Abstract
Objective
The purpose of this study was to summarize and evaluate the research on the accuracy of provocative maneuvers to diagnose carpal tunnel syndrome (CTS).
Methods
The MEDLINE, CINAHL, Cochrane, and Embase databases were searched, and studies that assessed the diagnostic accuracy of at least 1 provocative test for CTS were selected. Study characteristics and data about the diagnostic accuracy of the provocative tests for CTS were extracted. A random-effects meta-analysis of the sensitivity (Sn) and specificity (Sp) of the Phalen test and Tinel sign was conducted. The risk of bias (ROB) was rated using the QUADAS-2 tool.
Results
Thirty-one studies that assessed 12 provocative maneuvers were included. The Phalen test and the Tinel sign were the 2 most assessed tests (in 22 and 20 studies, respectively). The ROB was unclear or low in 20 studies, and at least 1 item was rated as having high ROB in 11 studies. Based on a meta-analysis of 7 studies (604 patients), the Phalen test had a pooled Sn of 0.57 (95% CI = 0.44–0.68; range = 0.12–0.92) and a pooled Sp of 0.67 (95% CI = 0.52–0.79; range = 0.30–0.95). For the Tinel sign (7 studies, 748 patients), the pooled Sn was 0.45 (95% CI = 0.34–0.57; range = 0.17–0.97) and the pooled Sp was 0.78 (95% CI = 0.60–0.89; range = 0.40–0.92). Other provocative maneuvers were less frequently studied and had conflicting diagnostic accuracies.
Conclusion
Meta-analyses are imprecise but suggest that the Phalen test has moderate Sn and Sp, whereas the Tinel test has low Sn and high Sp. Clinicians should combine provocative maneuvers with sensorimotor tests, hand diagrams, and diagnostic questionnaires to achieve better overall diagnostic accuracy rather than relying on individual clinical tests.
Impact
Evidence of unclear and high ROB do not support the use of any single provocative maneuver for the diagnosis of CTS. Clinicians should consider a combination of noninvasive clinical diagnostic tests as the first choice for the diagnosis of CTS.
Keywords: Carpal Tunnel Syndrome, Diagnostic Accuracy, Phalen Test, Provocative Tests, Systematic Review, Tinel Sign
Introduction
Carpal tunnel syndrome (CTS) is caused by the compression of the median nerve in the carpal canal and is the most prevalent compression neuropathy of the upper extremity (UE).1 The prevalence of CTS has been estimated to be 6% in men and 9.2% in women.1 Symptoms include pain, tingling, and numbness in the palmar surface of the radial 3.5 digits (the area innervated by the median nerve), as well as thenar muscle weakness and atrophy in more severe instances.2 CTS is a significant contributor to days lost from work, with an average of $2 billion in annual costs of medical care.3
Diagnosing CTS is an essential step in the treatment of this condition. CTS can be treated conservatively if diagnosed early, whereas a late diagnosis might limit the treatment options for severe or persistent cases of carpal tunnel release surgery.4 Several diagnostic options are currently available, with the most common ones being electrodiagnosis or nerve conduction velocity testing. These tests are often costly, increase the wait time to receiving management, are painful, and maybe not be available at all settings. Clinicians can benefit from using clinical diagnostic tools, such as questionnaires, scales, hand diagrams, provocative tests, and sensorimotor tests, as outlined by the most recent guideline of the American Academy of Orthopedic Surgeons.5 Unlike nerve conduction velocity testing, clinical examination tests can be done in all clinical settings and yield immediate results.
A systematic review (SR) of the accuracy of clinical examination tests was done by a member of our research team in 2004 but is currently outdated.6 This SR is the last of a series assessing all categories of clinical examination tests for CTS diagnosis. We assessed the accuracy of the questionnaires, scales, hand symptom diagrams/maps,7 and sensorimotor tests8 in 2 previous SRs. We also assessed the accuracy of clinical diagnostic tests and questionnaires in screening for CTS among workers.9 In this SR, we focused on provocative maneuvers for CTS diagnosis, such as the Phalen test, Tinel sign, Durkan test, etc. Therefore, the purpose of the current SR was to identify, critically appraise, and synthesize the evidence on the diagnostic accuracy of provocative tests for diagnosing CTS in people with suspected CTS.
Methods
On December 20, 2018, we registered this SR with the International Prospective Register of Systematic Reviews (PROSPERO), with the registration number CRD42018109031. We followed the Diagnostic Test Accuracy extension of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and the Cochrane collaboration guidelines.10
Information Sources
In consultation with a health sciences librarian at McMaster University, we searched 4 electronic databases on January 20, 2020. We updated our search in February 2022. The electronic databases that we searched were MEDLINE (through Ovid from 1946), Embase, the Cochrane Database of Systematic Reviews, and CINAHL. We designed a search strategy to include studies evaluating the accuracy of any clinical examination tests for CTS (Suppl. Appendix A). We combined keywords and search terms for diagnostic accuracy with clinical diagnostic tests for CTS. The search terms regarding the names of the CTS clinical diagnostic tools were further reviewed for comprehensiveness by 2 authors (A.D. and J.M.), who are a physical therapist and a hand therapist. Finally, we hand-searched the reference lists of the included papers.
Study Selection
Two reviewers (A.D. and J.Y.) independently screened the articles for inclusion in this SR in 2 consecutive phases. In the first phase, we reviewed the titles and abstracts according to a pre-determined set of eligibility criteria. We rated the agreement of the reviewers using κ statistics, which we calculated by STATA statistical analysis software, version 15. κ values <0.20 indicate poor agreement between the reviewers, 0.21 to 0.40 indicate fair agreement, 0.41 to 0.60 indicate moderate agreement, 0.61 to 0.80 indicate substantial agreement. Lastly, values of 0.81 to 1.00 indicate almost perfect agreement.11 In the second phase of study selection, we retrieved the full texts of the articles and reviewed them for inclusion. If disagreements occurred between the 2 reviewers selecting the studies in the first or the second phases, a third research team member (J.M.) resolved the disagreement through discussion.
Eligibility Criteria
We did not exclude articles based on language, sex/gender of the participants, sample size, year of publication, or the type of reference standards. We excluded studies on conditions other than CTS and studies that did not address the diagnostic accuracy of provocative maneuvers. We included studies that met the following criteria.
Design: We included cohort, case–control, or cross-sectional studies with either prospective or retrospective data collections in a full-report format.
Participants: Studies with adult participants (18 years and older) with signs and symptoms of CTS. We excluded studies using participants who were healthy as “controls,” to avoid underestimating accuracy in clinical contexts.
Diagnostic test: Any provocative test for CTS as the diagnostic (or index) test.
Comparison: Studies using a comprehensive clinical examination by an appropriate hand specialist, electrodiagnosis, or a combination of the 2 as a reference standard were included.
Outcome: Studies assessing at least 1 diagnostic accuracy property for CTS diagnoses, such as sensitivity (Sn), specificity (Sp), positive likelihood ratio (+LR), negative likelihood ratio (−LR), and positive predictive values and negative predictive values (PPVs or NPVs).
Time: Any timeframe for the diagnosis of CTS using provocative tests.
Data Extraction
One research team member (E.B.) extracted data from included articles, and 2 authors (A.D. and J.Y.) checked the extracted information. We extracted data using a self-developed, pre-determined data extraction sheet adapted from a previous SR on the accuracy of scales, questionnaires, and hand symptom diagrams/maps for CTS diagnosis. J.M. was contacted if any uncertainty occurred in the data extraction process, and a consensus was established through discussion. We extracted the following information: authors, year of publication, country, conflicts of interest, study design, sample size, number of participants in the CTS and the control groups, characteristics of the participants (gender or sex, age, CTS duration, and severity), inclusion and exclusion criteria, the provocative maneuver, and its testing procedure, as well as its positive threshold criteria, reference standard, and any available information on the diagnostic accuracy properties.
