Abstract
Young children’s mastery motivation and neurodevelopmental evaluation can contribute to overall early assessment for early intervention evaluation. At present, children born preterm (<37 weeks gestation) and with a low birth weight (LBW; <2500 g) are at increased risk of experiencing developmental delays and more nuanced cognitive and language challenges. The main objective of this exploratory study was to examine the connection between preterm children’s mastery motivation and their neurodevelopment, as well as to determine whether assessing mastery motivation can enhance assessment practices for early intervention (EI) programs. Parents of children born preterm completed the revised Dimensions of Mastery Motivation Questionnaire (DMQ18). Neurodevelopment was measured on the Bayley Scales of Infant and Toddler Development (BSID-III). Results revealed significant correlations between DMQ18 and BSID-III measures. Multivariate analysis showed that infants and toddlers born with a very low birth weight (VLBW; <1500 g) scored significantly lower on the infant DMQ18 and the BSID-III measures. Regression analyses revealed that birth weight and home environment were significant predictors of the children’s eligibility for EI programs. Infants’ social persistence with other children, gross motor persistence, and mastery pleasure, as well as toddlers’ objective cognitive persistence, social persistence with adults, gross motor persistence, mastery pleasure, and negative reaction to frustration, were important markers for evidenced-based practices in EI programs. This study demonstrates the utility of the DMQ18 as a contributory assessment measure and the importance of birth weight and home environment in predicting EI enrollment.
Keywords: infants, developmental assessment, early intervention, eligibility, toddlers, mastery motivation, neurodevelopmental status
1. Introduction
The survival rate of preterm infants increased worldwide in recent years, and their high rate of neurological problems has become a considerable concern for the general public health and human development professionals (Lugli et al. 2020). Medical experts and educators held the belief for a considerable period that low-birth-weight (LBW) or preterm infants who did not have significant cerebral damage would catch up with their peers in terms of development once they became medically stable (French 2017). However, several studies have demonstrated that these children are at a higher risk of developing conditions related to pervasive developmental disorders, experiencing developmental delays, and facing more complex language and cognitive challenges, including deficits in executive function (EF) (Aarnoudse-Moens et al. 2009; Barre et al. 2011; Blasco et al. 2020; Duvall et al. 2015; Guarini et al. 2009; Hutchinson et al. 2013; Lee et al. 2011). Saigal and Doyle (2008) found that most studies of infants with very low birth weight (VLBW, <1500 g) reported ongoing difficulties related to cognitive impairment and academic underachievement.
To help infants with LBW or VLBW overcome different kinds of developmental challenges, neonatal intensive care unit (NICU) follow-up clinics track early development, often up to 3 years of age. Other research has also suggested that preterm infants are more likely to require special education at school age than their full-term peers (De Jong et al. 2012; Griffiths et al. 2019; McGowan 2022). Furthermore, researchers have found later social–emotional difficulties that impact learning and lead to lifelong risks (Linsell et al. 2015; Scott et al. 2017). Therefore, it is necessary to identify preterm children’s developmental delays early and to connect families with necessary early intervention (EI) services (Vohr et al. 2004).
Educators and researchers (Green and Morgan 2017; Hashemi et al. 2017; Huang et al. 2022; Józsa et al. 2017; MacTurk et al. 1995; Morgan et al. 2017a; Wang et al. 2011) have used the revised Dimensions of Mastery Questionnaire (DMQ18) based on observations, structured challenging tasks, and rating scales to determine whether preterm children qualify for/require EI services. Mastery motivation is a powerful latent factor that encourages individuals to achieve their potential (Wang et al. 2011, 2017). Morgan et al. (1990) similarly defined mastery motivation as a strong driving force for individuals to master challenging tasks. Later, Barrett and Morgan (2018) redefined it as “the urge or psychological push to solve problems, meet challenges, and master ourselves and our world” (p. 4). Therefore, it is crucial to investigate the link between the mastery motivation of children who are at high risk of developmental delays and their neurodevelopmental status. In this study, we explore the correlation between mastery motivation and neurodevelopmental status among children at high risk of developmental delays and examine the potential advantages of assessing mastery motivation for EI programs specially designed for these children.
1.1. Role of Mastery Motivation for Preterm High-Risk Children
Mastery motivation has been defined as one of the most important aspects of a child’s development, and it is useful for his/her developmental evaluation process. It can stimulate a child’s attempts to master some kinds of difficulties challenging him/her (Green and Morgan 2017). The developmental construct of mastery motivation refers to a child’s ability to independently engage in goal-directed behavior by attempting to master a task that is at least moderately challenging (Morgan et al. 2017a; Borbélyová et al. 2019). Mastery motivation emerges in late infancy and is a major construct in understanding early cognitive and social attempts at problem solving (Keilty et al. 2015). It can readily be assessed in the developmental period (Kelley et al. 2000).
Mastery motivation is an individual’s driving force to overcome the problems they experience (Wang et al. 2020), and it is an important developmental concept to use in assessing children’s developmental factors (Green and Morgan 2017; Marcineková et al. 2020). Children with developmental delays have demonstrated lower levels of mastery motivation compared to children born full-term (Young and Hauser-Cram 2006). To help these children, mastery motivation has the predictive power of children’s developmental assessment (Józsa and Molnár 2013) and is supported by Wang et al. (2016) finding that mastery task persistence can predict both cognitive and fine motor skills in preterm high-risk children at 6 months of age. Task persistence and mastery pleasure are key components of mastery motivation. Therefore, we assume that mastery motivation assessment can predict preterm high-risk children’s educational development and eligibility for EI. According to Hashemi et al. (2017), preterm high-risk children’s persistence in facing challenges and compliance with their peers/caregivers shows the requirement for emotional self-regulation. Therefore, the role of mastery motivation, which can assess children’s persistence, is of considerable importance for developing and implementing early childhood developmental programs.
In a recent study conducted in Hungary, researchers examined a measure of mastery motivation using the DMQ18 (Borbélyová 2016; Morgan et al. 2020), a parent report questionnaire, and compared scores to traditional academic measures of math, reading, etc. Results for 327 school-age children (M = 5 years of age) showed that children’s negative reactions to failure/challenge as measured on the DMQ18 predicted multiple measures of school performance, over and above the role of child IQ and socioeconomic background. Mastery pleasure as measured on the scale predicted reading, and persistence in peer interaction predicted social skills in the primary grades. These findings demonstrate the importance of motivation and achievement-related emotions in school readiness and school success. Other researchers have found that the measurement of mastery motivation is a useful tool for children with known disabilities, such as cerebral palsy (CP) (Salavati et al. 2018). The authors concluded that the DMQ18 provided helpful findings with respect to different aspects of motivation in children with CP as defined by the parents’ perspectives; hence, the DMQ18 can be used as an intervention tool.
The studies described above highlight the importance of alternative assessments, including mastery motivation, for all populations of children but particularly for those at risk of developmental delay and those with disabilities. Including parent report measures is recommended for both practice and use of informed clinical opinion in eligibility determination to address additional areas of concern (Lucas and Shaw 2012). As such, assessment of the construct of mastery motivation becomes important and may become a useful part of the “toolbox” for EI referral and practice.
1.2. Role of Neurodevelopmental Skills for Preterm High-Risk Children
The first years of life from gestation onward represent a period of rapid brain growth and development with fluctuating growth spurts (Kvestad et al. 2022). Therefore, neurodevelopmental skills are very important and frequently assessed in young children with high-risk developmental delays (Jary et al. 2011). Regarding the neurodevelopmental skills of infants and toddlers, research has been conducted in clinical fields investigating multiple infants behaviors, such as visual processing, preferences, motor skills, affective processes, social/playful behaviors, and verbal or non-verbal cognitive skills (Galsworthy et al. 2000; Klein-Radukic and Zmyj 2023; Krogh and Væver 2019). Researchers who study the early development of the brain utilize advanced techniques such as magnetic resonance imaging (MRI) to identify and evaluate neurological outcomes for this group by detecting changes in the brain (Camerota et al. 2022; Miller et al. 2020).
Preterm children’s cognitive skills include their sensorimotor development, exploration and manipulation, object relatedness, memory, habituation, visual preference, object permanence, and other related aspects (Klein-Radukic and Zmyj 2023). Their language skills are composed of preverbal behaviors, vocabulary development, social referencing and verbal comprehension, preverbal communication, vocabulary development, and morphosyntactic development (Borrero et al. 2022). Their motor skills generally consist of motor planning, motor speed, perceptual–motor integration, functional hand skills, and motor skills, primarily in the limbs and torso, such as locomotion, coordination, balance, and motor planning (Bayley 2006).
There is currently a limited understanding of neurodevelopmental, social–emotional, and environmental (including socioeconomic and racial, ethnic, and health disparities) factors concerning children’s high risk of developmental delays and their consequences in the future (McLester-Davis et al. 2021). Therefore, the early identification of children at risk of neurodevelopmental disabilities may increase access to intervention, potentially improving the outcome (Kvestad et al. 2022). The WHO recognizes neurofunctional evaluation using the International Classification of Disability and Health as a valid developmental screening tool, which is gaining popularity for the assessment of development (World Health Organization 2007). For neurodevelopmental evaluation, the use of the Bayley Scales of Infant and Toddler Development—third version (BSID-III, now Bayley 4) is also widely accepted around the world (Hoskens et al. 2018). Researchers have used the BSID-III to evaluate neurodevelopment in preterm children for the purpose of EI qualification and intervention (Atkins et al. 2019; Borrero et al. 2022; Klein-Radukic and Zmyj 2023; Long et al. 2012; Perra et al. 2015).
1.3. Assessment of Children’s Mastery Motivation and Neurodevelopment
Concerning the assessment of preterm children’s mastery motivation, studies (Barrett et al. 2017; Busch-Rossnagel and Morgan 2013; Józsa and Molnár 2013; Morgan et al. 2017b) have suggested two means of assessment, i.e., the use of the DMQ18 and individualized challenging behavioral tasks. Several ways of assessing children’s mastery motivation have been implemented in studies (e.g., by observing the context of children’s free play; Jennings et al. 1988), such as the use of structured challenging tasks (Barrett et al. 2017; Józsa et al. 2017), the application of rating scales by parents or teachers (Hwang et al. 2017; Józsa and Molnár 2013; Morgan et al. 2017b), and the use of self-rating scales by children (Józsa and Morgan 2014, 2017; Józsa et al. 2014).
According to Morgan et al. (2020), the DMQ18 considers six factors of children’s mastery-related behaviors based on adults’ perceptions. Out of these six factors of the DMQ18, the first four factors are included to measure the instrumental context of children’s cognitive/object-oriented persistence, gross motor persistence, and social persistence with their peers or adults. The remaining two factors assess expressive aspects of mastery motivation, such as mastery pleasure and negative reactions to the failure of mastery motivation. Morgan et al. (2020) claimed that the DMQ18 can also measure children’s skills with respect to mastery tasks, such as general competence. Different versions of the DMQ18 are available because children of different ages face different levels of difficulty and challenges (Green and Morgan 2017).
