Abstract
The purpose of this study was to identify message features that motivate patients to initiate clinical conversations about Chronic Obstructive Pulmonary Disease (COPD). A secondary aim was to determine whether preferred message features vary by socio-demographic and behavioral characteristics. A discrete choice experiment was conducted in August 2020. Participants were asked to select which messages would motivate them to speak with a clinician about COPD. This included selecting messages across 8 choice sets, or a systematic combination of messages reflecting 6 attributes (e.g., susceptibility, call-to-action, emotion-frame, efficacy, message source, organizational support). The final sample was 928, which included adults (M = 62.07; SD = 10.14 years old) who identified as non-Hispanic, white, and with at least some college experience. Message attributes ranked from most to least important were COPD susceptibility (25.53% [95% CI = 24.39, 26.66]), message source (19.32% [95% CI = 18.41–20.24]), COPD organization logo (19.13%; [95% CI = 18.26, 20.01]), call-to-action (14.12%; [95% CI = 13.40, 14.85], emotion-frame (13.24% [95% CI = 12.55–13.94]), and efficacy (8.65%; [95% CI = 8.20–9.09]). Participants preferred susceptibility messages about COPD signs/symptoms rather than risk behaviors related to smoking tobacco and environmental exposures. They also preferred messages from medical authorities (i.e., clinicians, COPD organization), a call-to-action that supports their autonomy in screening decision-making, and a message that conveys hope for living a healthy life with COPD and builds their self-efficacy to get screened. Differences in message preferences were detected according to age, gender, race, ethnicity, education level, and current vs. former smoking status. This study identified message features that motivate clinical conversations about COPD, especially those from subgroups who are disproportionately at-risk for its late-stage diagnosis.
Keywords: COPD, Health communication, Discrete choice experiment, Intervention
Highlights
-
•
We uncovered message features to increase clinical discussions about COPD screening.
-
•
Patients prefer screening messages conveying symptom susceptibility vs. risk behaviors.
-
•
Messages from medical authorities (e.g., clinicians, COPD organization) are preferred.
-
•
A call-to-action that supports patient autonomy to talk with a clinician is important.
-
•
Evoking hope for early detection with screening self-efficacy is a key message feature.
1. Introduction
Chronic Obstructive Pulmonary Disease (COPD) caused 3.23 million deaths worldwide in 2019 [1], and it is estimated that approximately 70% of symptomatic adults (e.g., dyspnea, wheezing) are unaware they are living with COPD [2]. Signs and symptoms of COPD typically begin to appear by age 35 [3]. The US Preventive Services Task Force and the Global Initiative for Chronic Obstructive Lung Disease recommends that symptomatic patients receive a spirometry test under the supervision of a clinician [4,5]. A spirometry test is a pulmonary function test that measures an individual's forced vital capacity (FVC) and forced expiratory volume (FEV1), or how much and how quickly a person can exhale [5]. Underdiagnosis of COPD has been attributed to limited spirometry access, but there are also patient-oriented factors that contribute to underdiagnosis, including poor COPD knowledge, negative emotion surrounding a diagnosis, and underestimating their respiratory symptoms are from a smoking history or another comorbidity [2,[6], [7], [8]]. The National Institutes of Health, Centers for Disease Control and Prevention, The COPD Foundation, and other health organizations offer educational resources to inform the general public about COPD and the importance of early detection (e.g., opportunity to prescribe appropriate pharmacological treatment to patients and refer them to evidence-based, behavioral solutions for proactively addressing risk factors and reducing complications during a time when their FEV1 is rapidly declining [2,3]), but it is unknown whether this information alone motivates adults to speak with a clinician about COPD.
Adults who reside in rural regions, especially those living with a low socioeconomic status and report a history of smoking tobacco, are disproportionately affected by COPD [9,10], and they are subgroup of the population likely to be undiagnosed or receive a late-stage diagnosis [10]. A recent study found that current smokers are motivated to speak with their clinician about COPD after completing a risk assessment that instructs them to speak with a clinician [11]. However, the relationship between smoking status and talking with a clinician about COPD was no longer statistically significant after adjusting for rurality, income, and education among other demographic variables. Accordingly, there is a need to understand which messages motivate individuals to talk with a clinician about COPD according to socio-demographics and smoking tobacco status (current vs. former). This evidence will inform efforts to optimize tailored messaging for underserved, high-risk patient groups to improve patient-clinician communication about COPD. Maximizing efforts to promote the early detection of COPD is a goal outlined in the COPD National Action Plan [12]. The purpose of this study was two-fold: (1) to identify message features that motivate patients to initiate conversations with their clinician about COPD; and (2) to determine whether preferred message features vary according to patients' socio-demographic (e.g., age, gender, race, ethnicity) and disease-specific (e.g., smoking status, COPD risk score) characteristics.
