Abstract
Purpose
To examine the clinical outcomes and return to sport rates after treatment of combined, complete (grade III) injuries of the anterior cruciate ligament (ACL) and medial collateral ligament (MCL).
Methods
A literature search of the following databases was completed using key words related to combined ACL and (MCL) tears: MEDLINE, Embase, Cochrane Controlled Trials Register, Cochrane Database of Systematic Reviews, Cumulative Index to Nursing and Allied Health Literature, and SPORTDiscus. Level I-IV studies that examined patients with complete tears of the ACL and grade III tears of the MCL, diagnosed by either magnetic resonance imaging or clinical examination of valgus instability, were included. Study inclusion was determined by 2 independent reviewers. Patient demographics, treatment choices, and patient outcomes, including clinical examination (i.e., range of motion, hamstring strength) and subjective assessments (i.e., International Knee Documentation Committee, Lysholm scores, Tegner activity scores) were collected.
Results
Six possible treatment combinations were assessed. Good or excellent outcomes related to range of motion, knee stability, subjective assessments, and return to play were reported after ACL reconstruction regardless of MCL treatment. Those with combined ACL and MCL reconstruction returned to their previous level of activity at a high rate (range, 87.5%-90.6%) with low rates of recurrent valgus instability. Triangular MCL reconstruction with a posterior limb that serves to reconstruct the posterior-oblique ligament best-restored anteromedial rotatory stability of the knee when compared with anatomic MCL reconstruction (90.6% and 65.6%, respectively). Nonsurgical management of the ACL injury, regardless of MCL treatment, demonstrated low return to activity (29%) and frequent secondary knee injuries.
Conclusions
High rates of return to sport with low risk of recurrent valgus instability have been demonstrated after MCL reconstruction, and triangular MCL reconstruction can more effectively restore anteromedial rotatory instability compared with MCL repair. Restoration of valgus stability can be common after reconstruction of the ACL with or without surgical management of the MCL, although patients with grade III tibial-sided or mid-substance injuries were less likely to regain valgus stability with nonoperative treatment than femoral-sided injuries.
Level of Evidence
Level IV; systematic review of Level I-IV studies.
Combined anterior cruciate ligament (ACL) and medial collateral ligament (MCL) injuries are the most common pattern of multiligamentous knee injury.1 The ACL is a primary stabilizer against anterior tibial translation and rotatory instability of the knee, and it has limited ability to heal after a complete tear because it is an intra-articular structure.2 Therefore, tears of the ACL typically require reconstruction in patients with high levels of activity, in order to decrease the risk of further injury to the meniscus and articular cartilage.2 The MCL is a primary stabilizer against valgus stress of the knee, and, in contrast to the ACL, it is extra-articular and has the capacity to heal after injury and restore valgus stability. As a result, most grade I and II MCL injuries can be treated successfully without surgery in the setting of an ACL injury.3 Algorithmic nonoperative approaches have been proposed for grade I and grade II MCL injuries. Smyth and Koh4 suggests treating grade I and II MCL injuries nonoperatively and completing the ACL reconstruction once range of motion is recovered and the MCL has healed.
Grade III MCL injuries cause more severe valgus instability to the knee, and multiple operative and nonoperative treatment methods have been described for grade III injuries. Options in the literature range from nonoperative treatment in a brace, to primary MCL repair, to anatomic MCL reconstruction with autograft or allograft. Interest in surgical treatment of MCL injuries has grown more recently, in part because of the concern for increased stresses across the ACL graft in knees with residual valgus laxity, and therefore increased risk for ACL graft failure.5,6
A systematic review of combined ACL and MCL injuries was published in 2012; however, the literature at the time included very few studies of surgical management of MCL injuries, particularly MCL reconstruction.7 Therefore, the purpose of this systematic review is to examine the clinical outcomes and return to sport rates after treatment of combined, complete (grade III) injuries of the ACL and MCL. The authors of the current study hypothesized that there would be no significant difference between acute operative repair of the MCL in comparison with conservative treatment with delayed ACL reconstruction for a combined ACL and high-grade MCL injury of the knee.
