Abstract
Background
: Mortality increased during the COVID-19 pandemic, and many bereaved individuals were not able to gather to memorialize their loved ones, yet it is unknown if this contributed to worsening mental health.
Objective
: Examine the association of bereavement in the early part of the COVID-19 pandemic with subsequent psychological distress and the role of memorial attendance in reducing psychological distress among the bereaved.
Design, Settings, Subjects
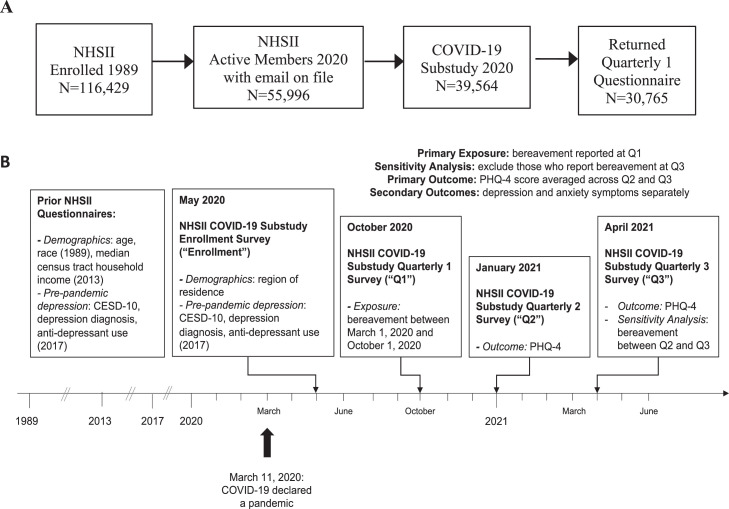
: In May 2020, 39,564 older females from the Nurses’ Health Study II enrolled in a longitudinal COVID-19 substudy (meanage = 65.2 years, SD = 4.5).
Methods
: Linear regression analyses estimated associations of bereavement reported between March and October, 2020 with subsequent psychological distress between January and October 2021, adjusting for sociodemographic and prepandemic depression symptoms. Secondary models examined associations between memorial attendance and psychological distress.
Results
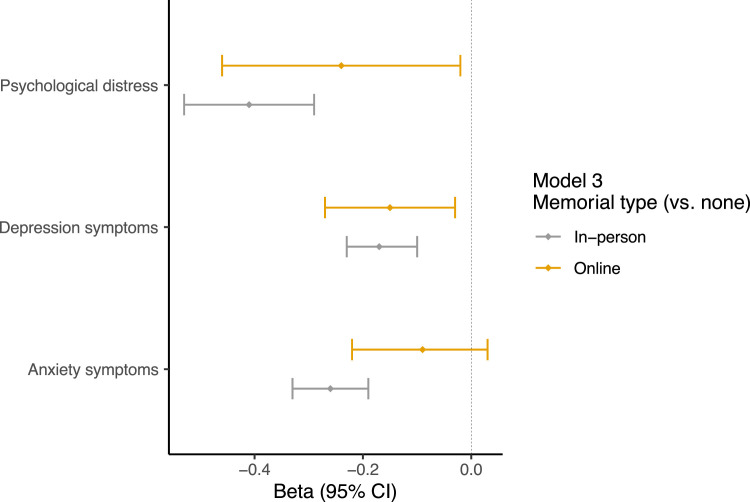
: Bereavement during the early part of the COVID-19 pandemic was associated with higher psychological distress (adjusted β=0.21, 95% CI: 0.15, 0.26) assessed over the next year. Among the bereaved, memorial attendance was associated with lower psychological distress (in-person: adjusted β=-0.41, 95% CI: -0.53, -0.29; online: adjusted β=-0.24, 95% CI: -0.46, -0.02).
Conclusion
: Attending memorials was associated with lower subsequent psychological distress among bereaved older females.
Individuals who experience bereavement at any life-stage may develop mental health complications, yet aging individuals face unique challenges that are exacerbated by the COVID-19 pandemic [1]. First, aging individuals are more likely to experience the death of loved ones, and extant research has found that the death of spouses/partners [2], children [3], siblings [4,5], and even close friends [6] is associated with increased symptoms of psychopathology among older adults. For most people, the acute period of grief will slowly recede over time, as the bereaved person makes peace with the loss [7,8]. However, a non-trivial proportion of bereaved individuals will experience adverse mental health outcomes after bereavement, including depression [9], anxiety [10], and Prolonged Grief Disorder (PGD) [7,11]. The general population burden of depression is especially high for women, with most evidence finding double the risk relative to men [12]; this pattern holds true even among older women [13]. Similar patterns exist for anxiety disorders [14] and (PGD) [15], although results are less consistent for PGD. Consistent with these patterns, a recent study noted that bereavement during the COVID-19 pandemic was associated with higher depression risk, and that women demonstrated worsened depression relative to men [16].
Amid the widespread social changes that occurred due to COVID-19 restrictions on social gatherings that disproportionately impacted older adults, we expect that bereavement during this crisis may elevate risk for adverse mental health conditions, especially among aging individuals, for several reasons. First, the COVID-19 pandemic has increased incident bereavement, especially among aging individuals who faced increased mortality [17]. Second, recent work suggests that bereavement due to COVID-19 is associated with greater acute grief compared to bereavement due to other causes [18], and that bereavement during the pandemic is associated with more acute grief symptoms compared to losses incurred before the pandemic [19]. One potential reason for the elevations in post-bereavement emotional symptoms could be due to pragmatic difficulties [20] including pandemic-imposed changes to bereavement support [21,22]. Specifically, disruptions in the traditional ability to gather and mourn could impact grieving trajectories, although existing studies have been inconclusive (e.g., a recent review noted that of 11 quantitative studies, only 5 noted benefits from funeral participation, and 6 found no association 23, 24, 25). Studies conducted during the COVID-19 pandemic noted similarly mixed findings. For example, a US study noted reductions in general psychological distress among bereaved individuals who attended a memorial either in-person or online [26]. On the other hand, memorials were not associated with a reduction in grief symptoms in a community sample in the Netherlands, despite reporting a perceived positive effect of attending a memorial [27]. A potential explanation for these mixed findings is that prior work has not used prospective mental health data within a longitudinal study design.
