Abstract
Superior mesenteric artery (SMA) syndrome (also known as Wilkie's syndrome, cast syndrome, or aorto-mesenteric compass syndrome) is an obstruction of the duodenum caused by extrinsic compression between the SMA and the aorta. The median age of patients is 23 years old (range 0-91 years old) and predominant in females over males with a ratio of 3:2. The symptoms are variable, consisting of postprandial abdominal pain, nausea and vomiting, early satiety, anorexia, and weight loss and can mimic anorexia nervosa or functional dyspepsia. Because recurrent vomiting leads to aspiration pneumonia or respiratory depression via metabolic alkalosis, early diagnosis is required. The useful diagnostic modalities are computed tomography as a standard tool and ultrasonography, which has advantages in safety and capability of real-time assessments of SMA mobility and duodenum passage. The initial treatment is usually conservative, including postural change, gastroduodenal decompression, and nutrient management (success rates: 70%-80%). If conservative therapy fails, surgical treatment (i.e., laparoscopic duodenojejunostomy) is recommended (success rates: 80%-100%).
Keywords: Superior mesenteric artery syndrome, Wilkie’s syndrome, Cast syndrome, Aorto-mesenteric compass syndrome
Core Tip: To summarize, superior mesenteric artery syndrome (SMAS) is a rare condition that occurs when the superior mesenteric artery compresses the third part of the duodenum. This compression can cause obstructive symptoms and weight loss. SMAS can be caused by a variety of factors, including abnormal anatomy, rapid weight loss, and previous abdominal surgery. It is most commonly seen in young, thin females, but can occur in males and people of any age or body type. Treatment may involve dietary modifications, medications, and surgery to correct the underlying cause. If left untreated, SMAS can lead to serious complications, including malnutrition and intestinal damage.
INTRODUCTION
Superior mesenteric artery (SMA) syndrome is a rare cause of duodenal obstruction by extrinsic compression between SMA and the aorta (SMA-Ao) (Figure 1), and a morbid entity when the diagnosis is delayed[1-3]. Von Rokitansky[1] first described this entity in his textbook with a case presentation in 1842. Later, Wilkie[2] described pathological and diagnostic findings in details with 75 cases of his own in 1927, thus SMA syndrome is also known as Wilkie’s syndrome. The other names are reported as cast syndrome, aorto-mesenteric compass syndrome, or mesenteric duodenal obstruction[3]. A cast, which is used to treat certain congenital deformities such as scoliosis and hip displacement, is a major cause of SMA syndrome[4-6]. By the year 2022, more than 730 articles with approximately 2400 cases of SMA syndrome had been reported (author’s review in PubMed). Initial conservative therapy occasionally fails, and surgical or, more recently, endoscopic surgical duodenojejunostomy is successfully performed. This review provides clinical information of SMA syndrome in details.
Figure 1.
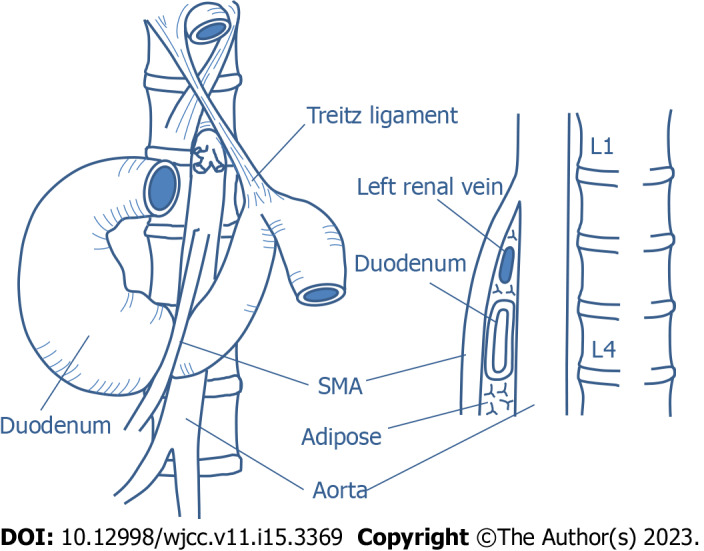
Anatomy related to superior mesenteric artery syndrome. SMA: Superior mesenteric artery.
EPIDEMIOLOGY AND ETIOLOGY
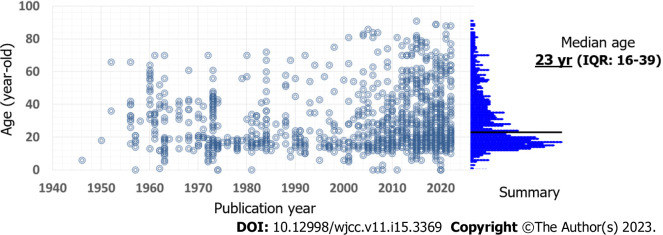
SMA syndrome frequently concerns young adult female[2,7-12]. Our review found the median age is 23 years old (inter-quartile range: 16-39) but any age can be affected (range 0-91 years old), with increasing trends of elder patients with SMA syndrome in recent literatures (Figure 2). The affected age seems to be related to underlying patients’ conditions (i.e., congenital scoliosis at children or weight loss due to chemotherapy). Whereas the affected gender is, as reported previously, predominant in females over males with a ratio of 3:2. The incidence of SMA syndrome in the general population has been estimated at 0.013%-0.78% based on radiographic studies[7,13-16], though an accurate prevalence of the disease is unknown, depending on under- or over-diagnosis in clinical practice and each patient’s condition[10,17] (Table 1)[12,18-34]. A prospective case-control study conducted by Xu et al[27] found the incidence of SMA syndrome is 2.67% (26/973 admissions for 9 years). Scoliosis and burn injuries are well-known etiologies of SMA syndrome and clinicians should be aware of this entity. In contrast, in functional dyspepsia patients, the incidence is much higher (10.8%) than in the general population, which is explained by clinicians under-diagnosing.
Figure 2.
Published patient age. Dot indicates an individual case. The data is based on our review. IQR: Interquartile range.
Table 1.
Incidence of superior mesenteric artery syndrome in several populations
|
Population
|
Incidence (%)
|
Ref.
|
| Acute general hospitals | 0.001-0.0052 | [18] |
| Chronic-care hospital | 0.097 | [18] |
| Hospital admissions | 0.05-2.67 | [12,27,28] |
| Upper gastrointestinal endoscopy | 0.48 | [29] |
| Post-scoliosis surgery + cast | 0.5-3.4 | [19,30-34] |
| Spinal cord injury | 0.53 | [21] |
| Burn injury | 1.0-1.12 | [22-24] |
| Anorexia nervosa (admitted) | 2.73 | [25] |
| Functional dyspepsia | 10.8 | [26] |
PATHOPHYSIOLOGY
Decreasing SMA-Ao angle causes compression to the third part of the duodenum (see “DIAGNOSIS” part). Decreases in the SMA-Ao angle can be either congenital or acquired (Table 2)[2,4-6,17-19,22,25,30,33-60]. The major causes of SMA syndrome involve body weight loss and resulting loss of mesenteric fat tissue between SMA-Ao, which in turn, makes a narrower angle between the vessels. The reasons for weight loss include several types of dietary conditions (eating disorders and malabsorptive diseases), hypermetabolism (drugs and burns), and cachexia causing conditions (tuberculosis and malignancy). Especially in severe injuries and burns, prolonged bedrest in a supine position increases risk of compression of the duodenum. Scoliosis treatments (surgery and cast) and scoliosis itself are well-known causes of SMA syndrome. The lengthening of the spine during scoliosis surgery is thought to be the underlying pathophysiology. Intestinal surgeries including ileal pouch-anal anastomosis and colectomy are also well-described causes, reducing the SMA-Ao angle due to pulling on the mesentery. Congenitally short or hypertrophic ligament of Treitz is a major cause in children.
Table 2.
Etiology of superior mesenteric artery syndrome
|
Etiology
|
Ref.
|
|
| Congenital | ||
| Short or high insertion of Treitz ligament | [60] | |
| Low origin of the SMA | [35] | |
| Spinal deformity (Scoliosis, Marfan, etc.) | [36,37] | |
| Familial | [38,39] | |
| Malrotation of SMA and SMV | [40,41] | |
| Malrotation of intestine | [2] | |
| Body weight loss | ||
| Diet and obesity surgery (sleeve surgery) | [5,42] | |
| Eating disorders (anorexia nervosa, anorexia bulimia) | [25,36] | |
| Malabsorption | [17] | |
| Malignancy | [17,18,35] | |
| Tuberculosis | [44] | |
| Chemotherapy | [45,46] | |
| Trauma (Burn injury, brain injury, spinal cord injuries, etc.) | [22,47,48] | |
| Neural disorders (ALS, MELAS, paraplegia, cerebral palsy, etc.) | [49,50] | |
| Drug or alcohol abuse | [36] | |
| Rheumatoid arthritis | [51] | |
| Scoliosis surgery | [19,30-34] | |
| Intestinal surgery (IPAA, colectomy, etc.) | [36,52,53] | |
| Aging (bed rest, frail, vascular calcification, etc.) | [54,55] | |
| Body cast | [4-6] | |
| "Pseudo-" SMA syndrome | ||
| Aortic artery aneurysm (Aortoduodenal syndrome) | [56-58] | |
| Surgery near or around the SMA and 3rd duodenum | [59] | |
SMA: Superior mesenteric artery; SMV: Superior mesenteric vein; ALS: Amyotrophic lateral sclerosis; MELAS: Mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes; IPAA: Ileal pouch-anal anastomosis.