Data Synthesis and Analysis
Where possible, we extracted Sn, Sp, PPV, NPV, +LR, and −LR of the provocative tests for CTS. If these variables were not reported directly in the articles, we calculated them based on the reported true positives and negatives and false positives and negatives. If enough information was reported, we created 2×2 contingency tables and calculated Sn, Sp, +LR, and −LR for each provocative test.
Sn is the ability of a test to identify people with truly positive results, and Sp is defined as the ability of a diagnostic test to truly identify people without a given condition (true negatives).12 For example, with a Sn of 0.70, a diagnostic test can correctly identify 70% of the persons with a disease and misses 30% of them. With a Sp of 0.70, a diagnostic test correctly identifies 70% of persons who do NOT have a disease and falsely labels 30% of healthy people as having a disease. We calculated Sn as true positive/ (true positive + false negative) and Sp as true negative/ (true negative + false positive).12
Likelihood ratios are the only diagnostic properties that are not affected by the prevalence of the condition (pretest probability) and are valuable tools in the clinical decision-making process.13 We calculated + LR as Sn/ (1-Sp) and −LR as (1-Sn)/Sp. Positive likelihood ratios > 10 and −LRs < 0.10 indicate the highest diagnostic accuracies.14 Positive likelihood ratios < 5 and −LRs > 0.5 indicate poor diagnostic accuracy and the limited ability of a diagnostic test to be impactful in clinical decision-making.14
Lastly, the diagnostic odds ratio is a measure of the possibility of a diagnosis, combining both Sn and Sp into 1 value. The odds ratio can range from 1 to infinity, with 1 equal to 0 diagnostic odds and higher values corresponding to a higher possibility of a given diagnosis.15
Meta-Analyses
We ran a meta-analysis on studies when data were available (or could be calculated) on the true positive, false positive, true negative, and false negative values of the included participants. We used MetaDTA software (v2.01) to perform the meta-analysis (https://crsu.shinyapps.io/dta_ma/).16,17 The MetaDTA software uses the R statistical software and runs a bivariate random-effects model, considering the possible correlations between Sn and Sp.16 For diagnostic test accuracy studies, bivariate models are increasingly recommended as the standard method of meta-analysis, as they are sophisticated enough to capture the complexity of the generally inversed Sn and Sp.18 Furthermore, we did not perform a heterogeneity analysis, since for meta-analysis of studies of diagnostic test accuracy, a high heterogeneity is always assumed as a rule of thumb. This is due to the variation in the tests’ methodologies and the reference standards and could be influenced by a threshold effect, which leads to generally high heterogeneity.18,19 To tackle this, we performed a random-effects model, which is the recommended method when a high heterogeneity is assumed.18
We estimated the pooled Sn, Sp, +LR, −LR, diagnostic odds ratio, and their associated 95% CIs for the Phalen test and the Tinel sign. We did not do a meta-analysis of the other provocative tests for CTS when fewer than 4 studies were available to avoid any bias introduced by the correlation between Sn and Sp and to produce reliable estimates of the diagnostic accuracies.18
For a graphical display of the findings of the meta-analysis of diagnostic test accuracy studies, 2 methods are recommended by the Cochrane Handbook20 and an extension of PRISMA.10 We incorporated both methods, which were: (1) Forest plots of the individual study results and meta-analysis pooled results for Sp and Sn separately and (2) Summary Receiver Operating Characteristic (SROC) plots of the global summary of the Phalen test and the Tinel sign. For the SROC plots, we used the quality assessment-enhanced method suggested by Patel et al.17 This method provides better visual feedback of the QUADAS-2 risk of bias (ROB) appraisal incorporated markers of study ROB into the SROC plots. Each data point on the SROC plot demonstrates the relationship between true positive and false positive rates in a single study.
Assessment of ROB and Applicability Concerns
Two authors (A.D. and J.Y.) independently rated the ROB and the applicability concerns of the included studies. If any disagreements occurred, a third author (the most senior 1, J.M.) was reached, and a consensus was achieved with discussion. We used the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool to assess ROB and applicability concerns.21 QUADAS-2 tool rates the ROB of the studies in 4 domains: (1) Patient selection: Prior testing, presentation, the intended use of index test and setting; (2) index test: How it was conducted and interpreted using a pre-specified threshold; (3) reference standard: Its likeliness to correctly identify the patients, and if the results were interpreted without the knowledge of the index test; (4) flow and timing: If there was an appropriate interval between index and reference test, and if the patients all received the same reference standards and were included in the analysis.21 Applicability concerns are rated in the same domains, except for flow and timing.21
For each domain, the signaling questions can be rated as low, unclear, or high ROB or applicability concerns.21 To generate an overall rating of ROB and applicability concerns, we rated the overall ROB as low if a study had low ROB in all 4 domains. Similarly, if a study had low concerns regarding applicability in all 3 domains, we rated that study as having “low applicability concerns.” On the contrary, studies with high or unclear ratings in any domain (even 1) were rated as having a high ROB or applicability concerns.21
Role of the Funding Source
The funders played no role in this study’s design, conduct, and reporting.
Results
Study Selection
We identified 5555 citations by electronic database search. When the duplicates were removed, we screened 4052 titles and abstracts, of which 161 articles were eligible for full-text screening. At last, 31 articles met the inclusion criteria of this SR as presented in the PRISMA flow chart (Suppl. Appendix B). The κ agreement of the reviewers in the screening of titles and abstracts was 0.70 (95% CI = 0.66–0.74; SE = 0.02).
Characteristics of Studies
A thorough description of the study characteristics, including authors, year, study design, country, number of participants and hands with CTS, diagnostic tool, and reference standards, is presented in Table 1. Most of the included studies (n = 28) had prospective cross-sectional study designs, with only 3 having retrospective cross-sectional study designs.22–24 The studies were conducted in Brazil, Canada, Columbia, Egypt, France, India, Israel, Italy, Serbia, Spain, Turkey, the UK, and the USA. All studies were published in English, except for the study by Amo et al, which was published in Spanish,25 and the study by Yilmaz et al, which was published in Turkish.26 We translated these studies using Google translate and invited native speakers to verify the extracted information.
Table 1.
