Abstract
Background
The decline in estrogen levels from several years before (perimenopause) and during menopause has various negative effects, including skin specific issues, which often receive less attention than other menopausal symptoms despite having a significant negative effect on quality of life (QoL). The objective of this study was to evaluate the effectiveness of anti‐aging dermocosmetic products designed for women during the perimenopause and menopause.
Materials and methods
An open study of 101 perimenopausal women (no menstruation for 4–12 months or irregular menstruation for <5 years) and 101 menopausal women (no menstruation for >12 months), not taking hormone replacement therapy, was conducted. Adapted dermocosmetic regimens, specific to each group (day cream, night cream and serum), were applied for 56 days. Assessments included automatic artificial intelligence diagnostics of eight clinical facial signs, hydration and transepidermal water loss (TEWL), and a menopause skin QoL questionnaire.
Results
Mean age was 50 ± 3.9 years (range 41–57) and 59 ± 3.8 years (range 50–66) for the perimenopause and menopause groups, respectively. Significant improvements in wrinkles and vascular signs, increases in hydration, decreases in TEWL, and a positive impact on QoL were observed after 56 days of application of the respective dermocosmetic regimens for both the perimenopause and menopause groups.
Conclusion
The anti‐aging skin care products designed specifically for perimenopausal and menopausal women increased skin hydration and improved wrinkles with a positive impact on QoL.
Keywords: artificial intelligence, dermocosmetic, menopause, quality of life, skin aging
1. INTRODUCTION
In addition to natural chronological skin aging, exposome factors also contribute to skin aging, including environmental factors, especially solar radiation, and internal factors, such as hormone changes. 1 The main hormone changes affecting skin aging during menopause are the dramatic decline in estrogen (specifically 17β‐estradiol) and DHEA, as well as the increase in cortisol. 2 , 3 In the skin, the decrease in estrogen during menopause leads to changes in the collagen content and the ratio of type III/I collagen causing atrophy (declining dermal collagen content results in epidermal thinning and decreased skin elasticity), while a decrease in glycoaminoglycans causes diminished skin moisture and skin dryness. 2 , 4 Together these changes in the skin lead to more pronounced wrinkles and, subsequently, xerosis, possible pruritus, increased transepidermal water loss (TEWL), as well as poor wound healing, and reduced vascularity. 4 Reducing these skin aging signs may be a potential benefit of taking hormone replacement therapy (HRT) during menopause (if prescribed for other symptoms). 5 , 6 , 7 , 8 , 9 , 10 However, HRT would never be indicated for skin symptoms alone due to the risk‐benefit balance.
Natural menopause generally occurs around 50 years of age and is defined as the permanent cessation of menstruation resulting from the loss of ovarian follicular activity after 12 consecutive months of amenorrhoea. 11 Menopause is generally preceded by a course of perimenopause (around 2–8 years) when the clinical and biological features of approaching menopause commence and hormone levels fluctuate (this includes the 12 months following the last menstrual cycle). 11
Specially adapted dermocosmetic regimens have been developed for women during perimenopause and menopause aimed at mitigating the effects of hormonal changes on the skin. Proxylane, a C‐xylopyranoside derivative, is a cosmetic active ingredient shown to stimulate the synthesis of mucopolysaccharides in the dermis and epidermis to improve skin elasticity and tonicity. 12 Furthermore, topical C‐xyloside application in vivo may be efficient in inducing a better dermal‐epidermal cohesion in photoaged or chronologically aged skin. 13 In a previous randomized controlled trial in post‐menopausal women, aged 55 and 65 years and not taking HRT, a serum containing proxylane 3%, hedione 1%, hydrovance, and hepes 5% each (Laboratoires Vichy, Asnières sur Seine, France), and a moisturizing cream containing water, glycerin, cyclohexasiloxane, stearic acid, and butylene glycol, was shown to reduce visible signs of skin aging and changes in sebum composition. 14
Cassia extract, from a traditional medicinal plant, has anti‐aging effects on the skin by reducing the impact of cortisol on collagen and hyaluronic acid synthesis to stimulate extracellular matrix synthesis. 15 , 16
Vichy volcanic mineralizing water (VVMW) is a highly mineralized water containing 15 minerals that confer antioxidant properties to strengthen the skin barrier and help protect the skin against exposome aggressions. 17
Niacinamide (vitamin B3) has been shown to have an exfoliating effect, reduce dark spots, improve skin barrier function, 18 increase lipid biosynthesis, and reduce TEWL 19 , 20 to improve skin hydration and wrinkles. 21 Vitamin C and vitamin E have antioxidant, photoprotective, and hydration benefits. 22 , 23
Hyaluronic acid is a major component of the extra‐cellular matrix, with viscoelastic and hygroscopic properties, with a unique capacity in retaining water and preventing skin dryness, atrophy, and loss of elasticity. 24
Lipohydroxy acid (LHA) has been shown to induce dermal thickening by stimulating glycosaminoglycans, collagen, and elastin production; glycolic acid increases cell turnover to reduce dark spots. 25 , 26
A range of anti‐aging dermocosmetics has been specifically developed for women in menopause and during perimenopause. A serum aimed at both groups (Neovadiol meno 5 bi‐serum; Laboratoires Vichy, France) contains VVMW, proxylane, cassia extract, vitamins B3, C, and E, omegas 6 and 9, LHA and glycolic acid. Additional key ingredients are HA in the perimenopause creams (Neovadiol redensifying day cream [cream A] and night cream [cream B]) for its hydration properties; 27 and omegas 3,6 and 9 in the creams for women during the menopause (Neovadiol replenishing day cream [cream C] and night cream [cream D]) to replenish lipid loss.
