Abstract
(1) Background: Infections are among the most frequent and life-threatening complications of cardiovascular implantable electronic device (CIED) implantation. The aim of this study is to compare the outcome and safety of a single-procedure device extraction and contralateral implantation versus the standard-of-care (SoC) two-stage replacement for infected CIEDs. (2) Methods: We retrospectively included 66 patients with CIED infections who were treated at two Italian hospitals. Of the 66 patients enrolled in the study, 27 underwent a single procedure, whereas 39 received SoC treatment. All patients were followed up for 12 months after the procedure. (3) Results: Considering those lost to follow-up, there were no differences in the mortality rates between the two cohorts, with survival rates of 81.5% in the single-procedure group and 84.6% in the SoC group (p = 0.075). (4) Conclusions: Single-procedure reimplantation associated with an active antibiofilm therapy may be a feasible and effective therapeutic option in CIED-dependent and frail patients. Further studies are warranted to define the best treatment regimen and strategies to select patients suitable for the single-procedure reimplantation.
Keywords: CIED infection, single procedure, device extraction, antibiofilm
1. Introduction
CIED implants are lifesaving, albeit not riskless procedures. Rates of implants have increased over the past years due to the interplay of several factors, including increasing age and life expectancy and new pacing indications. Such patients frequently present with significant comorbidities and have an increased susceptibility to infectious complications [1,2,3]. Hence, as more complex patients undergo CIED implants, a concomitant rise in infections has also been observed [4,5,6,7], to the extent that the CIED infection rate is greater than the implants themselves [8]. CIED infections are associated with substantial morbidity and mortality [9] and impact quality of life, healthcare resource use, and costs [2,10]. Recent joint guidelines reported a more than two-fold increase in in-hospital mortality, with an estimated in-hospital 30-day mortality due to CIED infection of 5%–8% [1]. The most common pathogens responsible for CIED infections are Gram-positive bacteria, especially S. epidermidis and S. aureus, while Gram-negative bacteria and fungi are rarer microorganisms in this kind of infection [3,11,12]. The pathogens responsible for CIED infections are biofilm-forming microorganisms in most cases [13]. This microorganism feature makes CIED infections extremely difficult-to-treat diseases. Guidelines consider mandatory leads extraction, as treatment of CIED infections typically includes the removal/extraction of the entire infected CIED system, debridement, and administration of systemic antibiotics to eradicate the infection [1,14]. However, there is poor and conflicting data concerning the timing of the new device re-implant [1,4,14,15]. As with other device infections, such as prosthetic cardiac valve endocarditis, reimplantation cannot be delayed until infection eradication in case of surgery, and the relapse rate in these cases is very low [16].
Same-day extraction and reimplantation in patients with infected CIEDs is a viable but non-standardized option, with only small cohorts of patients [17,18,19,20] and scarce data on patients with systemic infections, particularly endocarditis.
The aim of this study was to assess the outcome of a single procedure of extraction and contralateral reimplantation in patients with CIED infections.
2. Materials and Methods
2.1. Definitions
Hospital admission was defined as the date of the patients’ admission to the hospitals included in the study. Hospitalization was defined as the period between the hospital admission and the date of discharge from the hospital. CIED infections were defined according to the European Heart Rhythm Association (EHRA) criteria [1]. Local infection was defined as an infection localized to the CIED pocket. Endocarditis was defined according to the European Society of Cardiology’s 2015 modified criteria [21]. Vegetation was defined as an intracardiac mass on the valve or the implanted intracardiac material, identified with transthoracic and/or transesophageal echocardiography. The infecting pathogens were determined with blood cultures and/or lead cultures at the time of diagnosis or extraction. Anti-Gram-negative antibiotic therapy was defined as an antibiotic therapy with displayed activity against Gram-negative bacteria. Antibiofilm therapy/combination was defined as an antibiotic therapy with activity against the common biofilm-producing bacteria isolated in our cohort (the antibiofilm therapy used in our cohort was daptomycin/rifampicin alone or in combination with a beta-lactam molecule) [22,23,24,25,26].
2.2. Population Study
Patients presenting in the centers of Pisa and Cotugno (Naples) hospitals between January and December 2019 requiring pacemaker or defibrillator system extraction and new device implantation were retrospectively assessed. Patients with a local, systemic infection or CIED-related infective endocarditis were enrolled.
Patients treated at the Pisa University hospital, considered a national referral center for challenging CIED infections, underwent standard-of-care two-stage replacement, whereas patients in Naples, Cotugno hospital, were treated by means of one-stage device reimplantation on the same day. The Pisa cohort was considered the reference SoC cohort. Of notice, patients referred to the Pisa center are often considered at higher risk of complexity and negative outcomes; therefore, in the SoC, only pacemaker infections were enrolled because these infections are usually less severe compared with indwelling defibrillator infections.
Patients were followed up at both institutions for up to 12 months post-procedure. Those lost to follow-up were also included in the final analysis.
All patients underwent device extraction and new device implantation. In the single-procedure cohort, the benefit of early reimplantation of a contralateral device in the setting of device dependence was considered to outweigh the small theoretical risk of reinfection of the new device. This was also due to the features of the center, which did not enable a SoC procedure. Clinical and procedural data were collected along with therapeutical intervention long-term outcomes.
2.3. Transvenous Lead Extraction Procedure
The method used as the standard of care at Pisa hospital was an evolution of the technique introduced by Byrd in the 1980s [27]. Polypropylene dilating sheaths (Cook Vascular Inc., Leechburg, PA, USA) were used to dilate the adherences between the leads and venous/cardiac structures, usually with a single-sheath technique using a standard stylet instead of a locking stylet. The dilation was attempted when manual gentle traction was unsuccessful. In case of failure from the venous entry side, a jugular-vein or multiple-vein approach was considered to succeed (the so-called Pisa approach). Free-floating lead extractions and combined approaches for challenging leads were performed using an intravascular workstation (Cook Vasc. Inc., Leechburg, PA, USA) with tip-deflecting wires, baskets, and loop retrievers [28]. Additional intravascular tools included catchers (remote-control clippers) and lassos (remote-control loop retrievers) by Osypka Gmbh (Grenzach-Wyhlen, Germany).