Study Characteristicsa
| Author (Year), Study Design | Country | N-Individuals | N-Hands | N-CTS | Provocative Test | Reference Standard | ROB |
|---|---|---|---|---|---|---|---|
| Amo et al25 (1998), Prospective cross-sectional | Spain | 57 | 100 | NR | Tinel, Phalen | NCS | Unclear |
| Bilkis et al 27 (2012), Prospective cross-sectional | USA | 37 | 66 | 46 | Modified Phalen, Phalen | NCS | Unclear |
| Blok et al49 (2013), Prospective cross-sectional | USA | 41 | NR | 31 | Scratch-collapse test | NCS | Unclear |
| Buch-Jaeger & Foucher45 (1994), Prospective cross-sectional | France | 112 | 172 | 68 | Phalen, Tinel, Gilliatt | NCS | Unclear |
| Dale et al29 (2011), Prospective cross-sectional | USA | 1108 | 2216 | 35 | Tinel, Phalen | Modified Katz Hand Diagram; NCS; The Consensus Criteria CTS Case Definition |
High |
| Denham et al 30 (2015), Prospective cross-sectional | USA | 18 | 30 | 30 | Phalen, ULTT II | Diagnosis of CTS by physical exam, EMG, NCS | High |
| Franzblau et al 31 (1993), Prospective cross-sectional | USA | 130 | 260 | Tinel, Phalen | EDX; EDX+ surveillance symptom definitions for CTS; Physical examination + surveillance symptom definitions for CTS | High | |
| de Jesus Filho et al24 (2014), Retrospective cross-sectional | Brazil | 56 | 70 | 70 | Tinel, Durkan, Phalen | EMG; Ultrasound | High |
| Hansen et al32 (2004), Prospective cross-sectional | USA | 142 | NR | 95 | Flick, Tinel, Phalen | NCS | High |
| Heller et al33 (1986), Prospective cross-sectional | Israel | 60 | 80 | 58 | Phalen, Tinel | EMG | Unclear |
| Karl et al53 (2001), Prospective cross-sectional | USA | 96 | 96 | 51 | Lumbrical Provocation test | EDX; Katz hand diagrams | Unclear |
| Katz et al23 (1990), Retrospective cross-sectional | USA | 110 | 220 | 44 | Tinel, Phalen | NCS | High |
| Kaul et al52 (2000), Prospective cross-sectional | USA | 112 | NR | 58 | Tethered median nerve stress test | NCS | High |
| Kaul et al47 (2001), Prospective cross-sectional | USA | 269 | 269 | 58 | CCT, PPT | EMG | High |
| Kuhlman et al34 (1997), Prospective cross-sectional | USA | 143 | 228 | 142 | Phalen, Hoffman-Tinel | NCS | High |
| Lajoie et al22 (2005), Retrospective cross-sectional | India | 81 | 162 | NR | Tinel, Phalen | Latent Class Analysis of provocative test and NCS | Unclear |
| MacDermid et al35 (1997), Prospective cross-sectional | Canada | 42 | 84 | 36 hands | Tinel, Phalen, Rev-Phalen, Tethered median nerve stress test |
EMG; Clinical examination | Low |
| Makanji et al50 (2013), Prospective Cohort | USA | 88 | NR | 65 | Scratch-collapse test | EMG & NCS | Unclear |
| Martic46 (2015), Prospective cross-sectional | Serbia | 181 | NR | 60 | History, clinical diagnosis, reflex activity, impaired sensation; Combination of muscle strength and trophic changes, reflex activity, impaired sensation, Bickeles, Tinel, and Flick | EMG | Unclear |
| Naranjo et al36 (2007), Prospective cross-sectional | Spain | 68 | 105 | 80 hands | Tinel, Phalen | US; NCS; Clinical history | Unclear |
| O’Gradaigh & Merry37 (2000), Prospective cross-sectional | UK | 105 | NR | 75 | Phalen, Tinel | NCS | Unclear |
| Raudino38 (2000), Prospective cross-sectional | Italy | 83 | 140 | 140 | Tinel, Phalen, Median nerve Stress test | EMG | Unclear |
| Sawaya & Sakr39 (2009), Prospective cross-sectional | Lebanon | 27 | 54 | 27 hands | Phalen | EMG & NCS | Unclear |
| Simon et al51 (2017), Prospective cross-sectional | USA | 40 | 40 | 32 | Scratch-collapse test | EMG | Unclear |
(Continued)
Supplementary Appendix C summarizes the included studies’ conflicts of interest (if declared). Participants’ characteristics, including their age, sex/gender, duration of CTS symptoms, inclusion and exclusion criteria, are presented in Supplementary Appendix D.
We identified the following provocative maneuvers for CTS diagnosis from the included clinical studies, in order of frequency: Phalen test (22 studies, 2906 patients), Tinel sign (20 studies, 3005 patients), Durkan test or carpal compression test (CCT, 5 studies, 609 patients), scratch collapse test (SCT, 3 studies, 167 patients), tethered median nerve stress test (3 studies, 237 patients), upper limb tension tests I & II (ULTT, 2 studies, 136 patients), Flick sign (1 study, 142 patients), Gilliatt test (1 study, 112 patients), lumbrical provocation test (1 study, 96 patients), modified Phalen test (MPT, 1 study, 37 patients), pressure provocative test (1 study, 269 patients), and reverse Phalen test (1 study, 42 patients). Table 2 describes the methodology and positive test criteria for these provocative maneuvers.
Table 2.
Description of Provocative Maneuvers for Carpal Tunnel Syndrome Diagnosis
| Diagnostic Test | Method | Positive Result Threshold |
|---|---|---|
| Carpal Compression test47,48 or Durkan test24,40,43 |
“Applying moderate pressure with both thumbs over the transverse carpal ligament. The patient’s wrist was in the neutral position with the forearm supinated.”47 “The subject’s hand was comfortably positioned on a table with the palm facing up. The footplate of the gauge was placed on the volar surface of the wrist, directly over the transverse carpal ligament, and 12–15 psi of pressure was applied for a 30-s period.”48 “Durkan test was performed using a calibrated piston (Gorge Medical, Hood River, OR) to apply 9 to 10 N/cm2 to the palm over the transverse carpal ligament.”40 |
If median-distribution paresthesia was induced within 30 s47 Reproduction of CTS symptoms within 30 s48 |
| Flick sign32 | “By asking the patient what they do with their hands and wrists when symptoms are most severe.”32 | If the patient demonstrates a flicking motion of the hands and wrists (like shaking down a thermometer) |
| Gilliatt test28 | “Was performed by inflating a blood pressure cuff around the arm beyond systemic pressure for 1 minute.”28 | If this caused paresthesia in the median nerve territory |
| Lumbrical Provocation Test53 | “Each patient was asked to make a fist for 1 minute”53 | If median-inclusive paresthesia was induced or exacerbated |
| Modified Phalen test27 | “The MPT places the hands as in Phalen test while performing sensory testing with a Semmes-Weinstein 2.83-unit monofilament applied perpendicular to the skin surface until it bends. The monofilament was applied to the palmar surface and lateral side of each finger’s distal phalanx 3 times.”27 | If the participant did not register the touch in any 1 or more fingers in a median nerve distribution |
| Phalen test22–43 | “The testing position for the Phalen test required participants to sit with a relaxed posture, with shoulders flexed to approximately 70° and elbows flexed to approximately 90°. Participants were then asked to actively assume a position of extreme but not forced wrist flexion for one minute.”30 “Phalen test was performed as originally described. Subjects were asked to hold their forearms upright, resting their elbows on the examination table and letting their wrists drop into flexion with gravity assistance”40 |
The onset or increase in numbness or paresthesia in the median nerve distribution within 60 s of holding the wrists in a position of fixed flexion40 |
| Pressure Provocative test47 | “A pressure cuff 1 inch wide was applied to the patient’s wrist. The patient’s arm was placed on a table in the supinated forearm position, wrist in neutral. The cuff was inflated to 50 mmHg. Direct pressure was then applied on the cuff over the median nerve to bring the sphygmomanometer reading to 150 mmHg. This pressure was sustained for 30 s.”47 | If median-distribution paresthesia was induced within 30 s and symptom relief when the pressure was removed |
| Reverse Phalen test35 | “Reverse Phalen was performed by placing the palms together and maintaining a position of full passive extension.”35 | If CTS symptoms reproduced after holding the position for 60 s |
| Scratch-Collapse test49–51 | “The examiner applies bilateral shoulder adduction / internal rotation to the forearms and the patient tries to resist the examiner’s force; Next, the examiner ‘scratches or swipes with the fingertips over the area of the transverse carpal ligament, where the median nerve is potentially compressed; and Immediately afterwards Step 1 is repeated.”49 | If momentary loss of the patient’s external resistance tone is observed, in other words the patient’s arm collapses against the resistance |
| Tinel sign22–26,28,29,31–33,35–38, 40–42,46 or Hoffman-Tinel34 |
“Tinel test was performed by a reflex hammer to percuss over the palm from the proximal palmar crease to the distal wrist.”35 | If percussion over the median nerve at the wrist produced paresthesia in the median nerve distribution40 |
| Tethered median nerve stress test35,38,62 | “The median nerve was placed on stretch by passively hyperextending the supinated wrist and distal interphalangeal joint of the index finger.”38 | If proximal volar forearm pain was produced38,62 |
| Upper Limb Tension Test I & IIa30,54 | ULTT IIa: “The subjects were asked to lay supine and relaxed. The therapist first depressed the shoulder girdle, while simultaneously abducting the humerus to approximately 10°, fully extending the elbow, laterally rotating the humerus, and extending the wrist, fingers, and thumb. The position was held for one minute, and participants were then asked to describe any sensory changes in the tested limb.”30 ULTT I: “Participants lay supine without a pillow, arms along the body, and legs straight. Tests were carried out slowly, and participants were instructed to indicate the point at which it was too uncomfortable to continue with the movement (point of pain tolerance). Angle measurements were then taken at this point. The total time for each test was always under 1 minute, but there was no standardization of the movement time. Once the test was ended, the location and nature of the sensory response was marked on a body chart. The starting position for ULNT1 was 90 abduction and 90 external rotations of the shoulder, 90 elbow flexion, forearms supination, maximum extension of wrist and fingers, and abduction of the thumb. One of the physiotherapist’s hands was placed on the scapula to prevent elevation, the other hand-maintained finger abduction. The elbow was then slowly extended until the point of pain tolerance, and the elbow angle was measured.”54 |
If the participant reported pain, numbness, or tingling along the median nerve distribution.30 “Was graded according to Wainner criteria, and symptoms were located as proposed by Lohkamp and Small.”54 |
Risk of Bias and Applicability Concerns
Overall, the ROB and applicability concerns of the included studies were low or unclear in 20 of the studies. Eleven studies were at high ROB or applicability concerns in at least 1 domain. The “flow and timing” domain of the ROB assessment was unclear in 18 studies. Furthermore, the “reference standard” domain was rated as having a ROB in 23 studies, as studies did not consistently report the reference standards test procedures.