Although it is not pure SMA syndrome, aortic artery aneurysm (AAA) and surgery near or around the SMA and 3rd duodenum induces “pseudo-” SMA syndrome. AAA-related SMA syndrome was first reported by Dr. Osler as aortoduodenal syndrome[57-59].
SYMPTOMS
Patients with SMA syndrome suffer from vague and nonspecific symptoms, such as nausea, vomiting, epigastric pain, early satiety and post-prandial discomfort, bloating (abdominal distension), and weight loss, which can mimic anorexia nervosa and functional dyspepsia[8,12,61]. The epigastric pain and discomfort are more severe in a supine position and relieved in the lateral decubitus position (positioning knees to the chest) which reduces tension on the small bowel mesentery[61]. Especially in acute phase, severe duodenal obstruction leads to severe symptoms and life-threatening dilatation of the stomach[8,12,61]. In contrast, in chronic phase, the recurrent nausea and vomiting leads to inadequate food intake, resulting in severe weight loss and thus, aggravation of the syndrome[8,12,61].
COMPLICATIONS AND COMORBIDITIES
Various complications of SMA syndrome have been reported (Table 3)[35,62-86]. Notably, unrecognized or severe cases may progress to life-threatening complications, such as hypovolemic shock, aspiration pneumonia, and sudden death, even in young patients. Mechanisms of sudden death remain unclear, and several hypotheses, however, can be raised based on published cases including autopsies - arrhythmia by severe hypokalemia, severe compression of the inferior vena cava by dilated duodenum, or severe pulmonary depression induced by alkalosis and increased abdominal pressure. Thus, immediate corrections of blood election and volume and early reduction of intestinal pressure should be required in severe cases. The most frequent complication is gastrointestinal injury caused by retained or refluxed peptic acid and bile acid as well as elevated intraluminal pressure. The incidence of mucosal injury has been reported as 25%-59% in patients with SMA syndrome[62,73]. Inadequately treated or chronic mucosal injuries may progress to emphysema, necrosis, portal venous gas, and pneumoperitoneum. Elevated intraluminal pressure at the second portion of the duodenum disturbs the flow of pancreatic juice, occasionally resulting in elevated pancreatic enzymes and acute pancreatitis. Vomiting itself can increase serum amylase (mainly from salivary glands), so pancreatic amylase isozyme and lipase should help to recognize pancreatic abnormalities. Recurrent vomiting also leads to aspiration pneumonia, dehydration, electrolyte abnormalities, and severe malnutrition. SMA syndrome sometimes co-exists with other vascular compression diseases (Table 3)[87-90]. Of these, nutcracker phenomenon is the most frequent based on anatomic location to the SMA. It is a condition that occurs when the left renal vein becomes compressed between the aorta and SMA with similar symptoms as SMA syndrome.
Table 3.
Complications and comorbidities of superior mesenteric artery syndrome
|
Complications
|
Ref.
|
||
| Gastrointestinal complications 25%-59% in SMA syndrome | [62,73] | ||
| Esophageal inflammation, bleeding, and ulcer | [60,80,81] | ||
| Gastric inflammation, ulcer, emphysema, ischemia, necrosis, perforation, and bezoar | [82-85] | ||
| Duodenal inflammation, ulcer, mucosal necrosis, emphysema, and bezoar | [63,64,86] | ||
| Portal venous gas and thrombosis | [65,66,84] | ||
| Pneumoperitoneum and pneumomediastinum | [67,68] | ||
| Pancreato-biliary complications | |||
| Elevated serum pancreatic and/or biliary enzymes | [69] | ||
| Acute and chronic pancreatitis | [85] | ||
| Jaundice | [70] | ||
| Pulmonary complications | |||
| Aspiration pneumonia | [71] | ||
| Adult respiratory distress syndrome | [72] | ||
| Dehydration | |||
| Low blood pressure | [75] | ||
| Acute kidney injury | [75] | ||
| Shock | [75] | ||
| Electrolytes and gas abnormalities | |||
| Hypokalemia | [76] | ||
| Hyponatremia | [76] | ||
| Metabolic alkalosis | [76] | ||
| Severe malnutrition | [77] | ||
| Recurrent pregnancy loss | [78] | ||
| Sudden death | [82] | ||
| Comorbidities related to SMA syndrome | |||
| Nutcracker phenomenon | [87,88] | ||
| Celiac axis compression syndrome (median arcuate ligament syndrome) | [89,90] | ||
SMA: Superior mesenteric artery.
DIAGNOSIS
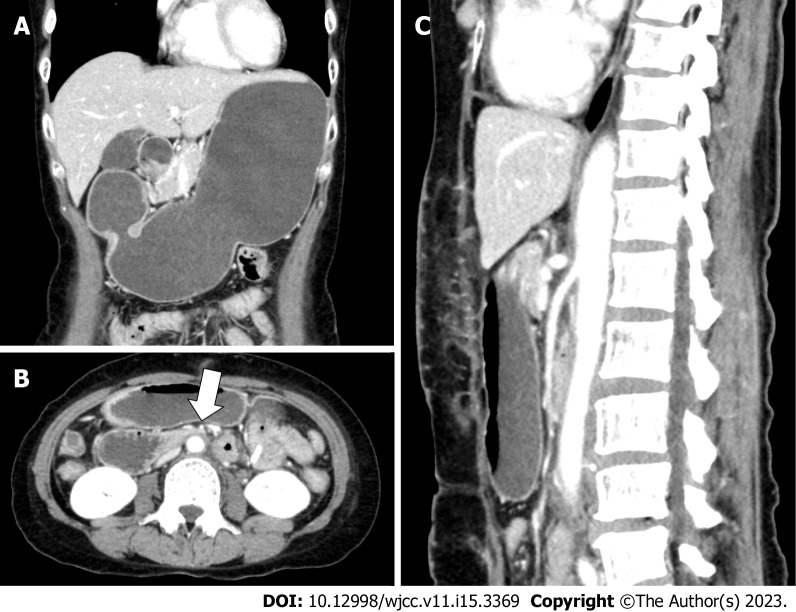
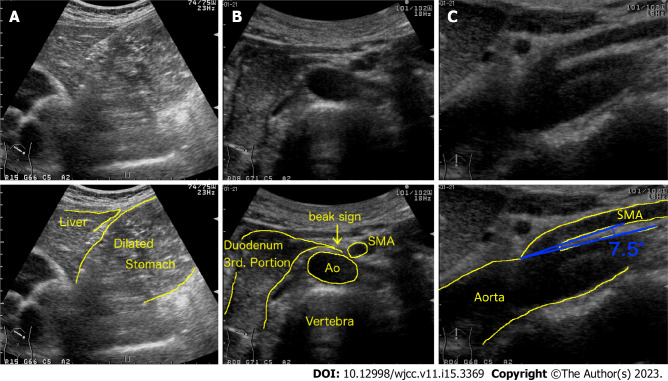
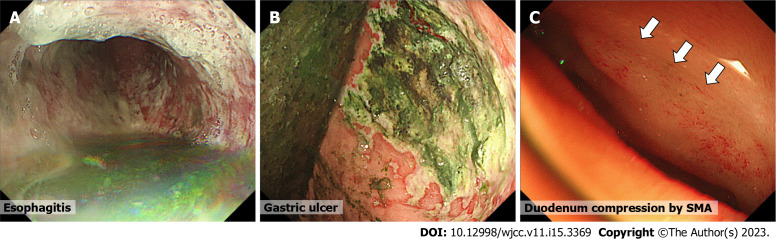
Due to its non-specific symptoms, SMA syndrome might be overlooked in clinical practice[26,91]. Even in radiologists, the duodenum seems to be a neglected segment in the intestine[92]. SMA syndrome requires a high degree of clinical suspicion and few teaching methods have been reported[93,94]. The diagnosis is based on clinical symptoms supported by radiological evidence of duodenal obstruction. Traditional criteria for SMA syndrome are based on barium X-ray studies (Figure 3): (1) Dilatation of the first and second parts of the duodenum with or without gastric dilatation; (2) abrupt vertical or oblique compression of the third part of the duodenum; (3) reverse flow of contrast proximal to the obstruction; (4) significant delay (4-6 h) in gastroduodenal transit; and (5) relief of obstruction after postural changes (the prone knee-chest or lateral decubitus position)[17,18,95]. Recently, in addition to barium studies, various imaging modalities have been used to confirm SMA syndrome, such as computed tomography (CT), abdominal ultrasound (US), magnetic resonance imaging (MRI), endoscopy and endoscopic ultrasonography (EUS), etc. (Table 4). Many cases are diagnosed by these modalities, which can directly visualize the SMA compression of the duodenum without barium studies. The standard diagnostic modality is CT scan (Figure 4) which allows for both diagnosis of SMA syndrome with measurement of the SMA-Ao angle and distance as well as detection of complications, such as gastric necrosis, portal vein gas, acute pancreatitis etc. 3D-CT is more helpful in recognizing the anatomy of SMA, the aorta and duodenum[96]. The normal SMA-Ao angle is between 38 to 65 degrees and has a distance of 10 to 33 mm[5,97]. Unal et al[97] reported the cutoff value is 22 degrees on the SMA-Ao angle and 8 mm on a distance with a 42.8% sensitivity and 100% specificity. Abdominal US is another modality that provides a convenient, quick, noninvasive tool to diagnose SMA syndrome[97-99]. The sensitivity of abdominal US in diagnosis of SMA syndrome has been confirmed in a comparison study with CT findings[97]. Abdominal US benefits from an improvement of image resolution and can clearly visualize the duodenum and SMA-Ao angle (Figure 5 and Video 1). Endoscopy can detect gastrointestinal complications, such as mucosal injury, bleeding, and bezoar, etc. (Figures 6A and B). It can also reveal extrinsic compression (by SMA) at the 3rd portion of duodenum (Figure 6C). Further, EUS with mini-probes can be used to confirm the compression by SMA and also measure SMA-Ao distance[36,100]. Recently, linear EUS has been used for measuring the SMA-Ao angle and also endoscopic duodenojejunostomy (see TREATMENTS). Laboratory tests are not diagnostic, but they are necessary to identify the presence of electrolytic complications and pancreato-biliary abnormalities. As for differential diagnosis, almost all disorders mimicking SMA syndrome are summarized in Table 5[14,26,44,55-59,86,101-127]. Patients with eating disorders, functional dyspepsia, and peptic ulcer disease present non-specific symptoms masquerading as SMA syndrome. In addition, many diseases that potentially involve or compress duodenum should be suspected of and ruled out by CT, abdominal US, or other modalities.
