Highlights
-
•
Evidence alone does not guarantee the use of evidence in decision-making.
-
•
Evidence and values are needed to make an optimal decision.
-
•
VEDMAP is a novel and flexible decision-making framework.
-
•
The VEDMAP framework aligns values and evidence to produce an optimal decision.
-
•
The VEDMAP scorecard packages evidence for easier understanding for policy and decision-makers.
Keywords: VEDMAP, Evidence-based decision making, Health policy, Malawi, Decision-making
Abstract
The existence and availability of evidence on its own does not guarantee that the evidence will be demanded and used by decision and policy makers. Decision and policy-makers, especially in low-income settings, often confront ethical dilemmas about determining the best available evidence and its utilization. This dilemma can be in the form of conflict of evidence, scientific and ethical equipoise and competing evidence or interests. Consequently, decisions are made based on convenience, personal preference, donor requirements, and political and social considerations which can result in wastage of resources and inefficiency. To mitigate these challenges, the use of “Value- and Evidence-Based Decision Making and Practice” (VEDMAP) framework is proposed. This framework was developed by Joseph Mfutso-Bengo in 2017 through a desk review. It was pretested through a scoping study under the Thanzi la Onse (TLO) Project which assessed the feasibility and acceptability of using the VEDMAP as a priority setting tool for Health Technology Assessment (HTA) in Malawi. The study used mixed methods whereby it conducted a desk review to map out and benchmark normative values of different countries in Africa and HTA; focus group discussion and key informant interviews to map out the actual (practised) values in Malawi. The results of this review confirmed that the use of VEDMAP framework was feasible and acceptable and can bring efficiency, traceability, transparency and integrity in decision- policy making process and implementation.
1. Introduction
Many low and middle income countries (LMICs) including Malawi have embarked on health system reforms aimed at achieving Universal Health Coverage (UHC) [1]. Implementing sound health policies and strengthening health and financial systems are some of the ways UHC can be achieved [2]. Health care delivery in Malawi is primarily through government facilities. As a low income country with a narrow financial resource envelope and competing unmet demands, the Malawian healthcare system is heavily dependent on donor aid (Masefield,2020). Despite availability of free healthcare services, there are challenges that still persist such as travel costs to public health facilities from hard to reach areas [3]. Despite availability of free healthcare services, there are challenges that still persist such as travel costs to public health facilities from hard to reach areas where the majority of the poor populations live, insufficient drug stock, low quality services delivery, inadequate qualified staff, and chronic funding shortages (Nakovics,2020). To ensure the sustainability of the healthcare system, improvements in governance, evidence -based policy and decision- making are therefore inevitable [4]. To ensure the sustainability of the healthcare system, improvements in governance, evidence-based policy and decision- making are therefore inevitable.
There is consensus that policy making should be evidence-based and informed [5]. To create demand and application of evidence, Malawi, among other LMICs, under the Evidence-Informed Policy Network (EVIPNet), created the Knowledge Translation Platforms (KTPs) [6]. KTPs have been defined as organizations, initiatives and networks that focus on supporting evidence-informed policymaking. They set out the governance; evaluate programmes, services and products to ensure they are delivered to meet the needs of the population [7]. These platforms aim to generate, assess, translate and package evidence into a precise and straightforward format to facilitate the use of the best available evidence to inform new policies or improve existing policies, policy making and analysis. KTPs root themselves in evidence-based decision making (EBDM). EBDM has been defined in the clinical setting as the formalized process of using the skills for identifying, searching for, and interpreting the results of the best scientific evidence, which is considered in conjunction with the clinician's experience and judgment, the patient's preferences and values, and the clinical/patient circumstances when making patient care decisions [8]. The use of EBDM in a policy setting ensures that relevant and rigorous data is critiqued and informs decision-making. Evidence increases the likelihood of meeting the intended health policy goals, including discovering solutions to emerging health challenges [9] However, mistrust between policy makers and researchers, particularly in LMICs [19] results in little or no demand for evidence [11]. Consequently, evidence is often ignored in the decision-making process even if it exists and is available [12], [13]. Therefore, KTPs are repeatedly faced with the ethical dilemma of determining the best available evidence, satisfying the needs of interest and lobby groups; remaining impartial to political influences and deciding how best to manage limited resources [12]. A possible solution to address this dilemma would be the use of value-based decision making (VBDM). VBDM refers to weighing of cost against the benefits of the available options to arrive at an optimal decision. The options can be explicit, small or large rewards resulting from the different costs, or implicit, whether or not to continue behaviors that are no longer enforced [12]. VBDM serves as an ethical or moral compass that guides the decision-making process to ensure that decisions made reflect the goals of an organization or health care system. VBDM examines context-specific values, focusing on what an organization aims to achieve and looking beyond cost-effectiveness. Unfortunately, this decision-making process is not always supported by evidence [12], resulting in subjective decision-making, which can be inefficient and ineffective. LMICs like Malawi lack proper linkage between evidence generation and utilization of the best available evidence through policymaking. The weak linkage led to the development of the “Value- and Evidence-Based Decision Making and Practice” (VEDMAP), a novel framework that states that values and evidence cannot live in isolation. The framework is based on the premise that values for optimal organizational decision making should complement evidence-based decisions. For instance, if the evidence is not valued where corruption runs high, evidence can easily be ignored, and corruption continues. Recognizing that professional or organizational values play a critical role in motivating professional practice, VEDMAP makes explicit the values ideal for decision making and supports the identified values with rigorous evidence, thereby aligning the values to organizational goals. This would thus result in optimal decision making. In this regard, VEDMAP is a decision-making framework designed to translate organizational values into practice. This paper aims to describe and assess applicability of VEDMAP framework in improving decision-making in LMIC settings like Malawi.