2. Methods
In August 2020, we recruited a sample of US adults from a Qualtrics panel to complete a 15-min online survey. The sample was stratified by smoking status (50% every/someday smokers and 50% former smokers) and rurality (50% rural and 50% non-rural). Participants were screened for eligibility, and they had the opportunity to complete the survey if they (1) had never been diagnosed with COPD by a clinician; (2) smoked at least 100 cigarettes in their lifetime; and (3) were at least 35 years old. After completing the screening questions, eligible participants were directed to complete socio-demographic questions followed by a discrete choice experiment (DCE). A total of 928 eligible adults completed the DCE. Participants received a $5 e-gift card for their participation. Institutional Review Board (#201800755) approval was obtained for the study and secured prior to data collection.
2.1. Discrete choice experiment
A DCE is a patient- and preference-driven method to strategically identify the combination of attributes that yield the highest probability of “selling” a health product or program to an intended audience [13]. DCEs are a quantitative method with theoretical underpinnings in experimental design theory, economic theory of consumer behavior, and random utility theory [13,14]. The method statistically demonstrates how participants are willing to actively choose between different attribute levels to inform a health decision [15,16].
2.1.1. Choice set design
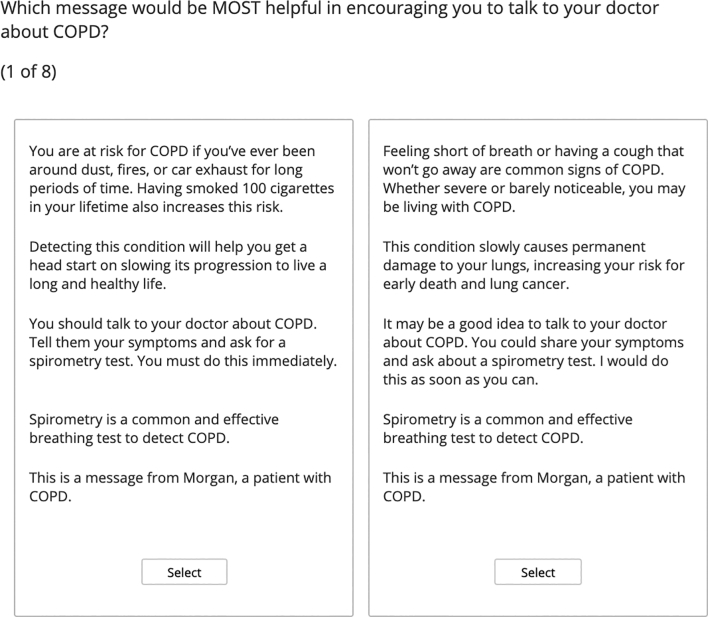
We followed best practices in DCE choice set design, including 6 mutually exclusive attributes at 2 levels [17]. Table 1 shows these attributes and their corresponding levels. According to the Persuasive Message Framework, effective health communication messages (1) tell someone they are susceptible to a condition, (2) evoke an emotion about the condition that motivates one to act (e.g., fear- or hope-appeals), and (3) tell them they have the skills and resources to act (e.g., self- and response efficacy) [18]. Peripheral cues (e.g., the source of the message) strengthen the persuasive effects of a message. In this study, we tested preferences across two sources of information – the person who is relaying the message (i.e., clinician vs. patient) and the overseeing agency or resource that is hosting the message [18]. A call-to-action is highly recommended in public-facing messages to ensure that the intended audience knows what to do [19]. We included two call-to-action levels – an autonomy-supportive message where recommendations are provided in a way that supports a choice, and a controlling-directive message where people are told what to do without offering a choice. The content in Table 1 representing messages for each attribute level were designed through an iterative process. First, a team of experts in health behavior change, health message design, patient-provider communication, and a family medicine clinician designed the messages. Next, 100 adults who were members of the study's target population provided feedback about message effectiveness (i.e., clarity, believable, informative, relevant). The messages were refined prior to testing. Fig. 1 shows an example choice set with two options reflecting these attributes and different levels.
