Abstract
Background:
Multiple rehabilitation protocols after shoulder surgery have been proposed. The coronavirus pandemic adds an extra layer of complexity to postoperative rehabilitation after shoulder surgery.
Hypothesis:
The combined use of a home-based rehabilitation system, the Shoulder Strengthening and Stabilization System (SSS), and telehealth visits will lead to acceptable patient self-reported outcomes and satisfaction after shoulder surgery.
Study Design:
Prospective observational cohort.
Level of Evidence:
Level 4.
Methods:
A total of 132 patients were prescribed SSS after shoulder surgery. A virtual clinical specialist monitored patients through telehealth visits as prescribed by the treating physician. Data were collected prospectively during each telehealth visit. Patients completed an exit survey during their last telehealth visit.
Results:
The use of SSS with telehealth revealed a positive impact on postoperative shoulder rehabilitation (96%), pain (71%), and stiffness (92%) as reported by patients. Both pain scores and pain medication use decreased from the 1st to 8th postoperative telehealth session (P < 0.01). Nearly all (93%) patients recommended SSS after shoulder surgery upon completing the SSS protocol.
Conclusion:
Postoperative management of shoulder surgery with SSS combined with telehealth results in a reduction in patient pain levels in the early postoperative period. Patients reported high levels of improvement with SSS in shoulder rehabilitation, pain, and stiffness. The overwhelming majority (93%) of patients recommended SSS for postoperative shoulder rehabilitation and SSS yielded high patient satisfaction scores. Elucidating the impact of SSS on clinical outcomes and function in comparison with traditional rehabilitation protocols is warranted.
Clinical Relevance:
SSS in combination with telehealth was tolerated well by patients and may represent an alternative or adjunct to traditional rehabilitation protocols.
Keywords: rehabilitation protocol, rotator cuff repair, Shoulder Strengthening and Stabilization System, shoulder surgery, telehealth, telerehabilitation
The vast majority of shoulder surgeries relate to rotator cuff or labral repair, with over 250,000 rotator cuff procedures alone performed annually.1,18 Postoperative rehabilitation is critical for optimization of patient outcomes after shoulder surgery; however, the optimal postoperative rehabilitation strategy has yet to be established.4,16 As of March 2020, the coronavirus pandemic created new challenges in the management of orthopaedic surgery patients. Not only were surgeries put on hold but face-to-face contact between the patient and provider was decreased drastically to minimize the risk of spreading and contracting the coronavirus. Consequently, the management of orthopaedic patients changed significantly as a result of the coronavirus pandemic.7,13,15
The practice of telemedicine, or providing healthcare through digital methods, is a primary example of change resulting from the coronavirus pandemic.7,22 Before the pandemic, there was interest in integrating telehealth into the management of orthopaedic patients to allow an alternative approach to traditional inperson visits.10,17 The circumstances of the coronavirus pandemic brought telehealth services to the forefront, necessitating appropriate delivery of healthcare to patients while also limiting the risk of spreading the virus.7,22 Moreover, telerehabilitation was adopted by rehabilitation specialists, including those in the field of physical therapy, for the treatment of chronic musculoskeletal issues as well as for postoperative care. 23 Despite the change from the traditional paradigm of face-to-face rehabilitation, patients and physical therapists (PTs) found telerehabilitation to be safe and efficacious. 3 As the coronavirus pandemic persists, methods of providing effective care without placing patients and providers at undue risk remain necessary.
The Shoulder Strengthening and Stabilization System (SSS) (Advanced Integrated Motion, ēlizur) was developed for use as an adjunct to the eSling Shoulder Immobilizer (Advanced Integrated Motion, ēlizur) to improve the efficiency of care in the immediate postoperative period. SSS is a home-based exercise device that allows patient-controlled shoulder motion to be performed within parameters prescribed by the treating physician. Moreover, rehabilitation can be monitored with digital technology via virtual clinical specialists (VCSs) through the use of a personal phone or tablet to ensure safe and appropriate use of the machine. To date, no studies have validated implementation of SSS in postoperative shoulder rehabilitation with regard to feasibility and patient satisfaction.