2. The development of VEDMAP
“The VEDMAP framework was developed due to a gap identified in evidence generation, and evidence packaging and evidence utilization. There has been awareness that despite the availability of best available evidence, due to lack of appropriate values, the best evidence was neither demanded nor utilized. In published literature, and concerns from the Ministry of Health about the technical, complex and voluminous amount of evidence presented to them during policy and decision-making. The poor presentation of evidence and the lack of value mapping in guiding decisions led to a proposal titled; “Assessing the acceptability and feasibility of using VEDMAP as a decision modelling tool for HTA and its potential to map out values for HTA decision-making.” being submitted to the TLO flexible fund for funding which was reviewed and approved by the College of Medicine Research Ethics Committee.
3. Evidence and Value-Based Decision-Making frameworks
3.1. Evidence-Based decision making (EBDM)
EBDM uses a set of norms, initiatives and methods, specifically systematic reviews, to improve the use of evidence in policy and decision making. As a key development initiative, EBDM uses the best available scientific evidence regarding the effectiveness of various programs and policies and translates evidence into real-world practice by incorporating community-level data, resources and priorities [12], [13], [14]. Policies supported by evidence often provide an in-depth analysis and understanding of a problem for that particular context and focus on identifying potential solutions [9], [15], thereby increasing transparency, equity and accountability in policy making. From an economic perspective, EBDM can reduce the wastage of scarce public resources [14], thus increasing government capacity to improve efficiency and the quality of services. On the other hand, non-evidence decision making results in public policies and programs that are introduced at a substandard scale resulting in well-intended programs that can have unintended outcomes [16]. This underscores a social and ethical need to consider evidence during policy design and implementation [14]. A disconnect between moral support and practical application [14], [17], [18], unavailability of context-specific data, poor communication and dissemination of data and the lack of technical support are significant barriers in EBDM limiting understanding of the message presented by the data and its importance [19]. Evidence is seldom adequate, and the research conducted is not always used to inform the ultimate decision but is instead used to motivate, persuade or defend decisions already made [20]. Furthermore, there is little demand for evidence from officials, possibly due to lack of incentivization or lack of appetite for transparent and effective evaluation [18], [20], [21]. Cronin and Sadan (2015) stated that there is a lack of shared values and standards to guide and assess policy development practices, leading to inconsistent use of EBDM approaches due to a lack of expertise and resources; lack of evidence-based programs which can be adapted to local contexts [20], [22]. This is possibly why a minority of senior decision-makers and policymakers use evidence in policy making [14], [18], [20].
3.2. Why is EBDM preferred over evidence informed decision making (EIDM)?
It has been argued by the proponents [23] of EIDM that a more practical way of making decisions is when the evidence is not exclusive of other considerations, for instance experience, values and client preferences. Nevo & Slonim‐Nevo, (2011) are of the view that the application of evidence in decision-, policy making and practice should, in principle, be “informed by” evidence and not necessarily “based on” evidence alone [32]. This suggests that decision, policy- making and practice “might be enriched by prior research but not limited to it” [33]. Having observed this, VEDMAP framework prefers EBDM to EIDM because it brings other considerations to evidence decision-making without reducing the importance and primacy of evidence, such values that include personal preferences, experience, ethical, social, political, cultural, technological and environmental determinants. Therefore, the preference weighs more on EBDM because, EIDM may run a risk of totally ignoring the best available evidence in the favour of political interests as well as personal preferences. This has been evident in many African countries and beyond where best available evidence has been ignored in favour of personal and political interest at the expense of public good [24]. This is the case when evidence is considered as one among many, and not first among many.
3.3. Value-Based decision making (VBDM)
Values are principles or standards that reflect the common morality among a group of people [12], [21] that motivates and guides actions to desirable goals [25]. VBDM is an ethical or moral compass that guides the decision-making process ensuring that decision making demonstrates the vision of a healthcare system [26]. It also guides the process of work [27] as well as aids in establishing and maintaining or improving upon the integrity of healthcare or organization [26]. In the context of a health system, Riva and Pravettioni (2016) state that values help a healthcare system look beyond the economics of running the system and consider making decisions geared towards “adding value to the patient” [28]. Incorporating values in decision making would ensure that care for the patient encompasses their overall health-related quality of life, patient well-being, and health outcome [28]. Furthermore, VBDM helps to produce the maximum good [29], [30], prevent professional misconduct and negligence, manage conflict of interest and ethical issues and promote moral capital [29]. McCartney (2005) suggested that VBDM can only be successful if the problem at hand is clearly defined [26]. The values used should be specific, aligned, appropriate and supported by evidence. The role of values ensures a clear plan of action [31], but also serves as a constant reminder of the goals, ensures the production of the maximum good and the ethical conduct to reflect the organization's goals are reflected [9], However, not all values are the same or considered equal, with some values overriding others [32], [33]. In addition, values are not always supported by evidence, leading to subjective value selection, resulting in poor decision making thereby wasting time and resources.
3.4. Limitations of EBDM and VBDM
The outlined limitations related to both EBDM and VBDM (see Table 1) call for developing and using a new framework that integrates values and evidence in the decision-making process so that health policy decisions are both value- and evidence-informed. VEDMAP as a novel theoretical framework for decision- making or policymaking fits this role as it is based on two necessary complementary pillars, namely “evidence of values” and “value of evidence”. The framework was developed by Professor Joseph Mfutso- Bengo, Director of the Health Economics and Policy Unit (HEPU) at the Kamuzu University of Health Sciences (formerly known as College of Medicine of the University of Malawi) in Malawi under the Thanzi la Onse Project.
Table 1.