The objective of this study was to evaluate the effectiveness and impact on QoL of these anti‐aging dermocosmetic products specially designed for women during perimenopause or menopause.
2. METHODS
2.1. Subjects
The study was performed between March and May 2021 on 202 French women. In this open, uncontrolled study, recruitment into two groups was determined via questionnaire responses:
Peri‐Menopause group of 101 women who had cessation of menstruation for more than 4 months but less than 12 months or irregular menstruation for less than 5 years. These women experienced hot flashes and/or night sweats and were not receiving hormone treatments for menopause.
Post‐Menopause group of 101 women who had permanent irreversible cessation of menstruation for more than 12 months and were not receiving hormone treatments for menopause.
Inclusion criteria were possessing a smartphone (any brand) with a high‐resolution camera (≥10 Megapixels); being familiar with taking selfie pictures; and absence of any facial skin disease, disorder or scars (e.g., rosacea, acne, and angioma). Recruitment was not based on clinical scoring of facial skin aging signs.
2.2. Dermocosmetic regimen
Test products were applied on the whole face for 2 months (56 days). Both groups were provided with serum for twice daily application (morning and evening).
The perimenopause group also applied Day cream A (morning) and Night cream B (evening).
The menopause group also applied Day cream C (morning) and Night cream D (evening).
2.3. Assessments
Subjects visited the consumer agency at the same time of the day on Day 0 (D0) and D56. Subjects were asked not to apply any products on their face before the visit. Study evaluations were carried out in a temperature and humidity‐controlled room (temperature 21 ± 1°C; relative humidity 45 ± 5%) after an acclimation period of 30 min.
Facial skin diagnostics were performed with a smartphone application (SkinconsultAI, Vichy, France) leveraging deep learning potentialities, as previously described. 28 This artificial intelligence (AI)‐based algorithm was used to automatically assess smartphone selfie images for eight clinical facial aging signs of European women (Fitzpatrick skin phototypes I‐III), related to Wrinkles/Texture, Ptosis/Sagging, or Vascular signs (Table 1). Subjects were asked, in the presence of an operator at the agency to take one frontal selfie picture (full face) and to adopt the most neutral expression while standing in the same position and under the same lighting conditions. Of note, all subjects were asked to wear the same clothes to both assessments on D0 and D56 to avoid any light dispersion and discrepancies in the collected images. Some examples of exploitable selfie pictures were provided to all women to help them obtain the most accurate image (distance and angle) stored by the smartphone. All pictures were then sent to the dedicated and secured website for further processing.
TABLE 1.
The eight clinical facial signs of Caucasian women, related to wrinkles/texture, ptosis/sagging, or vascular signs.
| Facial Signs | Definition of scored observation | Scale | Visual |
|---|---|---|---|
| Glabellar wrinkles | Depth of vertical wrinkles between eyebrows. | 0–5 |

|
| Crow's feet wrinkles | Depth of deepest wrinkle at the area of outer eye corner (5 mm at least outside from the corner). | 0−6 |

|
| Periorbital wrinkles (upper cheek area) | Depth of folds at the malar area below Crow's feet, eye orbit excepted. | 0−5 |

|
| Nasolabial fold | Depth of the fold present on the face between the base of the nose and lips. | 0−5 |

|
| Cheek folds | Depth of folds in the cheek area. | 0−8 |

|
| Marionette lines | Depth of folds at the corner of lips. | 0−6 |

|
| Ptosis of the lower part of the face | Sagging severity of the lower parts of each side of the chin. | 0−5 |

|
| Vascular signs | Diffused redness and microvessels are visible on the face and especially the cheeks. | 0−7 |

|
The GPSkin Barrier (GPSB; GPOWER Inc, Seoul, South Korea) nomad device, as previously described, 29 , 30 was used to assess hydration and TEWL. Three measurements (close areas) were performed on the right and left cheeks by a trained operator during visits to the agency at the same time of day on D0 and D56.
The 28‐item Menopausal Skin Quality of Life self‐questionnaire (MSkinQoL) 31 was completed by all subjects in French at D0 and D56.
2.4. Statistics
For the GpSkin Barrier nomad device measurements of hydration and TEWL, readings obtained on D0 and D56 were compared using a Student T‐Test (bilateral for paired samples).
For AI‐based algorithm assessments, each facial sign and the clinical cluster were automatically graded at D0 and D56, and the respective mean scores were compared, using a Student's t‐test (bilateral on paired samples), by analysis performed with Xlstat software (Addinsoft, Bordeaux, France). Comparing Values at D0 and D56, computed p‐values of p < 0.05 were taken as statistically significant.
Performance and QoL self‐questionnaire responses at D0 and D56 were compared using a Khi2 Test on global repartition (SPSS Software Package, Chicago, IL, USA).
