Abstract
Background
Famine is a risk factor for non-communicable chronic diseases (NCDs), which account for over 80% of deaths in China. The effect of famine on the prevalence of NCDs in terms of various age groups, time periods and cohorts is currently poorly understood.
Objective
This study aims to explore long-term trends in the impact of China’s Great Famine (1959–1961) on NCDs in China.
Methods
This study used data from the 2010–2020 China Family Panel Longitudinal Survey across 25 provinces in China. The subjects were aged 18–85 years, and the total number of subjects was 174,894. The prevalence of NCDs was derived from the China Family Panel Studies database (CFPS). An age-period-cohort (APC) model was used to estimate the age, period and cohort effects of NCDs in 2010–2020 and the effect of famine on the risk of NCDs in terms of cohort effects.
Results
The prevalence of NCDs increased with age. Additionally, the prevalence did not clearly decrease over the survey period. Regarding the cohort effect, people born in the years adjacent to the famine period had a higher risk of NCDs; additionally, females, those born in rural areas, and those who lived in provinces with severe famine and post-famine had a higher likelihood of NCDs.
Conclusions
Experiencing famine at an early age or the experience of famine in a close relative’s generation (births after the onset of famine) are associated with an increased risk of NCDs. Additionally, more severe famine is associated with a higher risk of NCDs.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-16142-4.
Keywords: Famine, Non-communicable chronic diseases, Age-period-cohort models, Prevalence, China Family Panel Studies
Introduction
China has the largest ageing society in the world, with the number of people aged 60 and over already reaching 264 million in 2020, accounting for 18.7%, and expected to increase to 28% in 2040 [1, 2]. Aging population increasing the risk and burden of non-communicable diseases (NCDs) and posing a major challenge to the public health services [1]. NCDs, which are characterized by high morbidity, disability and mortality, are the leading cause of death worldwide [3]. In the World Health Statistics 2022 report, the World Health Organization (WHO) noted that the global proportion of deaths attributable to NCDs increased from almost 60.8% in 2000 to 73.6% in 2019 [4, 5]. Previous studies have shown that NCDs are mostly influenced by personal factors that can be prevented and improved during the life cycle, such as an unhealthy diet, physical inactivity, obesity, smoking and excessive alcohol consumption [5–10]. Furthermore, for the entire population, NCDs are also affected by economic, social, ecological and early life events, of which famine is one key factor that requires further research attention [11].
Famine is defined as an acute onset of extreme starvation that leads to excess mortality and reduced fertility [12, 13]. Famine may lead to weight loss, growth retardation and malnutrition [14]. Indeed, famine even causes premature death and has a serious impact on mortality [11, 14], which cannot be predicted or changed. In addition, early evidence suggests that prenatal malnutrition and childhood famine exposure are associated with an increased risk of NCDs [15–21]. Between the spring of 1959 and the end of 1961, China experienced one of the worst famines in its history, resulting in the premature death of tens of millions [22]. Those who experienced famine and were born during the famine are now aging and face NCDs that required more attention. Most of the studies recently mainly explore the association between famine exposure and single NCDs. Exploring the effects can provide a valid basis for healthy development for older adults in ageing time.
Methods
Data source
The data for this study were sourced from the China Family Panel Studies (CFPS) database, a national, large-scale, multidisciplinary social tracking survey project. These data reflect changes in China’s society, economy, population, education and health. The CFPS database is implemented by the Institute of Social Science Survey (ISSS) of Peking University, and it provides a database for academic research and public policy analysis. In the CFPS, computer-aided survey technology is used to conduct the interviews with the participants in order to meet diverse design needs, improve the access efficiency and ensure the data quality. The CFPS sample covers 25 provinces/municipalities/autonomous regions, with good regional representation [23]. Ethical approval was granted by the Biomedical Ethics Committee of Peking University. The CFPS database is a biennial survey, and this study used data from the survey years 2010, 2012, 2014, 2016, 2018 and 2020 for the population aged 18–85 years.
Statistical analyses
According to the requirements of the APC model, birth cohort = period − age needs to be satisfied; the famine lasted for a 3 year period from 1959–1961, so the study period was arranged in 3 year intervals. As the CFPS database is a biennial follow-up study, we used the calculated NCD prevalence rates for 2012, 2014, 2018 and 2020 as reasonable estimates for the NCD prevalence in 2013 and 2019 to obtain data for survey years 2010, 2013, 2016 and 2019. The ages of the participants ranged from 18 to 85 years, and they were divided into 21 consecutive age intervals(19–21,22–25…82–84), with 18 and 85 years being placed in the first and last age groups. The birth cohorts comprised 23 consecutive 3 year cohort intervals from 1925 to 2002. The 2013 survey year and 1948 birth cohorts were specified as the reference groups for the period and cohort effects, and the relative risk ratios for the period and cohort relative to the respective reference groups for the disease were calculated separately. We used the age-period-cohort web tool (Age Period Cohort Analysis Tool [cancer.gov]) [24–26] provided by the National Cancer Institute for the parameter estimation and analysis [26].