Summary of decision-making framework.
| Description | Weakness | |
|---|---|---|
| Evidence-Based Decision Making (EBDM) | The practice of making better decisions using a combination of critical thinking and the available evidence. This framework provides an analysis of the problem and identifies potential solutions. |
|
| Value-Based Decision Making (VBDM) | Values are context-specific and aim to guide the decision-making process assisting decision-makers to recall how an organisation describes itself in terms of its mission and analyses the good the decision can generate. |
|
3.5. Value and Evidence-Based decision making and practice (VEDMAP) modelling framework
The proposed VEDMAP is a simple and flexible framework that integrates values and evidence in the decision-making process to produce an optimal decision; that is the decision that will produce the maximum good. VEDMAP incorporates the two existing decision-making frameworks, described above, for optimal decision making. Values are used to appraise evidence, and rigorous solid evidence is required to support values. The VEDMAP framework can also be used to create an ethical environment in which optimal values can successfully thrive through the following:
-
•
Production of Value and Evidence Map
-
•
Decision-Making Routes
-
•
Value Alignment Process
-
•
Evidence and Value Alignment (EVA)
3.6. Use of value and Evidence-Based modelling framework to map out values
An ethical environment must exist in order for optimal decisions to operate and be respected. Understanding this, the VEDMAP framework creates such an environment through value mapping. Value mapping refers to the process of identifying values and evidence and determining how they create the route in which a decision is made to achieve the overall goal. First, the goal of the organization is identified. Next, the values and vices that influence an organization’s decision-making practices are examined. After that, a series of steps is designed to identify and prioritize context-specific values that align with organizational goals ensuring optimal decision making. The steps are as follows:
The Production of Value and Evidence Maps
The first step on the map identifies values used by the organization. There are three categories of values– normative, actual and optimal – all of which influence an organizations operation.
3.7. Normative values
Normative values are a set of agreed-upon societal characteristics or actions considered ideal for producing a desirable outcome[13], [34] and are aligned to achieve a goal. Furthermore, normative values assess what one ought to do to be considered a moral or professional individual. These values can also determine the professionalism of an organization by examining ethical standards that regulate right or wrong conduct[35], [36], [37]. Examples of normative values are moral rules, policies, principles/values of strategic plans, ethical guidelines, code of ethics, resource allocation value frameworks and equitable access value framework.
3.8. Actual (Practised) values
Actual values or vices refer to “lived” or applied values in real-time to achieve one's desired goal. Actual values can be normative values – values that one is expected to use – or unexpected or unacceptable – that may be applied but not formally agreed on. Thus, they can be formalized or non-formalized. As such, actual values can be aligned to the goal or non-aligned.
For example, despite the liberalization of abortion laws in countries such as Canada, South Africa and Ireland, termination of pregnancy remains an ethical dilemma. Health professionals may object to performing an abortion as the practice does not align with their pro-life beliefs, which may consider abortion as morally unacceptable. Their decision not to terminate a pregnancy due to their belief is outside the normative value, the termination laws. Hence, the actual value is the refusal to terminate.
3.9. Optimal (professional) values
Optimal or professional values are empirical professional values and are the final set of identified values that are the most desirable and most aligned values to maximize the objective function. They are the final set of agreed-upon and formalized values one is expected to use in the decision-making process. Unlike normative values, optimal values are supported by evidence. They are context-specific, reflecting an organization’s goal; ensuring decisions are made with optimal values maximizing results of the goal. The right to life and the right to freedom of speech are both considered optimal values. However, in an emergency the right to life overrides the right to freedom of speech.
Decision-Making Route
The decision-making route refers to the empirical values that are context-specific, used to direct a decision on the course to achieve a goal. To illustrate, assume policymakers in Malawi are assigned with the task to identify an intervention to reduce the HIV prevalence rate. Although successful interventions have resulted in a substantial decrease in HIV prevalence, the country still has one of the highest HIV prevalence globally (8.9 %) [34]. Societal and cultural constructs leave Malawian women disproportionately affected by HIV, with about 4.2 % of women being HIV positive compared to 2.1 % of men in 2019 [38], [39]. The Malawi government aims to further reduce the HIV prevalence by increasing coverage of vulnerable populations with effective prevention strategies, including condoms. However, with two condom types to choose from, male or female, and the scarcity of resources, the government can only afford to invest in one condom type. The government turns to policy makers to assist in determining which of the condoms to invest in. The policymakers, together with researchers, advocate groups, public health practitioners, and other relevant stakeholders will have to choose the appropriate values needed to reduce HIV prevalence. From their discussion, they will determine the values of efficacy and safety that need to be deliberated. With limited resources available, cost-effectiveness is an inevitable value that needs to be addressed. This set of values would aid the policymakers in comparing the efficacy, safety and cost-effectiveness of each condom type, thus directing resources to the more favourable intervention.
Value Alignment Process
To assess the degree to which values align to the goal, values are taken through value alignment. Value alignment follows the following eight steps: (1) Text, (2) Context, (3) Promise, (4) Process, (5) Competence, (6) Practice, (7) Value Fidelity Assessment and (8) Monitoring and Evaluation. To begin the process of aligning values, a basis of the normative values needs to be established. As stated earlier, these values can be found in text such as policies and strategic documents or guidelines. As previously noted, in order for values to aid in decision-making successfully, they must apply to the context in which they live.
Many organizations have codes of ethics or a normative set of values to ensure that all organization members understand acceptable behaviour, highlighting how individuals should act within the organization. According to VEDMAP, this is the promise. Accepting to work in an organization by signing a contract, one promises to adhere to the code of ethics and act accordingly. The process refers to the systems put in place to ensure adherence to the promise made.
Competence is the ability of policymakers to apply the optimal values to make a wholesome decision successfully. The element of practice refers to using optimal values to guide one's professional behaviour and organizational culture. Practice refers to the actual application of values in decision making, i.e., are the policymakers considering the condom acceptability by healthcare professionals and clients patients? Are they taking into account the cost-effectiveness, clinical effectiveness and safety? Are they considering the evidence?
