Abstract
Recent studies have begun to understand sleep not only as a whole-brain process but also as a complex local phenomenon controlled by specific neurotransmitters that act in different neural networks, which is called “local sleep”. Moreover, the basic states of human consciousness—wakefulness, sleep onset (N1), light sleep (N2), deep sleep (N3), and rapid eye movement (REM) sleep—can concurrently appear, which may result in different sleep-related dissociative states. In this article, we classify these sleep-related dissociative states into physiological, pathological, and altered states of consciousness. Physiological states are daydreaming, lucid dreaming, and false awakenings. Pathological states include sleep paralysis, sleepwalking, and REM sleep behavior disorder. Altered states are hypnosis, anesthesia, and psychedelics. We review the neurophysiology and phenomenology of these sleep-related dissociative states of consciousness and update them with recent studies. We conclude that these sleep-related dissociative states have a significant basic and clinical impact since their study contributes to the understanding of consciousness and the proper treatment of neuropsychiatric diseases.
Keywords: dissociative states, sleep dissociation, daydreaming, lucid dreaming, false awakenings, sleep paralysis, sleepwalking, REM sleep behavior disorder, hypnosis, anesthesia, psychedelics
1. Introduction
Contemporary works on sleep regulation proposed the term “local sleep” to define physiological characteristics that can be found in specific regions of the brain during the basic states of consciousness, i.e., wakefulness, rapid eye movement (REM) sleep, and non-REM sleep (sleep onset—N1, light sleep—N2, deep sleep—N3) [1,2,3,4]. These physiological states of consciousness tend to cycle in a stable manner; however, the transitions among these states are gradual and inconsistent, with the concomitant presence of multiple state-determining biomarkers. Accordingly, this may result in mixed states in which sleep and wakefulness occur asynchronously in different regions of the brain, resulting in the so-called sleep-related dissociative states [5].
In this work, we aim to first classify these sleep-related dissociative states into physiological, pathological, and altered states of consciousness (Table 1) to then review their neurobiological substrates and related subjective experiences. By “physiological”, we mean that these states tend to occur in regular, healthy subjects, as opposed to “pathological” states that are usually associated with some disease or disturbance. Moreover, “altered” states are neither physiological nor pathological; they are exogenously induced, either by psychological or by pharmacological interventions. To illustrate these physiological, pathological, and altered sleep-related dissociative states, we describe three examples of each: (a) daydreaming, lucid dreaming, and false awakenings (physiological), (b) sleep paralysis, sleepwalking, and REM sleep behavior disorder (pathological), and (c) hypnosis, anesthesia, and psychedelics (altered).
Table 1.
Sleep-related, dissociative states of consciousness.
| Physiological | Altered | Pathological |
|---|---|---|
| Daydreaming | Hypnosis | Sleep paralysis |
| Lucid dreaming | Anesthesia | Sleepwalking |
| False awakening | Psychedelics | REM behavior disorder |
It is important to note that the limits between these categories are fluid. For example, daydreams, which are here first considered physiological, can become pathological in specific situations, such as depression. Moreover, sleep paralysis and somnambulism are considered real diseases only if they become too frequent and/or intense. Investigating these dissociative states of consciousness is important because it contributes to furthering the understanding of human consciousness and the correct treatment of neurologic or psychiatric disturbances. In the next sections, we will describe these categories and states in detail.
2. Physiological States of Consciousness
2.1. Daydreaming
Singer and McCraven [6] defined daydreaming (or mind wandering) as a partial detachment from the reality around, directing consciousness towards the own imagination with personal content. Although this state of consciousness is part of human nature and an everyday experience, there is still little systematic knowledge about its frequency, duration, spontaneity of appearance, variations, and patterns.
Researchers have hypothesized about the advantages and importance of daydreaming, considering that it occupies more than half of the time we are awake [7]. According to these authors, daydreaming may serve for (1) Adaptive function: allowing for planning future activities, creativity, attentional cycling, and resting [8]; (2) Event simulation: there is a correlation between self-reflection, autobiographical memories, and task performance, suggesting that daydreams (as well as night dreaming) may simulate future events [9]; (3) Interpersonal relationships: allowing the development of interpersonal skills, such as compassion, moral reasoning, empathy, etc. [10]; (4) Volitional processes: one can choose to detach from the reality around to focus on one’s own thoughts [11]; (5) Personal goals: self-awareness, personal planning, goal-directed thinking, simulating another person’s perspective, and compassion [7]; (6) Mental health: daydreaming components such as imagination and fantasy support mental health, allowing the mind to varying its attentional content [7].
Singer [12] divided daydreams into three types: positive-constructive daydreaming, guilty-dysphoric daydreaming, and poor attentional control. positive-constructive daydreaming consists of carefree, positive desires and plans, such as imagining inviting a friend to dinner or being in a park with your pet. Guilty-dysphoric daydreaming is about worries and undesirable scenes, such as revenge, and undesirable experiences, such as deaths and separations. Poor attention control is not necessarily related to the emotional charge but rather an obstacle to the individual’s attention. These daydreaming experiences were studied in different ages, ethnicities, and genders [13,14].
People with more negative daydreaming, such as the guilty-dysphoric type, tend to lack volitional control over their own experience. They are more prone to less self-awareness, difficulty with concentration, and neuropsychiatric diseases such as depression and anxiety [15], as described below.
2.1.1. Self-Generated Thoughts, Daydreaming, and Depression
Self-generated thoughts are intrusive imaginations, ideas, and desires that are not directly related to environmental stimuli and may arise from daydreaming [16]. Self-generated thoughts are associated with loss of reading comprehension [17], sustained attention capacity [18], and working memory [19]. Self-generated thoughts characterized by predominantly negative thoughts correlate with mental diseases, such as depression, anxiety, schizophrenia, and other pathological states of consciousness [20].
The tendency to fall into negative daydreamings, such as ruminating thoughts, correlates with depression; daydreaming can not only be related to depression but also self-generated thoughts can be a symptom of depression [21,22]. It was shown that this relationship between daydreaming and depression was more due to the type of daydreaming, that is, always ruminating on the same thoughts [18,23]. In this sense, it was found that the greater the focus and attention to the own thoughts, the greater the rumination and, consequently, the more depressed mood [23].
Marchetti, Van de Putte, and Koster [24] showed that daydreaming can predict the onset of depressive symptoms since, within the self-generated thoughts, people are faced with their own fears, desires, anxieties, and concerns, which are often accompanied by judgments that increase beliefs in more negative worldviews in relation to their own performance. According to Aldao and colleagues [25], such beliefs tend to induce depression.
2.1.2. Daydreaming and the Default Mode Network
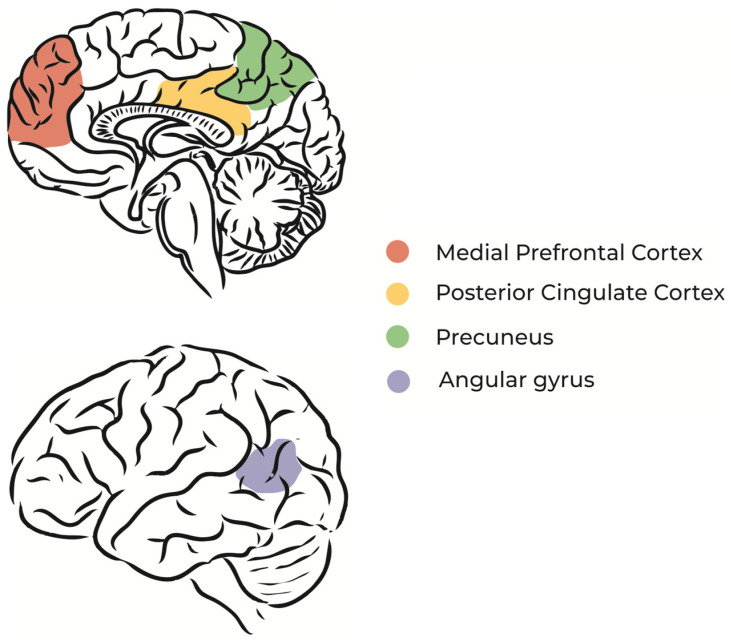
The default mode network (DMN) is a brain circuit that is activated when a person does not direct attention to environmental stimuli, during REM sleep, or during daydreaming [26,27] (Figure 1). In other words, the regions of the brain that constitute the DMN are more active in the absence of external stimuli and sustained attention [28], which means that dreaming and imagination processes share neurophysiological similarities [9].
Figure 1.
Schematic illustration of DMN main regions.
Specific regions of the DMN, such as the dorsomedial prefrontal cortex and medial temporal lobe, are associated with thoughts about oneself (self-referential thoughts) and the construction of future scenarios based on memories [29]. Studies using functional magnetic resonance imaging during unconscious states, such as sleep and coma, found that the spatial organization of neural networks is similar to that of the resting state [30,31]. Resting-state functional magnetic resonance imaging studies show fluctuations between a positive pole that carries out activities that require attention and concentration and a negative (or default) pole that activates a specific network (DMN) during the resting state. When the DMN is activated, other networks responsible for task processing are deactivated. Concurrently, daydreaming becomes predominant, thus there is less attention span [32].
In a recent study, Hilland and colleagues [33] aimed to explore correlations between DMN dysfunction and early-onset psychosis, since there a correlation has been shown between poor DMN connectivity and schizophrenia. The analysis showed a significant reduction in DMN activity in early-onset psychosis patients compared with the healthy control group. There was no relationship between DMN activity and the use of psychotropic drugs in patients with early-onset psychosis.
2.1.3. Daydreaming and Brain Rhythms
Even in tasks that require focus, shifts in the attentional focus to internal issues often occur; therefore, changes in the rhythms of the neural networks can be expected. Brabosczc and Delorme [34] analyzed the electroencephalographic signals of 12 volunteers who performed a breath-counting test and were supposed to press a button whenever they realized they had another thought occupying their minds. In these moments of concentration break, there was an increase in the frequency power of the slower theta (4–7 Hz) and delta (2–3.5 Hz) waves, whereas the frequency of the faster alpha (9–11 Hz) and beta (15–30 Hz) waves decreased. Therefore, daydreaming is associated with less vigilance and alertness, similar to sleep [35].
Supporting this idea, during daydreaming there is a performance decrease in the detection of a stimulus [14]. Since daydreaming is characterized by decreased alertness, concentration, and attention, the brain’s reaction time to external stimuli decreases. For example, a sudden change in an auditory stimulus pattern is more difficult to perceive. It was observed that the neurophysiologic reaction to this pattern change, called mismatch negativity, which is attention dependent, is smaller in the daydreaming group than in the breath-counting group. This suggests a dissociation of attention during daydreaming. In parallel, when individuals enter into a state of somnolence, the mismatch negativity is characteristic of sleep onset [36]. Subjects are absorbed in their own thoughts and personal issues and cannot maintain attention, becoming disconnected from the world [37,38].
2.2. Lucid Dreaming
Lucid dreaming (LD) is a specific type of dreaming characterized by the awareness that one is dreaming and the capacity to control the oneiric content [39]. LD has been mentioned in several religions and by many philosophers for thousands of years [40,41]. However, more recently, some authors were skeptical about this dream phenomenon, arguing that individuals were actually awake or had some kind of misperception [42], which might be due to the lacking evidence of LDs as genuine subjective experiences at that time.
This changed with the pioneering work of Stephen Laberge in 1980. This was based on prior research showing that: (1) eye muscles are exempt from the muscular atonia that accompanies REM sleep [43,44] and (2) direction shifts of the gaze within a dream can be accompanied by real movements of the sleeper’s eyeballs [45,46]. Laberge and colleagues thus asked lucid dreamers to move their eyes in a pre-agreed sequence (left–right movements, for example) as soon as they became lucid in the dream. This technique succeeded and laid the foundation for the scientific studies of LD [47].
2.2.1. Lucid Dreaming, REM Sleep, and the Brain Rhythms
LD occurs predominantly during REM sleep [48,49]. LD has also been reported during the N1 (sleep onset) and N2 (light sleep) stages but not during the N3 stage (deep sleep) [50,51]. As for the ordinary non-LD, the LD during non-REM sleep stages 1 and 2 tends to be shorter, less vivid, less story-telling-like, and more similar to a thought or a waking memory [50] It is not clear, however, why LD is not common in the general population [52], although the majority of people show REM sleep every night. A possible explanation for this inconsistency is that LD is probably associated with specific brain rhythms during REM sleep, with different spectral characteristics from non-lucid REM sleep.
The first works observed a relationship between LD and the global alpha band power (8–12 Hz) [53,54]. Later, a study detected an increase in the beta band power (13–20 Hz) in the parietal region [55]. Subsequent works found an increased gamma band (~40 Hz) in the frontal region [56]). This observation led Voss and colleagues to propose that LD is a mixture of waking and REM sleep, which characterizes a sleep-related dissociated state [5]. A decrease in the delta band (1–4 Hz) power was also observed in the frontal and central regions [57]. Therefore, despite the numerous works reporting different spectral characteristics during LD compared with non-lucid REM sleep, there are considerable controversies regarding the brain regions and frequency bands. Possible explanations for these discrepancies are: (a) methodological aspects—limited electrode montages and different frequency bands analyses [58], (b) subjective features—different experiences and contents during LD with specific neurobiological substrates [59], and (c) proficiency levels—experienced lucid dreamers tend to have longer LD and exert more control over its content [46].
A recent work by Baird and colleagues [60] observed that LD is associated with physiological activation during REM sleep, supporting the results of previous studies of increased phasic activity during LD, including increased REM density, heart rate, respiration rate, and skin potential [48]. These findings suggest that LD correlates with increased cortical activation that peaks during phasic REM sleep. Baird et al. also observed that the increase in frontal gamma during LD [56] reflects saccadic spike potentials due to the higher eye movement density instead of heightened brain activation.