Table 1.
Message attributes and content representing each level.
| Attribute | Levels | Message Content |
|---|---|---|
| Susceptibility |
|
|
|
|
|
| Emotion Frame |
|
|
|
|
|
| Call-to-Action |
|
|
| Efficacy Frame |
|
|
|
|
|
| Message Source |
|
|
|
|
|
| COPD Organization Logo |
|
 |
Fig. 1.
Example of a choice set.
Note. Each choice set includes two options from which a participant was instructed to choose one. Each option reflects messages with six standard attributes at varying levels.
2.1.2. Experimental design
The DCE included a series of 8 choice sets created by the choice-based conjoint feature of Sawtooth Software v9.9.2 [20]. Given the number of attributes and levels, we needed to use a fractional factorial design to reduce the number of the choice sets participants would review. Each choice set included two options for which a participant was instructed to select as being most helpful in encouraging them to talk to a doctor about COPD. The two options in each choice set included a standard set of six attributes but a different combination of levels (See Table 1). The presentation of these levels was determined according to statistical properties of the fractional factorial design, which was managed and executed via the DCE software. Please note that in the results and discussion sections, the preferred attribute levels across choice sets are referred to as “messages” for purposes of clarity and practical transferability.
2.2. Data analysis
Hierarchical Bayes estimations for choice-based conjoint (CBC/HB) analyses of individual level utilities were conducted with Sawtooth Software v.9.9.2 [20]. Individual estimates for each attribute were averaged after 10,000 random draws. A series of independent samples t-tests were conducted with SPSS v27 to examine differences in average utility scores (normalized, zero-centered) of each attribute's highest ranking message option according to sociodemographic variables (e.g., age, gender, race, rurality). Utility scores were transformed into probability scaled scores (i.e., relative importance scores), which allowed for comparisons across attributes. The importance score defines how much impact the attribute had upon choice, given the range of message attributes under evaluation. Importance scores were calculated as percentages and summed to 100% across all message attributes.
3. Results
3.1. Sample characteristics
Table 2 shows sample demographics, who were 62.07 (SD = 10.14) years old on average and predominantly non-Hispanic White with at least some college experience. Approximately 75% (n = 646) of participants reported a low COPD risk on a validated instrument to measure COPD risk [21], and the remaining 25% reported a high COPD risk.
Table 2.
Socio-demographics, N = 928.
| Variable | n (%) |
|---|---|
| Age, M (SD) | 62.07 (10.14) |
| Gender, n (%) | |
| Male | 474 (51.1) |
| Female | 451 (48.6) |
| Missing | 3 (0.3) |
| Race, n (%) | |
| White | 831 (89.5) |
| Non-White | 97 (10.5) |
| Ethnicity, n (%) | |
| Hispanic | 31 (3.3) |
| Non-Hispanic | 890 (95.9) |
| Missing | 7 (0.8) |
| Annual Income, n (%) | |
| Less than $49,999 | 377 (40.6) |
| $50,000 or more | 540 (58.2) |
| Missing | 11 (1.2) |
| Education, n (%) | |
| High school or less | 197 (21.2) |
| At least some college | 731 (78.8) |
3.2. Importance and preferences of message attributes
Table 3 shows the results from the Hierarchical Bayes estimations for choice-based conjoint (CBC/HB) analysis. Susceptibility was ranked as the most important attribute (25.53%). And according to the utility scores, participants preferred learning about susceptibility of COPD based on its symptoms rather than behavioral risk exposures (e.g., smoking status). Following susceptibility, the source of the message (19.32%) and a message that included a COPD organization logo (19.13%) reported a similar level of high importance. Utility scores indicated that participants generally preferred a message from a clinician rather than a patient, and they preferred a message that includes a reputable COPD organization logo. A call-to-action (14.12%) and an emotion frame (13.24%) were ranked as less important. However, when they were included, participants reported a higher utility score for autonomy-supportive language (i.e., “You could…”, “I would…”) rather than controlling-directive language (i.e., “You should…”, “Tell them…”). They also preferred messages that evoke a feeling of hope rather than fear. The efficacy frame was ranked as the least important message attribute (8.65%). However, if efficacy-building content was included, then participants preferred a message outlining how easy it is to complete a spirometry test (i.e., self-efficacy) than how effective a spirometry test is to detect COPD (i.e., response efficacy).