Popularly used in implementation science, fidelity assessment refers to how an intervention has been delivered compared to the original design [40]. In addition, fidelity assessment aims to understand the alignment or misalignment between the intended program design and the implemented program to the goal, assessing how successful the implemented program was to achieve the goal [29], [40], [41].
Similarly, the VEDMAP framework uses value fidelity assessment to measure the alignment or misalignment of normative and actual values, actual and optimal values to the overall goal and practice.
The value fidelity assessment process helps uncover factors that lead to the misalignment of values and facilitates programs to reduce the misalignment. Value fidelity assessment assesses all the barriers and enablers at the implementation point of a program or strategy, prioritization and allocation criteria value sets. For example, the Malawi National Condom Strategy 2015–2020 aimed to improve the availability and access to male and female condoms, thereby preventing HIV transmission and unwanted pregnancies. Increasing the demand for male and female condoms and improving access by having open dialogue, identifying and training local champions to create awareness and expanding condom distribution through NGOs and commercial sectors [42] were identified strategies in achieving the goal. Since its inception, the strategy successfully increased by 70 % both knowledge of condom use and safe sexual intercourse, and male condom distribution [43]. While an increase in the female condom was demonstrated, uptake and acceptability were disappointedly low despite having high efficacy and safety data. This was due to unfamiliarity, the condom not being user-friendly, limited knowledge and understanding, misconceptions and acceptability issues around the female condom and limited access [44], [45], [46], [47]. Lastly, monitoring and evaluation measure whether the normative values truly achieve their purpose on the ground and the actual values utilised.
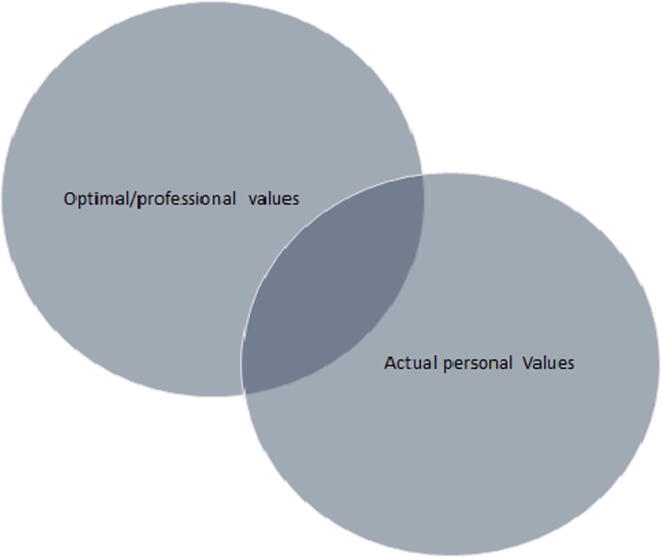
3.10. The highest optimal point of alignment
In order to have an ethical environment, the individuals in that context must themselves be ethical or at the very least understand the ethical culture of that environment and act accordingly. The disconnect between optimal values and personal values is, as argued by VEDMAP, one of the major contributing factors to the mismanagement of health resources.
For VEDMAP to be successful, the use of inappropriate values must be substantially minimized, and an organization’s optimal values must become part and parcel of one's values. One way in which this can be achieved is through the use of the Leadership, Ethics, Governance and Systems (LEGS) framework. This framework guides decision-makers on how to achieve their goals emphasizing the need of moral capital ensuring transparent, robust and ethical decisions are made [48]. The LEGS framework enables the professional values to become part of the personal values and becomes part of organizational culture, thus influencing personal attitudes and professional behavior. The integration of optimal values and personal or actual values is known as the highest point of alignment. Once integrated into an individual's value system, these values are more likely to be used in decision-making, thus optimizing decision-making. This can be achieved through training and incentives, sanctions, rules, codes of ethics, policy monitoring and evaluation. It is important to note that time values and evidence are meant to complement and align to each other in decision and policy making but there are also cases where the best available evidence is not demanded and used due to inappropriate values or conflict of interest. They are meant to complement but at times they can be in conflict. However, VEDMAP employs a value fidelity scorecard to assess the highest point of alignment in cases where they are not aligned. To assess the highest point of alignment VEDMAP employs a value fidelity scorecard. The value fidelity scorecard determines the alignment between actual and optimal values among organization members. By means of a knowledge, attitude and practice (KAP) survey, the scorecard will consist of closed and open-ended questions to determine knowledge attitudes and practice of values. The results of the survey can produce five probable outcomes:
Individuals are unaware of the values, do not value them and do not apply values in practice
Individuals know the values, value them but do not apply them in practice
Individuals know the values, do not value them but apply values in practice
Individuals know the values, value them and apply the values in practice
Individuals do not know the values, but practice them as it is the right thing to do
For instance, HIV professionals must have an understanding of issues related to access, acceptability and cost. Additionally, knowledge on safety and efficacy on condoms as well as demonstrate an understanding on HIV and AIDS, its transmission and prevention methods. They must be dependable, trustworthy, creative and have the ability to respond to changing HIV trends. Participants will be required to score the KAP survey statements between 1 and 5, with 1 = strongly disagree, 2 = agree, 3 = undecided, 4 = disagree and 5 = strongly agree. Questions are given a score between 1 and 5. A score between 4 and 5 is classified as optimal, while a score between 2.5 and 3 is standard. A score below two is considered suboptimal. Fig. 1, Fig. 2 below show the difference between optimal and suboptimal alignment.
Evidence and Value Alignment (EVA)
Fig. 1.
Highest Optimal Point of Alignment.
Fig. 2.
Suboptimal alignment.