2.2.2. Neuroimaging of Non-Lucid and Lucid REM Sleep
During non-lucid REM sleep, the limbic system is activated (hippocampus, amygdala, medial prefrontal cortex, and anterior cingulate cortex), which might be related to the intense emotions that are usually experienced during dreams [61,62]. On the other hand, the activity in the prefrontal cortex decreases, which may be related to the lack of self-consciousness and meta-cognition during non-lucid dreams [63,64].
Dresler and collaborators [65] observed that during LD frontal regions are activated, including the anterior prefrontal cortex, which may be associated with the insight and self-reflection abilities that characterize LD. More recently, Baird et al. [66] observed that frequent lucid dreamers showed increased resting-state functional connectivity between the anterior prefrontal cortex and other frontal, parietal, and temporal regions. Other studies suggested that LD may be associated with large-scale networks that control executive processes, such as the frontoparietal network [67]. Supporting this hypothesis, Baird et al. [66] also found that frequent lucid dreamers had increased functional connectivity between the anterior prefrontal cortex and a frontoparietal sub-network [68,69]. Another cerebral region—the temporoparietal junction—integrates visual, tactile, proprioceptive, and vestibular information, which contributes to self-consciousness and body internal imagery [70]. Overall, these findings seem to suggest that the self-consciousness and metacognitive abilities that characterize LD may be the result of a network synchronization between the frontal and temporoparietal regions. This hypothesis needs to be explored in future studies.
2.3. False Awakenings
False awakening (FA) is a type of dream in which people believe they have woken up since the dream content is similar to their daily life, especially regarding their activities when waking up, such as rising from bed, going to the bathroom, having breakfast, brushing the teeth, etc. Only when the subjects actually wake up do they realize they were dreaming [71]. In a study with 974 participants, 45% of them had experienced at least one episode of FA in their lifetime, 28% have it sometimes, 8% have experienced a single episode, and 7% have it often. Participants above 50 years have fewer experiences of FA (4%) than the younger ones, especially those between 21–30 years (9%) [72].
During an FA episode, the dream scenario is likely to be similar to the usual environment of the dreamer. Often, the trigger for the FAs are external factors, such as a ringing cell phone; however, sometimes even the trigger may be dreamed [71]. On the other hand, some people refer to FA as “a dream within a dream”.
2.3.1. False Awakenings and REM Sleep
FA happens mostly during REM sleep, which is similar to LD, sleep paralysis (SP; see next section), and out-of-body experiences. Since they all occur in the same sleep stage (REM), these phenomena may be linked to each other. Raduga, Kuyava, and Sevcenko [72] found that people who have already experienced one of these REM sleep-dissociated states are likely to have experienced another. SP and FA share the feeling of being in a familiar environment (usually their bed), the perception of being awake, and feelings of anxiety. One main difference is the inability versus freedom to move during SP and FA episodes, respectively.
To induce FA experiences, Hearne tried to reproduce scenarios in which disturbed sleep is likely to occur, such as expectations and anxieties related to the next day. The reason for this technique is that preoccupations with upcoming events can be anticipated during dreams in the form of FA. This can occur mainly but not solely after an external trigger during sleep. Ways to identify FA depend on the person’s motivation and habit of asking him-/herself, immediately upon waking up, whether he/she was dreaming or sleeping.
2.3.2. False Awakenings and the Brain Rhythms
Using polysomnography during FA, an increase in alpha frequency alternating with states of REM sleep, slow eye movement, and low muscle tone was found [73]. This study also found that, although FA and SP are experiences similar to each other and mimic a waking state, in both of them the individual is dreaming and in the REM sleep stage (associated with the predominance of theta waves in the electroencephalogram). Thus, commonalities between SP and FA regarding the characteristics of REM sleep and wakefulness can be explained by the fact that different stages of sleep or wakefulness, especially their transitions, show mixed features that characterize a sleep-related dissociated state [5]. Moreover, the nocturnal sleep of patients with SP contains a greater predominance of delta waves than in healthy individuals, suggesting an alteration in the regulation of non-REM and REM sleep [73].
3. Pathological States of Consciousness
3.1. Sleep Paralysis
Sleep paralysis (SP) is a dissociative state of consciousness that is characterized by motor, sensory, and cognitive abnormalities that usually happen in the transition from REM sleep to the waking state. It comprises the inability to move, visual hallucinations, tightness in the chest, fear of death, and perception of threatening creatures. The SP experience can induce intense frightening and anxiety due to the loss of voluntary motor activity, which can cause the inability to scream, open the eyes, cry, and even breathe [74,75]. Most people have experienced a few episodes of SP in their lifetime, but when SP occurs frequently or involves intense negative emotional components, impairing well-being, and social functioning, it can be considered a sleeping disorder (parasomnia).
Only sparsely studied by science, many cultures have interpreted SP from a supernatural perspective until today [76]. In Japan, the “kanashibari”, which can be translated as “the state of being totally bound, as if constrained by metal chains”, is caused by a vengeful spirit who suffocates his enemies [77]. In Thailand, the “phi am” is a ghost that appears when subjects are half asleep and unable to move [78]. Egyptians believe that SP is caused by the “jinn”, which are malevolent spirit-like creatures [75]. Ethiopians consider the “dukak” an evil spirit that haunts sleep [79]. In the USA, the report of “alien abductions”—experienced as the inability to move during awakening with visual hallucinations of aliens—is considered a manifestation of SP [80].
The emotional components of SP have been explained by cognitive distortions such as hallucinations, which can be grouped into “Intruder”, “Unusual Bodily Experiences”, and “Incubus”. The first is characterized by the feeling of fear or the sensation of a presence in space accompanied by visual and auditory hallucinations. The second is related to out-of-body experiences. The third refers to the feeling of tightness in the chest and difficulty to breath [81], as depicted by the painter Henry Fuseli (Figure 2).
Figure 2.
The Nightmare (1871), by Henry Fuseli.
The different societies share a common frightening component due to the person’s inability to move and visual hallucinations according to the individual’s culture [82]. However, some authors interpret SP in a strictly pathological way. In the past, SP was underdiagnosed and understood as a symptom of narcolepsy. This disorder is characterized by abnormalities of sleep regulation, in which the individual falls asleep abruptly associated with cataplexy, when muscle tone is lost, usually after a very emotional episode. However, despite its similarities with narcolepsy, SP can occur separately from narcolepsy and, overall, shares few relationships with neuropsychiatric disorders. However, SP must be seen from a pathological point of view when the episodes are very frequent or intense, thus implicating physical, mental, and/or social suffering.
3.1.1. Epidemiology of Sleep Paralysis
In a recent systematic review, sociodemographic and other variables related to SP were studied, including age, ethnicity, residential area, salary, breakfast consumption, alcohol consumption, substance use, stress, and trauma [83]. The authors of this systematic review found no significant age effect on the prevalence of SP. African Americans and other non-Caucasian populations showed a higher incidence of SP than Caucasians. However, other studies do not confirm this direct relationship. Among Chinese adolescents, SP was more frequent in rural than urban areas. In a study from Japan, people with higher incomes had a slightly higher incidence of SP (10.9%) than people with lower incomes (7.3%). People who eat breakfast every day had a lower incidence of SP than those who did not, although the results are inconsistent. This last association might be explained by findings that the period of food consumption may be important for the regulation of the internal circadian clock. Two large samples from China and Japan found that those who had at least one alcoholic drink the previous month were more likely (9–12%) than others (6%) to experience SP. However, in a study from the United Kingdom, this association was not found, even if related to anxiety and depressive symptoms. A history of childhood sexual abuse is strongly related to episodes of SP. Furthermore, these individuals show qualitatively more “intruder” and “incubus” hallucinations during the SP episodes. Moreover, the number of traumatic events was associated with SP cases [83].
It was reported that SP occurs more in women than men and in the supine position when sleeping. In general, at least one episode of SP during a lifetime is reported by 7.6% of the population, 28.3% among students, and 31.9% among psychiatric patients [74].
3.1.2. Neurobiological Mechanisms of Sleep Paralysis
SP is related to the abrupt arrival in (or exiting from) REM sleep, when dreams occur more often and vividly. Therefore, the visual, auditory, emotional, and cognitive alterations of dreams accompany the muscle atony that characterizes REM sleep [43,84]. Similarly, brain activity during REM sleep is associated with a lack of voluntary muscle mobilization. Muscle atonia during REM sleep happens due to the presence of a descending inhibitory system from specific brainstem nuclei that projects to the anterior column of the spinal cord and then to skeletal muscles [85]. The main neurotransmitters of this complex network are GABA and glycine [86]. This intricate system prevents us from acting “in real life” the imaginary movements that we perform when dreaming, which would make us vulnerable and thus subject to being preyed upon. This notion comes from Jouvet’s work, who damaged specific brainstem nuclei and observed that animals started running, cleaning themselves, and masticating during REM sleep since they have no more muscle inhibition. These behaviors were related to dreaming [44,85]. Dahlitz and Parkes [87] consider that the mechanism responsible for bodily immobilization during SP is the lack of synchrony between changes in brain activity and muscle atonia. Thus, during SP individuals show brain activity similar to the waking period; however, the muscles are unable to move. Therefore, subjects feel awake but cannot move, a main feature of a sleep-related dissociative state [5].
Since SP is often associated with the supine body position, Jalal and Ramachandran believe that SP is linked to disorders in the parietal cortex, where monitoring of motor programs through proprioceptive feedback normally occurs. During SP, the persistent muscle atony can create a mismatch that contributes to abnormal physical perceptions and modifies the self–body image [88].
3.2. Sleepwalking
Sleepwalking (or somnambulism) is a condition that has been documented by humanity for a long time. In the third century AD, the Stoic philosopher Diogenes Laertius was said to read and write his works while he slept. In the second century, Galen, the “father” of anatomy, reported in his work “De motu musculorum” that he had spent a whole night walking in his sleep and only woke up after stumbling over a stone. These lines are very reminiscent of sleepwalking but they can also have alternative interpretations, especially from a poetic point of view. In the medieval period, sleepwalking and other sleep disorders were intrinsically related to religious beliefs and interpreted as divine designations or diabolical acts. The sixteenth-century Spanish writer Antonio de Torquemada wrote that the devil makes us “dream lascivious dreams” and provokes the sleepers “to commit follies for which we can lose body and mind once”. Supernatural explanations such as these still exist in many cultures [89].
Sleepwalking is a type of arousal parasomnia disorder that occurs during NREM sleep but in which the usual distinctions between wakefulness, REM, and NREM sleep are blurred, which is the precise definition of a sleep-related dissociative state. Sleepwalking is closely related to other NREM parasomnias (confusional arousals, sleep terrors, sleep-related sexual behavior, and sleep-related violence) since these sleep disturbs are mostly classified by the displayed behaviors [90]. The term disorders of arousal encompass sleepwalking, night terrors, and confusional arousals and also a broader spectrum of specific forms of NREM parasomnias, such as sexsomnia, sleep-related eating, and sleep-related asphyxia syndrome. The underlying factors associated with confusional arousal disorders are mostly unknown [91].
Sleepwalking episodes draw a lot of attention because the person is sleeping and performing complex activities, such as gesturing, pointing, walking, or even dressing, cooking, and driving. These activities can last from seconds to more than 30 min. Its main characteristics are speech in response to external stimuli, as the person is sleeping, mental confusion, variable retrograde amnesia, perceived threat, and misperception [92]. Moreover, descriptive reports show that, in children, complete amnesia is more common, as well as sleepwalking behavior characterized by automatic movements and higher arousal thresholds. Unlike children, many adults remember at least parts of the events upon waking [93]. The condition is most common in children, whereas only 2–3% of adults show sleepwalking and only 0.4% of adults sleepwalk every night. About 80% of adult sleepwalkers showed childhood sleepwalking, perhaps due to an immaturity of the sleep state [94]. Therefore, this phenomenon might be understood as a complex condition that involves high motor control levels, which we detail next.
3.2.1. The Neurobiology and Pathophysiology of Sleepwalking
During the night, NREM sleep and REM sleep alternate in cycles of about 90 min. NREM sleep occurs mainly during the first half of the night’s sleep, whereas periods of REM sleep with vivid and longer dreams are predominant during the second half of the night. As said before, sleepwalking occurs especially in the deepest stage of sleep, which is the N3 sleep stage or slow wave sleep. For this reason, sleepwalking tends to occur during the first half of the night [91].
The pathophysiology of sleepwalking is not well known. Electroencephalographic studies demonstrated that sleep depth is not evenly reflected throughout the brain, with frequency differences throughout its anteroposterior axis. For example, in an epileptic patient, the motor and cingulate cortices activities differed from the associative cortical activity during the sleepwalking episode [95]. These electroencephalographic recordings showed that sleep and waking states can coexist in different regions of the brain, which characterizes a sleep-related dissociative state of consciousness [5].
In both children and adults, chronic sleepwalking is associated with other sleep disorders, which further worsen sleep quality. These include upper airway resistance syndrome, mild obstructive sleep apnea, and restless legs syndrome [96]. Therefore, sleepwalking should be seen as a sleep problem that can have negative implications for the individual’s life and thus requires specialized treatment [97].
3.2.2. Treatment of Sleepwalking
Sleepwalking can bring suffering and physical dangers to the patients without their awareness, such as the risk of accidents, injuries, trauma, etc. Moreover, a study with ten sleepwalkers found that they showed daytime sleepiness even after nights with no episodes. Consequently, besides the suffering and physical dangers, this parasomnia seems to negatively impact work and overall life [98].
The main risk factors for sleepwalking are episodes that increase the need for slow-wave sleep, such as sleep deprivation or poor-quality sleep, precipitating arousal disturbances in predisposed individuals. For this reason, healthcare professionals should emphasize the importance of sufficient good-quality sleep, avoiding irregular sleep times, and having a sleep routine. `Moreover, environmental factors—such as anxiety and stress—can trigger an episode and thus should be avoided. In addition, it is important to evaluate concomitant sleep disorders that cause recurrent micro-arousals. For this, clinicians must assess and treat respiratory problems and movement disorders during sleep to control parasomnia [99]. Sleepwalking is also related to states of dissociation or confusion since it is observed in patients with psychiatric disorders and in those receiving sedatives, hypnotics, antidepressants, neuroleptics, stimulants, and antihistamines. Therefore, disorders, medications, and their combination might facilitate regional dissociation and modulate sleep and alert states leading to sleepwalking [100].
