogeneity 21 ; then, the random-effects model was selected. Analyses were conducted using Review Manager (Version 5.3). 6
Ethical Approval
Ethical approval was not necessary because only publicly accessible records were used, without any contact with individual participants.
Results
Description of Selected Studies
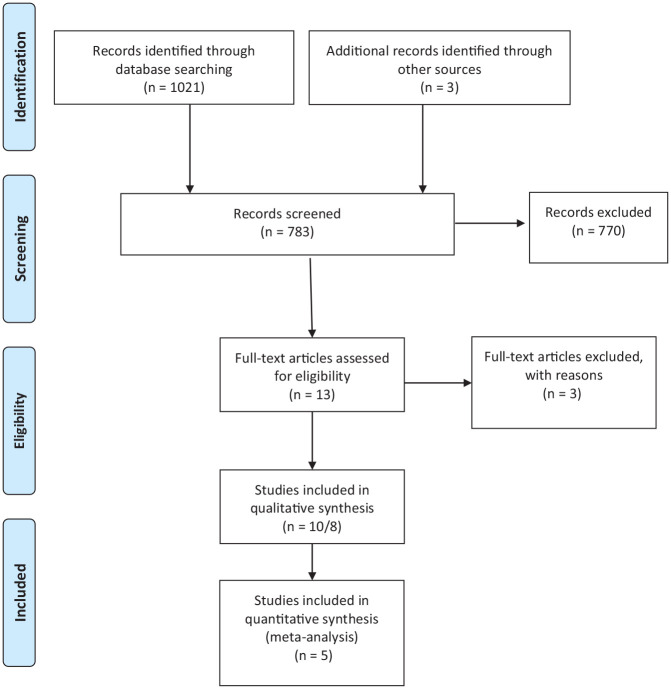
The initial search led to the identification of 1430 abstracts, from which 14 studies were considered potentially relevant and retrieved for detailed analysis. Three studies were excluded after reading the full text of the 14 papers. Of the remaining 11 studies,1,2,15,16,23,24,31,33, 34 ,39,41 2 were duplicates, ie, studies involving the same participants. The study by Aguirre-Betolaza et al 2 used the same participants as the study by Gorostegi-Anduaga et al, 15 and the study by Soltani et al 39 used the same participants as the study by Aghaei Bahmanbeglou et al 1 . These 2 pairs were thus treated as 2 single studies. In all, 9 studies finally met the eligibility criteria.1,15,16,23,24,31,33,34,41Figure 1 shows the PRISMA flow diagram of studies used in the present review. Both authors scored all studies using the PEDro scale methodology, whose results are presented individually in Appendix Table A2, available online. Following the Cochrane guidelines, 6 a study by Gui 16 was included, even though the full version of the text was unavailable. Consecutive emails requesting the full version of the text were sent, but none were answered.
Figure 1.
Flow diagram showing reference screening and study selection.
Study Characteristics
The number of participants randomized in the studies included in this meta-analysis ranged from 30 to 163, with a mean age ranging from 40 to 65 years. Four studies included patients of both sexes,15,23,24,34 while 1 included only males, 1 2 included only females,33,41 and 2 did not report the sex of participants.16,31 The sample sizes, outcomes, and results of the studies are summarized in Appendix Table A3, available online. The HIIT characteristics were reported in most of the 9 studies included (Appendix Table A4, available online). Of these 9 studies, 5 compared HIIT with MICT and with the control (no exercise),15,24,33,34,41 1 study compared HIIT with MICT, 16 and 3 studies compared HIIT with the control.1,23,31
Effects of HIIT Compared With Those of MICT
VO2 peak
Three studies assessed the VO2 peak as an outcome.15,24,34 The total number of patients in the HIIT group was 87, while 86 patients were included in the MICT group. The HIIT studies showed a baseline average of 27.8 mL.kg-1.min-1 and a postintervention average of 35.2 mL.kg-1.min-1. The MICT studies showed a baseline average of 26.1 mL.kg-1.min-1 and a postintervention average of 29.7 mL.kg-1. min-1. There was no strong evidence of a difference in VO2 peak between HIIT and MICT analyzing the individual findings of all studies. The meta-analysis (Figure 2A) showed a significant improvement of 2.7 mL.kg-1.min-1 (95% CI, 0.9-4.4; N = 173) for participants in the HIIT group compared with those in the MICT group.