Figure 3.

Upper gastrointestinal series (barium X-ray) of a 16-year-old male with superior mesenteric artery syndrome. Arrow indicates obstructive compression of the third portion of the duodenum.
Table 4.
Diagnostic modalities for superior mesenteric artery syndrome
|
Modalities
| |
| Plain film X-ray | |
| Barium X-ray | |
| Angiogram | |
| CT | |
| Plain | |
| Enhanced (3D-CT) | |
| Abdominal ultrasound | |
| B-mode | |
| Doppler-mode | |
| MRI | |
| MR angiography | |
| MR enterography | |
| Endoscopy | |
| White light imaging | |
| Ultrasonography (EUS) | |
| Gastric-emptying scintigraphy | |
| Multi-channel manometry | |
CT: Computed tomography; 3D: Three-dimensional; MRI: Magnetic resonance imaging; EUS: Endoscopic ultrasonography.
Figure 4.
Enhanced computed tomography images of a 56-year-old female with superior mesenteric artery syndrome. A: Coronal view; B: Axial view; C: Sagittal view. Computed tomography images show a markedly distended stomach and proximal duodenum by extrinsic compression between the superior mesenteric artery (arrow in panel B) and aorta.
Figure 5.
Abdominal ultrasonographic images of a 53-year-old female with superior mesenteric artery syndrome. A and B: Upper abdominal ultrasonography shows a markedly dilated stomach (A) and obstruction of duodenum (B, which looks like beak, beak sign) by extrinsic compression between the superior mesenteric artery (SMA) and aorta (Ao); C: The SMA-Ao angle (7.5 degree) and distance (5 mm) are decreased. SMA: Superior mesenteric artery; Ao: Aorta.
Figure 6.
Endoscopic findings of patients with superior mesenteric artery syndrome. A and B: Esophagitis (A) and gastric ulcer (B) with retained luminal contents; C: compression area in the third portion of the duodenum.
Table 5.
Differential diagnoses of superior mesenteric artery syndrome
|
Disorders mimicking SMA syndrome
|
Ref.
|
||
| Similar symptoms by... | |||
| Eating disorder | |||
| Anorexia nervosa, anorexia bulimia | [125] | ||
| CIPO | [126] | ||
| Peptic ulcer disease | [127] | ||
| Reflux esophagitis | [101] | ||
| Functional dyspepsia | [26] | ||
| Cyclic vomiting syndrome | [102] | ||
| Pancreatitis | [103] | ||
| Gastric outlet obstruction | [104] | ||
| Involvement of duodenum by... (other disorders) | |||
| Tubercular infection | [105,106] | ||
| Megaduodenum (localized CIPO) | [107] | ||
| Henoch-Schönlein purpura | [108-110] | ||
| Crohn's disease | [111,112] | ||
| Celiac disease | [86] | ||
| Ectopic pancreas | [113] | ||
| Duodenal diverticula | [114] | ||
| Duodenal edema | [115] | ||
| Tumor | |||
| Primary or metastatic duodenal cancer, pancreatic cancer, lymphoma, etc. | [14,116] | ||
| Anatomical abnormality (web, diaphragm) | [117] | ||
| Foreign body (bezoar, etc.) | [118] | ||
| Extrinsic compression by... (non-SMA) | |||
| Aortic artery aneurysm (Aortoduodenal syndrome) | [56-58] | ||
| Stent or filter | |||
| Mesenteric artery, aorta, IVC, etc. | [119,120] | ||
| Horseshoe kidney | [121] | ||
| Lymph node | [122] | ||
| Abscess | [123] | ||
| Traumatic false aneurysm | [124] | ||
SMA: Superior mesenteric artery; CIPO: Chronic idiopathic intestinal pseudo-obstruction; IVC: Inferior vena cava.
TREATMENTS
The therapeutic options are summarized in Table 6. The initial treatment is usually managed conservatively by decompression of dilated stomach and duodenum by postural change and/or nasal gastric tube suction[128,129]. Positioning the patient in the left lateral or sitting position should be helpful[95,130]. However, the best position for each patient may vary because recent studies revealed there is a variation of the SMA position and movement[131-133]. In addition to gastric tube suction, intravenous metoclopramide can enhance gastrointestinal motility and help decompression[134,135]. After decompression therapy, gaining weight to increase adipose tissue between SMA and aorta should be considered. Nasal gastric feeding is effective, but the jejunal tube is more ideal while endoscopic assistant should be considered[136]. Total parenteral nutrition is a useful option for initial nutrient treatment and if the intestinal feedings are impossible. These nutrition managements contribute to the restoration of adipose tissue to increase the angle at the origin of the SMA[28].
Table 6.
Treatments for superior mesenteric artery syndrome
|
Therapeutic methods
| ||
| Conservative therapy | ||
| Decompression of dilated stomach and duodenum by | ||
| Postural change (left lateral, sitting position) | ||
| Nasal gastric tube suction | ||
| Medication (metoclopramide) | ||
| Gaining weight by | ||
| Giving multiple small feeds | ||
| Feeding tube (nasal gastric or jejunal) | ||
| Total parenteral nutrition | ||
| Surgical therapy | ||
| Anterior transposition of the third part of duodenum | ||
| Gastroduodenostomy | ||
| Gastrojejunostomy | ||
| Duodenojejunostomy | ||
| Strong’s procedure (a division of the ligament of Treitz) | ||
| Duodenal lowering | ||
| Ladd's procedure | ||
| Endoscopic therapy | ||
| Lumen-apposing metal stent1 by | ||
| EUS-guided gastrojejunostomy | ||
Lumen-apposing metal stent: Potential option based on case reports.
EUS: Endoscopic ultrasonography.
Surgical therapy, however, can be recommended if conservative therapies fail especially in elder patients with multiple abdominal operation histories, immobility (bed rest), long history of SMA syndrome and arteriosclerosis of SMA. Surgical therapy might be considered earlier before a patient’s conditions worsen and complications occur[129]. The best timing for transition to surgical options is not clear. Shin et al[137] recommend 6 wk at least of conservative therapy based on the average response rate to this method. There is currently no randomized study conservative vs surgical therapy. A recent large cohort with 80 patients with SMA syndrome by Lee et al[128] revealed the overall success and recurrence rates of conservative therapy were 71.3 and 15.8%, respectively. The need for surgical therapy was 18.7% of patients (15/80 cases), which is similar to other recent cohorts 11.5%-22.2%[8,138,139]. These recent operation rates are lower than previously reported (70%) in 1974[140], likely due to advances in nutritional therapies and medications[128]. Various surgical procedures include laparoscopic, laparotomic, or robotic gastrojejunostomy, gastroduodenostomy and duodenojejunostomy, Strong’s procedure (a division of the ligament of Treitz), anterior transposition of the third part of duodenum, duodenal lowering, Ladd's procedure, and transabdominal duodenojejunostomy[141-145]. Since 1998, when the first successful laparoscopic duodenojejunostomy was performed, most surgeons prefer laparoscopic duodenojejunostomy because of its safety and effectiveness (success rates: 80%-100%)[141-143]. Laparoscopic approach has been reported to shorten post-operative length of hospital stay[129,142]. Most recently, a new technique of endoscopic gastrojejunostomy (so called lumen-apposing metal stent) has also been reported in several case reports as a safe and effective therapeutic option[146-148].