For applicability concerns, the domain with the most “applicability concerns” rating (n = 7) was the patient selection domain. Most of the studies (n = 19) had no concerns regarding applicability in the “patient selection” and “reference standard” domains. The ROB and applicability concerns are presented in Figure 1.
Figure 1.

Risk of bias and applicability concerns
Table 1.
Continued
| Author (Year), Study Design | Country | N-Individuals | N-Hands | N-CTS | Provocative Test | Reference Standard | ROB |
|---|---|---|---|---|---|---|---|
| Szabo et al40 (1999), Prospective cross-sectional | USA | CTS = 87, other diagnoses of UE = 90 | 100 | 50 (87 hands) | Phalen, Tinel, Durkan | NCS | Unclear |
| Trillos et al54 (2016), Prospective cross-sectional | Colombia | 118 | 230 | 186 | ULTT I | NCS | Low |
| Wainner et al48 (2000), Prospective cross-sectional | USA | 52 | 55 | 25 | CCT with Durkan gauge | NCS | High |
| Walters & Rice41 (2002), Prospective cross-sectional | USA | 55 | 77 | NR | Phalen, Tinel | NCS | High |
| Yilmaz et al26 (2002), Prospective cross-sectional | Turkey | 188 | 346 | NR | Phalen, Tinel | EMG | Unclear |
| Zaher et al42 (2012), Prospective cross-sectional | Egypt | 52 | 52 | 52 | Phalen, Tinel | EDX; MRI; US | Unclear |
| Zhang et al43 (2020), Prospective cross-sectional | USA | 55 | 85 | 76 | Phalen, Tinel, Durkan | EDX | Low |
CCT = carpal compression test; EDS = electrodiagnosis; EMG = electromyography; HSD = hand symptom diagram; MPT = modified Phalen test; MRI = magnetic resonance imaging; NCS = nerve conduction studies; PPT = pressure provocative test; ULLT = upper limb tension test; US = ultrasound.
Diagnostic Accuracy of the Phalen Test and Variations for CTS Diagnosis
The diagnostic accuracy of the Phalen test was assessed in 22 studies22–43 with 2906 patients (Suppl. Appendix E). The methodology was consistent across the included studies and performed according to the original method described by Phalen, which is explained in Table 2.44 The Sn ranged from 0.1229 to 0.92,22 and the Sp ranged from 0.3036 to 0.95.25 The meta-analysis of 7 studies,27,32–34,41,43,45 (604 patients), revealed pooled Sn of 0.57 (95% CI = 0.44–0.68), pooled Sp of 0.67 (95% CI = 0.52–0.79), pooled +LR of 1.71 (95% CI = 1.18–2.50), pooled −LR of 0.65 (95% CI = 0.50–0.84), and pooled diagnostic odds ratio of 2.65 (95% CI = 1.56–4.80). The SROC and forest plots of the Phalen test are presented in Figure 2. Only 1 study assessed the diagnostic accuracy of the Reverse Phalen test, which demonstrated good Sn (0.69) and excellent Sp (0.96).35
Figure 2.
Phalen test meta-analyses summary receiver operating characteristic (SROC) and forest plots
Diagnostic Accuracy of the Tinel Sign for CTS Diagnosis
The Tinel sign was assessed in 20 studies with 3005 patients.22–26,28,29,31–33,35–38,40–42,46 One study referred to this test as “Hoffman-Tinel”,34 but the methodology was consistent across all the studies, as summarized in Table 2. The Sn ranged from 0.1729 to 0.97,22 and the Sp ranged from 0.4036 to 0.92.35 The meta-analysis of 7 studies,32–34,41,43,45,46 (748 patients), indicated pooled Sn of 0.45 (95% CI = 0.34–0.57), pooled Sp of 0.78 (95% CI = 0.60–0.89), pooled +LR of 2.10 (95% CI = 1.16–3.83), pooled −LR of 0.67 (95% CI = 0.56–0.76), and pooled diagnostic odds ratio of 3.01 (1.40–6.47). Supplementary Appendix F summarizes the diagnostic accuracies for the Tinel sign, and Figure 3 depicts the SROC and the forest plots of Sn and Sp of this test.
Figure 3.