Mass bereavement among middle-older adults raises public health concerns, including the effects of social isolation among a population more likely to depend on support [28] and widespread loss of economic, interpersonal, and psychological resources on distress [29,30]. In this prospective, longitudinal cohort COVID-19 substudy in the parent Nurses’ Health Study II (NHSII), we had two aims: 1) to examine the association between bereavement in the early part of the COVID-19 pandemic with anxiety and depression symptoms assessed several months later; and 2) to estimate the association with memorialization of deceased loved ones on downstream symptoms of depression and anxiety. In exploratory analyses, we compared associations by COVID-19 deaths vs. non-COVID deaths, given prior work noting more elevated acute grief among those bereaved due to COVID [18]. Consistent with previous literature [31,26], we hypothesized that bereavement would be associated with higher subsequent anxiety and depression and that attending a memorial service would be associated with reduced post-bereavement anxiety and depression symptoms; memorialization may offer the bereaved an opportunity to experience social support [32] and engage with new information about the death and its consequences to support the resolution of acute grief [33,34].
Methods
Participants
NHSII is an ongoing cohort study that began in 1989 with 116,429 enrolled female-sex registered nurses in the US aged 25-42 years [35]. Participants have been invited to complete questionnaires biennially, with follow-up surveys ongoing. NHSII data are not publicly available but may be made available upon request to the Channing Division of Network Medicine at the Brigham and Women's Hospital. Further information, including the procedures to obtain and access data from the Nurses’ Health Studies, is described at https://www.nurseshealthstudy.org/researchers.
In May 2020, 55,996 active NHSII participants with a known email address were invited to enroll in a COVID-19 substudy. Of those, 39,564 (71%; mean age 65.2 years, SD 4.5 years) participants returned a substudy enrollment questionnaire. Follow-up questionnaires were sent monthly until October 2020 and then quarterly until April, 2021. Bereavement questions were first asked in the October 2020 questionnaire (N=30,765) (Quarterly 1 or “baseline” for this analysis) and were repeated in the final questionnaire of the study April–October 2021 (N=34,381) (Quarterly 3). The present study sample included all respondents to the October 2020 questionnaire. The substudy protocol was approved by the institutional review boards of the Brigham and Women's Hospital and the Harvard T.H. Chan School of Public Health, allowing participants’ completion of questionnaires to imply consent.
Measures
Bereavement. We assessed bereavement (yes / no) at Quarterly 1 and 3. Bereavement relationship types were grouped into three categories representing 1) Spouse/partner or Child, 2) Grandparent, Parent, or Sibling; 3) Other (Other family member, Friend, or Neighbor). COVID as cause of death was assessed (yes/no), as well as memorial attendance (none/online/in-person).
Psychological distress. The Patient Health Questionnaire-4 (PHQ-4) assesses self-reported psychological distress [36]. The 4-item scale is a brief screener comprising the two items from the Generalized Anxiety Disorder-2 (anxiety symptoms) [37] and two items from the PHQ-2 (depression symptoms) [38]. We modeled scores on the PHQ-4 using all items jointly (single-factor solution of psychological distress [range = 0 to 12]) as well as separately (two-factor solution of anxiety symptoms [range = 0 to 6] and depression symptoms [range = 0 to 6]). Evidence from prior research supports the convergent validity, discriminant validity, criterion validity, and internal consistency of scores on the PHQ-4, PHQ-2, and GAD-2 39, 40, 41, 42. In this study, estimated internal consistency was α = .86 for the PHQ-4, α = .84 for the PHQ-2, and α = .79 for the GAD-2 at baseline.
Prepandemic depression symptoms. Three measures from the 2017 NHSII biennial questionnaire were used to construct an index of prepandemic depression symptoms: (1) the Center for Epidemiological Studies-Depression (CESD-10; [43] score, (2) self-report of a physician's diagnosis of depression, (3) self-report of having taken selective serotonin reuptake inhibitor (SSRI) or non-SSRI antidepressants in the past two years. Participants met criteria for prepandemic depression symptoms if they had a CESD-10 score of at least 10 [44], reported taking any antidepressant medication in the past two years, or reported a clinical diagnosis of depression.
Demographic covariates. Age and self-identified race (nonwhite, white) were obtained in 1989, region of residence (midwest, south, west, other, northeast) was assessed at the COVID substudy enrollment, and median census tract household income was available as of the 2013 biennial NHSII questionnaire and calculated from the 2010 census.
Statistical Analysis
First, we conducted between-group age-adjusted comparisons on demographic and primary variables among bereaved and non-bereaved participants. We compared non-responders to responders and to the total sample of invited individuals on demographic factors collected in earlier NHSII questionnaires to assess the presence of potential bias. Linear regression models were used for primary analyses to estimate the main association between baseline bereavement (both as a binary exposure (‘did a loved one die, yes/no’) and as a four-category exposure (no loved one died (reference), child or spouse, grandparent, parents, or sibling, and other)) with subsequent Quarterly 2 and Quarterly 3 PHQ-4 assessed depression and anxiety symptoms, modeled continuously. We modeled post-bereavement depression and anxiety symptoms as an average across two follow-up waves in light of fluctuating pandemic-related conditions (e.g., relaxed public health guidelines at Quarterly 3 relative to Quarterly 2) to take a balanced approach to look at the medium-term associations with bereavement.
Linear regression models were used for secondary analyses to estimate the association with attending a memorial service on post-bereavement symptoms of depression and anxiety averaged across Quarterly 2 and 3. Finally, linear regression was used in three steps to 1) model the main association with losing a loved one to COVID-19 vs. other causes on symptoms of anxiety and depression, 2) stratify bereaved participants into loved one's cause of death due to COVID-19 vs. other causes, and estimate the association with attending a memorial service on symptoms of depression and anxiety, and 3) to assess effect modification of memorial attendance on cause of death and depression and anxiety symptoms by specifying an interaction term of memorial attendance (yes/no) by COVID-19 cause of death (yes/no).
