Abstract
Functional disorders represent a prevalent health issue, significantly impacting both individuals and healthcare systems. This multidisciplinary dataset aims to enhance our comprehension of the complex interplay among various factors that contribute to functional somatic syndromes. The dataset comprises data from seemingly healthy adults (aged 18-65) in Isfahan, Iran, who were randomly selected and monitored for four consecutive years. The research data encompasses seven distinct datasets: (a) functional symptom evaluations across multiple body organs, (b) psychological assessments, (c) lifestyle factors, (d) demographic and socioeconomic variables, (e) laboratory measurements, (f) clinical examinations, and (g) historical information. A total of 1930 participants were enrolled at the study's outset in 2017. The first, second, and third annual follow-up rounds were completed with 1697 (2018), 1616 (2019), and 1176 (2020) participants, respectively. This dataset is made available for further analysis by a diverse range of researchers, healthcare policymakers, and clinicians.
Keywords: Cohort profile, Functional somatic syndromes, Phenomics
Specifications Table
| Subject | Health and medical sciences |
| Specific subject area | Gastroenterology |
| Type of data | Primary data, Dataset |
| How the data were acquired | data were collected through medical examination, biochemical profiling, questionnaire-based assessment and anthropometric measurement at each stage. We collected our data for three consecutive years. That is, after collecting Baseline data in 2017, we conducted three annual follow-ups in 2018, 2019 and 2020. in each phase, we invited participants to visit the health center in Kerdabad neighborhood for clinical examinations and evaluations, laboratory measurements, and completing research questionnaires. Self-reported data was validated by a medical interview. |
| Data format | Raw |
| Description of data collection | This cohort study is centered in the Kerdabad neighborhood of Isfahan, Iran. Isfahan is located in central Iran and is the third most populous city with a population of more than 1.8 million. The main criteria for selecting this location were population diversity of the inhabitants and its generalizability to the main population of Isfahan city according to their mean household income and socio-economic status. One person from each household was randomly selected and if this nominee did not meet our eligibility criteria, another individual from the same household was randomly selected and invited to join the study. This process continued until we reached the required sample size of individuals who consented to enrol in this survey. The eligibility criteria were as follows: consent to participation 18-65 years of age non-pregnant women Intellectual ability to correctly understand and fill the provided questionnaire Physical ability to come to the local health canter and undergo the data collection process Not having a terminal disease Not under active treatment for malignancies Not relative of a previously selected individual (up to the 3rd degree) |
| Data source location | City/Town/Region: Isfahan/ Esfahan/ Kerdabad neighborhood Country: Iran Latitude and longitude for collected samples/data: 32.6432° N, 51.7348° E |
| Data accessibility | Our data is not publicly available. For ethical reasons, our data has access controls. We have made available to the public only one codebook of the data of the current research in the form of an Excel file, In codebook file,we have provided the detailed specifications of medical examination, biochemical profiling, questionnaire-based assessment and anthropometric measurement at each stage. In addition, we have presented the data of 50 participants over 4 years as an example. To access the file including all data of the the project, researchers can complete the Data Use Agreement (DUA) file and send an email to Peyman Adibi; the main project manager, at adibi@med.mui.ac.ir. DUA is uploaded in supplementary files. Direct URL to codebook, data of 50 participants and DUA: https://doi.org/10.7910/DVN/BR2VLZ |
Value of the Data
-
•
The data is significant as it is the first in Iran and among the leading centers worldwide to have designed and generated such a multi-domain, interdisciplinary dataset, aiming to understand the interplay between different factors in shaping functional somatic syndromes.
-
•
Functional somatic syndromes are challenging to diagnose for clinicians. In some cases, symptoms are attributable to a known disease entity, while in others, they result from an unrecognized disorder. Therefore, our knowledge of functional somatic syndromes is incomplete, and we do not fully understand the role of various factors in these syndromes. As a result, a multi-disciplinary dataset covering functional symptoms, psychological assessment, lifestyle, and laboratory data is required for better patient management.
-
•
The detailed and validated time series data collected in this study can be used to clarify functional disorder entities and analyze participants' symptom/syndrome variability over time.
-
•
The datasets provided in this study can be utilized by researchers in different medical disciplines, such as internal medicine specialists and psychiatrists, health psychologists, health policymakers, and clinicians.