Benign episodes of sleepwalking occur occasionally and do not require pharmacological treatment. Instead, they can be addressed by changes in lifestyle, sleep hygiene, and other techniques such as psychotherapy, hypnosis (see next section), and programmed awakenings [101]. However, it is necessary to guarantee the patients’ safety if the episodes become frequent. This includes: (a) removing potentially dangerous objects from the sleeping environment, such as mirrors, glasses, and decorations, (b) locking doors and windows, and (c) sleeping on a mattress on the floor (since the subject can fall from the bed). These measures reduce the risks during the episode but do not prevent its onset [102]. These non-pharmacological measures are the first-line treatment for sleepwalking, whereas other neuropsychiatric disorders need to be excluded. Otherwise, treatment will be directed toward the underlying disease. Medical treatment for adults is only necessary if these measures are unsuccessful and the condition is associated with physical, psychological, and/or social harm [103]. However, no drug is currently approved for the treatment of sleepwalking. A few studies have been published on pharmacotherapy for sleepwalking with benzodiazepines, tricyclic antidepressants, and selective serotonin reuptake inhibitors [99].
On the other hand, many drugs can induce sleepwalking as an adverse effect. In the study by Stallman, Kohler, and White [104], the benzodiazepine receptor agonist zolpidem induced sleepwalking in a clinical trial, giving rise to numerous case reports of sleepwalking. Moreover, given the differences in individual predisposition, sleepwalking needs to be considered within the adverse risk profile, particularly for drugs that increase the GABA receptor activity, increase serotonin, or block noradrenaline activity at β-receptors [105]. Sleepwalking also needs to be considered as a possible side effect of antipsychotic drugs, although the mechanisms that may exert this effect are unknown [106].
3.3. REM Sleep Behavior Disorder
Rapid eye movement (REM) sleep behavior disorder (RBD) is a behavioral and experiential parasomnia that consists of abnormal behavioral release during REM sleep with loss of generalized skeletal muscle paralysis or “REM-atonia” [107]. RBD was first identified in humans in a series of five patients [108] and resembled findings from an experimental model in cats with pontine tegmental lesions [85]. Mahowald and Schenck [109] also described the dissociation and admixture of different states of consciousness that underscores the neurophysiological phenomenon in which REM-atonia is compromised and wakeful muscle tone and twitching intrudes, resulting in clinically relevant behavioral release during REM sleep. During an RBD episode, the person moves with eyes closed while attending to the inner dream action and being unaware of the actual bedside surroundings [107]. Behavioral release during REM sleep often involves acting out of dreams that are confrontational, aggressive, and violent. The enacted dreams usually involve hostile people and animals and the dreamer is often defending him/herself or loved ones against the perpetrator. The reported dream imagery closely matches the observed physical behaviors during video-polysomnography evaluation. RBD is a dream disorder almost as much as a sleep behavioral disorder. The first textbook on RBD describes various considerations in detail [110].
3.3.1. Epidemiology of REM Sleep Behavior Disorder
According to a recent meta-analysis, the prevalence of idiopathic RBD is 0.68% and probable RBD was estimated at 5.65%. The prevalence was lower for European studies (3.75%) compared with American (7.94%) and Asian studies (5.39%) [111]. The typical RBD clinical profile involves middle-aged and older men with violent and injurious dream-enacting behaviors, with over 80% of these patients eventually developing an α-synuclein neurodegenerative disorder, usually Parkinson’s disease or Lewy body dementia, with an interval of about a decade from RBD onset to overt neurodegeneration [112]. A population-based study of middle-aged to older adults with polysomnographic-confirmed RBD found a 1.06% prevalence of RBD, with gender parity [113]. Younger RBD patients show greater gender parity, less severe RBD, greater association with narcolepsy-cataplexy (narcolepsy type 1), and greater association with psychiatric disorders and antidepressant use. Most antidepressant medications (especially selective serotonin reuptake inhibitors, venlafaxine, and tricyclic antidepressants) can trigger or aggravate RBD, except for the dopaminergic–noradrenergic agent bupropion [114]. Familial RBD has been reported in one family, with autosomal transmission and altered GABAergic circuits [115].
3.3.2. Neurobiology and Pathophysiology of REM Sleep Behavior Disorder
RBD can manifest de novo as idiopathic RBD or can be associated with a heterogeneous group of conditions including narcolepsy, alpha-synuclein neurodegenerative disorders (especially Parkinson’s disease and dementia with Lewy bodies), paraneoplastic neurological syndromes, autoimmune disorders, central nervous system lesions (e.g., tumors, stroke), other neurological disorders, psychiatric disorders (post-traumatic stress disorders and mood disorders), antidepressant/other medications, drug withdrawal states, and toxic metabolic states.
It was demonstrated that inactivation of the sublateral dorsal nucleus in the pontine tegmentum and GABAergic/glycinergic in ventromedial medullary inhibitory neurons in murine models resulted in RBD. Neuropathological and pharmacological damage to the same nuclei in humans can lead to RBD manifestation [116,117].
3.3.3. Evaluation of REM Sleep Behavior Disorder
RBD is characterized by clinically relevant motor behaviors and/or vocalizations representing dream enactment in REM sleep. The motor activity ranges from subtle upper extremity movements (often referred to as hand babbling) to more aggressive, violent, rapid jerky, and apparently purposeful oneiric behaviors such as punching, kicking, running, and jumping. These actions can be potentially injurious to patients and bed partners [107]. The frequency of dream enactment behaviors can vary from several times per night to once a month or even less. Dream recall may be inconsistent with over 40% of patients being unaware of RBD episodes, although bed partners commonly observe behaviors indicating dream enactment. RBD is the only parasomnia that requires objective video-polysomnographic confirmation to establish the diagnosis. The polysomnographic hallmark of RBD consists of electromyographic abnormalities during REM sleep called “loss of REM atonia” or “REM sleep without atonia”, with increased muscle tone and/or increased phasic muscle twitching. Other polysomnographic features include excessive tonic activity in REM sleep in chin electromyogram and/or phasic activity in REM sleep in chin or limb activity. Meticulous historical accounting and carefully monitored video-polysomnography facilitate excluding other differential diagnoses such as obstructive sleep apnea, periodic limb movements, sleepwalking, sleep talking, confusional arousals, night terrors (NREM parasomnias), and nightmares [107].
3.3.4. Management of REM Sleep Behavior Disorder
The main goal of RBD management is to reduce disruptive nightmares to prevent injuries to the patient and bed partner and improve quality of life by reducing interruptions in sleep, as detailed next.
-
(a)
Environmental modification:
Environmental accommodations to ensure safety is the mainstay of treatment (Level A evidence) according to standard guidelines [118]. Patients and bed partners should be advised to remove sharp objects, furniture, and weapons from the immediate sleeping environment to avoid injuries. Any factors that can interrupt sleep such as sleep deprivation or insufficient sleep should be addressed. Co-morbid obstructive sleep apnea should be treated to reduce arousal from the increased respiratory effort, which can be more frequent in REM sleep [119]. A pressurized bed alarm with a pre-recorded calming message in a familiar voice has been shown to help gently prompt the patient to return to sleep but is not widely used [118]. Hypnosis (see next section for more details) has been attempted to treat parasomnia including RBD with some success but is not standard practice [120]. If feasible, drugs aggravating or unmasking RBD symptoms such as selective serotonin reuptake inhibitors, serotonin and norepinephrine reuptake inhibitors, and tricyclic antidepressants should be reduced or replaced judiciously with agents that do not cause dream enactment, such as bupropion.
-
(b)
Pharmacotherapy:
Clonazepam has been used successfully as a first-line therapy in doses of 0.5 mg to 2 mg with 90% control of nighttime behaviors (Level B evidence) [118]. Adverse effects are dose-related and include respiratory depression, somnolence, gait trouble, altered cognition, dizziness, and falls. Melatonin (dose 3–15 mg) has been increasingly used as a first-line agent (Level B evidence) due to the preferable side effect profile, especially in elderly patients with cognitive impairment [121]. A combination of both agents may be needed if single therapy is not efficacious. If these drugs fail, dopamine agonists (pramipexole, rotigotine) have also been used to treat RBD especially if periodic limb movements are also present. Other agents used are based on limited case reports and series including cholinesterase inhibitors (donepezil, rivastigmine), anticonvulsants (carbamazepine), benzodiazepines (triazolam), antipsychotics (clozapine, quetiapine), levodopa, sodium oxybate, and ramelteon.
-
(c)
Counseling:
Patients with idiopathic RBD should be appropriately counseled about the risk of future development of alpha-synucleinopathies; this is a complex issue that has recently been comprehensively addressed [122]. Yearly surveillance should be conducted with detailed clinical evaluation for early detection and proper management of any emergent neurodegenerative disorder. This is especially relevant in our current times since the International RBD Study Group and the North American Prodromal Synucleinopathy Consortium (funded by the NIH) are enrolling idiopathic RBD patients for imminent neuroprotective trials.
4. Altered States of Consciousness
4.1. Hypnosis
The term “hypnosis” derives from the Greek Hypnos, meaning “to sleep”. It was popularized by James Braid in the middle of the 19th century to designate a sleep-like, highly suggestible state based on induction and relaxation techniques [123]. In the middle of the 20th century, Milton Erickson revolutionized hypnosis application with his individualized, non-authoritarian approaches, which laid the foundation for the development, use, and acceptance of modern clinical hypnosis [124]. Today, hypnosis is often embedded in a broader therapeutic approach and recognized as complemental treatment in psychotherapy, medicine, sports, and forensics [125]. In clinical application, it is mostly known as an efficient tool for pain reduction but might also be useful in phobias, depression, eating disorders, posttraumatic stress disorders, and substance use disorders, among many others [126].
Over two centuries of research have always strived to better describe the phenomenology, efficacy, and challenges of hypnosis; however, the technique is far from being thoroughly explored. Hypnosis can be understood as an altered state of consciousness produced by suggestions from a hypnotist to a hypnotized person to induce changes in perception, cognition, or behavior [125]. In general, the suggestions consist of three phases of: 1—induction, including general suggestions to guide the person into a hypnotic trance; 2—application, including directed suggestions around the specific topic; and 3—termination, including general suggestions to guide the person out of the trance.
4.1.1. Hypnosis, Sleep, and Dreaming
Despite its name, hypnosis reflects few properties of deep sleep. Some external appearances during the hypnotic trance might resemble sleep-like behavior, such as a deeply relaxed body and behavior resembling sleepwalking when the person talks or acts, which contributed to the name of the technique [127]. Moreover, hypnotic suggestions commonly reflect sleep-related terminology, such as inducing a “deep relaxation/sleep” and terminating with “waking up”. However, these associations are rather superficial and more characteristic of the early developments of hypnosis, whereas later research has made efforts to avoid these comparisons and focus on the more central features of hypnosis. Nevertheless, hypnosis shares neurophenomenological similarities with dreaming and can interact with dreaming and sleep behavior.
Overall, hypnosis is thought to be composed of the three main mechanisms of: 1—suggestibility (i.e., non-voluntary and uncritical compliance with suggestions); 2—absorption (i.e., total perceptual, imaginative, and ideational attention); and 3—dissociation (i.e., experiences and actions detached from self-control) [128]. These may also play a role in dreaming, for example, through the spontaneous integration of external or internal stimuli (e.g., alarm clock or school exam [52]) in the dream experience (suggestibility), the total, unreflective immersion into the dream narrative (absorption), and the uncritical acceptance of bizarre dream elements (dissociation) (compare with Psychedelics Section).
Hypnosis and dreaming are characterized by an overall detachment from the external environment with an attentional focus on the current internal experience, which, in hypnosis, is externally suggested by a hypnotist [128,129]. This experience mostly consists of visual narratives but can involve all senses depending on the suggestions, similar to dreaming [64,130]). Hypnosis and dreaming are characterized by reduced self-reflective processing and loosened self-boundaries [128,130]. Both can evoke autobiographical memories but also generate false memories [131,132]. Hypnosis and dreaming also can spontaneously activate symbolic content and bizarre features [133]. Whereas meta-awareness is present in lucid but not in non-lucid dreams, it can be fostered but also inhibited in hypnosis depending on the suggestion, establishing hypnosis as compared to both dream types [67,134].
Hypnosis, dreaming, and sleep states might also be entangled and influence each other. Hypnosis can improve sleep quality [135] and be helpful in parasomnias such as nightmares, sleep terror, and sleepwalking [120]. Hypnotic dreams, i.e., suggestions to dream during the hypnotic state, can be used to induce, re-experience, intensify, and modulate nocturnal dreams or daydreams [136] and are phenomenologically similar to these [137].
Notably, associations were found between hypnotizability, i.e., the capacity to enter hypnosis, and sleep/dreaming behaviors. Hypnotizability correlated with the ease of falling asleep at night [127], the capacity to dream on a chosen topic, and the frequency of (precognitive and out-of-body) dreams [138]. Moreover, hypnotic dreams in highly hypnotizable persons resemble more nocturnal dreams than daydreams regarding length, emotionality, characters, setting, and distortions [137].
4.1.2. Hypnosis and the Brain
Neurophysiologically, hypnosis has been thought to induce brain states characterized by attention, relaxation, and dissociation [139]. Numerous neuroimaging studies have examined the brain activity associated with hypnosis and found some support for these assumptions (as described below), although diverse findings beyond that have emerged. A summary of results is difficult due to the multifaceted nature of techniques, purposes, internal, and external factors, making every study unique and considerably influencing the neuronal responses. In this light, it is not astonishing that a recent meta-analysis of neuroimaging data solely reported the activation of one region correlated with hypnosis, namely the lingual gyrus [140]. This region is involved in higher-order visual perception and mental imagery, highlighting the importance of visual imagery for the hypnotic state and reinforcing subjective findings.
