Abstract
Objectives
Visual aids (VAs) seem effective to improve doctor-patient communication. The objective was to describe how VAs are used in consultation and what French general practitioners (GPs) expect of them.
Methods
Cross-sectional study using a self-administered questionnaire among French GPs in 2019. Descriptive and multinominal logistic regression analyses were performed.
Results
Of the 376 respondents, 70% used VAs at least weekly and 34% daily; 94% considered VAs useful/very useful; 77% felt they did not use VAs enough. Sketches were the most used VAs and considered the most useful. Younger age was significantly associated with a higher rate of use of simple digital images. VAs were mainly used to describe anatomy and facilitate patient comprehension. Main reasons for not using VAs more often were time spent searching, lack of habit and poor quality of available VAs. Many GPs requested a database of good quality VAs.
Conclusions
GPs use VAs regularly in consultations but would like to use them more often. Informing GPs of the usefulness of VAs, training them to draw adapted sketches and creating a good quality databank are some possible strategies to increase the use of VAs.
Innovation
This study described in detail the use of VAs as tool for doctor-patient communication.
Keywords: Medical illustration, Audiovisual aids, General practice, Health communication, Patient education as a topic, Surveys and questionnaires
Highlights
-
•
GPs often find visual aids as useful during consultations.
-
•
Information about utility of visual aids could increase their use.
-
•
The most used visual aids in general practice consultations are sketches.
-
•
Simple digital images are particularly appreciated by younger GPs.
-
•
GPs requested a digital database of good quality visual aids.
1. Introduction
1.1. Context
Good doctor-patient communication enables shared decision making and therapeutic education, which are two concepts promoted by many countries [1]. It also helps to improve health parameters [2,3], particularly in the context of individual education in general practice [4]. However, improvement needs to be made in terms of communication: much of the information delivered by doctors is not understood or retained by their patients [5], and patients feel that information sharing is insufficient [6]. In particular, there are significant inequalities in access to medical information depending on patients' health literacy levels. Fighting against these inequalities is currently one of the priorities of the High Council for Public Health to improve overall health in France [7].
Visual aids (VAs) are theoretically an ideal way to support medical communication. Research in education has shown that memory processing involves hearing in 11% of cases and vision in 83% of cases. Sixty percent of the population has a dominant visual memory [8].
According to the medical literature, VAs are popular with patients [[9], [10], [11]]. They have been shown to have a positive impact on information recall, comprehension, attention, adherence, and patient satisfaction, in particular for patients with low health literacy [[12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33]]. Effectiveness has been shown for media that can be used outside consultation and navigated by patients on their own (stand-alone VAs) such as illustrated written information [12,[21], [22], [23], [24]], illustrated prescriptions or medication leaflets [13,25,26], and digital VAs [[27], [28], [29], [30], [31], [32], [33]]. In other cases, the effectiveness of VAs is more controversial [[34], [35], [36], [37], [38], [39], [40], [41]].
Patient information tools are more effective if they are used during consultation and in the context of a caregiver-patient encounter [42,43]. General practice consultation is a privileged and effective place for individual health education for all types of patients [4,44]. Only two studies were found on the use of VAs in general practitioners (GPs)' consultations and they are discordant. On the one hand, a Swiss study reported that VAs were used to describe cardiovascular risk assessment in only 16% of the 70 consultations studied [45]. On the other hand, a medical thesis found that 62% of 117 GPs surveyed reported using VAs during their consultations in 2018. However, this study had several biases and this finding was a secondary outcome [46]. We found no studies exploring the opinion of GPs in France on the use of VAs and their perceived usefulness. Factors that may influence the use of VAs are not known. In the context of the controversy over the effectiveness of VAs [[34], [35], [36], [37], [38], [39], [40], [41]], it is important to know the opinion of GPs on their usefulness. Therefore, it seemed necessary to carry out this study.
We will use the term visual aid (VA) to refer to any communication tool that can be used in a consultation that relies mainly on the sense of sight (image, video, sketch, anatomical model, etc.).
1.2. Objectives
The main objective was to collect quantitative data on the use of VAs by French GPs in consultations with respect to their sociodemographic characteristics, the quality of the computer equipment in their workplace and the health literacy level of their registered patients.
The secondary objective was to propose possible strategies to increase the use of VAs based on GPs' expectations of them and perceptions of their usefulness.
2. Methods
2.1. Study design
This national cross-sectional study was conducted between March and April 2019 using online self-administered questionnaires. Data were reported in accordance with the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) criteria.
2.2. Inclusion and exclusion criteria
French physicians practicing in general practice (target population) were included. Questionnaires with no response to the questions of interest (except for respondents' characteristics) and duplicates (same respondents' characteristics) were excluded.
2.3. Recruitment
A survey invitation was sent to the mailing lists of departmental delegations of the French Medical Council willing to participate and the Department of General Practice at University Paris-Est Créteil. GPs were free to answer or not, and no incentives were provided. Respondents were able to review and change their answers before submission. Physicians meeting the inclusion criteria were identified with the first question of the survey.
2.4. Gathered data
The questionnaire was created on the secure and independent online survey platform Eval&Go. It was produced and reviewed by 3 academic GPs based on their experience and the collected literature. The questionnaire was divided into 5 parts and included 19 questions.
2.4.1. Respondents' characteristics
Information was gathered on respondents' age, gender, training supervisor status, perceived speed of hardware used (5-point Likert scale), perceived knowledge of literature data about VAs (5-point Likert scale), and perceived literacy of registered patients.
No criteria were found in the current literature to easily measure the literacy of registered patients. This data was estimated by 2 questions: subjective opinion of the respondent on the percentage of low-literacy patients and address of the respondent. Responses to the latter question were crossed with data from the French National Institute of Statistics and Economic Studies (INSEE) [47] to determine the level of education in the territory of practice, a factor strongly correlated with literacy [48]. These two indicators were coherent with posterior probability (Pearson's correlation coefficient, Rho = 0.308). GPs who had registered patients with lower literacy were identified with at least one of these indicators.
2.4.2. Exploration of the rate of use of VAs during consultation
Six questions and a free comment explored the rate of use of different types of VAs (hand-drawn sketch, anatomical model, wall poster, printed image, simple digital image, video, interactive digital support, illustrated medication instructions), as well as sources, purposes, communicational objectives, quality, and impediments to their use. The time scale was divided into “never”, “yearly”, “monthly”, “weekly”, and “daily” since this scale had been previously used in a general practice study [49]. The highest rate mentioned in each questionnaire was used to estimate the rate of use of any type of VA.
2.4.3. Exploration of GPs' expectations about VAs during consultation
Three questions and one free comment explored the quality of VAs used, expected objectives of VAs used and perceived usefulness of different types of VAs (5-point Likert scale).
2.5. Analyses
Categorical variables were presented as numbers and percentages, and numeric variables as means (standard deviation) or medians (interquartile range) depending on their distribution.
