ABSTRACT
Thymolipomas are slow-growing benign tumors arising from the thymus. They are rare in children, are usually asymptomatic, and can attain enormous size at diagnosis. Contrast-enhanced computerized tomography (CECT) scan characterizes the thymolipomas as a fat-attenuating lesions in the anterior mediastinum. Surgical excision provides relief from symptoms and is the definitive management. We report a case of a symptomatic giant thymolipoma in a 5-year child to highlight issues in diagnosis and management.
KEY WORDS: Anterior mediastinal mass, pediatric thymolipoma, thymolipoma
INTRODUCTION
Thymic lesions in children are rare and constitute only 2-4% of anterior mediastinal masses.[1] One of the thymic tumors is a thymolipoma, an uncommon benign tumor consisting of thymic tissue and mature adipose tissue. These occur usually in adults and account for a mere 2-9% of thymic masses in children.[2] Usually asymptomatic, they can attain a large size and can mold according to the contour of the chest cavity before becoming symptomatic. About 200 cases of thymolipomas have been reported in literature to date and of these, less than 20% are in children below 15 years of age.[3]
We present a child with a large symptomatic bilateral mediastinal mass that proved to be a thymolipoma on histopathology with a summary of optimal management strategies.
CASE REPORT
A 5-year-old girl, weighing 15 kilograms, presented with gradual onset dyspnoea on exertion with acute worsening of symptoms following an episode of upper respiratory tract infection. Physical examination revealed a heart rate of 140/min, regular rhythm, a blood pressure of 110/60 mm hg, and respiratory rate of 36 beats/min. Breath sounds were absent in the right hemithorax except in the suprascapular area and diminished in the left chest.
The child was clinically more comfortable in the left lateral decubitus position. The initial diagnosis suspected by the referring pediatrician was a massive pericardial effusion based on her chest X-ray which showed widened mediastinum with an enlarged cardiac silhouette. But this was ruled out by 2-Dimensional echocardiography.
Contrast-enhanced computerized tomography (CECT) scan of the thorax showed a large well defined fat attenuated lesion (17 × 11 × 10.8 cm) in the anterior mediastinum with a predominant mass component in the right chest cavity displacing right lung parenchyma postero-superiorly and extending into left thorax over the pericardium [Figure 1]. Laboratory findings were unremarkable.
Figure 1.
(a) Pre operative Chest X-ray showing enlarged cardiac silhoute mimicking pericardial effusion (b and c) CECT Thorax showing well encapsulated fat attenuating mass lesion occupying entire right hemithorax and extending to left
In view of the acute symptoms and with imaging showing a huge anterior mediastinal mass of thymic origin, the patient was planned for surgical excision. The patient underwent awake intubation with a 5.5 cuffed endotracheal tube advanced to the left main bronchus for right lung isolation. An anterolateral thoracotomy was done through the right 5th intercostal space extending to the left side by dividing the sternum horizontally. There was a large anterior mediastinal mass, well defined, firm in consistency, completely filling the right thorax displacing the lung postero-superiorly, and extending into the left thorax over the pericardium. There was no pericardial effusion. The mass was adherent to the pericardium and free from the right lung and chest wall. It was mobilized and delivered from the incision after dividing the 4th, 5th, and 6th costal cartilages [Figure 2]. The mass was then dissected from the brachiocephalic vein, and removed enbloc [Figure 3]. Bilateral drains were placed. No suction was applied to the chest drains. The sternum was fixed and the thoracotomy closed in layers.
Figure 2.

(a) Initial planned clamshell incision (b) Right anterolateral thoracotomy incision (c) Dissecting the stalk after delivering out the tumour
Figure 3.