Powered sheaths with lasers were used in the Naples approach [29,30,31]. This technique is characterized by using locking stylets and laser energy to overcome the adherences. A laser sheath 12/14/16F with a “cool” pulsed ultraviolet laser at a wavelength of 308 nm was used to remove all the adherences on the leads (Spectranetics Laser Sheath).
All the procedures were performed with aseptic technique; surgical services were available in the departments and emergency cardiovascular surgical staff was on standby at all times.
2.4. Microbiology and Medical Treatment
The microbiology of the infections was documented with cultures obtained from the removed leads (proximal and distal parts) and/or infected material. Blood cultures were collected at the discretion of the treating physicians when considered appropriate.
Patients received antimicrobial treatments based on the pathogen or epidemiological features. Treatment regimens were modified according to renal functions and patient characteristics at the discretion of the treating physician. Antibiofilm combinations were generally used to achieve microbiological clearance.
2.5. Statistical Analysis
Depending on their distributions, the variables were represented as mean +/− standard deviation, median and inter-quartile interval, or sum and percentage. Accordingly, comparisons between groups were performed with an unpaired sample t-test, Mann–Whitney test, or chi-square test with continuity correction. A value of p less than 0.05 was considered statistically significant. All the analyses were performed with R statistical software [32].
3. Results
Overall, 27 and 39 patients were enrolled from the single-procedure and SoC sites, respectively. All demographic data along with predisposing factors, device type, infection, and treatments are reported in Table 1 and Table 2. No significant differences in demographic characteristics or predisposing factors were detected among the two cohorts, with the exception of weight. All devices/leads were extracted from all patients. The device type differed among the groups: while all SoC devices comprised pacemakers (PMKs), the single-procedure group presented with a variety of devices, including PMKs (40.7%), implantable cardioverter defibrillators (ICDs) 22.3%, and biventricular defibrillator implants (BDIs) 37.0%. No significant differences were observed when the infection diagnoses were assessed, with similar distributions for endocarditis and local infections (66.7% vs. 43.6%, p = 0.082 in patients with endocarditis; 33.3% vs. 56.4%, p = 0.144 in patients with local infections, for single-procedure versus SoC, respectively). Positive blood cultures for bacteria at hospital admission were reported in 12 (44.4%) and 13 (33.3%) patients from the single-procedure and SoC groups, respectively (p = 0.511). Patients with sepsis were reported in 11.1% and 5.1% of cases in the single-procedure and SoC cohorts, respectively, with no significant differences among the groups (p = 0.393).
Table 1.
Patients characteristics in both the Single Procedure group and in the SoC group.
| Patient Characteristics | Single Procedure (n = 27) |
SoC (n = 39) |
p |
|---|---|---|---|
| Sex (males) | 19 (70.4%) | 30 (76.9%) | 0.755 |
| Age (years) | 72.07 ± 14.96 | 73.79 ± 8.89 | 0.560 |
| Weight (kg) | 73.04 ± 10.60 | 78.89 ± 11.51 | 0.046 |
| Predisposing factors | |||
| Skin infection | 0 (0%) | 4 (10.3%) | 0.233 |
| Previous endovascular infection | 9 (33.3%) | 5 (12.8%) | 0.090 |
| Cancer | 5 (18.5%) | 2 (5.1%) | 0.701 |
| Chronic kidney disease | 11 (40.7%) | 9 (23.1%) | 0.207 |
| Stroke | 1 (3.7%) | 3 (7.7%) | 0.886 |
| Dialysis | 4 (14.8%) | 0 (0%) | 0.051 |
| COPD | 7 (25.9%) | 10 (25.6%) | 1 |
| Previous CIED interventions | |||
| Revision/upgrade/replacement/malfunction | 11 (40.7%) | 23 (59.0%) | 0.227 |
| Device | |||
| Pacemaker | 11 (40.7%) | 39 (100%) | <0.001 |
| Implantable cardioverter defibrillator (ICD) | 6 (22.2%) | 0 (0%) | 0.008 |
| Biventricular defibrillator implant | 10 (37.0%) | 0 (0%) | <0.001 |
| Device extraction and implant | |||
| Time from device implant (years) | 2 (1–7) | 9 (4–13) | 0.002 |
| Time from diagnosis to extraction (days) | 27 (12–30) | 60 (30–90) | <0.001 |
| Length of procedure (minutes) | 140 (102–180) | 151 (120–224) | 0.192 |
| Final diagnosis | |||
| Endocarditis | 18 (66.7%) | 17 (43.06%) | 0.082 |
| Localized infection | 17 (33.3%) | 18 (56.4%) | 0.144 |
| Vegetation | |||
| Vegetation | 14 (51.9%) | 15 (38.5%) | 0.409 |
| Vegetation size (median, range-mm) | 3.12 ± 0.91 | 4.07 ± 1.12 | 0.857 |
| Positive blood culture | 12 (44.44%) | 13 (33.3%) | 0.511 |
| Concomitant sepsis | 3 (11.1%) | 2 (5.1%) | 0.393 |
| Anticoagulant therapy | 15 (55.6%) | 16 (41.0%) | 0.318 |
| Antibiotic therapy (admission) | |||
| Overall | 9 (33.3%) | 21 (53.6%) | 0.163 |
| Anti-Gram-negative * | 7 (25.9%) | 9 (23.0%) | 1.000 |
| Antibiotic therapy (hospitalization) | |||
| Overall | 24 (88.9%) | 39 (100%) | 0.064 |
| Anti-Gram-negative * | 20 (74.1%) | 15 (38.5%) | 0.006 |
| Activity against biofilm † | 22 (81.5%) | 15 (38.5%) | 0.001 |
| Outcome | |||
| Survival (1 month) | 24 (88.9%) | 39 (100%) | 0.126 |
| Survival (12 months) | 22 (81.5%) | 33 (84.6%) | 0.737 |
| Lost to follow-up | 5 (18.5%) | 6 (15.4%) | 0.737 |
| Reinfection | 0 (0%) | NA | --- |
* Anti-Gram-negative: antibiotic agents with displayed activity against Gram-negative bacteria. † Activity against biofilm: antibiotic combination (daptomycin/rifampicin + beta-lactam) with antimicrobial activity demonstrated in vitro against common biofilm-producing bacteria isolated in our cohort [22,23,24].