1. Objective
Functional somatic syndromes present a challenge to clinicians for several reasons, as patients with functional somatic symptoms exhibit considerably diverse symptoms. The diversity of symptoms in patients with chronic functional somatic symptoms supports the concept that symptoms do not cluster into well-defined, distinct syndromes. Additionally, although affected patients frequently present with predominant symptom features pertaining to one organ system at the time of consultation, the majority have multisystemic symptomatology when assessed comprehensively. There are variations over periods of time in symptoms that may affect patient-reported diagnosis in a fixed-time format.
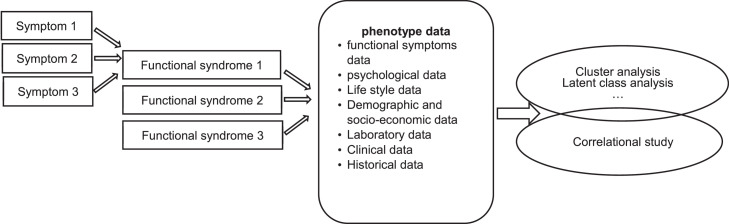
Furthermore, diseases are usually defined by specific pathophysiological processes using generally agreed-upon biological markers. In the case of functional somatic syndromes, the etiology and pathophysiology are yet to be identified. The lack of detectable physiological or anatomical abnormalities often diminishes the relevance, or even questions the actual existence of such symptoms and syndromes [1], [2], [3], [4], [5]. Our knowledge of functional somatic syndromes is incomplete, and we do not fully understand the etiologic roles of biological, psychological, and sociocultural factors in these syndromes. Therefore, a multi-disciplinary dataset covering functional symptoms, psychological assessment, lifestyle, and laboratory data is required for better patient management. This dataset was created as part of the Isfahan Functional disorders (ISFUN) study [6] (see Fig. 1).
Fig. 1.
Gathering a multi-faceted big data to overcome the ambiguity of functional disorders.
2. Data Description
In this project, we collected seven datasets: (a) functional symptom assessment across multiple body organs, (b) psychological assessment, (c) lifestyle variables, (d) demographic and socio-economic variables, (e) laboratory measurements, (f) clinical examination, and (g) historical information.
Functional symptom assessment included the evaluation of somatoform symptoms, functional gastrointestinal symptoms, fibromyalgia diagnostic criteria, non-cardiac chest pain, low back pain, chronic pelvic pain, sexual dysfunction, headache, and allergic reactions.
Psychological assessments included the evaluation of anxiety, depression, post-traumatic stress, stressful life events, psychosomatic disorders, somatic symptom disorder, body image, eating attitudes, severity of pain, neuroticism, and extraversion. We also assessed attachment, coping style, life satisfaction, perceived social support, and wellbeing. Additionally, in the fourth year of follow-up, we changed the questions of the post-traumatic stress questionnaire to focus on the COVID-19 epidemic.
Lifestyle variables included meal patterns, smoking, drinking, sleep quality, physical activity, and food frequency.
Demographic and socio-economic variables included age, gender, occupation, marital status, years of education (excluding rejection), number of children, and socio-economic status.
Laboratory measurements captured fasting blood glucose, renal, liver, and thyroid function panel, lipid profile, minerals, complete blood count, inflammatory panel, stool, and urine samples.
Clinical examination included measurements of blood pressure, anthropometric parameters (i.e., weight, height, neck, chest, waist, and hip circumferences), body composition analysis (by bioelectrical impedance), lung function (i.e., spirometry), pain sensitivity (using a handheld algometer), and adipose tissue thickness (by skinfold caliper).
Historical information included past history of disease, history of medicine use, and family history of disease.
3. Experimental Design, Materials and Methods
This cohort study is centered in the Kerdabad neighborhood of Isfahan, Iran. Isfahan is located in central Iran and is the third most populous city, with a population of more than 1.8 million. The main criteria for selecting this location were the population diversity of the inhabitants and its generalizability to the main population of Isfahan city, according to their mean household income and socio-economic status.
This multidisciplinary, population-based longitudinal cohort study did not have a disease-oriented approach. Seemingly healthy individuals were recruited, and a diverse range of data was collected. Self-reported data was validated by a medical interview.