2.5. Ethical statement
Ethics committee approval was not required for this consumer test of a dermocosmetic product. All subjects were fully informed about the objectives of the study and provided signed informed consent (in French) which specified that their photographs were totally confidential (blind‐coded) and would be deleted after analysis.
3. RESULTS
3.1. Demographic and clinical baseline characteristics
The mean age was 50 ± 3.9 years old (range 41–57) and 59 ± 3.8 years old (range 50–66) for the perimenopause and menopause groups, respectively.
At baseline, more subjects in the perimenopause group (12%) indicated they often/always suffer hot flashes than in the menopause group (9%). Similarly, more subjects in the perimenopause group (40%) indicated they often/always have trouble sleeping than in the menopause group (25%).
3.2. AI‐based automatic grading system clinical assessments
In the menopause group, automatic grading scores statistically significantly improved for the five wrinkles/texture facial signs of the nasolabial fold, glabellar wrinkles, periorbital wrinkles, marionette lines, and cheek folds (all p < 0.04), as well as sagging or ptosis of the lower part of the face (p < 0.0001) and vascular signs (p = 0.001) (Figure 1A).
FIGURE 1.
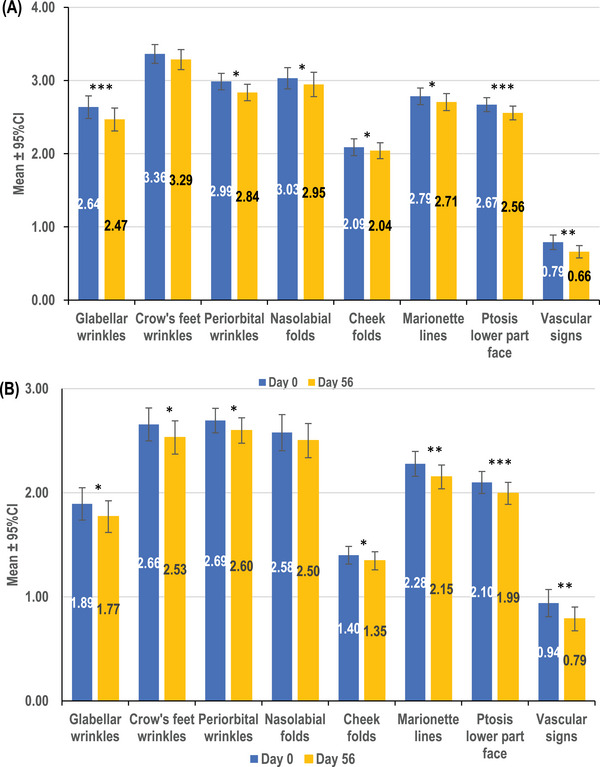
Mean values (±95% confidence interval [CI]) of severity of eight facial signs, as assessed by the artificial intelligence (AI)‐based automatic grading system, before and after 2 months of twice daily application of the respective dermocosmetic products in the menopause (A) and perimenopause (B) groups. ***p ≤ 0.0001, **p ≤ 0.001, *p < 0.05; CI, confidence interval.
In the perimenopause group, automatic grading scores statistically significantly improved for the five wrinkles/texture facial signs of glabellar wrinkles, periorbital wrinkles, marionette lines, crow's feet wrinkles, and cheek folds (all p < 0.04), as well as sagging or ptosis of the lower part of the face (p = 0.0001) and vascular signs (p = 0.0002) (Figure 1B).
3.3. Nomad device GPSkin Barrier assessments
After 56 days of application of the anti‐aging dermocosmetic regimen, significant improvements in hydration of around 29% and 21% were observed in the menopause (Figure 2A) and perimenopause groups, respectively (Figure 2B) (both p < 0.0001).
FIGURE 2.
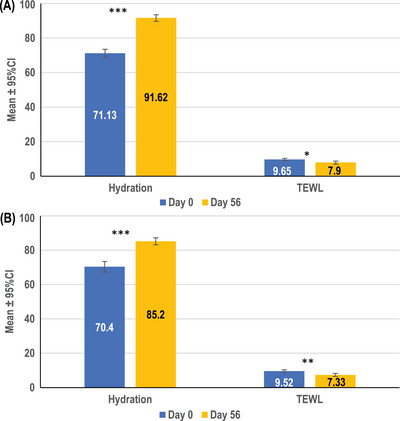
Mean values (± 95% confidence interval [CI]) of skin hydration and trans‐epidermal water loss assessed by GPSkin Barrier before and after 2 months of twice daily application of the respective dermocosmetic products in the menopause (A) and perimenopause (B) groups. ***p < 0.0001, **p < 0.001, *p < 0.01; CI, confidence interval; TEWL, trans‐epidermal water loss.
Between D0 and D56, an 18% decrease in TEWL was observed in the menopause group (p = 0.002; Figure 2A) and a 23% decrease in the perimenopause group (p = 0.0004; Figure 2B).
3.4. Quality of life self‐questionnaire
In both the menopause and perimenopause groups, the responses to the health status dimension questions were not significantly different between D0 and D56, except the percentage of women in the perimenopause group indicating they often/always felt tired decreased from 27% to 12% after applying the dermocosmetic regimen for 56 days (p < 0.05).