CONCLUSION
In conclusion, superior mesenteric syndrome is a serious condition that requires prompt diagnosis and treatment to prevent long-term complications. Diagnosis can be challenging and may involve imaging studies, such as CT or MR, and upper gastrointestinal endoscopy. Due to the non-specific nature of clinical obstructive presentations, recognition of risk factors such as rapid weight loss, previous abdominal surgery (typically bariatric surgery), trauma or congenital anomalies can predispose patients toward the development of SMA syndrome. These conditions are typically driven by a reduction in the mesenteric fat pad or an abnormal angle between the SMA and duodenum. Early diagnosis and treatment are essential to prevent complications and ensure a successful outcome.
ACKNOWLEDGEMENTS
We thank Masuzaki K and Adachi Y for the excellent reference contribution.
Footnotes
Conflict-of-interest statement: All authors have no conflict-of-interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: December 29, 2022
First decision: February 2, 2023
Article in press: April 18, 2023
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kharlamov AN, Netherlands; Osatakul S, Thailand; So Taa Kum A, Brazil S-Editor: Yan JP L-Editor: A P-Editor: Chen YX
Contributor Information
Akihiko Oka, Department of Internal Medicine II, Shimane University Faculty of Medicine, Izumo 693-8501, Shimane, Japan. aoka@med.shimane-u.ac.jp.
Muyiwa Awoniyi, Department of Gastroenterology, Hepatology and Nutrition, Digestive Disease and Surgery Institute, Hepatology Section, Cleveland Clinic, Cleveland, OH 44195, United States.
Nobuaki Hasegawa, Department of Internal Medicine II, Shimane University Faculty of Medicine, Izumo 693-8501, Shimane, Japan.
Yuri Yoshida, Clinical Laboratory Division, Shimane University Hospital, Izumo 693-8501, Shimane, Japan.
Hiroshi Tobita, Division of Hepatology, Shimane University Hospital, Izumo 693-8501, Shimane, Japan.
Norihisa Ishimura, Department of Internal Medicine II, Shimane University Faculty of Medicine, Izumo 693-8501, Shimane, Japan.
Shunji Ishihara, Department of Internal Medicine II, Shimane University Faculty of Medicine, Izumo 693-8501, Shimane, Japan.
References
- 1.von Rokitansky C. Handbuch der pathologischen Anatomie. 1st edition. Vienna Branmuller and Seidel, 1842; 187. [Google Scholar]
- 2.Wilkie B. Chronic duodenal ileus. Am J Med Sci. 1927;173:643–650. [Google Scholar]
- 3.Grauer FW. Duodenal ileus (Wilkie's syndrome) arterio-mesenteric ileus. Bull Vanc Med Assoc. 1948;24:116–118. [PubMed] [Google Scholar]
- 4.Dorph MH. The cast syndrome; review of the literature and report of a case. N Engl J Med. 1950;243:440–442. doi: 10.1056/NEJM195009212431203. [DOI] [PubMed] [Google Scholar]
- 5.Hearn JB. Duodenal ileus; with reference to superior mesenteric artery compression. Md State Med J. 1965;14:65–68. [PubMed] [Google Scholar]
- 6.Berk RN, Coulson DB. The body cast syndrome. Radiology. 1970;94:303–305. doi: 10.1148/94.2.303. [DOI] [PubMed] [Google Scholar]
- 7.Ylinen P, Kinnunen J, Höckerstedt K. Superior mesenteric artery syndrome. A follow-up study of 16 operated patients. J Clin Gastroenterol. 1989;11:386–391. [PubMed] [Google Scholar]
- 8.Biank V, Werlin S. Superior mesenteric artery syndrome in children: a 20-year experience. J Pediatr Gastroenterol Nutr. 2006;42:522–525. doi: 10.1097/01.mpg.0000221888.36501.f2. [DOI] [PubMed] [Google Scholar]
- 9.Pedoto MJ, O'Dell MW, Thrun M, Hollifield D. Superior mesenteric artery syndrome in traumatic brain injury: two cases. Arch Phys Med Rehabil. 1995;76:871–875. doi: 10.1016/s0003-9993(95)80555-9. [DOI] [PubMed] [Google Scholar]
- 10.Barner HB, Sherman CD Jr. Vascular compression of the duodenum. Int Abstr Surg. 1963;117:103–118. [PubMed] [Google Scholar]
- 11.Gustafsson L, Falk A, Lukes PJ, Gamklou R. Diagnosis and treatment of superior mesenteric artery syndrome. Br J Surg. 1984;71:499–501. doi: 10.1002/bjs.1800710706. [DOI] [PubMed] [Google Scholar]
- 12.Mandarry MT, Zhao L, Zhang C, Wei ZQ. A comprehensive review of superior mesenteric artery syndrome. Eur Surg. 2010;42:229–236. [Google Scholar]
- 13.Yamamoto T, Okada K, Kasugai M, Kato M, Kan S. Laboratory and clinical studies on cefatrizine (author's transl) Jpn J Antibiot. 1977;30:763–769. [PubMed] [Google Scholar]
- 14.Anderson JR, Earnshaw PM, Fraser GM. Extrinsic compression of the third part of the duodenum. Clin Radiol. 1982;33:75–81. doi: 10.1016/s0009-9260(82)80358-9. [DOI] [PubMed] [Google Scholar]
- 15.Rosa-Jiménez F, Rodríguez González FJ, Puente Gutiérrez JJ, Muñoz Sánchez R, Adarraga Cansino MD, Zambrana García JL. Duodenal compression caused by superior mesenteric artery: study of 10 patients. Rev Esp Enferm Dig. 2003;95:485–489, 480. [PubMed] [Google Scholar]
- 16.GOIN LS, WILK SP. Intermittent arteriomesenteric occlusion of the duodenum. Radiology. 1956;67:729–737. doi: 10.1148/67.5.729. [DOI] [PubMed] [Google Scholar]
- 17.Hines JR, Gore RM, Ballantyne GH. Superior mesenteric artery syndrome. Diagnostic criteria and therapeutic approaches. Am J Surg. 1984;148:630–632. doi: 10.1016/0002-9610(84)90339-8. [DOI] [PubMed] [Google Scholar]
- 18.Lee CS, Mangla JC. Superior mesenteric artery compression syndrome. Am J Gastroenterol. 1978;70:141–150. [PubMed] [Google Scholar]
- 19.Munns SW, Morrissy RT, Golladay ES, McKenzie CN. Hyperalimentation for superior mesenteric-artery (cast) syndrome following correction of spinal deformity. J Bone Joint Surg Am. 1984;66:1175–1177. [PubMed] [Google Scholar]
- 20.Zhu Z, Qiu Y, Wang B, Yu Y. Superior mesenteric artery syndrome following scoliosis surgery: its risk indicators and treatment strategy. Stud Health Technol Inform. 2006;123:610–614. [PubMed] [Google Scholar]
- 21.Gore RM, Mintzer RA, Calenoff L. Gastrointestinal complications of spinal cord injury. Spine (Phila Pa 1976) 1981;6:538–544. doi: 10.1097/00007632-198111000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Ogbuokiri CG, Law EJ, MacMillan BG. Superior mesenteric artery syndrome in burned children. Am J Surg. 1972;124:75–79. doi: 10.1016/0002-9610(72)90172-9. [DOI] [PubMed] [Google Scholar]
- 23.Lescher TJ, Sirinek KR, Pruitt BA Jr. Superior mesenteric artery syndrome in thermally injured patients. J Trauma. 1979;19:567–571. doi: 10.1097/00005373-197908000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Reckler JM, Bruck HM, Munster AM, Curreri PW, Pruitt BA Jr. Superior mesenteric artery syndrome as a consequence of burn injury. J Trauma. 1972;12:979–985. doi: 10.1097/00005373-197211000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Watters A, Gibson D, Dee E, Mascolo M, Mehler PS. Superior mesenteric artery syndrome in severe anorexia nervosa: A case series. Clin Case Rep. 2020;8:185–189. doi: 10.1002/ccr3.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kawanishi K, Shojima K, Nishimoto M, Abe H, Kakimoto T, Yasuda Y, Hara T, Kato J. Superior Mesenteric Artery Syndrome May Be Overlooked in Women with Functional Dyspepsia. Intern Med. 2017;56:2549–2554. doi: 10.2169/internalmedicine.8647-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu L, Yu WK, Lin ZL, Jiang J, Feng XB, Li N. Predictors and outcomes of superior mesenteric artery syndrome in patients with constipation: a prospective, nested case-control study. Hepatogastroenterology. 2014;61:1995–2000. [PubMed] [Google Scholar]