Results are reported for combined depression and anxiety symptoms (PHQ-4), as well as depression symptoms (PHQ-2) and anxiety symptoms (GAD-2) separately to estimate symptom variation between these two conditions. Item level missingness when calculating PHQ-4 scale scores was handled by imputing missing values when fewer than half the items missing. For scales containing only two items (PHQ-2 and GAD-2), we did not impute missing data. Finally, all linear regression models were specified first as unadjusted, and uniformly adjusted for sociodemographic characteristics including age, race (nonwhite/white reference), region of residence (midwest, south, west, other, northeast reference), median census tract household income. Standardized regression coefficients are reported throughout. To estimate the potential confounding effect of depression symptoms present prior to an individual's bereavement event, primary models were further adjusted for prepandemic depression symptoms, assessed in 2017 (see above, measures section; see also Supplement for unadjusted model coefficients).
Results
Table 1 contains age standardized characteristics of the NHSII COVID-19 substudy participants stratified by bereavement status at the first baseline assessment. Comparisons between non-responders, responders and the total sample of invited individuals on demographic factors collected in earlier NHSII questionnaires revealed no meaningful between-group differences (see Supplemental Tables 1-3). Of the 30,578 participants who responded to the bereavement questions in the COVID-19 substudy, 6,901 (22.6%) women reported losing a loved one (Table 1).
Table 1.
Age-standardized Characteristics of the NHSII COVID-19 Substudy by Bereavement Status at Q1 (October, 2020).
| Characteristic | Death of a loved one |
|
|---|---|---|
| No (N = 23,677) | Yes (N = 6,901) | |
| Age* (years), M (SD) | 65.40 (4.49) | 65.29 (4.50) |
| Median household family income (based on 2010 Census) as of 2013, US dollars, M (SD) | 84,038 (32,633) | 82,484 (31,449) |
| Prepandemic depression symptoms, % | 25 | 24 |
| Psychological distress (PHQ-4), M (SD) | 1.96 (2.20) | 2.15 (2.32) |
| Depression symptoms (PHQ-2), M (SD) | 0.90 (1.18) | 0.99 (1.23) |
| Anxiety symptoms (GAD-2), M (SD) | 1.15 (1.27) | 1.26 (1.32) |
| Nonwhite, % | 2 | 4 |
| Geographic region, % | ||
| Northeast | 28 | 28 |
| Midwest | 30 | 31 |
| South | 23 | 24 |
| West | 18 | 17 |
| Other | 0 | 0 |
| Deceased relationship, % | ||
| Spouse or child | 3 | |
| Parent‚ grandparent‚ or sibling | 22 | |
| Other family member, friend, or neighbor | 76 | |
| COVID-19 cause of death, % | 19 | |
| Type of memorial, % | ||
| None | 51 | |
| Online only | 7 | |
| In-person | 41 | |
Note. Values are standardized to the age distribution of the study population.
Values of polytomous variables may not sum to 100% due to rounding. PHQ-4 = Patient Health Questionnaire-4 item, PHQ-2 = Patient Health Questionnaire-2 item, GAD-2 = Generalized Anxiety Disorder-2.
Value is not age adjusted.
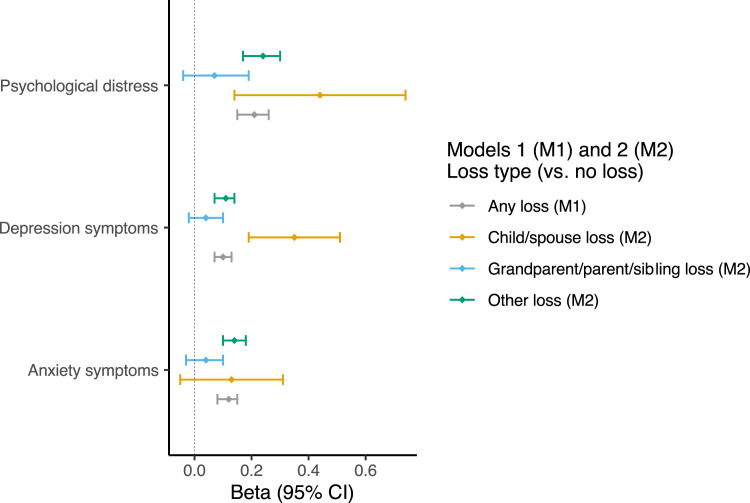
To test the primary study aim, we fit linear regression models that adjusted for sociodemographic characteristics and prepandemic depression symptoms to test whether bereavement was associated with elevated psychological distress. (See supplement Table 4 for unadjusted model results). Model 1 results suggested that bereavement was associated with higher psychological distress (R2 = 0.006, F(8, 29,354) = 22.27, p<0.00001) relative to non-bereaved participants. Model 2 demonstrates that elevated psychological distress was present only in bereaved adults who lost a child or spouse (n=200) or friends, neighbors, or other relatives (n=5,207) (R2 = 0.006, F(10, 29,345)=18.62, p<0.0001). Loss of a grandparent, sibling, or parent (n=1,486) was not significantly associated with elevated psychological distress. Full results are presented in Table 2 . In sensitivity analyses, we found that sixty percent of our analytic sample reported experiencing the death of a loved one at baseline but not in Quarterly 3. Sensitivity analyses excluding those who also reported a loss in Quarterly 3 did not change our main findings, but analyses are speculative given the unmeasured differences between groups bereaved at baseline and Quarterly 3.
Table 4.