Table 2.
Antibiotic treatment during hospitalization.
| Antibiotic |
Single Procedure
(27) |
SoC
(39) |
|---|---|---|
| Overall | 24 (88.9%) | 39 (100%) |
| Oxacillin/flucloxacillin | 0 (0%) | 4 (10.3%) |
| Cefazolin | 7 (25.9%) | 0 (0%) |
| Daptomycin | 20 (74.1%) | 20 (51.3%) |
| Vancomycin | 0 (0%) | 2 (5.13%) |
| Teicoplanin | 0 (0%) | 5 (12.8%) |
| Linezolid | 0 (0%) | 2 (5.13%) |
| Ceftobiprole | 7 (25.9%) | 0 (0%) |
| Ceftaroline | 2 (7.41%) | 3 (7.69%) |
| Others | 5 (18.5%) | 20 (51.3%) |
| Monotherapy | 3 (11.1%) | 14 (35.9%) |
| Combination therapy | 21 (77.8%) | 25 (64.1%) |
Vegetations were reported in 14 (51.9%) and 15 (38.5%) of patients from the single-procedure and the SoC cohorts, respectively. Vegetation size (median, range-mm) ranged from 3.12 ± 0.91 cm in the single-procedure cohort to 4.07 ± 1.12 cm in the SoC cohort.
The time from device implant to extraction differed among the two cohorts, as well as the time from diagnosis to extraction. In the single-procedure group, the time from implant to extraction ranged between 1 and 7 years, with a median time of 2 years, while in the SoC group there was a significantly longer lag time to extraction, ranging from 4 to 13 years, with a median time of 9 years (p = 0.002). Similarly, in the single-procedure cohort, the median interval time from diagnosis of device infection to extraction was significantly shorter (median time, range = 27 (12–30 days) compared with SoC (median, range = 60 (30–90) days from diagnosis to extraction) (p < 0.001).
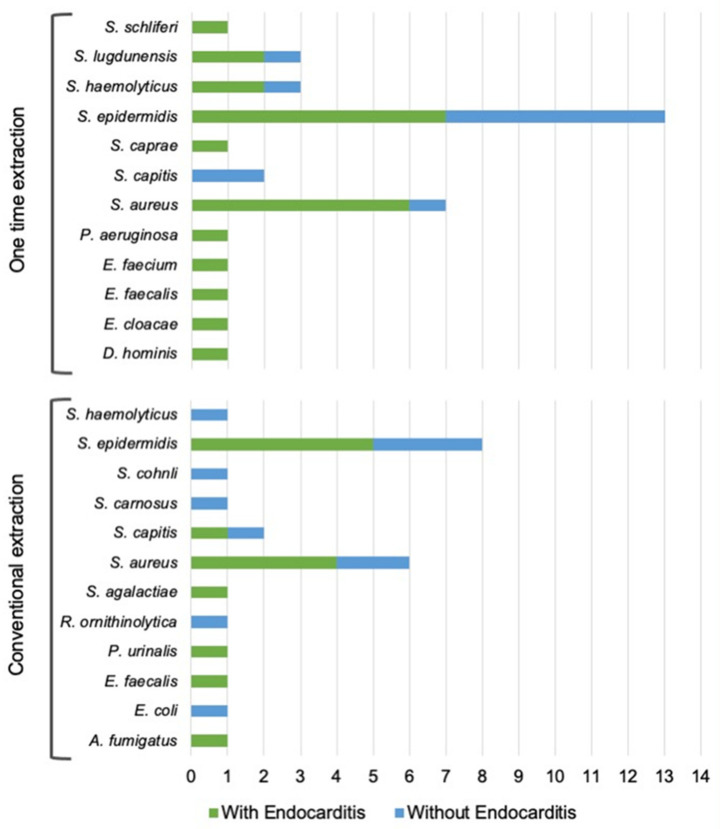
A total of 58 strains were isolated overall, 35 in the single-procedure and 23 in the SoC group. S. epidermidis was the most prevalent pathogen (37.1%, in the single-procedure and 30.4% in the SoC group), followed by S. aureus (20.0% single-procedure and 26.1% SoC). All pathogen distributions are reported in Figure 1. Methicillin resistance rates varied from 33.3% for S. haemolyticus to 100% for the single strain of S. hominis in the single-procedure group. Only S. epidermidis and S. aureus showed methicillin resistance (42.9% and 16.7%, respectively) in the SoC group, compared with 61.5% and 42.9% for the same pathogens, respectively, in the single-procedure group. Other pathogens, including Gram-negative bacteria and fungi, were also isolated. Tissue cultures and catheters sent for culture most often yielded S. epidermidis. Refer to Figure 1 for further data.
Figure 1.
Pathogens responsible for CIED infections in both the single-procedure group and the SoC group.