The findings of one Italian study on neurodevelopmental skills (Gasparini et al. 2017) showed that Italian preterm infants’ performance level was significantly lower than that of their full-term peers, with the exception of their expressive language and gross motor subscales. In the investigation of the predictive value of the BSID-III with respect to the development of very preterm/very low-birth-weight children, one study (dos Santos et al. 2013) found that children’s motor scale scores on the Bayley scale had a moderate predictive value with respect to their later motor functions. Furthermore, the BSID-III is still widely used in follow-up clinics that serve as a primary referral source to EI (Blasco et al. 2020; Tang et al. 2012; Wang et al. 2017). It is also the most commonly applied method for assessment of children’s developmental aspects. The BSID-III measures five main factors of children’s developmental aspects, i.e., as cognitive, expressive language, receptive language, fine motor, and gross motor skills.
1.4. Predictions for Early Intervention (EI)
Multiple researchers have reported chronic underenrollment of children born LBW/preterm in EI programs in the United States (Atkins et al. 2017, 2019; Blasco et al. 2017; Hebbeler et al. 2007; Tang et al. 2012). Previous research indicates that preterm children who exhibit lower scores on developmental assessments and more severe medical indications, such as younger gestational ages and longer hospital stays in the NICU, are more likely to be enrolled in EI programs (Atkins et al. 2017; Litt and Perrin 2014; Tang et al. 2012). Age at testing and birth weight have also been found to be significant predictors of EI attendance (Blasco et al. 2017). Psychosocial factors (e.g., education level and income) also play a mediating role in the utilization of services such as EI (Hoffman et al. 2015).
The increasing number of preterm infants has created a trend of children who are at high risk for developmental delay and who would subsequently benefit from EI services, including speech therapy, physical therapy, and/or other types of services based on the child’s and family’s needs (Martin et al. 2018). Unfortunately, traditional standardized assessment measures often fall short of identifying cognitive and social delays in children born with LBW/preterm that could assist in EI qualification and enrollment (Blasco et al. 2017; Keilty et al. 2015). Spencer-Smith et al. (2015) found that cognitive and language scores on the BSID-III did not predict later impairments in these areas. Additionally, there has been significant concern that the corrected age on the BSID-III overestimates a child’s cognitive and developmental abilities (Acton et al. 2011), and it has been found to be a poor predictor of later academic performance (Anderson and Burnett 2017). Hence, it is crucial to evaluate how effective mastery motivation is in terms of contributing to the overall evaluation of young children who have experienced developmental delays.
1.5. Research Aims and Questions
The literature cited above demonstrates that some researchers used the DMQ18 only (e.g., Green and Morgan 2017; Hwang et al. 2017; Morgan et al. 2017b; Wang et al. 2011), and some researchers applied only BSID-III tests (e.g., Bayley 2006; Kvestad et al. 2022; Tang et al. 2012; Wang et al. 2017) for the assessment of children’s neurodevelopment. Therefore, it is necessary to assess the relationship between preterm children’s DMQ18 scale scores and their BSID-III test scores and to investigate differences between infants and toddlers among these two types of measurements.
Second, for young children at high risk of developmental delays, EI services are crucial for their developmental process. Therefore, it is also essential to investigate predictors (e.g., mastery motivation, other developmental processes, parents’ education level, and birth weight), which are important for identifying the early intervention engagement for these high-risk children.
Based on these aims, we plan to address the following research questions:
What is the relationship between preterm children’s (infants/toddlers’) DMQ18 scale scores and BSID-III scale scores based on LBW and VLBW?
What are the differences between preterm infants and toddlers born with LBW (<2500 g) or VLBW (<1500 g) in terms of their DMQ18 and BSID-III scores?
What are the predictors for the early intervention of young high-risk children with developmental delays?
2. Methods
2.1. Design and Procedure
In this study, we investigated preterm infants and toddlers aged between three months and three years old who were born with LBW and VLBW. These participants were seen in a high-risk infant follow-up clinic located in a major metropolitan area in the Pacific Northwest region of the United States. Children were included in the study if they were seen in the clinic between May 2015 and December 2018. Children with a known genetic disorder and/or previously diagnosed disabilities such as cerebral palsy attended another clinic. Demographic and medical information was obtained from a parent-completed clinical intake form, including gender, number of siblings, and home environment (single, two parents, relatives (e.g., grandmother)), as well as the qualification and attendance in early intervention.
Children completed a standardized infant/toddler developmental assessment (i.e., BSID-III), while parents completed a Likert questionnaire on mastery motivation (DMQ18). The DMQ18 was provided to parents in either English or Spanish, depending on the family’s preferred language. Hospital-qualified interpreters were used as part of routine clinical care when a child and/or family did not speak English as a first language. In this study, we utilized data from a larger clinical dataset approved by the organization’s Institutional Review Board. The study was completed in accordance with prevailing ethical standards. All private medical information (child and parent names and medical identification numbers) was removed prior to data analyses.
2.2. Participants
Children in the study (N = 233) ranged from a chronological age of 6.87 months to 39.03 months (M = 14, SD = 8.23) at the time of their assessment. The total sample was divided into an infant group (n = 178; M = 10.0 months) and a toddler group (N = 55; M = 26.7 months). Of those children, 209 had scores corrected for prematurity, as specified in the BSID-III administration manual (Bayley 2006; range five months to 23.9 months). The remaining children were over 24 months of age, so the BSID-III scores were based on chronological age. The gestational age for the sample ranged from 23.57 to 36.86 weeks (M = 32, SD 2.92). The average birth weight was 1666 g (range: 415 to 2470 g; SD: 498 g). We also categorized preterm children into two groups based on their birth weights: those with very low birth weight (VLBW), weighing < 1500 g (N = 133, M = 1006 g, SD = 278 g), and those with low birth weight (LBW), weighing > 1500 g and < 2500 g (N = 100, M = 2059 g, SD = 372 g). The groups of participants are also displayed within Table 1 for enhanced visibility. Over half (57%) of the children were male. Type of insurance (public vs. private) was used as a proxy for socioeconomic status; over half (52%) of the sample had public insurance (n = 113). Of the 219 participants that provided a response to a question regarding EI, 75 (34%) were receiving EI support at the time of their appointment. For additional demographic information, please refer to Table 2.
Table 1.
Number of participants in groups.
| Group | Very Low Birth Weight | Low Birth Weight | Total |
|---|---|---|---|
| Infants | 95 | 83 | 178 |
| Toddlers | 38 | 17 | 55 |
| Total | 133 | 100 | 233 |
2.3. Measures
2.3.1. Revised Dimensions of Mastery Questionnaire (DMQ18)
The revised DMQ18 has been used worldwide to assess mastery motivation (Morgan et al. 2017b). The current DMQ18 was revised in the fall of 2014 and is available in English, Chinese, Hungarian, and Spanish (Morgan et al. 2020). The revised DMQ18 has three age-based versions (infant—6 to 18 months, preschool age—19 months to 5 years, and school-age—over 5 years) (Green and Morgan 2017). For this study, the infant version of the revised DMQ18 was used for infants, and the preschool version was used for toddlers. Of the sample, 89.5% completed the English revised DMQ18, and 10.5% completed a revised Spanish DMQ18. We used the revised DMQ18 to ask a parent and/or teacher to rate their perception of the child’s behavior from 1 (“not at all like this child”) to 5 (“exactly like this child”).
The revised DMQ18 infant version comprises thirty-eight items that measure seven dimensions of mastery motivation: (1) cognitive/object persistence (6 items), (2) gross motor persistence (5 items), (3) social persistence with adults (6 items), (4) social persistence with children (6 items), (5) mastery pleasure (5 items), (6) negative reactions to challenge—frustration/anger (5 items), and (7) general competence (5 items).
Table 2.
Demographic information (N = 233).
| Variable | N | Percent |
|---|---|---|
| Sex | ||
| Male | 132 | 56.7 |
| Female | 101 | 43.3 |
| Race/ethnicity * (N = 181) | ||
| Caucasian | 116 | 64.1 |
| African American | 7 | 3.9 |
| American Indian | 1 | 0.6 |
| Native Hawaiian or Pacific Islander | 4 | 2.2 |
| Asian American | 12 | 6.6 |
| Hispanic | 27 | 14.9 |
| Multiple ethnicities | 14 | 7.7 |
| Mother’s education * (N = 198) | ||
| Some high school | 23 | 11.6 |
| High school graduate | 43 | 21.7 |
| Some college | 49 | 24.7 |
| College graduate | 51 | 25.8 |
| Post college | 32 | 16.2 |
| Father’s education * (N = 190) | ||
| Some high school | 37 | 19.5 |
| High school graduate | 36 | 18.9 |
| Some college | 51 | 26.8 |
| College graduate | 47 | 24.7 |
| Post college | 19 | 10.0 |
| Insurance (N = 216) | ||
| Public | 113 | 52.3 |
| Private | 103 | 47.7 |
| Language (N = 233) | ||
| English | 198 | 86.5 |
| Spanish | 24 | 10.5 |
| Other | 7 | 3.0 |
* Note: Percentages are based on valid responses. Information on demographic variables is missing for some respondents.
The revised DMQ18 toddler (preschool) version, and (7) general competence measures the seven dimensions of mastery motivation listed above. However, as toddlers can describe sadness or shame, we divided the dimension of negative reaction to challenge—frustration/anger into two parts: negative reaction to frustration—anger and negative reaction to frustration–sadness/shame, creating eight total domains in the 39-item toddler version: (1) cognitive/object persistence (5 items), (2) gross motor persistence (5 items), (3) social persistence with adults (5 items), (4) social persistence with children (6 items), (5) mastery pleasure (5 items), (6) negative reaction to frustration—anger (4 items), (7) negative reaction to frustration—sadness/shame (4 items), and (8) general competence (5 items). Table 3 provides an example of DMQ18 items for both the infant and toddler versions.
Table 3.
Sample DMQ18 questions for each dimension rated by a parent.
| Dimension | Infant | Toddler |
|---|---|---|
| Cognitive/object persistence | “Repeats a new skill until he or she can do it.” | “Works for a long time trying to do something challenging.” |
| Gross motor persistence | “Tries to do well in physical activities even when they are difficult.” | “Tries to do well in physical actives even when they are challenging.” |
| Social persistence with adults | “Tries to influence play with me or other adults.” | “Tries hard to get adults to understand him or her.” |
| Social persistence with children | “Tries to make other children feel better if they cry or seem sad.” | “Tries to say and do things that keep other kids interested.” |
| Mastery pleasure | “Claps hands or shows excitement when he or she is successful.” | “Gets excited when he or she figures something out.” |
| Negative reaction to challenge—frustration/anger | “Gets frustrated when not successful immediately.” | N/A |
| Negative reaction—frustration/anger | N/A | “Gets frustrated when not able to complete a challenging task.” |
| Negative reaction—sadness/shame | N/A | “Looks away when tries but cannot do something.” |
| General competence | “Does things that are difficult for children his or her age.” | “Does things that are difficult for children his or her age.” |
2.3.2. Bayley Scales of Infant and Toddler Development-III
The BSID-III is a norm-referenced tool that measures cognitive, expressive language, receptive language, fine motor, and gross motor skills for children between the ages of 16 days and 42 months (Bayley 2006). The scale provides composite scores with a mean of 100 and a standard deviation of 15 for the cognitive, language, and motor scales. Scaled scores for the cognitive, receptive, and expressive language, as well as the fine and gross motor subtests, have a mean of 10 and a standard deviation of 3.