Associations of COVID-19 Bereavement and Memorial Attendance by Cause of Death with Subsequent Psychological Distress, Depression Symptoms, and Anxiety Symptoms
| Predictor | Psychological distress (Model 4a), N = 6,625, df=8 |
||||
|---|---|---|---|---|---|
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| COVID-19 cause of death | 5.71 | <0.0001 | |||
| Yes | 0.15 | 0.01 | 0.29 | 0.0371 | |
| No | ref | ref | ref | ||
| Depression symptoms (Model 4b), N = 6,622, df=8 | |||||
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| COVID-19 cause of death | 3.07 | 0.0019 | |||
| Yes | 0.03 | -0.04 | 0.11 | 0.4112 | |
| No | ref | ref | ref | ||
| Anxiety Symptoms (Model 4c), N = 6,621, df=8 | |||||
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| COVID-19 cause of death | 7.11 | <0.0001 | |||
| Yes | 0.12 | 0.04 | 0.20 | 0.0039 | |
| No | ref | ref | ref | ||
| Psychological distress (Model 5a)a, N = 6,625, df=10 | |||||
| β | Lower 95% CI | Upper 95% CI | p-value | ||
| Memorial (yes) x COVID-19 cause of death (yes) | 0.10 | -0.20 | 0.40 | 0.5064 | |
| Depression symptoms (Model 5b)b, N = 6,622, df=10 | |||||
| β | Lower 95% CI | Upper 95% CI | p-value | ||
| Memorial (yes) x COVID-19 cause of death (yes) | 0.03 | -0.13 | 0.19 | 0.6752 | |
| Anxiety Symptoms (Model 5c)c, N = 6,621, df=10 | |||||
| β | Lower 95% CI | Upper 95% CI | p-value | ||
| Memorial (yes) x COVID-19 cause of death (yes) | 0.03 | -0.14 | 0.20 | 0.6999 | |
Note. β = standardized effect size, CI = confidence interval. Interaction models 5a-c F-values are: aModel 5a F-value = 8.79. p<0.001
Model 5b F-value=5.31, p<0.001
Model 5c F-value=10.30, p<0.001. Linear regression models were used to estimate a β for each outcome. Models adjusted for age, race, geographic location, and median census tract household income. To achieve model parsimony, models were not adjusted for prepandemic depression symptoms given non-significant associations noted in primary models.
Table 2.
Association of Bereavement Experienced between March 2020 – October 2020 (Q1) and Subsequent Psychological Distress, Depression Symptoms, and Anxiety Symptoms at Q2 and Q3 (January 2021-October 2021).
| Predictor | Psychological distress (Model 1), N = 29,363, df=8 |
||||
|---|---|---|---|---|---|
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| Bereaved | 330.42 | <0.0001 | |||
| Yes | 0.21 | 0.15 | 0.26 | <0.0001 | |
| No | ref | ref | ref | ||
| Depression symptoms (Model 1), N = 29,354, df=8 | |||||
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| Bereaved | 357.35 | <0.0001 | |||
| Yes | 0.10 | 0.07 | 0.13 | <0.0001 | |
| No | ref | ref | ref | ||
| Anxiety Symptoms (Model 1), N = 29,352, df=8 | |||||
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| Bereaved | 217.53 | <0.0001 | |||
| Yes | 0.12 | 0.08 | 0.15 | <0.0001 | |
| No | ref | ref | ref | ||
| Predictor | Psychological distress (Model 2), N = 29,356, df=10 | ||||
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| Relationship type | 271.02 | <0.0001 | |||
| Child or spouse | 0.44 | 0.14 | 0.74 | 0.005 | |
| Grandparent, parent, or sibling | 0.07 | -0.04 | 0.19 | 0.200 | |
| Friends, neighbors, or other family members | 0.24 | 0.17 | 0.30 | <0.0001 | |
| No death | ref | ref | ref | ||
| Depression symptoms (Model 2), N = 29,347, df=10 | |||||
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| Relationship type | 293.56 | <0.0001 | |||
| Child or spouse | 0.35 | 0.19 | 0.51 | <0.0001 | |
| Grandparent, parent, or sibling | 0.07 | -0.04 | 0.19 | 0.195 | |
| Friends, neighbors, or other family members | 0.24 | 0.17 | 0.30 | <0.0001 | |
| No death | ref | ref | ref | ||
| Anxiety Symptoms (Model 2), N = 29,345, df=10 | |||||
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| Relationship type | 178.62 | <0.0001 | |||
| Child or spouse | 0.13 | -0.05 | 0.31 | 0.152 | |
| Grandparent, parent, or sibling | 0.04 | -0.03 | 0.10 | 0.262 | |
| Friends, neighbors, or other family members | 0.14 | 0.10 | 0.18 | <0.0001 | |
| No death | ref | ref | ref | ||
Note. Linear regression models were used to estimate standardized regression weights (β) for the outcome. 95% CI is the standardized 95% confidence interval. Model 1, N=30,765; 30,765 (22.4%) bereaved; 23,677 (77%) not bereaved. Model 2, N(child or spouse)=200(0.7%), N(grandparent, parent, or sibling)=1,486 (4.8%); N(friends, neighbors, or other family members)=5,207(16.9%), N(no death)-23,677 (77%). tPsychological distress, depression, and anxiety were assessed at Q2 and Q3 via the Patient Health Questionnaire (PHQ-4) and averaged for a single outcome value. When calculating the scale scores, if a scale had fewer than half the items missing, we imputed the missing items. Thus the 4-item scale has a few more individuals than either of the two-item scales. Models adjusted for age, race, geographic location, median census tract household income, and prepandemic depression symptoms assessed in 2017.
To test secondary aims, we fit linear regression models to test whether memorial attendance was associated with reduced post-bereavement psychological distress. In models adjusted for baseline sociodemographic variables (see Supplemental Table 5 for unadjusted model results), we found that among the bereaved, attending either an in-person memorial (n=2834) or online memorial (n=506)) was associated with reduced symptoms of psychological distress at follow up compared to bereaved individuals who did not attend a memorial (n=3533) (R2=0.013, F(9, 6587)=9.84, p<0.0001). Full results are presented in Table 3 .
Table 3.
