ABSTRACT
The purpose of the research was to pool the intention to receive the COVID-19 vaccine and its health belief model (HBM)-based predictors, which is helpful for decision-makers and program managers around the globe. The relevant database was searched and Joanna Briggs Institute (JBI) appraisal checklist was used to evaluate the studies. I2 test and funnel plot was utilized to check heterogeneity and publication bias, respectively. DerSimonian and Laird random-effects model was used. The overall pooled intention to receive COVID-19 vaccine globally was 67.69%. Higher levels of perceived susceptibility (AOR = 1.85), perceived severity (AOR = 1.45), perceived benefits (AOR = 3.10), and cues to action (AOR = 3.40) positively predicted the intention; whereas high level of perceived barrier negatively predicted it (AOR = 0.53). Health beliefs influenced COVID-19 vaccine intention globally. This implies that individuals need sound health education and publicity about vaccines before vaccination.
KEYWORDS: COVID-19, predictors, vaccine, HBM, meta-analysis
Introduction
COVID-19 has spread at an alarming rate around the planet and has been officially declared by the World Health Organization (WHO) as a pandemic and public health emergency of international concern (PHEIC).1 Various approaches have been applied at the individual, environmental, and community levels to counter the spread of the COVID-19 pandemic, including Places where people gather, such as public transportation.2
When combined with appropriate testing, treatment, and existing precautions, the COVID-19 vaccination is the most effective and economical preventive and protective measure compared to other preventative and protective measures because it helps to minimize and lessen the burden of a pandemic.3 COVID-19 vaccine development began in many research centers, governments, and pharmaceutical companies shortly thereafter when the epidemic broke out.4
Furthermore, the pandemic itself and related regulatory measures such as social distancing and mobility restriction as well as adaptive behaviors to COVID-19 have substantially impacted the physical and mental health of the population and flattened the epidemic curve of COVID-19.5 In addition, the pandemic significantly limited access utilization of health care services6 and worsened the quality-of-life health outcomes, such as depression, psychological stress, and anxiety.7
High COVID-19 vaccination rates could be essential to prevent, mitigate, or manage the COVID-19 pandemic. Since the new pandemic, a total of 6 billion COVID-19 vaccines have been distributed globally to end this public health crisis. It showed that the trend of participants approved to receive the COVID-19 vaccine was because of concerns about its safety and efficacy. A 69.4% of people worldwide will have gotten at least one dose of vaccination by the end of January 2023. However, in Low income countries, vaccination coverage drops to just 26.4% of this total, leaving the remaining 75% of their people completely unprotected.8
In light of the pandemic crisis, the launch of the COVID-19 vaccine was a light of hope. However, accessing an immunization program and successfully conducting a herd immunization campaign is another thing.9
In addition, there are doubts regarding some functions of the COVID-19 vaccine: doubts regarding long-term safety and the call for usual deprescription, given the facts of SARS-CoV2 development and the emergence of hereditary variants.10 In addition to their significance and efficiency in combating pandemics, individuals have expressed fear and misunderstanding about COVID-19 vaccination programs.11 The guidelines for the COVID-19 vaccination program take part in an unrestricted task of COVID-19 vaccination to marked populations in specific countries. Some COVID-19 vaccination guidelines focus on health promotion, while others focus on inclusion.12
Effective vaccine development takes greater than 10 years, in the case of COVID-19 vaccines this period is ignored due to the pandemic morbidity, mortality, economic loss, and socio-cultural effect, 10 vaccines were developed and were being tested in clinical trials by June 2020. This unprecedented success is a major challenge in COVID-19 vaccine acceptance.8
There are different types of vaccines have been approved for marketing such as Pfizer-BioNTech, AstraZeneca, Janssen Ad26.COV2, Moderna mRNA-1273, Sinopharm, BBV152 COVAXIN, Nuvaxovid NVX-CoV2373 and Sinovac-CoronaVac vaccine. The application of vaccine was given to different age groups. Pfizer-BioNTech and Moderna mRNA-1273 are safe and effective for all individuals aged 6 months and above. On the other hand, only Nuvaxovid NVX-CoV2373 vaccine is given to individuals aged 12 and above, but the other vaccines are safe and effective for all individuals aged 18 and above.9 Intention to the COVID-19 vaccine can be defined as vaccine acceptability including desirability, willingness to be vaccinated, vaccine demand, and positive attitudes toward the given vaccine, which is contrasted to vaccine resistance, the refusal to be vaccinated.10
To lessen the weight of COVID-19 and to reduce the socio-monetary effect on the populace, governments implemented diverse protective strategies and enrolled the COVID-19 vaccine for the high-hazard population at the primary stage, presently vaccinating the whole populace at large, to determine the magnitude of this problem, understanding the desire to get the COVID-19 vaccine, as well as its health belief model (HBM)-based predictors are critical for the effectiveness of mass immunization and limiting the disease’s global spread.
Health Belief Model (HBM), can be used to understand the personal intention in health-related behaviors and had four dimensions. The first dimension is perceived susceptibility a person who had a perception of risk, or susceptibility of contracting a condition, second perceived severity, which relates to the seriousness of contracting a particular illness and the potential consequences that result, thirdly perceived benefits, which relates to the belief that an action will be effective in reducing a threat and the fourth dimension is perceived barriers, are the potential challenges with undertaking a recommended behavior.11
During the COVID-19 pandemic, concerns about the innovation of vaccines but after the innovation of vaccines the urgent issue is the hesitancy of COVID-19 vaccines.12 Moreover, recent studies recommend the acceptance rate and challenges of new vaccines against COVID-19 for children and adolescents at the global level based on the HBM approach because HBM is widely accepted to determine the factors affecting the vaccine intent.13
Therefore, this study aimed to draw a comprehensive picture of vaccine acceptance and various predictors related to COVID-19 vaccines, so this systematic review and meta-analysis provide a better reference for future vaccine coverage which would promote the development of herd immunity to the pandemic as well as for health authorities and professionals to respond to potential problems in an adequate and targeted manner.
Methods
Review question
Clear and focused review question – not too vague, too specific, or too broad (Using PICO) The PICO mnemonics were used: population (P): general population, Intervention (I): HBM-based predictors, Comparison (C): The reported reference group for each associated factor e.g., who have the intention to acquire the COVID-19 vaccine versus no intention to acquire the COVID-19 vaccine, outcomes (O): intention to acquire the COVID-19 vaccine
Registration of research protocols
The goal of this systematic review and meta-analysis was to present the most up-to-date information on the pooled intention to acquire the COVID-19 vaccine and its HBM-based predictors. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Protocol 2019 statement was used to establish the protocol for this systematic review and meta-analysis14 and PROSPERO International Prospective Register of Systematic Reviews (PROSPERO) (CRD42022313961).