2.3.3. Assessment for the Qualification of Early Intervention Enrollment
We applied one dichotomous item (“Yes” or “No”) to assess whether preterm children are qualified to enroll in an EI program.
3. Results
3.1. Reliability, Validity, and Homogeneity Measures of Instruments
For the internal consistency reliability of instruments, we analyzed the scale reliability using Cronbach’s alpha. The DMQ18 measures of both infant and toddler versions (r = 0.81 and r = 0.83) were acceptable to address our research questions (Morgan et al. 2020). The means and standard deviation of the infant version of the DMQ were 3.39 and 0.73, respectively, while for toddlers, they were 4.24 and 0.12, respectively. The infant version of the DMQ follows a normal distribution, as evidenced by the acceptable values of skewness (−0.59) and kurtosis (−0.38). Similarly, the toddler version also conforms to a normal distribution, with a skewness value of −0.84 and a kurtosis value of −0.22. For the BSID-III measures of assessing children’s mastery tasks, the internal consistency reliability values of the infant and toddler versions are 0.89 and 0.88, respectively (see Table 4). The mean, standard deviation, skewness, and kurtosis of the infant version of the BSID-III measure are 8.59, 2.51, 0.30, and 0.36, respectively, demonstrating that the test follows a normal distribution. Similarly, the toddler version of the BSID-III measure also exhibits acceptable values for the mean (8.11), standard deviation (2.47), skewness (0.19), and kurtosis (0.55), indicating that the test is in accordance with a normal distribution.
Table 4.
Reliability measures (Cronbach’s alpha) of instruments.
| Instrument | Number of Domains | Version (Cronbach’s Alpha) | Total (Cronbach’s Alpha) | ||
|---|---|---|---|---|---|
| Infants | Toddlers | Infants | Toddlers | ||
| DMQ18 | 7 | 8 | 0.81 | 0.83 | 0.83 |
| BSID-III | 5 | 5 | 0.89 | 0.88 | 0.89 |
Investigating the instrument (DMQ18) developers’ studies (Józsa and Barrett 2018; Józsa and Morgan 2014; Józsa et al. 2014, 2019; Morgan et al. 2017a, 1990, 2020), it was found that the DMQ18 instrument was reliable and valid according to test–retest reliability and parallel-forms reliability measures. The test–retest reliability of the DMQ18 rated by parents varied between r = 0.70 and r = 0.97, and parallel-forms reliability ranged between 0.72 and 0.87. In terms of content validity, the DMQ18 had a strong foundation (starting in the 1980s), with different versions implemented in some studies (Jennings et al. 1988; Morgan et al. 1990). Infant and toddler versions have been translated and validated in five different languages: Hungarian, Turkish, Chinese, Spanish, and Persian (Shaoli et al. 2019). In order to determine the content validity when administered in different languages, some studies have already validated the DMQ18 English version with experts input (e.g., using the Bangla version by Shaoli et al. 2019), applying the Indonesian version by Rahmawati et al. (2020), and using the Swahili version on Kenyan preschool children by Amukune et al. (2021). The experts consulted in these studies also approved the content validity of the DMQ18. In this study, we also proved the criterion validity of the DMQ18 in terms of concurrent evidence and predictive evidence. For concurrent evidence, our DMQ18 versions are closely related to the standardized test (BSID-III) of children’s developmental scales, which can be used as a criterion for testing children’s behavioral mastery tasks (Huang and Lo 2019). Huang and Lo’s (2019) study showed that children’s DMQ18 social persistence, total persistence, and total mastery motivation were significantly and positively related (rs = 0.25–0.27, ps < .05) to the global motivation scales of young children. For predictive evidence, the DMQ18 was used to examine the effectiveness of mobility intervention in a randomized control for preterm children with developmental delays (Huang et al. 2022).
With respect to the reliability of the BSID-III, we investigated the test developers’ studies (Bayley 1949, 2006, 2014) through split-half and test–retest stability measures. The split-half reliability coefficients for all subtests and scales ranged from 0.71 to 0.98, whereas the test–retest stability coefficients varied between 0.80 and 0.87. The validity of the BSID-III test was also investigated through a series of studies (Bayley 1949, 2006, 2014; Krogh and Væver 2019) focusing on the intercorrelations between the subtests, the factor structure of the test, correlation with other measures, and special group studies. These studies provided insights, showing that the subtests of the BSID-III were correlated with one another and that the hypothesized models fit the data best. Moreover, the test correlations were also consistent, as expected. It was also confirmed that the BSID-III test was valid as a way to differentiate healthy children from those at high risk (Bayley 2006).
3.2. DMQ18 Homogeneity Measures for Both Infants and Toddlers
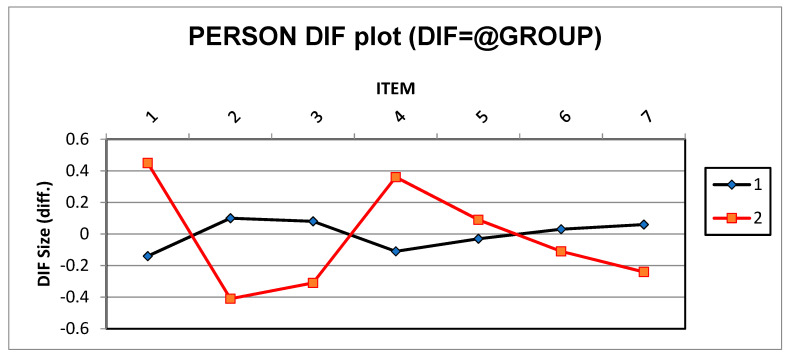
Differential item functioning (DIF) analysis was conducted to check whether there were item biases based in the versions (infant or toddler) of the DMQ18. DIF analysis suggested participant responses based on the version for each item of measuring children’s mastery motivation (Oo et al. 2023a). Categorization of DIF analysis results into three categories was recommended by Oo et al. (2023a), namely negligible, slight to moderate (DIF ≥ 0.43 logits), and moderate to large (DIF ≥ 0.64 logits). DIF analysis (see Figure 1) showed that none of the items from either version had biased measures (DIF = 0.45 logits). DIF logits in the toddler version were slightly higher than the recommended values (Oo et al. 2023b), possibly because the toddler version included two more factors, i.e., negative reactions—frustration/anger and negative reactions—sadness/shame.
Figure 1.
Differential item functioning for both infant and toddler versions of the DMQ18. Note: 1 (infant version), 2 (toddler version).
The normality of the DMQ18 measures was also confirmed between both infant and toddler versions. As a result, the overall skewness values of the infant and toddler versions were −1.99 and 2.32, and their overall kurtosis scores were −0.04 and −0.02, respectively (consistent with Kline’s (2011) recommendation for violation values of Sk > 0.3 for skewness and K > 0.10 for kurtosis). These values suggest that all variables were relatively normally distributed. Based on the above results, we confirmed that our instruments were homogeneous for both infant and toddler versions, making them suitable to address our research questions.
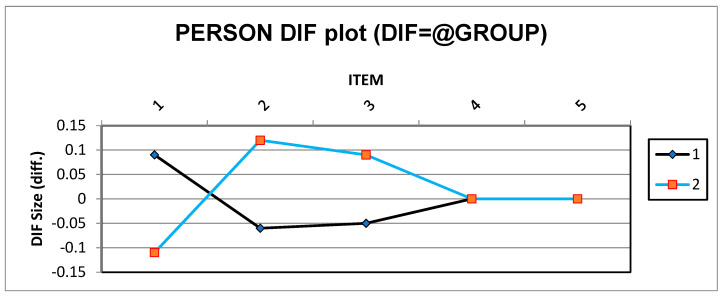
3.3. BSID-III Homogeneity Measures for Both Infants and Toddlers
Figure 2 shows the acceptable logit numbers of the infant and toddler versions (DIF logits between −0.15 and 0.15) of the BSID-III measurement (Oo et al. 2023b). Therefore, we can assume that there are no biased measures in either the infants or toddler version of the BSID-III. The normality measures of skewness and kurtosis were 1.66 and 0.19 for the infant version, and 0.03, and 0.05 for the toddler version, respectively. Therefore, we can say that both BSID-III tests were homogenous and normal, making them suitable to measure preterm children’s mastery motivation (based on individualized behavioral tasks).
Figure 2.
Differential item functioning for both infant and toddler versions of the BSID-III. Note: 1 (infant version), 2 (toddler version).
3.4. Addressing RQ1
All statistical data were analyzed using SPSS software. We used correlations to examine the relationships between the Bayley-III and the DMQ18. Multivariate tests were used to compare children born with VLBW and those born with LBW. For the infant group, there were relatively few significant correlations (14%; Table 5). DMQ18 gross motor persistence and general competence were significantly related to the BSID-III gross motor scale. DMQ18 general competence and negative reaction to challenge—frustration/anger were significantly related to the BSID-III fine motor scale. Finally, DMQ18 social persistence with children was significantly related to the BSID-III cognitive scale.
Table 5.
Correlations between infants’ DMQ18 scale scores and BSID-III scaled scores.
| Measure | Cognitive | Receptive Language |
Expressive Language |
Fine Motor | Gross Motor |
|---|---|---|---|---|---|
| Cognitive/object persistence | 0.036 | −0.091 | 0.030 | −0.009 | 0.045 |
| Social persistence with adults | 0.076 | −0.065 | 0.002 | 0.005 | −0.007 |
| Social persistence with children | 0.153 * | 0.021 | −0.030 | 0.017 | 0.003 |
| Gross motor persistence | 0.049 | 0.045 | 0.115 | 0.085 | 0.188 * |
| Mastery pleasure | 0.115 | −0.060 | 0.043 | 0.008 | 0.075 |
| Negative reactions to challenge—frustration/anger | −0.002 | −0.105 | −0.088 | −0.151 * | −0.113 |
| General competence | 0.126 | 0.052 | 0.104 | 0.232 ** | 0.201 ** |
** Correlation is significant at the 0.01 level (two-tailed); * correlation is significant at the 0.05 level (two-tailed).