Associations between Memorial Attendancea in Q1 (October 2020) and Subsequent Psychological Distress, Depression Symptoms, and Anxiety Symptoms at Q2 and Q3 (January 2021-October 2021).
| Predictor | Psychological distress (Model 3a), N = 6,597, df=9 |
||||
|---|---|---|---|---|---|
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| Type of memorial | 9.84 | <0.0001 | |||
| In-person | -0.41 | -0.53 | -0.29 | <0.0001 | |
| Online | -0.24 | -0.46 | -0.02 | 0.0315 | |
| None | ref. | ||||
| Depression symptoms (Model 3b), N = 6,593, df=9 | |||||
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| Type of memorial | 5.89 | <0.0001 | |||
| In-person | -0.17 | -0.23 | -0.10 | <0.0001 | |
| Online | -0.15 | -0.27 | -0.03 | 0.0310 | |
| None | ref. | ||||
| Anxiety Symptoms (Model 3c), N = 6,594, df=9 | |||||
| β | Lower 95% CI | Upper 95% CI | F-value | p-value | |
| Type of memorial | 11.79 | <0.0001 | |||
| In-person | -0.26 | -0.33 | -0.19 | <0.0001 | |
| Online | -0.09 | -0.22 | 0.03 | 0.1383 | |
| None | ref. | ||||
Note. Linear regression models were used to estimate a β for each outcome. β = standardized effect size, CI = confidence interval. When calculating the scale scores, if a scale had fewer than half the items missing, we imputed the missing items. For scales containing only two items, we did not impute missing data. Models adjusted for age, race, geographic location, and median census tract household income. To achieve model parsimony, models were not adjusted for prepandemic depression symptoms given non-significant associations noted in primary models. aIn-person memorial: N = 506 (7.3%), online memorial: N = 2,834 (41.1%), no memorial: N = 3,533 (51.2%).
Finally, we evaluated whether the previous analyses differed by COVID-19 cause of death (yes/no) in three steps. First, we found that the death of a loved one due to COVID-19 (n= 1312) was associated with elevated psychological distress (Model 4a) relative to non-COVID deaths (n= 5589) (R2=0.01, F(8, 6616)=5.71, p<0.0001). Yet when anxiety symptoms (Model 4b) and depression symptoms (Model 4c) were examined separately, results suggest that anxiety symptoms, not depression symptoms, explained this association (Model 4b: R2=0.008, F(8, 6613)=3.07, p=0.002; Model 4c: R2=0.01, F(8, 6612)=7.11, p<0.001). Then, we extend Model 4 to evaluate if the association between memorial attendance and psychological distress differed by cause of death, finding no association relative to COVID-19 vs. other causes of death (Model 5a: R2=0.013, F(10, 6586)=8.79, p<0.0001; Model 5b: R2=0.008, F(10, 6583)=5.31, p<0.001; Model 5c: R2=0.015, F(10, 6582)=10.3, p<0.0001). Table 4 shows full model results, including coefficients reported separately for models predicting psychological distress, depression symptoms, and anxiety symptoms. Supplemental Table 6 contains results of additional analyses estimating the effects of memorial type on psychological distress stratified by cause of death, confirming that in-person memorial attendance is associated with lower psychological distress in both COVID-19 and non-COVID-19 deaths.
Discussion
This study leveraged a unique, large, community-based longitudinal sample of older women to investigate whether bereavement during the COVID-19 pandemic was associated with psychological distress assessed in follow-up waves, and if attending a memorial service attenuated post-bereavement symptoms of depression and anxiety. Our results suggested a moderate association of bereavement during COVID-19 with higher subsequent psychological distress (r = .26). For context, the strength of this association is slightly larger than that reported in one prepandemic study on the association between bereavement and depression among both older men and women (e.g., r = .12 [45]), but is less than the larger effect size noted in a metanalysis on the association between early trauma and adult depression (e.g. r = ∼.50 [46]). Exploratory supplemental analyses investigated whether associations between bereavement and mental health symptoms varied by COVID-19 vs. non-COVID-19 causes of death. We found that bereavement during the pandemic was associated with elevated psychological distress, relative to not experiencing the death of a loved one during the same period, but only for those experiencing the death of a spouse/partner or child, as well as a friend, other family member, or neighbor, and not the death of a parent, grandparent or sibling. Results suggest that among aging individuals, bereavement of non-kin relationships could be an additional source of distress, consistent with literature suggesting that extended non-kin support networks are important sources of well-being for older adults [47]. Finally, our exploratory analyses found that among those bereaved, levels of anxiety, but not depression, were higher when the cause of death was COVID-19, relative to non-COVID causes. These novel findings are consistent with literature suggesting that the qualities of an older adult's death affects surviving spouses psychological adjustment after bereavement, such that a painful death, in particular, is associated with elevated anxiety [48]. Given the unprecedented challenges associated with COVID-19 fatalities among aging populations, including social isolation, difficulty breathing, and physical discomfort, our results align with calls for improving healthcare capacity for bereavement care in the context of COVID-19 [49]. Taken together, our study findings suggest important public health implications for aging females in the context of the COVID-19 pandemic that has put elderly individuals specifically at risk [17]. Given the associations among bereavement and elevated risk for depression [9], anxiety [10], and Prolonged Grief Disorder [7,11], the very high rates of bereavement during COVID-19 [50,51] will likely be associated with a population-level rise in psychological distress, consistent with extant epidemiological evidence [52].
The COVID-19 pandemic dramatically impacted bereavement care for millions of individuals regardless of cause of death, and the public health measures that were implemented to limit or control the transmission of SARS-CoV-2 restricted many people from participating in traditional memorialization and mourning practices. We found that attending a memorial service, either online or in-person, was associated with lower levels of depression and anxiety compared to not attending a memorial, regardless of the cause of death. Unfortunately, we could not test for more specific effects among COVID-19 related deaths because we were underpowered to examine interaction effects by the specific type of memorial (on-line or in-person) and associations among depression and anxiety symptoms in the sub-group. Future research in well-powered analyses with sufficient sample sizes are needed to address this question more definitively. Initial results from this study augment existing evidence [26] documenting the protective effect of memorial attendance on mental health by investigating the specific impact of in-person, online, or no memorial attendance on subsequent symptoms of depression and anxiety in a large, community-dwelling aging cohort, considering prepandemic prospective mental health data.