Overall, 33.3% and 53.6% of patients in the single-procedure and the SoC cohorts, respectively, were undergoing antibiotic therapy upon hospital admission, with no differences in the two sets of patients. Anti-Gram-negative antibiotic therapy was reported in similar proportions (25.9% and 23.0% in the single-procedure and SoC groups, respectively). Upon hospital admission, 88.9% of patients from the single-procedure group and 100% of patients in the SoC group were administered antibiotics. Significantly different proportions of patients received an active antibiofilm antimicrobial therapy (including daptomycin or rifampicin, alone or in combination with a beta-lactam, especially novel fifth-generation molecules). Active antibiofilm therapy was administered in 81.5% of the single-procedure patients, while only 38.5% of patients from the SoC group received similar treatments, with a significant difference between the two groups (p = 0.001). Anti-Gram-negative antibiotic therapy was administered in 74.1% of the single-procedure and 38.5% of SoC cases (p = 0.006), respectively. Data concerning treatments and devices are detailed in Table 1.
Overall, 18.5% and 12.5% of patients were lost to follow-up (FU) in the single-procedure and SoC groups, respectively, while the rest were followed up for 12 months post-procedure. No serious adverse events related to the procedure or the antibiotic therapy occurred. No re-infection was reported in the followed-up population.
Considering those lost to FU, there were no statistically significant differences in mortality rates among both cohorts, with survival rates of patients available at follow-up at one year of 81.5% in the single-procedure group and 84.6%% in the SoC group (p = 0.737).
4. Discussion
As rates of CIED implants increase, the concomitant growing complexity of patients and procedures implies greater infection rates, consequently hindering life expectancy and quality.
Guidelines and consensus suggest waiting for the absence of signs and symptoms of infections (local and/or systemic) and for persistently negative blood cultures for at least 72 h post-extraction. The waiting period should be extended to 14 days before reimplanting in the presence of valvular vegetations. Evidence and indications are supported by the low quality of the evidence and expert consensus [1,14,33], and there are currently no randomized trials addressing the timing of reimplantation in CIED infections.
As a result, the currently advised timing from explant to implant is still based on limited evidence; therefore, the higher risk of infection in early reimplanting may be due to inadequate infection eradication. On the other hand, delaying reimplantation may be just as threatening due to potential adverse events related to the absence of the devices or electrical therapies, especially in heart failure patients, along with the potential acquisition of nosocomial infections [34]. Of course, the need for a temporary pacing lead in pacemaker-dependent patients waiting for reimplantation can increase the risk of thrombosis and perforation. Bridging with leadless devices is nowadays available to reduce this issue, though poor evidence is available on the possible benefits [35]. Hence, decisions on proper treatment should consider the overall factors and risks and should be customized according to feasibility and patient features. While waiting a couple of days may be reasonable in some instances presenting with lower severity, a 2- to 3-day delay while waiting for cultures to clear before device reimplantation may be challenging in dependent or frail patients. Moreover, incubation periods for blood cultures vary widely across laboratories and countries; guidelines suggest a minimum of 5 days [1,36], which may be extended to over 2 weeks in cases of fastidious or atypical organisms [1]. This generally contemplates a minimum waiting period of 7–8 days before reimplantation, implying an increased length of stay along with the associated costs and increased risks of acquiring nosocomial infections. Conventional practice is in line with guideline timings, with a median wait time of 3–7 days in the published series [19].
Increasing evidence suggests that the benefit–risk ratio of delaying permanent device reimplantation in a high-risk patient population is possibly limited, given a lower risk of reinfection. Findings from a systematic review and meta-analysis by Chew et al. did not support a greater risk of infection and negative outcomes in single-procedure extraction and implant. Indeed, the authors found that reimplantation beyond 72 h was associated with increased infection rates [34]. In line with their data, our observations indicate no increased risk of negative outcome and reinfection. Indeed, there were no statistical differences in outcome at 12 months. Death rates were similar across both groups, with a 12-month survival rate of 81.5% in the single-procedure and 84.6% in the SoC group, respectively (p = 0.075). Lost to follow-up rates were similar, with 18.5% and 15.4% in the single-procedure and SoC groups, respectively (p = 0.737).
In the single-procedure group, patients were followed up for 4 years, and no further deaths attributable to CIED-related infections or relapses were reported. Two patients died due to COVID-19. No other safety events were reported in the followed-up patients.
Hence, though the single procedure of extraction and reimplantation is deemed safe for patients with localized infections only and with negative pre-procedure blood cultures, our data suggest it may be feasible when applied to selected cohorts.
A similar approach has also been pursued in infected prosthetic joint infections, where a two-stage exchange is the technique of choice. While some drawbacks exist, such as peri-operative mortality, increased hospitalization length and increased healthcare costs are associated with the SoC. For all these reasons, especially in extremes of age, the single-procedure reimplant is advised in the presence of conditions that avoid relapse [37]. On the same line, a similar approach thus may be considered for some patient groups requiring device management and at high risk of negative outcomes.
Moreover, timing may also be dependent on the causative pathogen. Sohail et al. reported a median time of reimplantation of 7 days for non-bacteremic patients versus 13 days in cases of bacteremic patients. However, there was a difference in the causative organisms. Indeed, the median waiting time was 12 days in cases of S. aureus versus 7 days for coagulase-negative staphylococci (CoNS) [38].
Albeit not statistically assessed, the microbiology findings from both cohorts were similar and in line with those in other reported series, with coagulase-negative Staphylococcus spp. being the most prevalent pathogens. However, the single-procedure extraction and reimplantation cohort presented with numerically higher resistance rates and hypervirulent strains. Similar to Sohail et al., our case single-procedure series included seven S. aureus (42.9% methicillin-resistant S. aureus [MRSA] versus 16.7% in the SoC group) and three hypervirulent CoNS such as S. lugdunensis, while S. epidermidis also showed 61.5% resistance rates (versus 42.8% in the SoC group). In all cases, irrespective of resistance and strain, patients were re-implanted in the single-procedure group without relapsing.