Among the toddler groups, there was an increased number of significant correlations (33%; Table 6). Specifically, DMQ18 cognitive/object persistence, gross motor persistence, negative reaction—sadness/shame, and general competence were significantly related to the BSID-III receptive language scale. DMQ18 cognitive persistence/object persistence, mastery pleasure, and general competence were significantly related to the BSID-III expressive language scale. Over half of the DMQ18 scales (i.e., cognitive/object persistence, gross motor persistence, mastery pleasure, negative reaction—sadness/shame, and general competence) were significantly related to the BSID-III cognitive scale.
Table 6.
Correlations between toddlers’ DMQ18 scaled scores and BSID-III scaled scores.
| Measures | Cognitive | Receptive Language |
Expressive Language |
Fine Motor | Gross Motor |
|---|---|---|---|---|---|
| Cognitive/object persistence | 0.419 ** | 0.529 ** | 0.330 * | 0.222 | 0.339 * |
| Social persistence with adults | 0.177 | 0.250 | 0.261 | 0.074 | 0.177 |
| Social persistence with children | 0.204 | 0.211 | 0.080 | 0.253 | 0.121 |
| Gross motor persistence | 0.342 * | 0.412 ** | 0.201 | 0.242 | 0.228 |
| Mastery pleasure | 0.365 ** | 0.236 | 0.323 * | 0.139 | 0.098 |
| Negative reaction—frustration/anger | 0.204 | 0.113 | 0.035 | −0.051 | 0.179 |
| Negative reaction—sadness/shame | 0.377 * | 0.363 * | 0.252 | 0.265 | 0.167 |
| General competence | 0.420 ** | 0.469 ** | 0.330 * | 0.241 | 0.277 |
** Correlation is significant at the 0.01 level (two-tailed); * correlation is significant at the 0.05 level (two-tailed).
3.5. Addressing RQ2
To address this research question, multivariate analysis was used to assess whether there were overall differences between LBW and VLBW infants on the DMQ18 scales; this test was statistically significant (F (7, 167) = 2.38, p = .024), with a medium to large effect size (η2 = 0.091) according to Cohen (1988). Follow-up univariate ANOVAs indicated that infants born with VLBW scored significantly higher (showed more frustration/anger) on negative reaction to challenge—frustration/anger, with a medium effect size. Infants born with VLBW scored significantly higher on the DMQ18 negative reaction than item than infants born with LBW (Table 7).
Table 7.
Differences between infants born with LBW and VLBW on the DMQ18 scales.
| Measure | df | F | p | η2 |
|---|---|---|---|---|
| Multivariate test | 7.167 | 2.381 | 0.024 | 0.091 |
| Cognitive/object persistence | 1.173 | 0.309 | 0.579 | 0.002 |
| Social persistence with adults | 1.173 | 0.451 | 0.503 | 0.003 |
| Social persistence with children | 1.173 | 1.223 | 0.270 | 0.007 |
| Gross motor persistence | 1.173 | 0.764 | 0.383 | 0.004 |
| Mastery pleasure | 1.173 | 0.193 | 0.661 | 0.001 |
| Negative reaction to challenge—frustration/anger | 1.173 | 13.323 | ≤0.001 | 0.072 |
| General competence | 1.173 | 0.270 | 0.604 | 0.002 |
Note: n = 175.
A subsequent multivariate analysis was used to assess differences on BSID-III scales between infants born with LBW and VLBW, which were found to be statistically significant (F (5, 171) = 5.28, p < .001), with a large to medium effect size (η2 = 0.134). Follow-up univariate ANOVAs indicated that infants born with VLBW scored statistically significantly lower on the BSID-III cognitive, receptive language, fine motor, and gross motor scales, with small to medium-sized effects (Table 8). There was not a significant difference found between infants born with LBW and VLBW on the BSID-III expressive language scale.
Table 8.
Differences between infants born with LBW and VLBW on the BSID-III scales.
| Measure | df | F | p | η2 |
|---|---|---|---|---|
| Multivariate test | 5.171 | 5.275 | ≤0.001 | 0.134 |
| Cognitive | 1.175 | 6.269 | 0.013 | 0.035 |
| Receptive language | 1.175 | 13.652 | ≤0.001 | 0.072 |
| Expressive language | 1.175 | 2.490 | 0.116 | 0.014 |
| Fine motor | 1.175 | 19.288 | ≤0.001 | 0.099 |
| Gross motor | 1.175 | 8.642 | 0.004 | 0.047 |
Note: n = 177.
Infants born with VLBW scored significantly lower on the BSID-III cognitive, receptive language, fine motor, and gross motor items than infants born with LBW.
We conducted the same multivariate analysis to assess whether there were differences between toddlers born with LBW and VLBW on the BSID-III scores; this test was statistically significant (F (5, 40) = 2.71, p = .034, η2 = 0.253), with a large effect size. Follow-up univariate ANOVAs indicated that toddlers born with VLBW scored statistically and significantly lower on the cognitive, expressive language, and fine motor BSID-III scales (Table 9), with medium to large effect sizes for the significant ANOVAs. There were no significant differences found between toddlers born with LBW and VLBW on the BSID-III receptive language and gross motor scales. A subsequent multivariate analysis was used to assess differences on DMQ18 scales for toddlers born with LBW and VLBW; this test was not statistically significant (F (8, 39) = 1.77, p = .11). Therefore, univariate F values are not reported.
Table 9.
Differences between toddlers born with LBW and VLBW on the BSID-III.
| df | F | p | η2 | |
|---|---|---|---|---|
| Multivariate test | 5.40 | 2.708 | 0.034 | 0.253 |
| BSID-III scales | ||||
| Cognitive | 1.44 | 7.930 | 0.007 | 0.153 |
| Receptive language | 1.44 | 3.163 | 0.082 | 0.067 |
| Expressive language | 1.44 | 7.125 | 0.011 | 0.139 |
| Fine motor | 1.44 | 11.809 | 0.001 | 0.212 |
| Gross motor | 1.44 | 2.036 | 0.161 | 0.044 |
Note: n = 46.
Toddlers born with VLBW scored significantly lower on the BSID-III cognitive, expressive language, and fine motor scales than toddlers born with LBW.
3.6. Addressing RQ3
Binary logistic regression was conducted to examine whether five predictor variables, i.e., birth weight, number of siblings, mother’s education, father’s education, and home living environment (mother only, father only, mother and father, other relatives, two mothers, and other), significantly predicted whether or not preterm children would enroll in EI. When all five variables were considered together, they significantly predicted whether or not the preterm children would enroll in EI (χ2 = 8.125, df = 5, N = 233, p < 0.05). Table 10 presents the odds ratios (Exp(β)), which suggest that the odds of correctly estimating who will enroll in EI improve by 40% if one knows preterm children’s birth weight and by 36% if one knows children’s home environmental status (i.e., mother only, father only, mother and father, other relatives, two mothers, or other).
Table 10.
Logistic regression predicting who will enroll in early intervention (N = 233).
| Variable. | β | SE | Wald | p | Exp(β), Odds Ratio |
|---|---|---|---|---|---|
| Birth weight | 0.20 | 0.09 | 5.06 | 0.018 * | 1.40 |
| Number of siblings | 0.94 | 0.12 | 0.61 | 0.434 | 1.10 |
| Mother’s education | −0.08 | 0.08 | 1.06 | 0.304 | 0.92 |
| Father’s education | 0.01 | 0.08 | 0.02 | 0.895 | 1.01 |
| Home environment | 0.30 | 0.14 | 4.49 | 0.034 * | 1.36 |
Note: * p < .05
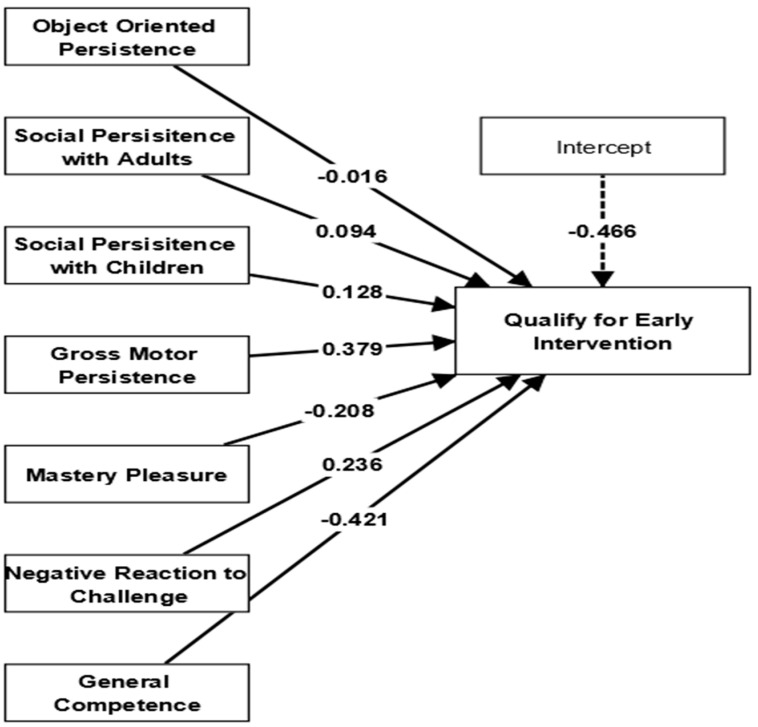
In addition to examining the predictors mentioned earlier, we also assessed the effectiveness of evaluating mastery motivation to determine whether preterm children are eligible for EI programs. As a result, we fitted the logistic regression model using SmartPLS software to develop models of association that can forecast the factors that impact preterm children’s mastery motivation in relation to their suitability for enrollment in EI programs. In this logistic regression analysis, the outcome variable was the qualification for EI (represented on a binary scale), while the predictor variables included ‘object-oriented persistence, social persistence with adults, social persistence with children, gross motor persistence, mastery pleasure, negative reaction to challenge, and general competence’. The logistic regression model was set up with a two-tailed test, a significance level of .05, a maximum of 1000 iterations, and a stop criterion of 10−5 (accurate). Subsequently, the calculations were initiated. Findings showed that the mastery motivation of infants with respect to their eligibility for EI had a good fit for the accurate interpretation, as evidenced by lower values of the Akaike information criterion (AIC = 248.40) and Bayesian information criterion (BIC = 251.58), as well as Nagelkerke’s R-square value of 0.46. Consequently, the study results suggest that a child’s social persistence with other children (β = 0.128, SE = 0.309, * p < .05), gross motor persistence (β = 0.379, SE = 0.201, * p < .05), and negative reaction to challenge (β = 0.236, SE = 0.332, * p < .05) are significant factors in determining their eligibility for early intervention programs (as shown in Figure 3).
Figure 3.
Impacts of infants’ mastery motivation on early intervention qualification.