Univariate comparison analyses studied the relationship between age and gender of the respondent, training supervisor status, perceived speed of hardware, perceived knowledge about VAs, educational level of inhabitants in the territory of practice, and rate of use of different types of VAs. For a more precise odds ratio calculation, univariate analyses were performed by grouping Likert scale questions in 2 classes (the 2 inferior items were compared to the 3 superior items). The usual comparison tests were performed, with the Pearson's chi-squared test (or Fisher's exact test in case of small sample size) for categorical variables.
Univariate analyses with multinomial logistic regressions were conducted for categorical variables with more than 2 categories to identify potential confounders. One was performed between the variable “rate of use of simple digital images” (with 5 classes) and potential confounders (age and gender). Another was performed between the variable “the rate of use of any VAs” (with 5 classes) and potential confounders (age and gender). Reference groups were set as “Never” for the rate of use of simple digital images and “Yearly” for the rate of use of any VAs. Associations were estimated with univariate odds ratios and their 95% confidence interval. Multivariate modelling was then performed, adjusting for all identified confounders (both age and gender).
All tests were two-tailed. Statistical significance for all analyses was set at p < 0.05. All statistical analyses were performed using GMRC Shiny stats and STATA SE15.0 (College Station, TX, USA).
3. Results
3.1. Respondents' characteristics
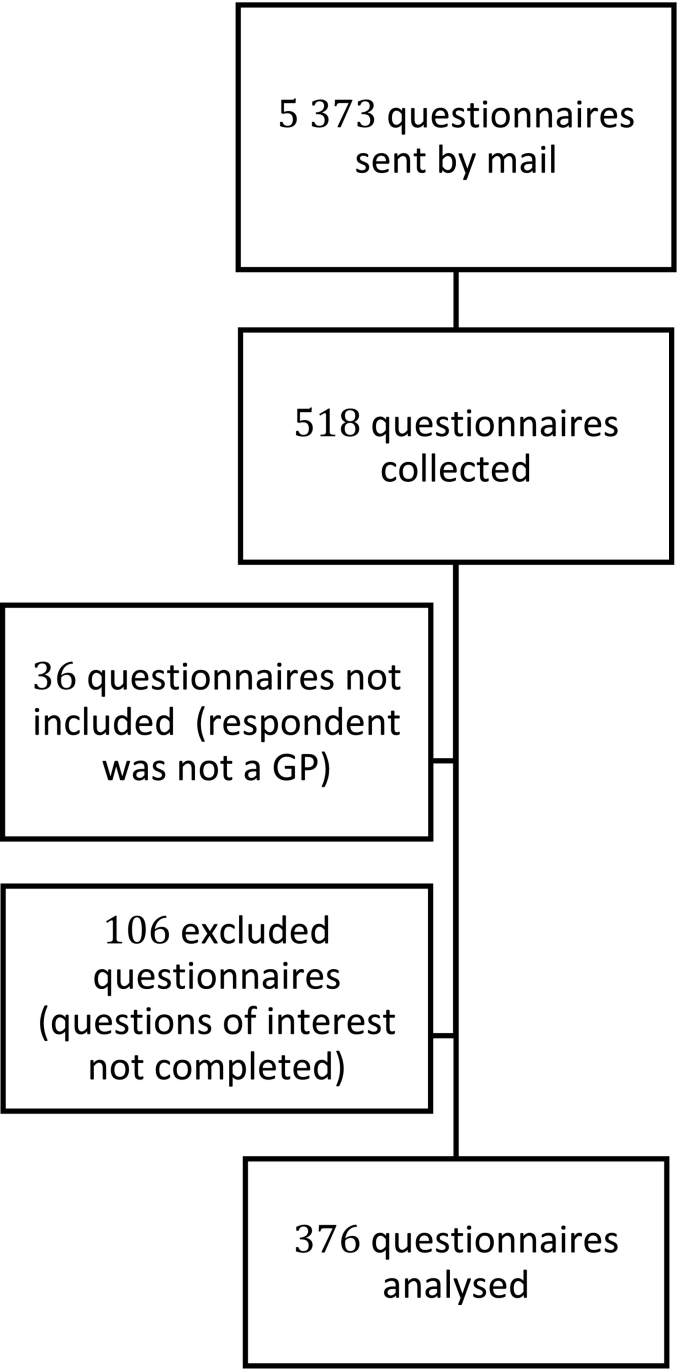
Of the 5373 questionnaires sent, 376 were analysed (Fig. 1). The response rate was 7% in 2 months. The mean rate of completion of the 376 analysed questionnaires was 90%. The average time to complete the survey was 12 min. Respondents were GPs from all metropolitan French regions and overseas. Median age was 40 (33–53). Sex ratio was 0.69. Regarding the literature data on VAs presented to GPs, 64% of the respondents said they were not aware of them at all. All respondent characteristics are reported in Table 1.
Fig. 1.
Flow chart.
Table 1.
Respondents' characteristics (n = 376).
| Age (years), median [interquartile range] | 40 [33–53] |
|---|---|
| Gender, n (%) | |
| Male | 154 (41) |
| Female | 222 (59) |
| Training supervisors, n (%) | 147 (39) |
| Perceived speed of hardware in the practice (computers and Internet connection), n (%) | |
| Very poor | 7 (1.9) |
| Poor | 22 (5.9) |
| Average | 92 (25) |
| Good | 173 (46) |
| Very good | 82 (22) |
| Estimated proportion of registered patients with lower literacy (n = 360), median (%) [interquartile range] | 25 [15–40] |
| Proportion of inhabitants with lower levels of education in the territory of practice1(n = 253), median (%) [interquartile range] | 29 [24–37] |
| Awareness of the presented data from the literature on VAs' usefulness (n = 357), n (%) | |
| Fully unaware | 229 (64) |
| Somewhat unaware | 59 (17) |
| Neither aware nor unaware | 45 (13) |
| Somewhat aware | 21 (5.9) |
| Fully aware | 3 (0.8) |
According to the 2015 data of the French National Institute of Statistics and Economic Studies (INSEE).
3.2. Use of VAs during general practice consultation
The results present all univariate analyses, as well as the multivariate analysis, considering the confounding factors: age and gender were associated with the use of simple digital images and any type of VAs.
3.2.1. Rate of average use of different types of VAs by GPs during consultation
The proportion of at least weekly use of VAs was estimated to be 71% (95% CI = 66–76), with 34% (95% CI = 29–39) of respondents reporting daily use (Table 2). Sketches were the most used VA, used at least weekly by 46% (95% CI = 41–51) of the respondents and daily by 16% (95% CI = 12–19). Printed images and simple digital images were used at least monthly by 52% (95% CI = 47–57) and 51% (95% CI = 46–56) of the respondents respectively. Other types of VA were mostly not used by GPs in the sample: 50% (95% CI = 45–55) never used anatomical models, 57% (95% CI = 52–62) wall posters, 72% (95% CI = 68–77) videos, 78% (95% CI = 73–82) interactive digital supports and 85% (95% CI = 81–89) illustrated medication instructions. The use of real objects, such as an intrauterine device or a packet of birth control pills, was reported in the free comment section.