Our findings raise questions as to what mechanisms might underpin the association between memorial attendance and attenuated depression and anxiety symptoms. First, it may be that memorial attendance is a proxy for structural factors, such as household income, that may best explain the association between memorial attendance and reduced depression and anxiety symptoms, though this possibly is diminished given that we did control for household income in our analyses. Alternatively, it may be that the social support and connectedness associated with memorial attendance is a protective factor. This is a stronger possibility given the female sample, where the ‘tend and befriend’ stress response hypothesis involves nurturant activities designed to protect the self and others to reduce distress, including the creation and maintenance of social networks [53]. Finally, memorial attendance may be correlated with higher religious or spiritual practices, and access to religious or spiritually meaningful practices post-bereavement, in turn, may support well-being after loss. However, prior work has shown mixed findings with some work noting a protective effect of religious coping against elevated grief [54,55], and others noting a negative association between religious coping and post-bereavement well-being [56]. Thus, considering the present results in the context of prior work, future research is warranted to investigate candidate protective mechanisms associated with memorial attendance.
Several limitations should be taken into consideration before generalizing the present findings to a broader population. First, the present analytic sample included only information about depression and anxiety symptoms. We did not assess symptoms of prolonged grief, including the core symptoms of yearning, longing, or preoccupying thoughts and memories of the deceased, and we have no way of knowing whether some of the symptoms of anxiety and depression are better explained by grief. Future studies of bereavement outcomes need to include measures of grief and PGD. Also, the sample included only older women, and therefore it is not clear if the results here could be generalized to men or those in other lifespan stages. Future work with adequately powered samples to examine sex differences is warranted. Our primary findings should also be interpreted while keeping in mind the possibility that some individuals could have also experienced additional Quarterly 3 bereavement for which we could not fully consider the additional impact in our study design. Sensitivity analyses excluding those who also reported a loss in Quarterly 3 did not change our main findings, but analyses are speculative given the unmeasured differences between groups bereaved at baseline and Quarterly 3. Assessment of memorial attendance was in reference to a single, most important loss as determined by the study participant. It could be that participants experienced multiple losses and did attend a memorial for another target loss. Finally, even though our sample size was large, we were still underpowered to stratify by the specific type of relationship with the deceased for evaluating a possible protective effect of memorial attendance. It could be that not attending an in-person memorial service is more distressing when the deceased is one's child or spouse, versus a neighbor, for example. Similarly, we did not have detailed information on the specific nature of the memorial attendance; it could be that other kinds of resources, such as religious services, may be even more protective. Future studies focused on post-bereavement social activities that reduce risk for psychopathology are warranted. While a significant strength of our study included assessment of prepandemic depression symptoms in 2017, we did not have a similar measure for prepandemic anxiety symptoms. Therefore, we cannot rule out that prepandemic anxiety is a factor in elevated levels of anxiety during the COVID substudy period. Also, we did not have measures of prepandemic depression between 2017 and early 2020. It is possible that depression or anxiety symptoms presented during this interval, especially among individuals facing the potential death of a loved one. Future research would benefit from more precise timing of post – and pre-bereavement distress. Relatedly, though we controlled for prepandemic depression symptoms in primary models, it may be that depression symptoms exerted a causal effect on reduced memorial attendance. Ruling this possibility out was not possible, given the constraints of our data. Additionally, the context of the pandemic exerted independent effects on memorial attendance behaviors, given widespread social distancing. Finally, 96% of participants were White, resulting in an underrepresentation of other racial/ethnic groups. This is a considerable limitation given studies demonstrating that Black and Hispanic individuals bear a relatively higher burden of familial death than White individuals [50,57], implying that our estimates of the prevalence of loss may be lower than those for the general population. It is possible that participants’ healthcare worker occupational status meant that participants were more often included in end-of-life care for loved ones and therefore knew more people who died, this possibility cannot be conclusively explored in the current analyses.
In conclusion, results suggest a potential protective association between memorial attendance on post-bereavement symptoms of depression and anxiety. If confirmed, results suggest that access to memorial services could contribute to reducing risk for post-bereavement anxiety and depressive symptoms. Future research is needed to better understand potential preventative mechanisms that reduce the risk of elevated post-bereavement distress at the population health level.
Figure 1.
Nurses Health Study II (NHSII) COVID-Substudy participant flowchart (A) and timeline (B)
Note: NHS: Nurses Health Study; Quotation marks in panel B detail the abbreviated naming system that appears throughout the manuscript to index study waves.
Figure 2.
Associations of Bereavement with Subsequent Psychological Distress by Type of Loss.
Figure 3.
Associations of In-person and Online Memorial Attendance with Subsequent Psychological Distress Among the Bereaved.
Authorship contributions
CAD (conceptual design, supervising analysis, writing and revising), JH (lead analyst, data management, revision) RC (methodology, writing and revising), SO (writing), KG (writing), ALED (visualization, validation, editing), SJ (administration, editing) JK (data management, revising), KS (conceptual design, revising).
Data Statement
The data has been previously presented as a poster at the following scientific meeting:
Denckla CA, Hahn J, Cowden, R. Bereavement, memorial attendance, and mental health during the COVID-19 pandemic: Longitudinal results from the Nurses’ Health Study. Poster presented at the American Association for Geriatric Psychiatry Annual Conference. March 4th, 2023; New Orleans, USA
Declaration of Competing Interest
None declared.
Acknowledgments
Funding
This work was supported by the National Institutes of Health (U01 CA176726 NHSII cohort infrastructure grant) National Institute of Mental Health (CAD K23MH117278). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors have no competing interests to declare that are relevant to the content of this article.