Figure 2.
HIIT versus MICT changes in outcomes VO2 peak, SBP, DBP, and resting HR. Review Manager (RevMan). Version 5.3 The Cochrane Collaboration, 2013. DPB, diastolic blood pressure, HIIT, high-intensity interval training; HR, heart rate; IV, inverse variance; MICT, moderate-intensity continuous training; SBP, systolic blood pressure; VO2 peak, peak oxygen consumption.
Systolic Blood Pressure
Three studies assessed SBP as an outcome.15,33,34 The total number of patients in the HIIT group was 88, while 84 patients were included in the MICT group. The meta-analysis (Figure 2B) showed a nonsignificant difference in SBP of -1.8 mmHg (95% CI, -5.8 to 2.3; N = 172) for participants in the HIIT group compared with those in the MICT group.
Diastolic Blood Pressure
Two studies assessed DBP as an outcome.15,34 The total number of patients in the HIIT group was 67, and 63 patients were included in the MICT group. The meta-analysis (Figure 2C) showed a nonsignificant difference in DBP of -3.8 mmHg (95% CI, -8.8 to 1.2; N = 130) for participants in the HIIT group compared with those in the MICT group.
Resting HR
Three studies assessed resting HR as an outcome.15,33,34 The total number of patients in the HIIT group was 88, while 84 patients were included in the MICT group. The meta-analysis (Figure 2D) showed a nonsignificant difference in resting HR of -0.7 beats per minute (bpm) (95% CI, -2.5 to 1.1; N = 172) for participants in the HIIT group compared with those in the MICT group.
Effects of HIIT Versus Control
VO2 peak
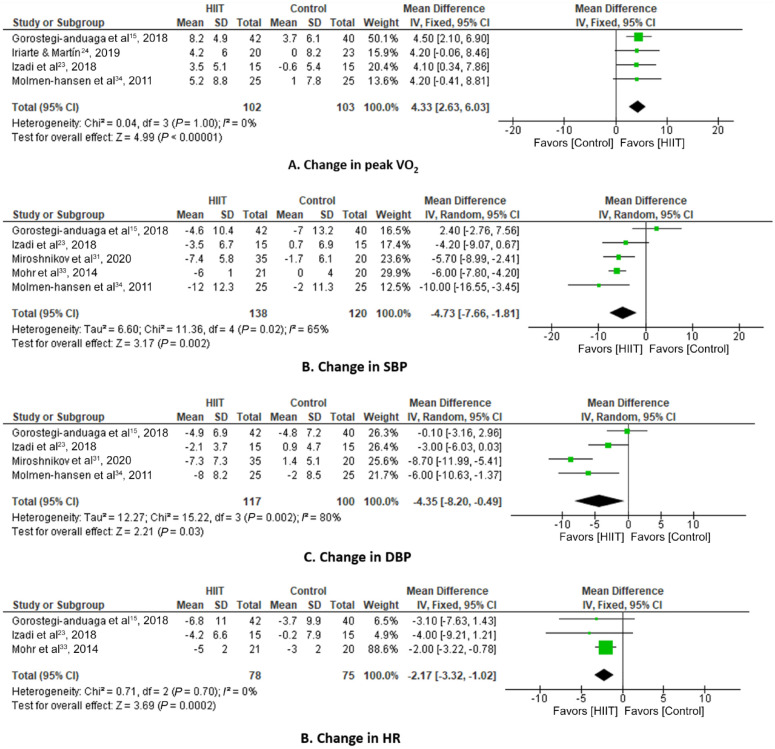
Four studies assessed VO2 peak as an outcome.15,23,24,34 The total number of patients in the HIIT group was 102, while 103 patients were included in the control group. The HIIT studies showed a baseline average of 27.8 mL.kg-1.min-1 and a postintervention average of 35.2 mL.kg-1.min-1. The control group studies showed a baseline average of 28.6 mL.kg-1.min-1 and a postintervention average of 29.6 mL.kg-1.min-1. The meta-analysis (Figure 3A) showed a statistically significant improvement of 4.3 mL.kg-1.min-1 (95% CI, 2.6-6.0; N = 205) for participants in the HIIT group compared with those in the control group.