Beyond that, hypnosis seems to modulate three main brain networks, namely, the central executive network, salience network, and default mode network (DMN) (Figure 1), pointing to the profound impact of hypnosis on fundamental brain processes. Specifically, hypnotic depth and absorption seem to be related to changes in the dorsolateral prefrontal cortex and inferior parietal cortex (central executive network), changes in the insula and anterior cingulate cortex (salience network), and decreases in the medial prefrontal cortex and precuneus (DMN) [140]. Changes in these networks for processing task-related activities (central executive network) and self-related daydreaming (DMN), together with reductions in the processing perception of sensory networks, might underlie the subjective and behavioral findings of hypnosis-related increased attention, changed meta/body awareness, and decreased environmental processing and mind-wandering [140,141].
This notion is supported by studies investigating electroencephalographic rhythms. Here, hypnosis seems generally characterized by increased occipital gamma, a frequency related to attention and concentration in a region of visual processing, reinforcing the notion of the predominance of visual imagery in hypnosis [141]. Moreover, hypnosis was associated with increased frontal alpha and decreased central, frontal, and parietal gamma, potentially related to increased relaxation [141]. Hypnosis is also commonly associated with increased theta, a frequency related to relaxation and sleep but also to emotion and memory encoding and recall, which is why it has been speculated that theta might facilitate the response to suggestions by retrieving the corresponding perceptual/cognitive experiences from memory [142]. Notably, decreased alpha might play a role in the more specific facets of hypnosis. Precisely, subjective dissociation under hypnosis was associated with decreased frontal–parietal alpha synchrony, pointing to a role of this brain network in dissociated awareness under hypnosis [143]. Furthermore, hypnotic dreams (compared with rest hypnosis) were associated with decreased alpha, pointing to brain activations related to dream suggestions [144].
4.2. Anesthesia
“You will fall asleep now” is the most common sentence anesthesiologists use before administering hypnotics [145]. Trying to understand the biological basis of how the human mind shifts from an alert (or responsive) state to (natural) sleep or (artificial) anesthesia is a recent and important object of study in neuroscience. First, it is necessary to differentiate two confusing concepts: wakefulness and an “unconscious” state. In the context of anesthesia, despite the state of consciousness being defined by the behavior of the individual, the lack of response does not indicate unawareness or lack of experiences that were generated only internally, so it does not mean unconsciousness [146]. During wakefulness—the “connected” state—the contents that reach consciousness are modulated through a sensory filter, which allows the conscious perception of stimuli. However, during anesthesia—the “disconnected (or dissociated)” state—the contents of consciousness revolve around internally generated experiences, such as the individual’s imagination [147].
4.2.1. Sleep, Anesthesia, and the Brain Rhythms
Sleep and general anesthesia are characterized by similar behavioral correlates, such as decreased responsiveness, arousal, and movement. In terms of brain activity, scalp electroencephalographic recordings demonstrated analogous spectral characteristics of both states, such as the presence of slow waves (~1 Hz) or delta oscillations (1–4 Hz), as observed mainly in deep sleep (N3) [145].
Modern theories of memory consolidation during sleep postulate that novel information is initially encoded in hippocampal regions and, as time passes, becomes mainly neocortical [148]. Hippocampus-dependent information is replayed during sleep, and this replay is connected to a hippocampal sharp-wave ripple (80–120 Hz), which is nested in thalamocortical spindles (12–16 Hz) and cortical slow waves (~1 Hz) [149]. Intracranial recordings during anesthesia show altered delta–alpha or delta–gamma cross-frequency coupling on the temporal scale and delta, alpha, or gamma phase synchronization on the l spatial scale [146]. These authors argue that decreased cortical network synchronization is unfavorable for information integration in large-scale networks, which is in accordance with the finding that processing in primary sensory areas is intact under general anesthesia, whereas processing in secondary sensory and higher-order association areas was reduced [150].
Recently, Zimmern [151] proposed that neural networks operate close to “criticality”, that is, at a transition between ordered and chaotic states, which could be optimal for processing and transferring information. It was observed that anesthesia renders neural activity less critical, i.e., more predictable [152]. It has been hypothesized that a high variability near the network transitions is necessary to be conscious, whereas anesthesia promotes unconsciousness by inducing a shift away from the network bifurcation [145].
4.2.2. Neuroimaging Anesthesia
A recent work by Scheinin [153] tried to study the gray area between the connected and the disconnected states, such as consciousness and unconsciousness, aiming to answer the question of what happens to brain activity when conscious awareness of the world disappears. Thus, they separated volunteers into two groups: in the first, participants were awake and were randomized to receive propofol or dexmedetomidine until they stopped responding. The second group consisted of deprived wakefulness and NREM sleep. To study the transition between the levels of consciousness and the main areas of the brain affected, awakenings were applied in a forced way to capture this moment using positron emission tomography. In this way, one could observe the unresponsive state transitioning to the responsive state, followed by immediate stimuli to assess internal experiences during the preceding unresponsive condition. Functional brain imaging comparing responsive, connected versus unresponsive, and disconnected states of consciousness during constant anesthetic exposure revealed increased activity of the thalamus, cingulate cortices, and angular gyri during responsive states, indicating that these areas are fundamental for human consciousness. These structures were affected independently by the pharmacologic agent, drug concentration, and direction of change in the state of consciousness. State-specific findings were distinct and separable from the overall effects of the interventions, which included widespread depression of brain activity across cortical areas. These findings identify the central brain network for human consciousness.
4.3. Psychedelics
Classic serotonergic psychedelics, such as lysergic acid diethylamide (LSD), psilocybin, and ayahuasca, are gaining growing scientific attention due to their therapeutic potential in diverse psychiatric conditions, especially mood and substance use disorders [154,155,156]. After a research hiatus following political motivations by the end of the 1960s, their profound effects on the human mind are being increasingly studied [157]. Findings from the last century and modern studies highlight the fundamental effects of psychedelics on perception, cognition, and emotion, including altered perceptions of the senses, self, body, time, and space, reduced cognitive control, and heightened emotionality [158,159].
4.3.1. Psychedelics and Dreaming
Psychedelics were also termed “oneirogens”, from the Greek óneiros meaning “dream” and gen “to create”, due to their phenomenological similarity to dreams regarding visual, body- and self-perception, emotionality, memory, and cognition [160]. Accordingly, psychedelics have been conceptualized as experimental dreams and dreams as hallucinatory experiences [129,161].
Regarding perception, psychedelics increase the sensitivity to and distort the perception of external and internal stimuli [158]. Dreams often induce sensorimotor hallucinations that are embedded in a narrative context and mostly detached from environmental and bodily stimuli [162]. A marked feature is a lack of awareness that one is dreaming, which is gained in LD [58,67]. Therefore, psychedelics are thought to be phenomenologically most similar to LD, a notion supported by recent findings of linguistic similarity between reports on psychedelic and dream experiences [163]. Notably, the reports on Datura plants, containing tropane alkaloids, showed linguistic similarities to non-lucid dreams, whereas sedatives, stimulants, antipsychotics, and antidepressants showed no similarity to dream reports.
On the topic of self and body, psychedelics are well known to distort, weaken, or dissolve perceived self and body boundaries, including impaired self-control, separation from and unreality of the body, and self-transcendence [164]. Dreams are mostly reflected by a self-centered perspective, although self and body boundaries might be weakened or dissolved, especially in non-lucid dreams [129], and even reflect self-transcendence [165]. In LD, body boundaries are usually strong [129], whereas the self can be divided into one experiencing and one watching part, the latter of which can influence the narrative [166].
Considering emotion and memory, dreams are characterized by high, often negative emotionality, which is thought of as the adaptive function for fear extinction through deconditioning [167]. Similarly, psychedelics intensify emotionality, including mainly positive affects but also anxiety and challenging experiences [168] and may activate autobiographical memories, memory recall, and consolidation [169,170]. Therefore, psychedelics might aid the fear memory extinction by reactivation, modulation, and reconsolidation, a notion supported by animal studies [171,172].
Regarding cognition, psychedelics decrease coherent, rational, targeted thinking, as well as attention, working memory, and cognitive control, and induce chaotic and bizarre thinking [173,174]. On the other hand, they increase associative, surprising, meaningful, and symbolic thinking [175]. Dreams are reflected by cognitive bizarreness, including incongruities, uncertainties, and discontinuities in the narrative [133] but might also facilitate cognitive flexibility, associative thinking, creativity, and insights [176,177,178,179].
Despite these similarities, there are some main differences between psychedelic and dream states, including perceived characteristic geometric patterns and a decoupled conscious perception from external stimuli under psychedelics and the lack of meta-cognition in (non-lucid) dreams. Therefore, psychedelic experiences seem to especially resemble LD [160].
4.3.2. Psychedelics and the Brain
Besides phenomenology, psychedelics and dreams show neurophysiological similarities from the receptor to the brain network level. The cerebral serotonin (5-HT) receptors seem essential for mediating psychedelic effects [157]. 5-HT2A receptors mediated the “dreamlike” effects of psychedelics during mental imagery [180]. 5-HT receptors also play a key role in the sleep–wake cycle and dreaming [181]. 5-HT2 receptors mediate some of the psychedelic effects on sleep regulation, including increased wakefulness, reduced slow-wave sleep and activity, and changed REM sleep latency, duration, and episodes [157,182,183].
Brain imaging studies reported functional changes in regions processing sensory, self, and body perception and emotion, memory, and cognition. Regarding sensory perception, psychedelics impair thalamocortical feedback loops, potentially accounting for impaired sensory filtering and inducing an information overload [158]. Moreover, they activate primary, secondary, and associative visual areas and frontal areas that partially correlate with complex imagery; in line with this, these areas are similarly activated during imagination and perception of images under psychedelics [184,185]. In dreaming, the brainstem, primary and secondary visual areas, and higher-order frontal areas are activated during the characteristic visual mental imagery. For psychedelics and dreaming, it is still a matter of debate whether these activations occur in bottom-up or top-down directions [160].
Regarding self and body perception, among the most prominently and consistently reported psychedelic effects are decreases in the default mode network (DMN) [186] (Figure 1). As said before, the DMN is considered the neural correlate of the self, daydreaming, and dreaming [27,187]. Specifically, dreams seem to deactivate the posterior cingulate cortex and precuneus [188], two DMN regions important for self-reflection and perspective-taking [189], which might explain the loosened self and body boundaries. The precuneus was increased during lucid compared with non-lucid dreaming [65]. Psychedelics activate areas processing emotion and memory, including the amygdala, hippocampus, and anterior cingulate cortex [190,191], and these areas are also activated during dreaming [61].
Regarding cognition, psychedelics decrease frontal activity and connectivity, such as in the dorsolateral prefrontal cortex, which is important for cognitive control and contextual processing, potentially accounting for less critical and controlled but more bizarre thinking styles [192,193,194]. This region is also deactivated during dreaming, which might explain the acceptance of bizarre narratives, lack of meta-awareness, and volitional control [188]. These phenomena might also be explained by reduced gamma activity, a frequency important for the integration of content from different regions and related to waking consciousness [63]. Notably, frontotemporal gamma is increased during LD [56,58] and under psychedelics [195].
Overall, these studies suggest a crucial role of the 5-HT receptors in mediating dream-like, subjective effects under psychedelics closely related to the mechanisms of dreaming. Moreover, a substantial body of evidence indicates activation of brain areas processing vision, emotion, memory, and cognition in both states, highlighting their neurophysiological similarity. Together with the abovementioned perceptual, emotional, and cognitive similarities, these findings point to neurophenomenological similarities between psychedelics and dreams, particularly LD.
5. Conclusions and Future Directions
In this review, we classified the sleep-related dissociative states into three categories—physiological, pathological, and altered states of consciousness—and described their neurobiology and phenomenology based on three examples each. Some of these dissociative states are directly related to sleep and dreaming, such as lucid dreaming (physiological) and REM sleep behavior disorder (pathological). However, others are more indirectly related, such as psychedelics (altered), resembling more the state of lucid dreaming. It is also important to highlight that, despite some states being classified as pathological, such as sleep paralysis and sleepwalking, they are only considered a disorder if they occur too often and/or intensely, resulting in sociological, psychological, or physical harm to the person.
For sleep research in general, the close exchange between basic and clinical investigators is crucial, since basic science can be answered by clinical questions and clinical questions can guide the direction of basic research [5]. Studying daydreams improves our understanding of depression because it is related to negative daydreaming, also known as rumination. Hypnosis is a remarkable technique that supports the treatment of many symptoms, especially pain. Since REM sleep behavior disorder is associated with Parkinson’s disease, recognizing this sleep disturbance can facilitate early diagnosis and increase treatment efficacy for patients with Parkinson’s. Future research on sleep-related dissociative states could also bring us significant results. For example, Peters and colleagues [196] recently reviewed works that investigated LD as a form of mental training of motor skills and observed that this special kind of dreaming has the potential to improve motor performance during waking, which could be a revolution in sports science. Moreover, psychedelics such as ayahuasca have shown promising results for treatment-resistant depression and are now being tested in other psychiatric syndromes.
Beyond this collaboration between basic and clinical research, to fully understand the different physiological, pathological, and altered sleep-related dissociative states, anthropological, historical, and philosophical approaches are equally necessary. The collaboration of biomedical and social sciences can be extremely fruitful for future studies that aim to investigate the nature of human consciousness, as well as for developing new treatments for neuropsychiatric diseases.
Acknowledgments
We thank Ingrid Pereira Alves for helping with language translation and Davi Drieskens for the artwork of Figure 1.