The final VEDMAP process is called evidence and value alignment (EVA) and is built upon two pillars, evidence of value and value of evidence. The EVA process ensures that the evidence is aligned to the optimal values identified to achieve the goal. Evidence of value is a scientific method used to identify and map out values or vices that influence decision-making at an individual or organisational level. Simply, evidence of value uses empirical data to distinguish why specific values need to be considered in decision making. Acceptability, for instance, is arguably-one of the critical considerations in the success of any new intervention. Suppose a health intervention does not cater to the patient's needs, is of low quality and is not satisfactory. In that case, the likelihood of the intervention being accepted is low. Thus, the intervention might not be used[46], [47]. This demonstrates that not all values are of the same value. The importance of a value will be dependent on the context in which they operate; thus, there is a hierarchy of values.
On the other hand, value alignment utilizes the optimal values to determine the supply and demand of empirical evidence used to support an optimal value resolving conflict on which evidence to use in decision making. For example, when examining the value of access, the empirical evidence searched for must speak to issues of access to condoms in Malawi or a similar setting.
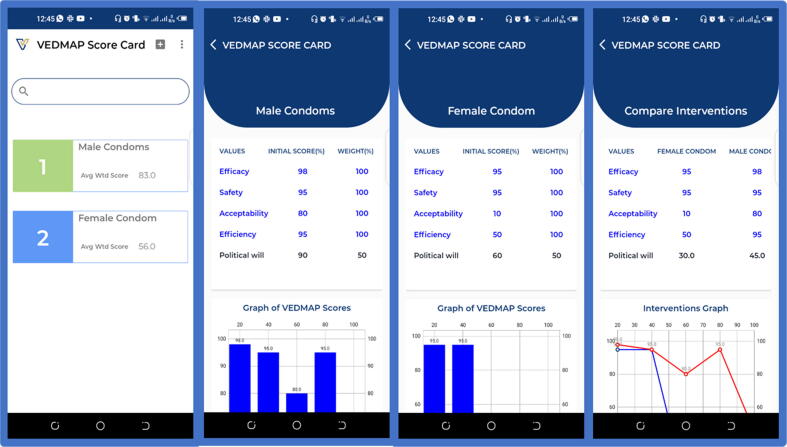
3.11. VEDMAP scorecard
Once an ethical environment has been established, a decision can be made. The VEDMAP framework uses both qualitative and quantitative methods. The first step is to examine the qualitative aspect of VEDMAP. As previously mentioned, a group involving policymakers, researchers, and relevant stakeholders need to debate and agree upon values for evidence valuing. The values agreed upon will be optimal, but as aforementioned, not all values are the same or equal. The weight and importance of values will differ depending on the context and the decision to be made. The VEDMAP score card allows for a maximum of ten values, five core values and five auxiliary values, to ensure only the crucial values are considered. Core values are those that are fundamental and cannot be ignored in the policy and decision-making process. Core values consist of empirical, professional values and an ethical value, thus ensuring professionalism, integrity, equity, and transparency of the decision made. The core values are susceptible to change depending on the context and the decision to be made. To determine if the decision is ethically sound, decision-makers can use one of the following two tests; - Navran’s Three Moral Reasoning Quick Tests and Joseph Fletcher’s Moral Reasoning Test [29]. The use of the Belmont Report Principles (beneficence, respect of persons and justice) [49] or the Reasonable Professional Standard [48] is also beneficial in evaluating the ethical aspects of a decision. On the other hand, auxiliary values serve as tie-breakers, or additional values deemed necessary to make an optimal decision. Auxiliary values are social determinants of health and include education, culture, environment, gender, availability and poverty.
Continuing with the example, as resources are severely limited in Malawi, decisions should minimize the wastage of resources. Hence the core values include efficacy, safety, acceptability, efficiency and the ethical principle of, political will. After a fruitful focus group discussion, it may be agreed that in addition to the five core values – efficacy, safety, acceptability and efficiency – one auxiliary value– political will– may be included.
The quantitative aspect of VEDMAP involves ranking the identified empirical evidence. Each value is given a score between 1 and 5 using the VEDMAP scaling system based on the rigorousness of the evidence. A score of 1 means poor quality, 2 means the quality is below average, 3 represents an average score, a score of 4 is good and 5 is excellent. The values are selected by policy-makers or decision makers. The scores of each value are dictated by the evidence which could be both qualitative and quantitative depending on the type of question being addressed. This is explained. This is explained further with the assistance of Table 2 below. However, not all values are the same, nor are they all equal. The core values cannot be ignored as they are essential in ensuring optimal decision making. Therefore, they are given more weight, and their score is weighted at 100 %. As auxiliary values are only complimentary, their score is weighted at 50 %. Fig. 3 below illustrates the application of the VEDMAP scorecard.
Table 2.
Illustrative example of the VEDMAP application in Malawi.
| Condom type |
Values for evidence preference* |
Total | ||||||
|---|---|---|---|---|---|---|---|---|
| Efficacy+□ | Safety□ | Acceptability+□ | Cost-effectiveness + | Beneficence+ | Political Will | |||
| Male | 4 | 4 | 5 | 5 | 5 | 5 | 28 | |
| Female | 5 | 5 | 1 | 3 | 5 | 3 | 21.5 | |
*The values for evidence preference are scored from 1 to 5. 1 is the minimum while 5 is the maximum value.
□These are core values, weighted at 100% and should not be ignored, Complimentary values are weighted at 50%.
Fig. 3.
Illustration on how the VEDMAP Framework functions Using a Semi-automated Application.
Table 2 shows that despite the high efficacy of female condoms, acceptability was low due to limited understanding, the condom not being user friendly and unfamiliarity. For this reason, acceptability receives a score of one. Once value scaling is complete and the total summed up, you can safely conclude that the best intervention to invest in is the male condom.