Table 2.
Use of VAs.
| Never n (%) |
Yearly n (%) |
Monthly n (%) |
Weekly n (%) |
Daily n (%) |
Comparison with age |
Comparison with gender |
Comparison with perceived literacy of registered patients |
Comparison with educational level of registered patients |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p | Reference group | p | Reference group | p | Reference group | p | Reference group | ||||||
| Type of VA used (n = 370) | |||||||||||||
| Sketch | 18 (4.9) | 75 (20) | 107 (29) | 112 (30) | 58 (16) | 0.39* | 0.22* | 0.65** | 0.20* | ||||
| Anatomical model | 184 (50) | 71 (19) | 57 (15) | 43 (12) | 15 (4.1) | <0.01* | Older | 0.18* | 0.56** | 0.18** | |||
| Wall poster | 210 (57) | 71 (19) | 50 (14) | 26 (7) | 13 (3.5) | 0.10* | 0.65* | 0.12* | 0.84** | ||||
| Printed image of a fact sheet, booklet, book… | 90 (24) | 89 (24) | 114 (31) | 62 (17) | 15 (4.1) | 0.87* | 0.04* | Male | 0.02* | Low literacy | |||
| Simple digital image | 103 (28) | 78 (21) | 95 (26) | 67 (18) | 27 (7.3) | 0.001*** | Younger | <0.001*** | Male | 0.31* | 0.02* | High level | |
| Video | 268 (72) | 61 (17) | 28 (7.6) | 10 (2.7) | 3 (0.8) | 0.64** | 0.11** | 0.65* | 0.05** | ||||
| Interactive digital support | 287 (78) | 36 (9.7) | 25 (6.8) | 16 (4.3) | 6 (1.6) | 0.64** | 0.06** | 0.97* | 0.02** | High level | |||
| Illustrated medication instructions | 314 (85) | 32 (8.7) | 7 (1.9) | 12 (3.2) | 5 (1.4) | 0.93** | 0.71** | 0.08* | 0.43** | ||||
| Any VAs 1 | 0 (0) | 22 (5.9) | 86 (23) | 137 (37) | 126 (34) | 0.012*** | Older | 0.363*** | 0.18* | 0.57* | |||
| Main uses of VAs (n = 371) | |||||||||||||
| To describe anatomy | 10 (2.7) | 67 (18) | 123 (33) | 120 (32) | 51 (14) | 0.09** | <0.01* | Male | 0.24** | 0.01** | High level | ||
| To explain pathophysiology of disease | 72 (19) | 105 (28) | 112 (30) | 63 (17) | 19 (5.1) | 0.54* | <0.01* | Male | 0.75* | 0.62* | |||
| To explain drug action | 176 (47) | 105 (28) | 60 (16) | 24 (6.5) | 6 (1.6) | 0.45** | 0.78** | 0.53** | 0.51** | ||||
| To describe proceedings of a treatment or an exam the patient will undertake him- or herself | 129 (35) | 110 (30) | 83 (22) | 36 (9.7) | 13 (3.5) | 0.14* | 0.02* | Male | 0.05* | 0.58** | |||
| To describe proceedings of a treatment or an exam the patient will undergo | 150 (40) | 121 (33) | 66 (18) | 31 (8.4) | 3 (0.8) | 0.04** | Older | 0.02** | Male | 0.3** | 0.58** | ||
| To help shared decision making | 121 (33) | 94 (25) | 94 (25) | 47 (13) | 15 (4) | 0.28* | 0.61* | 0.18* | 0.24** | ||||
| To explore emotions, to provide psychotherapy | 302 (81) | 40 (11) | 17 (4.6) | 8 (2.2) | 4 (1.1) | 0.46** | 0.59** | 0.24** | 0.52** | ||||
| Communicational purposes of using VAs (n = 371) | |||||||||||||
| To facilitate comprehension of information | 4 (1.1) | 41 (11) | 101 (27) | 125 (34) | 100 (27) | 0.03** | Younger | 0.03** | Male | 0.34** | 0.07** | ||
| To improve recall of information | 60 (16) | 80 (22) | 95 (26) | 92 (25) | 43 (12) | 0.41* | 0.15* | 0.1* | 0.08* | ||||
| To get patient's attention | 82 (22) | 77 (21) | 91 (25) | 82 (22) | 39 (11) | 0.41 | <0.01* | Male | 0.16* | 0.17* | |||
| To persuade the patient, to improve compliance | 62 (17) | 76 (21) | 92 (25) | 93 (25) | 48 (13) | 0.07* | 0.01* | Male | 0.05* | 0.05* | |||
| To explain quicker | 98 (26) | 67 (18) | 86 (23) | 70 (19) | 50 (14) | 0.02* | Older | 0.01* | Male | 0.56* | 0.72* | ||
| To structure consultation to not forget important elements | 199 (54) | 73 (20) | 50 (14) | 32 (8.6) | 17 (4.6) | 0.03* | Older | 0.43* | 0.18* | 0.69** | |||
Estimated data, *chi-square test, ** Fisher's exact test, *** multivariable multinomial logistic regression with Wald test.
Younger age was independently associated with a higher rate of use of any VAs (p = 0.012), and especially with simple digital images (p = 0.001). Gender did not influence the rate of use of VAs in multivariate analysis. Training supervisors' status or perceived speed of hardware did not influence the use of VAs. Respondents with low-literacy patients used sketches more often (p = 0.007) and less simple digital images (p = 0.04).
3.2.2. Main sources of VAs used
Half of GPs mainly used VAs from unknown sources (for instance images found on Google Images). Some GPs also reported that they created their own VAs if needed, without specifying in the questionnaire what type of VAs they created (they may have taken the pictures or made the videos they needed or drawn sketches, etc.). Nearly half of the GPs reported using VAs they created themselves, at 42% (95% CI = 37–47). The main sources of VAs respondents mentioned were a public institution at 35% (95% CI = 30–40), a scientific society at 31% (95% CI = 27–36) or a pharmaceutical industry at 10% (95% CI = 7.3–13).
3.2.3. Main uses of VAs
VAs were mainly used to describe anatomy (79%, 95% CI = 75–83, at least monthly use) or to explain the pathophysiology of disease (52%, 95% CI = 47–57, at least monthly use) (Table 2).
GPs made little use of VAs in several of the listed situations. VAs were used less than once a month to help shared decision making by 58% (95% CI = 53–63) of GPs, to explain a treatment or examination procedure carried out by patients themselves by 64% (95% CI = 59–69), to explain treatment or examination procedures that the patient was going to undergo by 73% (95% CI = 69–78), to explain drug action by 76% (95% CI = 72–80), and to explore emotions and provide psychotherapy by 92% (95% CI = 89–95).