Author Contributions
All authors participated in the original draft preparation, review, and editing. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
This is a review article, thus there is no data to share.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by CAPES and CNPq (Brazil).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Krueger J.M., Nguyen J.T., Dykstra-Aiello C.J., Taishi P. Local Sleep. Sleep Med. Rev. 2019;43:14–21. doi: 10.1016/j.smrv.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scarpelli S., Alfonsi V., Gorgoni M. Parasomnias and Disruptive Sleep-Related Disorders: Insights from Local Sleep Findings. J. Clin. Med. 2022;11:4435. doi: 10.3390/jcm11154435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huber R., Felice Ghilardi M., Massimini M., Tononi G. Local Sleep and Learning. Nature. 2004;430:78–81. doi: 10.1038/nature02663. [DOI] [PubMed] [Google Scholar]
- 4.Vyazovskiy V.V., Olcese U., Hanlon E.C., Nir Y., Cirelli C., Tononi G. Local Sleep in Awake Rats. Nature. 2011;472:443–447. doi: 10.1038/nature10009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahowald M.W., Cramer Bornemann M.A., Schenck C.H. State Dissociation, Human Behavior, and Consciousness. Curr. Top. Med. Chem. 2011;11:2392–2402. doi: 10.2174/156802611797470277. [DOI] [PubMed] [Google Scholar]
- 6.Singer J.L., McCraven V.G. Some Characteristics of Adult Daydreaming. J. Psychol. 1961;51:151–164. doi: 10.1080/00223980.1961.9916467. [DOI] [Google Scholar]
- 7.McMillan R.L., Kaufman S.B., Singer J.L. Ode to Positive Constructive Daydreaming. Front. Psychol. 2013;4:626. doi: 10.3389/fpsyg.2013.00626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schooler J.W., Smallwood J., Christoff K., Handy T.C., Reichle E.D., Sayette M.A. Meta-Awareness, Perceptual Decoupling and the Wandering Mind. Trends Cogn. Sci. 2011;15:319–326. doi: 10.1016/j.tics.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Ribeiro S. O Oráculo Da Noite: A História e a Ciência Do Sonho. Editora Companhia das Letras; Rio de Janeiro, Brazil: 2019. [Google Scholar]
- 10.Immordino-Yang M.H., Christodoulou J.A., Singh V. Rest Is Not Idleness: Implications of the Brain’s Default Mode for Human Development and Education. Perspect. Psychol. Sci. 2012;7:352–364. doi: 10.1177/1745691612447308. [DOI] [PubMed] [Google Scholar]
- 11.Smallwood J., Fitzgerald A., Miles L.K., Phillips L.H. Shifting Moods, Wandering Minds: Negative Moods Lead the Mind to Wander. Emotion. 2009;9:271–276. doi: 10.1037/a0014855. [DOI] [PubMed] [Google Scholar]
- 12.Singer J.L. The Inner World of Daydreaming. 1st ed. Harper & Row; New York, NY, USA: 1975. [Google Scholar]
- 13.Giambra L.M. Daydreaming across the Life Span: Late Adolescent to Senior Citizen. Int. J. Aging Hum. Dev. 1974;5:115–140. doi: 10.2190/7AEJ-T3MA-QLGD-CCF5. [DOI] [PubMed] [Google Scholar]
- 14.Giambra L.M. A Laboratory Method for Investigating Influences on Switching Attention to Task-Unrelated Imagery and Thought. Conscious. Cogn. 1995;4:1–21. doi: 10.1006/ccog.1995.1001. [DOI] [PubMed] [Google Scholar]
- 15.Zhiyan T., Singer J.L. Daydreaming Styles, Emotionality and the Big Five Personality Dimensions. Imagin. Cogn. Personal. 1997;16:399–414. doi: 10.2190/ATEH-96EV-EXYX-2ADB. [DOI] [Google Scholar]
- 16.Klinger E. Goal Commitments and the Content of Thoughts and Dreams: Basic Principles. Front. Psychol. 2013;4:415. doi: 10.3389/fpsyg.2013.00415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Franklin M.S., Smallwood J., Schooler J.W. Catching the Mind in Flight: Using Behavioral Indices to Detect Mindless Reading in Real Time. Psychon. Bull. Rev. 2011;18:992–997. doi: 10.3758/s13423-011-0109-6. [DOI] [PubMed] [Google Scholar]
- 18.Smallwood J., O’Connor R.C., Heim D. Rumination, Dysphoria, and Subjective Experience. Imagin. Cogn. Personal. 2005;24:355–367. doi: 10.2190/AE18-AD1V-YF7L-EKBX. [DOI] [Google Scholar]
- 19.McVay J.C., Kane M.J. Why Does Working Memory Capacity Predict Variation in Reading Comprehension? On the Influence of Mind Wandering and Executive Attention. J. Exp. Psychol. Gen. 2012;141:302–320. doi: 10.1037/a0025250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whitfield-Gabrieli S., Ford J.M. Default Mode Network Activity and Connectivity in Psychopathology. Annu. Rev. Clin. Psychol. 2012;8:49–76. doi: 10.1146/annurev-clinpsy-032511-143049. [DOI] [PubMed] [Google Scholar]
- 21.Giambra L.M., Traynor T.D. Depression and Daydreaming; an Analysis Based on Self-Ratings. J. Clin. Psychol. 1978;34:14–25. [PubMed] [Google Scholar]
- 22.Meyer T.D., Finucane L., Jordan G. Is Risk for Mania Associated with Increased Daydreaming as a Form of Mental Imagery? J. Affect. Disord. 2011;135:380–383. doi: 10.1016/j.jad.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Marchetti I., Koster E.H.W., De Raedt R. Mindwandering Heightens the Accessibility of Negative Relative to Positive Thought. Conscious. Cogn. 2012;21:1517–1525. doi: 10.1016/j.concog.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 24.Marchetti I., Van de Putte E., Koster E. Self-Generated Thoughts and Depression: From Daydreaming to Depressive Symptoms. Front. Hum. Neurosci. 2014;8:131. doi: 10.3389/fnhum.2014.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aldao A., Nolen-Hoeksema S., Schweizer S. Emotion-Regulation Strategies across Psychopathology: A Meta-Analytic Review. Clin. Psychol. Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 26.Raichle M.E., MacLeod A.M., Snyder A.Z., Powers W.J., Gusnard D.A., Shulman G.L. A Default Mode of Brain Function. Proc. Natl. Acad. Sci. USA. 2001;98:676–682. doi: 10.1073/pnas.98.2.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Domhoff G.W., Fox K.C.R. Dreaming and the Default Network: A Review, Synthesis, and Counterintuitive Research Proposal. Conscious. Cogn. 2015;33:342–353. doi: 10.1016/j.concog.2015.01.019. [DOI] [PubMed] [Google Scholar]
- 28.Raichle M.E., Snyder A.Z. A Default Mode of Brain Function: A Brief History of an Evolving Idea. NeuroImage. 2007;37:1083–1090; discussion 1097–1099. doi: 10.1016/j.neuroimage.2007.02.041. [DOI] [PubMed] [Google Scholar]
- 29.Andrews-Hanna J.R., Reidler J.S., Sepulcre J., Poulin R., Buckner R.L. Functional-Anatomic Fractionation of the Brain’s Default Network. Neuron. 2010;65:550–562. doi: 10.1016/j.neuron.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horovitz S.G., Fukunaga M., de Zwart J.A., van Gelderen P., Fulton S.C., Balkin T.J., Duyn J.H. Low Frequency BOLD Fluctuations during Resting Wakefulness and Light Sleep: A Simultaneous EEG-FMRI Study. Hum. Brain Mapp. 2008;29:671–682. doi: 10.1002/hbm.20428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vincent J.L., Patel G.H., Fox M.D., Snyder A.Z., Baker J.T., Van Essen D.C., Zempel J.M., Snyder L.H., Corbetta M., Raichle M.E. Intrinsic Functional Architecture in the Anaesthetized Monkey Brain. Nature. 2007;447:83–86. doi: 10.1038/nature05758. [DOI] [PubMed] [Google Scholar]
- 32.Fox M.D., Snyder A.Z., Vincent J.L., Corbetta M., Van Essen D.C., Raichle M.E. The Human Brain Is Intrinsically Organized into Dynamic, Anticorrelated Functional Networks. Proc. Natl. Acad. Sci. USA. 2005;102:9673–9678. doi: 10.1073/pnas.0504136102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hilland E., Johannessen C., Jonassen R., Alnæs D., Jørgensen K.N., Barth C., Andreou D., Nerland S., Wortinger L.A., Smelror R.E., et al. Aberrant Default Mode Connectivity in Adolescents with Early-Onset Psychosis: A Resting State FMRI Study. NeuroImage Clin. 2022;33:102881. doi: 10.1016/j.nicl.2021.102881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Braboszcz C., Delorme A. Lost in Thoughts: Neural Markers of Low Alertness during Mind Wandering. NeuroImage. 2011;54:3040–3047. doi: 10.1016/j.neuroimage.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 35.Oken B.S., Salinsky M.C., Elsas S.M. Vigilance, Alertness, or Sustained Attention: Physiological Basis and Measurement. Clin. Neurophysiol. Off. J. Int. Fed. Clin. Neurophysiol. 2006;117:1885–1901. doi: 10.1016/j.clinph.2006.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sabri M., Labelle S., Gosselin A., Campbell K.B. Effects of Sleep Onset on the Mismatch Negativity (MMN) to Frequency Deviants Using a Rapid Rate of Presentation. Brain Res. Cogn. Brain Res. 2003;17:164–176. doi: 10.1016/S0926-6410(03)00090-9. [DOI] [PubMed] [Google Scholar]
- 37.Lang A.H., Eerola O., Korpilahti P., Holopainen I., Salo S., Aaltonen O. Practical Issues in the Clinical Application of Mismatch Negativity. Ear Hear. 1995;16:118–130. doi: 10.1097/00003446-199502000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Winter O., Kok A., Kenemans J.L., Elton M. Auditory Event-Related Potentials to Deviant Stimuli during Drowsiness and Stage 2 Sleep. Electroencephalogr. Clin. Neurophysiol. 1995;96:398–412. doi: 10.1016/0168-5597(95)00030-V. [DOI] [PubMed] [Google Scholar]
- 39.La Berge S.P. Lucid Dreaming as a Learnable Skill: A Case Study. Percept. Mot. Ski. 1980;51:1039–1042. doi: 10.2466/pms.1980.51.3f.1039. [DOI] [Google Scholar]
- 40.Mota-Rolim S.A., Bulkeley K., Campanelli S., Lobão-Soares B., de Araujo D.B., Ribeiro S. The Dream of God: How Do Religion and Science See Lucid Dreaming and Other Conscious States During Sleep? Front. Psychol. 2020;11:555731. doi: 10.3389/fpsyg.2020.555731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferreira G.H., Prata T.d.A., Fontenele-Araujo J., de Carvalho F.T., Mota-Rolim S.A. I Dream Therefore I Am: A Review on Lucid Dreaming in Western Philosophy. Dreaming. 2021;31:69–87. doi: 10.1037/drm0000156. [DOI] [Google Scholar]
- 42.Dennett D.C. Are Dreams Experiences? Philos. Rev. 1976;85:151. doi: 10.2307/2183728. [DOI] [Google Scholar]
- 43.Aserinsky E., Kleitman N. Regularly Occurring Periods of Eye Motility, and Concomitant Phenomena, During Sleep. Science. 1953;118:273–274. doi: 10.1126/science.118.3062.273. [DOI] [PubMed] [Google Scholar]
- 44.Jouvet M. Research on the neural structures and responsible mechanisms in different phases of physiological sleep. Arch. Ital. Biol. 1962;100:125–206. [PubMed] [Google Scholar]
- 45.Dement W., Wolpert E.A. The Relation of Eye Movements, Body Motility, and External Stimuli to Dream Content. J. Exp. Psychol. 1958;55:543–553. doi: 10.1037/h0040031. [DOI] [PubMed] [Google Scholar]
- 46.Mota-Rolim S.A. On Moving the Eyes to Flag Lucid Dreaming. Front. Neurosci. 2020;14:361. doi: 10.3389/fnins.2020.00361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.La Berge S.P., Nagel L.E., Dement W.C., Zarcone V.P. Lucid Dreaming Verified by Volitional Communication during REM Sleep. Percept. Mot. Ski. 1981;52:727–732. doi: 10.2466/pms.1981.52.3.727. [DOI] [PubMed] [Google Scholar]