The purpose of this prospective observational cohort study was to evaluate SSS as a home-based exercise apparatus with the use of telemedicine through a VCS after shoulder surgery in the immediate 6-week postoperative period. We hypothesized that SSS, in combination with telehealth visits, would lead to high levels of patient adherence, satisfaction, and reduction in pain levels.
Methods
The study was granted exempt status by the Institutional Review Board of the University of Pittsburgh (PRO18050058). Patients undergoing shoulder surgery who were prescribed SSS in the early postoperative period were included in the study with data collected prospectively. A total of 11 physicians prescribed SSS in conjunction with the eSling Shoulder Immobilizer after arthroscopic shoulder surgery (Figure 1). The treating physician prescribed the home exercise program for the patient using SSS, including postoperative timing and limits of allowable motion. The postoperative protocol provided parameters to be followed by the VCS during virtual visits. The SSS machine can then be set to prevent motion beyond the parameters established by the prescribing physician. The eSling was worn by patients according to the surgeon-prescribed protocol but was removed when using SSS.
Figure 1.

eSling shoulder immobilizer (Advanced Integrated Motion; ēlizur).
Each patient had an SSS unit delivered to their home, and an onsite orientation and training session was completed. On the day after the initial onsite visit, a remote VCS monitored the patient during their exercise sessions in a video chat session using digital technology. The VCS, who included athletic trainers and orthopaedic nurses, had healthcare and rehabilitation experience and received training with SSS before patient interaction.
The telehealth visits with a VCS were scheduled 1 to 2 times per week during the 5 to 6 week rehabilitation protocol. Patient-controlled shoulder movements allowed during use of SSS included passive and active-assisted range of motion (ROM) exercises for glenohumeral internal and external rotation, forward flexion and extension, and scapulothoracic protraction and retraction (Figure 2). Motions of the operative arm were controlled by the unaffected contralateral extremity through an attached wand to the SSS machine. The VCS instructed patients during virtual visits to not push beyond low-level stretch and discomfort into sharp pain and discomfort. Typically, passive ROM within the allowed limits was performed for approximately 6 weeks after surgery and then protocols progressed to self-limited active-assisted ROM (Table 1). Patients were generally transitioned to traditional face-to-face PT upon completion of the SSS protocol, which often occurred at 6 to 8 weeks after surgery.
Figure 2.
Motions allowed by SSS machine including (a) internal rotation, (b) external rotation, (c) forward flexion, and (d) extension. Note white wand held in contralateral hand to control motion of affected extremity. SSS, Shoulder Strengthening and Stabilization System.
Table 1.
Sample postoperative protocol for rotator cuff repairs and labrum repairs
| PROM | |||||
|---|---|---|---|---|---|
| Postoperative Week | FF | ER | IR | Protraction/Retraction | Isometrics |
| Small/medium rotator cuff repair | |||||
| Weeks 1-3 | 100° | 15-30° | 15-30° | WNL; no resistance bands | Yes |
| Weeks 3-6 | WNL | 30-60° | 30-60° | WNL; no resistance bands | Yes |
| Massive rotator cuff repair | |||||
| Weeks 1-3 | 100° | 0-15° | 15-30° | WNL; no resistance bands | Yes |
| Weeks 3-6 | WNL | 15-30° | 30-60° | WNL; no resistance bands | Yes |
| Labrum repair | |||||
| Weeks 1-6 | WNL | 15° | 15-30° | WNL; no resistance bands | Yes |
ER, external rotation; FF, forward flexion; IR, internal rotation; PROM, patient-reported outcome measures; WNL, within normal limits.
Patient surveys were performed during the initial onsite visit and during telehealth visits with the VCS, including an exit survey. Data collected included pain ratings during telehealth visits before SSS exercise, use of pain medication (non-narcotic and narcotic), and quality of sleep from the start of the home exercise program until its completion. Questions from the exit survey are shown in Table 2. A positive impact was defined as patient responses in which improvement (greatly improved and slightly improved) was recorded.
Table 2.