Table 3.
Results from the hierarchical bayes estimations of importance scores.
| Message Attributes | Importance Scores |
Utility Scores |
||||
|---|---|---|---|---|---|---|
| Scorea, (SD) |
Lower 95% CI | Upper 95% CI | Score, (SD) |
Lower 95% CI |
Upper 95% CI |
|
| Susceptibility | 25.53 (17.70) | 24.39 | 26.66 | |||
| Symptoms (vs. Risk Exposure) | 8.81 (92.80) | 2.84 | 14.78 | |||
| Emotion Frame | 13.24 (10.78) | 12.55 | 13.94 | |||
| Hope (vs. Fear) | 4.22 (51.07) | 0.93 | 7.50 | |||
| Call-to-Action | 14.12 (11.19) | 13.40 | 14.85 | |||
| Autonomy-Supportive (vs. Controlling-Directive) | 18.26 (50.90) | 14.99 | 21.54 | |||
| Efficacy Frame | 8.65 (6.88) | 8.20 | 9.09 | |||
| Self-Efficacy (vs. Response Efficacy) | 8.72 (31.99) | 6.66 | 10.78 | |||
| Message Source | 19.32 (14.32) | 18.41 | 20.24 | |||
| Clinician (vs. Patient) | 28.03 (66.30) | 23.76 | 32.29 | |||
| COPD Organization Logo | 19.13 (13.63) | 18.26 | 20.01 | |||
| Included (vs. Excluded) | 39.24 (58.56) | 35.47 | 43.01 | |||
Note.aSum of importance scores is 100%.
3.3. Preference by socio-behavioral factors
Age and Gender. Compared with younger adults (35–64 years old), adults ages 65 and older reported a greater preference for receiving a message from a clinician, (p < .05). Women reported a greater preference than men for call-to-action messages that use autonomy-supportive language (p < .01).
Race. Compared with white participants, non-white participants reported greater preference for messages that communicate hope surrounding the benefit of a timely COPD diagnosis as opposed to threats of a late-stage diagnosis (p < .01). Although not reaching statistical significance, white participants reported a greater preference than non-white participants for messages communicated from a clinician rather than another patient (p = .07).
Ethnicity. Non-Hispanic participants reported a greater preference than Hispanic participants for messages that communicate susceptibility to COPD in terms of symptoms rather than risk behaviors (p < .05). Non-Hispanic participants preferred a call-to-action message that uses autonomy-supportive language (p < .05) and displays a COPD organization logo (p < .05). These findings should be interpreted with caution, given the low proportion of Hispanic adults recruited into this survey study.
Education, Income, and Rurality. Compared with their less educated counterparts, participants with at least some college education preferred messages that use autonomy-supportive language rather than controlling-directive language (p = .05). They also preferred a message from a clinician rather than another patient (p < .05). There were no statistically significant differences in message preferences according to income and rurality.
Smoking status and COPD risk. Compared with current smokers, former smokers had a greater preference for messages that communicated susceptibility about COPD according to symptoms (e.g., shortness of breath) rather than behavioral risks (e.g., smoking behaviors) (p < .01). Former smokers, however, reported a greater preference for a call-to-action message that employed autonomy-supportive language (p < .01) and they reported a greater preference for a message that includes a COPD organization logo (p < .01). There was no significant difference in message preference according to COPD risk score.
4. Discussion and conclusion
To our knowledge, this is the first study to investigate which messages motivate adults to speak with their clinician about COPD. In general, participants had a strong preference for messages from healthcare experts that communicate susceptibility to COPD. Message preferences varied across socio-demographic subgroups, including age, gender, race, ethnicity, education level, and current smoking status. Findings have important implications for redesigning COPD screening messages, such as tailoring elements for specific subgroups of the population who are at the greatest risk for COPD and its late-stage diagnosis.
4.1. Discussion
Promoting susceptibility to COPD was the most important message attribute in motivating participants to talk with their clinician about the disease. This is not surprising, given that people are most likely to pay attention to messages that are relevant to them and because perceived susceptibility is a common construct of behavior change theories [22,23]. However, participants preferred susceptibility to be communicated in the form of signs and symptoms (e.g., shortness of breath, persistent cough) rather than based on prior risks exposures and behaviors (e.g., breathing in dust or exhaust, smoking 100 cigarettes in their lifetime). This is surprising, given that all the participants in this study had a history of smoking at least 100 cigarettes in their lifetime but not everyone experienced the symptoms of COPD (e.g., cough, persistent cough). The preference for symptom-based susceptibility messaging was strongest among current smokers and non-Hispanic adults, as compared with former smokers and their Hispanic counterparts. It is possible that perceptions of stigma were a driving force in preferences surrounding the symptoms of COPD rather than behavioral risks.