3.2.4. Communicational purpose of using VAs
On the one hand, the main reason GPs used VAs during consultation was to facilitate comprehension of information: 61% (95% CI = 56–66) of the respondents reported using them at least weekly for this purpose (Table 2). On the other hand, structuring consultations to not forget important elements was the rarest objective with 74% (95% CI = 69–79) of respondents reporting using VAs less than monthly for this purpose. Objectives such as improving recall of information, getting the patient's attention, persuading the patient or improving compliance, and explaining quicker were heterogeneously cited; about 60% (95% CI = 55–65) of the GPs had these objectives monthly.
3.2.5. Respondents felt they used VAs enough
Of the respondents, 88 (23%, 95% CI = 19–28) felt they used VAs enough, as opposed to 288 (77%, 95% CI = 72–81) who felt they didn't use VAs enough.
GPs with low-literacy patients were more likely to report feeling that they didn't use VAs enough (p = 0.01).
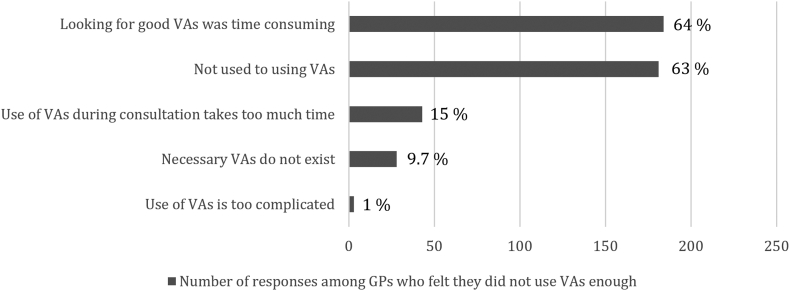
3.2.6. Reasons not to use VAs more often among GPs who felt they did not use them enough
Most of the respondents who felt they didn't use VAs enough mentioned 2 reasons. Looking for good VAs was time-consuming for 64% (95% CI = 58–69), and 63% (95% CI = 57–68) said they were not familiar with using them more often (Fig. 2). Other listed reasons were heterogeneous: the use during consultation was taking too much time for 15% (95% CI = 11–19) of the GPs, necessary VAs did not exist for 10% (95% CI = 6.3–13) and their use was too complicated for 1% (95% CI = 0.0–2,2).
Fig. 2.
Reasons not to use visual aids more often.
In the free comment section, being unable to draw was mentioned 5 times. Two respondents evoked the high cost of anatomical models. Inappropriate organisation of the desk to use VAs was also mentioned.
GPs with low-literacy patients or using VAs daily more often believed necessary VAs did not exist (p = 0.03 and p = 0.01 respectively).
3.2.7. Perceived quality of VAs used
VAs used were considered in accordance with the latest evidence-based practice by 55% (95% CI = 50–60) of the respondents and easily understandable by patients by 53%, (95% CI = 48–58) (Table 3). On the contrary, 60% (95% CI = 55–65) respondents felt that VAs did not have a global approach, 64% (95% CI = 59–68) thought they could not deal with any subject, and 87% (95% CI = 84–91) did not find them humoristic. GPs' opinion on VAs was divided into an easy use by physicians and an adaptative capacity.
Table 3.
Perceived quality of used VAs, pooled data (n = 374).
| Visual aids: | Strongly disagree n (%) |
Disagree n (%) |
Undecided n (%) |
Agree n (%) |
Strongly agree n (%) |
Comparison with age |
Comparison with gender |
Comparison with perceived literacy of registered patients |
Comparison with educational level of registered patients |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p | p | Reference group | p | Reference group | p | Reference group | ||||||
| Are in accordance with latest evidence-based practice | 12 (3,2) | 35 (9) | 122 (33) | 132 (35) | 73 (19.6) | 0.59* | 0.27** | 0.37* | 0.01* | High level | ||
| Exist for any subject | 109 (29) | 128 (34) | 84 (23) | 36 (9,6) | 17 (4.5) | 0.31* | 0.01* | Male | 0.12* | 0.01* | High level | |
| Have a global approach to a subject (anatomy + pathophysiology + treatment…) | 89 (24) | 134 (36) | 94 (25) | 37 (10%) | 18 (4.8) | 0.88* | 0.01* | Male | 0.06* | <0.01** | High level | |
| Are easily understandable by patient | 6 (1.6) | 41 (11) | 129 (35) | 134 (36) | 63 (17) | 0.78** | 0.06** | 0.01** | High literacy | <0.01** | High level | |
| Are patient-centred = possibility to give precise and restricted information to a specific patient | 45 (12) | 61 (16) | 113 (31) | 102 (28) | 50 (14) | 0.65* | 0.02* | Male | 0.14* | 0.53* | ||
| Are humorous | 215 (58) | 111 (30) | 31 (8.3) | 12 (3.2) | 3 (0.8) | 0.36** | 0.05** | 0.85** | 0.59** | |||
| Are easy and intuitive for GPs to use | 39 (11) | 56 (15) | 132 (36) | 98 (26) | 47 (13) | 0.45* | 0.34* | 0.01* | High literacy | 0.31* | ||
* chi-square test, ** Fisher's exact test.
GPs with low-literacy patients found the VAs used to be less understandable by patients (p = 0.02), to not have a global approach (p < 0.001), and of poorer scientific quality (p = 0.002).
3.3. GPs' expectations for the use of VAs during consultation
3.3.1. Ideal quality of VAs
In GPs' opinion, VAs should above all be easily understandable by patients (Fig. 3). Then, they should be useful for physicians, patient-centred and in accordance with latest evidence-based practice. Being the least time-consuming during consultation and having an exhaustive approach seemed to be secondary qualities. Humour did not seem to be an expected feature.
Fig. 3.
Rank of importance for VAs' quality.
Rank number one corresponds to the most important rank for the respondent.
3.3.2. Purposes requiring good quality VAs
Good quality VAs were requested by 91% (95% CI = 88–94) of GPs (Fig. 4). The purposes of using VAs included to describe anatomy, mentioned by 75% (95% CI = 70–79) of respondents; to explain pathophysiology of disease, mentioned by 64% (95% CI = 59–69); to help shared decision making, mentioned by 64% (95% CI = 59–69); to describe treatment or an examination procedure that the patient was going to undergo, mentioned by 57% (95% CI = 53–62); to explain drug action, mentioned by 49%, (95% CI = 44–54); and to explore emotions or to provide psychotherapy, mentioned by 19% (95% CI = 15–24).
Fig. 4.
Purposes requiring good quality VAs.
3.3.3. Perceived usefulness of VAs
Use of any type of VA was considered useful or very useful by 94% (95% CI = 91–96) of surveyed GPs (Table 4). Sketches were the most useful according to the respondents, with 75% (95% CI = 70–79) finding them useful or very useful. Other VAs were considered useful or very useful by the majority of respondents: anatomical models by 64% (95% CI = 58–69), simple digital images by 62% (95% CI = 57–67), and printed images by 57% (95% CI = 52–62). The remaining VAs were by respondents to varying degrees.