Males versus females, individuals living in urban versus rural areas, and individuals from different provinces experienced varying famine intensity [27–30]. We defined seven provinces as experiencing severe famine exposure (Sichuan, Anhui, Guizhou, Qinghai, Gansu, Guangxi, Henan), and the other provinces were defined as experiencing mild famine [22]. Firstly, we examined the trends in the prevalence of NCDs in China by gender, urban versus rural areas, and provinces with different famine intensities from 2010 to 2020. The age, period and cohort effects in the APC model were then assessed using the APC framework.
Results
Trends in NCD Prevalence
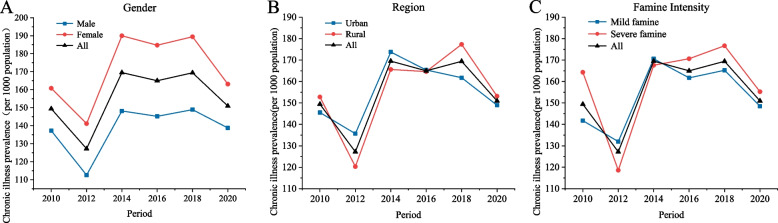
The average prevalence of NCDs among individuals aged 18–85 years surveyed in the CFPS from 2010 to 2020 was 155.4 per 1,000 people (Table 1, Fig. 1). For both genders, the NCD prevalence was lowest in 2012 and highest in 2014, and there was a higher prevalence among females than males in all the survey periods (Fig. 1A). There were no major differences in the prevalence of NCDs in urban versus rural areas within each survey period, and 2012 showed the lowest NCD prevalence across urban and rural areas (Fig. 1B). Additionally, a similar pattern was observed in terms of the provinces with different famine intensities (Fig. 1C).
Table 1.
Incidence of NCDs by group classification, 2010–2020
| Group/Year | 2010 (n‰) | 2012 (n‰) | 2014 (n‰) | 2016 (n‰) | 2018 (n‰) | 2020 (n‰) | Total (n‰) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | 2148 | (137.2) | 1664 | (112.5) | 2182 | (148.2) | 2309 | (145.2) | 2138 | (148.9) | 1478 | (138.8) | 11,919 | (138.5) |
| Female | 2683 | (160.8) | 2195 | (141.2) | 2913 | (190.0) | 2941 | (184.7) | 2781 | (189.4) | 1739 | (163.1) | 15,252 | (171.7) |
| Urban | 2191 | (145.5) | 1852 | (135.7) | 2503 | (173.7) | 2595 | (165.4) | 2390 | (161.8) | 1657 | (148.9) | 13,188 | (155.7) |