- 48.LaBerge S., Levitan L., Dement W.C. Lucid Dreaming: Physiological Correlates of Consciousness during REM Sleep. J. Mind Behav. 1986;7:251–258. [Google Scholar]
- 49.Brylowski A., Levitan L., LaBerge S. H-Reflex Suppression and Autonomic Activation during Lucid REM Sleep: A Case Study. Sleep. 1989;12:374–378. doi: 10.1093/sleep/12.4.374. [DOI] [PubMed] [Google Scholar]
- 50.Stumbrys T., Erlacher D. Lucid Dreaming during NREM Sleep: Two Case Reports. Int. J. Dream Res. 2012;5:151–155. doi: 10.11588/IJODR.2012.2.9483. [DOI] [Google Scholar]
- 51.Mota Rolim S.A., Brandão D.S., Andrade K.C., de Queiroz C.M.T., Araujo J.F., de Araujo D.B., Ribeiro S. Neurophysiological Features of Lucid Dreaming During N1 And N2 Sleep Stages: Two Case Reports. Sleep Sci. 2015;8:215. doi: 10.1016/j.slsci.2016.02.093. [DOI] [Google Scholar]
- 52.Mota-Rolim S., Targino Z., Souza B., Blanco W., Araujo J., Ribeiro S. Dream Characteristics in a Brazilian Sample: An Online Survey Focusing on Lucid Dreaming. Front. Hum. Neurosci. 2013;7:836. doi: 10.3389/fnhum.2013.00836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ogilvie R.D., Hunt H.T., Tyson P.D., Lucescu M.L., Jeakins D.B. Lucid Dreaming and Alpha Activity: A Preliminary Report. Percept. Mot. Ski. 1982;55:795–808. doi: 10.2466/pms.1982.55.3.795. [DOI] [PubMed] [Google Scholar]
- 54.Tyson P.D., Ogilvie R.D., Hunt H.T. Lucid, Prelucid, and Nonlucid Dreams Related to the Amount of EEG Alpha Activity during REM Sleep. Psychophysiology. 1984;21:442–451. doi: 10.1111/j.1469-8986.1984.tb00224.x. [DOI] [PubMed] [Google Scholar]
- 55.Holzinger B., LaBerge S., Levitan L. Psychophysiological Correlates of Lucid Dreaming. Dreaming. 2006;16:88–95. doi: 10.1037/1053-0797.16.2.88. [DOI] [Google Scholar]
- 56.Voss U., Holzmann R., Tuin I., Hobson J.A. Lucid Dreaming: A State of Consciousness with Features of Both Waking and Non-Lucid Dreaming. Sleep. 2009;32:1191–1200. doi: 10.1093/sleep/32.9.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dodet P., Chavez M., Leu-Semenescu S., Golmard J.-L., Arnulf I. Lucid Dreaming in Narcolepsy. Sleep. 2015;38:487–497. doi: 10.5665/sleep.4516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Baird B., Mota-Rolim S.A., Dresler M. The Cognitive Neuroscience of Lucid Dreaming. Neurosci. Biobehav. Rev. 2019;100:305–323. doi: 10.1016/j.neubiorev.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mota-Rolim S.A., Erlacher D., Tort A.B.L., Araujo J.F., Ribeiro S. Different Kinds of Subjective Experience during Lucid Dreaming May Have Different Neural Substrates. J. Neurosci. 2010;25:550–557. doi: 10.11588/IJODR.2010.1.596. [DOI] [Google Scholar]
- 60.Baird B., Tononi G., LaBerge S. Lucid Dreaming Occurs in Activated Rapid Eye Movement Sleep, Not a Mixture of Sleep and Wakefulness. Sleep. 2022;45:zsab294. doi: 10.1093/sleep/zsab294. [DOI] [PubMed] [Google Scholar]
- 61.Braun A. Regional Cerebral Blood Flow throughout the Sleep-Wake Cycle. An H2(15)O PET Study. Brain. 1997;120:1173–1197. doi: 10.1093/brain/120.7.1173. [DOI] [PubMed] [Google Scholar]
- 62.Maquet P., Péters J., Aerts J., Delfiore G., Degueldre C., Luxen A., Franck G. Functional Neuroanatomy of Human Rapid-Eye-Movement Sleep and Dreaming. Nature. 1996;383:163–166. doi: 10.1038/383163a0. [DOI] [PubMed] [Google Scholar]
- 63.Hobson J.A. REM Sleep and Dreaming: Towards a Theory of Protoconsciousness. Nat. Rev. Neurosci. 2009;10:803–813. doi: 10.1038/nrn2716. [DOI] [PubMed] [Google Scholar]
- 64.Nir Y., Tononi G. Dreaming and the Brain: From Phenomenology to Neurophysiology. Trends Cogn. Sci. 2010;14:88–100. doi: 10.1016/j.tics.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dresler M., Wehrle R., Spoormaker V.I., Koch S.P., Holsboer F., Steiger A., Obrig H., Sämann P.G., Czisch M. Neural Correlates of Dream Lucidity Obtained from Contrasting Lucid versus Non-Lucid REM Sleep: A Combined EEG/FMRI Case Study. Sleep. 2012;35:1017–1020. doi: 10.5665/sleep.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Baird B., Castelnovo A., Gosseries O., Tononi G. Frequent Lucid Dreaming Associated with Increased Functional Connectivity between Frontopolar Cortex and Temporoparietal Association Areas. Sci. Rep. 2018;8:17798. doi: 10.1038/s41598-018-36190-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Filevich E., Dresler M., Brick T.R., Kühn S. Metacognitive Mechanisms Underlying Lucid Dreaming. J. Neurosci. 2015;35:1082–1088. doi: 10.1523/JNEUROSCI.3342-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dixon M.L., De La Vega A., Mills C., Andrews-Hanna J., Spreng R.N., Cole M.W., Christoff K. Heterogeneity within the Frontoparietal Control Network and Its Relationship to the Default and Dorsal Attention Networks. Proc. Natl. Acad. Sci. USA. 2018;115:E1598–E1607. doi: 10.1073/pnas.1715766115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thomas Yeo B.T., Krienen F.M., Sepulcre J., Sabuncu M.R., Lashkari D., Hollinshead M., Roffman J.L., Smoller J.W., Zöllei L., Polimeni J.R., et al. The Organization of the Human Cerebral Cortex Estimated by Intrinsic Functional Connectivity. J. Neurophysiol. 2011;106:1125–1165. doi: 10.1152/jn.00338.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Blanke O., Mohr C., Michel C.M., Pascual-Leone A., Brugger P., Seeck M., Landis T., Thut G. Linking Out-of-Body Experience and Self Processing to Mental Own-Body Imagery at the Temporoparietal Junction. J. Neurosci. 2005;25:550–557. doi: 10.1523/JNEUROSCI.2612-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Buzzi G. False Awakenings in Light of the Dream Protoconsciousness Theory: A Study in Lucid Dreamers. Int. J. Dream Res. 2011;4:110–116. doi: 10.11588/IJODR.2011.2.9085. [DOI] [Google Scholar]
- 72.Raduga M., Kuyava O., Sevcenko N. Is There a Relation among REM Sleep Dissociated Phenomena, like Lucid Dreaming, Sleep Paralysis, out-of-Body Experiences, and False Awakening? Med. Hypotheses. 2020;144:110169. doi: 10.1016/j.mehy.2020.110169. [DOI] [PubMed] [Google Scholar]
- 73.Mainieri G., Maranci J.-B., Champetier P., Leu-Semenescu S., Gales A., Dodet P., Arnulf I. Are Sleep Paralysis and False Awakenings Different from REM Sleep and from Lucid REM Sleep? A Spectral EEG Analysis. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2021;17:719–727. doi: 10.5664/jcsm.9056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sharpless B.A., McCarthy K.S., Chambless D.L., Milrod B.L., Khalsa S.-R., Barber J.P. Isolated Sleep Paralysis and Fearful Isolated Sleep Paralysis in Outpatients with Panic Attacksb. J. Clin. Psychol. 2010;66:1292–1306. doi: 10.1002/jclp.20724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jalal B., Hinton D.E. Rates and Characteristics of Sleep Paralysis in the General Population of Denmark and Egypt. Cult. Med. Psychiatry. 2013;37:534–548. doi: 10.1007/s11013-013-9327-x. [DOI] [PubMed] [Google Scholar]
- 76.de Sá J.F.R., Mota-Rolim S.A. Sleep Paralysis in Brazilian Folklore and Other Cultures: A Brief Review. Front. Psychol. 2016;7:1294. doi: 10.3389/fpsyg.2016.01294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fukuda K., Miyasita A., Inugami M., Ishihara K. High Prevalence of Isolated Sleep Paralysis: Kanashibari Phenomenon in Japan. Sleep. 1987;10:279–286. doi: 10.1093/sleep/10.3.279. [DOI] [PubMed] [Google Scholar]
- 78.Cassaniti J.L., Luhrmann T.M. The Cultural Kindling of Spiritual Experiences. Curr. Anthropol. 2014;55:S333–S343. doi: 10.1086/677881. [DOI] [Google Scholar]
- 79.Sharpless B.A., Doghramji K. Sleep Paralysis: Historical, Psychological, and Medical Perspectives. Oxford University Press; New York, NY, USA: 2015. [Google Scholar]
- 80.McNally R.J., Clancy S.A. Sleep Paralysis, Sexual Abuse, and Space Alien Abduction. [(accessed on 18 March 2023)];Transcult. Psychiatry. 2005 42:113–122. doi: 10.1177/1363461505050715. Available online: https://journals.sagepub.com/doi/10.1177/1363461505050715. [DOI] [PubMed] [Google Scholar]
- 81.Cheyne J.A., Rueffer S.D., Newby-Clark I.R. Hypnagogic and Hypnopompic Hallucinations during Sleep Paralysis: Neurological and Cultural Construction of the Night-Mare. Conscious. Cogn. 1999;8:319–337. doi: 10.1006/ccog.1999.0404. [DOI] [PubMed] [Google Scholar]
- 82.Hinton D.E., Hufford D.J., Kirmayer L.J. Culture and Sleep Paralysis. Transcult. Psychiatry. 2005;42:5–10. doi: 10.1177/1363461505050708. [DOI] [Google Scholar]
- 83.Denis D., French C.C., Gregory A.M. A Systematic Review of Variables Associated with Sleep Paralysis. Sleep Med. Rev. 2018;38:141–157. doi: 10.1016/j.smrv.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 84.Dement W., Kleitman N. The Relation of Eye Movements during Sleep to Dream Activity: An Objective Method for the Study of Dreaming. J. Exp. Psychol. 1957;53:339–346. doi: 10.1037/h0048189. [DOI] [PubMed] [Google Scholar]
- 85.Jouvet M. Locus Coeruleus et Sommeil Paradoxal. Comptes Rendus Séances Société Biol. Ses Fil. 1965;159:895–899. [PubMed] [Google Scholar]
- 86.Brooks P.L., Peever J.H. Identification of the Transmitter and Receptor Mechanisms Responsible for REM Sleep Paralysis. J. Neurosci. 2012;32:9785–9795. doi: 10.1523/JNEUROSCI.0482-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Dahlitz M., Parkes J.D. Sleep Paralysis. Lancet. 1993;341:406–407. doi: 10.1016/0140-6736(93)92992-3. [DOI] [PubMed] [Google Scholar]
- 88.Jalal B., Ramachandran V.S. Sleep Paralysis and “the Bedroom Intruder”: The Role of the Right Superior Parietal, Phantom Pain and Body Image Projection. Med. Hypotheses. 2014;83:755–757. doi: 10.1016/j.mehy.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 89.Umanath S., Sarezky D., Finger S. Sleepwalking through History: Medicine, Arts, and Courts of Law. J. Hist. Neurosci. 2011;20:253–276. doi: 10.1080/0964704X.2010.513475. [DOI] [PubMed] [Google Scholar]
- 90.Harris M., Grunstein R.R. Treatments for Somnambulism in Adults: Assessing the Evidence. Sleep Med. Rev. 2009;13:295–297. doi: 10.1016/j.smrv.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 91.Idir Y., Oudiette D., Arnulf I. Sleepwalking, Sleep Terrors, Sexsomnia and Other Disorders of Arousal: The Old and the New. J. Sleep Res. 2022;31:e13596. doi: 10.1111/jsr.13596. [DOI] [PubMed] [Google Scholar]
- 92.Zadra A., Desautels A., Petit D., Montplaisir J. Somnambulism: Clinical Aspects and Pathophysiological Hypotheses. Lancet Neurol. 2013;12:285–294. doi: 10.1016/S1474-4422(12)70322-8. [DOI] [PubMed] [Google Scholar]
- 93.Busby K.A., Mercier L., Pivik R.T. Ontogenetic Variations in Auditory Arousal Threshold during Sleep. Psychophysiology. 1994;31:182–188. doi: 10.1111/j.1469-8986.1994.tb01038.x. [DOI] [PubMed] [Google Scholar]