- 28.Welsch T, Büchler MW, Kienle P. Recalling superior mesenteric artery syndrome. Dig Surg. 2007;24:149–156. doi: 10.1159/000102097. [DOI] [PubMed] [Google Scholar]
- 29.Sinagra E, Raimondo D, Albano D, Guarnotta V, Blasco M, Testai S, Marasà M, Mastrella V, Alaimo V, Bova V, Albano G, Sorrentino D, Tomasello G, Cappello F, Leone A, Rossi F, Galia M, Lagalla R, Midiri F, Morreale GC, Amvrosiadis G, Martorana G, Spampinato MG, Virgilio V, Midiri M. Superior Mesenteric Artery Syndrome: Clinical, Endoscopic, and Radiological Findings. Gastroenterol Res Pract. 2018;2018:1937416. doi: 10.1155/2018/1937416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xia L, Li N, Wang D, Liu M, Li JW, Bao DM, Li P. One-stage Posterior Spinal Osteotomy in Severe Spinal Deformities: A Total of 147 Cases. Clin Spine Surg. 2017;30:E448–E453. doi: 10.1097/BSD.0000000000000227. [DOI] [PubMed] [Google Scholar]
- 31.Altiok H, Lubicky JP, DeWald CJ, Herman JE. The superior mesenteric artery syndrome in patients with spinal deformity. Spine (Phila Pa 1976) 2005;30:2164–2170. doi: 10.1097/01.brs.0000181059.83265.b2. [DOI] [PubMed] [Google Scholar]
- 32.Zhu ZZ, Qiu Y. Superior mesenteric artery syndrome following scoliosis surgery: its risk indicators and treatment strategy. World J Gastroenterol. 2005;11:3307–3310. doi: 10.3748/wjg.v11.i21.3307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hod-Feins R, Copeliovitch L, Abu-Kishk I, Eshel G, Lotan G, Shalmon E, Anekstein Y, Mirovsky Y, Masharawi Y. Superior mesenteric artery syndrome after scoliosis repair surgery: a case study and reassessment of the syndrome's pathogenesis. J Pediatr Orthop B. 2007;16:345–349. doi: 10.1097/BPB.0b013e32826d1d9b. [DOI] [PubMed] [Google Scholar]
- 34.Tsirikos AI, Jeans LA. Superior mesenteric artery syndrome in children and adolescents with spine deformities undergoing corrective surgery. J Spinal Disord Tech. 2005;18:263–271. [PubMed] [Google Scholar]
- 35.Ko KH, Tsai SH, Yu CY, Huang GS, Liu CH, Chang WC. Unusual complication of superior mesenteric artery syndrome: spontaneous upper gastrointestinal bleeding with hypovolemic shock. J Chin Med Assoc. 2009;72:45–47. doi: 10.1016/S1726-4901(09)70020-6. [DOI] [PubMed] [Google Scholar]
- 36.Lippl F, Hannig C, Weiss W, Allescher HD, Classen M, Kurjak M. Superior mesenteric artery syndrome: diagnosis and treatment from the gastroenterologist's view. J Gastroenterol. 2002;37:640–643. doi: 10.1007/s005350200101. [DOI] [PubMed] [Google Scholar]
- 37.Sun Z, Rodriguez J, McMichael J, Walsh RM, Chalikonda S, Rosenthal RJ, Kroh MD, El-Hayek K. Minimally invasive duodenojejunostomy for superior mesenteric artery syndrome: a case series and review of the literature. Surg Endosc. 2015;29:1137–1144. doi: 10.1007/s00464-014-3775-4. [DOI] [PubMed] [Google Scholar]
- 38.Jain V, Singal AK, Ramu C, Raghunaathan KD. Superior mesenteric artery syndrome: a rare complication in a child with Marfan syndrome. Arch Dis Child. 2013;98:754–755. doi: 10.1136/archdischild-2013-304321. [DOI] [PubMed] [Google Scholar]
- 39.Ortiz C, Cleveland RH, Blickman JG, Jaramillo D, Kim SH. Familial superior mesenteric artery syndrome. Pediatr Radiol. 1990;20:588–589. doi: 10.1007/BF02129061. [DOI] [PubMed] [Google Scholar]
- 40.Iwaoka Y, Yamada M, Takehira Y, Hanajima K, Nakamura T, Murohisa G, Hirai R, Kitagawa M. Superior mesenteric artery syndrome in identical twin brothers. Intern Med. 2001;40:713–715. doi: 10.2169/internalmedicine.40.713. [DOI] [PubMed] [Google Scholar]
- 41.Green P, Swischuk LE, Hernandez JA. Delayed presentation of malrotation and midgut volvulus: imaging findings. Emerg Radiol. 2007;14:379–382. doi: 10.1007/s10140-007-0662-5. [DOI] [PubMed] [Google Scholar]
- 42.Shin J, Shin PJ, Bartolotta RJ. SMA-like syndrome with variant mesenteric venous anatomy. Clin Imaging. 2018;48:86–89. doi: 10.1016/j.clinimag.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 43.Neto NI, Godoy EP, Campos JM, Abrantes T, Quinino R, Barbosa AL, Fonseca CA. Superior mesenteric artery syndrome after laparoscopic sleeve gastrectomy. Obes Surg. 2007;17:825–827. doi: 10.1007/s11695-007-9125-z. [DOI] [PubMed] [Google Scholar]
- 44.Lin JA, Woods ER, Bern EM. Common and Emergent Oral and Gastrointestinal Manifestations of Eating Disorders. Gastroenterol Hepatol (N Y) 2021;17:157–167. [PMC free article] [PubMed] [Google Scholar]
- 45.Limaye CS, Karande SP, Aher SP, Pati KA. Superior mesenteric artery syndrome secondary to tuberculosis induced cachexia. J Assoc Physicians India. 2011;59:670–671. [PubMed] [Google Scholar]
- 46.Ushiki A, Koizumi T, Yamamoto H, Hanaoka M, Kubo K, Matsushita M. Superior mesenteric artery syndrome following initiation of cisplatin-containing chemotherapy: a case report. J Med Case Rep. 2012;6:14. doi: 10.1186/1752-1947-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Girotra M, Shah HR, Rego RF. An intriguing cause of intractable nausea and vomiting. Saudi J Gastroenterol. 2013;19:190–191. doi: 10.4103/1319-3767.114510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Philip PA. Superior mesenteric artery syndrome: an unusual cause of intestinal obstruction in brain-injured children. Brain Inj. 1992;6:351–358. doi: 10.3109/02699059209034949. [DOI] [PubMed] [Google Scholar]
- 49.Laffont I, Bensmail D, Rech C, Prigent G, Loubert G, Dizien O. Late superior mesenteric artery syndrome in paraplegia: case report and review. Spinal Cord. 2002;40:88–91. doi: 10.1038/sj.sc.3101255. [DOI] [PubMed] [Google Scholar]
- 50.Kwon OY, Lim SG, Park SH. Mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episode leading to recurrent superior mesenteric artery syndrome. Am J Emerg Med. 2014;32:951.e1–951.e2. doi: 10.1016/j.ajem.2014.01.059. [DOI] [PubMed] [Google Scholar]
- 51.Neuman A, Desai B, Glass D, Diab W. Superior mesenteric artery syndrome in a patient with cerebral palsy. Case Rep Med. 2014;2014:538289. doi: 10.1155/2014/538289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Padhan P, Moses V, Danda D. Superior mesenteric artery syndrome in an adult rheumatoid arthritis patient. Int J Rheum Dis. 2012;15:e4–e5. doi: 10.1111/j.1756-185X.2011.01647.x. [DOI] [PubMed] [Google Scholar]
- 53.Kremers PW, Scholz FJ, Schoetz DJ Jr, Veidenheimer MC, Coller JA. Radiology of the ileoanal reservoir. AJR Am J Roentgenol. 1985;145:559–567. doi: 10.2214/ajr.145.3.559. [DOI] [PubMed] [Google Scholar]
- 54.Gonzalez DO, Nwomeh BC. Complications in children with ulcerative colitis undergoing ileal pouch-anal anastomosis. Semin Pediatr Surg. 2017;26:384–390. doi: 10.1053/j.sempedsurg.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 55.Kitaura K, Harima K. Superior mesenteric artery syndrome with vascular calcification in a maintenance hemodialysis patient. Clin Nephrol. 2009;71:228–230. doi: 10.5414/cnp71228. [DOI] [PubMed] [Google Scholar]
- 56.Okazaki Y, Higashi Y, Takigawa H. Unusual Complication of Frailty: Superior Mesenteric Artery Syndrome. Intern Med. 2019;58:2119–2120. doi: 10.2169/internalmedicine.2493-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Osler W. Aneurysm of the abdominal aorta. Lancet. 1905;166:1089–1096. [Google Scholar]
