Abstract
Background
The gut microbiota plays an important role in human health, as it can affect host immunity and susceptibility to infectious diseases. Invasive intestinal candidiasis is strongly associated with gut microbiota homeostasis. However, the nature of the interaction between Candida albicans and gut bacteria remains unclear.
Objective
This review aimed to determine the nature of interaction and the effects of gut bacteria on C. albicans so as to comprehend an approach to reducing intestinal invasive infection by C. albicans.
Methods
This review examined 11 common gut bacteria’s interactions with C. albicans, including Escherichia coli, Pseudomonas aeruginosa, Acinetobacter baumannii, Enterococcus faecalis, Staphylococcus aureus, Salmonella spp., Helicobacter pylori, Lactobacillus spp., Bacteroides spp., Clostridium difficile, and Streptococcus spp.
Results
Most of the studied bacteria demonstrated both synergistic and antagonistic effects with C. albicans, and just a few bacteria such as P. aeruginosa, Salmonella spp., and Lactobacillus spp. demonstrated only antagonism against C. albicans.
Conclusions
Based on the nature of interactions reported so far by the literature between gut bacteria and C. albicans, it is expected to provide new ideas for the prevention and treatment of invasive intestinal candidiasis.
Keywords: Candida albicans, Fungal-bacterial interactions, Gut microbiota, Polymicrobial infection
Background
Invasive candidiasis is a common fungal infection that majorly affects immunocompromised individuals and it is an important cause of death in severely ill patients [1]. It can be caused by several Candida spp., which are common commensal organisms of the skin and gut microbiota, and disruptions in the cutaneous and gastrointestinal barriers; however, the prevalence of these organisms varies considerably depending on geographical location [2]. This disease presents as an entire spectrum of diseases, ranging from fungemia to deep-seated candidiasis and to septic shock with multiorgan failure, with an associated mortality rate of > 70% [2, 3]. Clinically, the treatment of systemic fungal infections often requires large doses and long courses of antifungal drug treatments; nonetheless, the mortality rate of severe patients remains as high as 40–50% [4], which makes the treatment of invasive fungal infections a major clinical challenge. C. albicans, which colonizes the gut, is the most dominant pathogen of invasive candidiasis. In a disordered system of the intestinal microenvironment and microecology, C. albicans takes the opportunity to multiply excessively, the transition from the yeast phase to the pathogenic mycelial phase, express adhesion molecules, release C. albicans toxin, destroy the gut mucosal barrier, and invade the blood, resulting in sepsis and multiple organ insufficiency, both of which are fatal [5]. Considering that the gut microbiota is the most important line of defense to maintain the intestinal epithelial barrier and block the invasion of intestinal C. albicans [6], understanding the multiple interactions occurring between the gut bacteria and C. albicans is a very promising research field. In recent years, an increasing number of studies on the human gut microbiota have presented several discoveries, which continue to constantly refresh our understanding of this field. Several past reviews have attempted to summarize the nature of interactions between C. albicans and gut bacteria as either antagonistic or synergistic; however, several of the reported interactions are not a single pattern, rather they are both synergistic and antagonistic. Therefore, we have provided a comprehensive summary of the interactions between C. albicans and some valuable gut bacteria in an attempt to achieve better insight into the current state of research in this field as well as to develop new ideas for designing strategies toward the prevention and treatment of invasive intestinal candidiasis.
Main text
The adaptations of C. albicans in the gut
The rapid adaptation of C. albicans to the gut microenvironment is closely associated with its colonization ability. The formation of hyphae is directly associated with the virulence of C. albicans, which represents a greater destructive power; hence, it is difficult for C. albicans in its hyphal form to establish a good intestinal symbiotic homeostasis [7–11]. Thus, the filamentation of C. albicans is inhibited to colonize the gut. In this process, Efg1 plays an important role, although it is affected by hypoxia and the host’s immune status [11, 12]. In addition, C. albicans can transform itself into an opaque (a/α), grey, and gastrointestinally induced transition (GUT) cell to adapt to the changing gastrointestinal environment [8, 13, 14].
In addition to changing their phenotypes for establishing intestinal symbiotic homeostasis, C. albicans has to adapt to other gut conditions, including the carbon source problem.
Glucose is the preferred carbon source for C. albicans, but the amount of glucose varies in different parts of the gut. For example, the glucose level in the large intestine, especially the colon, is low as most of the glucose is absorbed by the small intestine before it enters the large intestine. Thus, C. albicans is often forced to use alternative carbon sources that allow it to survive at the ecological sites with or without glucose [15–19]. Moreover, C. albicans can sense amino acids through the Ssy1p-Ptr3p-Ssy5p (SPS) sensor and hydrolyze activated transcription factors Stp1 and Stp2 to utilize amino acids as a carbon source [20–23]. Rtg3 and Sfp1 can help C. albicans to adjust the utilization of lactic acid and glucose according to environmental changes [24]. Fatty acids can be used as a substitute carbon source for C. albicans through β-oxidation [25]. Moreover, because gluconeogenic and glyoxylate cycle enzymes are unaffected by ubiquitin-mediated decomposition of metabolites, both the glycolysis and gluconeogenesis pathways remain active in C. albicans, such that C. albicans can utilize multiple carbon sources simultaneously [16, 26–30]. This flexible carbon-assimilation strategy of C. albicans enhances its ability to colonize and infect mammalian hosts [27]..
While living in the gut, C. albicans often face the issue of scarce resources or excessive ingestion. To better absorb iron from the environment, C. albicans has developed a safe mechanism for iron uptake and utilization whereby it absorbs iron using several different strategies, such as acquiring RBC-derived iron and inducing the expression of high-affinity iron permease gene CaFTR1 and ferrichrome-type siderophores [31–34]. Meanwhile, to avoid toxicity caused by excessive iron, C. albicans possesses the transcription factor Sfu1 that inhibits iron uptake, various transcription factors that control iron permeability (such as plasma membrane-related Ftr1 and Ftr2 and vacuole-related Fth1 and Fth2) [34–36], and a variety of iron oxidases [36–39] .
Copper uptake is also a crucial factor. The key aspect in the copper uptake by C. albicans is ScCc2, a copper-transporting P-type ATPase that has an important role in iron transport [40]. It can express transcription factors Mac1 and Ctr1, which promote copper absorption, and can also avoid toxic effects caused by excessive copper accumulation through its unique plasma membrane structure and the activation of the copper resistance assay gene CRD1 [41–45].
In addition to iron and copper, zinc is essential for the growth and biofilm formation of C. albicans. To obtain zinc from the host, C. albicans possess a complete set of regulatory modes. Past studies have demonstrated that under the mediation of Zrt1 and Zrt2, C. albicans can obtain zinc from the host environment with the help of pH-regulated antigen 1 (Pra1), a secreted zinc scavenger (“zincophore”), and a secreted aspartic protease Sap6. The ZnT-type transporter Zrc1 then stores zinc in the vacuole [46–49]. Zrt2 also ensures zinc uptake in an acidic environment, and Zap1 regulates the zinc homeostasis in C. albicans. [47, 49].
In addition to the problem of carbon sources and trace elements, C. albicans faces pressure from the guts’ physical and chemical environment, but C. albicans can resist them through specific signaling pathways [50, 51]. For example, resistance to the osmotic pressure and oxidative stress can be promoted through the Hog1-mediated MAP kinase pathway [52–54]; the gene CAP1, which codes for a bZip transcription factor of the AP-1 family, drives transcriptional responses to oxidative stress [55–57]; Mkc1- and Cek1-mediated MAP kinase pathways promote C. albicans resistance to cell wall stress [51, 58, 59]; transcription factors Cta4 and Hsf1 respond to the intestinal nitrosation stress and heat shock [60–62]. In addition, C. albicans can produce prostaglandin PGE2 from host-derived arachidonic acid to potentiate fungal fitness by acting on the fungi themselves and/or host tissue phagocytes to improve the ability of C. albicans to evade killing by phagocytes, thereby creating more favorable conditions for colonization [63]. These stress responses are essential for the survival of C. albicans in the gut, and, if the key stress responses get inactivated, colonization and virulence of C. albicans are significantly reduced.
While C. albicans struggles to adapt to the gut environment, these adaptability changes also inevitably reshape its original virulence, invasiveness, ability to defend itself against the host’s immune system, and susceptibility to antifungal drugs. The colonization ability of this fungal strain is driven by a complex regulatory network that connects metabolism, morphogenesis, stress adaptation, and cell wall remodeling, thereby affecting its symbiotic and infection-causing ability [64]..
C. albicans and gut bacteria
C. albicans and Escherichia coli
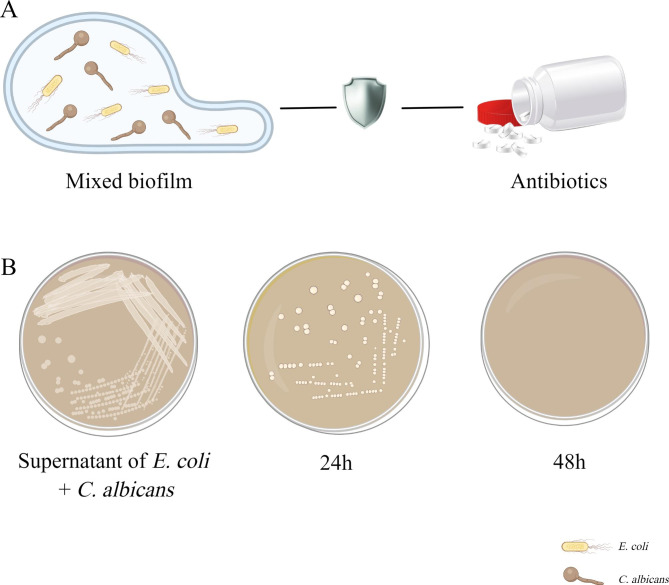
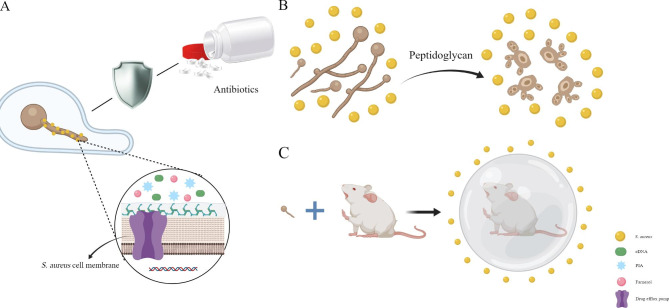
E. coli is a gram-negative bacterium and one of the major bacterial species found in the gastrointestinal tract of warm-blooded animals. This species consists of harmless, symbiotic bacterial and different pathogenic variants that can cause intestinal or extra-intestinal diseases, including diarrhea, respiratory tract infections, wound infections, and septicemia, in humans and several animal hosts [65, 66]. E. coli and C. albicans often co-exist in human tissues and body fluids. Considering that they are common symbiotic bacteria found in the mammalian gut, their interaction deserves further investigation. Past studies have demonstrated that the interaction between E. coli and C. albicans is synergistic and that their combination significantly increases the risk of mortality when compared to that of either of them individually [67, 68]. The specific mechanism underlying the increase in mortality may be associated with the regulation of biofilm formation, biofilm dispersion, hyphae growth, and antifungal sensitivity of C. albicans by E. coli [67, 69]. Past reports have suggested that, after the formation of fungal/bacterial mixed biofilm, the formation of C. albicans biofilm increased by 2.2 times [67, 69] and the spread of C. albicans increased by 2.7 times. Moreover, the sensitivity of C. albicans to nystatin decreased, and the minimum inhibitory concentration increased from 25 µg/mL to 50 µg/mL [70]. ( Fig. 1A).
Fig. 1.
The interaction between C. albicans and E. coli. (A) Mixed biofilms formed by C. albicans and E. coli are more beneficial for resistance to antibiotics. (B) The supernatant of E. coli biofilm can restrain C. albicans
However, studies on the influence of the supernatant of E. coli biofilm on the development of C. albicans biofilm demonstrated that E. coli biofilm secretions could regulate C. albicans hypha-specific genes (HSGs) expression and significantly impair its biofilm development. This secretion considerably restrained C. krusei, C. tropicalis, C. glabrata, and C. albicans biofilms at 24 h, and all Candida spp. at 48 h [71]. (Fig. 1B) In addition, Cabral et al. reported that a soluble factor secreted by E. coli can kill C. albicans in a magnesium-dependent manner [72]..
C. albicans and Pseudomonas aeruginosa
P. aeruginosa, a common gram-negative bacterium, is an important pathogenic factor that causes serious infections in humans. Owing to its natural resistance to antibiotics, an infection caused by this pathogen can result in serious clinical complications [73]. Clinically, C. albicans and P. aeruginosa are frequently isolated from various sites of the body and body fluids simultaneously, including the urine, venous ducts, the lungs of cystic fibrosis patients, and the gut [74]..
In patients with cystic fibrosis and ventilator-acquired pneumonia (VAP), the co-presence of P. aeruginosa and C. albicans is associated with a higher fatality rate [75, 76]. Colonization at the respiratory tract by C. albicans increases patients’ risk to develop a P. aeruginosa VAP [75, 77, 78]. Antifungal therapy for patients with C. albicans colonization in the tracheobronchus can reduce the risk of P. aeruginosa VAP or its colonization in the tracheobronchus [79], which, in turn, proves that C. albicans plays an important role in promoting P. aeruginosa infection. C. albicans has also been found to induce the growth of P. aeruginosa in the gut [80]..