We collected our data for four consecutive years. That is, after collecting baseline data in 2017, we conducted three annual follow-ups in 2018, 2019, and 2020. The baseline data collection phase was completed in 2018. A total of 2867 individuals were invited (mean age=39.59±10.4, 1436 male), from which 1943 consented to enroll in the study (mean age=39.6±10.22, 885 male). Thirteen individuals who did not fully contribute were later excluded. Demographic characteristics between those who consented to join and those who did not were compared, and no significant statistical difference was observed in age, gender, and educational level of the two groups. All participants from the base cohort were recalled for the first follow-up visit after one year. In this phase, 1697 participants responded (response rate=88%, mean age=40.03±10.2, 756 male). Of those, 233 individuals who were lost to follow-up, one had passed away, 12 had migrated out of the area, 59 could not be located, and 161 were not willing to continue their participation. The second annual follow-up was concluded with 1616 participants (response rate=95%, mean age=40.15±10.2, 728 male). Three of the former participants had died, 18 had migrated out of the area, and 63 were not willing to continue their participation in this cohort study. Finally, the third annual follow-up was concluded with 1176 participants.
Ethics Statements
Written informed consent was obtained from all participants prior to data collection. Approval for conducting the study was granted by the ethics committee of the Ministry of Health and Medical Education and Isfahan University of Medical Sciences [IR.MUI.REC.1395.1.149].
CRediT authorship contribution statement
Peyman Adibi: Conceptualization, Supervision, Funding acquisition. Simindokht Kalani: Writing – original draft, Writing – review & editing, Data curation. Alireza Ani: Writing – review & editing. Hassan Shahoon: Investigation, Resources. Awat Feizi: Data curation, Methodology. Hamidreza Roohafza: Conceptualization, Project administration, Data curation, Methodology.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We wish to thank all participants and their families for their commitment to this study. We acknowledge the management of Isfahan province health center and Isfahan health center #1 for their administrative supports. We also acknowledge the staff and health workers at Kerdabad health center for their gracious role in recruiting and following the participants. We appreciate the support from Ammar Hassanzadeh Keshteli and Hassan Shahoon for their time and effort supporting this project.
This work has been supported by the Iranian Ministry of Health and Medical Education [700/144], Isfahan University of Medical Sciences [195149] and the Iranian National Institute for Medical Research Development (NIMAD) [972953].
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dib.2023.109267.
Appendix. Supplementary materials
Data Availability
References
- 1.Kitselaar W.M., Van Der Vaart R., Perschl J., Numans M.E., Evers A.W. Predictors of persistent somatic symptoms in the general population: a systematic review of cohort studies. Psychosom. Med. 2023;85(1):71–78. doi: 10.1097/PSY.0000000000001145. [DOI] [PubMed] [Google Scholar]
- 2.Roenneberg C., Sattel H., Schaefert R., Henningsen P., Hausteiner-Wiehle C. Functional somatic symptoms. Dtsch Arztebl. Int. 2019;116(33-34):553–560. doi: 10.3238/arztebl.2019.0553. PMID: 31554544; PMCID: PMC6794707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donnachie E., Schneider A., Enck P. Comorbidities of patients with functional somatic syndromes before, during and after first diagnosis: a population-based study using Bavarian routine data. Sci. Rep. 2020;10(1):9810. doi: 10.1038/s41598-020-66685-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finset A. Why do doctors not learn how to explain “medically unexplained symptoms”? Patient Educ. Couns. 2018;101(5):763–764. doi: 10.1016/j.pec.2018.03.022. PMID: 29678266. [DOI] [PubMed] [Google Scholar]
- 5.Henningsen P., Zipfel S., Sattel H., Creed F. Management of functional somatic syndromes and bodily distress. Psychother. Psychosom. 2018;87(1):12–31. doi: 10.1159/000484413. Epub 2018 Jan 6. PMID: 29306954. [DOI] [PubMed] [Google Scholar]
- 6.Adibi P, Ani A, Vaez A, Hadizadeh F, Snieder H, Roohafza H. Multidisciplinary approach to functional somatic syndromes: study protocol for a population-based prospective cohort study. BMJ Open. 2022;12(7) doi: 10.1136/bmjopen-2021-048941. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.