Questions asked to patients during visits with the VCS
| Overall, please rate the SSS system’s impact on your shoulder rehabilitation | Greatly improved |
| Slightly improved | |
| Neutral | |
| Slightly worsened | |
| Greatly worsened | |
| Please rate the SSS system’s impact on your pain | Greatly improved |
| Slightly improved | |
| Neutral | |
| Slightly worsened | |
| Greatly worsened | |
| Please rate the SSS system’s impact on your stiffness | Greatly improved |
| Slightly improved | |
| Neutral | |
| Slightly worsened | |
| Greatly worsened | |
| Please rate the impact of video telehealth on your experience with the SSS | Greatly improved |
| Slightly improved | |
| Neutral | |
| Slightly worsened | |
| Greatly worsened | |
| If known, please rate your PT’s opinion of the SSS system’s impact on your shoulder rehabilitation | Greatly improved |
| Slightly improved | |
| Neutral | |
| Slightly worsened | |
| Greatly worsened | |
| Would you recommend the SSS system to patients undergoing shoulder surgery? | Yes |
| Maybe | |
| No |
PT, physical therapist; SSS, Shoulder Strengthening and Stabilization System; VCS, virtual clinical specialist.
Statistical analysis
Descriptive statistics including frequency counts and percentages were used for nominal data. Means and SDs were used for continuous data. Subset analyses were performed for self-reported pain, non-narcotic pain medication usage, and narcotic pain medication usage for those participants with data completed at both timepoints. Differences in self-reported pain were examined with the Paired Wilcoxon Signed Ranks test, while differences in non-narcotic pain medication and narcotic pain usage were investigated with McNemar tests.
Results
Demographics and Adherence
A total of 11 surgeons performed procedures on 132 patients (55 of whom were women) with a mean age 47.9 ± 16.7 years. The majority of procedures were rotator cuff (n = 95; 74.2%) or labral (n = 26; 20.3%) repairs. The initial telehealth session occurred at a mean of 17.7 ± 12.6 days after surgery. Use of SSS decreased from 82% to 61% of patients from the 6th to 8th postoperative visit, which occurred during postoperative weeks 5 and 6, respectively.
Pain
Self-reported pain scores decreased over time in the early postoperative period with use of SSS. The mean self-reported pain rating did not exceed 3 out of 10 at any timepoint (Figure 3). Mean self-reported pain ratings decreased from 2.9 ± 2.1 at the first postoperative session to 2.2 ± 2.0 at session 8 (P < 0.01). There was a reduction in the number of patients using opioid medication over time, as opioid use decreased from 55.3% of patients at session 1 to 28.9% of patients at session 8 (P < 0.01). There was also a reduction in patients using non-narcotic medication over time, as 73.8% of patients reported use at session 1 and 60% reported use at session 8 (P < 0.01).
Figure 3.
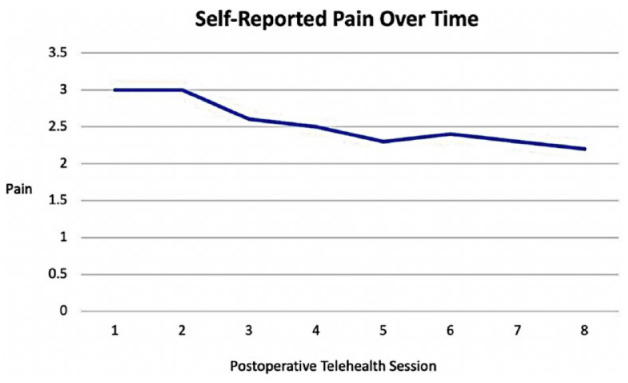
Mean patient-reported postoperative pain ratings during use of SSS by session with the VCS. SSS, Shoulder Strengthening and Stabilization System; VCS, virtual clinical specialist.
Exit Survey
Patient self-reported ratings demonstrated that SSS had a positive impact on shoulder rehabilitation in 96% of patients, a positive impact on pain in 71% of patients, and a positive impact on stiffness in 92% of patients (Table 3). No patients reported a negative impact of telemedicine with the use of SSS, while 98% of patients reported a positive impact. There were no patients that would not recommend SSS after shoulder surgery, while 7% of patients responded “maybe,” and 93% of patients responded “yes” to recommending SSS after shoulder surgery.
Table 3.