Figure 3.
HIIT versus control changes in outcomes VO2 peak, SBP, DBP, resting HR. Review Manager (RevMan). Version 5.3 The Cochrane Collaboration, 2013. DPB, diastolic blood pressure, HIIT, high-intensity interval training; HR, heart rate; IV, inverse variance; MICT, moderate-intensity continuous training; SBP, systolic blood pressure; VO2 peak, peak oxygen consumption.
Systolic Blood Pressure
Five studies assessed SBP as an outcome.15,23,31,33,34 The total number of patients in the HIIT group was 138, while 120 patients were included in the control group. The HIIT studies showed a baseline average of 138.3 mmHg and a postintervention average of 131.8 mmHg. The control group studies showed a baseline average of 139.5 mmHg and a postintervention average of 137.3 mmHg. The meta-analysis (Figure 3B) showed a significant reduction in SBP of -4.7 mmHg (95% CI, -7.7 to -1.8; N = 258) for participants in the HIIT group compared with those in the control group.
Diastolic Blood Pressure
Four studies assessed DBP as an outcome.15,23,31,34 The total number of patients in the HIIT group was 117, while 100 patients were included in the control group. The meta-analysis (Figure 3C) showed a significant reduction in DBP of -4.4 mmHg (95% CI, -8.2 to -0.5; N = 217) for participants in the HIIT group compared with those in the control group.
Resting HR
Three studies assessed resting HR as an outcome.15,23,33 The total number of patients in the HIIT group was 78, whereas 75 patients were included in the control group. The meta-analysis (Figure 3D) showed a significant reduction in resting HR of -2.2 bpm (95% CI, -2.3 to -1.0; N = 153) for participants in the HIIT group compared with those in the control group.
Cardiac Autonomic Modulation
Aguirre-Betolaza et al 2 examined the effects of 16 weeks of practicing different aerobic training programs on cardiac autonomic modulation and hemodynamics in patients with hypertension. Participants were randomly assigned to an attention control (AC) group (physical activity recommendations) or 1 of 3 supervised exercise training groups: high-volume MICT, high-volume HIIT, and low-volume HIIT. After the intervention, the HR, SBP, and DBP at rest and during submaximal exercise, and the diurnal and nocturnal SBP and DBP values decreased (P < 0.05) in all groups with no differences between them. When the exercise training groups were combined, submaximal SBP (P = 0.05) and DBP (P = 0.004), VO2 peak (P = 0.01), and HR reserve (P = 0.03) were significantly improved compared with AC. Moreover, they concluded that the greatest improvements in autonomic function were found when the aerobic training was individually designed and supervised, irrespective of intensity and volume of exercise. 2
GRADE Assessments
The GRADE assessments are presented in the Summary of Findings Table A5 and A6 (Appendix, available online). Compared with MICT (Table A5), the quality of evidence for the VO2 peak was assessed as high; for SBP, low; and for DPB and resting HR, moderate. Compared with the control (Table A6), the quality of evidence for the VO2 peak was assessed as high; for SBP and DBP, low; and for resting HR, moderate.