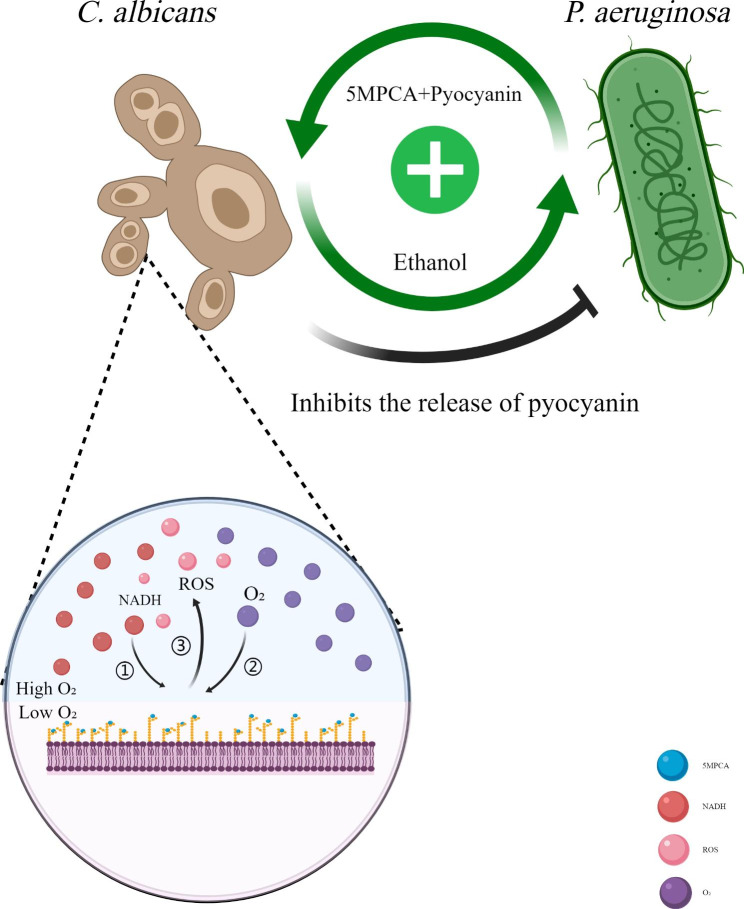
Nevertheless, the two organisms have demonstrated obvious antagonism in a bi-species environment [81]. P. aeruginosa can produce a variety of phenazines that are harmful to C. albicans, such as pyocyanin (PYO) and 5-methyl-phenazine-1-carboxylic acid (5MPCA) [82, 83]. Past researchers used the analog PMS of 5MPCA to characterize the specific antifungal machinery of 5MPCA and found that phenazines could covalently bind soluble proteins in C. albicans biofilms in vivo. As a result, these soluble proteins of C. albicans were reduced by NADH and then spontaneously oxidized by oxygen to produce reactive oxygen species (ROS) [82]. Thus, the pathway of oxygen acquisition and respiration metabolism of C. albicans biofilm were blocked. Hence, the hyphal formation, intercellular adhesion, and biofilm development of C. albicans were inhibited [83]. In addition, cell–cell signaling molecules such as 3-oxo-C12 homoserine lactone produced by P. aeruginosa can hinder the filamentation of C. albicans [84]..
Interestingly, ethanol produced by C. albicans induced by phenazines can promote P. aeruginosa to convert PCA into more phenazine final products such as PYO, phenazine-1-carboxamide, and 5MPCA. This positive feedback loop consisting of ethanol and phenazines drives a more P. aeruginosa-conducive interaction pattern between the two microbes [85]. However, for self-protection, C. albicans can reduce P. aeruginosa’ s virulence by inhibiting its release of pyochelin [86]. (Fig. 2).
Fig. 2.
The interaction between C. albicans and P. aeruginosa. P. aeruginosa can secrete phenazines such as 5MPCA and pyocyanin to block the pathway of oxygen acquisition and respiration metabolism of C. albicans. Ethanol produced by C. albicans induced by phenazines can promote P. aeruginosa to secrete more phenazines. But C. albicans can reduce P. aeruginosa’ s virulence by inhibiting its release of pyochelin
C. albicans and Acinetobacter baumannii
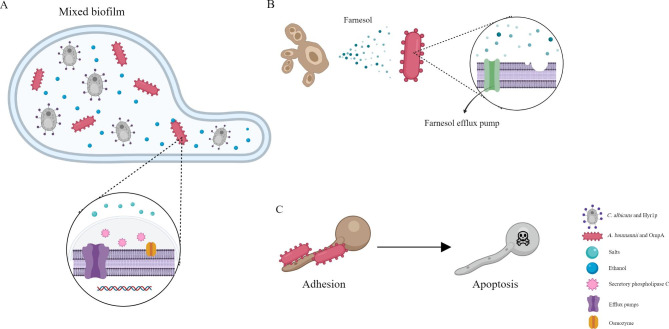
A. baumannii is certainly a very dangerous germ that can cause hospital-acquired infections (HAI) in the current healthcare systems, often causing refractory periodontitis, ventilator-associated infections and blood infections in critically ill patients. Owing to its multidrug-resistant nature, only rare antibiotics can cure infection caused by A. baumannii. Hence, the transmission of multidrug-resistant A. baumannii is worrying [87–89]. The gut, which serves as the body’s main reservoir for A. baumannii, may play an important role in the multidrug resistance of A. baumannii [90], which also arouses our curiosity about its interaction with C. albicans. Respiratory colonization of C. albicans has been reported to be an independent risk factor for A. baumannii VAP [91]. In a rat model of respiratory colonization of C. albicans, researchers found that the colonization of C. albicans made rats more prone to A. baumannii-associated pneumonia, with a higher CFU burden of A. baumannii and more severe lung damage [92]. The reason why C. albicans can make A. baumannii more likely to survive that, as a fungus, the ethanol produced by C. albicans can not only serve as a carbon source for A. baumannii but also upregulate the expression of 49 genes in A. baumannii, including genes encoding efflux pumps, secretory phospholipase C, osmozyme, and iron assimilation. In addition, ethanol can induce the high-affinity phosphate transport system of A. baumannii and help resist the toxic effects of salts [93, 94]. In addition, because of the significant structural homology between A. baumannii outer membrane protein A (OmpA) and C. albicans hyphal wall protein Hyr1p, Hyr1p can be used as a receptor for the binding of A. baumannii and C. albicans to form mixed-species biofilms [95]. ( Fig. 3A).
Fig. 3.
The interaction between C. albicans and A. baumannii. (A)C. albicans and A. baumannii can utilize the homology of Hyr1p and OmpA to form a mixed biofilm. At the same time, ethanol secreted by C. albicans can upregulate a range of genes in A. baumannii, making it more likely to survive. (B) Farnesol secreted by C. albicans can disrupt the membrane integrity of A. baumannii, but A. baumannii can use an efflux pump against it. (C)A. baumannii can attenuate the virulence of C. albicans by attaching the OmpA to C. albicans hyphae in order to induce its apoptosis
However, the interaction between C. albicans and A. baumannii is also paradoxical. It was found that the secretion of farnesol by C. albicans disrupts the membrane integrity of A. baumannii, impairs its virulence characteristics, and alters its cell morphology. However, A. baumannii can use an efflux pump against farnesol, which may work as a defense mechanism [96]. (Fig. 3B) In addition, A. baumannii can attenuate the virulence of C. albicans by inhibiting its filamentation process and attaching the outer membrane protein A (OmpA) to C. albicans hyphae in order to induce its apoptosis [97–99]. (Fig. 3C).
C. albicans and Enterococcus faecalis
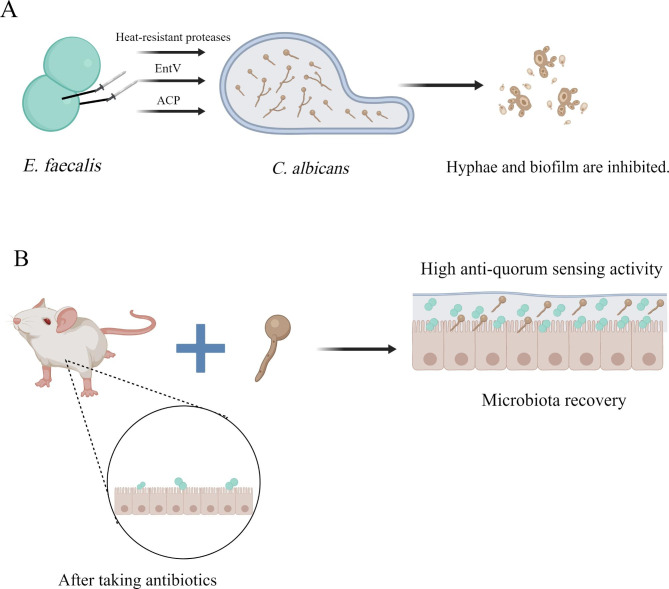
E. faecalis is a gram-positive pathogen. It is ubiquitous and can survive in various natural environments, including the human body. As an opportunistic pathogen, it colonizes the human gut surface, forms a biofilm, contributes to severe hospital infections, and shows high resistance to several antibiotics [100, 101]. Past studies have reported that E. faecalis has a protective effect against C. albicans infection. After oral administration of heat-inactivated E. faecalis to mice infected with C. albicans, E. faecalis can prevent thrush in mice by interacting directly with C. albicans in vivo and stimulating the host to enhance the immune response [102]. In a multi-microbial model of C. elegans, E. faecalis was observed to secrete heat-resistant proteases GelE and SerEin by relying on the Fsr quorum-sensing system to inhibit the hyphae morphogenesis of C. albicans, thereby negatively affecting its virulence [103]. E. faecalis can also encode EntV to block the biofilm development of C. albicans on a solid matrix and disrupt its pre-formed biofilm against the current antifungal drugs. The peptide also protects macrophages and enhances their antifungal abilities. These results suggest that EntV may be used as a potential fungal agent against C. albicans in the future [104]. Furthermore, Shekh et al. isolated and purified a non-hemolytic anti-C. albicans protein (ACP) from E. faecalis for the first time and proposed that this protein could be used to treat candidiasis in the future [105]. (Fig. 4A).
Fig. 4.
The interaction between C. albicans and E. faecalis. (A)E. faecalis can secrete EntV, ACP and heat-resistant proteases to block the biofilm development of C. albicans and inhibit its virulence. (B)C. albicans can help E. faecalis recover in antibiotic-treated gut
Although several studies have demonstrated that E. faecalis could help in the treatment of C. albicans infection, a study found that when E. faecalis and C. albicans were co-infected, a thicker, denser biofilm with stronger tolerance to harmful stresses was formed on root canal dentin and glass slides, which can increase bone resorption of osteoclasts, inhibit the bone formation of osteoblasts, upregulate inflammatory cytokines such as IL-6 and TNF-α, and ultimately increase the severity of dental pulp diseases. Moreover, past studies have reported that C. albicans can help E. faecalis become more resistant to starvation [106, 107]. Past studies using mouse models also demonstrated that the existence of C. albicans in cefoperazone-treated gut facilitated the rehabilitation of E. faecalis during antibiotic recovery [108, 109]. Meanwhile, the metabolites of carbohydrates, amino acids and polyamines in the mixed biofilm of the two changed, displaying higher anti-quorum sensing (QS) activity compared to that of a single biofilm [110]. (Fig. 4B).
C. albicans and Staphylococcus aureus
S. aureus is a clinically important pathogen that can give rise to various infections in the body, including mild skin infections, severe tissue infections, and septicemia, and it is a common reason for hospital-acquired and community-acquired infections [111]. Because S. aureus and C. albicans share several common host niches, including the gut, both are often co-isolated from mixed fungal-bacterial infections. Several studies and clinical cases have demonstrated that S. aureus and C. albicans have an infectious synergistic effect. The co-inoculation of C. albicans and S. aureus can cause more severe and extensive infection and higher mortality than the inoculation of either species alone [112–114]. Signaling pathways controlled by Efg1, a transcription factor used to induce C. albicans hyphal gene expression and hyphae growth, have been reported to be critical for C. albicans to strengthen S. aureus’s virulence in abdominal infection [115, 116]. However, C. albicans’ s ability to enhance S. aureus’s virulence in the peritoneal cavity has not been correlated with the presence or absence of the hyphae of C. albicans, suggesting that when the two microorganisms co-infect the peritoneal cavity, there may be other processes independent of morphology that are regulated by Efg1, which result in fatal synergies [117, 118].
In addition, co-infection with C. albicans and S. aureus reduces the sensitivity of S. aureus to antibiotics [113, 119]. Vancomycin has been reported to have a significant effect on the formation of a single biofilm of S. aureus, but a significantly reduced effect on mixed biofilms [119]. This effect is related to the adhesion between the two, farnesol-induced upregulation of the S. aureus drug efflux pump and increased eDNA and polysaccharide intercellular adhesin (PIA) in S. aureus biofilms, which induce the formation of network structures [120]. (Fig. 5A).
Fig. 5.
The interaction between C. albicans and S. aureus. (A)C. albicans can upregulate a range of genes that promote C. albicans to express drug efflux pumps and small molecules that help form network structures in biofilms to resist antibiotics. (B)S. aureus can secrete peptidoglycans to affect the metabolism, morphogenesis, and virulence of C. albicans. (C) Inoculating separately can induce a protective effect on the host, possibly because of the trained immunity induced by β-glucan of C. albicans
Interestingly, virulence factors and superantigen-like proteins, which play a huge role in the spread of C. albicans infection, were downregulated during co-infection, whereas the capsular polysaccharide gene was upregulated during co-infection, suggesting that C. albicans adopts a strategy that is more conducive to survival, as well as increased persistence and immune evasion of the host in cases of mixed infections [119]. The specific mechanism behind this may be that S. aureus affects the metabolism, morphogenesis, and virulence of C. albicans by producing peptidoglycans [117]. (Fig. 5B).
However, a protective effect on the host can be induced when the timing of C. albicans and S. aureus inoculation is different, possibly because of the trained immunity induced by β-glucan of C. albicans, which provides cross-protection against secondary S. aureus infection [121–126]. (Fig. 5C).