| Rural | 2640 | (152.8) | 2007 | (120.3) | 2592 | (165.6) | 2655 | (164.6) | 2529 | (177.3) | 1560 | (153.1) | 13,983 | (155.0) |
| Severe famine provinces | 1805 | (164.3) | 1282 | (118.6) | 1798 | (167.6) | 2001 | (170.6) | 1874 | (176.7) | 1204 | (155.2) | 9964 | (159.1) |
| Mild famine provinces | 3026 | (141.7) | 2577 | (132.0) | 3297 | (170.6) | 3249 | (161.7) | 3045 | (165.2) | 2013 | (148.5) | 17,207 | (153.2) |
| All | 4831 | (149.4) | 3859 | (127.2) | 5095 | (169.5) | 5250 | (165.0) | 4919 | (169.4) | 3217 | (150.9) | 27,171 | (155.4) |
n‰ is the number of NCDs per 1,000 individuals in the population
Fig. 1.
Trends in the prevalence of NCDs by (A) gender, (B) rural versus urban areas and (C) famine intensity
Age-Specific Prevalence Rates for NCDs
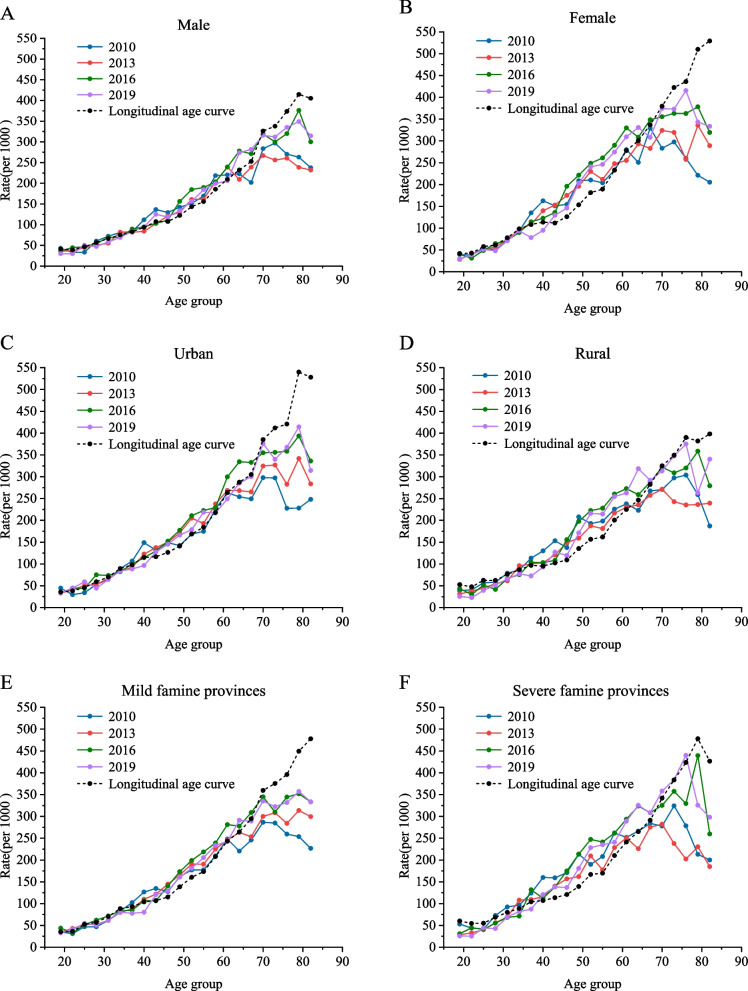
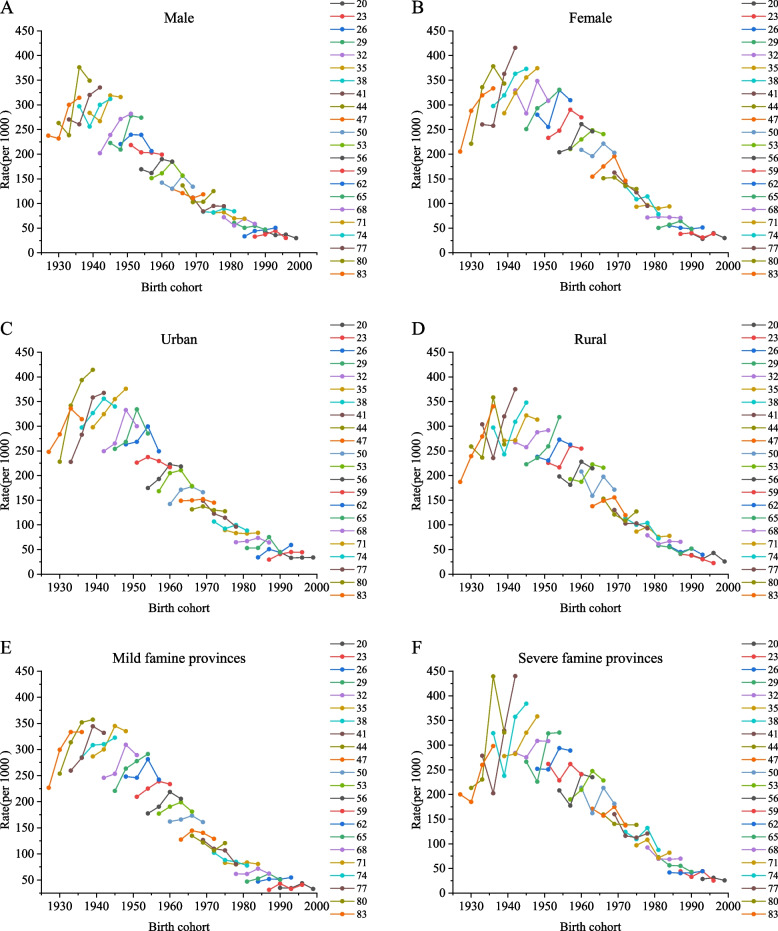
For our study, the population data and NCD prevalence rates for 2013 and 2019 were feasibly estimated, resulting in survey data in 3 year intervals for 2010, 2013, 2016 and 2019. The trends in NCD prevalence from 2010 to 2019 showed stable trends by gender, with the largest differences in males between 2013 and 2016 and a slight decrease in 2019 for females (SI Appendix Table S1, Fig. 2A and B). The prevalence of NCDs in urban areas decreased slightly in 2019, while the prevalence in rural areas showed a gradual increase after the lowest point in 2013 (Fig. 2C and D). There was an overall increasing trend in the prevalence of NCDs over time across the provinces with different famine intensities d (Fig. 2E and F). In terms of the NCD prevalence rates in each cohort by age group, there was a decreasing trend with more recent birth cohorts there was a decreasing trend t, thus indicating a lower prevalence of NCDs in the more recent birth cohorts (SI Appendix Table S2, Fig. 3).
Fig. 2.
Prevalence of NCDs by age for (A) male and (B) female gender, (C) urban versus (D) rural areas and (E) provinces with mild versus (F) severe famine intensity, 2010–2019
Fig. 3.