Conversely, the majority of social effect responses, and especially the self‐esteem dimension questions, indicated that women in both groups felt better about their skin after using the dermocosmetic regimens (see Table 2). In the menopause group, the percentage of women responding their skin often/always did not look as good significantly decreased from 31% to 7% after applying the dermocosmetic regimen for 56 days; the percentage of often/always not satisfied with their skin decreased from 37% to 9% after applying the dermocosmetic regimen; and the percentage indicating they often/always had trouble accepting their face decreased from 23% to 6% (all p < 0.05). The women in the perimenopause group were even less satisfied with their skin at baseline with the percentage responding their skin often/always did not look as good decreasing from 45% to 13% after applying the dermocosmetic regimen for 56 days; the percentage often/always not satisfied with their skin decreasing from 40% to 16% after using the dermocosmetic regimen; while the percentage indicating they often/always had trouble accepting their face decreased from 22% to 4% (all p < 0.05).
TABLE 2.
Quality of Life questionnaire responses on D0 and at D56 for the menopause and perimenopause groups. Possible answers were never (0), rarely (1), sometimes (2), often (3), always (4), and questions are grouped according to the MSkinQol dimensions.
| Menopause group | Perimenopause group | ||||||
|---|---|---|---|---|---|---|---|
| Frequency | D0 | D56 | p‐value | D0 | D56 | p‐value | |
| HEALTH STATUS | |||||||
| I feel more tired than usual | Never/Rarely | 46% | 53% | 0.10 | 27% | 42% | 0.05 |
| Often/Always | 2% | 5% | 27% | 12% | |||
| I suffer from hot flashes | Never/Rarely | 75% | 74% | 0.10 | 50% | 55% | 0.10 |
| Often/Always | 9% | 7% | 12% | 12% | |||
| I do not feel comfortable about myself | Never/Rarely | 67% | 66% | 0.10 | 41% | 51% | 0.10 |
| Often/Always | 13% | 14% | 26% | 14% | |||
| I have trouble sleeping | Never/Rarely | 45% | 47% | 0.10 | 23% | 36% | 0.10 |
| Often/Always | 25% | 22% | 40% | 26% | |||
| I feel very irritable | Never/Rarely | 74% | 81% | ≥0.10 | 53% | 57% | ≥0.10 |
| Often/Always | 3% | 1% | 14% | 6% | |||
| I suffer from mood swings | Never/Rarely | 75% | 76% | ≥0.10 | 57% | 69% | ≥0.10 |
| Often/Always | 11% | 5% | 13% | 11% | |||
| I have trouble remembering | Never/Rarely | 73% | 68% | ≥0.10 | 63% | 69% | ≥0.10 |
| Often/Always | 3% | 4% | 10% | 5% | |||
| I feel more fragile emotionally | Never/Rarely | 59% | 73% | < 0.10 | 55% | 63% | ≥0.10 |
| Often/Always | 10% | 9% | 17% | 10% | |||
| I get the blues sometimes | Never/Rarely | 72% | 84% | ≥0.10 | 58% | 67% | ≥0.10 |
| Often/Always | 5% | 2% | 9% | 6% | |||
| I feel vulnerable | Never/Rarely | 81% | 83% | ≥0.10 | 68% | 72% | ≥0.10 |
| Often/Always | 3% | 1% | 9% | 6% | |||
| SELF‐ESTEEM | |||||||
| I have trouble accepting my face | Never/Rarely | 42% | 65% | < 0.05 | 37% | 61% | < 0.05 |
| Often/Always | 23% | 6% | 22% | 4% | |||
| I have trouble accepting my figure | Never/Rarely | 32% | 45% | ≥0.10 | 24% | 29% | ≥0.10 |
| Often/Always | 34% | 23% | 47% | 35% | |||
| My skin gets me down | Never/Rarely | 49% | 76% | < 0.05 | 43% | 71% | < 0.05 |
| Often/Always | 12% | 7% | 11% | 5% | |||
| My skin does not look as good | Never/Rarely | 27% | 70% | < 0.05 | 22% | 65% | < 0.05 |
| Often/Always | 31% | 7% | 45% | 13% | |||
| I do not enjoy looking at my skin | Never/Rarely | 41% | 69% | < 0.05 | 39% | 66% | < 0.05 |
| Often/Always | 26% | 9% | 29% | 16% | |||
| I am not satisfied with my skin | Never/Rarely | 29% | 63% | < 0.05 | 27% | 54% | < 0.05 |
| Often/Always | 37% | 9% | 40% | 16% | |||
| I am obsessed with the appearance of my aging skin (it consumes my thoughts) | Never/Rarely | 51% | 73% | < 0.05 | 55% | 70% | < 0.05 |
| Often/Always | 18% | 7% | 18% | 5% | |||
| SOCIAL EFFECT | |||||||
| My skin's appearance affects my relationships with friends and family | Never/Rarely | 89% | 98% | ≥0.10 | 89% | 95% | ≥0.10 |
| Often/Always | 2% | 1% | 0% | 0% | |||
| My skin's appearance makes me cranky | Never/Rarely | 79% | 94% | < 0.05 | 77% | 93% | < 0.05 |
| Often/Always | 3% | 1% | 4% | 1% | |||
| I do not enjoy touching my skin | Never/Rarely | 78% | 92% | < 0.05 | 59% | 86% | < 0.05 |
| Often/Always | 4% | 1% | 15% | 4% | |||
| My skin's appearance affects my love life | Never/Rarely | 79% | 94% | < 0.05 | 80% | 94% | < 0.05 |
| Often/Always | 5% | 0% | 8% | 0% | |||
| The condition of my skin makes me feel stressed | Never/Rarely | 76% | 90% | < 0.05 | 57% | 83% | < 0.05 |
| Often/Always | 11% | 2% | 12% | 1% | |||
| My skin's appearance makes me feel unattractive | Never/Rarely | 47% | 85% | < 0.05 | 44% | 72% | < 0.05 |
| Often/Always | 12% | 7% | 17% | 5% | |||
| My self‐esteem suffers from the way my skin looks | Never/Rarely | 61% | 87% | < 0.05 | 57% | 84% | < 0.05 |
| Often/Always | 12% | 7% | 16% | 3% | |||
| I do not feel desirable because of the way my skin looks | Never/Rarely | 63% | 90% | < 0.05 | 55% | 84% | < 0.05 |
| Often/Always | 8% | 5% | 11% | 3% | |||
| My skin's appearance affects my femininity | Never/Rarely | 69% | 87% | < 0.05 | 54% | 84% | < 0.05 |
| Often/Always | 14% | 4% | 11% | 1% | |||
| NEUTRAL | |||||||
| Taking care of my skin is a hassle | Never/Rarely | 63% | 78% | < 0.10 | 51% | 65% | < 0.05 |