Patient-reported responses at exit survey regarding SSS.
| Question | Greatly Worsened | Slightly Worsened | Neutral | Slightly Improved | Greatly Improved |
|---|---|---|---|---|---|
| Overall, please rate the SSS system’s impact on your shoulder rehabilitation | 0 | 0 | 4.0 | 22.2 | 73.7 |
| Please rate the SSS system’s impact on your pain | 1.0 | 6.0 | 22.0 | 26.0 | 45.0 |
| Please rate the SSS system’s impact on your stiffness | 0 | 0 | 8.0 | 24.0 | 68.0 |
| Please rate the impact of video telehealth on your experience with the SSS | 0 | 0 | 2.0 | 5.1 | 92.9 |
| If known, please rate the opinion of your PT on the SSS impact on your shoulder function a | 0 | 2.0 | 29.0 | 7.0 | 27.0 |
PT, physical therapist; SSS, Shoulder Strengthening and Stabilization System.
34.3% of patients responded as unknown.
Discussion
This retrospective analysis of a prospectively collected cohort consisting of 132 patients receiving inhome SSS rehabilitation with telehealth after shoulder surgery demonstrated improvements in patient pain scores and stiffness, as well as high rates of patient satisfaction in the early postoperative period. These results confirmed our hypothesis, showing that SSS was successful in early postoperative rehabilitation after shoulder surgery. An overwhelming majority (96%) of patients reported a positive impact of SSS on shoulder rehabilitation, whereas 93% of patients would recommend SSS for rehabilitation after shoulder surgery. To date, the utility of SSS in the postoperative period after shoulder surgery has not been described. The results from this study suggest that SSS in conjunction with telehealth deserves consideration as a potential cost-effective alternative or adjunct to traditional rehabilitation protocols involving formal inperson physical therapy after shoulder surgery.
The majority of patients included underwent an arthroscopic rotator cuff repair. Unfortunately, the optimal rehabilitation protocol after rotator cuff repair has yet to be determined, with multiple studies comparing early motion protocols with delayed motion protocols.2,5,6,11,12 The proposed primary benefit of early motion protocols, in which patients begin ROM exercise early in the postoperative period, includes improvements of shoulder ROM. 5 However, lower rates of healing have been shown with early motion protocols when compared with delayed motion protocols, especially with larger sized rotator cuff tears.2,5,12 Thus, the ideal protocol would be early safe ROM that does not progress too quickly or aggressively to compromise healing. SSS has adaptive capabilities with precise limits to the amount of motion for any given movement, which allow surgeons to individualize postoperative rehabilitation protocols between patients to account for patient-specific risk factors, such as those at risk for postoperative stiffness or impaired tendon healing. Therefore, rehabilitation exercise occurs strictly within the parameters prescribed, eliminating the possibility of misunderstanding, excessive shoulder ROM, and treatment variability that may otherwise occur with traditional rehabilitation approaches. The ability to individualize rehabilitation protocols with strict motion parameters has the potential to decrease complications and improve overall patient outcomes.
A telehealth platform through the use of VCS was utilized in conjunction with SSS. Telerehabilitation in physical therapy has been shown to be effective for both nonorthopaedic conditions and orthopaedic conditions, such as osteoarthritis, low back pain, and total joint replacement.19,20,23 High rates of patient satisfaction were seen with the use of SSS with VCS in the current study, with 98% of patients responding positively to the impact of telehealth on the experience with SSS. Given a less than 100% rate in patient satisfaction, it stands to reason that SSS is not the optimal early postoperative rehabilitation modality for every patient. A separate study, in a similar fashion, found that more than 90% of patients receiving telerehabilitation were satisfied with the management that was provided, while more than 80% of PTs found the telerehabilitation method to be effective at providing care. 3 Moreover, patient satisfaction rates and functional outcomes have been shown to be similar with telerehabilitation when compared with traditional inperson rehabilitation.8,19,20 Benefits of telemedicine in physical therapy rehabilitation include decreased patient travel, lower coronavirus exposure risk, less wait time burden, and greater patient convenience, 14 all of which may lead to higher adherence rates. The majority of patients continued to use SSS during rehabilitation at 6 weeks postoperatively, indicating that the SSS device and protocols were tolerated by patients during the early postoperative period. These benefits have the potential to improve patient access to care while providing for improved continuity of care, which can optimize patient rehabilitation and outcomes. 9
Another important aspect that has been demonstrated with telemedicine is cost effectiveness. Virtual fracture clinics were found to have an annual cost reduction of up to $305,000 by Murphy et al, 21 while McKeon et al 19 reported cost savings of up to $4100 per patient during the rehabilitation after total joint arthroplasty. While SSS does have an associated cost that is billed into the cost of the sling, this is potentially offset by fewer PT visits, decreased travel time, and time off from work. Moreover, because some insurance companies have limitations on the number of PT visits per year, methods that retain inperson visits for when they are critical may benefit the patient. Further investigation into the cost effectiveness with telehealth visits is warranted.