Methods
This work was exempt from institutional review board approval. For this study, we sought to identify peer-reviewed publications that describe both the treatment and outcomes of complete ACL tears with concomitant grade III MCL tears. A literature search of the following databases was completed: MEDLINE, Embase, Cochrane Controlled Trials Register, Cochrane Database of Systematic Reviews, Cumulative Index to Nursing and Allied Health Literature, and SPORTDiscus. In order to include as many articles as possible, each database was searched using 1970-2020 as the publication dates. Each database was searched by 2 independent reviewers (M.L.W., C.C.) using a combination of the following key words: ACL and MCL, anterior cruciate ligament and MCL, ACL and medial collateral ligament, anterior cruciate ligament and medial collateral ligament, ACL and combined, anterior cruciate ligament and combined, MCL and combined, medial collateral ligament and combined, ACL and multiligamentous, anterior cruciate ligament and multiligamentous, MCL and multiligamentous, and medial collateral ligament and multiligamentous.
The search results were compiled separately by 2 independent reviewers (M.L.W., C.C.) before being combined; duplicates were then removed. The inclusion criteria were as follows: complete tears of the ACL, grade III tears of the MCL (diagnosed by either magnetic resonance imaging or clinical examination of valgus instability), minimum 6-month follow-up, English language, human subjects, and Level I-IV evidence. The exclusion criteria were as follows: partial ACL tears and/or ACL repair (not reconstruction), grade I or grade II MCL tears, data not stratified by MCL tear grade, concomitant tears of PCL or LCL, diagnosis of a knee dislocation, diagnosis of a knee fracture or avulsion injury, pediatric patients, open physes, or no documented treatment or follow-up. Two independent reviewers (M.L.W., C.C.) examined the articles first by title, then by abstract, and finally by full text. After each phase of examination, each reviewer’s list of included articles was compared. If a discrepancy between the lists existed, the article was reexamined to assess for inclusion with the principal investigator (K.B.F.) ultimately deciding upon inclusion or exclusion. During examination of abstracts, if an abstract was not readily available, the full text was reviewed instead. Once an article was determined to meet the inclusion criteria, the citations of said article were thoroughly examined for completeness.
Once a list of included articles was compiled, the methods, results, and discussion of each article were examined. Study quality was assessed using the Modified Coleman Methodology Score. Data of interest included patient demographics, surgical and nonsurgical management, surgical complications, time from injury to surgery, rehabilitation regimen, and patient outcomes, including clinical examination (i.e., range of motion, hamstring strength) and subjective assessments (i.e., International Knee Documentation Committee [IKDC], Lysholm scores, Tegner activity scores). Data from each article was extracted by 2 independent reviewers (M.L.W., C.C.) to ensure accuracy and stored in a separate file. Articles were then grouped by treatment modality for ease of comparison. Common data across studies were not combined for a specific treatment modality as the result of variability in data presentation.
Results