Prevalence of NCDs by age-group cohort for (A) male and (B) female gender, (C) urban versus (D) rural areas and provinces with (E) mild versus (F) severe famine intensity, 2010–2019
Age-Period-Cohort Effects on NCD Prevalence
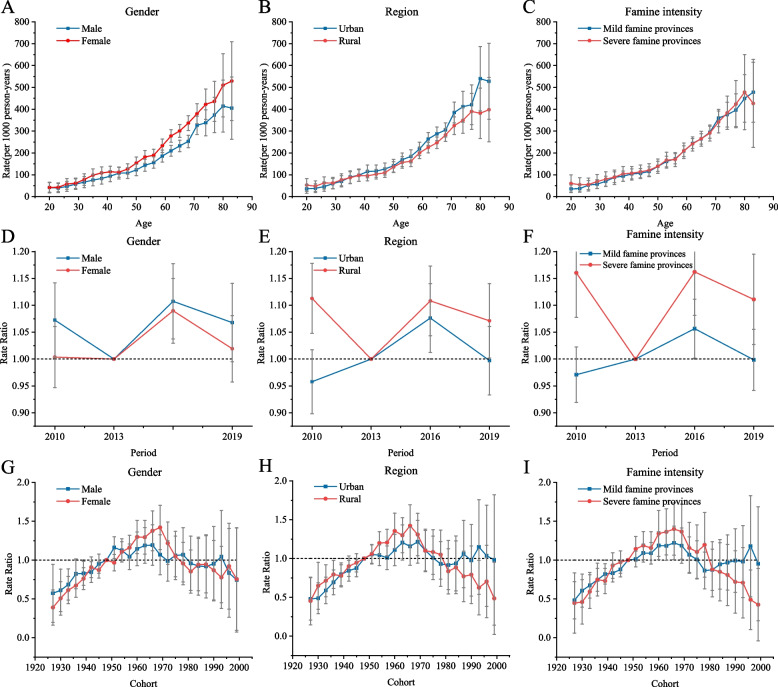
In the APC model, the longitudinal age curve is used to assess the age effects. The age trends in the prevalence of NCDs were similar throughout the study period, indicating that NCD prevalence increases with age (Fig. 4). In terms of gender, the prevalence of NCDs was higher in male at all ages (Fig. 4A). Furthermore, in those aged 35 years and above, there was a higher prevalence of NCDs in urban areas (Fig. 4B). In addition, the difference in prevalence across age groups was small between provinces exposed to severe versus mild famine, but the overall prevalence was higher in provinces with severe famine (Fig. 4C).
Fig. 4.
Parameter estimates of the age effects on NCD prevalence by (A) gender, (B) rural versus urban regions and (C) provinces with different famine intensities; parameter estimates of the period effects on NCD prevalence by (D) gender, (E) rural versus urban regions and (F) provinces with different famine intensities; and parameter estimates of the cohort effects on NCD prevalence by (G) gender, (H) rural versus urban regions and (I) provinces with different famine intensities, 2010–2019. Abbreviation: APC = age-period-cohort
Across genders, the prevalence of NCDs did not improve throughout the study period (Fig. 4D). As shown in the figure, the trend in NCD prevalence based on period was similar in urban and rural areas and in provinces with different famine intensities (Figs. 4E, 4F). The NCD prevalence did not improve significantly in any of the survey years except for in urban areas and provinces with mild famine exposure in 2010.
In terms of the cohort effect, the NCD prevalence followed an inverted U-shaped distribution across the cohorts in all three groups (gender, urban versus rural areas and province famine intensity; (Fig. 4G–I). Females born during and around the famine had a higher risk of NCDs (Fig. 4G). Additionally, those living in rural areas (Fig. 4H) and in provinces with severe famine exposure had a higher risk of NCDs.
Discussion
Our findings highlight the effect of the 1959–1961 Great China Famine on NCDs. Specifically, pre-birth famine exposure was associated with an increased risk of NCDs in later life. By combining longitudinal survey data with APC models to analyze trends in the prevalence of NCDs, we found similarities in prevalence across these three important time segments (age, period and cohort). The age effects indicated that the prevalence of NCDs increased with age. The period effect showed that the risk of NCDs varied between the survey times, but these differences were not significant. In terms of cohort effects, the risk was higher among those who were born during, before and soon after the famine.
The results regarding the age effect, which is the effect of age on disease prevalence, were similar to those of previous studies, as the prevalence of NCDs was highest among older people, regardless of gender, urban versus rural regions, or famine intensity in the province [31–33]. Similarly, the results in terms of gender were consistent with previous research showing a slightly higher prevalence of NCDs in females than males [34]. The higher prevalence of NCDs in urban areas observed in this study may be related to the increased health risk factors associated with urbanization, such as changes in dietary patterns and environmental pollution [27, 34, 35]. Finally, the age effects on NCD prevalence were similar across provinces with different intensities of famine exposure.
Period effects refer to changes in disease rates in populations affected by human or social factors. From the results, it is clear that the prevalence of NCDs did not improve throughout the survey period. It is likely that the risk of NCDs continues to rise due to the increased health risk factors resulting from the ageing population and rapid urbanization [35]. During the survey period, males had a higher risk of NCDs, possibly because males had more risk factors for NCDs, such as smoking and drinking [36]. Moreover, the speed of ageing in rural areas has been faster than in urban areas in recent years, and rural people are at a disadvantage in terms of social economy, medical resources and other aspects [27]. As such, people in rural areas are more susceptible to NCDs. The extreme similarities in NCD prevalence between different provinces and urban and rural areas suggests a greater risk of NCDs in provinces where the intensity of famine and rural was high during the survey period, which may be due to the health lag caused by famine [15–18, 37].