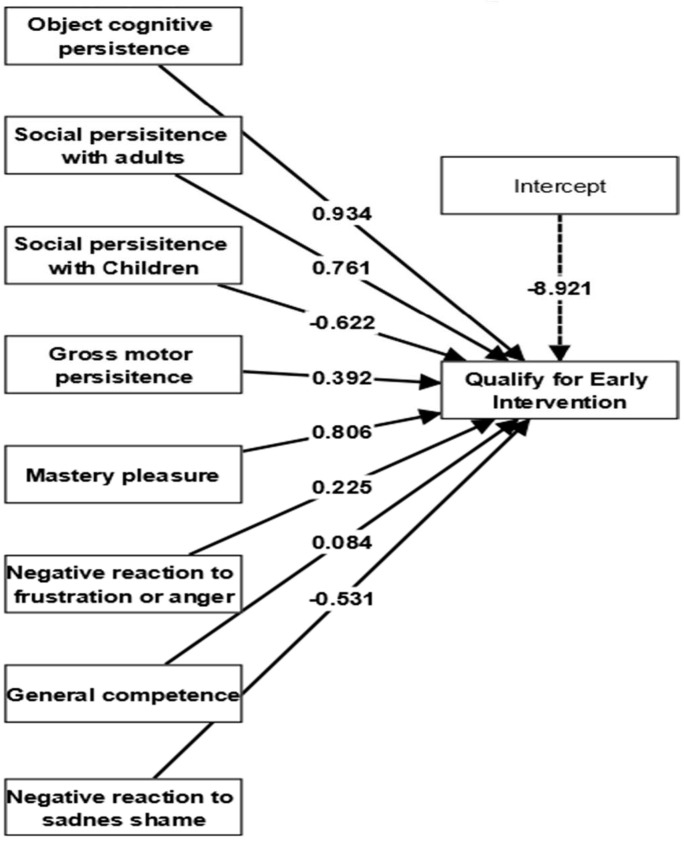
The effectiveness of toddlers’ mastery motivation in determining their eligibility for EI enrollment was also examined. In this logistic regression model for toddlers’ mastery motivation, EI qualification (serving as the dependent variable) was influenced by eight predictor variables: object cognitive persistence, social persistence with adults, social persistence with children, gross motor persistence, mastery pleasure, negative reaction to frustration or anger, negative reaction to sadness or shame, and mastery motivation. Similar to the above description, the logistic regression model was established with a two-tailed test, a significance level of .05, a maximum of 1000 iterations, and a stop criterion of 10−5 (accurate). Subsequently, the calculations were initiated. The logistic regression model showed a good fit, as indicated by the lower values of AIC (248.40) and BIC (251.39), as well as Nagelkerke’s R-square value of 0.55. The study results suggest that toddlers’ objective cognitive persistence (β = 0.934), social persistence with adults (β = 0.761, SE = 0.441, * p < .05), gross motor persistence (β = 0.392, SE = 0.375, * p < .05), mastery pleasure (β = 0.806, SE = 0.334, * p < .05), and negative reaction to frustration/anger (β = 0.225, SE = 0.582, * p < .05) had significant impacts on predicting for their EI enrollment qualification (as depicted in Figure 4).
Figure 4.
Impacts of toddlers’ mastery motivation on early intervention qualification.
4. Discussion
Our study measured infants’ and toddlers’ mastery motivation and neurodevelopment in order to identify young children at high risk of developmental delays. We applied two main types of measurement (e.g., the DMQ18 and BSID-III) to investigate the relationships between infants’ and toddlers’ mastery motivation and neurodevelopment, as well as differences between infants and toddlers born with LBW (<2500 g) and VLBW (<1500 g) on the DMQ18 and BSID-III scores. Different variables from children’s background information (e.g., birth weight, number of siblings, father’s education, mother’s education, and home environment) were also measured to determine which variables predicted their EI enrollment. Before addressing our research questions, first, we confirmed the reliability, validity, and homogeneity measures of our instruments. Internal consistency, reliability, skewness, kurtosis measures, and Rasch analyses proved that our instruments were reliable and homogeneous, making them suitable to address our research questions.
We found significant relationships between the DMQ18 and BSID-III; results revealed that the DMQ18 contributed meaningfully to the overall assessment of infants and toddlers. It is not surprising that DMQ18 general competence was significantly related to both BSID-III gross and fine motor skills at the infant level, as motor items are often most pertinent to infant developmental assessments. Likewise, at the toddler age, DMQ18 cognitive/object persistence and general competence were significantly related to BSID-III cognitive, expressive, and receptive language subscales. This may be the result of a toddler’s increased opportunity to demonstrate skills to their parents, as well as greater item density on the BSID-III, particularly for cognitive and motor skills at the toddler age. Wang et al. (2016) similarly found significant correlations between cognitive/object persistence ratings on the DMQ18 for toddlers who were developmentally delayed. These correlations demonstrate the relevance of parents’ reports in contributing to an overall view of a child’s ability and to provide support, including the DMQ18 in an EI “toolbox”, as it can reliably be used with children who have developmental delay and children born with LBW/preterm.
In this study, we also found a significant negative correlation between infant scores on the DMQ18 negative reaction to challenge–frustration/anger and the BSID-III fine motor scale. This is not surprising, as an infant who is competent with fine motor tasks is less likely to become frustrated when he/she is not immediately successful. Indeed, these fine motor abilities are some of the earliest persistent abilities demonstrated in developmental assessments (Barger et al. 2018). Negative reaction to challenge—frustration/anger is important, as it has been shown to be predictive of later emotional and cognitive development (Józsa and Barrett 2018). Niccols et al. (2003) proposed a bidirectional relationship between motivation and competence; if the child is more successful in attempts, he/she is more motivated to try, which makes sense, given the present findings. Therefore, interventionists should assist parents, care providers, and specialists who interact with infants and toddlers at increased risk of developmental disabilities to facilitate an early mastery of motivational skills. These findings have worldwide implications for EI, given previous international studies and successful translations of the DMQ18 (Liao et al. 2021).
Multivariate analyses of score differences revealed that infants born with VLBW scored lower than their peers with heavier birth weights on both the DMQ18 negative reaction to challenge—frustration/anger and all scales of the BSID-III except the expressive language subscale. This finding is not surprising, as there is low item density for expressive language on the BSID-III, especially during the infant years (Blasco et al. 2020). The mean age of infants included in this study was 10 months. In contrast, the expressive language subscale was significant for toddlers, which indicates that, similar to previous research, children born with VLBW are more likely to have trouble with emotional regulation, which can lead to lifelong struggles and at-risk behavior. In one study (Zablotsky et al. 2019), it was also found that there were significant differences in developmental delay for boys, children with birth weight ≥2500 g, children living in urban areas, and those with less-educated mothers. In the toddler group, although significant relationships were found between the DMQ18 and the BSID-III scales, there were no differences based on birth weight on the parents’ DMQ18 report. This finding may indicate that parents rated their children similarly despite their birth weight. This was the only incongruence between the parent report and the BSID-III, as children born with VLBW were rated lower on the BSID-III.
In terms of predictive modeling for EI enrollment, our regression model indicated that the enrollment for both infants and toddlers was predicted by the combined factors of birth weight, number of siblings, father’s education, mother’s education, and children’s home environment. Among these combined factors, preterm children’s birth weight and their home environment were found to be significant predictors of early intervention enrollment. Since our study has highlighted the significance of the family environment, we can support families through early intervention partnerships with infant/toddler mental health and social work partners. These results are in line with those reported in other studies (Atkins et al. 2017; Blasco et al. 2017; Litt and Perrin 2014; Tang et al. 2012) indicating that the lower the birth weight, the more likely the infant will be enrolled in EI services. Barger et al. (2018) also found birth weight to be a very common prevalent category predicting EI eligibility, used in 19 states in the United States. Wang et al.’s (2011) study also showed that the home living environment had moderate relationships with toddlers’ mastery motivation. Furthermore, parental support and toy responsiveness are crucially important for toddlers’ mastery motivation and EI engagement (Banerjee and Tamis-LeMonda 2007). Parental scaffolding of early mastery attempts has also been shown to promote a child’s persistence and later competence at school age (Prendergast and MacPhee 2018).
Finally, our study investigated whether infants’ and toddlers’ mastery motivation could contribute to the battery of assessments for EI enrollment. It was found that both infants’ and toddlers’ mastery motivation had a significant predictive effect on their EI engagement. Specifically, infants’ social persistence with other children, gross motor persistence, and mastery pleasure, as well as toddlers’ objective cognitive persistence, social persistence with adults, gross motor persistence, mastery pleasure, and negative reaction to frustration/anger, are significant factors that seem to influence eligibility for early intervention programs. This means that preterm children’s mastery motivation assessment by the DMQ18 is of considerable importance in predicting their EI enrollment. Our study results are line with those of a previous study (Huang et al. 2022) that suggested the importance of parents’ role and that mastery motivation of toddlers is necessary for EI programs. In our study, we found that the traditional standardized BSID-III assessment measures were not able to predict the enrollment of preterm children in EI programs. As a result, we excluded these insignificant findings and instead focused on the significant results obtained from the prediction values using mastery motivation measured by the DMQ18, along with five other predictor variables: birth weight, number of siblings, mother’s education, father’s education, and home living environment. Our findings also suggest that the traditional standardized assessment BSID-III measures cannot predict preterm children’s EI enrollment (Blasco et al. 2017; Keilty et al. 2015) in isolation. The findings of our study revealed that both children’s birthweight and the quality of their home environment emerged as significant predictors for their enrollment in EI programs. The factors influencing the prediction effects on EI enrollment may also be influenced by additional predictor variables. In contrast to the findings of previous researchers (Atkins et al. 2017, 2019; Blasco et al. 2017; Hebbeler et al. 2007; Tang et al. 2012) that demonstrated underenrollment of children born with low birthweight (LBW) in EI programs in the United States, our study yielded different results in terms of predicting the impact of birthweight on EI enrollment.
5. Limitations
In the present study, we utilized parent report data for the DMQ18 measure, which may include response bias. However, researchers using the DMQ18 reinforce the importance of parental reports and indicate that parents may be more accurate reporters of their child’s cognitive and social persistence than traditional measures, such as the BSID-III (Wang et al. 2011). Indeed, parent reports have been found to match well with behavioral developmental outcome measures at the toddler age (Wang et al. 2011). In our study, we used two language versions of the DMQ18 (English and Spanish), which may raise some cultural differences. However, both versions were previously translated into English and Spanish and were content-validated (Shaoli et al. 2019). Despite these limitations, this study included an assessment of the historically studied population, which provides useful information on our current DMQ18 and BSID-III measures in predicting EI enrollment. Our main emphasis was on children receiving medical care at the clinic, and we did not include data from the broader population of healthy children. Consequently, we acknowledge that excluding healthy children may have introduced sample bias, which could have potentially inflated the correlation between the two variables of the DMQ18 and BSID-III measures.