3.12. Limitation
Although this paper indicates that VEDMAP is potentially useful, further testing and validation is required before it can be widely adopted in practice. Additional limitations may include the time it will require to meet and debate upon the values needed. The VEDMAP tool intends to bring transparency and create a standardized tool in form of values to be used for decision making. The goal of VEDMAP is not remove disagreements but to create an environment for efficiency transparency, traceability and integrity by use of standardized framework.
3.13. Testing, validation and next steps
The Evidence Valuing Scoring card proposed above is ideal for manual use, i.e., all participants in the focus group score the agreed-upon values on an excel score sheet. This is an efficient way of decision-making using an objective, impartial tool and criteria and tallying the results. A VEDMAP Application has been developed and designed analyze data for selected values and weigh them automatically. The application has been presented and tested on Thanzi La Onse Research Dissemination conference 9th March 2022, stakeholders from the Ministry of Health, Malawi, during a June 2021 HEPU Think Tank meeting and on the Applying Research to Policy and Practice for Health (ARCH) program Oxford University team. It was also presented to the annual-to-annual conference of Malawi Institute of Procurement and Supply as a tool for the procurement for procurement committee on 24th September in Mangochi Malawi. Many participants described the application as “very important”, “with multiple use”, “timely, innovative and easy to use” in facilitating evidence informed -decisions and policy. Furthermore, the scoring can be quantitative or qualitative. The advantage of VEDMAP Score Card is the ability to provide transparency and traceability of decisions in real time by the choice of appropriate values and by weighing options by categorizing values as core or auxiliary. The ARC Oxford team commented that “The VEDMAP framework has the potential to be used will be used by decision maker and policy-makers to assist in priority settings for health technology assessment (HTA) not only in Malawi but beyond”. Furthermore, the scoring can be quantitative or qualitative. The advantage of VEDMAP Score Card is the ability to provide transparency and traceability of decisions and policy in real time by the choice of appropriate values and by weighing options by categorizing values as core or auxiliary. The next step is to use feedback obtained from these stakeholders’ fora to inform the validation study of the tool in a real-world setting.
4. Conclusion
This paper shows that VEDMAP is an objective and straightforward framework that policymakers can use in all settings to optimize and improve decision making. The VEDMAP framework integrates two decision-making frameworks; - evidence-based and value-based decision-making, to ensure optimal decision policymaking, and practice and implementation. VEDMAP allows you to map out values used and needed for decision-making and the values that will aid the process, identify the alignment or misalignment between values and the goal through value fidelity assessment, and identify relevant evidence. Furthermore, for optimal decisions to be made there must be alignment between evidence and value. The VEDMAP scorecard packages evidence for easier understanding for policy and decision-makers, thereby optimizing decision-making. This is particularly important for LMICs where resources are limited; you need both optimal values and the best available context-specific evidence to make decisions, thereby reducing mismanagement of resources through proper selection of interventions and proper alignment of value of evidence. Evidence and values independently are not enough to make an optimal decision. As the world moves more into the digital age, the use of technology is inevitable. Like all technologies, the VEDMAP, which is a semi-automated app, will assist policy and decision-makers in navigating the complexities of decision-making. The Application is advantageous as it is easy to use and flexible and can be used on mobile phones as well as other devices like desktops, laptops and dashboards. Its use is not limited to low-income countries only. The current tools for knowledge translation are in adequate.
CRediT authorship contribution statement
Joseph Mfutso-Bengo: Conceptualization, Supervision. Nthanda Nkungula: Writing – original draft, Writing – review & editing. Emmanuel Mnjowe: . Wingston Ng'ambi: Writing – review & editing, Visualization. Faless Jeremiah: Writing – review & editing. Florence Kasende- Chinguwo: Writing – review & editing. Fanuel Meckson Bickton: Writing – original draft. Dominic Nkhoma: Supervision. Jobiba Chinkhumba: . Sebastian Mboma: . Lucky Ngwira: . Mercy Juma: Writing – original draft. Isabel Kazanga-Chiumia: Supervision. Pakwanja Twea: Writing – review & editing. Gerald Manthalu: Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank Dr Marlen Chawani, Dr Tara D Mangal, Ms Precious Chibwe, Ms Chifundo Kunyenje, Professor Mark Sculpher, Dr Micheal Drummond, Dr Paul Revill and Professor Timothy Hallett for the comments on the first draft of this paper. We would like to give a special thanks to the Thanzi la Onse partners for technical support and MRC and UKRI for funding.