The source of the message also had a strong impact on motivations to talk with a clinician about COPD. Participants preferred messages from medical authorities, which included a clinician and a healthcare organization dedicated to advancing COPD research and care. Healthcare providers followed by government healthcare organizations have remained the most trusted sources of health information in the US since 2005 [24]. However, findings demonstrated that certain subgroups of the population are more motivated to speak with a clinician about COPD if they receive a message from a medical authority. This includes adults who are older (65+ years old), non-Hispanic, white, college educated, and identify as former smokers. There is a long history of medical distrust among racial/ethnic minority and low socioeconomic populations [25], and this study demonstrates that messages featuring both clinicians and patients may be the key to motivating minority groups to discuss their risk for COPD with a clinician. Prior research has found that current smoking status is a predictor of discussing respiratory ailments with clinicians [11,26]; however, this is the first study to demonstrate that messages from medical authorities significantly motivates former smokers to talk with a clinician about COPD.
A call-to-action was a moderately important message attribute in motivating adults to talk with a clinician about COPD. Participants preferred a message that supported their autonomy in the decision to talk with a clinician about COPD as opposed to a message with a demanding, directive tone. This was especially true for non-Hispanic adults, women, individuals with a college education and former smokers. Research has demonstrated value in using autonomy-supportive language in long-term adherence to public health recommendations [27]. However, future research is needed to understand why this message was preferred among former smokers and whether a lessening sense of urgency is communicated through this call-to-action.
The emotional frame used in the messaging had less of an impact on motivations to speak with a clinician about COPD, as compared with susceptibility, source of message, and call-to-action. When emotional messaging was used, participants preferred a message that was designed to evoke a feeling of hope rather than fear. The preference for hope was especially strong for racial minority participants as compared to their white counterparts. This is consistent with prior research demonstrating that hope is a protective factor against psychological distress among non-Hispanic Black/African American adults [28]. Findings of this study suggest that hope is a key ingredient for messages intending to motivate people to speak with their clinicians about COPD, especially racial minorities.
Efficacy was identified as the least important message feature. This is surprising given that self-efficacy is one of the strongest predictors of behavior change intention and action [29]. However, when efficacy was included in messages intended to promote clinical conversations about COPD, participants preferred messages that promoted self-efficacy rather than response efficacy. Prior research has found a linkage between self-efficacy and hope within a fearful context, wherein a person who feels hopeful and confident in their ability to carry out a behavior is most likely to engage in the recommended behavior [30]. Messages that include hope appeals should incorporate self-efficacy to ensure that the emotion is maximized, and a key ingredient of behavior change is present.
The results of this study should be interpreted with caution. First, the DCE method used in this study resulted in patient preferences for message features that respondents believe will increase the likelihood of speaking with a clinician about COPD in the future. Future research is needed to evaluate the external validity of the findings. Second, our sample may not be representative of the general US population that is at-risk for COPD. We collected a large sample of US adults from a panel of Internet-using adults stratified by geographic region (rural vs. non-rural) and smoking status (current vs. former), but future research should consider other risk factors such as air-quality, occupational setting, and region of the nation (e.g., southeast).
4.2. Innovation
Beyond offering insight to designing messages that promote clinical conversations about COPD, results of this study bring attention to existing communication interventions and their potential impact on motivating (or demotivating) patient-clinician communication about COPD. The Tips from Former Smokers (Tips®) campaign has been successful in reducing tobacco use in the US. The campaign targets adults (18–54 years old) by using evocative fear- and disgust-inducing narrative messages that denormal tobacco and build knowledge about tobacco-associated illnesses [31]. Tips® has been highly successful, as it was responsible for 522,000 sustained quit smoking attempts between 2012 and 2015 [32]. In recent years, the campaign has added disease-specific campaign messages, including gender-tailored COPD messages detailing the severe effects of the disease that are often present during late-stage diagnosis. Although the study increases knowledge about the linkage between smoking tobacco and COPD, the results of this study suggest that the Tips® campaign may inadvertently demotivate current and former smokers from discussing their COPD risk with a clinician. However, given that the campaign is from a medical authority (i.e., the Centers for Disease Control and Prevention), former smokers may be more inclined to initiate conversations with their clinicians about COPD than current smokers. The results of this study demonstrate potential adaptations to the Tips® campaign to support smoking cessation and early detection efforts in COPD.