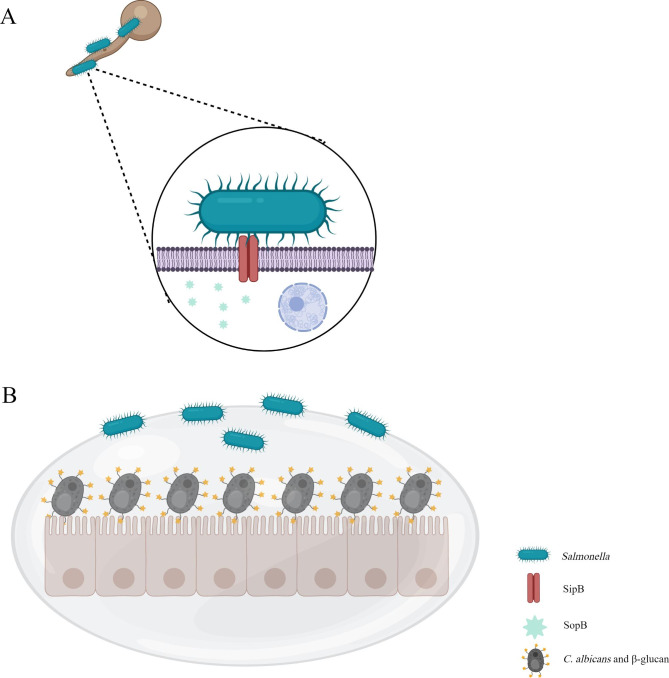
C. albicans and Salmonella
Salmonella is a gram-negative bacterium that causes gastrointestinal lesions ranging from asymptomatic carriers to gastroenteritis and typhoid fever [127, 128]. Based on the current studies, the relationship between Salmonella and C. albicans is only antagonistic. Past studies have demonstrated that when C. elegans are infected with both C. albicans and Salmonella typhimurium, the filamentation of C. albicans is hindered [129]. The underlying action mechanism is that the type III secretion systems encoded by SPI-1 and SPI-2 by Salmonella genes directly inject various effector proteins into C. albicans to exert the virulence of this species [130–132]. Among these effector proteins, the one encoded by sopB can be translocated into C. albicans hyphae through SipB to downregulates the transcription of CDC42, thereby destroying C. albicans’ s hyphae to attenuate its virulence [133]. (Fig. 6A).
Fig. 6.
The interaction between C. albicans and Salmonella. (A)Salmonella can inject SopB into C. albicans through SipB to attenuate its virulence. (B)C. albicans can use β-glucan to inhibit the colonization of S. typhimurium in the gut
Correspondingly, C. albicans can use β-glucan, an immunomodulatory substance in its cell wall, to inhibit the colonization of S. typhimurium in the gut and liver [134]. (Fig. 6B).
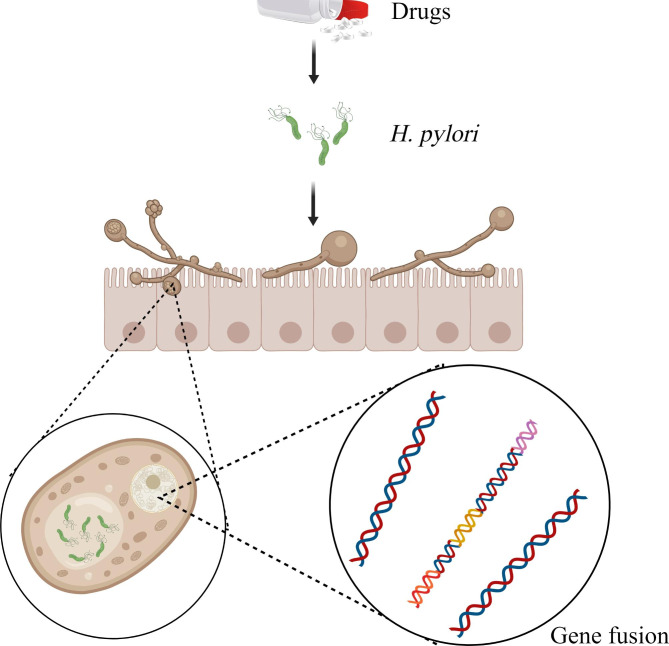
C. albicans and Helicobacter pylori
H. pylori, a gram-negative microaerobic bacterium, grows in the human gastroduodenal mucosa, causes inflammation and gastrointestinal diseases, and increases the risk of gastric cancer development [135, 136]. As a facultative intracellular bacterium, H. pylori can parasitize human gastric epithelial cells and immune cells. It has evolved to use the vacuoles of eukaryotic cells as a protective niche, which can help avoid the harsh gastric environment and produce obvious resistance to antibiotics, thereby allowing reproduction and persistence in the host for a long time [137–141]. H. pylori has been found to move and survive in the vacuole of C. albicans, suggesting that C. albicans can be used as a host and carrier by H. pylori to provide an alternative niche [142]. This is an unusual evolutionary phenomenon because the fungal cell wall typically limits endocytosis and the uptake of bacteria [143]. In this process, H. pylori can fuse its vacA s1s2, ureAB, 16 S rRNA, and ahpC genes into C. albicans DNA and create an ideal shelter for itself by taking advantage of the good tolerance of C. albicans to stress conditions, so that it can obtain nutrition, express proteins, and reproduce in C. albicans cells and continue to exist and reinfect the host [144–147].
Stress from the physicochemical environment and drugs in the gut is a powerful booster for H. pylori to enter C. albicans. A previous study showed that H. pylori, which can only adapt to fluctuations in pH in the range of 6–8, entered the cell of C. albicans, which can accept fluctuations in pH in the range of 2–10, to protect itself in an acidic environment that is not conducive to its survival; this phenomenon is more evident when the pH is lower [148]. Similarly, when H. pylori are treated with antibiotics such as amoxicillin, more numbers of H. pylori cells can be observed to enter C. albicans cells than usual, which causes treatment failure to a large extent [149]. (Fig. 7)Meantime, when H. pylori patients are older and their proton pump inhibitors (PPI) intake is higher, C. albicans’ s colonization in the human stomach gains an advantage, thus forming a positive cycle of mutual coordination [150]. On researching how H. pylori are safely released from C. albicans, some studies found that H. pylori can be released from C. albicans in the form of vesicles or free bacteria without causing damage to C. albicans [151]..
Fig. 7.
The interaction between C. albicans and H. pylori. H. pylori can be parasitic in C. albicans, especially under the pressure of drugs
This combination of pathogenic microorganisms is undoubtedly a great threat to human health, and oral and fecal-oral transmission of C. albicans also contributes to the wider spread of H. pylori. Moreover, C. albicans in the vagina is more efficient to H. pylori colonization than C. albicans in the mouth. If C. albicans is transmitted from the mother’s vagina to the mouth of the newborn, it may significantly increase the risk of H. pylori infection in the newborn [152]..
However, the relationship between H. pylori and C. albicans is not entirely mutually beneficial. Some studies have shown that the peptide HP [2–20] produced by H. pylori is highly toxic to C. albicans [153]. HP [2–20] can destroy the cell membrane structure of C. albicans or directly interact with the lipid bilayer, thereby increasing the outflow of potassium ions, reducing the intracellular trehalose content of C. albicans, and eventually exerting antifungal activities [153–156].
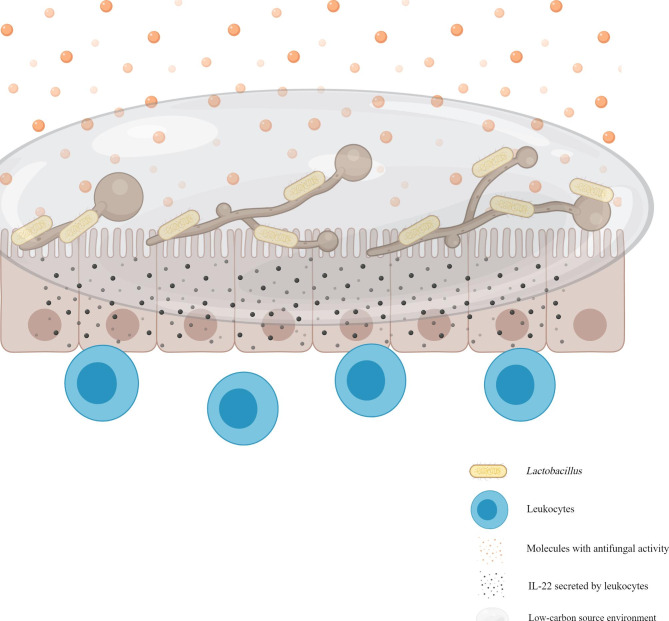
C. albicans and Lactobacillus
The genus Lactobacillus is taxonomically complex and consists of > 170 gram-positive species. Although they are a part of the normal human gastrointestinal and vaginal flora, they may act as opportunistic human pathogens [157]. They are often widely used in the preparation of various commercial products, as well as probiotics [158]. Several studies have demonstrated an obvious antagonism between Lactobacillus and C. albicans. Lactobacillus can protect against intestinal epithelial necrotizing injury caused by C. albicans [159, 160]; the supplementation of Lactobacillus and Bifidobacterium in premature and low-birth-weight infants can reduce C. albicans colonization in the gastrointestinal tract, thereby reducing the incidence of C. albicans sepsis and infant mortality [161]. Past studies have reported that the protection was time- and dose-dependent and independent of competition for the adhesion sites. This mechanism can be classified as direct physical antagonism and chemical antagonism with soluble molecules [25, 159]. In physical antagonism, Lactobacillus directly interacts with C. albicans and causes it to detach from the gut mucosa [159]. Chemical antagonism can be categorized as reshaping the metabolic environment of C. albicans (e.g., it consumes the main nutrient source of C. albicans and forces it to change its metabolic mode, thereby weakening its toxicity) and as a direct secretion of molecules with antifungal activities (e.g., lactic acid, short-chain fatty acids, hydrogen peroxide, bacteriocin-like substances, and biosurfactants) [25, 159, 162, 163]. In addition, Lactobacillus can produce indole-3-aldehyde, which acts on aryl hydrocarbon receptor (AhR) and activates leukocytes. The activation of group 3 ILCs (ILC3s) and regulatory T (Treg) cells produce a large amount of IL-22, which can hinder the colonization of C. albicans in the gut mucosa and create gut mucosal homeostasis that allows the survival of mixed microbial communities [164]. (Fig. 8) Moreover, Lactobacillus can inhibit the expression of drug efflux protein produced by drug-resistant C. albicans and reverse its drug resistance [165]..
Fig. 8.
The interaction between C. albicans and Lactobacillus. Lactobacillus can antagonize C. albicans by physical adhesion, secretion of molecules with antifungal activities, reshaping the metabolic environment and activating leukocytes in the gut
Under an appropriate conditions, C. albicans launches a counterattack against Lactobacillus. Past studies have shown that C. albicans prevented Lactobacillus regrowth in the stomach of mice treated with cefoperazone, an effect that persisted for at least 3 weeks after antibiotic treatment was discontinued, which induced stomach inflammation. However, this phenomenon can be easily suppressed. Some studies have shown that restoring the bacterial community in the stomach of mice within a week of discontinuing antibiotics was adequate to inhibit the development of gastritis [108, 109, 166].
C. albicans and Bacteroides
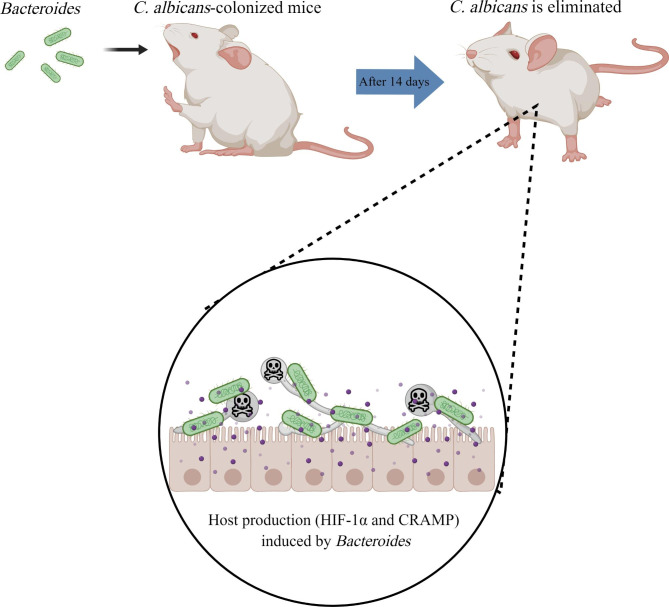
Bacteroides are clinically important pathogens that are commonly associated with most anaerobic infections, with a death rate of > 19% [167]. Bacteroides maintain a complex and beneficial relationship with their host when they remain in the gut, and their leaving this environment can induce significant pathological changes such as bacteremia and multiple abscesses all over the body [167]. Studies have found that Bacteroides can hinder C. albicans’s growth and virulence, making them the most effective bacterial group to promote the colonization resistance of C. albicans [168]. The oral administration of Bacteroides fragilis to antibiotic-treated C. albicans-colonized mice showed that C. albicans was eliminated from the gut after 14 days. During this process, host production (HIF-1α and CRAMP) induced by Bacteroides played a huge role in maintaining the colonization resistance of C. albicans [169]. As an important regulator of the mammalian innate defense, HIF-1α upregulates the expression of cathelicidin-related antimicrobial peptides (CRAMP) in the bone marrow cells, which play a key role in mammalian natural immune defense against bacterial infection. The human cathelicidin LL-37 has been demonstrated to possess anti-C. albicans ability to hinder C. albicans adhesion to the epithelium by preferentially binding to the components of C. albicans cell wall such as mannan, chitin, and dextran [170–173]. (Fig. 9).
Fig. 9.
The interaction between C. albicans and Bacteroides. Bacteroides can induce host production to promote the eliminated of C. albicans from the gut in antibiotic-treated C. albicans-colonized mice
Although these studies demonstrated that Bacteroides are almost lethal for C. albicans, the mucin produced by Bacteroides thetaiotaomicron has been found to promote the growth of C. albicans [174]. In addition, in the cecum of cefoperazone-treated mice, the existence of C. albicans facilitated the rehabilitation of Bacteroides during cefoperazone treatment [109, 166]. A possible mechanism for this is that C. albicans provides a hypoxic microenvironment for Bacteroides through aerobic respiration and produces antioxidants to promote its growth [175, 176].