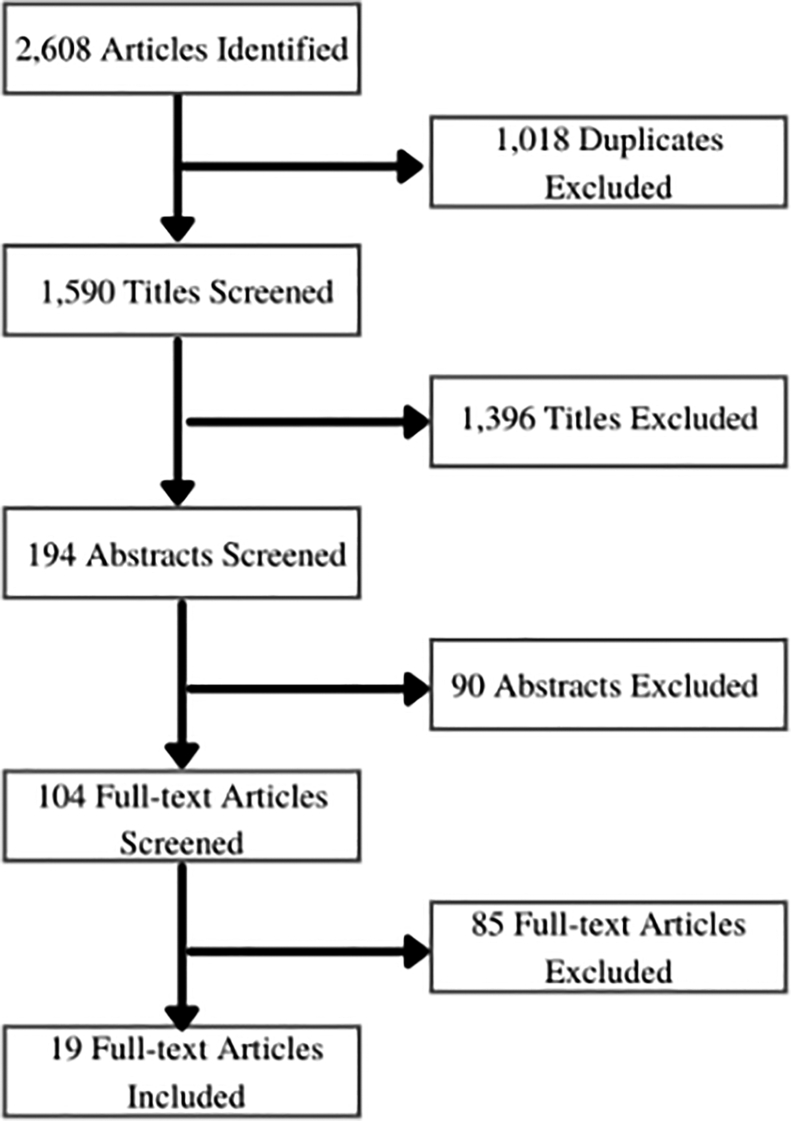
The initial search produced a total of 2,608 articles. This number was reduced to 1,590 articles after removal of duplicates. After review of the articles, application of inclusion and exclusion criteria, and examination of references, 19 articles were ultimately selected for inclusion, and 8 of these were comparative studies (Fig 1).2,8, 9, 10, 11, 12, 13, 14
Fig 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagram of article inclusion and exclusion.
Two studies were Level I, randomized controlled trials,8,10 but the same patient population was used for both studies. Therefore, these publications were considered as a single study for the purpose of this review. Two more studies were quasi-randomized controlled trials with Level II evidence.9,14 These studies were defined as quasi-randomized controlled trials due to the randomization being completed via allocation by order in which patients were recruited which has the potential for selection bias. A total of 4 cohort studies were included: 2 Level II prospective2,11 studies and 2 Level III retrospective studies.12,13 The remaining 11 studies were Level IV case series.15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 The mean Modified Coleman Methodology Score was 58.5 (range 34-91). In all, 6 different surgical treatment strategies were evaluated encompassing a total of 546 patients (mean 30 ± 20 patients). The 7 combinations of treatment included anterior cruciate ligament reconstruction (ACLR) with MCL reconstruction, ACLR and MCL repair, ACLR and MCL repair with allograft augmentation, ACLR and nonoperative MCL treatment, and nonoperative treatment of the ACL with either MCL reconstruction, MCL repair, or nonoperative MCL treatment. The mean follow-up was 35.58 ± 17.47 months (range 12-60 months) for all of the studies and the mean age was 29.63 years (range 22.8-40.3 years). Study summaries are found in the Table 1.2,8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25
Table 1.
Article Summaries
| Study | Level of Evidence | Groups | Patients | Outcome Measures | Results | Mean Follow-up (Range) | Coleman Methodology Score |
|---|---|---|---|---|---|---|---|
| Halinen et al., 20068 | Level I, RCT | 1: Early ACLR, MCL repair 2: Early ACLR, NSx MCL |
1: 23 (8 M, 15 F) 2: 24 (12 M, 12 F) |
ROM, AP laxity, valgus laxity, IKDC evaluation, Lysholm score, activity level, quadriceps muscle function, | No differences in ROM, AP laxity, IKDC score, Lysholm score, activity level, and quadriceps muscle function Valgus laxity greater in group 1 than group 2 |
27 mo (20-37 mo) | 78 |
| Halinen et al., 200910 | Level I, RCT | 1: Early ACLR, MCL repair 2: Early ACLR, NSx MCL |
1: 23 (8 M, 15 F) 2: 24 (12 M, 12 F |
Knee extension deficit, knee flexion, quadriceps muscle function | No differences in knee extension deficit Early knee flexion greater in group 2, but equal at final follow-up Early quadriceps muscle function greater in group 1, but equal at final follow-up |
27 mo (20-37 mo) | 78 |
| Dong et al., 20159 | Level II, quasi-RCT | 1: ACLR, anatomic ligament repair of the MCL 2: ACLR, triangular ligament reconstruction of the MCL |
1: 32 (18 M, 14 F) 2: 32 (19 M, 13 F) |
ROM, valgus laxity, anteromedial rotatory instability, IKDC score, return to sport, symptoms | No difference in ROM, valgus laxity, IKDC score, reported symptoms Incidence of anteromedial rotatory instability greater in group 1 Group 1 return to sport 87.5%, group 2 return to sport 93.8% |