References
- 1.Abiiro G.A., Mbera G.B., De Allegri M. Gaps in universal health coverage in Malawi: a qualitative study in rural communities. BMC Health Serv Res. 2014;14(1):1–10. doi: 10.1186/1472-6963-14-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Universal health coverage (UHC) [Internet]. 2021 [cited 2021 Aug 4]. Available from: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc)
- 3.Masefield S.C., Msosa A., Grugel J. Challenges to effective governance in a low income healthcare system: a qualitative study of stakeholder perceptions in Malawi. BMC Health Serv Res. 2020 Dec 1;20(1) doi: 10.1186/s12913-020-06002-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakovics M.I., Brenner S., Bongololo G., Chinkhumba J., Kalmus O., Leppert G., et al. Determinants of healthcare seeking and out-of-pocket expenditures in a “free” healthcare system: evidence from rural Malawi. Health. Econ Rev. 2020 May 27;10(1) doi: 10.1186/s13561-020-00271-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.VanLandingham G., Silloway T., Chang V., Klein M., White D., Davies E. Evidence-Based policymaking: a guide for effective government. Pew-MacArthur Results First Initiat [Internet] 2014:30. http://www.pewtrusts.org/es/research-and-analysis/reports/2014/11/evidence-based-policymaking-a-guide-for-effective-government Available from: [Google Scholar]
- 6.Berman J., Mitambo C., Matanje-Mwagomba B., Khan S., Kachimanga C., Wroe E., et al. Building a knowledge translation platform in Malawi to support evidence-informed health policy. Heal Res Policy Syst. 2015;13(73) doi: 10.1186/s12961-015-0061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Partridge A.C.R., Mansilla C., Randhawa H., Lavis J.N., El-Jardali F., Sewankambo N.K. Lessons learned from descriptions and evaluations of knowledge translation platforms supporting evidence-informed policy-making in low- and middle-income countries: a systematic review. Heal Res Policy Syst. 2020;18(1):1–22. doi: 10.1186/s12961-020-00626-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Forrest J.L., Miller S.A. Translating evidence-based decision making into Practice: EBDM concepts and finding the evidence. J Evid Based Dent Pract. 2009;9(2):59–72. doi: 10.1016/j.jebdp.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 9.McCaughey D., Bruning N. Rationality versus reality: the challenges of evidence-based decision making for health policy makers. Implement Sci. 2010;5(1):1–13. doi: 10.1186/1748-5908-5-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gollust S.E., Seymour J.W., Pany M.J., Goss A., Meisel Z.F., Grande D. Mutual distrust: perspectives from researchers and policy makers on the research to policy gap in 2013 and recommendations for the future. Inquiry. 2017;54 doi: 10.1177/0046958017705465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hewlett Foundation. Evidence-Informed Policymaking Strategy [Internet]. 2018. Available from: https://hewlett.org/wp-content/uploads/2018/04/EIP-Strategy-March-2018.pdf.
- 13.Setlow B, Bizon J. Amygdala and value-based decision making. Behav Brain Res [Internet]. 2021; Available from: https://www.sciencedirect.com/journal/behavioural-brain-research/special-issue/10XNC8MRN4G. [DOI] [PubMed]
- 14.Stewart R., Langer L., Erasmus Y. An integrated model for increasing the use of evidence by decision-makers for improved development. Dev South Afr. 2019;36(5):616–631. [Google Scholar]
- 15.Young E., Quinn L. Making reserach evidence matter. A Guide to Policy Advocacy in Transi_ on Countries [Internet] Open Society Foundations; Budapest: 2012. 2.3.1 What is evidence-based decisionmaking? pp. 31–43. Available from: [Google Scholar]
- 16.Bonell C., Jamal F., Melendez-Torres G.J., Cummins S. ‘Dark logic’: theorising the harmful consequences of public health interventions. J Epidemiol Community Health. 2015;69(1):95–98. doi: 10.1136/jech-2014-204671. [DOI] [PubMed] [Google Scholar]
- 17.Oliver K., Innvar S., Lorenc T., Woodman J., Thomas J. A systematic review of barriers to and facilitators of the use of evidence by policymakers. BMC Health Serv Res. 2014;14(2) doi: 10.1186/1472-6963-14-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Inguane C., Sawadogo-Lewis T., Chaquisse E., Roberton T., Ngale K., Fernandes Q., et al. Challenges and facilitators to evidence-based decision-making for maternal and child health in Mozambique: district, municipal and national case studies. BMC Health Serv Res. 2020;20(1):598. doi: 10.1186/s12913-020-05408-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hyder AA, Corluka A, Winch PJ, El-Shinnawy A, Ghassany H, Malekafzali H, Mfutso-Bengo J, et al. National And, 106. policy-makers speak out: Are researchers giving them what they need? Health Policy 2011;16:73–82., 337 Planning. [DOI] [PMC free article] [PubMed]
- 20.Paine Cronin G., Sadan M. Use of evidence in policy making in South Africa: an exploratory study of attitudes of senior government officials. African Eval J. 2015;3(1):1–10. [Google Scholar]
- 21.Rutter J. Evidence and evaluation in policymaking: a problem of supply or demand? London; 2012.
- 22.Li Y., Kong N., Lawley M., Weiss L., Pagán J.A. Advancing the use of evidence-based decision-making in local health departments with systems science methodologies. Am J Public Health. 2015;105(2):S217–S222. doi: 10.2105/AJPH.2014.302077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nevo I., Slonim-Nevo V. The myth of evidence-based practice: towards evidence-informed practice. Br J Soc Work. 2011 Sep;41(6):1176–1197. [Google Scholar]
- 24.Transparency International. Corruption Perception Index [Internet]. 2021. Available from: www.transparency.org/research/cpi/overview.