Search strategy & database
All research completed in various parts of the world is included in this Systematic Review and Meta-Analysis. National Library of Medicine (NLM), PubMed, and Medline databases were searched from 19 March 2020 to 14 October 2021, Joanna Briggs Institute (JBI) and Google scholar databases were from 15 October 2021 to 24 January 2022, and Cochrane Library database from 25 January 2022 to 04 March 2022. In addition, we conducted an internet search using the Google search engine to confirm that no relevant studies were overlooked, Online University repositories (UoG & AAU), and a reference list of retrieved studies. The PRISMA guideline for reporting protocol and the PRISMA checklist to screen papers were used to search the databases listed above. The following search terms and Boolean phrases were used to bring essential topics together to uncover HBM-based predictors and Intention to acquire the COVID-19 vaccine “Intention” OR “Willingness “AND “COVID-19 Vaccines” OR “SARS-CoV-2 virus Vaccine” OR “Coronavirus Disease 2019 Vaccines” OR “2019 Novel Coronavirus Vaccines” OR “Vaccination” OR “Immunization” AND “Associated factors” OR “determinants” OR “predictors” AND “Health belief model” OR “Behavioral model.” The review’s publication selection, data extraction, and reported results followed the PRISMA criteria.14
Selection of research
To exclude duplicate research, all publications retrieved by the search approach were exported to Endnote version 7. Following the elimination of duplicate research, writers independently examined titles and abstracts for inclusion in the full text assessment (CY, AS, AM, and AG). If there were any disagreements, they were settled using predetermined article selection criteria after the reviewers performed a single-anonymized and open peer review.
Inclusion and exclusion
This study collected all research from across the globe that reported on the intention to receive the COVID-19 vaccine and its HBM-based predictors. Studies that were only published in the English language were included to avoid problems during the translation process. Articles that did not report the intention to obtain the COVID-19 vaccine and OR but provided enough data to calculate the intention to receive the COVID-19 vaccine and OR were included. Non-accessible studies were rejected if they were unpublished, unretrievable from the internet, or if the associated authors had not responded to an e-mail. This study also excluded a study that did not provide enough data to calculate the desired outcome following a full text examination, as well as non-full-text papers and secondary studies.
Participation of patients and the general public
In this investigation, there was no direct connection with patients and no direct patient input in the design or execution of the study.
Criticism and evaluation of quality
The Joanna Briggs Institute (JBI) quality appraisal checklist adapted for cross-sectional, case-control, and cohort studies was used to assess the quality of each article selected for inclusion in the systematic review (that is, those that met the inclusion criteria specified above).15 Three authors (CY, AM, AA, and AG) independently rated the quality of each study using the tool as a protocol, and inconsistencies in the study ratings were addressed and resolved. The quality of the methodology, the comparability of the research, and the quality of their statistical analysis were the three metrics of the tool. And after much deliberation among the reviewers, a consensus was established. When a study’s quality evaluation score was 50% or higher, it was considered low risk.
Extraction of data
The author (AM) created a simple data extraction format in Microsoft Excel. Names of authors, publication year, target population, study nation, study design, sample size, response rate, prevalence, number of successes and failures in exposed and unexposed groups, and OR with CI of relevant factors were all included. Using this structured data extraction form, two authors (CY and AM) independently extracted the data. The phase was repeated if variations in the extracted data were noted. If disagreements between data extractors persisted, a 3rd reviewer (AA) and the 4th reviewer (AG) were consulted, and a consensus was obtained through debate among the reviewers (See Supporting information).
Data aggregation and analysis
The retrieved data in a Microsoft Excel spreadsheet was loaded into RevMan Software version 5.4.1 for analysis. The DerSimonian and Laird random-effects model, which assumes heterogeneity across trials, was used to do the pooled analysis. The heterogeneity of the included studies was checked using the I2 test. Low, moderate, and high heterogeneity were defined as 25%, 50%, and 75%, respectively. Significant difference; the presence of heterogeneity was determined by a P-value of less than .05. Subgroup analysis using area, design, and year of publication as grouping variables was conducted to further investigate the variability among studies. A sensitivity analysis was also performed to see if single research had an impact on the pooled prevalence estimates. The funnel plot and Eggers and Begg’s tests were used to check for publication bias across papers. The statistical significance of publication bias was determined using a P-value of less than .05. Trim and fill analysis was used to overcome publication bias if it existed. Separate categories of the meta-analysis were used to examine the effect of selected determinant variables. The results of the meta-analysis were displayed using a forest plot and an Odds Ratio (OR) with a 95% confidence interval.
Dissemination and ethics
Ethical approval was not necessary because this was a systematic review of already published data. The final report was presented at local, regional, national, and worldwide conferences and was published in a peer-reviewed scientific journal.
Results
Study selection
Through database searching, 320 studies records were found, of which 188 were deleted owing to duplication, 132 were discarded because they didn’t meet the prescreening criteria, and 33 were eliminated because the study was not similar to the study objective. Finally, 99 studies fully satisfied the prescreening criteria; 34 full-text papers were eliminated because they did not fully satisfy the study’s eligibility requirements. Following that, 66 studies were included in the systematic review and 19 papers were included in the meta-analysis (Figure 1).
Figure 1.