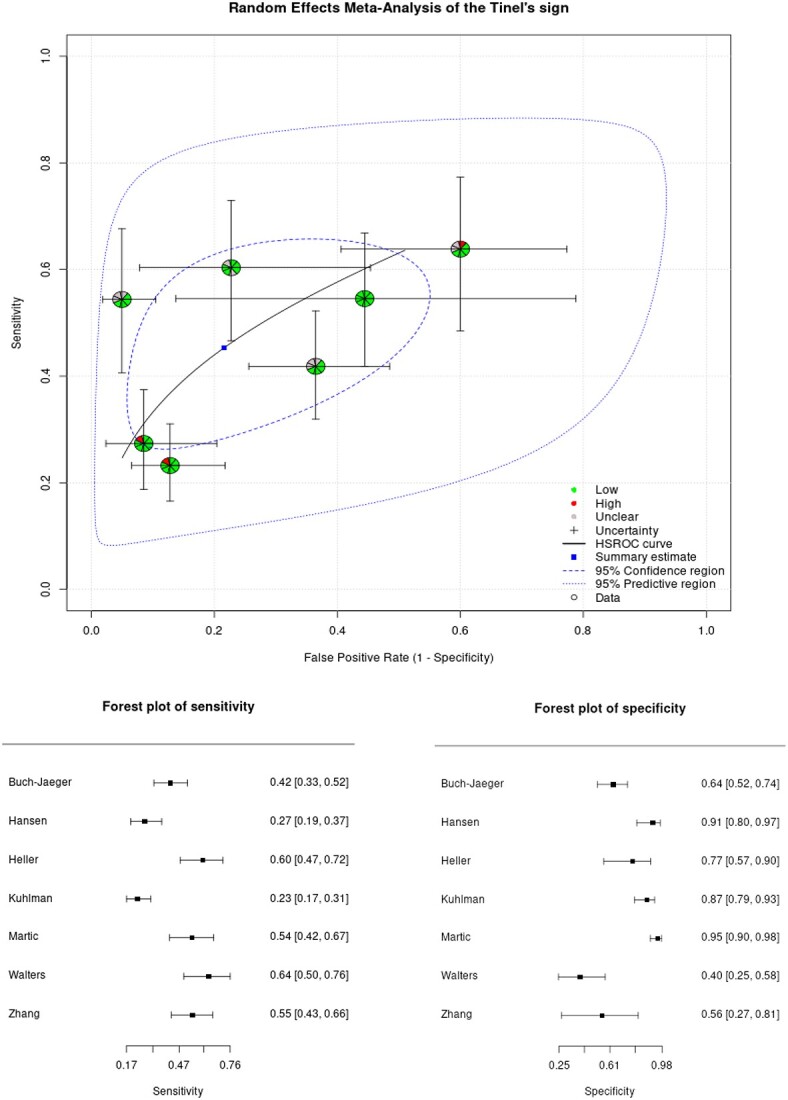
Tinel sign meta-analyses summary receiver operating characteristic (SROC) and forest plots
Diagnostic Accuracy of the Durkan Test for CTS Diagnosis
The diagnostic accuracy of the Durkan test (also known as the CCT or McMurtry sign or median nerve compression test) was assessed in 5 studies. Two of the 5 studies called this CCT47,48 and had the same test methodology as the Durkan test, where the pressure on the median nerve was applied at the transverse carpal ligament, either by the therapist’s thumbs, a gauge, or a calibrated piston.24,40,43 In all cases, the test was positive if symptoms were provoked in the median innervated territory within 30 seconds.24,40,43 This is further described in Table 2. For the Durkan test, Sn ranged from 0.3648 to 0.86,24 Sp ranged from 0.3343 to 0.62,47 +LR ranged from 0.8348 to 1.62,40 and −LR ranged from 0.2440 to 1.12.48 Diagnostic accuracy of the Durkan test is summarized in Table 3.
Table 3.
Diagnostic Accuracy of Other Provocative Tests for CTS Diagnosisa
|
Study
[Author (Year)] |
Sensitivity | Specificity | PPV | NPV | +LR | −LR | ROB |
|---|---|---|---|---|---|---|---|
| Durkan test | |||||||
| de Jesus Filho et al24 (2014) | 0.86 | NR | NR | NR | NR | NR | High |
| Kaul et al47 (2001) (CCT) | 0.53 | 0.62 | 0.67 | 0.47 | 1.39b | 0.76b | High |
| Szabo et al40 (1999) | 0.89 | 0.45 | 0.22 | 0.96 | 1.62b | 0.24b | Unclear |
| Wainner et al48 (2000) (CCT) | 0.36 | 0.57 | 0.84 | 1.12 | 0.83b | 1.12b | High |
| Zhang et al43 (2020) | 0.78 | 0.33 | 0.90 | 0.15 | 1.16b | 0.66b | Low |
| Flick test | |||||||
| Hansen et al32 (2004) | 0.37 | 0.74 | 0.74 | 0.37 | 1.42b | 0.85b | High |
| Gilliatt test | |||||||
| Buch-Jaeger & Foucher45 (1994) | 0.52 | 0.36 | 0.53 | 0.52 | 0.81b | 1.33b | Unclear |
| Lumbrical Provocation test | |||||||
| Karl et al53 (2001) | 0.37 | 0.71 | 0.59 | 0.50 | 1.27b | 0.88b | Unclear |
| Pressure Provocative test | |||||||
| Kaul et al47 (2001) | 0.55 | 0.68 | 0.70 | 0.53 | 1.71b | 0.66b | High |
| Scratch Collapse test | |||||||
| Blok et al49 (2013) | 0.32 | NR | NR | NR | NR | NR | Unclear |
| Makanji et al50 (2013) | 0.31 | 0.61 | 0.71 | 0.25 | 0.79b | 1.13b | Unclear |
| Simon et al51 (2017) | 0.24 | 0.62 | 0.75 | 0.18 | 0.75b | 1.22b | Unclear |
| Tethered Median Nerve Stress test | |||||||
| Kaul et al52 (2000) | 0.50 | 0.59 | 0.62 | 0.47 | 1.21b | 0.85b | High |
| MacDermid et al35 (1997) | 0.52 | 0.92 | NR | NR | 6.50b | 0.52b | Low |
| Raudino38 (2000) | 0.43 | NR | NR | NR | NR | NR | Unclear |
| Upper Limb Tension test | |||||||
| Denham et al30 (2015) | 0.73 | 0.50 | 0.98 | 0.06 | 1.46b | 0.54b | High |
| Trillos et al54 (2016) | 0.93 | 0.07 | 0.87 | 0.12 | 1.00 | 1.05 | Low |
CCT = carpal compression test; +LR = positive likelihood ratio; −LR: = negative likelihood ratio; NPV = negative predictive value; NR = not reported; PPV = positive predictive value.
Values calculated by the authors of this study.
One study combined Durkan test with the Phalen test and described it as the Phdurkan test which “was performed by manual compression of the carpal tunnel with the examiner’s index and middle fingers and flexion of the wrist with the examiner’s thumb and recorded as positive if associated with reproduction of distal paresthesia in the median nerve distribution.”43 Phdurkan test resulted in a high Sn of 0.84, but a low Sp of 0.11.43
Diagnostic Accuracy of Other Provocative Maneuvers for CTS Diagnosis
The diagnostic accuracy of other provocative maneuvers for CTS diagnosis, including Flick sign, SCT, tethered median nerve stress test, ULTT I and II, Gilliatt test, lumbrical provocation test, and pressure provocative test, was assessed in a fewer number of studies (n ≤ 3). The diagnostic accuracy properties of these tests are summarized in Table 3. In summary, SCT had consistently low Sn (0.32, 0.31, and 0.24) and Sp (0.61, 0.62) in 3 studies (167 patients) with unclear ROB.49–51 The tethered median nerve stress test consistently demonstrated low Sn (0.50, 0.52. 0.43)35,38,52 and high Sp of 0.92 in 1 study with low ROB.35 Other provocative maneuvers were assessed in fewer than 2 clinical studies and were at high ROB.28,30,32,47,53
Discussion
This SR summarizes 31 studies with highly variable qualities and results suggesting low-to-moderate accuracy for 12 provocative tests when used individually to diagnose CTS. Meta-analyses of 8 studies that addressed either the Phalen or Tinel test had wide CIs but suggested that the Phalen test has moderate Sn and Sp, whereas the Tinel test has low Sn and high Sp.
We found different diagnostic accuracy results for the provocative maneuvers compared with sensorimotor tests. In our previous SR of sensorimotor tests, we had half the number of studies included compared with this SR (16 sensorimotor vs 31 provocative maneuvers studies), and most of the sensorimotor studies had high ROB; therefore, making it impossible to make a firm conclusion about the diagnostic accuracy of sensorimotor tests for CTS diagnosis.8 In our SR of sensorimotor tests, we concluded that “among the included studies, none of the sensory or motor tests had consistently high diagnostic accuracy properties reported by high-quality evidence. Confirming the value of a single sensory or motor test for CTS diagnosis is pending future robust research.”8 This was different from the results of this study, where higher Sn and Sp values were reported for the Phalen test and Tinel sign.
We believe the differences observed in the diagnostic accuracy values of the provocative maneuvers compared with sensorimotor tests could be due to (1) different testing procedures and (2) they are testing different things, the provocation of the nerve and the other the effects of nerve injury. With provocative maneuvers, some sort of pressure (either with positioning, eg, the Phalen test, or with applying external pressure, eg, CCT) is applied in the carpal tunnel, which decreases the space of the tunnel.55 This decreased space in the carpal tunnel increases the pressure on the median nerve, hence the provocation of CTS symptoms.35,43 Whereas with sensorimotor testing for CTS, we test the skin area or muscles innervated by the median nerve and measure the loss in sensation, strength, or dexterity.31,35 In addition, sensory and strength measures may be good for examining sensory and strength loss, but these could result from a number of conditions, not just CTS. Therefore, they may be less valuable for confirming a CTS diagnosis. These differences in testing procedure further suggest the importance of including provocative maneuvers and sensorimotor tests in clinical practice to confirm the diagnosis of CTS.