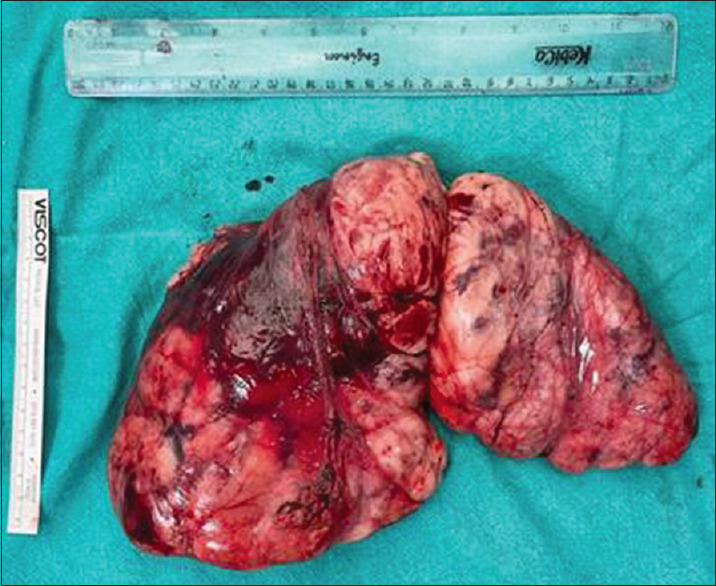
Enbloc resection of thymic mass showing yellowish surface with lobulations
The patient was extubated on the table and shifted to the pediatric intensive care unit. She was kept initially on Bilevel positive airway pressure support (BiPAP) and then shifted to high-flow nasal oxygen. On Postoperative day (POD) 3, both Intercostal drains (ICD) were removed, the patient was mobilized and discharged on POD4. On follow-up, she was healthy, asymptomatic with fully expanded lungs.
Histopathological examination revealed thymolipoma.
DISCUSSION
Thymic lesions are rare in childhood and thymolipomas are still rarer. In literature, less than 40 cases of childhood thymolipomas have been reported with 2 cases during infancy. Of these, the youngest patient was 6 months old.[3] No sex predilection has been noted in children.
Thymolipomas are benign tumors that arise from thymic fat and are composed of both mature thymic tissue as well as adipose tissue.[4] The differential diagnosis includes lipomas of thymic origin, mature thymic hyperplasia, teratoma, thymoma, thymohemangiolipoma, and rarely well-differentiated liposarcomas. Rarely lipomatous components of thymolipomas may undergo malignant transformation into liposarcoma. Pathogenesis of thymolipomas is still unclear with few studies pointing towards mutation of the high mobility group AT-hook 2 (HMGA2) gene in 12q15.[5]
At surgery, they are located in the anterior mediastinum with extension to either or both of the thoracic cavities.[6] They are well-circumscribed, encapsulated with few adhesions with surrounding structures and lungs, and have a vascular stalk. This makes the surgical excision easy.
In adults, the coincidental occurrence of myasthenia gravis, aplastic anemia, and Hodgkins lymphoma have been noted with thymolipomas while in children a single case of hypogammaglobulinemia with erythrocyte hypoplasia have been reported.[3] Our patient did not have any other associated clinical syndrome.
Most the childhood thymolipomas present with mild symptoms including cough, dyspnoea, and bulging of the chest. Many of them have a history of inadequate weight gain. In our patient, it was the respiratory tract infection that aggravated the dyspnoea and made the parents bring the child to medical attention. On clinical evaluation, widened cardiac borders and reduced breath sounds may be noted owing to the extent of the tumor which led to further imaging.
Diagnostic evaluation for suspected mediastinal mass ranges from Chest X-ray to Positron Emission Tomography (PET) scans. CECT thorax facilitates the differentiation of lung tissue, soft tissues, and highly perfused structures such as a thymohemangiolipoma. Diagnosis of thymolipomas is suggested by its appearance of a fatty mass, location, and continuity with the thymus. 3-Dimensional reconstruction of tumor usually helps in surgical planning including approach and incisions. Although specific diagnostic characteristics of MRI have been described, whether there is a need to use multiple imaging modalities in a given patient before the intervention, is unclear and uncertain.
Considering the rarity of tumours there are no clear recommendations for the management of these tumors in children. Common possible indications would probably include a large size where early excision would obviate the need for prolonged follow-up, the presence of symptoms, and the impossibility of ruling out malignancy. In this context, it must be emphasized that though the diagnosis is strongly suggested by imaging, it is not possible to make a definitive diagnosis or to differentiate between benign and malignant. Whether a preoperative cytological or histological diagnosis is necessary before intervention remains unclear and controversial since false positives have been reported.