Table 4.
Perceived usefulness of VAs used, pooled data (n = 334).
| Useless n (%) |
Poorly useful n (%) |
Slightly useful n (%) |
Useful n (%) |
Very useful n (%) |
Comparison with age |
Comparison with gender |
Comparison with perceived literacy of registered patients |
Comparison with educational level of registered patients |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p | Reference group | p | Reference group | p | Reference group | p | Reference group | ||||||
| Sketch | 4 (1.2) | 12 (3.6) | 67 (20) | 94 (28) | 157 (47) | 0.09** | 0.36** | 0.65** | 0.02** | Low level | |||
| Anatomical model | 11 (3.3) | 28 (8.4) | 82 (25) | 102 (31) | 111 (33) | 0.04* | Younger | <0.01** | Female | 0.56* | 0.74** | ||
| Wall poster | 48 (14) | 84 (25) | 103 (31) | 70 (21) | 29 (8.7) | 0.37* | 0.04* | Female | 0.12* | 0.48* | |||
| Printed image of a fact sheet, booklet, book… | 11 (3.3) | 44 (13) | 89 (27) | 121 (36) | 69 (21) | 0.16* | 0.03** | Female | 0.02* | Low literacy | 0.86** | ||
| Simple digital image | 20 (6) | 21 (6,3) | 88 (26) | 133 (40) | 72 (22) | <0.01* | Younger | 0.03* | Female | 0.31* | 0.42* | ||
| Video | 59 (18) | 71 (21) | 96 (29) | 55 (17) | 53 (16) | 0.08* | 0.28* | 0.65* | 0.93* | ||||
| Interactive digital support | 50 (15) | 73 (22) | 99 (30) | 65 (20) | 46 (14) | 0.03* | Younger | 0.33* | 0.97* | 0.80* | |||
| Illustrated medication instructions | 83 (25) | 81 (24) | 89 (27) | 55 (17) | 26 (7.8) | <0.01* | Younger | <0.01* | Female | 0.08* | 0.35* | ||
| Any VAs 1 | 0 (0) | 2 (0.6) | 19 (5.7) | 87 (26) | 226 (68) | 0.02** | Younger | 0.01** | Female | 0.04** | Low literacy | 0.19** | |
Estimated data, * chi-square test, ** Fisher's exact test.
Free comments (146 comments) reported that VAs were useful whatever the patient's level of literacy. Positive features of VAs were nuanced by some respondents. Some GPs mentioned that not all types of patients were interested in explanations with images and that the use of images was not adequate for all situations. They further mentioned that it was necessary to find a good balance between oral and visual explanations because too many visuals could distract from the primary goal. Several comments also described a realisation of the utility of VAs thanks to our questionnaire. Seventeen GPs requested a unique and reliable database gathering useful VAs, and ten among them explicitly requested a numeric format.
GPs with low-literacy patients considered printed VAs and illustrated medication instructions to be more useful (p = 0.004 and p = 0.009 respectively). Younger GPs were more likely than older GPs to find simple digital images and illustrated medication instructions useful (p = 0.01 and p < 0.001 respectively).
4. Discussion and conclusion
4.1. Discussion
This descriptive survey introduces new data on VAs used in general practice consultations, the objectives behind their use and GPs' opinions on their quality, usefulness, and potential improvements.
4.1.1. Use of VAs
Most of the surveyed GPs used VAs on a regular basis without being aware of the literature data on their effectiveness. Sketches were the most commonly used VA, followed by simple digital images and printed images. VAs were mainly used to describe anatomy and accessorily to explain pathophysiology of disease. They were underused for other purposes. From a communication perspective, VAs were essentially used to facilitate comprehension of information. Deliberate use of VAs to improve recall of information by patients, to improve adherence or to capture attention was less frequent, even though their utility in these areas is often described in the literature [12–17.20]. Our questionnaire also validates the hypothesis that VAs could sometimes help structure consultations.
This study helps fill the gap in the literature that was described in the introduction section [45,46] regarding the use of VAs by GPs. In addition, the effectiveness of VAs has been repeatedly demonstrated in the literature [[12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32]] but some studies have shown mixed results [[34], [35], [36], [37], [38], [39], [40], [41]]. In this context, the GPs of our survey strengthened the idea that VAs are very useful in many primary care situations [[34], [35], [36], [37], [38], [39], [40], [41]]. Further studies are needed to determine in which situations VAs are the most useful and to identify quality criteria for the most useful VAs.
4.1.2. Impediments to the use of VAs
Our study identifies 3 main impediments to the use of VAs.
Looking for good VAs was thought to be time-consuming. On the contrary, the time it took to use VAs during consultation was not considered a limitation for a majority of GPs. This result was also found in a study previously cited above [45]: median duration (interquartile range) of a consultation without VAs was 9 min (6–12 min), versus 10 min (8.6–12 min) if VAs were used, with no statistical significance (p = 0.70).
Perceived quality of VAs can be improved according to the surveyed GPs. A similar result was found in a study about the heterogeneous quality of pictograms on drugs packaging [22]. In 2017, among 26 illustrated fact sheets for patients with kidney failure [50], 20% were considered inappropriate, 60% had no link with the text, and 12% were in contradiction with the text. Guidelines for illustrations for patients [[51], [52], [53]] are poorly followed, as highlighted in a 2015 analysis of 147 printed images about cancer in the United States [54]. This calls into question the feasibility of making good VAs in terms of time and cost, but also their diffusion and their implementation. Other reasons for poor quality of VAs are cited by Rohret et al. [55]: many medical illustrations for patients are based on the subjective opinion of their creator, ease of creation, the cost of production and the potential market targeted. Besides, medical illustrators are used to working for medical students, and they seem to use the same techniques and codes for patient illustrations.
There was also a lack of habit of using existing VAs. A potential explanation is the lack of knowledge of the utility of VAs found in our sample. Several comments highlighted a realisation of the utility of VAs thanks to this questionnaire: we hypothesise that spreading data about their utility could increase the use of VAs.
4.1.3. Expectations of GPs
Almost all GPs found VAs useful or very useful, and a large majority of them felt they didn't use VAs enough, especially in case of potentially low-literacy patients. This favourable opinion of VAs strengthens the idea of their general utility found in the literature [[12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33]], which is sometimes debated [[34], [35], [36], [37], [38], [39], [40], [41]]. Our study also introduces data that help us understand the discrepancies in the literature. Poor quality VAs can lead to bad results, as shown in a study that found the use of unclear VAs to be frustrating for patients [56]. As expressed in the free comments, VAs are not suitable for all types of situations. This was pointed out in a study in which patients were shown an illustration with a needle to explain a breast cancer biopsy which was perceived as shocking by some patients and distracted them from the original purpose [23].
Described qualities of VAs used in our study contrasted with the GPs' expectations for VAs, such as being easily understandable by patients, being easy and intuitive for physicians to use, being in accordance with the latest evidence-based practice and being adaptable to each patient in a patient-centred approach. A study conducted in Colorado in 2015 [57] showed the importance of adapting pictures to patients as they increased the attractiveness of the information delivered, patients' attention and comprehension, and persuasion.