| Often/Always | 8% | 6% | 16% | 6% | |||
In the social effect dimension, in the menopause group, significant decreases were observed in the percentage indicating their skin's appearance often/always affects their love life (5% at baseline to 0% after 56 days of application of the dermocosmetic regimen, p < 0.05); their skin's appearance often/always affects their femininity (14% at baseline to 4% after 56 days application of the dermocosmetic regimen, p < 0.05); and their self‐esteem often/always suffers from the way their skin looks (12% at baseline to 7% after 56 days application of the dermocosmetic regimen, p < 0.05). Similarly, in the perimenopause group, significant decreases were observed for their skin's appearance often/always affects their love life (8% at baseline to 0% after 56 days of application of the dermocosmetic regimen, p < 0.05); their skin's appearance often/always affects their femininity (11% at baseline to 1% after 56 days application of the dermocosmetic regimen, p < 0.05); and their self‐esteem often/always suffers from the way their skin looks (16% at baseline to 3% after 56 days application of the dermocosmetic regimen, p < 0.05) (Table 2).
4. DISCUSSION
The application of a range of dermocosmetic products (day cream, night cream, and serum) for 2 months showed effectiveness in both groups of women, at perimenopause and menopause, on increasing hydration with improvements in wrinkles, vascular signs, and lower face ptosis. Furthermore, the questionnaire responses for the dimensions of self‐esteem and social effect indicated that the women in both groups felt better about their skin and their appearance after using the dermocosmetic regimen for two months.
Differences were observed in the two groups with higher baseline scores for wrinkles and ptosis in the menopause group, as measured by the AI‐based automatic grading system. At perimenopause, fluctuations in estrogen levels may have an effect on sebum levels, while later in menopause, when sebum production is markedly reduced, 32 the skin may become increasingly dry and itchy, followed by sagging and atrophy. Collagen levels decrease approximately 30% in the first five years in menopausal women, followed by a steady decline of around 2% per year. 33
The nomad evaluation methods are validated methods that allow remote assessment of the effect of active ingredients during real‐world use by women during menopause. The GPSB is a novel instrumental device used to assess skin hydration and TEWL 29 , 30 , 34 and has been previously used to show improvements in skin hydration of a dermocosmetic product in an intra‐individual split‐face study in subjects with rosacea. 35 Similarly, in our study GPSB showed statistically significant improvements in skin hydration after the use of the dermocosmetic regimen in both the menopause and perimenopause groups.
The AI‐based automatic grading of selfies has been trained and validated by dermatologists’ clinical assessments using photographic scales of referential atlases of skin aging. 28 , 36
AI‐based automatic grading was also used to assess the efficacy of a dermocosmetic product applied for one month on facial skin to compare the self‐perceived effects of a facial anti‐aging product to those automatically detected from selfie images of Chinese women of different ages and cities. 37
Although the use of an effective skin care regimen may not be expected to have an impact on the health status dimension, it has been reported that the use of an effective skin care regimen may have a positive effect on QoL 31 and we observed significant improvements for the vast majority of responses for the self‐esteem and social effect dimensions. In previous publications on the role of estrogen HRT in skin aging, the visible signs of dryness, wrinkles, and sagging contributed to an increased perception of aging and decreased attractiveness 38 with a significant impact on QoL. MSkinQoL was previously demonstrated to distinguish postmenopausal women from non‐menopausal women. After 4 weeks of treatment with a specially developed oil/water skincare product, the menopausal group showed improvements in their skin status as well as a concomitant but moderate improvement of the three MSkinQoL scores. 31
While cosmetics are not treatments for diseased skin conditions, several studies have provided evidence that dermatocosmetics containing effective compounds are able to markedly improve skin appearance in a measurable manner. 39 , 40 , 41 , 42 , 43 Among them, proxylane has been shown to reduce visible signs of skin aging and improve the sebum composition of the skin in postmenopausal women in randomized studies. 14
The main limitation of this study is the lack of a control group. However, the majority of women in both groups were using cream and/or moisturizer (96% in the menopause group and 86% in the perimenopause group) on a daily basis before the study and so improvements observed were not simply due to applying a product, especially as we saw improvements in both groups. Other limitations were the inclusion of only European women, and the short study duration, as well as the possible effect of other factors on the skin, for example, photoaging due to sun exposure. On the other hand, the short study period between March and May was selected to limit any variations in skin tone due to sun exposure.