C. albicans and Clostridium difficile
C. difficile, an anaerobic toxin-producing bacterium, is the main reason behind hospital-acquired infections. Multiple surface proteins and flagella allow C. difficile to colonize the gut, where it can cause gut diseases ranging from mild diarrhea to deadly infectious colitis, leading to significant morbidity and mortality worldwide [177, 178]. Fecal microbiota transplant (FMT) treatment in C. difficile infections (CDI) model mice demonstrated that the existence of C. albicans reduced the efficacy of FMT, whereas antifungal therapy restored the efficacy, indicating that C. albicans promotes C. difficile’s survival [179]. The underlying mechanism behind this may be that the existence of C. albicans creates an anoxic microenvironment for C. difficile, which allows C. difficile to continue to grow under aerobic conditions [175, 180]. Meanwhile, higher C. albicans infection rates have been reported in CDI patients, suggesting that C. difficile may promote the colonization of C. albicans [179, 181].
However, similar to Bacteroides species, C. difficile is the key to maintaining resistance to the colonization of C. albicans in the mice gut [169]. Past studies have demonstrated that taurocholate acid (TCA) can promote the colonization and transmission of C. albicans in the gastrointestinal tract by significantly reducing the abundance of C. difficile, which indirectly indicates that C. difficile plays a certain antagonistic role in the gastrointestinal tract against C. albicans [182]. In addition to activating HIF-1α and inducing CRAMP expression similar to Bacteroides for reducing gut colonization and post-infection mortality associated with C. albicans, C. difficile can produce para-cresol, a bacteriostatic compound that can alter the morphology, inhibit biofilm formation, and antagonize the growth of C. albicans via tyrosine fermentation [169, 180, 183].
C. albicans and Streptococcus
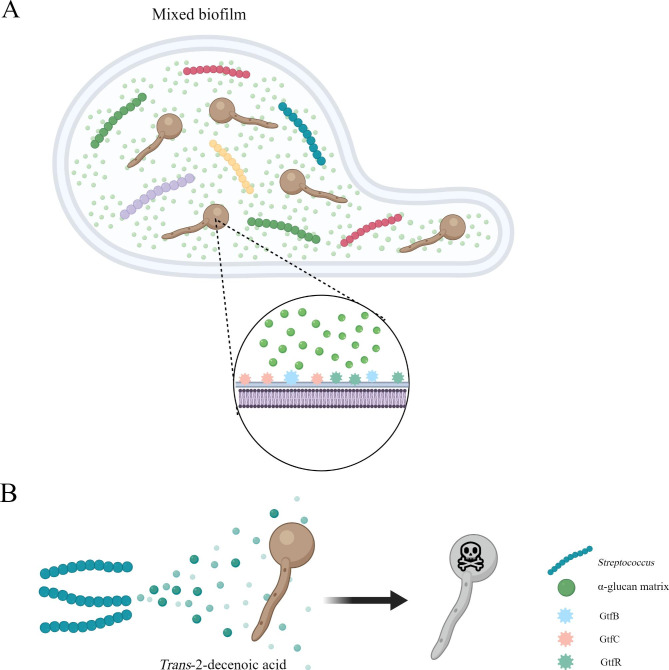
Streptococcus is a common gram-positive coccus, consisting of 104 strains, which mainly cause otitis media, pneumonia, bacteremia, and meningitis. When Streptococcus colonizes the digestive tract, it can cause diseases in the digestive system [184]. Because of their niche preference, Streptococcus and C. albicans mainly coexist in the human mouth. Presently, most studies on the interaction between Streptococcus and C. albicans are related to oral diseases. However, both microorganisms can be found and extracted from the gut as well. Because Streptococcus is composed of a complex variety of strains, the interactions and mechanisms between different Streptococcus types and C. albicans are different. Several Streptococcus strains have been confirmed to co-aggregate with C. albicans such as S. sanguis, S. gordonii, S. mutans, S. oralis, and S. anginosus [185]. Among them, S. mutans has been reported to form synergies with C. albicans. In early childhood caries, there occurs a cross-feeding mechanism between these two microorganisms, which is mediated by the glucotransferase GtfB secreted by S. mutans. GtfB can bind to mannan on the outer surface of the C. albicans cell wall to produce a large number of the α-glucan matrix into the mixed biofilm, which not only promotes the formation of mixed biofilms and provides enhanced binding sites for the two microorganisms but also improves the utilization of carbohydrates by C. albicans, thereby increasing the severity of the disease [186–189]. GtfC and GtfR play a role similar to that of GtfB in the interaction between the two microorganisms [190–192]. (Fig. 10 A) In addition, the antigen I/II of S. mutans can mediate the increase in the number of C. albicans and the production of acids in the mixed biofilm [193]. In the process of interaction, C. albicans promotes the growth of S. mutans by secreting farnesol and polysaccharides [188, 194]. In addition to S. mutans, another representative Streptococcus strain that can form a synergistic effect with C. albicans is S. gordonii, which promotes biofilm formation, filamentation, and adhesion of C. albicans. The formation of dual-species biofilm also shows a high degree of resistance to combined antifungal and antibacterial treatment [195–198]. The key to this interaction is the glucosyltransferase GtfG [199]. In addition, C. albicans can promote the growth and metabolism of S. gordonii by increasing the activity of S. gordonii cell-wall-anchored glycoside hydrolases [200]..
Fig. 10.
The interaction between C. albicans and Streptococcus. (A) After C. albicans and Streptococcus form a mixed biofilm, Streptococcus induces C. albicans to produce a large amount of α-glucan by secreting glucotransferases. (B)Trans-2-decenoic acid secreted by Streptococcus inhibits C. albicans’s virulence
However, the interaction between Streptococcus strains and C. albicans is also not a single synergy. Several Streptococcus strains mentioned above can secrete trans-2-decenoic acid to terminate the expression of HWP1 associated with the formation of C. albicans hyphae, thereby inhibiting its virulence [201]. (Fig. 10B)Another Streptococcus, S. gordonii, has been found to secrete competence-stimulating-peptide (CSP), which hinders C. albicans’s biofilm-formation [201]..
Conclusions
The colonization of C. albicans in the gut is a complex process that requires suppression of its filamentation and transformation into other cell types. In addition, C. albicans is required to adapt to the metabolic environment of the gut, resolve the carbon source problem as well as the intake and discharge balance of other micronutrients. Under the intestinal physical and chemical environmental pressures, the responses of C. albicans created by various signal pathways can determine its capacity to colonize the gut.
After colonizing the gut, the interactions between C. albicans and the gut bacteria become a significant part of the host’s health. With the continuous emergence of new findings, our understanding of the interactions between C. albicans and various gut bacteria continues to deepen. In general, the nature of the interactions of microbes can be classified into 5 broad categories: direct physical contact, chemical interaction by small secreting molecules involved in quorum sensing, alterations in host’s immune response, competition for carbon sources, and parasitism.
Among all the bacteria studied in this review, P. aeruginosa, Lactobacillus spp. and Salmonella spp. exhibit only antagonism against C. albicans, indicating that they are promising as the key to the treatment of C. albicans in the future [202]. Meanwhile, for bacteria that can secrete small molecules that antagonize C. albicans, purifying these secretions (e.g., soluble factors secreted by E. coli; phenazines and 3-oxo-C12 homoserine lactone secreted by P. aeruginosa; OmpA of A. baumannii; GelE, SerEin, EntV, and ACP secreted by E. faecalis; HP protein secreted by H. pylori; para-cresol secreted by C. difficile; trans-2-decenoic acid and CSP secreted by Streptococcus spp.) and using them to antagonize C. albicans is also a very promising approach. In addition, we can selectively knock out the synergistic genes of bacteria and introduce the mutant strains into the body, such as by knocking out the genes expressing various glucosyltransferases in Streptococcus spp. and only using its antagonism to C. albicans.
Nevertheless, several difficulties are encountered in the implementation of these treatment methods, such as the requirements of technical expertise in purifying small molecules, the dosage of small purified molecules to treatment, whether the harmful genes among the opportunistic pathogenic bacteria can be completely knocked out, and whether knocking out these bacterial genes have potential risks implications to the host health. All these aspects need to be constantly explored in practice. The synergistic effect of C. albicans and bacteria reveals that it is important to treat bacterial infections while treating C. albicans infection. We can apply their synergy to the treatment of mixed microbial infections. For example, owing to the homologous nature of Hyr1p of C. albicans and OmpA of A. baumannii, active immunization using rHyr1p-N or passive immunization using polyclonal antibodies against specific peptide motifs of rHyr1p-N provides new ideas for the future treatment for both C. albicans and A. baumannii [95]; Treatment of C. albicans is very beneficial in the treatment of H. pylori.
However, researches on the interactions between C. albicans and gut bacteria are still lacking. First, in the current studies, there are some conflicting observations, wherein the specific mechanisms are unknown. For example, although C. albicans can increase S. aureus’s resistance to antibiotics by secreting farnesol, this happens only when the concentration of farnesol is low. If the concentration of farnesol is high, its effect on S. aureus is opposite [203–205]. Second, most in vivo experiments were conducted using mouse, nematode, and fruit fly models, and not human ones. Finally, very little research has been conducted on the direct interactions of several bacteria with C. albicans in the gut.
Therefore, more number of researches on the human gut is necessary to understand, more deeply and comprehensively, the mechanisms of interactions between C. albicans and gut bacteria. In the future, mutant strains with deletions of specific gene fragments, vaccines, or purified biomacromolecules could serve as essential alternatives in the prevention and treatment of invasive intestinal candidiasis.
Figure lengends.
Acknowledgements
Not applicable.
List of abbreviations
- GUT
Gastrointestinally induced transition
- SPS
Ssy1p-Ptr3p-Ssy5p
- HSGs
Hypha-specific genes
- VAP
Ventilator-acquired pneumonia
- HAI
Hospital-acquired infections
- OmpA
Outer membrane protein A
- ACP
Anti-C. albicans protein
- QS
Quorum sensing
- PIA
Polysaccharide intercellular adhesin
- PPI
Proton pump inhibitors
- AhR
Aryl hydrocarbon receptor
- ILC3s
Group 3 ILCs
- Treg
Regulatory T
- CRAMP
Cathelicidin-related antimicrobial peptides
- FMT
Fecal microbiota transplant
- CDI
C. difficile infections
- TCA
Taurocholate acidbile acid
- CSP
Competence-stimulating-peptide
- 5MPCA
5-methyl-phenazine-1-carboxylic acid
- PYO
Pyocyanin
Authors’ contributions
Fei Wang was the main contributor to thein writing of the manuscript. Zetian Wang was responsible for the collection and collation of reference articles and participated in the writing of the manuscript. Jianguo Tang made great contributions to the subsequent revision and improvement work. The authorAuthor order was determined on the basis of seniority. All authors read and approved the final manuscript.
Funding
Not applicable.
Data Availability
Not applicable.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zetian Wang, Email: 18321127738@163.com.
Jianguo Tang, Email: tangjianguo@5thhospital.com.