Discussion
The main findings of the present study indicate that supervised HIIT improved VO2 peak more effectively than MICT in patients with hypertension (stage 1 and stage 2). However, we cannot claim that HIIT is completely safe for hypertensive patients with an elevated risk of cardiovascular mortality (hypertension; stage 1 with ≥3 risk factors; stage 2 with 1 or 2 risk factors; stage 3 regardless of other risk factors).
In summary, supervised HIIT effectively increases VO2 peak in stage 1 and stage 2 hypertensive patients during a short-term exercise program. The quality of evidence for the VO2 peak was assessed as high. The degree of improvement in VO2 peak with HIIT was approximately 2 times greater than with MICT and 5 times greater than in control groups. Thus, the strength of this study is that we included a VO2peak, which is an important outcome associated with prognosis in patients with hypertension.9,26 Faselis et al 9 found an inverse relationship between exercise capacity and progression from prehypertension to hypertension. There was also a significant negative correlation between BP and VO2 peak. 5
It is well established by previous meta-analyses that regular aerobic exercise is an effective strategy to reduce clinical BP measurements in normotensive, prehypertensive, and hypertensive adults. 28 However, in this study, although HIIT improved SBP when compared with control, the quality of evidence was low for SBP and DBP and moderate for resting HR. From a public health perspective, there is strong evidence to support that reduced SBP is linearly associated with a lower risk of cardiovascular morbidity and mortality in adults with hypertension.7,20,24,29,38 For instance, a reduction of 10 mmHg in SBP or 4 mmHg in DBP is associated with approximately 30% lower risk of stroke and approximately 20% lower risk of myocardial infarction. 40
The results of this meta-analysis concur with those of previous systematic reviews that compared the effects of HIIT and MICT on the VO2 peak in patients with heart disease.13,14 HIIT may improve peak oxygen uptake and should be considered as a component of care in the treatment of patients with cardiovascular disease with caution for those with underlying heart disease. 36 Recently, Hannan et al 20 published a systematic review and meta-analysis that investigated cardiorespiratory fitness changes resulting from HIIT or MICT in a population of patients with heart disease. They concluded that supervised HIIT performed better than MICT in improving cardiorespiratory fitness and that it is as safe as MICT for cardiac rehabilitation participants.18,20
Despite the favorable results, strategies to increase participation and adherence to HIIT in hypertensive patients are essential to maintain and improve their exercise capacity and BP. 3 It is also important to acknowledge the barriers to the implementation of a physical exercise program in this population. 36
Study Limitations
The results of this systematic review are limited by the lack of multicenter, high-quality, long-term studies. This highlights the paucity of high-quality research comparing HIIT and MICT in patients with hypertension. Given the significant heterogeneity found in the primary analyses—owing to the variety of HIIT protocols used (variable intensities and different exercise program durations)—and the very low-quality evidence, interpretation should be undertaken with considerable caution. Nonetheless, the biases involved in this systematic review are minimized by the methodological quality criteria, the 2 independent reviewers, the in-depth search in multiple databases with no restrictions of language or date of publication, and the specific analytical tools.
Conclusion
Supervised HIIT is superior to MICT in improving VO2 peak in patients with hypertension (stage 1 and stage 2). HIIT also effectively improved VO2 peak, BP, and resting HR in this population in comparison with controls. There is not enough evidence that supervised HIIT is more effective than MICT to improve cardiac autonomic modulation in patients with hypertension. Although certain benefits have been demonstrated, only the possible benefits of HIIT to VO2 peak can be stated because of the low-quality evidence. No serious adverse events were reported in the included studies; nevertheless, HIIT is not completely safe for hypertensive patients at considerable risk of cardiovascular mortality. This training proposal is safe only when supervised in fit patients at low cardiovascular risk (patients with stage 1 hypertension without associated risk factors).