Another limitation may be that at the time of BSID-III testing, a majority (90%) of the sample was corrected for prematurity in accordance with administration guidelines, which may have contributed to a lack of significant differences. This may be particularly true for the BSID-III at the infant age (Blasco et al. 2017). There have been long-standing concerns that the BSID-III provides higher-than-anticipated scores when correcting for prematurity (Anderson et al. 2010; Duncan et al. 2015; Hack et al. 2005). In a later study, Blasco et al. (2020) found no differences in BSID-III scores for 6-month-olds born with LBW and between preterm and full-term peers. However, differences were noted in DMQ18 cognitive and social persistence.
Finally, although we found significant differences in EI enrollment based on the home environment, it should be noted that this factor was based on who was living in the home at the time of the assessments, and it does not measure the home environment in terms of the quality of child materials and/or parent–child interaction in the home setting. This study could have been enhanced by including a measure of parent–child interaction or observation in the home environment with our EI partners. This would help us capture health disparities related to racial, ethnic, and cultural differences.
6. Conclusions
Our study shows that measurement of mastery motivation and neurodevelopment was crucial for identifying young children at high risk of developmental delays. It also highlights the importance of mastery motivation as a predictor for EI programs. Thus, mastery motivation is an important developmental factor in young children and should be evaluated and promoted in early education, given its predictive nature for preacademic and academic skills (Józsa and Barrett 2018). The DMQ18 could be considered as part of early childhood and early intervention authentic assessment as a key component of a comprehensive evaluation that includes parent and provider observations and informed clinical opinion. Team members should consider goal-directed behavior and social persistence, core skills of mastery motivation, as critical skills to address during early intervention (Keilty et al. 2015). Mastery motivation remains an overlooked construct that is critical for the development of young children. This is particularly true for children who are at high risk of developmental delay and who ideally receive developmental assessments early in life to assist in appropriate planning and interventions.
In conclusion, the DMQ18, a parent report, contributes meaningfully to the overall assessment of young children. Some significant correlations were also found among DMQ18 and BSID-III scaled scores (e.g., DMQ18 gross motor persistence and general competence were significantly related to the BSID-III gross motor scale) in the infant version. In the toddler version, DMQ18 cognitive persistence/object persistence, mastery pleasure, and general competence were significantly related to the BSID-III expressive language scale. Investigating the differences in mastery motivation among infants and toddlers, it was found that infants born with VLBW scored significantly higher than toddlers (showed more frustration/anger) on negative reaction to challenge—frustration/anger, with a medium effect size. No significant differences were observed between toddlers born with LBW and VLBW on the BSID-III receptive language and gross motor scales.
Author Contributions
Conceptualization, P.B.; Methodology, P.B. and K.J.; Formal analysis, K.J., T.Z.O. and S.A.; Investigation, P.B., S.S. and L.M.G.; Data curation, P.B., S.S. and L.M.G.; Writing—original draft, P.B., K.J. and T.Z.O.; Writing—review and editing, K.J., T.Z.O. and S.A.; Supervision, P.B.; Project administration, P.B.; Funding acquisition, K.J. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by Oregon Health & Science University, USA (IRB Office Approval Code: IRB00006326, Approval Date: 6 October 2022).
Informed Consent Statement
OHSU IRB waiver of authorization.
Data Availability Statement
This research is based on human participants, and thus data availability is impossible due to their privacy.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This study was funded by the Scientific Foundations of Education Research Program of the Hungarian Academy of Sciences and by the ICT and Societal Challenges Competence Centre of the Humanities and Social Sciences Cluster of the Centre of Excellence for Interdisciplinary Research, Development and Innovation of the University of Szeged. The authors are members of the New Tools and Techniques for Assessing Students Research Group.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- Aarnoudse-Moens Cornelieke Sandrine Hanan, Weisglas-Kuperus Nynke, Goudoever Johannes Bernard Van, Oosterlaan Jaap. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics. 2009;124:717–28. doi: 10.1542/peds.2008-2816. [DOI] [PubMed] [Google Scholar]
- Acton Bryan V., Biggs Wayne S. G., Creighton Dianne E., Penner Karen A. H., Switzer Heather N., Thomas Julianne H. Petrie, Joffe Ari R., Robertson Charlene M. T. Overestimating neuro-development using the Bayley-III after early complex cardiac surgery. Pediatrics. 2011;128:e794–e800. doi: 10.1542/peds.2011-0331. [DOI] [PubMed] [Google Scholar]
- Amukune Stephen, Calchei Marcela, Józsa Krisztián. Swahili version of the Dimensions of Mastery Questionnaire: Adaptation and Psychometric Properties. Electronic Journal of Research in Educational Psychology. 2021;19:625–50. doi: 10.25115/ejrep.v19i55.3910. [DOI] [Google Scholar]
- Anderson Peter J., Burnett Alice. Assessing developmental delay in early childhood—Concerns with the Bayley-III scales. Clinical Neuropsychologist. 2017;31:371–81. doi: 10.1080/13854046.2016.1216518. [DOI] [PubMed] [Google Scholar]
- Anderson Peter J., DeLuca Cinzia, Hutchinson R. Esther, Roberts Gehan, Doyle Lex. Underestimation of developmental delay by the new Bayley-III Scale. Archives of Pediatrics and Adolescent Medicine. 2010;164:352–56. doi: 10.1001/archpediatrics.2010.20. [DOI] [PubMed] [Google Scholar]
- Atkins Kristi L., Dolata Jill K., Blasco Patricia M., Saxton Sage N., Duvall Susanne W. Early Intervention Referral Outcomes for Children at Increased Risk of Experiencing Developmental Delays. Maternal Child Health Journal. 2019;24:204–12. doi: 10.1007/s10995-019-02830-4. [DOI] [PubMed] [Google Scholar]
- Atkins Kristi L., Duvall Susanne W., Dolata Jill K., Blasco Patricia M., Saxton Sage N. Part C early intervention enrollment in low birth weight infants at-risk for developmental delays. Maternal Child Health Journal. 2017;21:290–96. doi: 10.1007/s10995-016-2113-y. [DOI] [PubMed] [Google Scholar]
- Banerjee Poonam Nina, Tamis-LeMonda Catherine S. Infants’ persistence and mothers’ teaching as predictors of toddlers’ cognitive development. Infant Behavior and Development. 2007;30:479–91. doi: 10.1016/j.infbeh.2006.12.001. [DOI] [PubMed] [Google Scholar]
- Barger Brain, Rice Catherine, Wolf Rebecca, Roach Andrew. Better together: Developmental screening and monitoring best identify children who need early intervention. Disability and Health Journal. 2018;11:420–26. doi: 10.1016/j.dhjo.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barre Natalie, Morgan Angela, Doyle Lex W., Anderson Peter J. Language abilities in children who were very preterm and/or very low birth weight: A meta-analysis. Journal of Pediatrics. 2011;158:766–74. doi: 10.1016/j.jpeds.2010.10.032. [DOI] [PubMed] [Google Scholar]
- Barrett Karen Caplovitz, Morgan George A. Mastery motivation: Retrospect, present, and future directions. Advances in motivation science. In: Elliot Andrew., editor. Advances in Motivation Science. Elsevier; Amsterdam: 2018. pp. 2–39. [DOI] [Google Scholar]
- Barrett Karen Caplovitz, Józsa Krisztián, Morgan George A. New computer-based mastery motivation and executive function tasks for school readiness and school success in 3 to 8 year-old children. Hungarian Educational Research Journal. 2017;7:86–105. [Google Scholar]
- Bayley N. Consistency and variability in the growth of intelligence from birth to eighteen years. The Pedagogical Seminary and Journal of Genetic Psychology. 1949;75:165–96. doi: 10.1080/08856559.1949.10533516. [DOI] [PubMed] [Google Scholar]
- Bayley N. Bayley Scales of Infant and Toddler Development: Administration Manual. Harcourt Assessment; San Antonio: 2006. [Google Scholar]
- Bayley N. Bayley-III Bayley Scales of Infant Development. Deutsche Fassung: Manual zur Durchführung und Auswertung der Bayley-III Skalen. 3rd ed. Pearson; Frankfurt am Main: 2014. [Google Scholar]
- Blasco Patricia M., Acar Serra, Guy Sybille, Saxton Sage, Duvall Susanne, Morgan George. Executive function in infants and toddlers born low birth weight and preterm. Journal of Early Intervention. 2020;42:321–37. doi: 10.1177/1053815120921946. [DOI] [Google Scholar]
- Blasco Patricia M., Guy Serra, Saxton Sage N, Duvall Susanne W. Are we missing a vulnerable population in early intervention? Infants and Young Children. 2017;30:190–203. doi: 10.1097/IYC.0000000000000097. [DOI] [Google Scholar]
- Borbélyová D. Adaptation to the School Environment in Early Elementary Education. [(accessed on 6 October 2022)];Paidagogos. 2016 2:206–28. Available online: https://www.paidagogos.net/issues/2016/2/article.php?id=13. [Google Scholar]
- Borbélyová Diana, Slezáková Tatiana, Tirpáková Anna, Kurucová Zuzana. Using an adaptation programme to introduce children to the early years of schooling in Slovakia. Education 3–13: International Journal of Primary, Elementary and Early Years Education. 2019;47:730–45. doi: 10.1080/03004279.2018.1531045. [DOI] [Google Scholar]
- Borrero Martha Cristo, Trujillo Tammy Goretty, Sanchez Carolina, Salazar Andrea, Cárdenas María Paula, Charpak Nathalie. Bayley-III and Griffiths-II scales performance in a cohort of premature infants followed in Colombia. Early Human Development. 2022;173:105660. doi: 10.1016/j.earlhumdev.2022.105660. [DOI] [PubMed] [Google Scholar]
- Busch-Rossnagel Nancy A., Morgan George A. Introduction to the mastery motivation and self-regulation section. In: Barrett Karen Caplovitz, Fox Nathan A., Morgan George A., Fidler Deborah J., Daunhauer Lisa A., editors. Handbook of Self-Regulatory Processes in Development: New Directions and International Perspectives. Psychology Press; New York: 2013. pp. 247–64. [Google Scholar]