References
- 1.Jenks JD, Cornely OA, Chen SC, Thompson GR 3rd, Hoenigl M. Breakthrough invasive fungal infections: who is at risk? Mycoses. 2020;63(10):1021–32. [DOI] [PubMed]
- 2.Pappas PG, Lionakis MS, Arendrup MC, Ostrosky-Zeichner L, Kullberg BJ. Invasive candidiasis. Nat Rev Dis Primers. 2018;4:18026. doi: 10.1038/nrdp.2018.26. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Lara MF, Ostrosky-Zeichner L. Invasive candidiasis. Semin Respir Crit Care Med. 2020;41(1):3–12. doi: 10.1055/s-0040-1701215. [DOI] [PubMed] [Google Scholar]
- 4.Tso GHW, Reales-Calderon JA, Pavelka N. The elusive Anti-Candida Vaccine: Lessons from the Past and Opportunities for the future. Front Immunol. 2018;9:897. doi: 10.3389/fimmu.2018.00897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhong L, Zhang S, Tang K, Zhou F, Zheng C, Zhang K, et al. Clinical characteristics, risk factors and outcomes of mixed Candida albicans/bacterial bloodstream infections. BMC Infect Dis. 2020;20(1):810. doi: 10.1186/s12879-020-05536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fusco A, Savio V, Donniacuo M, Perfetto B, Donnarumma G. Antimicrobial peptides human Beta-Defensin-2 and – 3 protect the Gut during Candida albicans Infections enhancing the Intestinal Barrier Integrity: in Vitro Study. Front Cell Infect Microbiol. 2021;11:666900. doi: 10.3389/fcimb.2021.666900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai JV, Lionakis MS. Setting up home: fungal rules of Commensalism in the mammalian gut. Cell Host Microbe. 2019;25(3):347–9. doi: 10.1016/j.chom.2019.02.012. [DOI] [PubMed] [Google Scholar]
- 8.Noble SM, Gianetti BA, Witchley JN. Candida albicans cell-type switching and functional plasticity in the mammalian host. Nat Rev Microbiol. 2017;15(2):96–108. doi: 10.1038/nrmicro.2016.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tso GHW, Reales-Calderon JA, Tan ASM, Sem X, Le GTT, Tan TG, et al. Experimental evolution of a fungal pathogen into a gut symbiont. Science. 2018;362(6414):589–95. doi: 10.1126/science.aat0537. [DOI] [PubMed] [Google Scholar]
- 10.Witchley JN, Penumetcha P, Abon NV, Woolford CA, Mitchell AP, Noble SM. Candida albicans morphogenesis Programs Control the balance between gut commensalism and invasive infection. Cell Host Microbe. 2019;25(3):432–43e6. doi: 10.1016/j.chom.2019.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Desai PR, van Wijlick L, Kurtz D, Juchimiuk M, Ernst JF. Hypoxia and temperature regulated morphogenesis in Candida albicans. PLoS Genet. 2015;11(8):e1005447. doi: 10.1371/journal.pgen.1005447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pierce JV, Kumamoto CA. Variation in Candida albicans EFG1 expression enables host-dependent changes in colonizing fungal populations. mBio. 2012;3(4):e00117–12. doi: 10.1128/mBio.00117-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pande K, Chen C, Noble SM. Passage through the mammalian gut triggers a phenotypic switch that promotes Candida albicans commensalism. Nat Genet. 2013;45(9):1088–91. doi: 10.1038/ng.2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prieto D, Román E, Alonso-Monge R, Pla J. Overexpression of the Transcriptional Regulator WOR1 increases susceptibility to bile salts and adhesion to the mouse gut mucosa in Candida albicans. Front Cell Infect Microbiol. 2017;7:389. doi: 10.3389/fcimb.2017.00389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Avican K, Fahlgren A, Huss M, Heroven AK, Beckstette M, Dersch P, et al. Reprogramming of Yersinia from virulent to persistent mode revealed by complex in vivo RNA-seq analysis. PLoS Pathog. 2015;11(1):e1004600. doi: 10.1371/journal.ppat.1004600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barelle CJ, Priest CL, Maccallum DM, Gow NA, Odds FC, Brown AJ. Niche-specific regulation of central metabolic pathways in a fungal pathogen. Cell Microbiol. 2006;8(6):961–71. doi: 10.1111/j.1462-5822.2005.00676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hube B. From commensal to pathogen: stage- and tissue-specific gene expression of Candida albicans. Curr Opin Microbiol. 2004;7(4):336–41. doi: 10.1016/j.mib.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 18.Kröger C, Colgan A, Srikumar S, Händler K, Sivasankaran SK, Hammarlöf DL, et al. An infection-relevant transcriptomic compendium for Salmonella enterica Serovar Typhimurium. Cell Host Microbe. 2013;14(6):683–95. doi: 10.1016/j.chom.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Miramón P, Dunker C, Windecker H, Bohovych IM, Brown AJ, Kurzai O, et al. Cellular responses of Candida albicans to phagocytosis and the extracellular activities of neutrophils are critical to counteract carbohydrate starvation, oxidative and nitrosative stress. PLoS ONE. 2012;7(12):e52850. doi: 10.1371/journal.pone.0052850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martínez P, Ljungdahl PO. An ER packaging chaperone determines the amino acid uptake capacity and virulence of Candida albicans. Mol Microbiol. 2004;51(2):371–84. doi: 10.1046/j.1365-2958.2003.03845.x. [DOI] [PubMed] [Google Scholar]
- 21.Martínez P, Ljungdahl PO. Divergence of Stp1 and Stp2 transcription factors in Candida albicans places virulence factors required for proper nutrient acquisition under amino acid control. Mol Cell Biol. 2005;25(21):9435–46. doi: 10.1128/MCB.25.21.9435-9446.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Priest SJ, Lorenz MC. Characterization of virulence-related phenotypes in Candida Species of the CUG Clade. Eukaryot Cell. 2015;14(9):931–40. doi: 10.1128/EC.00062-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vylkova S, Carman AJ, Danhof HA, Collette JR, Zhou H, Lorenz MC. The fungal pathogen Candida albicans autoinduces hyphal morphogenesis by raising extracellular pH. mBio. 2011;2(3):e00055–11. doi: 10.1128/mBio.00055-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kastora SL, Herrero-de-Dios C, Avelar GM, Munro CA, Brown AJP. Sfp1 and Rtg3 reciprocally modulate carbon source-conditional stress adaptation in the pathogenic yeast Candida albicans. Mol Microbiol. 2017;105(4):620–36. doi: 10.1111/mmi.13722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alonso-Roman R, Last A, Mirhakkak MH, Sprague JL, Möller L, Großmann P, et al. Lactobacillus rhamnosus colonisation antagonizes Candida albicans by forcing metabolic adaptations that compromise pathogenicity. Nat Commun. 2022;13(1):3192. doi: 10.1038/s41467-022-30661-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andes D, Lepak A, Pitula A, Marchillo K, Clark J. A simple approach for estimating gene expression in Candida albicans directly from a systemic infection site. J Infect Dis. 2005;192(5):893–900. doi: 10.1086/432104. [DOI] [PubMed] [Google Scholar]
- 27.Childers DS, Raziunaite I, Mol Avelar G, Mackie J, Budge S, Stead D, et al. The rewiring of ubiquitination targets in a pathogenic yeast promotes metabolic flexibility, host colonization and virulence. PLoS Pathog. 2016;12(4):e1005566. doi: 10.1371/journal.ppat.1005566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fradin C, De Groot P, MacCallum D, Schaller M, Klis F, Odds FC, et al. Granulocytes govern the transcriptional response, morphology and proliferation of Candida albicans in human blood. Mol Microbiol. 2005;56(2):397–415. doi: 10.1111/j.1365-2958.2005.04557.x. [DOI] [PubMed] [Google Scholar]
- 29.Rosenbach A, Dignard D, Pierce JV, Whiteway M, Kumamoto CA. Adaptations of Candida albicans for growth in the mammalian intestinal tract. Eukaryot Cell. 2010;9(7):1075–86. doi: 10.1128/EC.00034-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walker LA, Munro CA, de Bruijn I, Lenardon MD, McKinnon A, Gow NA. Stimulation of chitin synthesis rescues Candida albicans from echinocandins. PLoS Pathog. 2008;4(4):e1000040. doi: 10.1371/journal.ppat.1000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heymann P, Gerads M, Schaller M, Dromer F, Winkelmann G, Ernst JF. The siderophore iron transporter of Candida albicans (Sit1p/Arn1p) mediates uptake of ferrichrome-type siderophores and is required for epithelial invasion. Infect Immun. 2002;70(9):5246–55. doi: 10.1128/IAI.70.9.5246-5255.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lesuisse E, Knight SA, Camadro JM, Dancis A. Siderophore uptake by Candida albicans: effect of serum treatment and comparison with Saccharomyces cerevisiae. Yeast. 2002;19(4):329–40. doi: 10.1002/yea.840. [DOI] [PubMed] [Google Scholar]
- 33.Moors MA, Stull TL, Blank KJ, Buckley HR, Mosser DM. A role for complement receptor-like molecules in iron acquisition by Candida albicans. J Exp Med. 1992;175(6):1643–51. doi: 10.1084/jem.175.6.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ramanan N, Wang Y. A high-affinity iron permease essential for Candida albicans virulence. Science. 2000;288(5468):1062–4. doi: 10.1126/science.288.5468.1062. [DOI] [PubMed] [Google Scholar]
- 35.Chen C, Pande K, French SD, Tuch BB, Noble SM. An iron homeostasis regulatory circuit with reciprocal roles in Candida albicans commensalism and pathogenesis. Cell Host Microbe. 2011;10(2):118–35. doi: 10.1016/j.chom.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mamouei Z, Zeng G, Wang YM, Wang Y. Candida albicans possess a highly versatile and dynamic high-affinity iron transport system important for its commensal-pathogenic lifestyle. Mol Microbiol. 2017;106(6):986–98. doi: 10.1111/mmi.13864. [DOI] [PubMed] [Google Scholar]
- 37.Eck R, Hundt S, Härtl A, Roemer E, Künkel W. A multicopper oxidase gene from Candida albicans: cloning, characterization and disruption. Microbiol (Reading) 1999;145(Pt 9):2415–22. doi: 10.1099/00221287-145-9-2415. [DOI] [PubMed] [Google Scholar]
- 38.Knight SAB, Lesuisse E, Stearman R, Klausner RD, Dancis A. Reductive iron uptake by Candida albicans: role of copper, iron and the TUP1 regulator. Microbiol (Reading) 2002;148(Pt 1):29–40. doi: 10.1099/00221287-148-1-29. [DOI] [PubMed] [Google Scholar]
- 39.Ziegler L, Terzulli A, Gaur R, McCarthy R, Kosman DJ. Functional characterization of the ferroxidase, permease high-affinity iron transport complex from Candida albicans. Mol Microbiol. 2011;81(2):473–85. doi: 10.1111/j.1365-2958.2011.07704.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weissman Z, Shemer R, Kornitzer D. Deletion of the copper transporter CaCCC2 reveals two distinct pathways for iron acquisition in Candida albicans. Mol Microbiol. 2002;44(6):1551–60. doi: 10.1046/j.1365-2958.2002.02976.x. [DOI] [PubMed] [Google Scholar]
- 41.Marvin ME, Mason RP, Cashmore AM. The CaCTR1 gene is required for high-affinity iron uptake and is transcriptionally controlled by a copper-sensing transactivator encoded by CaMAC1. Microbiol (Reading) 2004;150(Pt 7):2197–208. doi: 10.1099/mic.0.27004-0. [DOI] [PubMed] [Google Scholar]
- 42.Marvin ME, Williams PH, Cashmore AM. The Candida albicans CTR1 gene encodes a functional copper transporter. Microbiol (Reading) 2003;149(Pt 6):1461–74. doi: 10.1099/mic.0.26172-0. [DOI] [PubMed] [Google Scholar]
- 43.Riggle PJ, Kumamoto CA. Role of a Candida albicans P1-type ATPase in resistance to copper and silver ion toxicity. J Bacteriol. 2000;182(17):4899–905. doi: 10.1128/JB.182.17.4899-4905.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weissman Z, Berdicevsky I, Cavari BZ, Kornitzer D. The high copper tolerance of Candida albicans is mediated by a P-type ATPase. Proc Natl Acad Sci U S A. 2000;97(7):3520–5. doi: 10.1073/pnas.97.7.3520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Douglas LM, Konopka JB. Plasma membrane architecture protects Candida albicans from killing by copper. PLoS Genet. 2019;15(1):e1007911. doi: 10.1371/journal.pgen.1007911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Citiulo F, Jacobsen ID, Miramón P, Schild L, Brunke S, Zipfel P, et al. Candida albicans scavenges host zinc via Pra1 during endothelial invasion. PLoS Pathog. 2012;8(6):e1002777. doi: 10.1371/journal.ppat.1002777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim MJ, Kil M, Jung JH, Kim J. Roles of zinc-responsive transcription factor Csr1 in filamentous growth of the pathogenic yeast Candida albicans. J Microbiol Biotechnol. 2008;18(2):242–7. doi: 10.4014/jmb.1610.10050. [DOI] [PubMed] [Google Scholar]
- 48.Kumar R, Breindel C, Saraswat D, Cullen PJ, Edgerton M. Candida albicans Sap6 amyloid regions function in cellular aggregation and zinc binding, and contribute to zinc acquisition. Sci Rep. 2017;7(1):2908. doi: 10.1038/s41598-017-03082-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Crawford AC, Lehtovirta-Morley LE, Alamir O, Niemiec MJ, Alawfi B, Alsarraf M, et al. Biphasic zinc compartmentalisation in a human fungal pathogen. PLoS Pathog. 2018;14(5):e1007013. doi: 10.1371/journal.ppat.1007013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.de Dios CH, Román E, Monge RA, Pla J. The role of MAPK signal transduction pathways in the response to oxidative stress in the fungal pathogen Candida albicans: implications in virulence. Curr Protein Pept Sci. 2010;11(8):693–703. doi: 10.2174/138920310794557655. [DOI] [PubMed] [Google Scholar]
- 51.Monge RA, Román E, Nombela C, Pla J. The MAP kinase signal transduction network in Candida albicans. Microbiol (Reading) 2006;152(Pt 4):905–12. doi: 10.1099/mic.0.28616-0. [DOI] [PubMed] [Google Scholar]
- 52.Alonso-Monge R, Navarro-García F, Román E, Negredo AI, Eisman B, Nombela C, et al. The Hog1 mitogen-activated protein kinase is essential in the oxidative stress response and chlamydospore formation in Candida albicans. Eukaryot Cell. 2003;2(2):351–61. doi: 10.1128/EC.2.2.351-361.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.San José C, Monge RA, Pérez-Díaz R, Pla J, Nombela C. The mitogen-activated protein kinase homolog HOG1 gene controls glycerol accumulation in the pathogenic fungus Candida albicans. J Bacteriol. 1996;178(19):5850–2. doi: 10.1128/jb.178.19.5850-5852.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith DA, Nicholls S, Morgan BA, Brown AJ, Quinn J. A conserved stress-activated protein kinase regulates a core stress response in the human pathogen Candida albicans. Mol Biol Cell. 2004;15(9):4179–90. doi: 10.1091/mbc.e04-03-0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Alarco AM, Raymond M. The bZip transcription factor Cap1p is involved in multidrug resistance and oxidative stress response in Candida albicans. J Bacteriol. 1999;181(3):700–8. doi: 10.1128/JB.181.3.700-708.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kos I, Patterson MJ, Znaidi S, Kaloriti D, da Silva Dantas A, Herrero-de-Dios CM, et al. Mechanisms underlying the delayed activation of the Cap1 transcription factor in Candida albicans following combinatorial oxidative and cationic stress important for phagocytic potency. mBio. 2016;7(2):e00331. doi: 10.1128/mBio.00331-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Znaidi S, Barker KS, Weber S, Alarco AM, Liu TT, Boucher G, et al. Identification of the Candida albicans Cap1p regulon. Eukaryot Cell. 2009;8(6):806–20. doi: 10.1128/EC.00002-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Eisman B, Alonso-Monge R, Román E, Arana D, Nombela C, Pla J. The Cek1 and Hog1 mitogen-activated protein kinases play complementary roles in cell wall biogenesis and chlamydospore formation in the fungal pathogen Candida albicans. Eukaryot Cell. 2006;5(2):347–58. doi: 10.1128/EC.5.2.347-358.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Navarro-García F, Sánchez M, Pla J, Nombela C. Functional characterization of the MKC1 gene of Candida albicans, which encodes a mitogen-activated protein kinase homolog related to cell integrity. Mol Cell Biol. 1995;15(4):2197–206. doi: 10.1128/MCB.15.4.2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chiranand W, McLeod I, Zhou H, Lynn JJ, Vega LA, Myers H, et al. CTA4 transcription factor mediates induction of nitrosative stress response in Candida albicans. Eukaryot Cell. 2008;7(2):268–78. doi: 10.1128/EC.00240-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hromatka BS, Noble SM, Johnson AD. Transcriptional response of Candida albicans to nitric oxide and the role of the YHB1 gene in nitrosative stress and virulence. Mol Biol Cell. 2005;16(10):4814–26. doi: 10.1091/mbc.e05-05-0435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nicholls S, Leach MD, Priest CL, Brown AJ. Role of the heat shock transcription factor, Hsf1, in a major fungal pathogen that is obligately associated with warm-blooded animals. Mol Microbiol. 2009;74(4):844–61. doi: 10.1111/j.1365-2958.2009.06883.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tan TG, Lim YS, Tan A, Leong R, Pavelka N. Fungal symbionts produce prostaglandin E(2) to promote their intestinal colonization. Front Cell Infect Microbiol. 2019;9:359. doi: 10.3389/fcimb.2019.00359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brown AJ, Brown GD, Netea MG, Gow NA. Metabolism impacts upon Candida immunogenicity and pathogenicity at multiple levels. Trends Microbiol. 2014;22(11):614–22. doi: 10.1016/j.tim.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leimbach A, Hacker J, Dobrindt U. E. coli as an all-rounder: the thin line between commensalism and pathogenicity. Curr Top Microbiol Immunol. 2013;358:3–32. doi: 10.1007/82_2012_303. [DOI] [PubMed] [Google Scholar]
- 66.Tenaillon O, Skurnik D, Picard B, Denamur E. The population genetics of commensal Escherichia coli. Nat Rev Microbiol. 2010;8(3):207–17. doi: 10.1038/nrmicro2298. [DOI] [PubMed] [Google Scholar]
- 67.Farrokhi Y, Al-Shibli B, Al-Hameedawi DF, Neshati Z, Makhdoumi A. Escherichia coli enhances the virulence factors of Candida albicans, the cause of vulvovaginal candidiasis, in a dual bacterial/fungal biofilm. Res Microbiol. 2021;172(4–5):103849. doi: 10.1016/j.resmic.2021.103849. [DOI] [PubMed] [Google Scholar]
- 68.Klaerner HG, Uknis ME, Acton RD, Dahlberg PS, Carlone-Jambor C, Dunn DL. Candida albicans and Escherichia coli are synergistic pathogens during experimental microbial peritonitis. J Surg Res. 1997;70(2):161–5. doi: 10.1006/jsre.1997.5110. [DOI] [PubMed] [Google Scholar]
- 69.Bandara H, Yau JYY, Watt RM, Jin LJ, Samaranayake LP. Escherichia coli and its lipopolysaccharide modulate in vitro Candida biofilm formation. J Med Microbiol. 2009;58(Pt 12):1623–31. doi: 10.1099/jmm.0.012989-0. [DOI] [PubMed] [Google Scholar]
- 70.. !!! INVALID CITATION !!! (63)(65).