Clinical Messages
There is a lack of scientific evidence on the effects of supervised HIIT versus MICT on cardiac autonomic modulation, VO2 peak, BP, and resting HR in patients with hypertension.
There is not enough evidence that supervised HIIT is more effective than MICT to improve cardiac autonomic modulation in hypertensives.
Supervised HIIT was more effective than MICT in improving VO2 peak, with significant statistical and clinical improvements in stage 1 and stage 2 hypertensive patients.
HIIT cannot yet be considered completely safe for patients at considerable risk of cardiovascular mortality (hypertension; stage 1 with ≥3 risk factors; stage 2 with 1 or 2 risk factors; stage 3, regardless of other risk factors) without other underlying cardiovascular diseases.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_19417381221139343 for Effect of High-Intensity Interval Training on Exercise Capacity, Blood Pressure, and Autonomic Responses in Patients With Hypertension: A Systematic Review and Meta-Analysis by Fabricio Olinda de Souza Mesquita, Bruno Bavaresco Gambassi, Marcio de Oliveira Silva, Sérgio Rodrigues Moreira, Victor Ribeiro Neves, Mansueto Gomes-Neto and Paulo Adriano Schwingel in Sports Health: A Multidisciplinary Approach
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brazil (CAPES) [under Finance Code 001] and was supported by Fundação de Amparo à Ciência e Tecnologia do Estado de Pernambuco (FACEPE) [APQ-0246-4.06/14].
Data Accessibility Statement: All data analyzed during this study are included in this published article and its supplementary information files.
ORCID iDs: Mansueto Gomes-Neto  https://orcid.org/0000-0002-0717-9694
https://orcid.org/0000-0002-0717-9694
Bruno Bavaresco Gambassi  https://orcid.org/0000-0003-3852-0602
https://orcid.org/0000-0003-3852-0602
Paulo Adriano Schwingel  https://orcid.org/0000-0002-2935-3403
https://orcid.org/0000-0002-2935-3403
References
- 1.Aghaei Bahmanbeglou N, Ebrahim K, Maleki M, Nikpajouh A, Ahmadizad S. Short-duration high-intensity interval exercise training is more effective than long duration for blood pressure and arterial stiffness but not for inflammatory markers and lipid profiles in patients with stage 1 hypertension. J Cardiopulm Rehabil Prev. 2019;39(1):50-55. [DOI] [PubMed] [Google Scholar]
- 2.Aguirre-Betolaza A, Mujika I, Fryer SM, et al. Effects of different aerobic exercise programs on cardiac autonomic modulation and hemodynamics in hypertension: data from EXERDIET-HTA randomized trial. J Hum Hypertens. 2020;34(10):709-718. [DOI] [PubMed] [Google Scholar]
- 3.Alvarez P, Hannawi B, Guha A. Exercise and heart failure: advancing knowledge and improving care. Methodist Debakey Cardiovasc J. 2016;12(2):110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barroso WKS, Rodrigues CIS, Bortolotto LA, et al. Brazilian guidelines of hypertension - 2020. Arq Bras Cardiol. 2021;116(3):516-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Celic V, Tadic M, Suzic-Lazic J, et al. Two- and three-dimensional speckle tracking analysis of the relation between myocardial deformation and functional capacity in patients with systemic hypertension. Am J Cardiol. 2014;113(5):832-839. [DOI] [PubMed] [Google Scholar]
- 6.Cochrane. RevMan Web. Internet. Available from: https://revman.cochrane.org/. Accessed February 18, 2021.