5. CONCLUSIONS
The use of anti‐aging dermocosmetics specifically designed for women in perimenopause and menopause, containing proxylane and cassia extract, significantly improved wrinkles and vascular signs and increased skin hydration after 2 months of application (day cream, night cream, and serum) in both menopausal and perimenopausal women. Also, these dermocosmetic routines had a positive impact on QoL (social and self‐esteem dimensions). These findings highlight the importance of dermocosmetics specifically targeting skin issues that occur during peri‐menopause and menopause.
CONFLICT OF INTEREST STATEMENT
FF and CD are employees of L'Oréal Research & Innovation Dept and RJ is employee of the Modiface company. SLM is an employee of Laboratoires Vichy and DK was an employee of Laboratoires Vichy at the time the study was conducted. ER and MK received thematically relevant honoraria from L'Oreal. CCZ has received thematically relevant honoraria from L'Oreal, NAOS/Bioderma, and Laboratoires Vichy. TP has received grants and honorariums from L'Oréal. TH has no conflicts of interest to declare.
ETHICS STATEMENT
Ethics committee approval was not required for this consumer test of a dermocosmetic product. All subjects were fully informed about the objectives of the study and provided signed informed consent (in French) which specified that their photographs were totally confidential (blind‐coded) and would be deleted after analysis.
ACKNOWLEDGEMENTS
The study and medical writing assistance were supported by Laboratoires Vichy. The authors want to thank Aurelie Abric, Aurelie Maudet, Thierry Lageat, Frederique Labatut, Elena Catalan Martin, Laura Murphy, Geraldine Lecot, Jeff Houghton, Yuze Zhang, Camille Kroely, Olivier Coubard, Vania Lacascade and Marco Vicic for their help with the study and their support and enthusiasm. Writing assistance was provided by Helen Simpson PhD, CMPP™, of My Word Medical Writing.
Flament F, Jiang R, Delaunay C, et al. Evaluation of adapted dermocosmetic regimens for perimenopausal and menopausal women using an artificial intelligence‐based algorithm and quality of life questionnaires: An open observational study. Skin Res Technol. 2023;29:e13349. 10.1111/srt.13349
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Passeron T, Krutmann J, Andersen ML, Katta R, Zouboulis CC. Clinical and biological impact of the exposome on the skin. J Eur Acad Dermatol Venereol. 2020;34(4):4‐25. doi: 10.1111/jdv.16614 [DOI] [PubMed] [Google Scholar]
- 2. Zouboulis CC, Blume‐Peytavi U, Kosmadaki M, et al. Skin, hair and beyond: the impact of menopause. Climacteric. 2022;25(5):434‐442. doi: 10.1080/13697137.2022.2050206 [DOI] [PubMed] [Google Scholar]
- 3. Zouboulis CC, Chen WC, Thornton MJ, Qin K, Rosenfield R. Sexual hormones in human skin. Horm Metab Res. 2007;39(2):85‐95. doi: 10.1055/s-2007-961807 [DOI] [PubMed] [Google Scholar]
- 4. Raine‐Fenning NJ, Brincat MP, Muscat‐Baron Y. Skin aging and menopause : implications for treatment. Am J Clin Dermatol. 2003;4(6):371‐378. doi: 10.2165/00128071-200304060-00001 [DOI] [PubMed] [Google Scholar]
- 5. Maheux R, Naud F, Rioux M, et al. A randomized, double‐blind, placebo‐controlled study on the effect of conjugated estrogens on skin thickness. Am J Obstet Gynecol. 1994;170(2):642‐649. doi: 10.1016/s0002-9378(94)70242-x [DOI] [PubMed] [Google Scholar]
- 6. Sauerbronn AV, Fonseca AM, Bagnoli VR, Saldiva PH, Pinotti JA. The effects of systemic hormonal replacement therapy on the skin of postmenopausal women. Int J Gynaecol Obstet. 2000;68(1):35‐41. doi: 10.1016/s0020-7292(99)00166-6 [DOI] [PubMed] [Google Scholar]
- 7. Piérard‐Franchimont C, Piérard GE. Postmenopausal aging of the sebaceous follicle: a comparison between women receiving hormone replacement therapy or not. Dermatology. 2002;204(1):17‐22. doi: 10.1159/000051804 [DOI] [PubMed] [Google Scholar]
- 8. Rittié L, Kang S, Voorhees JJ, Fisher GJ. Induction of collagen by estradiol: difference between sun‐protected and photodamaged human skin in vivo. Arch Dermatol. 2008;144(9):1129‐11240. doi: 10.1001/archderm.144.9.1129 [DOI] [PubMed] [Google Scholar]