Cohort effects refer to changes in disease prevalence due to different levels of exposure to risk factors across generations; in this one, one notable finding was the high risk of NCDs in cohorts born during and around the famine and post-famine (This group is defined as those born after the famine and whose risk of chronic disease is referenced to the 1948 birth cohort). Studies have claimed that the adverse effects of famine on survivors mean they are more at risk of NCDs [38, 39]. Other studies have demonstrated that severe famine within 3 years can affect the health of at least two generations [40, 41]. Additionally, gender discrepancies have been found, with one study reporting that the mortality rate for girls was around 7% higher than that of boys during the famine, due to Chinese traditional cultural beliefs, more care for male babies and thus more opportunities for survival [28–30, 42]. Other explanations about the starvation exposure can lead to NCDs in females is the effects of genetic changes triggered by unfavorable prenatal environments that also vary by gender [43, 44]. In addition, rural areas were more affected by the famine due to severe food supply shortages and restrictions on rural–urban migration during the famine [22, 30, 45]. And seven provinces, including Sichuan, Anhui, Guizhou, Qinghai, Gansu, Guangxi and Henan, suffered greater loss of life during the famine compared to other provinces [11, 46]. The main reason for these large differences in famine intensity was that the implementation of the central government’s grain quota procurement differed across the provinces [22]. This is similar to the findings of some studies, such as the increased prevalence of diabetes among those born in more severely affected areas compared to less affected famine areas, and the same results may exist for other NCDs [18, 47].
The risk of NCDs varies significantly between males and females, urban and rural, and between groups of provinces with different famine intensities, these severity patterns may be the reason for the significant differences in the risk of NCDs. Indeed, those born in 1947–1961 were exposed to the famine during gestation, as infants, and as school children (0–12 years), and their high risk of NCDs may be due to their experience of famine [12, 16, 17, 46]. Furthermore, although those born in 1962–1978 did not experience famine themselves, parental exposure to famine prior to pregnancy. Some studies show that the children of hungry mothers are more likely to have health problems [18, 48, 49]. Maternal malnutrition or malnutrition in prenatal could exacerbates the risk of developing certain NCDs, reinforcing the source of the increased risk of NCDs prevalence in the post-famine birth cohort in the context of cumulative exposure [12, 18, 22, 31, 37, 50]. In addition, there are sibling-designed studies used to exclude and detect confounding factors, and the results suggest that individual epigenetic differences between famine-affected and non-fame-affected same-sex siblings in middle and old age, such as changes in methylation levels [18, 51]. Overall, the high risk of NCDs among this cohort may be associated with their parents’ experience of famine, which may subsequently affect the individuals throughout their life span [31, 52–54].
The latest report shows that the goal of eradicating hunger and malnutrition by 2030 is not expected to be achieved, and that 8% of the world's population will still face starvation [55]. Unhealthy diets have long been associated with increasing rates of NCDs globally, but the burden of disease from food shortages and famine is often underestimated [56]. As the problem of famine and malnutrition remains unsolved to date, we should be concerned about the future incidence of NCDs in famine-exposed populations and the burden of disease that it brings, in addition to the outcome that it leads to death. In addition, aging population is increasing in China and globally, and the consequent health problems should be focused that have experienced famine, with an emphasis on increased screening, treatment and management of diseases and better social protection.
Currently, few studies have used the APC model to explore the effect of famine exposure on the prevalence of NCDs. In our study, we examined the effects of age, period and cohort on the risk of NCDs and, thus, identified priority groups for prevention and treatment. The limitations of our study are as follows [1]. The database lacks migration data for people who experienced famine in the early years, and it was, thus, not possible to determine their demographic information at the time of the famine; as a result, some people living in urban or rural areas or certain provinces during the survey period may not have lived in those areas during the famine period [2]. Since the time span of the famine was 3 years and the CFPS database is followed up every 2 years, in order to meet the conditions of APC, we used the survey data from 2012 and 2014 to obtain the average prevalence to estimate the results of the 2013 survey year, and we used the survey data of 2018 and 2020 to obtain the average prevalence to estimate the results of the 2019 survey year; although all the data during the CFPS survey period were used, there may have been deviations among the years that were not accounted for by these estimates [3]. Famine is a natural event, and the population selected bias for this study is an unavoidable.
Conclusions
Famine exposure is associated with an increased risk of NCDs. The age effect showed that the prevalence of NCDs increased with age, the period effect showed that the prevalence differed across the survey period, and the cohort effect showed that those born during and around the time of the famine were at higher risk of NCDs. Across the population, groups that suffered more severely from famine, including females and those in rural areas and provinces with severe famine exposure, were at higher risk of NCDs. In conclusion, preventing famine and actively improving the nutritional status of females of childbearing age are important actions for reducing NCDs.
Supplementary Information
Additional file 1: Table S1. Prevalence of NCDs by age for male and female gender, urban versus rural areas and provinces with mild versus severe famine intensity, 2010–2019. Table S2. Prevalence of NCDs by age, period, and birth cohort, 2010-2019 (per 1000 population).
Acknowledgements
The authors sincerely thank all study participants and research staff that have contributed to this work.