5. Conclusion
Messages promoting clinical conversations about COPD should include information about susceptibility to the disease by highlighting the signs and symptoms of COPD from a medical authority, including a clinician or healthcare organization. Results also highlight that some message features must be emphasized when communicating with subgroups of the population who are at a disproportionately high risk for COPD and its late-stage diagnosis. Results should be considered in the context of designing new and refining existing communication to increase clinical conversations and screening for COPD.
Funding acknowledgement
This research was supported by the National Heart, Lung, and Blood Institute (F32HL143938).
Author statement
Conceptualization (SRP, JLK, MW, RS); Data Curation (SRP, JLK, RS); Formal Analysis (SRP, RS); Funding Acquisition (SRP); Investigation (SRP, JLK, MW, RS); Methodology (SRP, RS); Supervision (JLK, RS); Writing – original draft (SRP, RSP, JLK, MW).
Declaration of Competing Interest
SRP was an NIH-funded postdoctoral research fellow when this research was performed, results were interpreted, and manuscript was prepared for publication. She is currently an employee of Johnson & Johnson, Inc.
References
- 1.World Health Organization The top 10 causes of death. Top ten causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death December 9, 2020. Accessed November 8, 2021.
- 2.Diab N., Gershon A.S., Sin D.D., et al. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(9):1130–1139. doi: 10.1164/rccm.201804-0621CI. [DOI] [PubMed] [Google Scholar]
- 3.Antuni J.D., Barnes P.J. Evaluation of individuals at risk for COPD: beyond the scope of the global initiative for chronic obstructive lung disease. Chronic Obstr Pulm Dis (Miami) 2016;3(3):653–667. doi: 10.15326/jcopdf.3.3.2016.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Global Initiative for Chronic Obstructive Lung Disease . 2020. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. (2020 report). Published online. [Google Scholar]
- 5.US Preventive Services Task Force (USPSTF), Mangione C.M., Barry M.J., et al. Screening for chronic obstructive pulmonary disease: US Preventive Services Task Force reaffirmation and recommendation statement. JAMA. 2022;327(18):1806–1811. doi: 10.1001/jama.2022.5692. [DOI] [PubMed] [Google Scholar]
- 6.Lundell S., Wadell K., Wiklund M., Tistad M. Enhancing confidence and coping with stigma in an ambiguous interaction with primary care: a qualitative study of people with COPD. COPD. 2020;17(5):533–542. doi: 10.1080/15412555.2020.1824217. [DOI] [PubMed] [Google Scholar]
- 7.Russell S., Ogunbayo O.J., Newham J.J., et al. Qualitative systematic review of barriers and facilitators to self-management of chronic obstructive pulmonary disease: views of patients and healthcare professionals. NPJ Prim Care Respir Med. 2018;28(1):2. doi: 10.1038/s41533-017-0069-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ho T., Cusack R.P., Chaudhary N., Satia I., Kurmi O.P. Under- and over-diagnosis of COPD: a global perspective. Breathe (Sheff) 2019;15(1):24–35. doi: 10.1183/20734735.0346-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pleasants R.A., Riley I.L., Mannino D.M. Defining and targeting health disparities in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2016;11:2475–2496. doi: 10.2147/COPD.S79077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gaffney A.W., Hawks L., White A.C., et al. Health care disparities across the urban-rural divide: a National study of individuals with COPD. J Rural Health. 2020 doi: 10.1111/jrh.12525. Published online October 11. [DOI] [PubMed] [Google Scholar]
- 11.Paige S.R., Wilczewski H., Casale T.B., Bunnell B.E. Using a computer-tailored COPD screening assessment to promote advice-seeking behaviors. World Allergy Organiz J. 2021;14:100603. doi: 10.1016/j.waojou.2021.100603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institutes of Health COPD National Action Plan. 2017 https://www.nhlbi.nih.gov/health-topics/education-and-awareness/COPD-national-action-plan Accessed November 8, 2021. [Google Scholar]
- 13.Ryan M., Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy. 2003;2(1):55–64. [PubMed] [Google Scholar]