There are significant limitations to this investigation related to the heterogeneity of surgical patients included, as well as the lack of clinical measures, such as ROM, function, and patient-reported outcome measures. Notably, SSS does not eliminate the need for shoulder rehabilitation. Rather, SSS can be an alternative, or an adjunct, to traditional early postoperative rehabilitation with inperson physical therapy. It is important to note that rehabilitation after shoulder surgery necessitates the transition from SSS to inperson physical therapy. Nevertheless, the aim of this study was to assess the early patient experience with a new inhome device that assists with shoulder rehabilitation after shoulder surgery. The results from this study suggest that SSS provides patients with a reliable method of rehabilitation with high satisfaction rates, adherence, and reduction of pain scores in the initial postoperative period.
In conclusion, postoperative management after common shoulder surgeries using the SSS machine combined with telehealth results in reduced pain levels along with a reduction in pain medication usage in the early postoperative period. Use of SSS had a positive impact on postoperative shoulder rehabilitation as reported by 96% of patients. The overwhelming majority of patients (93%) recommended the use of SSS for postoperative shoulder rehabilitation.
Footnotes
The following authors declared potential conflicts of interest: B.P.L. has received royalty payments from Workers Kluwer Publishing. A.L. is a paid consultant of Arthrex and Stryker/Tornier. V.M. has received grants from Smith & Nephew and Arthrex; consultancy fee from Smith & Nephew; patents from University of Pittsburgh; and hospitality payments from ISAKOS. V.M., J.J.I., and A.J.P. have pending grants from NIH and Department of Defense; and have received royalty payments from ēlizur Corporation.
This work was supported by ēlizur Corporation (Pittsburgh, PA) through the providing of data and funding for the senior author’s time to complete all descriptive and statistical analyses, summaries and conclusions, and preparation of the manuscript.
ORCID iD: Justin J. Greiner  https://orcid.org/0000-0001-6189-6101
https://orcid.org/0000-0001-6189-6101
References
- 1.Amini MH, Ricchetti ET, Iannotti JP, Derwin KA. Rotator cuff repair: challenges and solutions. Orthop Res Rev. 2015;7:57-69. [Google Scholar]
- 2.Bakti N, Antonios T, Phadke A, Singh B. Early versus delayed mobilization following rotator cuff repair. J Clin Orthop Trauma. 2019;10:257-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bennell KL, Lawford BJ, Metcalf B, et al. Physiotherapists and patients report positive experiences overall with telehealth during the COVID-19 pandemic: a mixed-methods study. J Physiother. 2021;67:201-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boland K, Smith C, Bond H, Briggs S, Walton J. Current concepts in the rehabilitation of rotator cuff related disorders. J Clin Orthop Trauma. 2021;18:13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang KV, Hung CY, Han DS, et al. Early versus delayed passive range of motion exercise for arthroscopic rotator cuff repair: a meta-analysis of randomized controlled trials. Am J Sports Med. 2015;43:1265-1273. [DOI] [PubMed] [Google Scholar]