- 58.Saigusa S, Ohi M, Imaoka H, Inoue Y. Aortoduodenal syndrome in a patient receiving maintenance haemodialysis. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-206326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sudo G, Takagi H, Nakahara S, Goto A, Hinoda Y, Nakase H. Gastrointestinal: Abdominal aortic aneurysm caused symptoms mimicking superior mesenteric artery syndrome. J Gastroenterol Hepatol. 2021;36:43. doi: 10.1111/jgh.15149. [DOI] [PubMed] [Google Scholar]
- 60.Lin CY, Lin BY, Kang PL. Duodenal obstruction after elective abdominal aortic aneurysm repair: a case report. Kaohsiung J Med Sci. 2004;20:501–505. doi: 10.1016/S1607-551X(09)70249-9. [DOI] [PubMed] [Google Scholar]
- 61.Marecek GS, Barsness KA, Sarwark JF. Relief of superior mesenteric artery syndrome with correction of multiplanar spinal deformity by posterior spinal fusion. Orthopedics. 2010;33:519. doi: 10.3928/01477447-20100526-26. [DOI] [PubMed] [Google Scholar]
- 62.Anderson WC, Vivit R, Kirsh IE, Greenlee HB. Arteriomesenteric duodenal compression syndrome. Its association with peptic ulcer. Am J Surg. 1973;125:681–689. doi: 10.1016/0002-9610(73)90165-7. [DOI] [PubMed] [Google Scholar]
- 63.Uemura S, Suzuki K, Katayama N, Imai H. Superior mesenteric artery syndrome leading to reversible mucosal gangrene. Acute Med Surg. 2017;4:375–376. doi: 10.1002/ams2.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Doski JJ, Priebe CJ Jr, Smith T, Chumas JC. Duodenal trichobezoar caused by compression of the superior mesenteric artery. J Pediatr Surg. 1995;30:1598–1599. doi: 10.1016/0022-3468(95)90165-5. [DOI] [PubMed] [Google Scholar]
- 65.Tsai CL, Chen MJ, Tan CK, Chan KS, Cheng KC. Superior mesenteric artery syndrome with hepatic portal venous gas. Med J Aust. 2007;186:48. doi: 10.5694/j.1326-5377.2007.tb00794.x. [DOI] [PubMed] [Google Scholar]
- 66.Lim JE, Duke GL, Eachempati SR. Superior mesenteric artery syndrome presenting with acute massive gastric dilatation, gastric wall pneumatosis, and portal venous gas. Surgery. 2003;134:840–843. doi: 10.1016/s0039-6060(02)21677-3. [DOI] [PubMed] [Google Scholar]
- 67.Kensinger CD, Mukherjee K, Nealon WH, Solorzano CC. Superior mesenteric artery syndrome presenting with pneumoperitoneum and pneumomediastinum. Am Surg. 2013;79:E240–E242. [PubMed] [Google Scholar]
- 68.Lee CI, Wu YH. Pneumatosis intestinalis and pneumoretroperitoneum post steroid use in a patient with superior mesenteric artery syndrome. Am J Emerg Med. 2019;37:1993.e1–1993.e3. doi: 10.1016/j.ajem.2019.06.040. [DOI] [PubMed] [Google Scholar]
- 69.Majumder S, Shergill S, Loftus CG. A Young Man With Abdominal Pain, Weight Loss, and Jaundice. Gastroenterology. 2017;152:1836–1838. doi: 10.1053/j.gastro.2016.12.044. [DOI] [PubMed] [Google Scholar]
- 70.Jeune F, d'Assignies G, Sauvanet A, Gaujoux S. A rare cause of obstructive jaundice and gastric outlet obstruction. World J Gastrointest Surg. 2013;5:192–194. doi: 10.4240/wjgs.v5.i6.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bohanon FJ, Nunez Lopez O, Graham BM, Griffin LW, Radhakrishnan RS. A Case Series of Laparoscopic Duodenojejunostomy for the Treatment of Pediatric Superior Mesenteric Artery Syndrome. Int J Surg Res. 2016;2016:1–5. [PMC free article] [PubMed] [Google Scholar]
- 72.Banerjee A, O'Neil R, Bidstrup H. Adult respiratory distress syndrome caused by superior mesenteric artery syndrome. Anaesth Intensive Care. 1994;22:602–604. doi: 10.1177/0310057X9402200519. [DOI] [PubMed] [Google Scholar]
- 73.Haas PA, Akhtar J, Kobylak L. Compression of the duodenum by the root of the mesentery. Henry Ford Hosp Med J. 1982;30:85–89. [PubMed] [Google Scholar]
- 74.Abu-Zidan FM, Hefny AF, Saadeldinn YA, El-Ashaal YI. Sonographic findings of superior mesenteric artery syndrome causing massive gastric dilatation in a young healthy girl. Singapore Med J. 2010;51:e184–e186. [PubMed] [Google Scholar]
- 75.Mohammad Kazmin NE, Kamaruzaman L, Wong Z, Fong VK, Mohd R, Mustafar R. Acute Kidney Injury Caused by Superior Mesenteric Artery Syndrome. Case Rep Nephrol. 2020;2020:8364176. doi: 10.1155/2020/8364176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shajani-Yi Z, Lee HK, Cervinski MA. Hyponatremia, Hypokalemia, Hypochloremia, and Other Abnormalities. Clin Chem. 2016;62:898. doi: 10.1373/clinchem.2015.249292. [DOI] [PubMed] [Google Scholar]
- 77.Thieme ET, Postmus R. Superior mesenteric artery syndrome. Ann Surg. 1961;154 (Suppl 6):139–143. doi: 10.1097/00000658-196112000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Iko BO, Monu JU, Orhue A, Sarkar SK. The superior mesenteric artery syndrome in pregnancy: a case resulting in recurrent pregnancy loss. Eur J Obstet Gynecol Reprod Biol. 1986;21:233–236. doi: 10.1016/0028-2243(86)90021-3. [DOI] [PubMed] [Google Scholar]
- 79.Sato H, Tanaka T. Acute gastric dilatation due to a superior mesenteric artery syndrome: an autopsy case. BMC Gastroenterol. 2014;14:37. doi: 10.1186/1471-230X-14-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ratjen E. Concomitant arterio-mesenteric obstruction of the duodenum and chronic oesophagitis; case report. Acta radiol. 1952;37:369–373. doi: 10.3109/00016925209139893. [DOI] [PubMed] [Google Scholar]
- 81.Hamdeh S, Haddad TM, Kabach A. Image of the month: A Rare Case of Superior Mesenteric Artery Syndrome Causing Upper Gastrointestinal Bleeding. Am J Gastroenterol. 2015;110:1653. doi: 10.1038/ajg.2015.141. [DOI] [PubMed] [Google Scholar]
- 82.Murakami C, Irie W, Sasaki C, Nakamaru N, Sakamoto M, Nagato J, Satoh F. Extensive gastric necrosis secondary to acute gastric dilatation: A case report. Leg Med (Tokyo) 2019;36:85–88. doi: 10.1016/j.legalmed.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 83.Moyer K, Thompson GH, Poe-Kochert C, Splawski J. Superior Mesenteric Artery Syndrome Complicated by Gastric Mucosal Necrosis Following Congenital Scoliosis Surgery: A Case Report. JBJS Case Connect. 2019;9:e0380. doi: 10.2106/JBJS.CC.18.00380. [DOI] [PubMed] [Google Scholar]
- 84.Rod J, Sarnacki S, Petit T, Ravasse P. Portal venous gas and thrombosis complicating superior mesenteric artery syndrome (Wilkie's syndrome) in a child. J Pediatr Surg. 2010;45:826–829. doi: 10.1016/j.jpedsurg.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 85.Petrosyan M, Estrada JJ, Giuliani S, Williams M, Rosen H, Mason RJ. Gastric perforation and pancreatitis manifesting after an inadvertent nissen fundoplication in a patient with superior mesenteric artery syndrome. Case Rep Med. 2009;2009:426162. doi: 10.1155/2009/426162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Amadi C, Anderson S. Refractory coeliac disease: or is it? BMJ Case Rep. 2017;2017 doi: 10.1136/bcr-2017-219271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Oh MJ. Superior Mesenteric Artery Syndrome Combined with Renal Nutcracker Syndrome in a Young Male: A Case Report. Korean J Gastroenterol. 2017;70:253–260. doi: 10.4166/kjg.2017.70.5.253. [DOI] [PubMed] [Google Scholar]