- Camerota Maire, Wylie Amanda C., Goldblum Jessica, Wideman Laurie, Cheatham Carol L., Propper Cathi B. Testing a cascade model linking prenatal inflammation to child executive function. Behavioural Brain Research. 2022;431:113959. doi: 10.1016/j.bbr.2022.113959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Lawrence Erlbaum Associates, Publishers; Hillsdale: 1988. [Google Scholar]
- De Jong Marjanneke, Verhoeven Marjolein, Baar Anneloes van. School outcome, cognitive functioning, and behaviour problems in moderate and late preterm children and adults: A review. Seminars in Fetal and Neonatal Medicine. 2012;17:163–69. doi: 10.1016/j.siny.2012.02.003. [DOI] [PubMed] [Google Scholar]
- dos Santos Elsa S. Luttikhuizen, Kieviet Jorrit F. de, Königs Marsh, Elburg Ruurd M. van, Oosterlaan Jaap. Predictive value of the Bayley Scales of Infant Development on development of very preterm/very low birth weight children: A meta-analysis. Early Human Development. 2013;89:487–96. doi: 10.1016/j.earlhumdev.2013.03.008. [DOI] [PubMed] [Google Scholar]
- Duncan Andrea F., Bann Carla, Boatman Cathy, Hintz Susan, Vaucher Yvonne, Vohr Betty, Yolton Kimberly, Heyne Roy. Do currently recommended Bayley-III cutoffs overestimate motor impairment in infants born <27 weeks gestation? Journal of Perinatology. 2015;35:516–21. doi: 10.1038/jp.2014.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duvall Sussanne W., Erickson Sarah J., MacLean Peggy, Lowe Jean R. Perinatal medical variables predict executive function within a sample of preschoolers born very low birth weight. Journal of Child Neurology. 2015;30:735–40. doi: 10.1177/0883073814542945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French K. B. Care of extremely small premature infants in the neonatal intensive care unit: A parent’s perspective. Clinical Perinatology. 2017;44:275–82. doi: 10.1016/j.clp.2017.01.008. [DOI] [PubMed] [Google Scholar]
- Galsworthy Michael J., Dionne Ginette, Dale Philip S, Plomin Robert. Sex differences in early verbal and non-verbal cognitive development. Developmental Science. 2000;3:206–15. doi: 10.1111/1467-7687.00114. [DOI] [Google Scholar]
- Gasparini Corinna, Caravale Barbara, Rea Monica, Coletti Maria Franca, Tonchei Valentina, Bucci Salvia, Dotta Andrea, Curtis Mario De, Gentile Simonneta, Ferri Rosa. Neuro-developmental outcome of Italian preterm children at 1 year of corrected age by Bayley-III scales: An assessment using local norms. Early Human Development. 2017;113:1–6. doi: 10.1016/j.earlhumdev.2017.06.007. [DOI] [PubMed] [Google Scholar]
- Green Sheridan, Morgan George A. Patterns of mastery task behavior in early school-age children in the United States. Hungarian Educational Rsearch Journal. 2017;7:142–57. [Google Scholar]
- Griffiths Nadine, Spence Kaye, Loughran-Fowlds Alison, Westrup Bjorn. Individualised developmental care for babies and parents in the NICU: Evidence-based best practice guideline recommendations. Early Human Development. 2019;139:104840. doi: 10.1016/j.earlhumdev.2019.104840. [DOI] [PubMed] [Google Scholar]
- Guarini Annalisa, Sansavini Alessandra, Fabbri Cristina, Alessandroni Rosina, Faldella Giacomo, Karmiloff-Smith Annette. Reconsidering the impact of preterm birth on language outcome. Early Human Development. 2009;85:639–45. doi: 10.1016/j.earlhumdev.2009.08.061. [DOI] [PubMed] [Google Scholar]
- Hack Maureen, Taylor H. Gerry, Drotar Dennis, Schluchter Mark, Cartar Lydia, Wilson-Costello Deanne, Klein Nancy, Friedman Harriet, Mercuri-Minich Nori, Morrow Mary. Poor Predictive Validity of the Bayley Scales of Infant Development for Cognitive Function of Extremely Low Birth Weight Children at School Age. Pediatrics. 2005;116:333–41. doi: 10.1542/peds.2005-0173. [DOI] [PubMed] [Google Scholar]
- Hashemi Ezzat, Ariza Jeanelle, Rogers Haille, Noctor Stephen C., Martínez-Cerdeño Verónica. The Number of Parvalbumin-Expressing Interneurons Is Decreased in the Prefrontal Cortex in Autism. Cerebral Cortex. 2017;27:1931–43. doi: 10.1093/cercor/bhw021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebbeler Kathleen, Spiker Donna, Scarborough Anita, Mallik Sangeeta, Simeonsson Rune, Singer Marnie, Nelson Lauren. National Early Intervention Longitudinal Study (NEILS) Final Report. SRI International; Menlo Park: 2007. [Google Scholar]
- Hoffman Laurie, Bann Carla, Higgins Rosemary, Vohr Betty. Developmental outcomes of extremely preterm infants born to adolescent mothers. Pediatrics. 2015;135:1082–92. doi: 10.1542/peds.2014-3880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoskens Jasmine, Klingels Katrijn, Smits-Engelsman Bouwein. Validity and cross-cultural differences of the Bayley Scales of Infant and Toddler Development, Third Edition in typically developing infants. Early Human Development. 2018;125:17–25. doi: 10.1016/j.earlhumdev.2018.07.002. [DOI] [PubMed] [Google Scholar]
- Huang Su-Ying, Lo Hu-Fung. Unpublished Analyses of Reliability of the Preschool DMQ 18 and Correlations with WPPSI-IV IQ. Fu Jen Catholic University; Taipei: 2019. Unpublished Manuscript. [Google Scholar]
- Huang Su-Ying, Chang Ching-Yin, Wang Pei-Jung, Tang Su-Chin. Characteristics of mastery motivation and its relationship with parenting stress in toddlers with language delay. Acta Psychologica. 2022;230:103769. doi: 10.1016/j.actpsy.2022.103769. [DOI] [PubMed] [Google Scholar]
- Hutchinson Esther, Luca Cinzia De, Doyle Lex, Roberts Gehan, Anderson Peterson J. School-age outcomes of extremely preterm or extremely low birth weight children. Pediatrics. 2013;131:1053–61. doi: 10.1542/peds.2012-2311. [DOI] [PubMed] [Google Scholar]
- Hwang Ai-Wen, Wang Jun, Józsa Krisztián, Wang Pei-Jang, Liao Hua-Fang, Morgan George A. Cross cultural invariance and comparisons of Hungarian-, Chinese-, and English-speaking preschool children leading to the revised Dimensions of Mastery Questionnaire (DMQ 18) Hungarian Educational Research Journal. 2017;7:32–47. [Google Scholar]
- Jary Sally, Kmita Grazyna, Whitelaw Andrew. Differentiating developmental outcome between infants with severe disability in research studies: The role of Bayley developmental quotients. Journal of Pediatrics. 2011;159:211–14. doi: 10.1016/j.jpeds.2011.01.037. [DOI] [PubMed] [Google Scholar]
- Jennings Kay Donahue, Connors Robin E., Stegman And Charles E. Does a physical handicap alter the development of mastery motivation during the preschool years? Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:312–17. doi: 10.1097/00004583-198805000-00008. [DOI] [PubMed] [Google Scholar]
- Józsa Krisztián, Molnár Éva D. The relationship between mastery motivation, self-regulated learning and school success: A Hungarian and European perspective. In: Barrett Karen Caplovitz, Fox Nathan A., Morgan George A., Fidler Debora J., Daunhauer Lisa A., editors. Handbook on Self-Regulatory Processes in Development: New Directions and International Perspectives. Psychology Press; New York: 2013. pp. 265–304. [DOI] [Google Scholar]
- Józsa Krisztián, Morgan George A. Developmental changes in cognitive persistence and academic achievement between grade 4 and grade 8. European Journal of Psychology of Education. 2014;29:521–35. doi: 10.1007/s10212-014-0211-z. [DOI] [Google Scholar]
- Józsa Krisztián, Morgan George A. Reversed items in Likert scales: Filtering out invalid responders. Journal of Psychological and Educational Research. 2017;25:7–25. [Google Scholar]
- Józsa Krisztian, Barrett Karen Caplovitz. Affective and social mastery motivation in preschool as predictors of early school success: A longitudinal study. Early Childhood Research Quarterly. 2018;45:81–92. doi: 10.1016/j.ecresq.2018.05.007. [DOI] [Google Scholar]
- Józsa Krisztián, Wang Jun, Barrett Karen Caplovitz, Morgan George A. Age and cultural differences in self-perceptions of mastery motivation and competence in American, Chinese, and Hungarian school age Children. Child Development Research. 2014;2014:803061. doi: 10.1155/2014/803061. [DOI] [Google Scholar]
- Józsa Krisztián, Barrett Karen Caplovitz, Józsa Gabriella, Kis Noémi, Morgan George A. Development and initial evaluation of an individualized moderately challenging computer-tablet mastery motivation measure for 3–8 year-olds. Hungarian Educational Research Journal. 2017;7:106–26. [Google Scholar]
- Józsa Krisztián, Kis Noémi, Barrett Karen Caplovitz. Mastery motivation, parenting, and school achievement among Hungarian adolescents. European Journal of Psychology of Education. 2019;34:317–39. doi: 10.1007/s10212-018-0395-8. [DOI] [Google Scholar]
- Keilty Bonnie, Blasco Patricia M., Acar Serra. Re-Conceptualizing developmental areas of assessment for screening, eligibility determination and program planning in early intervention. Journal of Intellectual Disability—Diagnosis and Treatment. 2015;3:218–29. doi: 10.6000/2292-2598.2015.03.04.8. [DOI] [Google Scholar]
- Kelley Sue A., Brownnell Celia A., Campbell Susan B. Mastery motivation and self-evaluative affect and father’s: Longitudinal relations with maternal behavior. Child Development. 2000;71:1061–71. doi: 10.1111/1467-8624.00209. [DOI] [PubMed] [Google Scholar]
- Klein-Radukic Sarah, Zmyj Norbert. The predictive value of the cognitive scale of the Bayley Scales of Infant and Toddler Development-III. Cognitive Development. 2023:65. doi: 10.1016/j.cogdev.2022.101291. [DOI] [Google Scholar]
- Kline R. B. Principles and Practice ofStructural Equation Modeling. 3rd ed. Guilford Press; New York: 2011. [Google Scholar]
- Krogh Marianne T, Væver Mette S. Does gender affect Bayley-III scores and test-taking behavior? Infant Behavior and Development. 2019;57:101352. doi: 10.1016/j.infbeh.2019.101352. [DOI] [PubMed] [Google Scholar]
- Kvestad Ingrid, Hysing Mari, Ranjitkar Suman, Shrestha Merina, Ulak Manjeswori, Chandyo Ram K., Strand Tor A. The stability of the Bayley scales in early childhood and its relationship with future intellectual abilities in a low to middle income country. Early Human Development. 2022;170:1–8. doi: 10.1016/j.earlhumdev.2022.105610. [DOI] [PubMed] [Google Scholar]