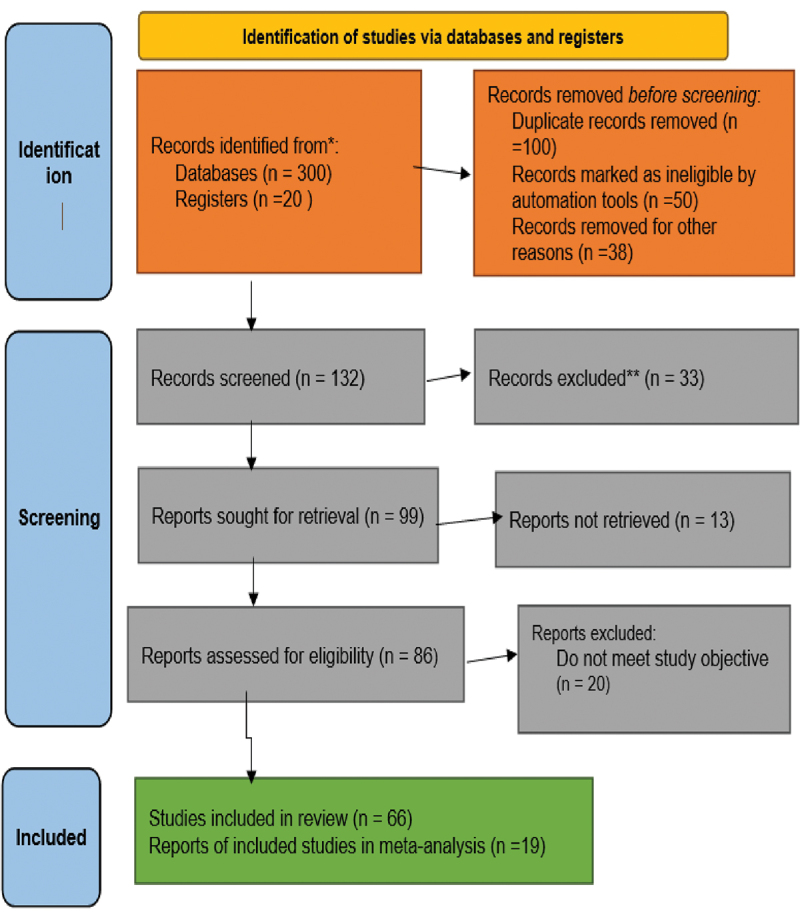
PRISMA 2020 flow diagram for systematic reviews which included searches of databases and registers.
Characteristics of the studies
Included Studies done from 13 countries with 47,873 participants, all studies employed a Cross-sectional study design; five studies were conducted in China, whereas equally 2 studies were reported in Ethiopia, Saudi Arabia, and Bangladesh. In addition, a single Study was performed in South Asia, Turk, Vietnam, Israel, India, Lebanon, Pakistan, Philippines (Additional file). All Studies to assess intention to receive the COVID-19 vaccine and its HBM-based predictors and additional important methodological features from each study were examined and the studies were low risk according to the quality assessment score (Table 1).
Table 1.
Characteristics of included studies in this systematic review and meta-analysis.
| Authors | Publication year | Study design | Study country | Sample size | Prevalence (%) | Quality |
|---|---|---|---|---|---|---|
| Toa L et al | 2021 | Cross-sectional | China | 1392 | 77.4 | Low risk |
| Okuyan B et al | 2021 | Cross-sectional | Turk | 961 | 74.7 | Low risk |
| Huynh G et al | 2021 | Cross-sectional | Vietnam | 410 | 76.1 | Low risk |
| Mahmud I et al | 2021 | Cross-sectional | Saudi Arabia | 1387 | 57.5 | Low risk |
| Seboka BT et al | 2021 | Cross-sectional | Ethiopia | 1116 | 46.6 | Low risk |
| Shitu K et al | 2021 | Cross-sectional | Ethiopia | 301 | 40.8 | Low risk |
| Shmueli L | 2021 | Cross-sectional | Israeli | 398 | 80 | Low risk |
| Wong MC et al | 2020 | Cross-sectional | China | 1200 | 42.2 | Low risk |
| Patwary MM et al | 2021 | Cross-sectional | Bangladish | 639 | 85 | Low risk |
| Goruntla N et al | 2021 | Cross-sectional | India | 2451 | 89.3 | Low risk |
| Youssef D et al | 2022 | Cross-sectional | Lebanon | 1800 | 58.1 | Low risk |
| Qin C et al | 2022 | Cross-sectional | China | 3119 | 93.7 | Low risk |
| Khalafalla HE et al | 2022 | Cross-sectional | Saudi Arabia | 1039 | 83.6 | Low risk |
| Chen H et al | 2021 | Cross-sectional | China | 2531 | 65.7 | Low risk |
| Hawlader MDH et al | 2022 | Cross-sectional | South Asia | 18201 | 69.05 | Low risk |
| Caple A et al | 2022 | Cross-sectional | Philippines | 7193 | 62.5 | Low risk |
| Yasmin F et al | 2021 | Cross-sectional | Pakistan | 1778 | 72 | Low risk |
| Kabir R et al | 2021 | Cross-sectional | Bangladish | 697 | 69 | Low risk |
| Yan E et al | 2021 | Cross-sectional | China | 1255 | 42 | Low risk |
Intention to receive COVID-19 vaccine
Using a DerSimonian and Laird random-effects model, the overall pooled prevalence of intention to receive COVID-19 vaccine globally was 67.69% (95% CI: 60.86%, 74.52%) with significant heterogeneity between studies (I2 = 99.66%, P < .001). The overall pooled prevalence of intention to receive the COVID-19 vaccine globally was presented using a forest plot (Figure 2).
Figure 2.
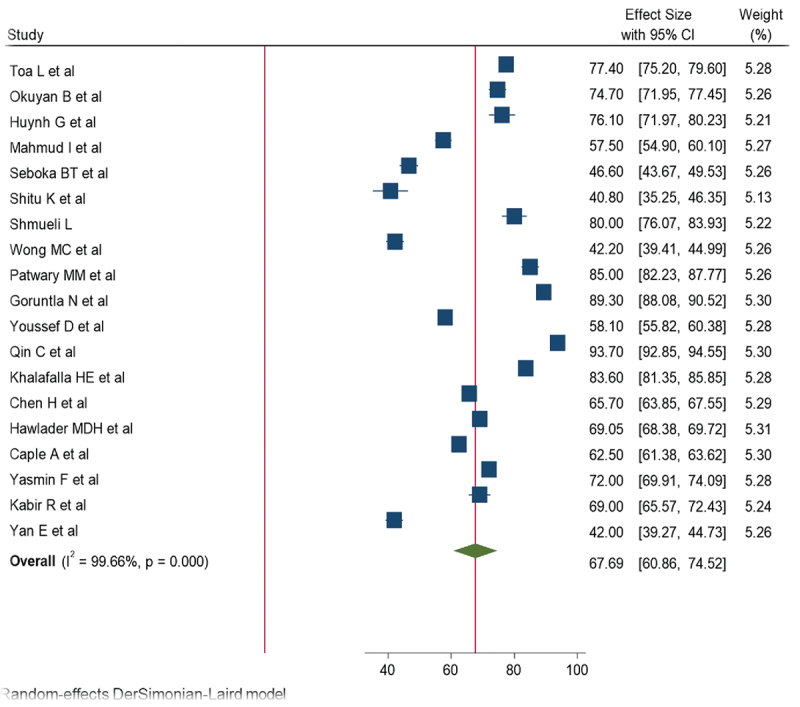
Frost plot for the global pooled prevalence of intention to receive COVID-19 vaccine.