- 71.Bandara HM, Cheung BP, Watt RM, Jin LJ, Samaranayake LP. Secretory products of Escherichia coli biofilm modulate Candida biofilm formation and hyphal development. J Investig Clin Dent. 2013;4(3):186–99. doi: 10.1111/jicd.12048. [DOI] [PubMed] [Google Scholar]
- 72.Cabral DJ, Penumutchu S, Norris C, Morones-Ramirez JR, Belenky P. Microbial competition between Escherichia coli and Candida albicans reveals a soluble fungicidal factor. Microb Cell. 2018;5(5):249–55. doi: 10.15698/mic2018.05.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mielko KA, Jabłoński SJ, Milczewska J, Sands D, Łukaszewicz M, Młynarz P. Metabolomic studies of Pseudomonas aeruginosa. World J Microbiol Biotechnol. 2019;35(11):178. doi: 10.1007/s11274-019-2739-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kasetty S, Mould DL, Hogan DA, Nadell CD. Both Pseudomonas aeruginosa and Candida albicans Accumulate Greater Biomass in Dual-Species Biofilms under Flow. mSphere. 2021;6(3):e0041621. doi: 10.1128/mSphere.00416-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hamet M, Pavon A, Dalle F, Pechinot A, Prin S, Quenot JP, et al. Candida spp. airway colonization could promote antibiotic-resistant bacteria selection in patients with suspected ventilator-associated pneumonia. Intensive Care Med. 2012;38(8):1272–9. doi: 10.1007/s00134-012-2584-2. [DOI] [PubMed] [Google Scholar]
- 76.Navarro J, Rainisio M, Harms HK, Hodson ME, Koch C, Mastella G, et al. Factors associated with poor pulmonary function: cross-sectional analysis of data from the ERCF. European epidemiologic Registry of cystic fibrosis. Eur Respir J. 2001;18(2):298–305. doi: 10.1183/09031936.01.00068901. [DOI] [PubMed] [Google Scholar]
- 77.Azoulay E, Timsit JF, Tafflet M, de Lassence A, Darmon M, Zahar JR, et al. Candida colonization of the respiratory tract and subsequent pseudomonas ventilator-associated pneumonia. Chest. 2006;129(1):110–7. doi: 10.1378/chest.129.1.110. [DOI] [PubMed] [Google Scholar]
- 78.Roux D, Gaudry S, Dreyfuss D, El-Benna J, de Prost N, Denamur E, et al. Candida albicans impairs macrophage function and facilitates Pseudomonas aeruginosa pneumonia in rat. Crit Care Med. 2009;37(3):1062–7. doi: 10.1097/CCM.0b013e31819629d2. [DOI] [PubMed] [Google Scholar]
- 79.Nseir S, Jozefowicz E, Cavestri B, Sendid B, Di Pompeo C, Dewavrin F, et al. Impact of antifungal treatment on Candida-Pseudomonas interaction: a preliminary retrospective case-control study. Intensive Care Med. 2007;33(1):137–42. doi: 10.1007/s00134-006-0422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hiengrach P, Panpetch W, Worasilchai N, Chindamporn A, Tumwasorn S, Jaroonwitchawan T, et al. Administration of Candida Albicans to dextran sulfate solution treated mice causes intestinal dysbiosis, emergence and dissemination of Intestinal Pseudomonas Aeruginosa and Lethal Sepsis. Shock. 2020;53(2):189–98. doi: 10.1097/SHK.0000000000001339. [DOI] [PubMed] [Google Scholar]
- 81.Keçeli Özcan S, Dündar D, Sönmez TG. [Anti-candidal activity of clinical Pseudomonas aeruginosa strains and in vitro inhibition of Candida biofilm formation] Mikrobiyol Bul. 2012;46(1):39–46. [PubMed] [Google Scholar]
- 82.Morales DK, Jacobs NJ, Rajamani S, Krishnamurthy M, Cubillos-Ruiz JR, Hogan DA. Antifungal mechanisms by which a novel Pseudomonas aeruginosa phenazine toxin kills Candida albicans in biofilms. Mol Microbiol. 2010;78(6):1379–92. doi: 10.1111/j.1365-2958.2010.07414.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Morales DK, Grahl N, Okegbe C, Dietrich LE, Jacobs NJ, Hogan DA. Control of Candida albicans metabolism and biofilm formation by Pseudomonas aeruginosa phenazines. mBio. 2013;4(1):e00526–12. doi: 10.1128/mBio.00526-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hogan DA, Vik A, Kolter R. A Pseudomonas aeruginosa quorum-sensing molecule influences Candida albicans morphology. Mol Microbiol. 2004;54(5):1212–23. doi: 10.1111/j.1365-2958.2004.04349.x. [DOI] [PubMed] [Google Scholar]
- 85.Chen AI, Dolben EF, Okegbe C, Harty CE, Golub Y, Thao S, et al. Candida albicans ethanol stimulates Pseudomonas aeruginosa WspR-controlled biofilm formation as part of a cyclic relationship involving phenazines. PLoS Pathog. 2014;10(10):e1004480. doi: 10.1371/journal.ppat.1004480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lopez-Medina E, Fan D, Coughlin LA, Ho EX, Lamont IL, Reimmann C, et al. Candida albicans inhibits Pseudomonas aeruginosa Virulence through suppression of pyochelin and pyoverdine biosynthesis. PLoS Pathog. 2015;11(8):e1005129. doi: 10.1371/journal.ppat.1005129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Harding CM, Hennon SW, Feldman MF. Uncovering the mechanisms of Acinetobacter baumannii virulence. Nat Rev Microbiol. 2018;16(2):91–102. doi: 10.1038/nrmicro.2017.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lee CR, Lee JH, Park M, Park KS, Bae IK, Kim YB, et al. Biology of Acinetobacter baumannii: Pathogenesis, Antibiotic Resistance Mechanisms, and prospective treatment options. Front Cell Infect Microbiol. 2017;7:55. doi: 10.3389/fcimb.2017.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Richards AM, Abu Kwaik Y, Lamont RJ. Code blue: Acinetobacter baumannii, a nosocomial pathogen with a role in the oral cavity. Mol Oral Microbiol. 2015;30(1):2–15. doi: 10.1111/omi.12072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ketter PM, Yu JJ, Guentzel MN, May HC, Gupta R, Eppinger M et al. Acinetobacter baumannii Gastrointestinal colonization is facilitated by secretory IgA which is reductively dissociated by bacterial thioredoxin A. mBio. 2018;9(4). [DOI] [PMC free article] [PubMed]
- 91.Tan X, Zhu S, Yan D, Chen W, Chen R, Zou J, et al. Candida spp. airway colonization: a potential risk factor for Acinetobacter baumannii ventilator-associated pneumonia. Med Mycol. 2016;54(6):557–66. doi: 10.1093/mmy/myw009. [DOI] [PubMed] [Google Scholar]
- 92.Tan X, Chen R, Zhu S, Wang H, Yan D, Zhang X, et al. Candida albicans Airway colonization facilitates subsequent Acinetobacter baumannii Pneumonia in a rat model. Antimicrob Agents Chemother. 2016;60(6):3348–54. doi: 10.1128/AAC.02180-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Smith MG, Des Etages SG, Snyder M. Microbial synergy via an ethanol-triggered pathway. Mol Cell Biol. 2004;24(9):3874–84. doi: 10.1128/MCB.24.9.3874-3884.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Camarena L, Bruno V, Euskirchen G, Poggio S, Snyder M. Molecular mechanisms of ethanol-induced pathogenesis revealed by RNA-sequencing. PLoS Pathog. 2010;6(4):e1000834. doi: 10.1371/journal.ppat.1000834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Uppuluri P, Lin L, Alqarihi A, Luo G, Youssef EG, Alkhazraji S, et al. The Hyr1 protein from the fungus Candida albicans is a cross kingdom immunotherapeutic target for Acinetobacter bacterial infection. PLoS Pathog. 2018;14(5):e1007056. doi: 10.1371/journal.ppat.1007056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kostoulias X, Murray GL, Cerqueira GM, Kong JB, Bantun F, Mylonakis E, et al. Impact of a Cross-Kingdom Signaling Molecule of Candida albicans on Acinetobacter baumannii Physiology. Antimicrob Agents Chemother. 2016;60(1):161–7. doi: 10.1128/AAC.01540-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Peleg AY, Tampakakis E, Fuchs BB, Eliopoulos GM, Moellering RC, Jr, Mylonakis E. Prokaryote-eukaryote interactions identified by using Caenorhabditis elegans. Proc Natl Acad Sci U S A. 2008;105(38):14585–90. doi: 10.1073/pnas.0805048105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gaddy JA, Tomaras AP, Actis LA. The Acinetobacter baumannii 19606 OmpA protein plays a role in biofilm formation on abiotic surfaces and in the interaction of this pathogen with eukaryotic cells. Infect Immun. 2009;77(8):3150–60. doi: 10.1128/IAI.00096-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.. !!! INVALID CITATION !!!.