Authors’ contributions
Xiaoxue He, Xiaojuan Shi and Degong Pan were responsible for data collection, data analysis, and drafting, writing the manuscript. Huihui Wang, Xue Zhang and Lining Pu were responsible for data curation, Formal analysis,Writing review and editing. Mingxiu Luo and Jiangping Li were responsible for study design, data analysis, drafting, writing and editing of the manuscript. All the authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
Publicly available datasets were analyzed in this study. This data can be found at: https://opendata.pku.edu.cn.
Declarations
Ethics approval and consent to participate
All respondents participated in the survey on the basis of informed consent, and this survey has been reviewed by the Biomedical Ethics Committee of Peking University (Approval number. IRB00001052-14010).
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mingxiu Luo, Email: luomingxiuwater@126.com.
Jiangping Li, Email: lijp@nxmu.edu.cn.
References:
- 1.The L. Population ageing in China: crisis or opportunity? Lancet. 2022;400(10366):1821. doi: 10.1016/S0140-6736(22)02410-2. [DOI] [PubMed] [Google Scholar]
- 2.Tatum M. China's population peak. Lancet. 2022;399(10324):509. doi: 10.1016/S0140-6736(22)00227-6. [DOI] [PubMed] [Google Scholar]
- 3.Williams J, Allen L, Wickramasinghe K, Mikkelsen B, Roberts N, Townsend N. A systematic review of associations between non-communicable diseases and socioeconomic status within low- and lower-middle-income countries. J Glob Health. 2018;8(2):020409. doi: 10.7189/jogh.08.020409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 5.WHO. World health statistics . monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2022. p. 2022. [Google Scholar]
- 6.Branca F, Lartey A, Oenema S, Aguayo V, Stordalen GA, Richardson R, et al. Transforming the food system to fight non-communicable diseases. BMJ. 2019;364:l296. doi: 10.1136/bmj.l296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Billingsley M. New advice on physical activity aims to prevent chronic disease from early years. BMJ. 2011;343:d4457. doi: 10.1136/bmj.d4457. [DOI] [PubMed] [Google Scholar]
- 8.Caprara G. Mediterranean-Type Dietary Pattern and Physical Activity: The Winning Combination to Counteract the Rising Burden of Non-Communicable Diseases (NCDs) Nutrients. 2021;13(2):429. doi: 10.3390/nu13020429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nyberg ST, Batty GD, Pentti J, Virtanen M, Alfredsson L, Fransson EI, et al. Obesity and loss of disease-free years owing to major non-communicable diseases: a multicohort study. The Lancet Public Health. 2018;3(10):e490–e497. doi: 10.1016/S2468-2667(18)30139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang GH, Wen GJ. Communal Dining and the Chinese Famine of 1958–1961. Econ Dev Cult Change. 1997;46(1):1–34. doi: 10.1086/452319. [DOI] [Google Scholar]
- 12.He S, Li J, Wang Z, Wang L, Liu L, Sun X, et al. Early-life exposure to famine and late-life depression: Does leukocyte telomere length mediate the association? J Affect Disord. 2020;274:223–228. doi: 10.1016/j.jad.2020.05.082. [DOI] [PubMed] [Google Scholar]
- 13.Hammen C. Risk Factors for Depression: An Autobiographical Review. Annu Rev Clin Psychol. 2018;14:1–28. doi: 10.1146/annurev-clinpsy-050817-084811. [DOI] [PubMed] [Google Scholar]
- 14.Li C, Lumey LH. Exposure to the Chinese famine of 1959–61 in early life and long-term health conditions: a systematic review and meta-analysis. Int J Epidemiol. 2017;46(4):1157–1170. doi: 10.1093/ije/dyx013. [DOI] [PubMed] [Google Scholar]
- 15.Gunnell D, Whitley E, Upton MN, McConnachie A, Smith GD, Watt GCM. Associations of height, leg length, and lung function with cardiovascular risk factors in the Midspan Family Study. J Epidemiol Community Health. 2003;57(2):141–146. doi: 10.1136/jech.57.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lelijveld N, Seal A, Wells JC, Kirkby J, Opondo C, Chimwezi E, et al. Chronic disease outcomes after severe acute malnutrition in Malawian children (ChroSAM): a cohort study. Lancet Glob Health. 2016;4(9):e654–e662. doi: 10.1016/S2214-109X(16)30133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grey K, Gonzales GB, Abera M, Lelijveld N, Thompson D, Berhane M, et al. Severe malnutrition or famine exposure in childhood and cardiometabolic non-communicable disease later in life: a systematic review. BMJ Glob Health. 2021;6(3):e003161. doi: 10.1136/bmjgh-2020-003161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lumey LH, Stein AD, Susser E. Prenatal famine and adult health. Annu Rev Public Health. 2011;32:237–262. doi: 10.1146/annurev-publhealth-031210-101230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Veenendaal MVE, Painter RC, de Rooij SR, Bossuyt PMM, van der Post JAM, Gluckman PD, et al. Transgenerational effects of prenatal exposure to the 1944–45 Dutch famine. BJOG. 2013;120(5):548–553. doi: 10.1111/1471-0528.12136. [DOI] [PubMed] [Google Scholar]