Sketches were considered the most useful VA. This is probably because they respond better to the limitations and expectations expressed by GPs. They don't require doctors to waste time searching, they can reach the required scientific level, and they can be adapted to each patient. However, several GPs claimed to be unable to draw and mentioned the heterogeneous quality of sketches. Comments did not reveal an interest in a training program to improve sketching skills. Moreover, younger GPs, who used VAs more often, were more likely to use digital VAs. It seems that digital tools could increase the use of VAs during consultation. The sampled GPs strongly requested a digital database of good VAs; this could be a solution to the limitations and needs expressed by GPs.
4.1.4. Strengths and limitations
This is an original study providing epidemiological data on the use of VAs by GPs, which were lacking in the literature.
Although the sample of surveyed French GPs was not intended to be representative of the French population, our results are worthy of consideration given the large sample of 376 GPs distributed across metropolitan and overseas French territory. Their age distribution by gender is similar to the demographic data on French GPs. Compared with the population of French GPs in 2019 [58,59], with a mean age of 50 and a percentage of training supervisors of 20%, our population included younger GPs and more training supervisors.
The strength of the questionnaire lies in the exploitation of a large literature and the academic experience of the questionnaire writers. However, it was only conducted based on the consensus of three people and was not pretested under real conditions, which could explain some of its imperfections. For the question on the use of different types of VAs, the item “any VAs” was not recorded and its relative importance was only noted afterwards. To compensate, an a posteriori estimate was made, which may have underestimated the use and perceived usefulness of “any VAs”, even though the estimated data were consistent with the complete responses of each respondent. Some of the wording of the questionnaire was not explicit enough, which led to misunderstandings that were highlighted in the free comments. This was the case for the formulations “illustrated medication instructions “ and “interactive digital support.” While the former was not understood because it was not well-known, the latter would probably have benefited from an explanation. This may have led to an underestimation of this data.
This epidemiological study is subject to the classic reporting bias and recruitment bias.
4.2. Innovation
Images appear to be an effective means of communication, and this study describes in detail the use of VAs in general practice consultations. While most existing studies investigate the use of VAs in booklets, videos or drug leaflets used by the patient alone, here the focus is on the use of VAs to improve GP-patient communication in daily practice.
The use of questionnaires and univariate and multivariate analyses was necessary to gather the first objective and quantified data on this topic. Our objective estimation of the health literacy level of each GP's registered patients was particularly innovative. It was based on the addresses of the respondents' practices and the INSEE educational data corresponding to these areas.
4.3. Conclusion
VAs are used in general practice consultations on a regular basis. However, GPs feel they are not used enough and that several purposes of use are insufficiently exploited. This can be explained by a lack of habit and a possible lack of awareness of the usefulness of VAs, as well as by the fact that it can take a long time to find good quality VAs during a consultation. However, the usefulness of VAs for most patients, and particularly those with low heath-literacy levels, is well documented and was clearly perceived by the surveyed GPs. Finally, there is a real unmet need in general practice for VAs that are quickly accessible, easily understood by patients, scientifically correct and adapted to each patient. Informing GPs of the usefulness of VAs in consultation, training them to draw adapted sketches and creating a database of good quality VAs are some possible strategies to increase the use of VAs in general practice consultation.
Funding
None. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics
All procedures followed were in accordance with the Directive (EU) 2016/679 of the General Data Protection Regulation (GDPR). Ethical approval was granted for this study by the Ethics Committee & Institutional Review Board of Mondor Hospital (IRB 00011558), Paris Est Creteil University.
Declaration of Competing Interest
None. The authors have no conflicts of interest to disclose.
Acknowledgements
The authors acknowledge Emmanuelle Boutin, biostatistician at the Université Paris-Est Créteil, Institut National de la Santé et de la Recherche Médicale (INSERM) U955, Institut Mondor de Recherche Biomédicale (IMRB), Equipe CEpiA (Epidémiologie Clinique et Vieillissement) for her assistance in this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pecinn.2023.100159.
Appendix A. Supplementary data
Supplementary material: the distributed questionnaire
References
- 1.Da Silva D. A review of evidence considering whether shared decision making is worthwhile. The Health Foundation; 2012. Evidence: Helping people share decision making; p. 78. [Google Scholar]
- 2.Vallot S., Yana J., Moscova L., Fabre J., Brossier S., Aubin I., et al. La décision médicale partagée: quelle efficacité sur les résultats de santé ? [Shared decision-making in medicine: how effective is it on health outcomes?] Exercer. 2019:25–39. [Google Scholar]
- 3.Stewart M.A. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 4.Gay B., Demeaux J.-L., Afonso M. Évaluation de l’éducation thérapeutique individuelle et collective chez les patients à risque cardiovasculaire: l’étude ETHICCAR [Evaluation of individual and group therapeutic education in patients at cardiovascular risk: ETHICCAR Study, Bulletin of the National Academy of Medicine] Bull Acad Natl Med. 2020;204:79–86. doi: 10.1016/j.banm.2019.04.016. [DOI] [Google Scholar]
- 5.Simpson M., Buckman R., Stewart M., Maguire P., Lipkin M., Novack D., et al. Doctor-patient communication: the Toronto consensus statement. BMJ. 1991;303:1385–1387. doi: 10.1136/bmj.303.6814.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coulter A., Entwistle V., Gilbert D. Sharing decisions with patients: is the information good enough? BMJ. 1999;318:318–322. doi: 10.1136/bmj.318.7179.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chauvin F. Dessiner la santé publique de demain [Designing tomorrow's public health], Haut Conseil de Santé Publique [French High Council for Public Health] 2021. https://solidarites-sante.gouv.fr/ministere/documentation-et-publications-officielles/rapports/sante/article/dessiner-la-sante-publique-de-demain