Heterogeneity and publication bias
The Cochrane I2 values in this meta-analysis were 99.66% with a P-value of .001, indicating that there was significantly high heterogeneity. Subgroup and sensitivity analysis was used to further explore it. According to a subgroup analysis based on the study country, the prevalence of intent to take the COVID-19 vaccine was high in India (89.30%, 95%CI: 88.10–90.52) and low in Ethiopia (44.20%, 95%CI: 38.60–49.80, I2 = 69.52, P = .07). Another subgroup analysis of participants also revealed that there was a high intention (69.57%) to receive the COVID-19 vaccine among health care workers. Sensitivity analysis was also used to look into the impact of a single study on the overall magnitude estimate, with the results indicating that a single study did not have a significant impact on the overall magnitude estimate. As a result, the point estimate of its omitted analysis falls within the combined analysis confidence interval (Figure 3).
Figure 3.
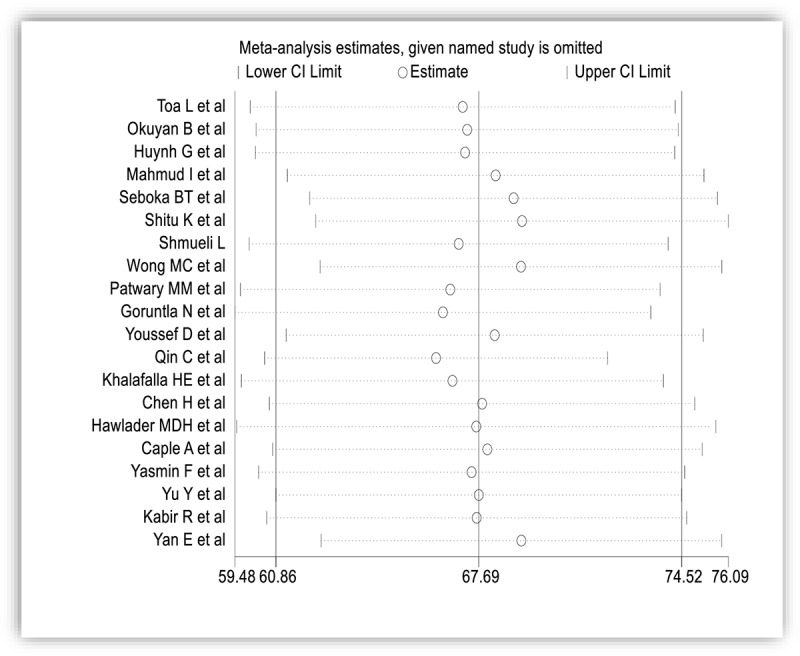
Sensitivity analysis of the pooled prevalence of intention to receive COVID-19 vaccine.
Using funnel plots and objective assessments (Egger and Begg), the presence of publication bias was investigated. The funnel plot showed a somewhat symmetrical distribution (Figure 4), which was confirmed by the Egger and Begg tests, which yielded a p-value of .163 (Table 2).
Figure 4.
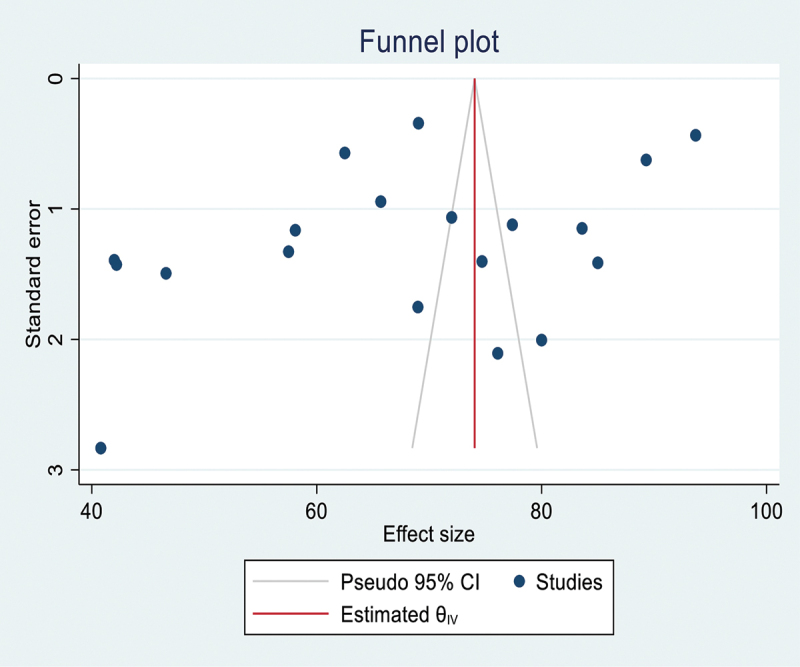
Funnel plot test for publication bias.
Table 2.
The Egger and Begg tests of the study for the presence of publication bias. Number of studies = 19; Root MSE = 16.72.
| Std_Eff | Coef. | Std. Err. | T | P>|t| | 95% Conf. Interval | |
|---|---|---|---|---|---|---|
| Slope | 81.33 | 5.92 | 13.74 | 0.001 | 68.84 | 93.81 |
| Bias | −10.42 | 7.15 | −1.46 | 0.163 | −25.49 | 4.65 |
Test of HO: no small-study effect; p = .163.
HBM-based predictors associated with intention to receive COVID-19 vaccines
The association of HBM constructs (perceived vulnerability, perceived severity, perceived benefit, perceived barrier, and due to action) to getting the COVID-19 vaccine was investigated. As a result, the pooled odds ratio revealed that there was a significant association between all HBM elements and the desire to acquire the COVID-19 vaccine. Higher levels of perceived susceptibility (OR = 1.85, 95% CI:1.33–2.56) (Figure 5), perceived severity (OR = 1.45, 95% CI:1.14–1.85) (Figure 6), perceived benefits (OR = 3.10, 95% CI: 2.13–4.36) (Figure 7), and cues to action (OR = 3.40, 95% CI: 2.15–5.36) (Figure 8) positively predicted intention to receive COVID-19 vaccines, whereas a high level of perceived barrier negatively predicted intention to receive COVID-19 vaccines(OR = 0.53, 95% CI: 0.43–0.66) (Figure 9).
Figure 5.