- 6.Choi S, Seo KB, Shim S, Shin JY, Kang H. Early and delayed postoperative rehabilitation after arthroscopic rotator cuff repair: a comparative study of clinical outcomes. Clin Shoulder Elb. 2019;22:190-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cole PA, Jr, Lezak BA, Schroder LK, Cole PA. Global orthopaedic trauma surgeons highlight telenomics during the COVID-19 era: a case for advancing telemedicine in orthopaedics. J Clin Orthop Trauma. 2021;17:182-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eannucci EF, Hazel K, Grundstein MJ, Nguyen JT, Gallegro J. Patient satisfaction for telehealth physical therapy services was comparable to that of in-person services during the COVID-19 pandemic. HSS J. 2020;16:10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grundstein MJ, Fisher C, Titmuss M, Cioppa-Mosca J. The role of virtual physical therapy in a post-pandemic world: pearls, pitfalls, challenges, and adaptations. Phys Ther. 2021;101:pzab145. [DOI] [PubMed] [Google Scholar]
- 10.Herrero CP, Bloom DA, Lin CC, et al. Patient satisfaction is equivalent using telemedicine versus office-based follow-up after arthroscopic meniscal surgery: a prospective, randomized controlled trial. J Bone Joint Surg Am. 2021;103:771-777. [DOI] [PubMed] [Google Scholar]
- 11.Kjaer BH, Magnusson SP, Henriksen M, et al. Effects of 12 weeks of progressive early active exercise therapy after surgical rotator cuff repair: 12 weeks and 1-year results from the CUT-N-MOVE randomized controlled trial. Am J Sports Med. 2021;49:321-331. [DOI] [PubMed] [Google Scholar]
- 12.Kluczynski MA, Nayyar S, Marzo JM, Bisson LJ. Early versus delayed passive range of motion after rotator cuff repair: a systematic review and meta-analysis. Am J Sports Med. 2015;43:2057-2063. [DOI] [PubMed] [Google Scholar]
- 13.Lezak BA, Cole PA, Jr, Schroder LK, Cole PA. Global experience of orthopaedic trauma surgeons facing COVID-19: a survey highlighting the global orthopaedic response. Int Orthop. 2020;44:1519-1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahmoud IAM, Sr. Usability of telemedicine in physical therapy rehabilitation: systematic review. JMIR Rehabil Assist Technol. Published online June 3, 2021. doi: 10.2196/25250. [DOI] [PubMed] [Google Scholar]
- 15.Massey PA, McClary K, Zhang AS, Savoie FH, Barton RS. Orthopaedic surgical selection and inpatient paradigms during the coronavirus (COVID-19) pandemic. J Am Acad Orthop Surg. 2020;28:436-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matlak S, Andrews A, Looney A, Tepper KB. Postoperative rehabilitation of rotator cuff repair: a systematic review. Sports Med Arthrosc Rev. 2021;29:119-129. [DOI] [PubMed] [Google Scholar]
- 17.McDonnell JM, Ahern DP, Ross TD, et al. The efficacy of remote virtual care in comparison to traditional clinical visits for elective orthopaedic patients: a meta-analysis of prospective randomised controlled trials. Surgeon. 2022;20(3):177-186. [DOI] [PubMed] [Google Scholar]
- 18.McElvany MD, McGoldrick E, Gee AO, Neradilek MB, Matsen FA, III. Rotator cuff repair: published evidence on factors associated with repair integrity and clinical outcome. Am J Sports Med. 2015;43:491-500. [DOI] [PubMed] [Google Scholar]
- 19.McKeon JF, Alvarez PM, Vajapey AS, et al. Expanding role of technology in rehabilitation after lower-extremity joint replacement: a systematic review.JBJS Rev. 2021;9:e21.00016. [DOI] [PubMed] [Google Scholar]
- 20.Moffet H, Tousignant M, Nadeau S, et al. Patient satisfaction with in-home telerehabilitation after total knee arthroplasty: results from a randomized controlled trial. Telemed J E Health. 2017;23:80-87. [DOI] [PubMed] [Google Scholar]
- 21.Murphy EP, Fenelon C, Murphy RP, et al. Are virtual fracture clinics during the COVID-19 pandemic a potential alternative for delivering fracture care? A systematic review. Clin Orthop Relat Res. 2020;478:2610-2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parisien RL, Shin M, Constant M, et al. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28:e487-e492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seron P, Oliveros MJ, Gutierrez-Arias R, et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther. 2021;101:pzab053. [DOI] [PMC free article] [PubMed] [Google Scholar]