- 9. Stevenson S, Thornton J. Effect of estrogens on skin aging and the potential role of SERMs. Clin Interv Aging. 2007;2(3):283‐297. doi: 10.2147/cia.s798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hall G, Phillips TJ. Estrogen and skin: the effects of estrogen, menopause, and hormone replacement therapy on the skin. J Am Acad Dermatol. 2005;53(4):555‐568. quiz 569‐72. doi: 10.1016/j.jaad.2004.08.039 [DOI] [PubMed] [Google Scholar]
- 11. Research on the menopause in the 1990s. Report of a WHO Scientific Group. World Health Organ Tech Rep Ser. 1996;866:1‐107. [PubMed] [Google Scholar]
- 12. Pineau N, Bernerd F, Cavezza A, Dalko‐Csiba M, Breton L. A new C‐xylopyranoside derivative induces skin expression of glycosaminoglycans and heparan sulphate proteoglycans. Eur J Dermatol. 2008;18(1):36‐40. doi: 10.1684/ejd.2008.0308 [DOI] [PubMed] [Google Scholar]
- 13. Deloche C, Minondo AM, Bernard BA, et al. Effect of C‐xyloside on morphogenesis of the dermal epidermal junction in aged female skin. An ultrastuctural pilot study. Eur J Dermatol. 2011;21(2):191‐196. doi: 10.1684/ejd.2010.1225 [DOI] [PubMed] [Google Scholar]
- 14. Bouloc A, Roo E, Moga A, Chadoutaud B, Zouboulis CC. A compensating skin care complex containing pro‐xylane in menopausal women: results from a multicentre, evaluator‐blinded, randomized study. Acta Derm Venereol. 2017;97(4):541‐542. doi: 10.2340/00015555-2572 [DOI] [PubMed] [Google Scholar]
- 15. Limtrakul P, Yodkeeree S, Thippraphan P, Punfa W, Srisomboon J. Anti‐aging and tyrosinase inhibition effects of Cassia fistula flower butanolic extract. BMC Complement Altern Med. 2016;16(1):497. doi: 10.1186/s12906-016-1484-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ahmed SI, Hayat MQ, Tahir M, et al. Pharmacologically active flavonoids from the anticancer, antioxidant and antimicrobial extracts of Cassia angustifolia Vahl. BMC Complement Altern Med. 2016;16(1):460. doi: 10.1186/s12906-016-1443-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rasmont V, Valois A, Gueniche A, et al. Vichy volcanic mineralizing water has unique properties to strengthen the skin barrier and skin defenses against exposome aggressions. J Eur Acad Dermatol Venereol. 2022;36(2):5‐15. doi: 10.1111/jdv.17784 [DOI] [PubMed] [Google Scholar]
- 18. Tan CL, Chin T, Tan CYR, et al. Nicotinamide metabolism modulates the proliferation/differentiation balance and senescence of human primary keratinocytes. J Invest Dermatol. 2019;139(8):1638‐1647.e3. doi: 10.1016/j.jid.2019.02.005 [DOI] [PubMed] [Google Scholar]
- 19. Tanno O, Ota Y, Kitamura N, Katsube T, Inoue S. Nicotinamide increases biosynthesis of ceramides as well as other stratum corneum lipids to improve the epidermal permeability barrier. Br J Dermatol. 2000;143(3):524‐531. doi: 10.1111/j.1365-2133.2000.03705.x [DOI] [PubMed] [Google Scholar]
- 20. Gehring W. Nicotinic acid/niacinamide and the skin. J Cosmet Dermatol. 2004;3(2):88‐93. doi: 10.1111/j.1473-2130.2004.00115.x [DOI] [PubMed] [Google Scholar]
- 21. Kawada A, Konishi N, Oiso N, Kawara S, Date A. Evaluation of anti‐wrinkle effects of a novel cosmetic containing niacinamide. J Dermatol. 2008;35(10):637‐642. doi: 10.1111/j.1346-8138.2008.00537.x [DOI] [PubMed] [Google Scholar]
- 22. Al‐Niaimi F, Chiang NYZ. Topical vitamin C and the skin: mechanisms of action and clinical applications. J Clin Aesthet Dermatol. 2017;10(7):14‐17. [PMC free article] [PubMed] [Google Scholar]
- 23. Burke KE. Interaction of vitamins C and E as better cosmeceuticals. Dermatol Ther. 2007;20(5):314‐321. doi: 10.1111/j.1529-8019.2007.00145.x [DOI] [PubMed] [Google Scholar]
- 24. Papakonstantinou E, Roth M, Karakiulakis G. Hyaluronic acid: A key molecule in skin aging. Dermatoendocrinol. 2012;4(3):253‐258. doi: 10.4161/derm.21923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Green BA, Yu RJ, Van Scott EJ. Clinical and cosmeceutical uses of hydroxyacids. Clin Dermatol. 2009;27(5):495‐501. doi: 10.1016/j.clindermatol.2009.06.023 [DOI] [PubMed] [Google Scholar]
- 26. Saint‐Léger D, Lévêque JL, Verschoore M. The use of hydroxy acids on the skin: characteristics of C8‐lipohydroxy acid. J Cosmet Dermatol. 2007;6(1):59‐65. doi: 10.1111/j.1473-2165.2007.00296.x [DOI] [PubMed] [Google Scholar]