Acknowledgments
The authors would like to acknowledge the Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital, and Harvard Medical School for managing the NHS II.
Footnotes
Disclosure: All authors have no conflicts of interest or financial disclosures related to this work to report. Primary datasets were not used to produce this proceedings paper, therefore data availability is not applicable.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jagp.2023.06.012.
Appendix. SUPPLEMENTARY MATERIALS
REFERENCES
- 1.Goveas JS, Shear MK. Grief and the COVID-19 pandemic in older adults. Focus. 2021;19:374–378. doi: 10.1176/appi.focus.19303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Onrust SA, Cuijpers P. Mood and anxiety disorders in widowhood: a systematic review. Aging Ment Health. 2006;10:327–334. doi: 10.1080/13607860600638529. [DOI] [PubMed] [Google Scholar]
- 3.Yang L, Weng X, Subramanian SV. Associations between older adults’ parental bereavement and their health and well-being: Evidence from the China health and retirement longitudinal study. J Affect Disord. 2020;272:207–214. doi: 10.1016/j.jad.2020.03.136. [DOI] [PubMed] [Google Scholar]
- 4.Rostila M, Saarela J, Kawachi I. The forgotten griever: a nationwide follow-up study of mortality subsequent to the death of a sibling. Am J Epidemiol. 2012;176:338–346. doi: 10.1093/aje/kws163. [DOI] [PubMed] [Google Scholar]
- 5.Bolton JM, Au W, Walld R, et al. Parental bereavement after the death of an offspring in a motor vehicle collision: a population-based study. Am J Epidemiol. 2014;179:177–185. doi: 10.1093/aje/kwt247. [DOI] [PubMed] [Google Scholar]
- 6.Liu W-M, Forbat L, Anderson K. Death of a close friend: Short and long-term impacts on physical, psychological and social well-being. PLoS One. 2019;14 doi: 10.1371/journal.pone.0214838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shear MK. Complicated Grief. N Engl J Med. 2015;372:153–160. doi: 10.1056/NEJMcp1315618. [DOI] [PubMed] [Google Scholar]
- 8.Bonanno GA, Wortman CB, Lehman DR, et al. Resilience to loss and chronic grief: a prospective study from preloss to 18-months postloss. J Pers Soc Psychol. 2002;83:1150–1164. doi: 10.1037//0022-3514.83.5.1150. [DOI] [PubMed] [Google Scholar]
- 9.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160:1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 10.Komischke-Konnerup KB, Zachariae R, Johannsen M, et al. Co-occurrence of prolonged grief symptoms and symptoms of depression, anxiety, and posttraumatic stress in bereaved adults: A systematic review and meta-analysis. Journal of Affective Disorders Reports. 2021;4 [Google Scholar]
- 11.Lundorff M, Holmgren H, Zachariae R, et al. Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. J Affect Disord. 2017;212:138–149. doi: 10.1016/j.jad.2017.01.030. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 13.Girgus JS, Yang K, Ferri CV. The gender difference in Depression: Are elderly women at greater risk for depression than elderly men? Geriatrics. 2017;2 doi: 10.3390/geriatrics2040035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 15.Kersting A, Brähler E, Glaesmer H, et al. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131:339–343. doi: 10.1016/j.jad.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 16.Wang H, Verdery AM, Margolis R, et al. Bereavement from COVID-19, gender, and reports of depression among older adults in Europe. J Gerontol B Psychol Sci Soc Sci. 2021 doi: 10.1093/geronb/gbab132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Y, Klein SL, Garibaldi BT, et al. Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res Rev. 2021;65 doi: 10.1016/j.arr.2020.101205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eisma MC, Tamminga A, Smid GE, et al. Acute grief after deaths due to COVID-19, natural causes and unnatural causes: An empirical comparison. J Affect Disord. 2021;278:54–56. doi: 10.1016/j.jad.2020.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eisma MC, Tamminga A. Grief Before and During the COVID-19 Pandemic: Multiple Group Comparisons. J Pain Symptom Manage. 2020;60:e1–e4. doi: 10.1016/j.jpainsymman.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Testoni I, Azzola C, Tribbia N, et al. The COVID-19 disappeared: From traumatic to ambiguous loss and the role of the internet for the bereaved in Italy. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.620583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pearce C, Honey JR, Lovick R, et al. A silent epidemic of grief”: a survey of bereavement care provision in the UK and Ireland during the COVID-19 pandemic. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-046872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harrop E, Goss S, Farnell D, et al. Support needs and barriers to accessing support: Baseline results of a mixed-methods national survey of people bereaved during the COVID-19 pandemic. Palliat Med. 2021;35:1985–1997. doi: 10.1177/02692163211043372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burrell A, Selman LE. How do funeral practices impact bereaved relatives’ mental health, grief and bereavement? A mixed methods review with implications for COVID-19. Omega. 2020 doi: 10.1177/0030222820941296. 30222820941296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woodthorpe K, Rumble H, Corden A, et al. My Memories of the Time We Had Together Are More Important’: Direct cremation and the privatisation of UK funerals. Sociology. 2021 00380385211036350. [Google Scholar]
- 25.Lowe J, Rumbold B, Aoun SM. Memorialisation during COVID-19: implications for the bereaved, service providers and policy makers. Palliat Care Soc Pract. 2020;14 doi: 10.1177/2632352420980456. 2632352420980456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen CY-C. Grieving during the COVID-19 pandemic: In-person and virtual “goodbye. Omega. 2022 doi: 10.1177/00302228221090754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitima-Verloop HB, Mooren TTM, Boelen PA. Facilitating grief: An exploration of the function of funerals and rituals in relation to grief reactions. Death Stud. 2021;45:735–745. doi: 10.1080/07481187.2019.1686090. [DOI] [PubMed] [Google Scholar]