- 100.Oh HK, Hwang YJ, Hong HW, Myung H. Comparison of Enterococcus faecalis Biofilm removal efficiency among bacteriophage PBEF129, its Endolysin, and Cefotaxime. Viruses. 2021;13(3). [DOI] [PMC free article] [PubMed]
- 101.Reffuveille F, Leneveu C, Chevalier S, Auffray Y, Rincé A. Lipoproteins of Enterococcus faecalis: bioinformatic identification, expression analysis and relation to virulence. Microbiol (Reading) 2011;157(Pt 11):3001–13. doi: 10.1099/mic.0.053314-0. [DOI] [PubMed] [Google Scholar]
- 102.Ishijima SA, Hayama K, Ninomiya K, Iwasa M, Yamazaki M, Abe S. Protection of mice from oral candidiasis by heat-killed enterococcus faecalis, possibly through its direct binding to Candida albicans. Med Mycol J. 2014;55(1):E9–e19. doi: 10.3314/mmj.55.E9. [DOI] [PubMed] [Google Scholar]
- 103.Cruz MR, Graham CE, Gagliano BC, Lorenz MC, Garsin DA. Enterococcus faecalis inhibits hyphal morphogenesis and virulence of Candida albicans. Infect Immun. 2013;81(1):189–200. doi: 10.1128/IAI.00914-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Graham CE, Cruz MR, Garsin DA, Lorenz MC. Enterococcus faecalis bacteriocin EntV inhibits hyphal morphogenesis, biofilm formation, and virulence of Candida albicans. Proc Natl Acad Sci U S A. 2017;114(17):4507–12. doi: 10.1073/pnas.1620432114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shekh RM, Roy U. Biochemical characterization of an anti-candida factor produced by Enterococcus faecalis. BMC Microbiol. 2012;12:132. doi: 10.1186/1471-2180-12-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Du Q, Yuan S, Zhao S, Fu D, Chen Y, Zhou Y, et al. Coexistence of Candida albicans and Enterococcus faecalis increases biofilm virulence and periapical lesions in rats. Biofouling. 2021;37(9–10):964–74. doi: 10.1080/08927014.2021.1993836. [DOI] [PubMed] [Google Scholar]
- 107.Gao Y, Jiang X, Lin D, Chen Y, Tong Z. The Starvation Resistance and Biofilm formation of Enterococcus faecalis in coexistence with Candida albicans, Streptococcus gordonii, Actinomyces viscosus, or Lactobacillus acidophilus. J Endod. 2016;42(8):1233–8. doi: 10.1016/j.joen.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 108.Mason KL, Erb Downward JR, Falkowski NR, Young VB, Kao JY, Huffnagle GB. Interplay between the gastric bacterial microbiota and Candida albicans during postantibiotic recolonization and gastritis. Infect Immun. 2012;80(1):150–8. doi: 10.1128/IAI.05162-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mason KL, Erb Downward JR, Mason KD, Falkowski NR, Eaton KA, Kao JY, et al. Candida albicans and bacterial microbiota interactions in the cecum during recolonization following broad-spectrum antibiotic therapy. Infect Immun. 2012;80(10):3371–80. doi: 10.1128/IAI.00449-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kart D, Yabanoğlu Çiftçi S, Nemutlu E. Metabolomics-driven approaches on interactions between Enterococcus faecalis and Candida albicans Biofilms. Turk J Pharm Sci. 2021;18(5):557–64. doi: 10.4274/tjps.galenos.2021.71235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ahmad-Mansour N, Loubet P, Pouget C, Dunyach-Remy C, Sotto A, Lavigne JP et al. Staphylococcus aureus Toxins: an update on their pathogenic Properties and potential treatments. Toxins (Basel). 2021;13(10). [DOI] [PMC free article] [PubMed]
- 112.Peters BM, Noverr MC. Candida albicans-Staphylococcus aureus polymicrobial peritonitis modulates host innate immunity. Infect Immun. 2013;81(6):2178–89. doi: 10.1128/IAI.00265-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Scheres N, Krom BP. Staphylococcus-Candida Interaction Models: antibiotic resistance testing and host interactions. Methods Mol Biol. 2016;1356:153–61. doi: 10.1007/978-1-4939-3052-4_11. [DOI] [PubMed] [Google Scholar]
- 114.Todd OA, Fidel PL Jr, Harro JM, Hilliard JJ, Tkaczyk C, Sellman BR et al. Candida albicans augments Staphylococcus aureus Virulence by engaging the staphylococcal agr Quorum Sensing System. mBio. 2019;10(3). [DOI] [PMC free article] [PubMed]
- 115.Lo HJ, Köhler JR, DiDomenico B, Loebenberg D, Cacciapuoti A, Fink GR. Nonfilamentous C. albicans mutants are avirulent. Cell. 1997;90(5):939–49. doi: 10.1016/S0092-8674(00)80358-X. [DOI] [PubMed] [Google Scholar]
- 116.Nash EE, Peters BM, Fidel PL, Noverr MC. Morphology-independent virulence of Candida Species during Polymicrobial intra-abdominal infections with Staphylococcus aureus. Infect Immun. 2016;84(1):90–8. doi: 10.1128/IAI.01059-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Eichelberger KR, Cassat JE. Metabolic Adaptations during Staphylococcus aureus and Candida albicans Co-Infection. Front Immunol. 2021;12:797550. doi: 10.3389/fimmu.2021.797550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nash EE, Peters BM, Palmer GE, Fidel PL, Noverr MC. Morphogenesis is not required for Candida albicans-Staphylococcus aureus intra-abdominal infection-mediated dissemination and lethal sepsis. Infect Immun. 2014;82(8):3426–35. doi: 10.1128/IAI.01746-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vila T, Kong EF, Montelongo-Jauregui D, Van Dijck P, Shetty AC, McCracken C, et al. Therapeutic implications of C. albicans-S. aureus mixed biofilm in a murine subcutaneous catheter model of polymicrobial infection. Virulence. 2021;12(1):835–51. doi: 10.1080/21505594.2021.1894834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kong EF, Tsui C, Kucharíková S, Van Dijck P, Jabra-Rizk MA. Modulation of Staphylococcus aureus Response to Antimicrobials by the Candida albicans Quorum sensing Molecule Farnesol. Antimicrob Agents Chemother. 2017;61(12). [DOI] [PMC free article] [PubMed]
- 121.Bistoni F, Vecchiarelli A, Cenci E, Puccetti P, Marconi P, Cassone A. Evidence for macrophage-mediated protection against lethal Candida albicans infection. Infect Immun. 1986;51(2):668–74. doi: 10.1128/iai.51.2.668-674.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cheng SC, Quintin J, Cramer RA, Shepardson KM, Saeed S, Kumar V, et al. mTOR- and HIF-1α-mediated aerobic glycolysis as metabolic basis for trained immunity. Science. 2014;345(6204):1250684. doi: 10.1126/science.1250684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Di Luzio NR, Williams DL. Protective effect of glucan against systemic Staphylococcus aureus septicemia in normal and leukemic mice. Infect Immun. 1978;20(3):804–10. doi: 10.1128/iai.20.3.804-810.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Netea MG, Domínguez-Andrés J, Barreiro LB, Chavakis T, Divangahi M, Fuchs E, et al. Defining trained immunity and its role in health and disease. Nat Rev Immunol. 2020;20(6):375–88. doi: 10.1038/s41577-020-0285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Netea MG, Quintin J, van der Meer JW. Trained immunity: a memory for innate host defense. Cell Host Microbe. 2011;9(5):355–61. doi: 10.1016/j.chom.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 126.Quintin J, Saeed S, Martens JHA, Giamarellos-Bourboulis EJ, Ifrim DC, Logie C, et al. Candida albicans infection affords protection against reinfection via functional reprogramming of monocytes. Cell Host Microbe. 2012;12(2):223–32. doi: 10.1016/j.chom.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hurley D, McCusker MP, Fanning S, Martins M. Salmonella-host interactions - modulation of the host innate immune system. Front Immunol. 2014;5:481. doi: 10.3389/fimmu.2014.00481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Petersen E, Miller SI. The cellular microbiology of Salmonellae interactions with macrophages. Cell Microbiol. 2019;21(11):e13116. doi: 10.1111/cmi.13116. [DOI] [PubMed] [Google Scholar]
- 129.Tampakakis E, Peleg AY, Mylonakis E. Interaction of Candida albicans with an intestinal pathogen, Salmonella enterica serovar typhimurium. Eukaryot Cell. 2009;8(5):732–7. doi: 10.1128/EC.00016-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ly KT, Casanova JE. Mechanisms of Salmonella entry into host cells. Cell Microbiol. 2007;9(9):2103–11. doi: 10.1111/j.1462-5822.2007.00992.x. [DOI] [PubMed] [Google Scholar]
- 131.McGhie EJ, Brawn LC, Hume PJ, Humphreys D, Koronakis V. Salmonella takes control: effector-driven manipulation of the host. Curr Opin Microbiol. 2009;12(1):117–24. doi: 10.1016/j.mib.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhou D, Galán J. Salmonella entry into host cells: the work in concert of type III secreted effector proteins. Microbes Infect. 2001;3(14–15):1293–8. doi: 10.1016/S1286-4579(01)01489-7. [DOI] [PubMed] [Google Scholar]
- 133.. !!! INVALID CITATION !!! (127)(132).
- 134.Winarsih S, Kosasih T, Putera MA, Rahmadhiani N, Poernomo EL, Runtuk KS, et al. β-Glucan of Candida albicans Cell Wall Extract inhibits Salmonella Typhimurium colonization by potentiating Cellular immunity (CD8 + and CD4 + T cells) Rev Soc Bras Med Trop. 2019;52:e20180254. doi: 10.1590/0037-8682-0254-2018. [DOI] [PubMed] [Google Scholar]
- 135.Correa P. Gastric cancer: overview. Gastroenterol Clin North Am. 2013;42(2):211–7. doi: 10.1016/j.gtc.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gu H. Role of Flagella in the pathogenesis of Helicobacter pylori. Curr Microbiol. 2017;74(7):863–9. doi: 10.1007/s00284-017-1256-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chu YT, Wang YH, Wu JJ, Lei HY. Invasion and multiplication of Helicobacter pylori in gastric epithelial cells and implications for antibiotic resistance. Infect Immun. 2010;78(10):4157–65. doi: 10.1128/IAI.00524-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Dubois A, Borén T. Helicobacter pylori is invasive and it may be a facultative intracellular organism. Cell Microbiol. 2007;9(5):1108–16. doi: 10.1111/j.1462-5822.2007.00921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Petersen AM, Krogfelt KA. Helicobacter pylori: an invading microorganism? A review. FEMS Immunol Med Microbiol. 2003;36(3):117–26. doi: 10.1016/S0928-8244(03)00020-8. [DOI] [PubMed] [Google Scholar]
- 140.Wang YH, Gorvel JP, Chu YT, Wu JJ, Lei HY. Helicobacter pylori impairs murine dendritic cell responses to infection. PLoS ONE. 2010;5(5):e10844. doi: 10.1371/journal.pone.0010844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wang YH, Wu JJ, Lei HY. The autophagic induction in Helicobacter pylori-infected macrophage. Exp Biol Med (Maywood) 2009;234(2):171–80. doi: 10.3181/0808-RM-252. [DOI] [PubMed] [Google Scholar]
- 142.Siavoshi F, Salmanian AH, Akbari F, Malekzadeh R, Massarrat S. Detection of Helicobacter pylori-specific genes in the oral yeast. Helicobacter. 2005;10(4):318–22. doi: 10.1111/j.1523-5378.2005.00319.x. [DOI] [PubMed] [Google Scholar]
- 143.Gehrig H, Schüssler A, Kluge M. Geosiphon pyriforme, a fungus forming endocytobiosis with Nostoc (cyanobacteria), is an ancestral member of the Glomales: evidence by SSU rRNA analysis. J Mol Evol. 1996;43(1):71–81. doi: 10.1007/BF02352301. [DOI] [PubMed] [Google Scholar]
- 144.Salmanian AH, Siavoshi F, Akbari F, Afshari A, Malekzadeh R. Yeast of the oral cavity is the reservoir of Heliobacter pylori. J Oral Pathol Med. 2008;37(6):324–8. doi: 10.1111/j.1600-0714.2007.00632.x. [DOI] [PubMed] [Google Scholar]
- 145.Saniee P, Siavoshi F, Nikbakht Broujeni G, Khormali M, Sarrafnejad A, Malekzadeh R. Localization of H.pylori within the vacuole of Candida yeast by direct immunofluorescence technique. Arch Iran Med. 2013;16(12):705–10. [PubMed] [Google Scholar]
- 146.Saniee P, Siavoshi F, Nikbakht Broujeni G, Khormali M, Sarrafnejad A, Malekzadeh R. Immunodetection of Helicobacter pylori-specific proteins in oral and gastric Candida yeasts. Arch Iran Med. 2013;16(11):624–30. [PubMed] [Google Scholar]
- 147.Siavoshi F, Saniee P. Vacuoles of Candida yeast as a specialized niche for Helicobacter pylori. World J Gastroenterol. 2014;20(18):5263–73. doi: 10.3748/wjg.v20.i18.5263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sánchez-Alonzo K, Parra-Sepúlveda C, Vega S, Bernasconi H, Campos VL, Smith CT et al. In Vitro Incorporation of Helicobacter pylori into Candida albicans caused by acidic pH stress. Pathogens. 2020;9(6). [DOI] [PMC free article] [PubMed]
- 149.Sánchez-Alonzo K, Belmar L, Parra-Sepúlveda C, Bernasconi H, Campos VL, Smith CT et al. Antibiotics as a stressing factor triggering the harboring of Helicobacter pylori J99 within Candida albicans ATCC10231. Pathogens. 2021;10(3). [DOI] [PMC free article] [PubMed]
- 150.Massarrat S, Saniee P, Siavoshi F, Mokhtari R, Mansour-Ghanaei F, Khalili-Samani S. The Effect of Helicobacter pylori infection, aging, and consumption of Proton Pump inhibitor on fungal colonization in the stomach of dyspeptic patients. Front Microbiol. 2016;7:801. doi: 10.3389/fmicb.2016.00801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Heydari S, Siavoshi F, Jazayeri MH, Sarrafnejad A, Saniee P. Helicobacter pylori release from yeast as a vesicle-encased or free bacterium. Helicobacter. 2020;25(5):e12725. doi: 10.1111/hel.12725. [DOI] [PubMed] [Google Scholar]
- 152.Siavoshi F, Taghikhani A, Malekzadeh R, Sarrafnejad A, Kashanian M, Jamal AS, et al. The role of mother’s oral and vaginal yeasts in transmission of Helicobacter pylori to neonates. Arch Iran Med. 2013;16(5):288–94. [PubMed] [Google Scholar]
- 153.Lee DG, Kim PI, Park Y, Jang SH, Park SC, Woo ER, et al. HP (2–20) derived from the amino terminal region of helicobacterpylori ribosomal protein L1 exerts its antifungal effects by damaging the plasma membranes of Candida albicans. J Pept Sci. 2002;8(8):453–60. doi: 10.1002/psc.405. [DOI] [PubMed] [Google Scholar]