- 8.Ministère de l'’éducation nationale (France) [Ministry of Education (France)] Développer sa mémoire, techniques de mémorisation - Séquence 1 [Develop memory, memorization techniques - Sequence 1] 2012. http://lettres-anglais.ac-amiens.fr/IMG/pdf/12-LyceeGT_Ressource_AP_Developper-memoire-technique-memorisation_sequence1.pdf
- 9.Joshi H.B., Newns N., Stainthorpe A., MacDonagh R.P., Keeley F.X., Timoney A.G. The development and validation of a patient-information booklet on ureteric stents. BJU Int. 2001;88:329–334. doi: 10.1046/j.1464-410x.2001.02356.x. [DOI] [PubMed] [Google Scholar]
- 10.Osborne H. Health literacy: how visuals can help tell the healthcare story. J Vis Commun Med. 2006;29:28–32. doi: 10.1080/01405110600772830. [DOI] [PubMed] [Google Scholar]
- 11.van Beusekom M.M., Grootens-Wiegers P., Bos M.J.W., Guchelaar H.-J., van den Broek J.M. Low literacy and written drug information: information-seeking, leaflet evaluation and preferences, and roles for images. Int J Clin Pharmacol. 2016;38:1372–1379. doi: 10.1007/s11096-016-0376-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Houts P.S., Doak C.C., Doak L.G., Loscalzo M.J. The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61:173–190. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Katz M.G., Kripalani S., Weiss B.D. Use of pictorial aids in medication instructions: A review of the literature. Am J Health Syst Pharm. 2006;63:2391–2397. doi: 10.2146/ajhp060162. [DOI] [PubMed] [Google Scholar]
- 14.Dahodwala M., Geransar R., Babion J., de Grood J., Sargious P. The impact of the use of video-based educational interventions on patient outcomes in hospital settings: A scoping review. Patient Educ Couns. 2018;101:2116–2124. doi: 10.1016/j.pec.2018.06.018. [DOI] [PubMed] [Google Scholar]
- 15.Winston K., Grendarova P., Rabi D. Video-based patient decision aids: a scoping review. Patient Educ Couns. 2018;101:558–578. doi: 10.1016/j.pec.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Farrell E.H., Whistance R.N., Phillips K., Morgan B., Savage K., Lewis V., et al. Systematic review and meta-analysis of audio-visual information aids for informed consent for invasive healthcare procedures in clinical practice. Patient Educ Couns. 2014;94:20–32. doi: 10.1016/j.pec.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 17.Mbanda N., Dada S., Bastable K., Ingalill G.-B., Ralf S. A scoping review of the use of visual aids in health education materials for persons with low-literacy levels. Patient Educ Couns. 2021;104:998–1017. doi: 10.1016/j.pec.2020.11.034. [DOI] [PubMed] [Google Scholar]
- 18.Wohrm A. Educational illustrations as an aid in patient-doctor communication, exemplified by patients with dyspepsia. Scand J Prim Health Care. 1994;12:84–87. doi: 10.3109/02813439409003680. [DOI] [PubMed] [Google Scholar]
- 19.Näslund U., Ng N., Lundgren A., Fhärm E., Grönlund C., Johansson H., et al. VIPVIZA trial group, Visualization of asymptomatic atherosclerotic disease for optimum cardiovascular prevention (VIPVIZA): a pragmatic, open-label, randomised controlled trial. Lancet. 2019;393:133–142. doi: 10.1016/S0140-6736(18)32818-6. [DOI] [PubMed] [Google Scholar]
- 20.Synnot A., Ryan R., Prictor M., Fetherstonhaugh D., Parker B. Audio-visual presentation of information for informed consent for participation in clinical trials. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD003717.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choi J. Effect of pictograph-based discharge instructions on older adults’ comprehension and recall: a pilot study. Res Gerontol Nurs. 2016;9:66–71. doi: 10.3928/19404921-20150513-05. [DOI] [PubMed] [Google Scholar]
- 22.Choi J. Older adults’ perceptions of pictograph-based discharge instructions after hip replacement surgery. J Gerontol Nurs. 2013;39:48–54. doi: 10.3928/00989134-20130415-02. [DOI] [PubMed] [Google Scholar]
- 23.Choi J. Development and pilot test of pictograph-enhanced breast health-care instructions for community-residing immigrant women. Int J Nurs Pract. 2012;18:373–378. doi: 10.1111/j.1440-172X.2012.02051.x. [DOI] [PubMed] [Google Scholar]
- 24.Garcia-Retamero R., Galesic M. Who profits from visual aids: overcoming challenges in people’s understanding of risks [corrected] Soc Sci Med. 2010;70:1019–1025. doi: 10.1016/j.socscimed.2009.11.031. [DOI] [PubMed] [Google Scholar]
- 25.Mansoor L.E., Dowse R. Effect of pictograms on readability of patient information materials. Ann Pharmacother. 2003;37:1003–1009. doi: 10.1345/aph.1C449. [DOI] [PubMed] [Google Scholar]
- 26.Mohan A., Riley B., Schmotzer B., Boyington D.R., Kripalani S. Improving medication understanding among Latinos through illustrated medication lists. Am J Manag Care. 2014;20:e547–e555. [PubMed] [Google Scholar]
- 27.Cleeren G., Quirynen M., Ozcelik O., Teughels W. Role of 3D animation in periodontal patient education: a randomized controlled trial. J Clin Periodontol. 2014;41:38–45. doi: 10.1111/jcpe.12170. [DOI] [PubMed] [Google Scholar]
- 28.Cook T.S., Oh S.C., Kahn C.E. Patients’ use and evaluation of an online system to annotate radiology reports with lay language definitions. Acad Radiol. 2017;24:1169–1174. doi: 10.1016/j.acra.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 29.Evans J.H., Collier J., Crook I., Garrud P., Harris P., MacKinlay D.R., et al. Using multimedia for patient information - a program about nocturnal enuresis. Br J Urol. 1998;81(Suppl. 3):120–122. doi: 10.1046/j.1464-410x.1998.00023.x. [DOI] [PubMed] [Google Scholar]
- 30.Kandula N.R., Nsiah-Kumi P.A., Makoul G., Sager J., Zei C.P., Glass S., et al. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient Educ Couns. 2009;75:321–327. doi: 10.1016/j.pec.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 31.Bol N., Smets E.M.A., Eddes E.H., de Haes J.C.J.M., Loos E.F., van Weert J.C.M. Illustrations enhance older colorectal cancer patients’ website satisfaction and recall of online cancer information. Eur J Cancer Care (Engl) 2015;24:213–223. doi: 10.1111/ecc.12283. [DOI] [PubMed] [Google Scholar]
- 32.Bol N., van Weert J.C.M., de Haes H.C.J.M., Loos E.F., de Heer S., Sikkel D., et al. Using cognitive and affective illustrations to enhance older adults’ website satisfaction and recall of online cancer-related information. Health Commun. 2014;29:678–688. doi: 10.1080/10410236.2013.771560. [DOI] [PubMed] [Google Scholar]
- 33.Meppelink C.S., van Weert J.C., Haven C.J., Smit E.G. The effectiveness of health animations in audiences with different health literacy levels: an experimental study. J Med Internet Res. 2015;17 doi: 10.2196/jmir.3979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dowse R., Ramela T., Barford K.-L., Browne S. Developing visual images for communicating information aboutantiretroviral side effects to a low-literate population. Afr J AIDS Res. 2010;9:213–224. doi: 10.2989/16085906.2010.530172. [DOI] [PubMed] [Google Scholar]
- 35.Henry E., Brown T., Bartlett C., Massoud E., Bance M. Informed consent in otologic surgery: prospective randomized study comparing risk recall with an illustrated handout and a nonillustrated handout. J Otolaryngol Head Neck Surg. 2008;37:273–278. [PubMed] [Google Scholar]