- 7.Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2(1):e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engel FA, Ackermann A, Chtourou H, Sperlich B. High-intensity interval training performed by young athletes: a systematic review and meta-analysis. Front Physiol. 2018;9:1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faselis C, Doumas M, Kokkinos JP, et al. Exercise capacity and progression from prehypertension to hypertension. Hypertension. 2012;60(2):333-338. [DOI] [PubMed] [Google Scholar]
- 10.Franklin BA. Evolution of the ACSM Guidelines: historical perspectives, new insights, and practical implications. ACSM Health Fit J. 2021;25:26-32. [Google Scholar]
- 11.Gambassi BB, Queiroz CO, Conceicao AF, et al. Acute effect of resistance exercise using the German Volume Training Method on blood pressure of prehypertensive subjects. Med Sport (Roma). 2020;73(3):443-52. [Google Scholar]
- 12.Gambassi BB, Coelho-Junior HJ, Paixão dos Santos C, et al. Dynamic resistance training improves cardiac autonomic modulation and oxidative stress parameters in chronic stroke survivors: a randomized controlled trial. Oxid Med Cell Longev. 2019;2019:5382843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gomes Neto M, Durães AR, Conceição LSR, Saquetto MB, Ellingsen Ø, Carvalho VO. High intensity interval training versus moderate intensity continuous training on exercise capacity and quality of life in patients with heart failure with reduced ejection fraction: a systematic review and meta-analysis. Int J Cardiol. 2018;261:134-141. [DOI] [PubMed] [Google Scholar]
- 14.Gomes-Neto M, Durães AR, Reis HFCD, Neves VR, Martinez BP, Carvalho VO. High-intensity interval training versus moderate-intensity continuous training on exercise capacity and quality of life in patients with coronary artery disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2017;24(16):1696-1707. [DOI] [PubMed] [Google Scholar]
- 15.Gorostegi-Anduaga I, Corres P, MartinezAguirre-Betolaza A, et al. Effects of different aerobic exercise programmes with nutritional intervention in sedentary adults with overweight/obesity and hypertension: EXERDIET-HTA study. Eur J Prev Cardiol. 2018;25(4):343-353. [DOI] [PubMed] [Google Scholar]
- 16.Gui Y. Intermittent exercises reduce the hypertension syndromes and improve the quality of life. J Sports Med Phys Fitness. 2016;56(1-2):133-140. [PubMed] [Google Scholar]
- 17.Guimarães GV, Ciolac EG, Carvalho VO, D’Avila VM, Bortolotto LA, Bocchi EA. Effects of continuous vs. interval exercise training on blood pressure and arterial stiffness in treated hypertension. Hypertens Res. 2010;33(6):627-632. [DOI] [PubMed] [Google Scholar]
- 18.Guiraud T, Nigam A, Gremeaux V, Meyer P, Juneau M, Bosquet L. High-intensity interval training in cardiac rehabilitation. Sports Med. 2012;42(7):587-605. [DOI] [PubMed] [Google Scholar]
- 19.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383-394. [DOI] [PubMed] [Google Scholar]
- 20.Hannan AL, Hing W, Simas V, et al. High-intensity interval training versus moderate-intensity continuous training within cardiac rehabilitation: a systematic review and meta-analysis. Open Access J Sports Med. 2018;9:1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327(7414):557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Higgins JPT, Thomas J, Chandler J, et al. eds. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 [updated July 2019]. Cochrane, 2019. Available from: https://www.training.cochrane.org/handbook.