- 88.Diab S, Hayek F. Combined Superior Mesenteric Artery Syndrome and Nutcracker Syndrome in a Young Patient: A Case Report and Review of the Literature. Am J Case Rep. 2020;21:e922619. doi: 10.12659/AJCR.922619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Farina R, Gozzo C, Foti PV, Conti A, Vasile T, Pennisi I, Venturini M, Basile A. A man with the rare simultaneous combination of three abdominal vascular compression syndromes: median arcuate ligament syndrome, superior mesenteric artery syndrome, and nutcracker syndrome. Radiol Case Rep. 2021;16:1264–1270. doi: 10.1016/j.radcr.2021.02.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tseng CK, Su WB, Lai HC, Chou JW, Feng CL, Peng CY, Chen YF. Superior mesenteric artery syndrome caused by celiac axis compression syndrome: a case report and review of the literature. Eur J Gastroenterol Hepatol. 2008;20:578–582. doi: 10.1097/MEG.0b013e3282f172fa. [DOI] [PubMed] [Google Scholar]
- 91.Elbadaway MH. Chronic superior mesenteric artery syndrome in anorexia nervosa. Br J Psychiatry. 1992;160:552–554. doi: 10.1192/bjp.160.4.552. [DOI] [PubMed] [Google Scholar]
- 92.Reghunath A, Kabilan K, Mittal MK. Exploring the neglected segment of the intestine: the duodenum and its pathologies. Pol J Radiol. 2020;85:e230–e244. doi: 10.5114/pjr.2020.95477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Han F, Cheng H, Hou M, Liu R. Application of the "Hand as Foot" teaching method in superior mesenteric artery syndrome. Asian J Surg. 2021;44:1562–1563. doi: 10.1016/j.asjsur.2021.08.070. [DOI] [PubMed] [Google Scholar]
- 94.Yongqing N, Chen D, Rui L, Linlin L. The "Hand as Foot" teaching method in superior mesenteric artery syndrome. Asian J Surg. 2022;45:618–619. doi: 10.1016/j.asjsur.2021.10.008. [DOI] [PubMed] [Google Scholar]
- 95.Neri S, Signorelli SS, Mondati E, Pulvirenti D, Campanile E, Di Pino L, Scuderi M, Giustolisi N, Di Prima P, Mauceri B, Abate G, Cilio D, Misseri M, Scuderi R. Ultrasound imaging in diagnosis of superior mesenteric artery syndrome. J Intern Med. 2005;257:346–351. doi: 10.1111/j.1365-2796.2005.01456.x. [DOI] [PubMed] [Google Scholar]
- 96.Raman SP, Neyman EG, Horton KM, Eckhauser FE, Fishman EK. Superior mesenteric artery syndrome: spectrum of CT findings with multiplanar reconstructions and 3-D imaging. Abdom Imaging. 2012;37:1079–1088. doi: 10.1007/s00261-012-9852-z. [DOI] [PubMed] [Google Scholar]
- 97.Unal B, Aktaş A, Kemal G, Bilgili Y, Güliter S, Daphan C, Aydinuraz K. Superior mesenteric artery syndrome: CT and ultrasonography findings. Diagn Interv Radiol. 2005;11:90–95. [PubMed] [Google Scholar]
- 98.Le D, Stirparo JJ, Magdaleno TF, Paulson CL, Roth KR. Point-of-care ultrasound findings in the diagnosis and management of Superior Mesenteric Artery (SMA) syndrome. Am J Emerg Med. 2022;55:233.e1–233.e4. doi: 10.1016/j.ajem.2022.02.018. [DOI] [PubMed] [Google Scholar]
- 99.Chin LW, Chou MC, Wang HP. Ultrasonography diagnosis of superior mesenteric artery syndrome in the ED. Am J Emerg Med. 2007;25:864.e5–864.e6. doi: 10.1016/j.ajem.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 100.Gottlieb K. Doppler-endosonography with the GF-UE 160 electronic radial echoendoscope - current use and future potential. J Gastrointestin Liver Dis. 2007;16:455–461. [PubMed] [Google Scholar]
- 101.Su MC, Lee CH, Wang CC. Education and Imaging. Gastrointestinal: Superior mesenteric artery syndrome initially presenting like reflux esophagitis. J Gastroenterol Hepatol. 2010;25:645. doi: 10.1111/j.1440-1746.2010.06259.x. [DOI] [PubMed] [Google Scholar]
- 102.Dimopoulou A, Zavras N, Alexopoulou E, Fessatou S, Dimopoulou D, Attilakos A. Superior mesenteric artery syndrome mimicking cyclic vomiting syndrome in a healthy 12-year-old boy. J Paediatr Child Health. 2020;56:168–170. doi: 10.1111/jpc.14592. [DOI] [PubMed] [Google Scholar]
- 103.Arbell D, Gross E, Koplewitz BZ, Vromen A, Bar-Ziv J, Udassin R. Superior mesenteric artery syndrome masquerading as recurrent biliary pancreatitis. Isr Med Assoc J. 2006;8:441–442. [PubMed] [Google Scholar]
- 104.Shah D, Naware S, Thind S, Kuber R. Superior mesenteric artery syndrome: an uncommon cause of abdominal pain mimicking gastric outlet obstruction. Ann Med Health Sci Res. 2013;3:S24–S26. doi: 10.4103/2141-9248.121214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sisodiya R, Ramachandra L. Tubercular duodenal, jejunal and ileocecal stricture in a patient. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-200347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Upadhyaya VD, Kumar B, Lal R, Sharma MS, Singh M. Primary duodenal tuberculosis presenting as gastric-outlet obstruction: Its diagnosis. Afr J Paediatr Surg. 2013;10:83–86. doi: 10.4103/0189-6725.115028. [DOI] [PubMed] [Google Scholar]
- 107.Fromm S, Cash JM. Superior mesenteric artery syndrome: an approach to the diagnosis and management of upper gastrointestinal obstruction of unclear etiology. S D J Med. 1990;43:5–10. [PubMed] [Google Scholar]
- 108.Harada T, Machida H, Ito S, Aihara Y, Yokota S. Henoch-Schonlein purpura presenting duodenal involvement similar to superior mesenteric artery syndrome in a girl. Eur J Pediatr. 2007;166:489–490. doi: 10.1007/s00431-006-0254-5. [DOI] [PubMed] [Google Scholar]
- 109.Harada T, Ito S, Mori M, Yokota S. Anatomical condition mimicking superior mesenteric artery syndrome might cause duodenal involvement in Henoch-Schönlein purpura. Pediatr Int. 2012;54:579. doi: 10.1111/j.1442-200X.2012.03659.x. [DOI] [PubMed] [Google Scholar]
- 110.Fujii Y, Kino M, Kimata T, Kaneko K. Abdominal pain in Henoch-Schönlein purpura and its association with superior mesenteric artery syndrome. Pediatr Int. 2012;54:313. doi: 10.1111/j.1442-200X.2012.03582.x. [DOI] [PubMed] [Google Scholar]
- 111.Lourenço LC, Martins A, Oliveira AM, Horta DV, Reis J. Wilkie Syndrome behind Crohn Disease? Superior Mesenteric Artery Syndrome Mimicking and Complicating Crohn Disease of the Upper Gastrointestinal Tract. GE Port J Gastroenterol. 2017;24:50–52. doi: 10.1159/000450873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cicero G, D'Angelo T, Bottari A, Costantino G, Visalli C, Racchiusa S, Marino MA, Cavallaro M, Frosina L, Blandino A, Mazziotti S. Superior Mesenteric Artery Syndrome in Patients with Crohn's Disease: A Description of 2 Cases Studied with a Novel Magnetic Resonance Enterography (MRE) Procedure. Am J Case Rep. 2018;19:431–437. doi: 10.12659/AJCR.908273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Verma R, Abraham DT, Joseph P, Nayak S, Agarwal S. Ectopic pancreas mimicking superior mesenteric artery syndrome. Indian J Gastroenterol. 2003;22:105–106. [PubMed] [Google Scholar]
- 114.Lambert CJ, Fitts FO Jr, Turk R. Duodenal diverticula. An unusual cause of "secondary superior mesenteric artery syndrome". Am J Surg. 1961;101:808–811. doi: 10.1016/0002-9610(61)90732-2. [DOI] [PubMed] [Google Scholar]
- 115.Goto S, Ookawara S, Sugai M. Superior mesenteric artery syndrome due to duodenal edema in a chronic renal failure patient: a case report. CEN Case Rep. 2014;3:14–17. doi: 10.1007/s13730-013-0076-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gopal M, Fisher R. A case report of B-cell lymphoma masquerading as superior mesenteric artery syndrome. J Pediatr Surg. 2007;42:1926–1927. doi: 10.1016/j.jpedsurg.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 117.Basu S, Srivastava V, Singh PK, Srivastava A, Shukla VK. Duodenojejunal junction web masquerading as Wilkie's syndrome: report of a case. Surg Today. 2011;41:409–411. doi: 10.1007/s00595-010-4258-4. [DOI] [PubMed] [Google Scholar]
- 118.Chung SC, Leung JW, Li AK. Phytobezoar masquerading as the superior mesenteric artery syndrome: successful endoscopic treatment using a colonoscope. J R Coll Surg Edinb. 1991;36:405–406. [PubMed] [Google Scholar]