- 154.Lee DG, Park Y, Kim HN, Kim HK, Kim PI, Choi BH, et al. Antifungal mechanism of an antimicrobial peptide, HP (2–20), derived from N-terminus of Helicobacter pylori ribosomal protein L1 against Candida albicans. Biochem Biophys Res Commun. 2002;291(4):1006–13. doi: 10.1006/bbrc.2002.6548. [DOI] [PubMed] [Google Scholar]
- 155.Lee DG, Park Y, Kim PI, Jeong HG, Woo ER, Hahm KS. Influence on the plasma membrane of Candida albicans by HP (2–9)-magainin 2 (1–12) hybrid peptide. Biochem Biophys Res Commun. 2002;297(4):885–9. doi: 10.1016/S0006-291X(02)02230-1. [DOI] [PubMed] [Google Scholar]
- 156.Park Y, Lee DG, Hahm KS. HP(2–9)-magainin 2(1–12), a synthetic hybrid peptide, exerts its antifungal effect on Candida albicans by damaging the plasma membrane. J Pept Sci. 2004;10(4):204–9. doi: 10.1002/psc.489. [DOI] [PubMed] [Google Scholar]
- 157.Rossi F, Amadoro C, Colavita G. Members of the Lactobacillus Genus Complex (LGC) as opportunistic pathogens: a review. Microorganisms. 2019;7(5). [DOI] [PMC free article] [PubMed]
- 158.Goldstein EJ, Tyrrell KL, Citron DM. Lactobacillus species: taxonomic complexity and controversial susceptibilities. Clin Infect Dis. 2015;60(Suppl 2):98–107. doi: 10.1093/cid/civ072. [DOI] [PubMed] [Google Scholar]
- 159.Graf K, Last A, Gratz R, Allert S, Linde S, Westermann M et al. Keeping Candida commensal: how lactobacilli antagonize pathogenicity of Candida albicans in an in vitro gut model. Dis Model Mech. 2019;12(9). [DOI] [PMC free article] [PubMed]
- 160.Panpetch W, Hiengrach P, Nilgate S, Tumwasorn S, Somboonna N, Wilantho A, et al. Additional Candida albicans administration enhances the severity of dextran sulfate solution induced colitis mouse model through leaky gut-enhanced systemic inflammation and gut-dysbiosis but attenuated by Lactobacillus rhamnosus L34. Gut Microbes. 2020;11(3):465–80. doi: 10.1080/19490976.2019.1662712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Roy A, Chaudhuri J, Sarkar D, Ghosh P, Chakraborty S. Role of enteric supplementation of Probiotics on late-onset Sepsis by Candida species in Preterm Low Birth Weight Neonates: a Randomized, double blind, placebo-controlled trial. N Am J Med Sci. 2014;6(1):50–7. doi: 10.4103/1947-2714.125870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Boris S, Barbés C. Role played by lactobacilli in controlling the population of vaginal pathogens. Microbes Infect. 2000;2(5):543–6. doi: 10.1016/S1286-4579(00)00313-0. [DOI] [PubMed] [Google Scholar]
- 163.Noverr MC, Huffnagle GB. Regulation of Candida albicans morphogenesis by fatty acid metabolites. Infect Immun. 2004;72(11):6206–10. doi: 10.1128/IAI.72.11.6206-6210.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zelante T, Iannitti RG, Cunha C, De Luca A, Giovannini G, Pieraccini G, et al. Tryptophan catabolites from microbiota engage aryl hydrocarbon receptor and balance mucosal reactivity via interleukin-22. Immunity. 2013;39(2):372–85. doi: 10.1016/j.immuni.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 165.Dube Y, Khan A, Marimani M, Ahmad A. Lactobacillus rhamnosus cell-free extract targets virulence and antifungal drug resistance in Candida albicans. Can J Microbiol. 2020;66(12):733–47. doi: 10.1139/cjm-2019-0491. [DOI] [PubMed] [Google Scholar]
- 166.Erb Downward JR, Falkowski NR, Mason KL, Muraglia R, Huffnagle GB. Modulation of post-antibiotic bacterial community reassembly and host response by Candida albicans. Sci Rep. 2013;3:2191. doi: 10.1038/srep02191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wexler HM. Bacteroides: the good, the bad, and the nitty-gritty. Clin Microbiol Rev. 2007;20(4):593–621. doi: 10.1128/CMR.00008-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.García C, Tebbji F, Daigneault M, Liu NN, Köhler JR, Allen-Vercoe E et al. The human gut Microbial Metabolome modulates fungal growth via the TOR Signaling Pathway. mSphere. 2017;2(6). [DOI] [PMC free article] [PubMed]
- 169.Fan D, Coughlin LA, Neubauer MM, Kim J, Kim MS, Zhan X, et al. Activation of HIF-1α and LL-37 by commensal bacteria inhibits Candida albicans colonization. Nat Med. 2015;21(7):808–14. doi: 10.1038/nm.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.López-García B, Lee PH, Yamasaki K, Gallo RL. Anti-fungal activity of cathelicidins and their potential role in Candida albicans skin infection. J Invest Dermatol. 2005;125(1):108–15. doi: 10.1111/j.0022-202X.2005.23713.x. [DOI] [PubMed] [Google Scholar]
- 171.Nizet V, Johnson RS. Interdependence of hypoxic and innate immune responses. Nat Rev Immunol. 2009;9(9):609–17. doi: 10.1038/nri2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Peyssonnaux C, Datta V, Cramer T, Doedens A, Theodorakis EA, Gallo RL, et al. HIF-1alpha expression regulates the bactericidal capacity of phagocytes. J Clin Invest. 2005;115(7):1806–15. doi: 10.1172/JCI23865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Tsai PW, Yang CY, Chang HT, Lan CY. Human antimicrobial peptide LL-37 inhibits adhesion of Candida albicans by interacting with yeast cell-wall carbohydrates. PLoS ONE. 2011;6(3):e17755. doi: 10.1371/journal.pone.0017755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Eckstein MT, Moreno-Velásquez SD, Pérez JC. Gut Bacteria shape intestinal Microhabitats occupied by the Fungus Candida albicans. Curr Biol. 2020;30(23):4799–807e4. doi: 10.1016/j.cub.2020.09.027. [DOI] [PubMed] [Google Scholar]
- 175.Fox EP, Cowley ES, Nobile CJ, Hartooni N, Newman DK, Johnson AD. Anaerobic bacteria grow within Candida albicans biofilms and induce biofilm formation in suspension cultures. Curr Biol. 2014;24(20):2411–6. doi: 10.1016/j.cub.2014.08.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Valentine M, Benadé E, Mouton M, Khan W, Botha A. Binary interactions between the yeast Candida albicans and two gut-associated Bacteroides species. Microb Pathog. 2019;135:103619. doi: 10.1016/j.micpath.2019.103619. [DOI] [PubMed] [Google Scholar]
- 177.Anjuwon-Foster BR, Tamayo R. Phase variation of Clostridium difficile virulence factors. Gut Microbes. 2018;9(1):76–83. doi: 10.1080/19490976.2017.1362526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Burke KE, Lamont JT. Clostridium difficile infection: a worldwide disease. Gut Liver. 2014;8(1):1–6. doi: 10.5009/gnl.2014.8.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zuo T, Wong SH, Cheung CP, Lam K, Lui R, Cheung K, et al. Gut fungal dysbiosis correlates with reduced efficacy of fecal microbiota transplantation in Clostridium difficile infection. Nat Commun. 2018;9(1):3663. doi: 10.1038/s41467-018-06103-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.van Leeuwen PT, van der Peet JM, Bikker FJ, Hoogenkamp MA, Oliveira Paiva AM, Kostidis S et al. Interspecies interactions between Clostridium difficile and Candida albicans. mSphere. 2016;1(6). [DOI] [PMC free article] [PubMed]
- 181.Raponi G, Visconti V, Brunetti G, Ghezzi MC. Clostridium difficile infection and Candida colonization of the gut: is there a correlation? Clin Infect Dis. 2014;59(11):1648–9. doi: 10.1093/cid/ciu637. [DOI] [PubMed] [Google Scholar]
- 182.Thangamani S, Monasky R, Lee JK, Antharam V, HogenEsch H, Hazbun TR et al. Bile acid regulates the colonization and dissemination of Candida albicans from the gastrointestinal tract by Controlling host Defense System and Microbiota. J Fungi (Basel). 2021;7(12). [DOI] [PMC free article] [PubMed]
- 183.Passmore IJ, Letertre MPM, Preston MD, Bianconi I, Harrison MA, Nasher F, et al. Para-cresol production by Clostridium difficile affects microbial diversity and membrane integrity of Gram-negative bacteria. PLoS Pathog. 2018;14(9):e1007191. doi: 10.1371/journal.ppat.1007191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Andam CP, Hanage WP. Mechanisms of genome evolution of Streptococcus. Infect Genet Evol. 2015;33:334–42. doi: 10.1016/j.meegid.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Jenkinson HF, Lala HC, Shepherd MG. Coaggregation of Streptococcus sanguis and other streptococci with Candida albicans. Infect Immun. 1990;58(5):1429–36. doi: 10.1128/iai.58.5.1429-1436.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Ellepola K, Truong T, Liu Y, Lin Q, Lim TK, Lee YM et al. Multi-omics analyses reveal synergistic Carbohydrate Metabolism in Streptococcus mutans-Candida albicans mixed-species biofilms. Infect Immun. 2019;87(10). [DOI] [PMC free article] [PubMed]
- 187.Falsetta ML, Klein MI, Colonne PM, Scott-Anne K, Gregoire S, Pai CH, et al. Symbiotic relationship between Streptococcus mutans and Candida albicans synergizes virulence of plaque biofilms in vivo. Infect Immun. 2014;82(5):1968–81. doi: 10.1128/IAI.00087-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Hwang G, Liu Y, Kim D, Li Y, Krysan DJ, Koo H. Candida albicans mannans mediate Streptococcus mutans exoenzyme GtfB binding to modulate cross-kingdom biofilm development in vivo. PLoS Pathog. 2017;13(6):e1006407. doi: 10.1371/journal.ppat.1006407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Hwang G, Marsh G, Gao L, Waugh R, Koo H. Binding Force Dynamics of Streptococcus mutans-glucosyltransferase B to Candida albicans. J Dent Res. 2015;94(9):1310–7. doi: 10.1177/0022034515592859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Koo H, Xiao J, Klein MI, Jeon JG. Exopolysaccharides produced by Streptococcus mutans glucosyltransferases modulate the establishment of microcolonies within multispecies biofilms. J Bacteriol. 2010;192(12):3024–32. doi: 10.1128/JB.01649-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Rainey K, Michalek SM, Wen ZT, Wu H. Glycosyltransferase-mediated Biofilm Matrix Dynamics and Virulence of Streptococcus mutans. Appl Environ Microbiol. 2019;85(5). [DOI] [PMC free article] [PubMed]
- 192.Souza JGS, Bertolini M, Thompson A, Mansfield JM, Grassmann AA, Maas K, et al. Role of glucosyltransferase R in biofilm interactions between Streptococcus oralis and Candida albicans. Isme j. 2020;14(5):1207–22. doi: 10.1038/s41396-020-0608-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Yang C, Scoffield J, Wu R, Deivanayagam C, Zou J, Wu H. Antigen I/II mediates interactions between Streptococcus mutans and Candida albicans. Mol Oral Microbiol. 2018;33(4):283–91. doi: 10.1111/omi.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Khoury ZH, Vila T, Puthran TR, Sultan AS, Montelongo-Jauregui D, Melo MAS, et al. The role of Candida albicans Secreted Polysaccharides in augmenting Streptococcus mutans adherence and mixed biofilm formation: in vitro and in vivo studies. Front Microbiol. 2020;11:307. doi: 10.3389/fmicb.2020.00307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Dutton LC, Paszkiewicz KH, Silverman RJ, Splatt PR, Shaw S, Nobbs AH, et al. Transcriptional landscape of trans-kingdom communication between Candida albicans and Streptococcus gordonii. Mol Oral Microbiol. 2016;31(2):136–61. doi: 10.1111/omi.12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Montelongo-Jauregui D, Saville SP, Lopez-Ribot JL. Contributions of Candida albicans Dimorphism, Adhesive interactions, and Extracellular Matrix to the formation of dual-species biofilms with Streptococcus gordonii. mBio. 2019;10(3). [DOI] [PMC free article] [PubMed]
- 197.Montelongo-Jauregui D, Srinivasan A, Ramasubramanian AK, Lopez-Ribot JL. An in Vitro Model for oral mixed biofilms of Candida albicans and Streptococcus gordonii in Synthetic Saliva. Front Microbiol. 2016;7:686. doi: 10.3389/fmicb.2016.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Montelongo-Jauregui D, Srinivasan A, Ramasubramanian AK, Lopez-Ribot JL. An in Vitro Model for Candida albicans-Streptococcus gordonii Biofilms on Titanium Surfaces. J Fungi (Basel). 2018;4(2). [DOI] [PMC free article] [PubMed]
- 199.Ricker A, Vickerman M, Dongari-Bagtzoglou A. Streptococcus gordonii glucosyltransferase promotes biofilm interactions with Candida albicans. J Oral Microbiol. 2014;6. [DOI] [PMC free article] [PubMed]
- 200.Zhou Z, Ren B, Li J, Zhou X, Xu X, Zhou Y. The role of Glycoside Hydrolases in S. gordonii and C. albicans interactions. Appl Environ Microbiol. 2022;88(10):e0011622. doi: 10.1128/aem.00116-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Jack AA, Daniels DE, Jepson MA, Vickerman MM, Lamont RJ, Jenkinson HF, et al. Streptococcus gordonii comCDE (competence) operon modulates biofilm formation with Candida albicans. Microbiol (Reading) 2015;161(Pt 2):411–21. doi: 10.1099/mic.0.000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Dausset C, Bornes S, Miquel S, Kondjoyan N, Angenieux M, Nakusi L, et al. Identification of sulfur components enhancing the anti-candida effect of Lactobacillus rhamnosus Lcr35. Sci Rep. 2020;10(1):17074. doi: 10.1038/s41598-020-74027-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Jabra-Rizk MA, Meiller TF, James CE, Shirtliff ME. Effect of farnesol on Staphylococcus aureus biofilm formation and antimicrobial susceptibility. Antimicrob Agents Chemother. 2006;50(4):1463–9. doi: 10.1128/AAC.50.4.1463-1469.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Polke M, Leonhardt I, Kurzai O, Jacobsen ID. Farnesol signalling in Candida albicans - more than just communication. Crit Rev Microbiol. 2018;44(2):230–43. doi: 10.1080/1040841X.2017.1337711. [DOI] [PubMed] [Google Scholar]
- 205.Yapıcı M, Gürsu BY, Dağ İ. In vitro antibiofilm efficacy of farnesol against Candida species. Int Microbiol. 2021;24(2):251–62. doi: 10.1007/s10123-021-00162-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.