Comparing our findings with the scales, diagnostic questionnaires, and hand symptom diagrams for CTS diagnosis from our previous SR, we note that scales, questionnaires, and hand symptom diagrams could play a critical role in diagnosing CTS.7 For example, the Kamath and Stothard Questionnaire (KSQ) had consistently high diagnostic accuracy values in several studies.2,56,57 These high accuracy values were further improved when combined with provocative maneuvers.7 For instance, Bland et al assessed the accuracy of the KSQ combined with the CTS-6 scale (a combination of sensorimotor tests, the Phalen test and Tinel sign), which led to an excellent Sn of 0.95.58 All of these confirm our conclusion that a combined testing approach, including history taking, sensorimotor testing, subjective assessment, and provocative maneuvers are the most definitive approaches for clinical diagnosis of CTS.
We did not include studies that had participants that were asymptomatic (healthy) as their comparators. This resulted in excluding 53 articles in the overall 3 SRs. While acknowledging the amount of information not considered in this SR by making this decision, we believe that by doing so, we provide a synthesis of studies that are the most similar to a clinical setting: A clinician would not see clients that were asymptomatic in daily practice. Furthermore, it has been proven statistically that including these participants who are healthy would inflate the diagnostic accuracy values and shift them toward better outcomes,12 which could introduce a measurement bias. When assessing any diagnostic tool in a sample of healthy people, the test would be 100% specific, meaning that nobody will be diagnosed as “sick”.59
Our results align with the clinical recommendations made by the most recent Academy of Hand and Upper Extremity Physical Therapy and the Academy of Orthopedic Physical Therapy of the American Physical Therapy Association clinical practice guidelines.60 Based on this guideline, “in those with suspected CTS, clinicians should use the Katz hand diagram, Phalen test, Tinel sign, and carpal compression test to determine the likelihood of CTS and interpret examination results in the context of all clinical exam findings.”60 Furthermore, although not the focus of the current study, but this guideline also suggested that the Phalen test can not only be used as a diagnostic method as suggested in this current study, but it can also be used as a responsiveness outcome measure to track change over time.60
Comparing our study to Núñez de Arenas-Arroyo et al,61 they reported higher Sn and Sp for the Phalen test, higher Sn and similar Sp for the Tinel sign. We believe these differences are due to the several methodological differences between the 2 SRs. First, Núñez de Arenas-Arroyo et al61 limited their reference standard test to electrodiagnosis, whereas we included studies with any type of reference standards used. Furthermore, as explained before, we did not include studies with asymptomatic participants as their comparators, as this has been statistically proven to artificially inflate the diagnostic accuracies.59 We suspect that the higher reported diagnostic accuracies could be attributed to the differences in the patients’ characteristics. Our study differed from Núñez de Arenas-Arroyo et al61 since they addressed the most common provocative maneuvers and not all the tests. Therefore, we believe the current SR and the other 2 published SRs on assessing the accuracy of the questionnaires, scales, hand symptom diagrams/maps,7 and sensorimotor tests8 are the most comprehensive updates of the literature and should be considered when developing the future clinical practice guidelines.
Study Limitations
The largest limitation in our work was related to deficiencies in the evidence, which included limited studies for many of the 12 identified tests. Even though we developed our search strategy in consultation with a health science librarian, we might have missed studies. Furthermore, a potential publication bias exists because we only included published articles, and we did not search the gray literature.
Although we reported promising results for some provocative maneuvers, one must be cautious when interpreting our results because some studies had unclear or high ROB and applicability concerns. To tackle this, we recommend future studies comply rigorously with the well-established recommendation guidelines and design and implement low ROB and high-quality studies. Furthermore, given the COVID-19 pandemic and the increased emphasis on the online diagnosis and management of CTS, we recommend future studies to assess the validity, reliability, and diagnostic accuracy of these clinical tests in online settings to produce clinically relevant evidence.
Clinical Implications
Accurate diagnosis of persons with suspected CTS symptoms seems warranted to improve treatment outcomes and individual patient care. Consequently, the efficiency of interventions for CTS management can be maximized by making a correct and timely diagnosis. To achieve this, clinicians must adhere to high-quality evidence for implementing clinical diagnostic tests in clinical settings. The provocative maneuvers studied in this review did not yield consistently high diagnostic accuracies; therefore, we do not recommend any single test for diagnosing CTS. Combining multiple tests, including history taking, sensorimotor testing, the Phalen test, and the Tinel sign, might optimize diagnostic accuracy.7 Studies examining different tests combinations are needed to verify the ideal combination of tests, balancing accuracy, and brevity.
Conclusion
This study synthesized 31 studies on the diagnostic accuracy of the provocative maneuvers in the differential diagnosis of CTS. Studies with moderate ROB and highly variable results suggest low-to-moderate accuracy for 12 provocative tests when used individually to diagnose carpal tunnel syndrome. Meta-analyses of 8 studies suggest that the Phalen test has moderate Sn and Sp, whereas the Tinel test has low Sn and high Sp.
Supplementary Material
Contributor Information
Armaghan Dabbagh, Faculty of Health Sciences, School of Physical Therapy, Western University, London, Ontario, Canada.
Joy C MacDermid, Faculty of Health Sciences, School of Physical Therapy, Western University, London, Ontario, Canada; School of Rehabilitation Science, McMaster University, Hamilton, Ontario, Canada; Roth McFarlane Hand and Upper Limb Centre, St. Joseph’s Hospital, London, Ontario, Canada.
Joshua Yong, Occupational Therapy Department, Sengkang General Hospital, , Singapore.
Tara L Packham, School of Rehabilitation Science, McMaster University, Hamilton, Ontario, Canada.
Ruby Grewal, Faculty of Health Sciences, School of Physical Therapy, Western University, London, Ontario, Canada; Department of Surgery, Western University, London, Ontario, Canada.
Eleni C Boutsikari, Department of Hygiene, Epidemiology and Medical Statistics, National and Kapodistrian University of Athens, Athens, Greece.
Author Contributions
Concept/idea/research design: A. Dabbagh, J.C. MacDermid, J. Yong, T.L. Packham
Writing: A. Dabbagh, J.C. MacDermid, T.L. Packham, R. Grewal
Data collection: A. Dabbagh, J. Yong, R. Grewal, E.C. Boutsikari
Data analysis: A. Dabbagh, J. Yong, E.C. Boutsikari
Project management: A. Dabbagh, J.C. MacDermid
Fund procurement: J.C. MacDermid
Providing participants: R. Grewal
Providing facilities/equipment: J.C. MacDermid
Consultation (including review of manuscript before submitting): J.C. MacDermid, J. Yong, R. Grewal
Funding
J. MacDermid was supported by a grant from the Canada Research Chair in Musculoskeletal Health Outcomes and Knowledge Translation and the Dr James Roth Chair in Musculoskeletal Measurement and Knowledge Translation. Her work is supported by a foundation grant from the Canadian Institutes of Health Research (#167284). C. Ziebart and R. Furtado were supported by the CIHR Doctoral Award. A. Dabbagh was supported by the Ontario Graduate Scholarship.
Systematic Review Registration
This review was registered in PROSPERO (CRD42018109031).
Data Availability Statement
Any required links or identifiers for data are present in the manuscript.