In accordance with these observations, longer courses of antibiotics are generally needed in addition to device extraction when bacteremia is initially present. A previous study by Mountantonakis et al. included 15 patients without bacteremia or positive blood cultures [19], while systemic infection was reported in 18 of the 68 patients from the Nandyala et al. study, adding to the complexity of the overall cohort [18]. Just like Nandyala et al., our cohorts were also quite heterogeneous and at elevated risk of negative outcomes. In our observations, almost one-third presented with bacteremia in the single-procedure group, with a similar proportion in the SoC patient population. Moreover, three patients in the single-procedure group (11.1%) and one in the SoC group (5.1%) also presented with sepsis.
Endocarditis and concomitant bacteremia was present in eight (29.6%) and six (15.4%) of the cases in the single-procedure and SoC groups, respectively, where a positive effect of the beta-lactam combination with daptomycin/rifampicin may be more impactful [39,40,41,42].
Hence, given the current availability of novel and more active treatments with antibiofilm activity, a different approach might be worthy of consideration. Indeed, in the single-procedure reimplantation cohort, most patients underwent therapy with antibiofilm and novel agents (81.5% versus 38.5%, p = 0.001) with displayed potent activity on Gram-positive bacteria, while also offering coverage of difficult-to-treat and resistant pathogens, especially MRSA [22,25,26,42,43]. The optimal treatment for S. aureus bacteremia and/or infective endocarditis remains a subject of debate. Some in vitro studies have demonstrated the synergism between daptomycin and beta-lactams, as beta-lactam antibiotics seem to increase the sensitivity of the bacterium to daptomycin (“seesaw effect”) [44]. However, some clinical studies failed to demonstrate a positive effect of the daptomycin/beta-lactam combination therapy compared with monotherapy in terms of mortality and duration of bacteremia, particularly for MRSA bacteremia [40,41]. Further clinical studies are needed to compare daptomycin/beta-lactam combination therapy with monotherapy for CIED infections, which are frequently associated with bacterial biofilm formation, as mentioned above.
Because early and appropriate treatment is known to account for increased survival rates and decreased incidence of endocarditis complications [45], the increased availability of active molecules with biofilm penetration and a favorable pharmacokinetic/pharmacodynamic index may encourage a paradigm shift in such contexts when complexity may hinder standard-of-care approaches leading to longer times to reimplantation.
We recently reported a case of a single-procedure patient with metallo-beta-lactamase producing, meropenem-resistant P. aeruginosa endocarditis, who was reimplanted during imipenem plus aztreonam therapy and continued with imipenem and cefiderocol therapy. We showed that the P. aeruginosa strain was a biofilm producer and that the combination of imipenem and cefiderocol was synergistic against this P. aeruginosa in a biofilm in vitro test [46].
5. Conclusions
While limited to a relatively small number of patients, the data from the present study support the safety of the single-procedure extraction and reimplantation of devices, even in the presence of MDR and difficult-to-treat species or concomitant bacteremia. While extraction timing may be complex in such patients, waiting may not always be feasible. As a result, a single-procedure extraction and contralateral replacement may represent a potentially optimal solution in such instances. Moreover, the growing availability of novel molecules with greater efficacy and biofilm activity may also offer support by providing coverage and avoiding relapse.
Similar to the observations of Nandyala et al. [18], our single-procedure patient group presented with a high risk of negative outcomes and an urgent need for device reimplantation. The presence of systemic infections implied a greater risk of reinfection to a certain degree. However, aggressive antibiotic treatment may have favored early clearance and sterilization even in such a cohort, where same-day or single-procedure reimplantation may represent the strategy with the best risk/benefit balance. To this extent, the 1-year follow-up revealed no re-infections or deaths due to CIED complications.
Finally, no statistically significant differences in mortality or relapses were observed, with similar rates of patients lost to follow-up. No re-infections were reported in both cohorts, supportive of the safety and feasibility of the single-procedure approach.
The limitations of the study include its retrospective nature along with the heterogeneous antibiotic approach. In addition, the lack of randomization and clustering management in two different centers may have introduced potential bias where surgical management is concerned. Furthermore, the SoC approach referred to only the pacemaker infections in an attempt to reduce the complexity of the patients cared for in a national reference center.
To conclude, our data suggest that tailoring time to reimplantation in patients with limited alternatives and adjunctive active antibiofilm therapy may represent a novel and more feasible approach in a selected cohort of patients.
Further research is warranted in order to define the best treatment regimen and strategies to define patient selection in order to minimize the length of stay (LoS) and bed occupancy when unnecessary.
Author Contributions
Conceptualization, C.T.; methodology, C.T. and A.R.; software, A.R.; validation, C.T., G.Z. and S.D.V.; formal analysis, G.M.L.; investigation, S.G., V.A., L.S., S.S., C.S., S.H.W., A.Z.-F., G.M.L., N.C., M.G.B. and A.D.C.; resources, V.A., L.S., S.S., C.S., S.H.W., N.C., M.G.B. and A.D.C.; data curation, A.R.; writing—original draft preparation, C.T., F.S. and G.M.L.; writing—review and editing, G.M.L., S.D.V. and G.Z.; visualization, F.S.; supervision, C.T.; project administration, C.T.; funding acquisition, C.T., G.Z. and S.D.V. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, but approval by any ethics committee was not required because it is a retrospective observational study.
Informed Consent Statement
Patient consent was waived due to the use of retrospective data routinely collected in an anonymous manner.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy reasons.