- 20.Li J, Na L, Ma H, Zhang Z, Li T, Lin L, et al. Multigenerational effects of parental prenatal exposure to famine on adult offspring cognitive function. Sci Rep. 2015;5:13792. doi: 10.1038/srep13792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li J, Liu S, Li S, Feng R, Na L, Chu X, et al. Prenatal exposure to famine and the development of hyperglycemia and type 2 diabetes in adulthood across consecutive generations: a population-based cohort study of families in Suihua. China Am J Clin Nutr. 2017;105(1):221–227. doi: 10.3945/ajcn.116.138792. [DOI] [PubMed] [Google Scholar]
- 22.Hu XF, Liu GG, Fan M. Long-Term Effects of Famine on Chronic Diseases: Evidence from China's Great Leap Forward Famine. Health Econ. 2017;26(7):922–936. doi: 10.1002/hec.3371. [DOI] [PubMed] [Google Scholar]
- 23.Xie Y, Lu P. The Sampling Design of the China Family Panel Studies (CFPS) Chin J Sociol. 2015;1(4):471–484. doi: 10.1177/2057150X15614535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zou Z, Cini K, Dong B, Ma Y, Ma J, Burgner DP, et al. Time Trends in Cardiovascular Disease Mortality Across the BRICS: An Age-Period-Cohort Analysis of Key Nations With Emerging Economies Using the Global Burden of Disease Study 2017. Circulation. 2020;141(10):790–799. doi: 10.1161/CIRCULATIONAHA.119.042864. [DOI] [PubMed] [Google Scholar]
- 25.Chen YY, Yang CT, Pinkney E, Yip PSF. The Age-Period-Cohort trends of suicide in Hong Kong and Taiwan, 1979–2018. J Affect Disord. 2021;295:587–593. doi: 10.1016/j.jad.2021.08.084. [DOI] [PubMed] [Google Scholar]
- 26.Rosenberg PS, Check DP, Anderson WF. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2014;23(11):2296–2302. doi: 10.1158/1055-9965.EPI-14-0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang S, Marquez P, Langenbrunner J, Niessen L, Suhrcke M, Song F. Toward a Healthy and Harmonious Life in China: Stemming the Rising Tide of Non-Communicable Diseases: World Bank HUMAN DEVELOPMENT UNIT East Asia and Pacific Region; 2012.
- 28.Mu R, Zhang X. Why does the Great Chinese Famine affect the male and female survivors differently? Mortality selection versus son preference. Econ Hum Biol. 2011;9(1):92–105. doi: 10.1016/j.ehb.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Yang Z, Zhao W, Zhang X, Mu R, Zhai Y, Kong L, et al. Impact of famine during pregnancy and infancy on health in adulthood. Obes Rev. 2008;9(Suppl 1):95–99. doi: 10.1111/j.1467-789X.2007.00447.x. [DOI] [PubMed] [Google Scholar]
- 30.Coale AJ, Banister J. Five decades of missing females in China. Demography. 1994;31(3):459–479. doi: 10.2307/2061752. [DOI] [PubMed] [Google Scholar]
- 31.Budreviciute A, Damiati S, Sabir DK, Onder K, Schuller-Goetzburg P, Plakys G, et al. Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Front Public Health. 2020;8:574111. doi: 10.3389/fpubh.2020.574111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jiang C, Wang Q. Analysis of Influencing Factors for Chronic Diseases: A Large Sample Epidemiological Survey from Liaoyang. Comput Math Methods Med. 2022;2022:1537906. doi: 10.1155/2022/1537906. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 33.Devaux M, Lerouge A, Giuffre G, Giesecke S, Baiocco S, Ricci A, et al. How will the main risk factors contribute to the burden of non-communicable diseases under different scenarios by 2050? A modelling study. PLoS ONE. 2020;15(4):e0231725. doi: 10.1371/journal.pone.0231725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jian W, Chan KY, Reidpath DD, Xu L. China's rural-urban care gap shrank for chronic disease patients, but inequities persist. Health Aff (Millwood) 2010;29(12):2189–2196. doi: 10.1377/hlthaff.2009.0989. [DOI] [PubMed] [Google Scholar]
- 35.Tang S, Ehiri J, Long Q. China's biggest, most neglected health challenge: Non-communicable diseases. Infect Dis Poverty. 2013;2(1):7. doi: 10.1186/2049-9957-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pratt A, Pastorelli A, Lee T. The bill China cannot afford: health, economic and social costs of China’s tobacco epidemic. Manila, Philippines: World Health Organization Regional Office for the Western Pacific; 2017.
- 37.Henriksen T, Clausen T. The fetal origins hypothesis: placental insufficiency and inheritance versus maternal malnutrition in well-nourished populations. Acta Obstet Gynecol Scand. 2002;81(2):112–114. doi: 10.1034/j.1600-0412.2002.810204.x. [DOI] [PubMed] [Google Scholar]
- 38.Meng X, Qian N. The Long Term Consequences of Famine on Survivors: Evidence from a Unique Natural Experiment Using China's Great Famine. National Bureau Of Economic Research. 2009(14917).