- Lee Eliana S., Yeatman Jason D., Luna Beatriz, Feldman Heidi M. Specific language and reading skills in school-aged children and adolescents are associated with prematurity after controlling for IQ. Neuropsychologia. 2011;49:906–13. doi: 10.1016/j.neuropsychologia.2010.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao Hua-Fang, Wang Pei-Jung, Józsa Krisztián, Blasco Patricia M., Morgan George A. Understanding and supporting mastery motivation in everyday activities: A focus on early childhood intervention. Journal of Psychological and Educational Research. 2021;29:150–73. [Google Scholar]
- Linsell Louise, Malouf Reem, Morris Joan, Kurinczuk Jennifer J., Marlow Neil. Prognostic Factors for Poor Cognitive Development in Children Born Very Preterm or With Very Low Birth Weight: A Systematic Review. JAMA. 2015;169:1162–72. doi: 10.1001/jamapediatrics.2015.2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt Jonathan S., Perrin James M. Influence of clinical and sociodemographic characteristics on early intervention enrollment after NICU discharge. Journal of Early Intervention. 2014;36:37–48. doi: 10.1177/1053815114555575. [DOI] [Google Scholar]
- Long Suzanne H., Galea Mary P., Eldridge Beverley J, Harris Susan R. Performance of 2-year-old children after early surgery for congenital heart disease on the Bayley Scales of Infant and Toddler Development, Third Edition. Early Human Development. 2012;88:603–7. doi: 10.1016/j.earlhumdev.2012.01.007. [DOI] [PubMed] [Google Scholar]
- Lucas Anne, Shaw Evelyn. The University of North Carolina, FPG Child Development Institute, National Early Childhood Technical Assistance Center website; Chapel Hill: 2012. [(accessed on 6 October 2022)]. Informed Clinical Opinion (NECTAC Notes No. 28) Available online: http://www.nectac.org/~pdfs/pubs/nnotes28.pdf. [Google Scholar]
- Lugli Licia, Pugliese Marisa, Plessi Carlotta, Berardi Alberto, Guidotti Isotta, Ancora Gina, Grandi Sara, Gargano Giancarlo, Braibanti Silvia, Sandri Fabrizio, et al. Neuroprem: The Neuro-developmental outcome of very low birth weight infants in an Italian region. Italian Journal of Pediatrics. 2020;46:26. doi: 10.1186/s13052-020-0787-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacTurk Robert B., Morgan George A, Jennings Karen D. Assessment of mastery motivation in infants and young children. In: MacTurk R. B., Morgan G. A., editors. Mastery Motivation: Origins, Conceptualizations, and Applications. Ablex; Norwood: 1995. pp. 19–56. [Google Scholar]
- Marcineková Tatiana, Borbélyová Diana, Tirpáková Anna. Optimization of children’s transition from preschool and family environment to the first grade of primary school in Slovakia by implementation of an adaptation programme. Children and Youth Services Review. 2020;119:105483. doi: 10.1016/j.childyouth.2020.105483. [DOI] [Google Scholar]
- Martin Joyce A., Hamilton Brady E., Osterman Michelle J. K., Driscoll Anne K., Drake Patrick. Births: Final Data for 2016. National Vital Statistics Report. 2018;67:1–55. [PubMed] [Google Scholar]
- McGowan S. Neurodevelopmental Outcomes Associated with Prematurity from Infancy Through Early School Age: A Literature Review. Pediatric Nursing. 2022;48:223–47. [Google Scholar]
- McLester-Davis L. W. Y., Shankar A., Kataria L. A., Hidalgo A. G., Eer E. D. van, Koendjbiharie A. P., Ramjatan R., Hatch V. I., Middleton M. A., Zijlmans C. W. R., et al. Validity, reliability, and transcultural adaptations of the Bayley Scales of Infant and Toddler Development (BSID-III-NL) for children in Suriname. Early Human Development. 2021;160:105416. doi: 10.1016/j.earlhumdev.2021.105416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller Jeffrey H., Bardo Diana M., Cornejo Patricia. Neonatal neuroimaging. Seminars in Pediatric Neurolog. 2020;33:100796. doi: 10.1016/j.spen.2020.100796. [DOI] [PubMed] [Google Scholar]
- Morgan George A., Liao Hua-Fang, Nyitrai Ágnes, Huang Suying, Wang Pei-Jung, Blasco Patricia M., Ramakrishnan Jyothi, Józsa Krisztián. The revised Dimensions of Mastery Questionnaire (DMQ 18) for infants and preschool children with and without risks or delays in Hungary, Taiwan, and the US. Hungarian Educational Research Journal. 2017a;7:48–67. [Google Scholar]
- Morgan George A., Liao Hua-Fang, Józsa Krisztián., editors. Assessing Mastery Motivation in Children Using the Dimensions of Mastery Questionnaire (DMQ) Szent Istvan University; Godollo: 2020. [Google Scholar]
- Morgan George A., Józsa Krisztián, Liao Hua-Fang. Introduction of the special issue on mastery motivation: Measures and results across cultures and ages. Hungarian Educational Research Journal. 2017b;2017:5–14. doi: 10.14413/HERJ/7/2/1. [DOI] [Google Scholar]
- Morgan George A., Harmon Robert J., Maslin-Cole Christine A. Mastery Motivation: Definition and Measurement. Early Education and Development. 1990;1:318–39. doi: 10.1207/s15566935eed0105_1. [DOI] [Google Scholar]
- Niccols Alison, Atkinson L., Pepler D. Mastery motivation in young children with Down’s syndrome: Relations with cognitive and adaptive competence. Journal of Intellectual Disabilities Research. 2003;47:121–33. doi: 10.1046/j.1365-2788.2003.00452.x. [DOI] [PubMed] [Google Scholar]
- Oo Tun Zaw, Habók Anita, Józsa Krisztián. Qualifying Method-Centered Teaching Approaches through the Reflective Teaching Model for Reading Comprehension. Education Sciences. 2023a;13:473. doi: 10.3390/educsci13050473. [DOI] [Google Scholar]
- Oo Tun Zaw, Habók Anita, Józsa Krisztián. Empowering Educators to Sustain Reflective Teaching Practices: The Validation of Instruments. Sustainability. 2023b;15:7640. doi: 10.3390/su15097640. [DOI] [Google Scholar]
- Perra Oliver, McGowan Jennifer E., Grunau Ruth E., Doran Jackie B., Craig Stanley, Johnston Linda, Jenkins John, Holmes Valerie A., Alderdice Fiona A. Parent ratings of child cognition and language compared with Bayley-III in preterm 3-year-olds. Early Human Development. 2015;91:211–16. doi: 10.1016/j.earlhumdev.2015.01.009. [DOI] [PubMed] [Google Scholar]
- Prendergast Sarah, MacPhee David. Parental contributors to children’s persistence and school readiness. Early Childhood Research Quarterly. 2018;45:31–44. doi: 10.1016/j.ecresq.2018.05.005. [DOI] [Google Scholar]
- Rahmawati Anayanti, Fajrianthi, Morgan George A., Józsa Krisztián. An adaptation of DMQ 18 for measuring mastery motivation in early childhood. Pedagogika. 2020;140:18–33. [Google Scholar]
- Saigal Saroj, Doyle Lex W. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371:261–69. doi: 10.1016/S0140-6736(08)60136-1. [DOI] [PubMed] [Google Scholar]
- Salavati Mahyar, Vameghi Roshanak, Hosseini Seyed A., Saeedi Ahmad, Gharib Masoud. Mastery Motivation in Children with Cerebral Palsy (CP) Based on Parental Report: Validity and Reliability of Dimensions of Mastery Questionnaire in Persian. Materia Socio-Medica. 2018;30:108–12. doi: 10.5455/msm.2018.30.108-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott Megan N., Hunter Scott J., Joseph Robert M., O’Shea Thomas Michael, Hooper Stephen R., Allred Elizabeth N., Leviton Alan, Kuban Karl. Neurocognitive Correlates of Attention-Deficit Hyperactivity Disorder Symptoms in Children Born at Extremely Low Gestational Age. Journal of Developmental and Behavioral Pediatrics. 2017;38:249–59. doi: 10.1097/DBP.0000000000000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaoli Salowa Salam, Islam Shaheen, Haque Shamsul, Islam Azharul. Validating the bangla version of the dimensions of mastery questionnaire (DMQ-18) for preschoolers. Asian Journal of Psychiatry. 2019;44:143–49. doi: 10.1016/j.ajp.2019.07.044. [DOI] [PubMed] [Google Scholar]
- Spencer-Smith Megan M., Spittle Alicia J., Lee Katherine J., Doyle Lex W., Anderson Peter J. Bayley-III cognitive and language scales in preterm children. Pediatrics. 2015;135:e1258–65. doi: 10.1542/peds.2014-3039. [DOI] [PubMed] [Google Scholar]
- Tang Brain G., Feldman Heidi M., Huffman Lynne C., Kagawa Kimie J., Gould Jeffrey B. Missed opportunities in the referral of high-risk infants to early intervention. Pediatrics. 2012;129:1027–34. doi: 10.1542/peds.2011-2720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vohr Betty, Wright Linda L., Hack Marie, Aylward Gayle, Hirtz Donald. Follow-up care of high-risk infants. Pediatrics. 2004;114:1377–97. [Google Scholar]
- Wang Pei-Jung, Hwang Ai-Wen, Liao Hua-Fang, Chen Pau-Chung, Hsieh Wu-Shiun. The stability of mastery motivation and its relationship with home environment in infants and toddlers. Infant Behavior and Development. 2011;34:434–42. doi: 10.1016/j.infbeh.2011.04.005. [DOI] [PubMed] [Google Scholar]
- Wang Pei-Jung, Liao Hua-Fang, Morgan George A. The Revised Individualized Moderately Challenging Mastery Tasks for 15 to 48 month-old children. Hungarian Educational Research Journal. 2017;7:68–85. [Google Scholar]
- Wang Pei-Jung, Morgan George A., Liao Hua-Fang, Chen Li-Chio, Hwang Ai-Wen, Lu Lu. Reliability and validity of the revised individualized structured mastery tasks in children with developmental delay. International Journal of Physical Medicine and Rehabilitation. 2016;4:374–80. doi: 10.4172/2329-9096.1000374. [DOI] [Google Scholar]
- Wang Wen, Vallotton Clarie D., Bowles Ryan P. Ethnic variances in socializing young children’s mastery motivation among White, African American, and Hispanic low-income families. Early Childhood Research Quarterly. 2020;51:329–37. doi: 10.1016/j.ecresq.2019.12.012. [DOI] [Google Scholar]
- World Health Organization . The international classification of functioning, disability and health for children and youth: ICF-CY. World Health Organization; Geneva: 2007. [Google Scholar]
- Young Jennifer M., Hauser-Cram Patricia. Mother-child interaction as a predictor of mastery motivation in children with disabilities born preterm. Journal of Early Intervention. 2006;28:252–63. doi: 10.1177/105381510602800402. [DOI] [Google Scholar]
- Zablotsky Benjamin, Black Lindsey, Maenner Matthew, Schieve Laura, Danielson Melissa, Bitsko Rebecca, Blumberg Stephen, Kogan Michael, Boyle Coleen A. Prevalence and Trends of Developmental Disabilities among Children in the United States: 2009–17. Pediatrics. 2019;144:e20190811. doi: 10.1542/peds.2019-0811. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This research is based on human participants, and thus data availability is impossible due to their privacy.