- 27. Bravo B, Correia P, Gonçalves Junior JE, Sant'Anna B, Kerob D. Benefits of topical hyaluronic acid for skin quality and signs of skin aging: From literature review to clinical evidence. Dermatol Ther. 2022;35(12):e15903. doi: 10.1111/dth.15903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jiang R, Kezele I, Levinshtein A, et al. A new procedure, free from human assessment that automatically grades some facial skin structural signs. Comparison with assessments by experts, using referential atlases of skin ageing. Int J Cosmet Sci. 2019;41(1):67‐78. doi: 10.1111/ics.12512 [DOI] [PubMed] [Google Scholar]
- 29. Caberlotto E, Cornillon C, Njikeu S, Monot M, Vicic M, Flament F. Synchronized in vivo measurements of skin hydration and trans‐epidermal water loss. Exploring their mutual influences. Int J Cosmet Sci. 2019;41(5):437‐442. doi: 10.1111/ics.12556 [DOI] [PubMed] [Google Scholar]
- 30. Ye L, Wang Z, Li Z, Lv C, Man MQ. Validation of GPSkin Barrier() for assessing epidermal permeability barrier function and stratum corneum hydration in humans. Skin Res Technol. 2019;25(1):25‐29. doi: 10.1111/srt.12590 [DOI] [PubMed] [Google Scholar]
- 31. Segot‐Chicq E, Fanchon C. Quality of life in postmenopausal women: translation and validation of MSkinQoL questionnaire to measure the effect of a skincare product in USA. J Cosmet Dermatol. 2013;12(4):267‐274. doi: 10.1111/jocd.12064 [DOI] [PubMed] [Google Scholar]
- 32. Zouboulis CC, Boschnakow A. Chronological ageing and photoageing of the human sebaceous gland. Clin Exp Dermatol. 2001;26(7):600‐607. doi: 10.1046/j.1365-2230.2001.00894.x [DOI] [PubMed] [Google Scholar]
- 33. Brincat M, Kabalan S, Studd JW, Moniz CF, de Trafford J, Montgomery J. A study of the decrease of skin collagen content, skin thickness, and bone mass in the postmenopausal woman. Obstet Gynecol. 1987;70(6):840‐845. [PubMed] [Google Scholar]
- 34. Grinich EE, Shah AV, Simpson EL. Validation of a novel smartphone application‐enabled, patient‐operated skin barrier device. Skin Res Technol. 2019;25(5):612‐617. doi: 10.1111/srt.12692 [DOI] [PubMed] [Google Scholar]
- 35. Berardesca E, Bonfigli A, Cribier B, et al. A split‐face study assessing the clinical benefit, tolerability and subject satisfaction of a dermocosmetic in subjects with rosacea associated with erythema and sensitive skin. Clin Cosmet Investig Dermatol. 2020;13:751‐758. doi: 10.2147/ccid.S266879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Flament F, Hofmann M, Roo E, et al. An automatic procedure that grades some facial skin structural signs: agreements and validation with clinical assessments made by dermatologists. Int J Cosmet Sci. 2019;41(5):472‐478. doi: 10.1111/ics.12563 [DOI] [PubMed] [Google Scholar]
- 37. Flament F, Maudet A, Ye C, et al. Comparing the self‐perceived effects of a facial anti‐aging product to those automatically detected from selfie images of Chinese women of different ages and cities. Skin Res Technol. 2021;27(5):880‐890. doi: 10.1111/srt.13037 [DOI] [PubMed] [Google Scholar]
- 38. Lephart ED. A review of the role of estrogen in dermal aging and facial attractiveness in women. J Cosmet Dermatol. 2018;17(3):282‐288. doi: 10.1111/jocd.12508 [DOI] [PubMed] [Google Scholar]
- 39. Lephart ED, Naftolin F. Menopause and the skin: old favorites and new innovations in cosmeceuticals for estrogen‐deficient skin. Dermatol Ther. 2021;11(1):53‐69. doi: 10.1007/s13555-020-00468-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Raab S, Yatskayer M, Lynch S, Manco M, Oresajo C. Clinical evaluation of a multi‐modal facial serum that addresses hyaluronic acid levels in skin. J Drugs Dermatol. 2017;16(9):884‐890. [PubMed] [Google Scholar]
- 41. Holzer G, Riegler E, Hönigsmann H, Farokhnia S, Schmidt JB. Effects and side‐effects of 2% progesterone cream on the skin of peri‐ and postmenopausal women: results from a double‐blind, vehicle‐controlled, randomized study. Br J Dermatol. 2005;153(3):626‐634. doi: 10.1111/j.1365-2133.2005.06685.x [DOI] [PubMed] [Google Scholar]
- 42. Creidi P, Faivre B, Agache P, Richard E, Haudiquet V, Sauvanet JP. Effect of a conjugated oestrogen (Premarin) cream on ageing facial skin. A comparative study with a placebo cream. Maturitas. 1994;19(3):211‐223. doi: 10.1016/0378-5122(94)90074-4 [DOI] [PubMed] [Google Scholar]
- 43. Wang ST, Neo BH, Betts RJ. Glycosaminoglycans: sweet as sugar targets for topical skin anti‐aging. Clin Cosmet Investig Dermatol. 2021;14:1227‐1246. doi: 10.2147/ccid.S328671 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