- 23.Izadi MR, Ghardashi Afousi A, Asvadi Fard M, Babaee Bigi MA. High-intensity interval training lowers blood pressure and improves apelin and NOx plasma levels in older treated hypertensive individuals. J Physiol Biochem. 2018;74(1):47-55. [DOI] [PubMed] [Google Scholar]
- 24.Jurio-Iriarte B, Maldonado-Martín S. Effects of different exercise training programs on cardiorespiratory fitness in overweight/obese adults with hypertension: a pilot study. Health Promot Pract. 2019;20(3):390-400. [DOI] [PubMed] [Google Scholar]
- 25.Kilpatrick MW, Jung ME, Little JP. High-intensity interval training: a review of physiological and psychological responses. ACSM Health Fit J. 2014(5);18:11-16. [Google Scholar]
- 26.Kokkinos P, Manolis A, Pittaras A, et al. Exercise capacity and mortality in hypertensive men with and without addition. Hypertension. 2009;53(3):494-499. [DOI] [PubMed] [Google Scholar]
- 27.Kuehn BM. Evidence for HIIT benefits in cardiac rehabilitation grow. Am Heart Assoc. 2019;140(6):514-515. [DOI] [PubMed] [Google Scholar]
- 28.Leal JM, Galliano LM, Del Vecchio FB. Effectiveness of high-intensity interval training versus moderate-intensity continuous training in hypertensive patients: a systematic review and meta-analysis. Curr Hypertens Rep. 2020;22(3):26. [DOI] [PubMed] [Google Scholar]
- 29.Lopes S, Mesquita-Bastos J, Alves AJ, Ribeiro F. Exercise as a tool for hypertension and resistant hypertension management: current insights. Integr Blood Press Control. 2018;11:65-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating of quality randomized controlled trials. Phys Ther. 2003;83(8):713-721. [PubMed] [Google Scholar]
- 31.Miroshnikov AB, Sergeeva KV, Formenov AD, Smolensky AV. [The role of interval training in the physical rehabilitation of strength sports athletes with hypertension: a randomized controlled study] in Russian. Vopr Kurortol Fizioter Lech Fiz Kult. 2020;97:5-10. [DOI] [PubMed] [Google Scholar]
- 32.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mohr M, Nordsborg NB, Lindenskov A, et al. High-intensity intermittent swimming improves cardiovascular health status for women with mild hypertension. Biomed Res Int. 2014;2014:728289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Molmen-Hansen HE, Stolen T, Tjonna AE, et al. Aerobic interval training reduces blood pressure and improves myocardial function in hypertensive patients. Eur J Prev Cardiol. 2012;19(2):151-160. [DOI] [PubMed] [Google Scholar]
- 35.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29-e322. [DOI] [PubMed] [Google Scholar]
- 36.Myers J. Principles of exercise prescription for patients with chronic heart failure. Heart Fail Rev. 2008;13(1):61-68. [DOI] [PubMed] [Google Scholar]
- 37.Pescatello LS, Buchner DM, Jakicic JM, et al. Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc. 2019;51(6):1314-1323. [DOI] [PubMed] [Google Scholar]
- 38.Rêgo ML, Cabral DA, Costa EC, Fontes EB. Physical exercise for individuals with hypertension: it is time to emphasize its benefits on the brain and cognition. Clin Med Insights Cardiol. 2019;13:1179546819839411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soltani M, Aghaei Bahmanbeglou N, Ahmadizad S. High-intensity interval training irrespective of its intensity improves markers of blood fluidity in hypertensive patients. Clin Exp Hypertens. 2020;42(4):309-314. [DOI] [PubMed] [Google Scholar]
- 40.Staessen JA, Wang JG, Thijs L. Cardiovascular protection and blood pressure reduction: a meta-analysis. Lancet. 2001;358(9290):1305-1315. [DOI] [PubMed] [Google Scholar]
- 41.Villaquiran-Hurtado AF, Jacome-Velasco S, Chantre-Ortega A, Mueses-Tupue L, Valencia OAR, Salazar C. Entrenamiento intermitente de alta intensidad versus continuo em mujeres con hipertensión. Av Enferm. 2020;38:202-215. [Google Scholar]
- 42.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_19417381221139343 for Effect of High-Intensity Interval Training on Exercise Capacity, Blood Pressure, and Autonomic Responses in Patients With Hypertension: A Systematic Review and Meta-Analysis by Fabricio Olinda de Souza Mesquita, Bruno Bavaresco Gambassi, Marcio de Oliveira Silva, Sérgio Rodrigues Moreira, Victor Ribeiro Neves, Mansueto Gomes-Neto and Paulo Adriano Schwingel in Sports Health: A Multidisciplinary Approach