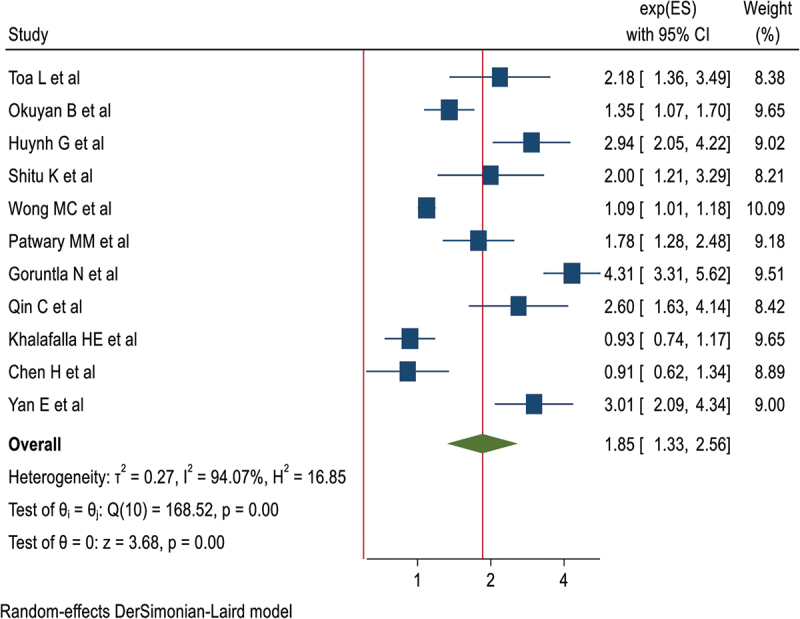
Frost plot for perceived susceptibility.
Figure 6.
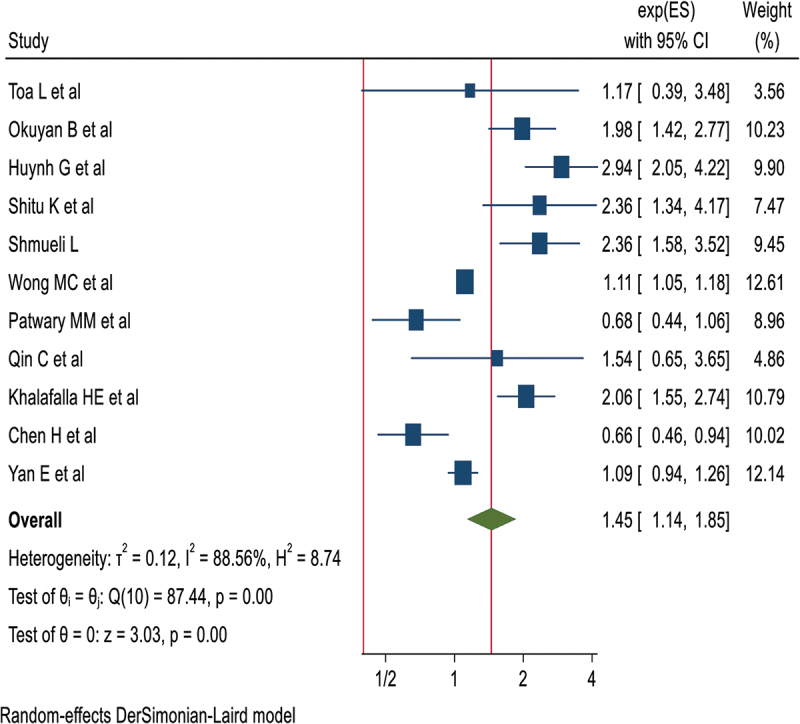
Frost plot for perceived severity.
Figure 7.
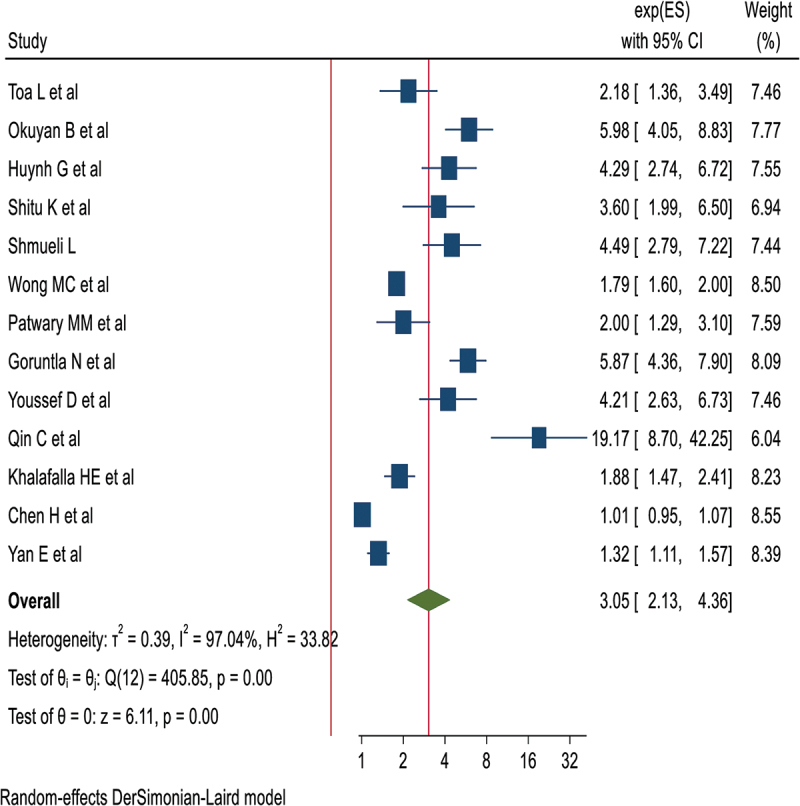
Frost plot for perceived benefit.
Figure 8.