- 94.Plazzi G., Vetrugno R., Provini F., Montagna P. Sleepwalking and Other Ambulatory Behaviours during Sleep. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 2005;26((Suppl. S3)):s193–s198. doi: 10.1007/s10072-005-0486-6. [DOI] [PubMed] [Google Scholar]
- 95.Mahowald M.W., Schenck C.H. Insights from Studying Human Sleep Disorders. Nature. 2005;437:1279–1285. doi: 10.1038/nature04287. [DOI] [PubMed] [Google Scholar]
- 96.Guilleminault C., Palombini L., Pelayo R., Chervin R.D. Sleepwalking and Sleep Terrors in Prepubertal Children: What Triggers Them? Pediatrics. 2003;111:e17–e25. doi: 10.1542/peds.111.1.e17. [DOI] [PubMed] [Google Scholar]
- 97.Goodwin J.L., Kaemingk K.L., Fregosi R.F., Rosen G.M., Morgan W.J., Smith T., Quan S.F. Parasomnias and Sleep Disordered Breathing in Caucasian and Hispanic Children—The Tucson Children’s Assessment of Sleep Apnea Study. BMC Med. 2004;2:14. doi: 10.1186/1741-7015-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Petit D., Pennestri M.-H., Paquet J., Desautels A., Zadra A., Vitaro F., Tremblay R.E., Boivin M., Montplaisir J. Childhood Sleepwalking and Sleep Terrors: A Longitudinal Study of Prevalence and Familial Aggregation. JAMA Pediatr. 2015;169:653–658. doi: 10.1001/jamapediatrics.2015.127. [DOI] [PubMed] [Google Scholar]
- 99.Remulla A., Guilleminault C. Somnambulism (Sleepwalking) Expert Opin. Pharmacother. 2004;5:2069–2074. doi: 10.1517/14656566.5.10.2069. [DOI] [PubMed] [Google Scholar]
- 100.Lam S.-P., Fong S.Y.-Y., Yu M.W.-M., Li S.X., Wing Y.-K. Sleepwalking in Psychiatric Patients: Comparison of Childhood and Adult Onset. [(accessed on 19 March 2023)];Aust. N. Z. J. Psychiatry. 2009 43:426–430. doi: 10.1080/00048670902817703. Available online: https://journals.sagepub.com/doi/10.1080/00048670902817703. [DOI] [PubMed] [Google Scholar]
- 101.Guilleminault C., Kirisoglu C., da Rosa A.C., Lopes C., Chan A. Sleepwalking, a Disorder of NREM Sleep Instability. Sleep Med. 2006;7:163–170. doi: 10.1016/j.sleep.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 102.Masand P., Popli A.P., Weilburg J.B. Sleepwalking. Am. Fam. Physician. 1995;51:649–654. [PubMed] [Google Scholar]
- 103.Wills L., Garcia J. Parasomnias: Epidemiology and Management. CNS Drugs. 2002;16:803–810. doi: 10.2165/00023210-200216120-00002. [DOI] [PubMed] [Google Scholar]
- 104.Stallman H.M., Kohler M., White J. Medication Induced Sleepwalking: A Systematic Review. Sleep Med. Rev. 2018;37:105–113. doi: 10.1016/j.smrv.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 105.Stallman H.M., Kohler M. Prevalence of Sleepwalking: A Systematic Review and Meta-Analysis. PLoS ONE. 2016;11:e0164769. doi: 10.1371/journal.pone.0164769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tsai H.-C., Zhang F., Adamantidis A., Stuber G.D., Bonci A., de Lecea L., Deisseroth K. Phasic Firing in Dopaminergic Neurons Is Sufficient for Behavioral Conditioning. Science. 2009;324:1080–1084. doi: 10.1126/science.1168878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Schenck C.H., Mahowald M.W. REM Sleep Behavior Disorder: Clinical, Developmental, and Neuroscience Perspectives 16 Years After Its Formal Identification in SLEEP. Sleep. 2002;25:120–138. doi: 10.1093/sleep/25.2.120. [DOI] [PubMed] [Google Scholar]
- 108.Schenck C.H., Bundlie S.R., Ettinger M.G., Mahowald M.W. Chronic Behavioral Disorders of Human REM Sleep: A New Category of Parasomnia. Sleep. 1986;9:293–308. doi: 10.1093/sleep/9.2.293. [DOI] [PubMed] [Google Scholar]
- 109.Mahowald M.W., Schenck C.H. Dissociated States of Wakefulness and Sleep. Neurology. 1992;42:44–51; discussion 52. [PubMed] [Google Scholar]
- 110.Schenck C., Högl B., Videnovic A., editors. Rapid-Eye-Movement Sleep Behavior Disorder. Springer; Cham, Switzerland: 2019. [Google Scholar]
- 111.Cicero C.E., Giuliano L., Luna J., Zappia M., Preux P.-M., Nicoletti A. Prevalence of Idiopathic REM Behavior Disorder: A Systematic Review and Meta-Analysis. Sleep. 2021;44:zsaa294. doi: 10.1093/sleep/zsaa294. [DOI] [PubMed] [Google Scholar]
- 112.Galbiati A., Verga L., Giora E., Zucconi M., Ferini-Strambi L. The Risk of Neurodegeneration in REM Sleep Behavior Disorder: A Systematic Review and Meta-Analysis of Longitudinal Studies. Sleep Med. Rev. 2019;43:37–46. doi: 10.1016/j.smrv.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 113.Haba-Rubio J., Frauscher B., Marques-Vidal P., Toriel J., Tobback N., Andries D., Preisig M., Vollenweider P., Postuma R., Heinzer R. Prevalence and Determinants of Rapid Eye Movement Sleep Behavior Disorder in the General Population. Sleep. 2018;41:zsx197. doi: 10.1093/sleep/zsx197. [DOI] [PubMed] [Google Scholar]
- 114.Li X.S., Lam S.P., Zhang J., Wing Y.K. Instruments for Screening, Diagnosis and Assessment of RBD Severity and Monitoring Treatment Outcome. Springer International Publishing, Part of Springer Nature; Berlin/Heidelberg, Germany: 2018. [Google Scholar]
- 115.Mateo-Montero R.C., Pedrera-Mazarro A., Martín-Palomeque G., del Mar Moreno-Galera M., Valera-Dávila C., Gómez-Ansede A., Braun J., Jiménez-Escrig A. Clinical and Genetical Study of a Familial Form of REM Sleep Behavior Disorder. Clin. Neurol. Neurosurg. 2018;175:130–133. doi: 10.1016/j.clineuro.2018.09.035. [DOI] [PubMed] [Google Scholar]
- 116.Valencia Garcia S., Libourel P.-A., Lazarus M., Grassi D., Luppi P.-H., Fort P. Genetic Inactivation of Glutamate Neurons in the Rat Sublaterodorsal Tegmental Nucleus Recapitulates REM Sleep Behaviour Disorder. Brain J. Neurol. 2017;140:414–428. doi: 10.1093/brain/aww310. [DOI] [PubMed] [Google Scholar]
- 117.Valencia Garcia S., Brischoux F., Clément O., Libourel P.-A., Arthaud S., Lazarus M., Luppi P.-H., Fort P. Ventromedial Medulla Inhibitory Neuron Inactivation Induces REM Sleep without Atonia and REM Sleep Behavior Disorder. Nat. Commun. 2018;9:504. doi: 10.1038/s41467-017-02761-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Howell M., Avidan A.Y., Foldvary-Schaefer N., Malkani R.G., During E.H., Roland J.P., McCarter S.J., Zak R.S., Carandang G., Kazmi U., et al. Management of REM Sleep Behavior Disorder: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2022;19:769–810. doi: 10.5664/jcsm.10426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Irfan M., Howell M.J. Rapid Eye Movement Sleep Behavior Disorder: Overview and Current Perspective. Curr. Sleep Med. Rep. 2016;2:64–73. doi: 10.1007/s40675-016-0038-z. [DOI] [Google Scholar]
- 120.Hauri P.J., Silber M.H., Boeve B.F. The Treatment of Parasomnias with Hypnosis: A 5-Year Follow-up Study. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2007;3:369–373. doi: 10.5664/jcsm.26858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.McGrane I.R., Leung J.G., St. Louis E.K., Boeve B.F. Melatonin Therapy for REM Sleep Behavior Disorder: A Critical Review of Evidence. Sleep Med. 2015;16:19–26. doi: 10.1016/j.sleep.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Stefani A., Mozersky J., Kotagal V., Högl B., Ingravallo F., Ju Y.-E.S., Avidan A., Sharp R., Videnovic A., Schenck C.H., et al. Ethical Aspects of Prodromal Synucleinopathy Prognostic Counseling. Semin. Neurol. 2023;43:166–177. doi: 10.1055/a-2019-0245. [DOI] [PubMed] [Google Scholar]
- 123.Hammond D.C. A Review of the History of Hypnosis through the Late 19th Century. Am. J. Clin. Hypn. 2013;56:174–191. doi: 10.1080/00029157.2013.826172. [DOI] [PubMed] [Google Scholar]
- 124.Matthews W.J., Lankton S., Lankton C. Handbook of Clinical Hypnosis. American Psychological Association; Washington, DC, USA: 1993. An Ericksonian Model of Hypnotherapy; pp. 187–214. [Google Scholar]
- 125.Kirsch I., Lynn S.J., Rhue J.W. Handbook of Clinical Hypnosis. American Psychological Association; Washington, DC, USA: 1993. Introduction to Clinical Hypnosis; pp. 3–22. [Google Scholar]
- 126.Montgomery G.H., DuHamel K.N., Redd W.H. A Meta-Analysis of Hypnotically Induced Analgesia: How Effective Is Hypnosis? Int. J. Clin. Exp. Hypn. 2000;48:138–153. doi: 10.1080/00207140008410045. [DOI] [PubMed] [Google Scholar]
- 127.Evans F.J. Sleep and Hypnosis: Accessibility of Altered States of Consciousness. In: Adam G., Meszaros I., Banyai E.I., editors. Advances in Physiological Science. Elsevier; Amsterdam, The Netherlands: 1981. pp. 17–453. [Google Scholar]
- 128.Spiegel D., Cardeña E. Disintegrated Experience: The Dissociative Disorders Revisited. J. Abnorm. Psychol. 1991;100:366–378. doi: 10.1037/0021-843X.100.3.366. [DOI] [PubMed] [Google Scholar]
- 129.Windt J.M. The Immersive Spatiotemporal Hallucination Model of Dreaming. Phenomenol. Cogn. Sci. 2010;9:295–316. doi: 10.1007/s11097-010-9163-1. [DOI] [Google Scholar]
- 130.Kubie L.S., Margolin S. The Process of Hypnotism and the Nature of the Hypnotic State. Am. J. Psychiatry. 1944;100:611–622. doi: 10.1176/ajp.100.5.611. [DOI] [Google Scholar]
- 131.Malinowski J.E., Horton C.L. Metaphor and Hyperassociativity: The Imagination Mechanisms behind Emotion Assimilation in Sleep and Dreaming. Front. Psychol. 2015;6:1132. doi: 10.3389/fpsyg.2015.01132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kihlstrom J.F. Memory, Abuse, and Science. Am. Psychol. 1997;52:994–995. doi: 10.1037/0003-066X.52.9.994. [DOI] [Google Scholar]
- 133.Hobson J.A., Hoffman S.A., Helfand R., Kostner D. Dream Bizarreness and the Activation-Synthesis Hypothesis. Hum. Neurobiol. 1987;6:157–164. [PubMed] [Google Scholar]
- 134.Lifshitz M., Cusumano E.P., Raz A. Hypnosis as Neurophenomenology. Front. Hum. Neurosci. 2013;7:469. doi: 10.3389/fnhum.2013.00469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Chamine I., Atchley R., Oken B.S. Hypnosis Intervention Effects on Sleep Outcomes: A Systematic Review. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2018;14:271–283. doi: 10.5664/jcsm.6952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Murray-Jobsis J. Handbook of Clinical Hypnosis. American Psychological Association; Washington, DC, USA: 1993. The Borderline Patient and the Psychotic Patient; pp. 425–451. [Google Scholar]
- 137.Barrett D. The Hypnotic Dream: Its Relation to Nocturnal Dreams and Waking Fantasies. J. Abnorm. Psychol. 1979;88:584–591. doi: 10.1037/0021-843X.88.5.584. [DOI] [Google Scholar]
- 138.Zamore N., Barrett D. Hypnotic Susceptibility and Dream Characteristics. Psychiatr. J. Univ. Ott. 1989;14:572–574. [PubMed] [Google Scholar]
- 139.Redefining Hypnosis: Theory, Methods and Integration—Gruzelier—2000—Contemporary Hypnosis—Wiley Online Library. [(accessed on 20 March 2023)]. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1002/ch.193.