Conflicts of Interest
C.T. has received funds for speaking at symposia organized on behalf of Pfizer, Novartis, Merck Gilead, Zambon, Infectopharm, Sionogy, Menarini, Angelini, and Astellas; M.G.B. has received honoraria from Abbott Medical Italia Società Per Azioni, Biotronik, Boston Scientific, and Medtronic. The other authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Blomström-Lundqvist C., Traykov V., Erba P.A., Burri H., Nielsen J.C., Bongiorni M.G., Poole J., Boriani G., Costa R., Deharo J.-C., et al. European Heart Rhythm Association (EHRA) international consensus document on how to prevent, diagnose, and treat cardiac implantable electronic device infections—Endorsed by the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Society (APHRS), the Latin American Heart Rhythm Society (LAHRS), International Society for Cardiovascular Infectious Diseases (ISCVID) and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS) EP Eur. 2020;22:515–549. doi: 10.1093/europace/euz246. [DOI] [PubMed] [Google Scholar]
- 2.Greenspon A.J., Patel J.D., Lau E., Ochoa J.A., Frisch D.R., Ho R.T., Pavri B.B., Kurtz S.M. 16-Year Trends in the Infection Burden for Pacemakers and Implantable Cardioverter-Defibrillators in the United States. J. Am. Coll. Cardiol. 2011;58:1001–1006. doi: 10.1016/j.jacc.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 3.Hernández-Meneses M., Llopis J., Sandoval E., Ninot S., Almela M., Falces C., Pericàs J.M., Vidal B., Perissinotti A., Marco F., et al. Forty-Year Trends in Cardiac Implantable Electronic Device Infective Endocarditis. Open Forum. Infect. Dis. 2022;9:ofac547. doi: 10.1093/ofid/ofac547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phillips P., Krahn A.D., Andrade J.G., Chakrabarti S., Thompson C.R., Harris D.J., Forman J.M., Karim S.S., Sterns L.D., Fedoruk L.M., et al. Treatment and Prevention of Cardiovascular Implantable Electronic Device (CIED) Infections. CJC Open. 2022;4:946–958. doi: 10.1016/j.cjco.2022.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mond H.G., Proclemer A. The 11th World Survey of Cardiac Pacing and Implantable Cardioverter-Defibrillators: Calendar Year 2009—A World Society of Arrhythmia’s Project: 2009 Survey Cardiac Pacemakers and Icds. Pacing Clin. Electrophysiol. 2011;34:1013–1027. doi: 10.1111/j.1540-8159.2011.03150.x. [DOI] [PubMed] [Google Scholar]
- 6.Valzania C., Torbica A., Tarricone R., Leyva F., Boriani G. Implant rates of cardiac implantable electrical devices in Europe: A systematic literature review. Health Policy. 2016;120:1–15. doi: 10.1016/j.healthpol.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Raatikainen M.J.P., Arnar D.O., Merkely B., Nielsen J.C., Hindricks G., Heidbuchel H., Camm J. A Decade of Information on the Use of Cardiac Implantable Electronic Devices and Interventional Electrophysiological Procedures in the European Society of Cardiology Countries: 2017 Report from the European Heart Rhythm Association. EP Eur. 2017;19:ii1–ii90. doi: 10.1093/europace/eux258. [DOI] [PubMed] [Google Scholar]
- 8.Voigt A., Shalaby A., Saba S. Continued Rise in Rates of Cardiovascular Implantable Electronic Device Infections in the United States: Temporal Trends and Causative Insights. Pacing Clin. Electrophysiol. 2010;33:414–419. doi: 10.1111/j.1540-8159.2009.02569.x. [DOI] [PubMed] [Google Scholar]
- 9.Polyzos K.A., Konstantelias A.A., Falagas M.E. Risk factors for cardiac implantable electronic device infection: A systematic review and meta-analysis. EP Eur. 2015;17:767–777. doi: 10.1093/europace/euv053. [DOI] [PubMed] [Google Scholar]
- 10.Wilkoff B.L., Boriani G., Mittal S., Poole J.E., Kennergren C., Corey G.R., Love J.C., Augostini R., Faerestrand S., Wiggins S.S., et al. Impact of Cardiac Implantable Electronic Device Infection: A Clinical and Economic Analysis of the WRAP-IT Trial. Circ. Arrhythmia Electrophysiol. 2020;13:e008280. doi: 10.1161/CIRCEP.119.008280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bongiorni M.G., Tascini C., Tagliaferri E., Cori A.D., Soldati E., Leonildi A., Zucchelli G., Ciullo I., Menichetti F. Microbiology of cardiac implantable electronic device infections. Europace. 2012;14:1334–1339. doi: 10.1093/europace/eus044. [DOI] [PubMed] [Google Scholar]
- 12.Korkerdsup T., Ngarmukos T., Sungkanuparph S., Phuphuakrat A. Cardiac implantable electronic device infection in the cardiac referral center in Thailand: Incidence, microbiology, risk factors, and outcomes. J. Arrhythmia. 2018;34:632–639. doi: 10.1002/joa3.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagpal A., Baddour L.M., Sohail M.R. Microbiology and Pathogenesis of Cardiovascular Implantable Electronic Device Infections. Circ. Arrhythmia Electrophysiol. 2012;5:433–441. doi: 10.1161/CIRCEP.111.962753. [DOI] [PubMed] [Google Scholar]
- 14.Kusumoto F.M., Schoenfeld M.H., Wilkoff B.L., Berul C.I., Birgersdotter-Green U.M., Carrillo R., Cha Y.-M., Clancy J., Deharo J.-C., Ellenbogen K.A., et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm. 2017;14:e503–e551. doi: 10.1016/j.hrthm.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Zucchelli G., Bongiorni M.G., Di Cori A., Soldati E., Solarino G., Fabiani I., Segreti L., De Lucia R., Viani S., Coluccia G., et al. Cardiac resynchronization therapy after coronary sinus lead extraction: Feasibility and mid-term outcome of transvenous reimplantation in a tertiary referral centre. Europace. 2012;14:515–521. doi: 10.1093/europace/eur339. [DOI] [PubMed] [Google Scholar]