- 14.Lancsar E., Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–677. doi: 10.2165/00019053-200826080-00004. [DOI] [PubMed] [Google Scholar]
- 15.Louviere J.J., Flynn T.N., Marley A.A.J. Cambridge University Press; 2015. Best-worst scaling: Theory, methods and applications. [DOI] [Google Scholar]
- 16.Cheung K.L., Wijnen B.F.M., Hollin I.L., et al. Using best-worst scaling to investigate preferences in health care. Pharmacoeconomics. 2016;34(12):1195–1209. doi: 10.1007/s40273-016-0429-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mangham L.J., Hanson K., McPake B. How to do (or not to do) ... Designing a discrete choice experiment for application in a low-income country. Health Policy Plan. 2009;24(2):151–158. doi: 10.1093/heapol/czn047. [DOI] [PubMed] [Google Scholar]
- 18.Witte K. In: Designing health messages: Approaches from communication theory and public health practice. Maibach E.W., Parrott R.L., editors. Inc; Sage Publications: 1995. Using the persuasive health message framework to generate effective campaign messages; pp. 145–166. [Google Scholar]
- 19.U.S. Department of Health and Human Services Health communication playbook: Resources to help you create effective materials. 2018. https://www.cdc.gov/nceh/clearwriting/docs/health-comm-playbook-508.pdf Accessed November 9, 2021.
- 20.CBC/HB Technical Paper 2009. https://sawtoothsoftware.com/resources/technical-papers/cbc-hb-technical-paper Accessed November 9, 2021.
- 21.Martinez F.J., Raczek A.E., Seifer F.D., et al. Development and initial validation of a self-scored chronic obstructive pulmonary disease population screener questionnaire. COPD. 2008;5(2):85–95. doi: 10.1080/15412550801940721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrer R., Klein W.M. Risk perceptions and health behavior. Curr Opin Psychol. 2015;5:85–89. doi: 10.1016/j.copsyc.2015.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petty R.E., Cacioppo J.T. The elaboration likelihood model of persuasion. Adv Exp Soc Psychol. 1986;19:123–205. doi: 10.1016/S0065-2601(08)60214-2. [DOI] [Google Scholar]
- 24.Jackson D.N., Peterson E.B., Blake K.D., Coa K., Chou W.Y.S. Americans’ trust in health information sources: trends and sociodemographics predictors. Am J Health Promot. 2019;33:1187–1193. doi: 10.1177/0890117119861280. [DOI] [PubMed] [Google Scholar]
- 25.Armstrong K., Ravenell K.L., McMurphy S., Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97:1283–1289. doi: 10.2105/AJPH.2005.080762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carter-Harris L., Tan A.S.L., Salloum R.G., Young-Wolff K.C. Patient-provider discussions about lung cancer screening pre- and post-guidelines: health information national trends survey (HINTS) Patient Educ Couns. 2016;99:1772–1777. doi: 10.1016/j.pec.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Legate N., Weinstein N. Can we communicate autonomy support and a mandate? How motivating messages relate to motivation for staying at home across time during the COVID-19 pandemic. Health Commun. 2021:1–8. doi: 10.1080/10410236.2021.1921907. [DOI] [PubMed] [Google Scholar]
- 28.McIntosh R., Ironson G., Krause N. Keeping hope alive: racial-ethnic disparities in distress tolerance are mitigated by religious/spiritual hope among Black Americans. J Psychosom Res. 2021;144 doi: 10.1016/j.jpsychores.2021.110403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maddux J.E. In: The Oxford handbook of positive psychology. Ed. 2. Lopez S.J., Snyder C.R., editors. 2009. Self-efficacy: The power of believing you can. [DOI] [Google Scholar]
- 30.Uplifting fear appeals Considering the role of hope in fear-based persuasive messages. Health Commun. 2019;34:463–474. doi: 10.1080/10410236.2017.1422847. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention Tips from former smokers®. https://www.cdc.gov/tobacco/campaign/tips/index.html Retrieved from.
- 32.Murphy-Hoefer R., Davis K.C., Beistle D., King B.A., Duke J., Rodes R., et al. Impact of the tips from former smokers campaign on population-level smoking cessation, 2012-2015. Prev Chronic Dis. 2018;15:E71. doi: 10.5888/pcd15.180051. [DOI] [PMC free article] [PubMed] [Google Scholar]