- 119.Cho YP, Ahn JH, Jang HJ, Kim YH, Lee SG. Superior mesenteric artery syndrome after successful coil embolization of a ruptured pancreaticoduodenal artery aneurysm: report of a case. Surg Today. 2004;34:276–278. doi: 10.1007/s00595-003-2681-5. [DOI] [PubMed] [Google Scholar]
- 120.Shen A, Tabello D, Merchant N, Portereiko JV, Croteau A, Gates JD. Functional Superior Mesenteric Artery Syndrome Induced by an Optional IVC Filter. Case Rep Surg. 2019;2019:6543934. doi: 10.1155/2019/6543934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Blouhos K, Boulas KA, Paraskeva A, Triantafyllidis A, Kariotis I, Hatzigeorgiadis A. A misdiagnosed cause of early postoperative bowel obstruction. Clin Case Rep. 2019;7:832–833. doi: 10.1002/ccr3.2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hussain Ashraf T, Chandra A, Jauhari RK, Kumar Singh S, Noushif M. Rosai-Dorfman disease with exclusive intra-abdominal lymphadenopathy masquerading as Wilkie's syndrome. Arab J Gastroenterol. 2014;15:40–41. doi: 10.1016/j.ajg.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 123.Siddiqui MN, Ahmad T, Jaffary A. Retroperitoneal fungal abscess presenting as superior mesenteric artery syndrome. Postgrad Med J. 1996;72:433–434. doi: 10.1136/pgmj.72.849.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Reed JK, McGiin RF, Gorman JF, Thomford NR. Traumatic mesenteric arteriovenous fistula presenting as the superior mesenteric artery syndrome. Arch Surg. 1986;121:1209. doi: 10.1001/archsurg.1986.01400100121023. [DOI] [PubMed] [Google Scholar]
- 125.Moreno MA, Smith MS. Anorexia in a 14-year-old girl: why won't she eat? J Adolesc Health. 2006;39:936–938. doi: 10.1016/j.jadohealth.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 126.Jinnouchi T, Sakurai Y, Miyoshi K, Koizumi C, Waki H, Kubota N, Yamauchi T. Chronic Intestinal Pseudo-obstruction with Mitochondrial Diseases. Intern Med. 2022;61:469–474. doi: 10.2169/internalmedicine.7714-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Guthrie RH Jr. Wilkie's syndrome. Ann Surg. 1971;173:290–293. doi: 10.1097/00000658-197102000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lee TH, Lee JS, Jo Y, Park KS, Cheon JH, Kim YS, Jang JY, Kang YW. Superior mesenteric artery syndrome: where do we stand today? J Gastrointest Surg. 2012;16:2203–2211. doi: 10.1007/s11605-012-2049-5. [DOI] [PubMed] [Google Scholar]
- 129.Merrett ND, Wilson RB, Cosman P, Biankin AV. Superior mesenteric artery syndrome: diagnosis and treatment strategies. J Gastrointest Surg. 2009;13:287–292. doi: 10.1007/s11605-008-0695-4. [DOI] [PubMed] [Google Scholar]
- 130.Evarts CM, Winter RB, Hall JE. Vascular compression of the duodenum associated with the treatment of scoliosis. Review of the literature and report of eighteen cases. J Bone Joint Surg Am. 1971;53:431–44 passim. [PubMed] [Google Scholar]
- 131.Dounas GD, Cundy TP, Smith ML, Gent R, Antoniou G, Sutherland LM, Cundy PJ. The coronal aorto-mesenteric orientation theory for post-operative nausea and vomiting following scoliosis surgery in children: a pilot study. ANZ J Surg. 2021;91:174–178. doi: 10.1111/ans.16438. [DOI] [PubMed] [Google Scholar]
- 132.Khan H, Al-Jabbari E, Shroff N, Barghash M, Shestopalov A, Bhargava P. Coexistence of superior mesenteric artery syndrome and nutcracker phenomenon. Radiol Case Rep. 2022;17:1927–1930. doi: 10.1016/j.radcr.2022.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Miyata J, Eshak ES, Yoshioka T, Iso H. Movement of the superior mesenteric artery in patients with superior mesenteric artery syndrome: A case-reference study. Clin Anat. 2022;35:891–898. doi: 10.1002/ca.23885. [DOI] [PubMed] [Google Scholar]
- 134.Applegate GR, Cohen AJ. Dynamic CT in superior mesenteric artery syndrome. J Comput Assist Tomogr. 1988;12:976–980. doi: 10.1097/00004728-198811000-00013. [DOI] [PubMed] [Google Scholar]
- 135.Ahmed AR, Taylor I. Superior mesenteric artery syndrome. Postgrad Med J. 1997;73:776–778. doi: 10.1136/pgmj.73.866.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kim J, Yang S, Im YC, Park I. Superior mesenteric artery syndrome treated successfully by endoscopy-assisted jejunal feeding tube placement. BMJ Case Rep. 2021;14 doi: 10.1136/bcr-2021-245104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Shin MS, Kim JY. Optimal duration of medical treatment in superior mesenteric artery syndrome in children. J Korean Med Sci. 2013;28:1220–1225. doi: 10.3346/jkms.2013.28.8.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wan S, Zhang L, Yang J, Gao X, Wang X. Superior Mesenteric Artery Syndrome Improved by Enteral Nutritional Therapy: A Retrospective Case-Series Study in a Single Institution. Ann Nutr Metab. 2020;76:37–43. doi: 10.1159/000506620. [DOI] [PubMed] [Google Scholar]
- 139.Shiu JR, Chao HC, Luo CC, Lai MW, Kong MS, Chen SY, Chen CC, Wang CJ. Clinical and nutritional outcomes in children with idiopathic superior mesenteric artery syndrome. J Pediatr Gastroenterol Nutr. 2010;51:177–182. doi: 10.1097/MPG.0b013e3181c7bdda. [DOI] [PubMed] [Google Scholar]
- 140.Burrington JD. Vascular compression of the duodenum. Surgery. 1976;80:655. [PubMed] [Google Scholar]
- 141.Pottorf BJ, Husain FA, Hollis HW Jr, Lin E. Laparoscopic management of duodenal obstruction resulting from superior mesenteric artery syndrome. JAMA Surg. 2014;149:1319–1322. doi: 10.1001/jamasurg.2014.1409. [DOI] [PubMed] [Google Scholar]
- 142.Fredericks C, Alex G, Kumar V, Luu M. Laparoscopic Duodenojejunostomy for Superior Mesenteric Artery Syndrome. Am Surg. 2016;82:e176–e177. [PubMed] [Google Scholar]
- 143.Jain N, Chopde A, Soni B, Sharma B, Saini S, Mishra S, Gupta R, Bhojwani R. SMA syndrome: management perspective with laparoscopic duodenojejunostomy and long-term results. Surg Endosc. 2021;35:2029–2038. doi: 10.1007/s00464-020-07598-1. [DOI] [PubMed] [Google Scholar]
- 144.Bing L, Shun-Lin X, Ji-Hua O, Wei-Bing C, Ye-Bo W. Laparascopic Ladd's procedure as treatment alternative, when parenteral or prolonged hospital nutrition is not an option for superior mesenteric artery syndrome. J Pediatr Surg. 2020;55:554–557. doi: 10.1016/j.jpedsurg.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 145.STRONG EK. Mechanics of arteriomesentric duodenal obstruction and direct surgical attack upon etiology. Ann Surg. 1958;148:725–730. doi: 10.1097/00000658-195811000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kouanda A, Watson R, Binmoeller KF, Nett A, Hamerski C. EUS-guided gastroenterostomy for duodenal obstruction secondary to superior mesenteric artery syndrome. VideoGIE. 2021;6:14–15. doi: 10.1016/j.vgie.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bronswijk M, Fransen L, Vanella G, Hiele M, van der Merwe S. Successful treatment of superior mesenteric artery syndrome by endoscopic ultrasound-guided gastrojejunostomy. Endoscopy. 2021;53:204–205. doi: 10.1055/a-1190-3228. [DOI] [PubMed] [Google Scholar]
- 148.Kawabata H, Sone D, Yamaguchi K, Inoue N, Okazaki Y, Ueda Y, Hitomi M, Miyata M, Motoi S. Endoscopic Gastrojejunostomy for Superior Mesenteric Artery Syndrome Using Magnetic Compression Anastomosis. Gastroenterology Res. 2019;12:320–323. doi: 10.14740/gr1229. [DOI] [PMC free article] [PubMed] [Google Scholar]