- 25.Schwartz S.H. An overview of the schwartz theory of basic values. Online Readings Psychol Cult. 2012 Dec 1;2(1) [Google Scholar]
- 26.Mccartney J.J. Values Based Decision Making in Healthcare : Introduction. Springer. April 2005;2005(1):1–5. doi: 10.1007/s10730-005-4946-4. [DOI] [PubMed] [Google Scholar]
- 27.Prilleltensky I. Value-Based Leadership in Organizations : balancing values, interests, and power among citizens, workers, and leaders. Ethics Behav. 2000;10(2):139–158. [Google Scholar]
- 28.Riva S., Pravettoni G. Value-based model: a new perspective in medical decision-making. Front Public Heal. 2016;4:118. doi: 10.3389/fpubh.2016.00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mfutso-Bengo J.M. Bioethics as moral capital in Africa/Malawi. Lambart Publishe. 2016:1–141. [Google Scholar]
- 30.Suri G., Gross J.J., Mcclelland J.L. Value-based decision making : an interactive activation perspective. Am Psychol Assoc. 2020;127(2):153–185. doi: 10.1037/rev0000164. [DOI] [PubMed] [Google Scholar]
- 31.Brandstedt E., Brännmark J. Rawlsian constructivism: a practical guide to reflective equilibrium. J Ethics [Internet] 2020;24(3):355–373. doi: 10.1007/s10892-020-09333-3. Available from: [DOI] [Google Scholar]
- 32.Zhang R., Weng L. Not all cultural values are created equal: cultural change in China reexamined through Google books. Int J Psychol. 2017;54(1):144–154. doi: 10.1002/ijop.12436. [DOI] [PubMed] [Google Scholar]
- 33.Winter V., Kattari S., Begun S., McKay K. Personal and professional values: relationships between social workers’ reproductive health knowledge, attitudes, and ethical decision-making. J Soc Work Values Ethics. 2016;13(2):35–46. [Google Scholar]
- 34.Wajuihian S.O. Normative values for clinical measures used to classify accommodative and vergence anomalies in a sample of high school children in South Africa. J Optom. 2019;12(3):143–160. doi: 10.1016/j.optom.2018.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beauchamp T.L., Childress J.F. Oxford University Press; New York: 2001. Principles of biomedical ethics. Fifth edit; pp. 1–408. [Google Scholar]
- 36.von der Pfordten D. Five Elements of Normative Ethics - a General Theory of Normative Individualism. Ethical Theory Moral Pract. 2012;15:449–471. [Google Scholar]
- 37.University of Wisconsin-Madison Libraries. General Philosophy : Ethics (Moral Philosophy) and Value Theory [Internet]. 2020 [cited 2020 Oct 26]. Available from: https://researchguides.library.wisc.edu/c.php?g=178198&p=1169035.
- 38.Knoema. Malawi - Prevalence of HIV among women [Internet]. [cited 2021 Jul 16]. Available from: https://knoema.com/atlas/Malawi/topics/Health/Risk-factors/Prevalence-of-HIV-among-women.
- 39.Knoema. Malawi - Prevalence of HIV among men [Internet]. [cited 2021 Jul 16]. Available from: https://knoema.com/atlas/Malawi/topics/Health/Risk-factors/Prevalence-of-HIV-among-men.
- 40.Breslow L, Pritchard DE, DeBoer J, Stump GS, Ho AD SD. Research & practice in 2013;8:13–26., 405. assessment. Research & Practice in Assessment.
- 41.Joni M. Lakin R-HK. Fidelity of Implementation: Understanding Why and When 2019;42 2 205–14., 410. Programs Work. Gifted Child Today.
- 42.Joni M. National AIDS Commission; Ministry of Health. Malawi National Condom Strategy 2015-2020 [Internet]. Lilongwe; 2017. Available from: http://www.healthpolicyplus.com/ns/pubs/7184-7325_MalawiNationalCondomStrategyJuly.pdf.
- 43.National AIDS Commission (NAC). Malawi National Strategic Plan for HIV and AIDS 2020 – 2025 [Internet]. Lilongwe; 2020. Available from: http://webmail.aidsmalawi.org.mw/view-resource/National Strategic Plan for HIV and AIDS 2020-25 Final.pdf.
- 44.Kavinya T. Have Malawian women embraced the female condom? Malawi Med J. 2013;25(3):95. [PMC free article] [PubMed] [Google Scholar]
- 45.Muula A. Prevvalence of use and perceptions on female condoms among women in Blantyre urban areas, Malawi. 2015; Available from: https://www.researchgate.net/publication/284511588_PREVALENCE_OF_USE_AND_PERCEPTIONS_ON_FEMALE_CONDOMS_AMONG_WOMEN_IN_BLANTYRE_URBAN_AREAS_MALAWI.
- 46.Peters A., van Driel F., Jansen W. Acceptability of the female condom by sub-Saharan African women: a literature review. Afr J Reprod Health. 2014;18(4):34–44. [PubMed] [Google Scholar]
- 47.Moore L., Beksinska M., Rumphs A., Festin M., Gollub E.L. Knowledge, attitudes, practices and behaviors associated with female condoms in developing countries: a scoping review. Open Access J Contracept. 2014;6:125–142. doi: 10.2147/OAJC.S55041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mfutso-Bengo J., Kalanga N., Mfutso-Bengo E.M. Proposing the LEGS framework to complement the WHO building blocks for strengthening health system: one needs a LEG to run an ethical, resilient for implementing health rights. Malawi Med J. 2017;29(4):317–321. doi: 10.4314/mmj.v29i4.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brady J V, Cooke RE, Heght DI, Jonsen AR, King P, Lebacqz K, et al. Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research [Internet]. Washington; 1978. Available from: http://videocast.nih.gov/pdf/ohrp_belmont_report.pdf.
Further reading
- 10.Mfutso-Bengo J, Nkungula N, Ng’ambi W, Jeremiah F. Proposing the “Value-and Evidence-Based Decision Making and Practice”(VEDMAP) framework for priority-setting and knowledge translation in low-and middle. PapersSsrnCom [Internet]. 2022;(March). Available from: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4047540. [DOI] [PMC free article] [PubMed]
- 50.Kavinya T. Opinions on the use of the female condoms by Malawian women. Malawi Med J. 2013;25(3) [PMC free article] [PubMed] [Google Scholar]
- 51.Miller AN, Mann C, Jackson A, Harris D, Credit P, Gareth PSI. Assessing the Total Market for Female Condoms in Malawi and Zambia [Internet]. 2018. Available from: https://marketbookshelf.com/publications/assessing-the-total-market-for-female-condoms-in-malawi-and-zambia/.
- 52.Kaunda-Khangamwa B.N., Kapwata P., Malisita K., Munthali A., Chipeta E., Phiri S., et al. Adolescents living with HIV, complex needs and resilience in Blantyre, Malawi. AIDS Res Ther. 2020:35. doi: 10.1186/s12981-020-00292-1. [DOI] [PMC free article] [PubMed] [Google Scholar]