- 28.Kotwal AA, Holt-Lunstad J, Newmark RL, et al. Social isolation and loneliness Among San Francisco Bay Area older adults during the COVID-19 shelter-in-place orders. J Am Geriatr Soc. 2021;69:20–29. doi: 10.1111/jgs.16865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cowden RG, Rueger SY, Davis EB, et al. Resource loss, positive religious coping, and suffering during the COVID-19 pandemic: a prospective cohort study of US adults with chronic illness. Ment Health Relig Cult. 2021:1–17. [Google Scholar]
- 30.Counted V, Cowden RG, Ramkissoon H. Springer Nature; 2021. Place and Post-Pandemic Flourishing: Disruption, Adjustment, and Healthy Behaviors. [Google Scholar]
- 31.Keyes KM, Pratt C, Galea S, et al. The burden of loss: unexpected death of a loved one and psychiatric disorders across the life course in a national study. Am J Psychiatry. 2014;171:864–871. doi: 10.1176/appi.ajp.2014.13081132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stroebe Zech. Stroebe. Does social support help in bereavement? Int J Soc Humanit Sci Res (JSHSR) 2005 [Google Scholar]
- 33.Shear MK. Grief and mourning gone awry: pathway and course of complicated grief. Dialogues Clin Neurosci. 2012;14:119–128. doi: 10.31887/DCNS.2012.14.2/mshear. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Connor M-F, Seeley SH. Grieving as a form of learning: Insights from neuroscience applied to grief and loss. Curr Opin Psychol. 2022;43:317–322. doi: 10.1016/j.copsyc.2021.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Colditz GA, Manson JE, Hankinson SE. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Womens Health. 1997;6:49–62. doi: 10.1089/jwh.1997.6.49. [DOI] [PubMed] [Google Scholar]
- 36.Kroenke K, Spitzer RL, Williams JBW, et al. An Ultra-Brief Screening Scale for Anxiety and Depression: The PHQ–4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K, Spitzer RL, Williams JBW, et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 38.Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) J Psychosom Res. 2005;58:163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 39.Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 40.Staples LG, Dear BF, Gandy M, et al. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: The PHQ-2, GAD-2, and K-6. Gen Hosp Psychiatry. 2019;56:13–18. doi: 10.1016/j.genhosppsych.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 41.Bisby MA, Karin E, Scott AJ, et al. Examining the psychometric properties of brief screening measures of depression and anxiety in chronic pain: The Patient Health Questionnaire 2-item and Generalized Anxiety Disorder 2-item. Pain Pract. 2022;22:478–486. doi: 10.1111/papr.13107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kroenke K, Spitzer RL, Williams JBW, et al. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 43.Radloff LS. The CES-D Scale: A self-report Depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 44.Huang T, Trudel-Fitzgerald C, Poole EM, et al. The Mind-Body Study: study design and reproducibility and interrelationships of psychosocial factors in the Nurses’ Health Study II. Cancer Causes Control. 2019;30:779–790. doi: 10.1007/s10552-019-01176-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gallagher DE, Breckenridge JN, Thompson LW, et al. Effects of bereavement on indicators of mental health in elderly widows and widowers. J Gerontol. 1983;38:565–571. doi: 10.1093/geronj/38.5.565. [DOI] [PubMed] [Google Scholar]
- 46.Mandelli L, Petrelli C, Serretti A. The role of specific early trauma in adult depression: A meta-analysis of published literature. Childhood trauma and adult depression. Eur Psychiatry. 2015;30:665–680. doi: 10.1016/j.eurpsy.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 47.Fiori KL, Antonucci TC, Cortina KS. Social network typologies and mental health among older adults. J Gerontol B Psychol Sci Soc Sci. 2006;61:P25–P32. doi: 10.1093/geronb/61.1.p25. [DOI] [PubMed] [Google Scholar]
- 48.Carr D. A “good death” for whom? Quality of spouse's death and psychological distress among older widowed persons. J Health Soc Behav. 2003;44:215–232. [PubMed] [Google Scholar]
- 49.Carr D, Boerner K, Moorman S. Bereavement in the time of coronavirus: Unprecedented challenges demand novel interventions. J Aging Soc Policy. 2020;32:425–431. doi: 10.1080/08959420.2020.1764320. [DOI] [PubMed] [Google Scholar]
- 50.Verdery AM, Smith-Greenaway E, Margolis R, et al. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proc Natl Acad Sci U S A. 2020;117:17695–17701. doi: 10.1073/pnas.2007476117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Woolf SH, Chapman DA, Sabo RT, et al. Excess deaths from COVID-19 and other causes in the US, March 1, 2020, to January 2, 2021. JAMA. 2021 doi: 10.1001/jama.2021.5199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Coley RL, Baum CF. Trends in mental health symptoms, service use, and unmet need for services among U.S. adults through the first 9 months of the COVID-19 pandemic. Transl Behav Med. 2021;11:1947–1956. doi: 10.1093/tbm/ibab030. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 53.Taylor SE, Klein LC, Lewis BP, et al. Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight. Psychol Rev. 2000;107:411–429. doi: 10.1037/0033-295x.107.3.411. [DOI] [PubMed] [Google Scholar]
- 54.Lövgren M, Sveen J, Steineck G, et al. Spirituality and religious coping are related to cancer-bereaved siblings’ long-term grief. Palliat Support Care. 2019;17:138–142. doi: 10.1017/S1478951517001146. [DOI] [PubMed] [Google Scholar]
- 55.Smith Lee JR, Hunter AG, Priolli F, et al. Pray that I live to see another day”: Religious and spiritual coping with vulnerability to violent injury, violent death, and homicide bereavement among young Black men. J Appl Dev Psychol. 2020;70 [Google Scholar]
- 56.Lee SA, Roberts LB, Gibbons JA. When religion makes grief worse: negative religious coping as associated with maladaptive emotional responding patterns. Ment Health Relig Cult. 2013;16:291–305. [Google Scholar]
- 57.Umberson D, Olson JS, Crosnoe R, et al. Death of family members as an overlooked source of racial disadvantage in the United States. Proc Natl Acad Sci U S A. 2017;114:915–920. doi: 10.1073/pnas.1605599114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.