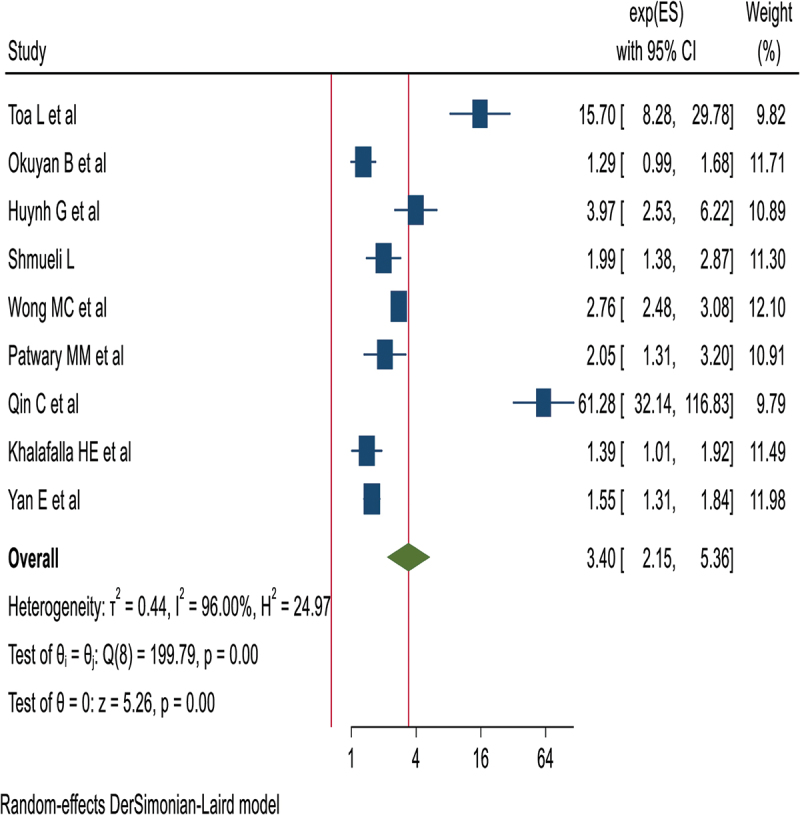
Frost plot for cue to action.
Figure 9.
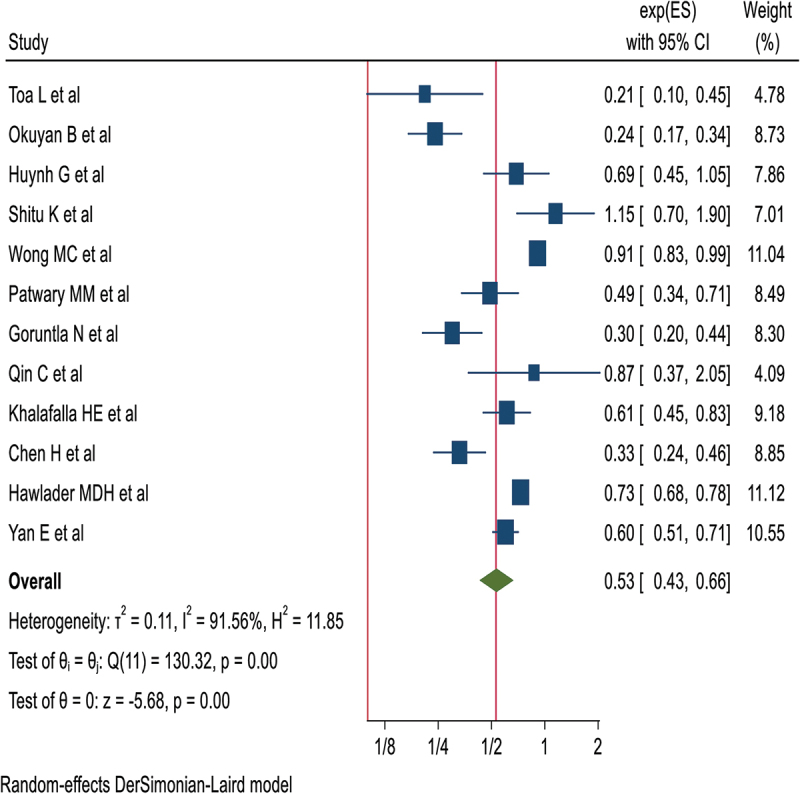
Frost plot perceived barrier.
Discussion
Most health professionals were mainly focused on the sufficient, effective, long duration of protective effective and optimum safety vaccine roll-out strategy for their population. Now a day’s dozens of vaccines are currently being implemented and developed to address the social, economic, and health impacts of pandemics on individuals around the globe. However, the success of a vaccination program will depend on the rates of intention to receive the vaccine among the population.16 The population immunity depends on the basic reproductive number to limit the pathogen spread, the latest estimate of the range of COVID-19 immunity to halt the transmission is 60–75%. These are to be improved by initiating a public awareness campaign, ongoing health education & promotion of the vaccine and vaccination.17
Achieving herd immunity is currently the best way to effectively limit the spread of COVID-19 without causing serious mental health issues. Therefore, it is crucial to immunize the general populace at a 100% immunization rate. But, having worries and psychological distress were barriers to improve their willingness.18
So, this systematic review mainly focuses on intention to receive the COVID-19 vaccine and HBM-based predictors to address COVID-19 vaccine acceptance rates among the general population and address barriers.19–21 Moreover, this study also examined the intention to receive the COVID-19 vaccine and how the HBM constructs predicted such intentions globally, as there is no comprehensive evidence. So, this review includes all articles conducted on the intention to receive the COVID-19 vaccine and its HBM-based predictors, it helps to design an effective mechanism to create awareness of the vaccine and significant determinants toward the intention to receive COVID-19 vaccine in the globe.22
The finding of this review on COVID-19 vaccination intention is consistent with previous systematic review reports conducted in Kuwait,23 Jordan,24 Italy,25 Russia,19 Poland,20 the United States,21 and France.26 And also, similar to the survey conducted in China by parents/guardians who worked.27 This might be related to stronger confidence in vaccine safety and effectiveness, as reported in previous studies. In this study, 20 articles from different groups within the population dealing with HBM-based predictors are included. The various HBM-related predictors found in this study had a positive or negative influence on COVID-19 immunization intention. These are perceived vulnerability, perceived severity, perceived benefits, perceived barriers, and behavioral cues. This may mean that individuals need sound health education and publicity about vaccines prior to vaccination.28
The result suggests that all components of HBM have a significant association with the development of intent to COVID-19 vaccination. Of the significant factors, respondents who had higher guidance levels of perceived vulnerability, perceived severity, perceived benefits, and behavior positively predicted the intent to receive the COVID-19 vaccine. This might be due to the disease morbidity and mortality People believe the high risk of getting COVID-19 disease case of this they are highly stimulus to get the COVID-19 vaccine to protect against the disease.29
In line with recent vaccine intent results of the general population, the acceptance of children’s COVID-19 vaccination was usually moderate among parents and guardians worldwide (61.40%). Based on their age, access to scientific knowledge and recommendations, routine and influenza vaccination behavior, and willingness to get vaccinated themselves, parents and caregivers were found to be possibly significant predictors of vaccination willingness.12
There was a significant association between the recognized vulnerability variables and the intent to receive the COVID-19 vaccine. People who have a raising level of perceived susceptibility may believe that they are at a higher risk of contracting the pandemic. This will make them want to get the COVID-19 vaccine.30 In this review 11 articles of the 19 articles found that perceived vulnerability and perceived severity played a key role in changing the intention of the study population to receive the COVID-19 vaccine. This might be due to people’s high sensory sensitivity indicating they believe they are at high risk of illness. Therefore, due to this reason highly recognized vulnerability, they will want to be vaccinated with the COVID-19 vaccine.31
The result of this systematic review and meta-analysis also shows that there is a positive relationship between the perceived severity component and the intent to receive the COVID-19 vaccine. Of the 19 articles, 13 of them reveal that perceived benefit had a positive association with intention to receive the COVID-19 vaccine. This is due to raising the level of perceived severity, individuals to know the seriousness of risks as individuals may believe that shortness of breath and extreme fatigue, impaired sense of smell and taste. Thus, the possibility of irreversible damage to other organs, brain dysfunction, stroke, or meningitis, which may be due to knowledge about, is one of the most important factors in increasing the perceived severity in this regard.32
The other positive predictor of intention to COVID-19 vaccination is a high level of perceived benefit and cue to action is critical in determining whether or not an individual should receive the vaccine because raising the level of understanding of the vaccine has an advantage in terms of protecting/maintaining their health. From the twenty articles 9 studies showed cue to act as a major contributing predictor for the intention to receive the COVID-19 vaccine. The position of perceived advantage and cue to movement performs a critical position in understanding the benefit of the vaccine and enforces people to take the vaccine. This is probably because the vaccine has a bonus in protecting/retaining them healthy.33