Surgical excision is curative and has been used commonly in most reports. While surgery is usually not problematic, special care is needed in the administration of anesthesia in these patients with large tumors especially in the presence of symptoms because there is a potential for severe and potentially fatal respiratory and cardiovascular problems during the induction of anesthesia.[7] The pathophysiology of this problem has been studied and published and anesthetic strategies have been formulated for its avoidance; these were used in our patient viz. awake intubation in lateral decubitus position, use of spontaneous ventilation, and avoidance of IPPV. Removal of large mediastinal tumors has been known to cause re-expansion edema; prolonged ventilation, use of IPPV, and application of suction to intercostal tubes have been implicated in its etiology, these maneuvres should be avoided as much as possible as was done in our patient. A coordinated multidisciplinary plan should be formulated by the treating team.
Although open approaches via median sternotomy which provides excellent exposure and control of vessels and lateral thoracotomies are mostly employed for thymolipomas in children as well as in adults due to the large size of tumors, minimal invasive excision of mediastinal mass in children including Video-assisted thoracoscopic surgery (VATS) excision[8] have also been reported.
In our patient, although initially a clamshell thoracotomy was planned, we could manage to deliver the tumor by a right anterolateral thoracotomy incision. We raised the skin flaps and divided the sternum transversely without lengthening the skin incision which provided good exposure and facilitated complete excision despite of the large size of tumor. Surgical excision offers an excellent prognosis for thymolipomas. Recurrences have not been reported.
CONCLUSION
Thymoma is a rare tumor in children. Although they are benign tumors with an indolent course, they can attain the huge sizes and can cause compressive symptoms. Tumor characterization can be done with CECT thorax which defines the tissue of origin and extent of tumor. Surgical excision is the definitive management. Surgical incision and its planning depend on the size and location of tumor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shrivastava T, Ntiamoah P. Rare cause of large anterior mediastinal mass––Thymolipoma. Radiol Case Rep. 2020;15:1538–40. doi: 10.1016/j.radcr.2020.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carapinha CP, Wainwright L, Loveland JA. A giant thymolipoma. S Afr J Child Health. 2010;4:20–1. [Google Scholar]
- 3.Kitano Y, Yokomori K, Ohkura M, Kataoka T, Narita M, Takemura T. Giant thymolipoma in a child. J Pediatr Surg. 1993;28:1622–5. doi: 10.1016/0022-3468(93)90121-z. [DOI] [PubMed] [Google Scholar]
- 4.Parakh A, Singh V, Subramaniam R, Narula MK, Agarwala SK, Shukla S. Giant thymolipoma in an infant. Paediatr Int Child Health. 2014;34:230–2. doi: 10.1179/2046905513Y.0000000108. [DOI] [PubMed] [Google Scholar]
- 5.Sharma KC, Bhakuni YS, Darlong LM, Pasricha S, Dewan AK, Chand R, et al. A giant mediastinal thymolipoma: A rare pathological entity. Indian J Thorac Cardiovasc Surg. 2019;35:115–7. doi: 10.1007/s12055-018-0700-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guleria P, Jain D. Thymic lesions of the paediatric age group: A comprehensive review of non-neoplastic and neoplastic etiologies. Mediastinum. 2019;3:24. doi: 10.21037/med.2019.05.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lerman J. In: Seminars in Anesthesia, Perioperative Medicine and Pain. Vol. 26. WB Saunders; 2007. Anterior mediastinal masses in children; pp. 133–40. [Google Scholar]
- 8.Tan TW, Kim DS, Wallach MT, Mangray S, Luks FI. Thoracoscopic resection of a giant thymolipoma in a 4-year-old girl. J Laparoendosc Adv Surg Tech. 2008;18:903–5. doi: 10.1089/lap.2008.0006. [DOI] [PubMed] [Google Scholar]