- 16.Tarakji K.G., Chan E.J., Cantillon D.J., Doonan A.L., Hu T., Schmitt S., Fraser T.G., Kim A., Gordon S.M., Wilkoff B.L. Cardiac implantable electronic device infections: Presentation, management, and patient outcomes. Heart Rhythm. 2010;7:1043–1047. doi: 10.1016/j.hrthm.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 17.Amraoui S., Sohal M., Li A., Williams S., Scully P., Jackson T., Claridge S., Behar J., Ritter P., Barandon L., et al. Comparison of delayed transvenous reimplantation and immediate surgical epicardial approach in pacing-dependent patients undergoing extraction of infected permanent pacemakers. Heart Rhythm. 2015;12:1209–1215. doi: 10.1016/j.hrthm.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 18.Nandyala R., Parsonnet V. One stage side-to-side replacement of infected pulse generators and leads. Pacing Clin. Electrophysiol. 2006;29:393–396. doi: 10.1111/j.1540-8159.2006.00359.x. [DOI] [PubMed] [Google Scholar]
- 19.Mountantonakis S.E., Tschabrunn C.M., Deyell M.W., Cooper J.M. Same-day contralateral implantation of a permanent device after lead extraction for isolated pocket infection. Europace. 2014;16:252–257. doi: 10.1093/europace/eut220. [DOI] [PubMed] [Google Scholar]
- 20.Kim S.S., Philips B., Smelley M., Shah D., Weisberg I., Mishra A., Lin A.C., Beshai J.F., Knight B.P., Burke M.C. Abstract 2491: Same-Day Device Reimplantation Following Cardiovascular Implantable Electronic Device Extraction for Isolated Pocket Infection. Circulation. 2009;120:S649. [Google Scholar]
- 21.Habib G., Lancellotti P., Antunes M.J., Bongiorni M.G., Casalta J.-P., Del Zotti F., Dulgheru R., El Khoury G., Erba P.A., Iung B., et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM) Eur. Heart J. 2015;36:3075–3128. doi: 10.1093/eurheartj/ehv319. [DOI] [PubMed] [Google Scholar]
- 22.Abbanat D., Shang W., Amsler K., Santoro C., Baum E., Crespo-Carbone S., Lynch A.S. Evaluation of the in vitro activities of ceftobiprole and comparators in staphylococcal colony or microtitre plate biofilm assays. Int. J. Antimicrob. Agents. 2014;43:32–39. doi: 10.1016/j.ijantimicag.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 23.Barber K.E., Werth B.J., McRoberts J.P., Rybak M.J. A Novel Approach Utilizing Biofilm Time-Kill Curves To Assess the Bactericidal Activity of Ceftaroline Combinations against Biofilm-Producing Methicillin-Resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2014;58:2989–2992. doi: 10.1128/AAC.02764-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barber K.E., Smith J.R., Ireland C.E., Boles B.R., Rose W.E., Rybak M.J. Evaluation of Ceftaroline Alone and in Combination against Biofilm-Producing Methicillin-Resistant Staphylococcus aureus with Reduced Susceptibility to Daptomycin and Vancomycin in an In Vitro Pharmacokinetic/Pharmacodynamic Model. Antimicrob. Agents Chemother. 2015;59:4497–4503. doi: 10.1128/AAC.00386-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barber K.E., Shammout Z., Smith J.R., Kebriaei R., Morrisette T., Rybak M.J. Biofilm Time-Kill Curves to Assess the Bactericidal Activity of Daptomycin Combinations against Biofilm-Producing Vancomycin-Resistant Enterococcus faecium and faecalis. Antibiotics. 2021;10:897. doi: 10.3390/antibiotics10080897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cirioni O., Mocchegiani F., Ghiselli R., Silvestri C., Gabrielli E., Marchionni E., Orlando F., Nicolini D., Risaliti A., Giacometti A. Daptomycin and Rifampin Alone and in Combination Prevent Vascular Graft Biofilm Formation and Emergence of Antibiotic Resistance in a Subcutaneous Rat Pouch Model of Staphylococcal Infection. Eur. J. Vasc. Endovasc. Surg. 2010;40:817–822. doi: 10.1016/j.ejvs.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Byrd C.L., Schwartz S.J., Hedin N.B., Goode L.B., Fearnot N.E., Smith H.J. Intravascular Lead Extraction Using Locking Stylets and Sheaths. Pacing Clin. Electrophysiol. 1990;13:1871–1875. doi: 10.1111/j.1540-8159.1990.tb06906.x. [DOI] [PubMed] [Google Scholar]
- 28.Bongiorni M.G., Segreti L., Di Cori A., Zucchelli G., Viani S., Paperini L., De Lucia R., Boem A., Levorato D., Soldati E. Safety and efficacy of internal transjugular approach for transvenous extraction of implantable cardioverter defibrillator leads. Europace. 2014;16:1356–1362. doi: 10.1093/europace/euu004. [DOI] [PubMed] [Google Scholar]
- 29.Kennergren C. First European experience using excimer laser for the extraction of permanent pacemaker leads. Pt 2Pacing Clin. Electrophysiol. 1998;21:268–270. doi: 10.1111/j.1540-8159.1998.tb01102.x. [DOI] [PubMed] [Google Scholar]
- 30.Wilkoff B.L., Byrd C.L., Love C.J., Hayes D.L., Sellers T.D., Schaerf R., Parsonnet V., Epstein L.M., Sorrentino R.A., Reiser C. Pacemaker lead extraction with the laser sheath: Results of the pacing lead extraction with the excimer sheath (PLEXES) trial11No financial support was received for performing the procedures or collecting the data, or for data analysis. J. Am. Coll. Cardiol. 1999;33:1671–1676. doi: 10.1016/S0735-1097(99)00074-1. [DOI] [PubMed] [Google Scholar]