The reasons for hesitation included beliefs about the vaccine’s benefits, a shortage of vaccines, unknown long-term adverse effects, low confidence in the healthcare system, and a lack of knowledge about potential adverse effects. Therefore, the government and decision-makers must take all necessary steps to guarantee that the vaccination program is effective.34
In the same way, this review also showed high levels of perceived barriers negatively predicted the intention to receive the COVID-19 vaccine. Twelve12 articles were identifying perceived barriers as a negative predictor for COVID-19 vaccination. This means that overestimating the barrier may reduce your chances of getting that COVID-19 vaccine.35 The most recognized barriers to COVID-19 immunity include vaccine side effects, efficacy, and safety concerns. These are the COVID-19 vaccine hesitation triggers that can be removed with scientific explanations. Health officials need to address these issues directly addressing these concerns by launching an awareness campaign and creating infographics and other promotional material to mitigate these concerns.36 Although the COVID-19 vaccine may cause side effects, these side effects may not be significant health issues. Therefore, to support the promotion of vaccination, healthcare professionals and health officials should inform the general public about the findings from the health belief model.37
Strength and limitations
The technique was created using the PRISMA guidelines; this is the first systematic review and meta-analysis, and it may be a global estimate. However, the review had also its limitations this is the articles included in the study were only in published English. And also, we cannot infer causality due to the cross-sectional nature of the study. Future research could usefully conduct age-stratified research to further understand how HBM-based intention might vary and interact to get vaccinated by age. Besides, the exclusion of articles due to non-online availability or no response from the author is another limitation.
Conclusions
The rate of willingness to get the COVID-19 vaccine was relatively low and positively/negatively affected by HBM-based predictors. These factors should be provided to individuals who need sound health education and publicity about vaccines before vaccination. The findings will provide information for the management authorities to develop relevant interventions and policies to promote COVID-19 vaccination uptake such as public awareness campaigns, ongoing health education & promotion about the risks of the pandemic, benefits, safety, and efficacy of the vaccine. The study proposed that under-vaccination must be addressed using a multifaceted, evidence-based strategy that correctly identifies barriers to create strategies that are appropriate for the context and population and that target both those who unintentionally under-vaccinate as well as the hesitant.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Authors’ contribution
CY and AG conceived the design, interpreted the findings, and wrote the manuscript. AM, and AA, select and assess the quality of the study, extract data, interpret the result, and review the manuscript. All authors read and approved the manuscript.
Data availability statement
All data and materials are available from the corresponding author. Therefore, at a reasonable request, the corresponding author shared it via e-mail.
References
- 1.Maxmen A. Why did the world’s pandemic warning system fail when COVID hit? Nature. 2021;589(7843):1–11. doi: 10.1038/d41586-021-00162-4. [DOI] [PubMed] [Google Scholar]
- 2.Sharifi A, Khavarian-Garmsir AR.. The COVID-19 pandemic: impacts on cities and major lessons for urban planning, design, and management. Sci Total Environ. 2020;749:142391. doi: 10.1016/j.scitotenv.2020.142391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yayehrad AT, Siraj EA, Wondie GB, Alemie AA, Derseh MT, Ambaye AS. Could nanotechnology help to end the fight against COVID-19? Review of current findings, challenges and future perspectives. Int J Nanomedicine. 2021;16:5713. doi: 10.2147/IJN.S327334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Felter C. A guide to global COVID-19 vaccine efforts. Counc Foreign Relat. 2021;1. [Google Scholar]
- 5.Prasiska DI, Muhlis ANA, Megatsari H. Effectiveness of the emergency public activity restrictions on COVID-19 epidemiological parameter in East Java Province, Indonesia: an ecological study. Asian J Soc Health Behav. 2022;5(1):33. doi: 10.4103/shb.shb_90_21. [DOI] [Google Scholar]
- 6.Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, Jones M, Kitchener E, Fox M, Johansson M, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11(3):e045343. doi: 10.1136/bmjopen-2020-045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fong T-H, Cheung T, Chan W-C, Cheng C-W. Depression, anxiety and stress on caregivers of persons with dementia (CGPWD) in Hong Kong amid COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(1):184. doi: 10.3390/ijerph19010184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mullard A. COVID-19 vaccine development pipeline gears up. Lancet. 2020;395(10239):1751–2. doi: 10.1016/S0140-6736(20)31252-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Han X, Xu P, Ye Q. Analysis of COVID‐19 vaccines: types, thoughts, and application. J Clin Lab Anal. 2021;35(9):e23937. doi: 10.1002/jcla.23937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gates A, Gates M, Rahman S, Guitard S, MacGregor T, Pillay J, Ismail SJ, Tunis MC, Young K, Hardy K, et al. A systematic review of factors that influence the acceptability of vaccines among Canadians. Vaccine. 2021;39(2):222–36. doi: 10.1016/j.vaccine.2020.10.038. [DOI] [PubMed] [Google Scholar]