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
References
- 1. Atroshi I, Gummesson C, Johnson R, Ornstein E, Ranstem J, Rosen I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;281:153–158. 10.3928/01477447-20130624-02. [DOI] [PubMed] [Google Scholar]
- 2. Wang WL, Buterbaugh K, Kadow TR, Goitz RJ, Fowler JR. A prospective comparison of diagnostic tools for the diagnosis of carpal tunnel syndrome. J Hand Surg. 2018;43:833–836.e2. 10.1016/j.jhsa.2018.05.022. [DOI] [PubMed] [Google Scholar]
- 3. Dale AM, Harris-Adamson C, Rempel D, et al. Prevalence and incidence of carpal tunnel syndrome in US working populations: pooled analysis of six prospective studies. Scand J Work Environ Health. 2013;39:495–505. 10.5271/sjweh.3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shi Q, Bobos P, Lalone EA, Warren L, MacDermid JC. Comparison of the short-term and long-term effects of surgery and nonsurgical intervention in treating carpal tunnel syndrome: a systematic review and meta-analysis. Hand (N Y). 2020;15:13–22. 10.1177/1558944718787892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. American Academy of Orthopaedic Surgeons . Management of Carpal Tunnel Syndrome Evidence-Based Clinical Practice Guideline. 2016. Accessed January 21, 2022. https://www.aaos.org/globalassets/quality-and-practice-resources/carpal-tunnel/cts_cpg_4-25-19.pdf. [DOI] [PubMed]
- 6. MacDermid JC, Wessel J. Clinical diagnosis of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004;17:309–319. 10.1197/j.jht.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 7. Dabbagh A, MacDermid JC, Yong J, Macedo LG, Packham TL. Diagnosing carpal tunnel syndrome: diagnostic test accuracy of scales, questionnaires, and hand symptom diagrams—a systematic review. J Orthop Sports Phys Ther. 2020;50:622–631. 10.2519/jospt.2020.9599. [DOI] [PubMed] [Google Scholar]
- 8. Dabbagh A, MacDermid JC, Yong J, Packham TL, Macedo LG, Ghodrati M. Diagnostic accuracy of sensory and motor tests for the diagnosis of carpal tunnel syndrome: a systematic review. BMC Musculoskelet Disord. 2021;22:337. 10.1186/s12891-021-04202-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dabbagh A, Ziebart C, MacDermid JC. Accuracy of diagnostic clinical tests and questionnaires in screening for carpal tunnel syndrome among workers—a systematic review. J Hand Ther. 2021;34:179–193. 10.1016/j.jht.2021.04.003. [DOI] [PubMed] [Google Scholar]
- 10. McInnes MDF, Moher D, Thombs BD, et al. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies. JAMA. 2018;319:388. 10.1001/jama.2017.19163. [DOI] [PubMed] [Google Scholar]
- 11. Landis RJ, Koch G. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33:363–374. 10.2307/2529786. [DOI] [PubMed] [Google Scholar]
- 12. Trevethan R. Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Front Public Health. 2017;5:1–7. 10.3389/fpubh.2017.00307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sedighi I. Interpretation of diagnostic tests: likelihood ratio vs. predictive value. Iran J Pediatr. 2013;23:717. [PMC free article] [PubMed] [Google Scholar]
- 14. Whiting P, Martin RM, Ben-Shlomo Y, Gunnell D, Sterne JAC. How to apply the results of a research paper on diagnosis to your patient. JRSM Short Rep. 2013;4:1–9. 10.1258/shorts.2012.012089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bland JM. Statistics notes: the odds ratio. BMJ. 2000;320:1468–1468. 10.1136/bmj.320.7247.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Freeman SC, Kerby CR, Patel A, Cooper NJ, Quinn T, Sutton AJ. Development of an interactive web-based tool to conduct and interrogate meta-analysis of diagnostic test accuracy studies: MetaDTA. BMC Med Res Methodol. 2019;19:1–11. 10.1186/s12874-019-0724-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Patel A, Cooper N, Freeman S, Sutton A. Graphical enhancements to summary receiver operating characteristic plots to facilitate the analysis and reporting of meta-analysis of diagnostic test accuracy data. Res Synth Methods. 2021;12:34–44. 10.1002/jrsm.1439. [DOI] [PubMed] [Google Scholar]
- 18. Kim KW, Lee J, Choi SH, Huh J, Park SH. A practical review for clinical researchers–part II. Statistical methods of meta-analysis. Korean J Radiol. 2015;16:1175–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Trikalinos TA, Balion CM, Coleman CI, et al. Chapter 8: meta-analysis of test performance when there is a “gold standard”. J Gen Intern Med. 2012;27:1–21. 10.1007/s11606-012-2029-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Macaskill P, Gatsonis C, Deeks JJ, Harbord RM, Takwoingi Y. Chapter 10: Analysing and presenting results. In: Deeks JJ, Bossuyt PM, Gatsonis C (eds.), Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 1.0. The Cochrane Collaboration, 2010.
- 21. Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 22. LaJoie AS, McCabe SJ, Thomas B, Edgell SE. Determining the sensitivity and specificity of common diagnostic tests for carpal tunnel syndrome using latent class analysis. Plast Reconstr Surg. 2005;116:502–507. 10.1097/01.prs.0000172894.21006.e2. [DOI] [PubMed] [Google Scholar]
- 23. Katz JN, Larson MG, Sabra A, et al. The carpal tunnel syndrome: diagnostic utility of the history and physical examination findings. Ann Intern Med. 1990;112:321–327. 10.7326/0003-4819-112-5-321. [DOI] [PubMed] [Google Scholar]
- 24. de Jesus Filho AG, do Nascimento BF, Amorim Mde C, RAS N, Loures Ede A, Moratelli L. Comparative study between physical examination, electroneuromyography and ultrasonography in diagnosing carpal tunnel syndrome. Rev Bras Ortop. 2014;49:446–451. 10.1016/j.rboe.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Amo C, Fernández-Gil S, Pérez-Fernández S, et al. Carpal tunnel syndrome. Clinical and neurophysiological correlation: review of 100 cases. Rev Neurol. 1998;27:490–493. [PubMed] [Google Scholar]
- 26. Yilmaz M, Karakurum G, Akilli Z, Gökalp N. Comparison of awakening from sleep with Phalen test and Tinel’s sign in patients with carpal tunnel syndrome. Artroplasti Artroskopik Cerrahi. 2002;13:10–14. [Google Scholar]
- 27. Bilkis S, Loveman DM, Eldridge JA, Ali SA, Kadir A, McConathy W. Modified Phalen’s test as an aid in diagnosing carpal tunnel syndrome. Arthritis Care Res (Hoboken). 2012;64:287–289. 10.1002/acr.20664. [DOI] [PubMed] [Google Scholar]
- 28. Buch-Jaeger N, Foucher G. Validity of clinical signs and provocative tests in carpal tunnel syndrome. Rev Chir Orthop Reparatrice Appar Mot. 1995;80:14–21. [PubMed] [Google Scholar]
- 29. Dale AM, Descatha A, Coomes J, Franzblau A, Evanoff B. Physical examination has a low yield in screening for carpal tunnel syndrome. Am J Ind Med. 2011;54:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Denham S, Lee J, Wilhite M, McGrady T, Booth B. Agreement between the upper limb tension test 2a and the Phalen test in the diagnosis of carpal tunnel syndrome. Orthopaedic Physical Therapy Practice. 2015;27:20–24. [Google Scholar]