- 39.Gørgens T, Meng X, Vaithianathan R. Stunting and selection effects of famine: A case study of the Great Chinese Famine. J Dev Econ. 2012;97:99–111. doi: 10.1016/j.jdeveco.2010.12.005. [DOI] [Google Scholar]
- 40.Li J, Yang Q, An R, Sesso HD, Zhong VW, Chan KHK, et al. Famine and Trajectories of Body Mass Index, Waist Circumference, and Blood Pressure in Two Generations: Results From the CHNS From 1993–2015. Hypertension. 2022;79(3):518–531. doi: 10.1161/HYPERTENSIONAHA.121.18022. [DOI] [PubMed] [Google Scholar]
- 41.Srichaikul K, Hegele RA, Jenkins DJA. Great Chinese Famine and the Effects on Cardiometabolic Health for Future Generations. Hypertension. 2022;79(3):532–535. doi: 10.1161/HYPERTENSIONAHA.121.18546. [DOI] [PubMed] [Google Scholar]
- 42.Chang X, Song P, Wang M, An L. The Risks of Overweight, Obesity and Abdominal Obesity in Middle Age after Exposure to Famine in Early Life: Evidence from the China's 1959–1961 Famine. J Nutr Health Aging. 2018;22(10):1198–1204. doi: 10.1007/s12603-018-1144-z. [DOI] [PubMed] [Google Scholar]
- 43.Gilbert JS, Nijland MJ. Sex differences in the developmental origins of hypertension and cardiorenal disease. Am J Physiol Regul Integr Comp Physiol. 2008;295(6):R1941–R1952. doi: 10.1152/ajpregu.90724.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hanley AJG, Wagenknecht LE, Norris JM, Bryer-Ash M, Chen YI, Anderson AM, et al. Insulin resistance, beta cell dysfunction and visceral adiposity as predictors of incident diabetes: the Insulin Resistance Atherosclerosis Study (IRAS) Family study. Diabetologia. 2009;52(10):2079–2086. doi: 10.1007/s00125-009-1464-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lin JY, Yang DT. FOOD AVAILABILITY, ENTITLEMENTS AND THE CHINESE FAMINE OF 1959±61. Econ J. 2000;110:130–158. doi: 10.1111/1468-0297.00494. [DOI] [Google Scholar]
- 46.Liu Y, Liu Y, Lu Y, Li J, He S. Association of Parental Famine Exposure With Offspring Depression and Cognition Function. Front Psychiatry. 2022;13:812805. doi: 10.3389/fpsyt.2022.812805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li Y, He Y, Qi L, Jaddoe VW, Feskens EJM, Yang X, et al. Exposure to the Chinese famine in early life and the risk of hyperglycemia and type 2 diabetes in adulthood. Diabetes. 2010;59(10):2400–2406. doi: 10.2337/db10-0385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Painter RC, Osmond C, Gluckman P, Hanson M, Phillips DIW, Roseboom TJ. Transgenerational effects of prenatal exposure to the Dutch famine on neonatal adiposity and health in later life. BJOG. 2008;115(10):1243–1249. doi: 10.1111/j.1471-0528.2008.01822.x. [DOI] [PubMed] [Google Scholar]
- 49.Huang C, Li Z, Narayan KMV, Williamson DF, Martorell R. Bigger babies born to women survivors of the 1959–1961 Chinese famine: a puzzle due to survival selection? J Dev Orig Health Dis. 2010;1(6):412–418. doi: 10.1017/S2040174410000504. [DOI] [PubMed] [Google Scholar]
- 50.Meng R, Lv J, Yu C, Guo Y, Bian Z, Yang L, et al. Prenatal famine exposure, adulthood obesity patterns and risk of type 2 diabetes. Int J Epidemiol. 2018;47(2):399–408. doi: 10.1093/ije/dyx228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Heijmans BT, Tobi EW, Stein AD, Putter H, Blauw GJ, Susser ES, et al. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc Natl Acad Sci U S A. 2008;105(44):17046–17049. doi: 10.1073/pnas.0806560105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barker DJ. In utero programming of chronic disease. Clin Sci (Lond) 1998;95(2):115–128. doi: 10.1042/cs0950115. [DOI] [PubMed] [Google Scholar]
- 53.Organization WH. Good Maternal Nutrition The best start in life. WHO Regional Office for Europe UN City, Marmorvej 51; 2016.
- 54.Mikkelsen B, Williams J, Rakovac I, Wickramasinghe K, Hennis A, Shin H-R, et al. Life course approach to prevention and control of non-communicable diseases. BMJ. 2019;364:1257. doi: 10.1136/bmj.l257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Burki T. Food security and nutrition in the world. Lancet Diabetes Endocrinol. 2022;10(9):622. doi: 10.1016/S2213-8587(22)00220-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cheng Q, Trangucci R, Nelson KN, Fu W, Collender PA, Head JR, et al. Prenatal and early-life exposure to the Great Chinese Famine increased the risk of tuberculosis in adulthood across two generations. Proc Natl Acad Sci U S A. 2020;117(44):27549–27555. doi: 10.1073/pnas.2008336117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Prevalence of NCDs by age for male and female gender, urban versus rural areas and provinces with mild versus severe famine intensity, 2010–2019. Table S2. Prevalence of NCDs by age, period, and birth cohort, 2010-2019 (per 1000 population).
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found at: https://opendata.pku.edu.cn.