- 11.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 12.Chen F, He Y, Shi Y. Parents’ and guardians’ willingness to vaccinate their children against COVID-19: a systematic review and meta-analysis. Vaccines. 2022;10(2):179. doi: 10.3390/vaccines10020179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ali K, Berman G, Zhou H, Deng W, Faughnan V, Coronado-Voges M, Ding B, Dooley J, Girard B, Hillebrand W, et al. Evaluation of mRNA-1273 SARS-CoV-2 vaccine in adolescents. N Engl J Med. 2021;385(24):2241–51. doi: 10.1056/NEJMoa2109522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, Tierney JF. Preferred reporting items for a systematic review and meta-analysis of individual participant data: the PRISMA-IPD statement. Jama. 2015;313(16):1657–65. doi: 10.1001/jama.2015.3656. [DOI] [PubMed] [Google Scholar]
- 15.Drukker M, Weltens I, van Hooijdonk CF, Vandenberk E, Bak M. Development of a methodological quality criteria list for observational studies: the observational study quality evaluation. Front Res Metr Anal. 2021;6:675071. doi: 10.3389/frma.2021.675071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berihun G, Walle Z, Berhanu L, Teshome D. Acceptance of COVID-19 vaccine and determinant factors among patients with chronic disease visiting Dessie comprehensive specialized hospital, Northeastern Ethiopia. Patient Prefer Adherence. 2021;15:1795–805. doi: 10.2147/PPA.S324564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alimoradi Z, Lin C-Y, Pakpour AH. Worldwide estimation of parental acceptance of COVID-19 vaccine for their children: a systematic review and meta-analysis. Vaccines. 2023;11(3):533. doi: 10.3390/vaccines11030533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–8. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malesza M, Sobolewska K. COVID-19 vaccine uptake, predictors of vaccination, and self-reported barriers to vaccination among primary school teachers in Poland. MedRxiv. 2021;2021.07. 11.21260317. [Google Scholar]
- 21.Nguyen KH, Srivastav A, Razzaghi H, Williams W, Lindley MC, Jorgensen C, Abad N, Singleton JA. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination — United States, September and December 2020. Am J Transplant. 2021;21(4):1650–6. Wiley Online Library. doi: 10.1111/ajt.16560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zheng H, Jiang S, Wu Q. Factors influencing COVID-19 vaccination intention: the roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Educ Couns. 2022;105(2):277–83. doi: 10.1016/j.pec.2021.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alqudeimat Y, Alenezi D, AlHajri B, Alfouzan H, Almokhaizeem Z, Altamimi S, Almansouri W, Alzalzalah S, Ziyab AH. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract. 2021;30(3):262–71. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mahmud I, Al Imam MH, Vinnakota D, Kheirallah KA, Jaber MF, Abalkhail A, Alasqah I, Alslamah T, Kabir R. Vaccination intention against COVID-19 among the unvaccinated in Jordan during the early phase of the vaccination drive: a cross-sectional survey. Vaccines. 2022;10(7):1159. doi: 10.3390/vaccines10071159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy’among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35(8):781–3. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tavolacci MP, Dechelotte P, Ladner J. COVID-19 vaccine acceptance, hesitancy, and resistancy among university students in France. Vaccines. 2021;9(6):654. doi: 10.3390/vaccines9060654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang X, Wang Z, Ren Z, Li Z, Ma W, Gao X, Zhang R, Qiao Y, Li J. HPV vaccine acceptability and willingness-related factors among Chinese adolescents: a nation-wide study. Hum Vaccin Immunoth. 2021;17(4):1025–32. doi: 10.1080/21645515.2020.1812314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen H, Li X, Gao J, Liu X, Mao Y, Wang R, Zheng P, Xiao Q, Jia Y, Fu H, et al. Health belief model perspective on the control of COVID-19 vaccine hesitancy and the promotion of vaccination in China: web-based cross-sectional study. J Med Internet Res. 2021;23(9):e29329. doi: 10.2196/29329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oțelea MR, Zugravu C, Rașcu A, Arghir OC, Manolescu LSC, Mates D, editors. Coronasomnia in employees without a direct contact with COVID-19 infected patients in their workplace. In Healthcare. MDPI; 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kearney JM, McElhone S. Perceived barriers in trying to eat healthier–results of a pan-EU consumer attitudinal survey. Br J Nutr. 1999;81(S1):S133–7. doi: 10.1017/S0007114599000987. [DOI] [PubMed] [Google Scholar]
- 31.Pandey K, Thurman M, Johnson SD, Acharya A, Johnston M, Klug EA, Olwenyi OA, Rajaiah R, Byrareddy SN. Mental health issues during and after COVID-19 vaccine era. Brain Res Bull. 2021;176:161–73. doi: 10.1016/j.brainresbull.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scaer R. The body bears the burden: trauma, dissociation, and disease. Routledge; 2014. [Google Scholar]
- 33.Karaaslan F, Dikilitas A. The effect of coronavirus disease 2019 pandemic on oral health behavior of Turkish society. J Oral Health Oral Epidemiol. 2020;9:187–95. [Google Scholar]
- 34.Ahorsu DK, Lin C-Y. The effect of COVID-19 vaccine acceptance, intention, and/or hesitancy and its association with our health and/or important areas of functioning. MDPI; 2023. p. 368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saied SM, Saied EM, Kabbash IA, SAEF A. Vaccine hesitancy: beliefs and barriers associated with COVID‐19 vaccination among Egyptian medical students. J Med Virol. 2021;93(7):4280–91. doi: 10.1002/jmv.26910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nuzhath T, Tasnim S, Sanjwal RK, Trisha NF, Rahman M, Mahmud SF, Arman A, Chakraborty S, Hossain MM. COVID-19 vaccination hesitancy, misinformation and conspiracy theories on social media: a content analysis of Twitter data. 2020. [Google Scholar]
- 37.Rifai A, W-C W, Tang Y-W, M-Y L, Chiu P-J, Strong C, Lin C-Y, Chen P-L, Ko W-C, Ko N-Y. Psychological distress and physical adverse events of COVID-19 vaccination among healthcare workers in Taiwan. Vaccines. 2023;11(1):129. doi: 10.3390/vaccines11010129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data and materials are available from the corresponding author. Therefore, at a reasonable request, the corresponding author shared it via e-mail.