- 31. Franzblau A, Werner R, Valle J, Johnston E. Workplace surveillance for carpal tunnel syndrome: a comparison of methods. J Occup Rehabil. 1993;3:1–14. [DOI] [PubMed] [Google Scholar]
- 32. Hansen PA, Micklesen P, Robinson LR. Clinical utility of the flick maneuver in diagnosing carpal tunnel syndrome. Am J Phys Med Rehabil. 2004;83:363–367. [DOI] [PubMed] [Google Scholar]
- 33. Heller L, Ring H, Costeff H, Solzi P. Evaluation of Tinel’s and Phalen’s signs in diagnosis of the carpal tunnel syndrome. Eur Neurol. 1986;25:40–42. [DOI] [PubMed] [Google Scholar]
- 34. Kuhlman KA, Hennessey WJ. Sensitivity and specificity of carpal tunnel syndrome signs. Am J Phys Med Rehabil. 1997;76:451–457. 10.1097/00002060-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 35. Macdermid JC, Kramer JF, McFarlane RM, Roth JH. Inter-rater agreement and accuracy of clinical tests used in diagnosis of carpal tunnel syndrome. Work. 1997;8:37–44. [DOI] [PubMed] [Google Scholar]
- 36. Naranjo A, Ojeda S, Mendoza D, Francisco F, Quevedo JC, Erausquin C. What is the diagnostic value of ultrasonography compared to physical evaluation in patients with idiopathic carpal tunnel syndrome? Clin Exp Rheumatol. 2007;25:853–859. [PubMed] [Google Scholar]
- 37. O’Gradaigh D, Merry P. A diagnostic algorithm for carpal tunnel syndrome based on Bayes’s theorem. Rheumatology. 2000;39:1040–1041. 10.1093/rheumatology/39.9.1040. [DOI] [PubMed] [Google Scholar]
- 38. Raudino F. Tethered median nerve stress test in the diagnosis of carpal tunnel syndrome. Electromyogr Clin Neurophysiol. 2000;40:57–60. [PubMed] [Google Scholar]
- 39. Sawaya RA, Sakr C. When is the Phalen’s test of diagnostic value: an electrophysiologic analysis? J Clin Neurophysiol. 2009;26:132–133. [DOI] [PubMed] [Google Scholar]
- 40. Szabo RM, Slater RR, Farver TB, Breger Stanton D, Sharman WK. The value of diagnostic testing in carpal tunnel syndrome. J Hand Surg. 1999;24:704–714. 10.1053/jhsu.1999.0704. [DOI] [PubMed] [Google Scholar]
- 41. Walters C, Rice V. An evaluation of provocative testing in the diagnosis of carpal tunnel syndrome. Mil Med. 2002;167:647–652. 10.1093/milmed/167.8.647. [DOI] [PubMed] [Google Scholar]
- 42. Zaher A, Mattar MA, Gomaa M. Value of contemporary investigation tools in management of carpal tunnel syndrome. Egypt J Neurol Psychiatr Neurosurg. 2012;49:375–380. [Google Scholar]
- 43. Zhang D, Chruscielski CM, Blazar P, Earp BE. Accuracy of provocative tests for carpal tunnel syndrome. J Hand Surg Glob Online. 2020;2:121–125. 10.1016/j.jhsg.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Phalen GS. The carpal-tunnel syndrome. J Bone Joint Surg. 1966;48-A:211–228. [PubMed] [Google Scholar]
- 45. BuchJaeger N, Foucher G. Correlation of clinical signs with nerve conduction tests in the diagnosis of carpal tunnel syndrome. J Hand Surg Br. 1994;19:720–724. [DOI] [PubMed] [Google Scholar]
- 46. Martic V. Concoradance of clinical and neurophysiologic diagnoses of carpal tunnel syndrome. Vojnosanit Pregl. 2015;72:247–250. [DOI] [PubMed] [Google Scholar]
- 47. Kaul MP, Pagel KJ, Wheatley MJ, Dryden JD. Carpal compression test and pressure provocative test in veterans with median-distribution paresthesias. Muscle Nerve. 2001;24:107–111. [DOI] [PubMed] [Google Scholar]
- 48. Wainner RS, Boninger ML, Balu G, Burdett R, Helkowski W. Durkan gauge and carpal compression test: accuracy and diagnostic test properties. J Orthop Sports Phys Ther. 2000;30:676–682. [DOI] [PubMed] [Google Scholar]
- 49. Blok RD, Becker SJE, Ring DC. Diagnosis of carpal tunnel syndrome: interobserver reliability of the blinded scratch-collapse test. J Hand Microsurg. 2014;6:5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Makanji HS, Becker SJE, Mudgal CS, Jupiter JB, Ring D. Evaluation of the scratch collapse test for the diagnosis of carpal tunnel syndrome. J Hand Surg. 2013;39:181–186. [DOI] [PubMed] [Google Scholar]
- 51. Simon J, Lutsky K, Maltenfort M, Beredjiklian PK. The accuracy of the scratch collapse test performed by blinded examiners on patients with suspected carpal tunnel syndrome assessed by Electrodiagnostic studies. J Hand Surg. 2017;42:386.e1–386.e5. [DOI] [PubMed] [Google Scholar]
- 52. Kaul R, Pagel KJ, Dryden JD. Lack of predictive power of the “tethered” in suspected carpal Ibnnel syndrome. Arch Phys Med Rehabil. 2000;81:348–350. [DOI] [PubMed] [Google Scholar]
- 53. Karl AI, Carney ML, Kaul MP. The lumbrical provocation test in subjects with median inclusive paresthesia. Arch Phys Med Rehabil. 2001;82:935–937. [DOI] [PubMed] [Google Scholar]
- 54. Trillos MC, Soto F, Briceno-Ayala L. Upper limb neurodynamic test 1 in patients with clinical diagnosis of carpal tunnel syndrome: a diagnostic accuracy study. J Hand Ther. 2017;3:333–338. [DOI] [PubMed] [Google Scholar]
- 55. Keir PJ, Bach JM, Hudes M, Rempel DM. Guidelines for wrist posture based on carpal tunnel pressure thresholds. Hum Factors. 2007;49:88–99. 10.1518/001872007779598127. [DOI] [PubMed] [Google Scholar]
- 56. Bridges MJ, Robertson DC, Chuck AJ. Predicting the result of nerve conduction tests in carpal tunnel syndrome using a questionnaire. Hand Surg. 2010;16:39–42. 10.1142/s0218810411005047. [DOI] [PubMed] [Google Scholar]
- 57. Kamath V, Stothard J. A clinical questionnaire for the diagnosis of carpal tunnel syndrome. J Hand Surg. 2003;28 B:455–459. 10.1016/S0266-7681(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 58. Bland JDPP, Weller P, Rudolfer S. Questionnaire tools for the diagnosis of carpal tunnel syndrome from the patient history. Muscle Nerve. 2011;44:757–762. 10.1002/mus.22158. [DOI] [PubMed] [Google Scholar]
- 59. Brenner H, Gefeller O. Variation of sensitivity, specificity, likelihood ratios and predictive values with disease prevalence. Stat Med. 1997;16:981–991. . [DOI] [PubMed] [Google Scholar]
- 60. Erickson M, Lawrence M, Jansen CWS, Coker D, Amadio P, Cleary C. Hand pain and sensory deficits: carpal tunnel syndrome. J Orthop Sports Phys Ther. 2019;49:CPG1–CPG85. 10.2519/jospt.2019.0301. [DOI] [PubMed] [Google Scholar]
- 61. Núñez de Arenas-Arroyo S, Cavero-Redondo I, Torres-Costoso A, Reina-Gutiérrez S, Guzmán-Pavón MJ, Martínez-Vizcaíno V. Accuracy of the most common provocation tests for diagnosing carpal tunnel syndrome: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2022;52:522–531. 10.2519/jospt.2022.10828. [DOI] [PubMed] [Google Scholar]
- 62. Kaul MP, Pagel KJ, Wheatley MJ, Dryden JD. Lack of predictive power of the “tethered” median stress test in suspected carpal tunnel syndrome. Arch Phys Med Rehabil. 2000;81:348–350. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Any required links or identifiers for data are present in the manuscript.