- 140.Landry M., Lifshitz M., Raz A. Brain Correlates of Hypnosis: A Systematic Review and Meta-Analytic Exploration. Neurosci. Biobehav. Rev. 2017;81:75–98. doi: 10.1016/j.neubiorev.2017.02.020. [DOI] [PubMed] [Google Scholar]
- 141.Vanhaudenhuyse A., Laureys S., Faymonville M.-E. Neurophysiology of Hypnosis. Neurophysiol. Clin. Clin. Neurophysiol. 2014;44:343–353. doi: 10.1016/j.neucli.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 142.Jensen M.P., Adachi T., Hakimian S. Brain Oscillations, Hypnosis, and Hypnotizability. Am. J. Clin. Hypn. 2015;57:230–253. doi: 10.1080/00029157.2014.976786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Terhune D.B., Cardeña E., Lindgren M. Differential Frontal-Parietal Phase Synchrony during Hypnosis as a Function of Hypnotic Suggestibility. Psychophysiology. 2011;48:1444–1447. doi: 10.1111/j.1469-8986.2011.01211.x. [DOI] [PubMed] [Google Scholar]
- 144.De Pascalis V. EEG Spectral Analysis during Hypnotic Induction, Hypnotic Dream and Age Regression. Int. J. Psychophysiol. Off. J. Int. Organ. Psychophysiol. 1993;15:153–166. doi: 10.1016/0167-8760(93)90073-X. [DOI] [PubMed] [Google Scholar]
- 145.Lendner J., Helfrich R. How Can I Run Sleep and Anesthesia Studies with Intracranial EEG? PsyArXiv. 2022 doi: 10.31234/osf.io/s65q4. [DOI] [Google Scholar]
- 146.Huang Z., Tarnal V., Vlisides P.E., Janke E.L., McKinney A.M., Picton P., Mashour G.A., Hudetz A.G. Asymmetric Neural Dynamics Characterize Loss and Recovery of Consciousness. NeuroImage. 2021;236:118042. doi: 10.1016/j.neuroimage.2021.118042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bonhomme V., Staquet C., Montupil J., Defresne A., Kirsch M., Martial C., Vanhaudenhuyse A., Chatelle C., Larroque S.K., Raimondo F., et al. General Anesthesia: A Probe to Explore Consciousness. Front. Syst. Neurosci. 2019;13:36. doi: 10.3389/fnsys.2019.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Klinzing J.G., Niethard N., Born J. Mechanisms of Systems Memory Consolidation during Sleep. Nat. Neurosci. 2019;22:1598–1610. doi: 10.1038/s41593-019-0467-3. [DOI] [PubMed] [Google Scholar]
- 149.Zhang H., Fell J., Axmacher N. Electrophysiological Mechanisms of Human Memory Consolidation. Nat. Commun. 2018;9:4103. doi: 10.1038/s41467-018-06553-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Banks M.I., Krause B.M., Endemann C.M., Campbell D.I., Kovach C.K., Dyken M.E., Kawasaki H., Nourski K.V. Cortical Functional Connectivity Indexes Arousal State during Sleep and Anesthesia. NeuroImage. 2020;211:116627. doi: 10.1016/j.neuroimage.2020.116627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zimmern V. Why Brain Criticality Is Clinically Relevant: A Scoping Review. Front. Neural Circuits. 2020;14:54. doi: 10.3389/fncir.2020.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Toker D., Pappas I., Lendner J.D., Frohlich J., Mateos D.M., Muthukumaraswamy S., Carhart-Harris R., Paff M., Vespa P.M., Monti M.M., et al. Consciousness Is Supported by Near-Critical Slow Cortical Electrodynamics. Proc. Natl. Acad. Sci. USA. 2022;119:e2024455119. doi: 10.1073/pnas.2024455119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Scheinin A., Kantonen O., Alkire M., Långsjö J., Kallionpää R.E., Kaisti K., Radek L., Johansson J., Sandman N., Nyman M., et al. Foundations of Human Consciousness: Imaging the Twilight Zone. J. Neurosci. Off. J. Soc. Neurosci. 2021;41:1769–1778. doi: 10.1523/JNEUROSCI.0775-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Domínguez-Clavé E., Soler J., Elices M., Pascual J.C., Álvarez E., de la Fuente Revenga M., Friedlander P., Feilding A., Riba J. Ayahuasca: Pharmacology, Neuroscience and Therapeutic Potential. Brain Res. Bull. 2016;126:89–101. doi: 10.1016/j.brainresbull.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 155.Reiff C.M., Richman E.E., Nemeroff C.B., Carpenter L.L., Widge A.S., Rodriguez C.I., Kalin N.H., McDonald W.M., The Work Group on Biomarkers and Novel Treatments. A Division of the American Psychiatric Association Council of Research Psychedelics and Psychedelic-Assisted Psychotherapy. Am. J. Psychiatry. 2020;177:391–410. doi: 10.1176/appi.ajp.2019.19010035. [DOI] [PubMed] [Google Scholar]
- 156.Palhano-Fontes F., Mota-Rolim S., Lobão-Soares B., Galvão-Coelho N., Maia-Oliveira J.P., Araújo D.B. Recent Evidence on the Antidepressant Effects of Ayahuasca. In: Labate B.C., Cavnar C., editors. Ayahuasca Healing and Science. Springer International Publishing; Cham, Switzerland: 2021. pp. 21–41. [Google Scholar]
- 157.Nichols D.E. Psychedelics. Pharmacol. Rev. 2016;68:264–355. doi: 10.1124/pr.115.011478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Vollenweider F.X., Preller K.H. Psychedelic Drugs: Neurobiology and Potential for Treatment of Psychiatric Disorders. Nat. Rev. Neurosci. 2020;21:611–624. doi: 10.1038/s41583-020-0367-2. [DOI] [PubMed] [Google Scholar]
- 159.Wießner I., Falchi M., Palhano-Fontes F., Feilding A., Ribeiro S., Tófoli L.F. LSD, Madness and Healing: Mystical Experiences as Possible Link between Psychosis Model and Therapy Model. Psychol. Med. 2023;53:1151–1165. doi: 10.1017/S0033291721002531. [DOI] [PubMed] [Google Scholar]
- 160.Kraehenmann R. Dreams and Psychedelics: Neurophenomenological Comparison and Therapeutic Implications. Curr. Neuropharmacol. 2017;15:1032–1042. doi: 10.2174/1573413713666170619092629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Friedrichs H., Passie T., Dierssen O. Die Psychologie des Meskalinrausches. VWB, Verl. für Wiss. und Bildung; Berlin, Germany: 2009. Bewusstsein, Kognition, Erleben. [Google Scholar]
- 162.Hobson J.A., Pace-Schott E.F., Stickgold R. Dreaming and the brain: Toward a cognitive neuroscience of conscious states. Behav. Brain Sci. 2000;23:793–842. doi: 10.1017/S0140525X00003976. [DOI] [PubMed] [Google Scholar]
- 163.Sanz C., Zamberlan F., Erowid E., Erowid F., Tagliazucchi E. The Experience Elicited by Hallucinogens Presents the Highest Similarity to Dreaming within a Large Database of Psychoactive Substance Reports. Front. Neurosci. 2018;12:7. doi: 10.3389/fnins.2018.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Millière R. Looking for the Self: Phenomenology, Neurophysiology and Philosophical Significance of Drug-Induced Ego Dissolution. Front. Hum. Neurosci. 2017;11:245. doi: 10.3389/fnhum.2017.00245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Mason L.I., Orme-Johnson D. Transcendental Consciousness Wakes up in Dreaming and Deep Sleep. Int. J. Dream Res. 2010;3:28–32. doi: 10.11588/IJODR.2010.1.595. [DOI] [Google Scholar]
- 166.Hobson J.A., Hong C.C.-H., Friston K.J. Virtual Reality and Consciousness Inference in Dreaming. Front. Psychol. 2014;5:1133. doi: 10.3389/fpsyg.2014.01133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Nielsen T., Levin R. Nightmares: A New Neurocognitive Model. Sleep Med. Rev. 2007;11:295–310. doi: 10.1016/j.smrv.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 168.van Elk M., Yaden D.B. Pharmacological, Neural, and Psychological Mechanisms Underlying Psychedelics: A Critical Review. Neurosci. Biobehav. Rev. 2022;140:104793. doi: 10.1016/j.neubiorev.2022.104793. [DOI] [PubMed] [Google Scholar]
- 169.Carhart-Harris R.L., Leech R., Williams T.M., Erritzoe D., Abbasi N., Bargiotas T., Hobden P., Sharp D.J., Evans J., Feilding A., et al. Implications for Psychedelic-Assisted Psychotherapy: Functional Magnetic Resonance Imaging Study with Psilocybin. Br. J. Psychiatry. 2012;200:238–244. doi: 10.1192/bjp.bp.111.103309. [DOI] [PubMed] [Google Scholar]
- 170.Wießner I., Olivieri R., Falchi M., Palhano-Fontes F., Oliveira Maia L., Feilding A., Araujo D.B., Ribeiro S., Tófoli L.F. LSD, Afterglow and Hangover: Increased Episodic Memory and Verbal Fluency, Decreased Cognitive Flexibility. Eur. Neuropsychopharmacol. 2022;58:7–19. doi: 10.1016/j.euroneuro.2022.01.114. [DOI] [PubMed] [Google Scholar]
- 171.Catlow B.J., Song S., Paredes D.A., Kirstein C.L., Sanchez-Ramos J. Effects of Psilocybin on Hippocampal Neurogenesis and Extinction of Trace Fear Conditioning. Exp. Brain Res. 2013;228:481–491. doi: 10.1007/s00221-013-3579-0. [DOI] [PubMed] [Google Scholar]
- 172.Zhang G., Ásgeirsdóttir H.N., Cohen S.J., Munchow A.H., Barrera M.P., Stackman R.W. Stimulation of Serotonin 2A Receptors Facilitates Consolidation and Extinction of Fear Memory in C57BL/6J Mice. Neuropharmacology. 2013;64:403–413. doi: 10.1016/j.neuropharm.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Barrett F.S., Carbonaro T.M., Hurwitz E., Johnson M.W., Griffiths R.R. Double-Blind Comparison of the Two Hallucinogens Psilocybin and Dextromethorphan: Effects on Cognition. Psychopharmacology. 2018;235:2915–2927. doi: 10.1007/s00213-018-4981-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wießner I., Falchi M., Palhano-Fontes F., Oliveira Maia L., Feilding A., Ribeiro S., Bezerra Mota N., Araujo D.B., Tófoli L.F. Low-Dose LSD and the Stream of Thought: Increased Discontinuity of Mind, Deep Thoughts and Abstract Flow. Psychopharmacology. 2022;239:1721–1733. doi: 10.1007/s00213-021-06006-3. [DOI] [PubMed] [Google Scholar]
- 175.Wießner I., Falchi M., Maia L.O., Daldegan-Bueno D., Palhano-Fontes F., Mason N.L., Ramaekers J.G., Gross M.E., Schooler J.W., Feilding A., et al. LSD and Creativity: Increased Novelty and Symbolic Thinking, Decreased Utility and Convergent Thinking. J. Psychopharmacol. 2022;36:348–359. doi: 10.1177/02698811211069113. [DOI] [PubMed] [Google Scholar]
- 176.Cai D.J., Mednick S.A., Harrison E.M., Kanady J.C., Mednick S.C. REM, Not Incubation, Improves Creativity by Priming Associative Networks. Proc. Natl. Acad. Sci. USA. 2009;106:10130–10134. doi: 10.1073/pnas.0900271106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Stickgold R., Scott L., Rittenhouse C., Hobson J.A. Sleep-Induced Changes in Associative Memory. J. Cogn. Neurosci. 1999;11:182–193. doi: 10.1162/089892999563319. [DOI] [PubMed] [Google Scholar]
- 178.Wagner U., Gais S., Haider H., Verleger R., Born J. Sleep Inspires Insight. Nature. 2004;427:352–355. doi: 10.1038/nature02223. [DOI] [PubMed] [Google Scholar]
- 179.Walker M.P., Liston C., Hobson J.A., Stickgold R. Cognitive Flexibility across the Sleep–Wake Cycle: REM-Sleep Enhancement of Anagram Problem Solving. Cogn. Brain Res. 2002;14:317–324. doi: 10.1016/S0926-6410(02)00134-9. [DOI] [PubMed] [Google Scholar]
- 180.Kraehenmann R., Pokorny D., Vollenweider L., Preller K.H., Pokorny T., Seifritz E., Vollenweider F.X. Dreamlike Effects of LSD on Waking Imagery in Humans Depend on Serotonin 2A Receptor Activation. Psychopharmacology. 2017;234:2031–2046. doi: 10.1007/s00213-017-4610-0. [DOI] [PubMed] [Google Scholar]
- 181.McGinty D.T. Serotonin and Sleep: Molecular, Functional, and Clinical Aspects. Sleep. 2009;32:699–700. doi: 10.1093/sleep/32.5.699. [DOI] [Google Scholar]
- 182.Dudysová D., Janků K., Šmotek M., Saifutdinova E., Kopřivová J., Bušková J., Mander B.A., Brunovský M., Zach P., Korčák J., et al. The Effects of Daytime Psilocybin Administration on Sleep: Implications for Antidepressant Action. Front. Pharmacol. 2020;11:602590. doi: 10.3389/fphar.2020.602590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Muzio J.N., Roffwarg H.P., Kaufman E. Alterations in the Nocturnal Sleep Cycle Resulting from LSD. Electroencephalogr. Clin. Neurophysiol. 1966;21:313–324. doi: 10.1016/0013-4694(66)90037-X. [DOI] [PubMed] [Google Scholar]
- 184.Carhart-Harris R.L., Muthukumaraswamy S., Roseman L., Kaelen M., Droog W., Murphy K., Tagliazucchi E., Schenberg E.E., Nest T., Orban C., et al. Neural Correlates of the LSD Experience Revealed by Multimodal Neuroimaging. Proc. Natl. Acad. Sci. USA. 2016;113:4853–4858. doi: 10.1073/pnas.1518377113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.de Araujo D.B., Ribeiro S., Cecchi G.A., Carvalho F.M., Sanchez T.A., Pinto J.P., de Martinis B.S., Crippa J.A., Hallak J.E.C., Santos A.C. Seeing with the Eyes Shut: Neural Basis of Enhanced Imagery Following Ayahuasca Ingestion. Hum. Brain Mapp. 2012;33:2550–2560. doi: 10.1002/hbm.21381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.dos Santos R.G., Osório F.L., Crippa J.A.S., Hallak J.E.C. Classical Hallucinogens and Neuroimaging: A Systematic Review of Human Studies. Neurosci. Biobehav. Rev. 2016;71:715–728. doi: 10.1016/j.neubiorev.2016.10.026. [DOI] [PubMed] [Google Scholar]
- 187.Buckner R.L., Andrews-Hanna J.R., Schacter D.L. The Brain’s Default Network: Anatomy, Function, and Relevance to Disease. Ann. N. Y. Acad. Sci. 2008;1124:1–38. doi: 10.1196/annals.1440.011. [DOI] [PubMed] [Google Scholar]
- 188.Desseilles M., Dang-Vu T.T., Sterpenich V., Schwartz S. Cognitive and Emotional Processes during Dreaming: A Neuroimaging View. Conscious. Cogn. 2011;20:998–1008. doi: 10.1016/j.concog.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 189.Vogt B.A., Laureys S. Posterior Cingulate, Precuneal and Retrosplenial Cortices: Cytology and Components of the Neural Network Correlates of Consciousness. Prog. Brain Res. 2005;150:205–217. doi: 10.1016/S0079-6123(05)50015-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Dolder P.C., Schmid Y., Müller F., Borgwardt S., Liechti M.E. LSD Acutely Impairs Fear Recognition and Enhances Emotional Empathy and Sociality. Neuropsychopharmacology. 2016;41:2638–2646. doi: 10.1038/npp.2016.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Kraehenmann R., Preller K.H., Scheidegger M., Pokorny T., Bosch O.G., Seifritz E., Vollenweider F.X. Psilocybin-Induced Decrease in Amygdala Reactivity Correlates with Enhanced Positive Mood in Healthy Volunteers. Biol. Psychiatry. 2015;78:572–581. doi: 10.1016/j.biopsych.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 192.Alonso J.F., Romero S., Mañanas M.À., Riba J. Serotonergic Psychedelics Temporarily Modify Information Transfer in Humans. Int. J. Neuropsychopharmacol. 2015;18:pyv039. doi: 10.1093/ijnp/pyv039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Muthukumaraswamy S.D., Carhart-Harris R.L., Moran R.J., Brookes M.J., Williams T.M., Errtizoe D., Sessa B., Papadopoulos A., Bolstridge M., Singh K.D., et al. Broadband Cortical Desynchronization Underlies the Human Psychedelic State. J. Neurosci. 2013;33:15171–15183. doi: 10.1523/JNEUROSCI.2063-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Tagliazucchi E., Carhart-Harris R., Leech R., Nutt D., Chialvo D.R. Enhanced Repertoire of Brain Dynamical States during the Psychedelic Experience: Enhanced Repertoire of Brain Dynamical States. Hum. Brain Mapp. 2014;35:5442–5456. doi: 10.1002/hbm.22562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Schenberg E.E., Alexandre J.F.M., Filev R., Cravo A.M., Sato J.R., Muthukumaraswamy S.D., Yonamine M., Waguespack M., Lomnicka I., Barker S.A., et al. Acute Biphasic Effects of Ayahuasca. PLoS ONE. 2015;10:e0137202. doi: 10.1371/journal.pone.0137202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Peters E., Golembiewski S., Erlacher D., Dresler M. Extending Mental Practice to Sleep: Enhancing Motor Skills through Lucid Dreaming. Med. Hypotheses. 2023;174:111066. doi: 10.1016/j.mehy.2023.111066. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This is a review article, thus there is no data to share.