- 36.Liu C., Kemper S., McDowd J. The use of illustration to improve older adults’ comprehension of health-related information: is it helpful? Patient Educ Couns. 2009;76:283–288. doi: 10.1016/j.pec.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 37.Hwang S.W., Tram C.Q., Knarr N. The effect of illustrations on patient comprehension of medication instruction labels. BMC Fam Pract. 2005;6:26. doi: 10.1186/1471-2296-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zikmund-Fisher B.J., Witteman H.O., Fuhrel-Forbis A., Exe N.L., Kahn V.C., Dickson M. Animated graphics for comparing two risks: a cautionary tale. J Med Internet Res. 2012;14 doi: 10.2196/jmir.2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kripalani S., Schmotzer B., Jacobson T.A. Improving medication adherence through graphically enhanced interventions in coronary heart disease (IMAGE-CHD): a randomized controlled trial. J Gen Intern Med. 2012;27:1609–1617. doi: 10.1007/s11606-012-2136-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hämeen-Anttila K., Kemppainen K., Enlund H., Bush Patricia J., Marja A. Do pictograms improve children’s understanding of medicine leaflet information? Patient Educ Couns. 2004;55:371–378. doi: 10.1016/j.pec.2003.04.006. [DOI] [PubMed] [Google Scholar]
- 41.Monroe A.K., Pena J.S., Moore R.D., Riekert K.A., Eakin M.N., Kripalani S., et al. Randomized controlled trial of a pictorial aid intervention for medication adherence among HIV-positive patients with comorbid diabetes or hypertension. AIDS Care. 2018;30:199–206. doi: 10.1080/09540121.2017.1360993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scalia P., Durand M.-A., Berkowitz J.L., Ramesh N.P., Faber M.J., Kremer J.A.M., et al. The impact and utility of encounter patient decision aids: systematic review, meta-analysis and narrative synthesis. Patient Educ Couns. 2019;102:817–841. doi: 10.1016/j.pec.2018.12.020. [DOI] [PubMed] [Google Scholar]
- 43.Stacey D., Légaré F., Lewis K., Barry M.J., Bennett C.L., Eden K.B., et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017 doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Compagnon L., Bail P., Huez J.-F., Stalnikiewicz B., Ghasarossian C., Zerbib Y., et al. Définitions et descriptions des compétences en médecine générale [Definitions and descriptions of skills in general practice] Exercer. 2013:148–155. [Google Scholar]
- 45.Neuner-Jehle S., Senn O., Wegwarth O., Rosemann T., Steurer J. How do family physicians communicate about cardiovascular risk? Frequencies and determinants of different communication formats. BMC Fam Pract. 2011;12:15. doi: 10.1186/1471-2296-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Qi L., Baruch D. Université Paris Diderot - Paris 7; 2018. DOCDECLIC: images médicales pour la communication avec le patient: création et évaluation du site [DOCDECLIC: medical images for communication with the patient: creation and evaluation of the website] [Google Scholar]
- 47.Institut national de la statistique et des études économiques [National Institute of Statistics and Economic Studies] 2018. Diplômes - Formation en 2015- Recensement de la population - Base infracommunale (IRIS) [Diplomas - Training in 2015 - Population census - Infra-municipal database (IRIS)] [Google Scholar]
- 48.Organisation for Economic Co-operation and Development . Organisation for Economic Co-operation and Development; Paris: 2016. Skills matter: further results from the survey of adult skills.https://www.oecd-ilibrary.org/education/skills-matter_9789264258051-en [Google Scholar]
- 49.Lundborg C.S., Hensjö L.-O., Gustafsson L.L. Drug information sources: reported preferences by general practitioners. Ther Innov Regul Sci. 1998;32:777–785. doi: 10.1177/009286159803200318. [DOI] [Google Scholar]
- 50.Morony S., McCaffery K.J., Kirkendall S., Jansen J., Webster A.C. Health literacy demand of printed lifestyle patient information materials aimed at people with chronic kidney disease: are materials easy to understand and act on and do they use meaningful visual aids? J Health Commun. 2017;22:163–170. doi: 10.1080/10810730.2016.1258744. [DOI] [PubMed] [Google Scholar]
- 51.Haute Autorité de santé [French National Authority for Health] Haute Autorité de santé [French National Authority for Health]; Paris: 2008. Élaboration d’un document écrit d’information à l’intention des patients et des usagers du système de santé [Development of a written information document for patients and users of the health system]https://www.has-sante.fr/upload/docs/application/pdf/2009-10/elaboration_document_dinformation_des_patients_-_guide_methodologique.pdf [Google Scholar]
- 52.Hôpital général juif [Jewish General Hospital] Hôpital général juif [Jewish General Hospital]; Montréal: 2008. Comment concevoir des documents d’enseignements écrits efficaces pour les patients [How to design effective written teaching materials for patients]https://cdn.ciussscentreouest.ca/documents/hgj/HSL/PEN/Website_Specific/HandbookFrJan20.pdf?1554835665 [Google Scholar]
- 53.Oliver C., Asselstine J., Peterson E., Stephenson L. MUHC standards for developing effective written patient learning materials. 2008. https://www.muhclibraries.ca/Documents/muhc_patient_education_standards.pdf
- 54.King A.J. A content analysis of visual cancer information: prevalence and use of photographs and illustrations in printed health materials. Health Commun. 2015;30:722–731. doi: 10.1080/10410236.2013.878778. [DOI] [PubMed] [Google Scholar]
- 55.Rohret L., Ferguson K.J. Effective use of patient education illustrations. Patient Educ Couns. 1990;15:73–75. doi: 10.1016/0738-3991(90)90010-I. [DOI] [PubMed] [Google Scholar]
- 56.Dobos A.R., Orthia L.A., Lamberts R. Does a picture tell a thousand words? The uses of digitally produced, multimodal pictures for communicating information about Alzheimer’s disease. Public Underst Sci. 2015;24:712–730. doi: 10.1177/0963662514533623. [DOI] [PubMed] [Google Scholar]
- 57.Buller M.K., Bettinghaus E., Buller D.B., Liu X., Fluharty L. Perceived availability of culturally and demographically diverse photographs for health education materials, Colorado, 2010. Prev Chronic Dis. 2015;12:E24. doi: 10.5888/pcd12.140450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bouet P., Gerard-Varet J.-F. Conseil National de l’Ordre Des Médecins [French General Medical Council]; Paris: 2019. Atlas de la démographie médicale en France : situation au 1er Janvier 2019 [Atlas of medical demography in France: situation on January 1, 2019]https://www.conseil-national.medecin.fr/sites/default/files/external-package/analyse_etude/npcskp/demo_2019_atlas.pdf [Google Scholar]
- 59.Collège National des Généralistes Enseignants [National College of Academic GPs] Collège National Des Généralistes Enseignants [National College of Academic GPs]; 2019. Les Maîtres de Stages Universitaires [Training supervisors]https://www.cnge.fr/les_enseignants/les_maitres_de_stages_universitaires/ [accessed June 3, 2019] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material: the distributed questionnaire