- 31.Byrd C.L., Wilkoff B.L., Love C.J., Sellers T.D., Reiser C. Clinical Study of the Laser Sheath for Lead Extraction: The Total Experience in the United States. Pacing Clin. Electrophysiol. 2002;25:804–808. doi: 10.1046/j.1460-9592.2002.t01-1-00804.x. [DOI] [PubMed] [Google Scholar]
- 32.R Core Team . R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2022. [Google Scholar]
- 33.Baddour L.M., Epstein A.E., Erickson C.C., Knight B.P., Levison M.E., Lockhart P.B., Masoudi F.A., Okum E.J., Wilson W.R., Beerman L.B., et al. Update on Cardiovascular Implantable Electronic Device Infections and Their Management: A Scientific Statement From the American Heart Association. Circulation. 2010;121:458–477. doi: 10.1161/CIRCULATIONAHA.109.192665. [DOI] [PubMed] [Google Scholar]
- 34.Chew D., Somayaji R., Conly J., Exner D., Rennert-May E. Timing of device reimplantation and reinfection rates following cardiac implantable electronic device infection: A systematic review and meta-analysis. BMJ Open. 2019;9:e029537. doi: 10.1136/bmjopen-2019-029537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zucchelli G., Barletta V., Della Tommasina V., Viani S., Parollo M., Mazzocchetti L., Cellamaro T., Paperini L., Di Cori A., De Lucia R., et al. Micra pacemaker implant after cardiac implantable electronic device extraction: Feasibility and long-term outcomes. EP Eur. 2019;21:1229–1236. doi: 10.1093/europace/euz160. [DOI] [PubMed] [Google Scholar]
- 36.Ransom E.M., Alipour Z., Wallace M.A., Burnham C.-A.D. Evaluation of Optimal Blood Culture Incubation Time To Maximize Clinically Relevant Results from a Contemporary Blood Culture Instrument and Media System. J. Clin. Microbiol. 2021;59:e02459-20. doi: 10.1128/JCM.02459-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zanna L., Sangaletti R., Lausmann C., Gehrke T., Citak M. Successful eradication rate following one-stage septic knee and hip exchange in selected pre-operative culture-negative periprosthetic joint infections. Int. Orthop. 2023;47:659–666. doi: 10.1007/s00264-022-05677-7. [DOI] [PubMed] [Google Scholar]
- 38.Sohail M.R., Uslan D.Z., Khan A.H., Friedman P.A., Hayes D.L., Wilson W.R., Steckelberg J.M., Stoner S., Baddour L.M. Management and Outcome of Permanent Pacemaker and Implantable Cardioverter-Defibrillator Infections. J. Am. Coll. Cardiol. 2007;49:1851–1859. doi: 10.1016/j.jacc.2007.01.072. [DOI] [PubMed] [Google Scholar]
- 39.Cuervo G., Escrihuela-Vidal F., Gudiol C., Carratalà J. Current Challenges in the Management of Infective Endocarditis. Front. Med. 2021;8:641243. doi: 10.3389/fmed.2021.641243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grillo S., Cuervo G., Carratalà J., Grau I., Tebé C., Tió L.G., Murillo O., Ardanuy C., Domínguez A., Shaw E., et al. Impact of beta-lactam and daptomycin combination therapy on clinical outcomes in methicillin-susceptible Staphylococcus aureus bacteremia: A propensity score-matched analysis. Clin. Infect. Dis. 2019;69:1480–1488. doi: 10.1093/cid/ciz018. [DOI] [PubMed] [Google Scholar]
- 41.Cheng M.P., Lawandi A., Butler-Laporte G., De l’Étoile-Morel S., Paquette K., Lee T.C. Adjunctive Daptomycin in the Treatment of Methicillin-susceptible Staphylococcus aureus Bacteremia: A Randomized, Controlled Trial. Clin. Infect. Dis. 2021;72:e196–e203. doi: 10.1093/cid/ciaa1000. [DOI] [PubMed] [Google Scholar]
- 42.Tascini C., Attanasio V., Ripa M., Carozza A., Pallotto C., Bernardo M., Francisci D., Oltolini C., Palmiero G., Scarpellini P. Ceftobiprole for the treatment of infective endocarditis: A case series. J. Glob. Antimicrob. Resist. 2020;20:56–59. doi: 10.1016/j.jgar.2019.07.020. [DOI] [PubMed] [Google Scholar]
- 43.Canton R., Hamed K., Wiktorowicz T., Redder N., Jemmely N., Quevedo J., Santerre Henriksen A. In vitro activity of ceftobiprole and comparator antibiotics against contemporary European isolates (2016–2019) JAC Antimicrob. Resist. 2022;4:dlac030. doi: 10.1093/jacamr/dlac030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barber K.E., Werth B.J., Ireland C.E., Stone N.E., Nonejuie P., Sakoulas G., Pogliano J., Rybak M.J. Potent synergy of ceftobiprole plus daptomycin against multiple strains of Staphylococcus aureus with various resistance phenotypes. J. Antimicrob. Chemother. 2014;69:3006–3010. doi: 10.1093/jac/dku236. [DOI] [PubMed] [Google Scholar]
- 45.Dickerman S.A., Abrutyn E., Barsic B., Bouza E., Cecchi E., Moreno A., Doco-Lecompte T., Eisen D.P., Fortes C.Q., Fowler V.G., et al. The relationship between the initiation of antimicrobial therapy and the incidence of stroke in infective endocarditis: An analysis from the ICE Prospective Cohort Study (ICE-PCS) Am. Heart J. 2007;154:1086–1094. doi: 10.1016/j.ahj.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 46.Tascini C., Antonelli A., Pini M., De Vivo S., Aiezza N., Bernardo M., Di Luca M., Rossolini G.M. Infective Endocarditis Associated with Implantable Cardiac Device by Metallo-β-Lactamase-Producing Pseudomonas aeruginosa, Successfully Treated with Source Control and Cefiderocol Plus Imipenem. Antimicrob. Agents Chemother. 2023;67:e01313-22. doi: 10.1128/aac.01313-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy reasons.