34.2 ± 6.4 mo (24-48 mo) | 91 |
| Andersson et al., 199214 | Level II, quasi-RCT | 1: ACLR, MCL repair 2: NSx ACL, MCL repair |
1: 24 2: 28 |
AP laxity, Lysholm score, Tegner activity level, return to sport, hamstring and quadriceps strength, objective knee performance test | Greater AP laxity in group 2 Greater Lysholm score in group 1 (92 vs 87) Group 1 greater proportion with Tegner score >7 (50% vs 28%) Greater return to sport in group 1 (50% vs 29%) No difference in hamstring or quadriceps muscle strength Greater objective knee performance (hop test, figure eight run) in group 1 |
52 ± 8 mo (35-74 mo) | 66 |
| Nakamura et al., 200311 | Level II, prospective cohort | 1: ACLR, NSx MCL 2: ACLR and MCLR |
1: 11 2: 6 |
AP laxity, valgus laxity, IKDC evaluation | No difference in any outcomes Femoral-sided injury less likely to need MCLR than tibial injury |
64 mo (48-74 mo) | 64 |
| Petersen et al., 19992 | Level II, prospective cohort | 1: Early ACLR, NSx MCL 2: Late ACLR, NSx MCL |
1: 27 (15 M, 12 F) 2: 37 (18 M, 19 F) |
ROM, AP laxity, valgus laxity, Lysholm score, Tegner activity level, quadriceps strength | ROM greater in group 2 at 4.3 mo, but not at final follow-up No difference in AP laxity, valgus laxity, Tegner activity level, quadriceps strength Lysholm score greater in group 2 (85.3 vs 89.9) |
22 mo (18-30 mo; quadriceps strength measured at 4.3 mo) | 71 |
| Robins et al., 199312 | Level III, retrospective cohort | All had ACLR, MCL repair 1: Proximal MCL injury 2: Distal MCL Injury |
1: 13 (9 M, 4 F) 2: 7 (3 M, 4 F) |
Rate of recovery of extension and flexion, maximal flexion and extension | Faster rate of recovery of both extension and flexion in group 2 Maximal flexion greater in group 2 |
12 mo (2-30 mo) | 49 |
| Westermann et al., 201813 | Level III, retrospective cohort | 1: ACLR, MCL repair (2 patients had MCLR) 2: ACLR, NSx MCL |
1: 16 2: 11 |
KOOS subscale, IKDC evaluation, Marx activity score | No clinical difference in KOOS symptoms, pain, or ADL score KOOS sports/recreation and knee-related quality of life clinically greater in group 2 IKDC score clinically greater in group 2 (76.0 vs 87.6) Marx activity score greater in group 2 (6.5 vs 10.7) |
All patients completed 2-year follow-up | 60 |
| Ballmer et al., 199115 | Level IV, case series | ACLR, NSx MCL | 14 (9 M, 4 F) | ROM, AP laxity, valgus laxity, subjective results | 12 patients with full ROM 5 patients had >2 mm anterior tibial translation in 30° of flexion 1 patient had 3-5 mm anterior tibial translation in 70° of flexion 2 patients had 3-5 mm medial joint opening in 30° of flexion 5 patients had > 2mm anterior tibial translation in 20°-30° of flexion, 3 patients had 3-5 mm medial joint opening in 20°-30° of flexion 12 patients reported excellent results |
14 mo (12-19 mo) | 34 |
| Frolke et al., 199816 | Level IV, case series | NSx ACL, MCLR | 22 (10 M, 12 F) | IKDC evaluation, clinical examination | 22 patients with normal ROM 12 patients with normal or nearly normal subjective assessments 22 patients with abnormal or severely abnormal ligament examinations |
2.5 y (14-62 mo) | 45 |
| Jokl et al., 198417 | Level IV, case series | NSx ACL, NSx MCL | 28 (19 M, 9 F) | HSS knee assessment form, level of activity | 20 reported excellent-to-good results, 3 fair-plus, 5 fair-minus 19 returned to preinjury activity, 6 secondary injuries |
3 y (8 mo-11 y) | 50 |
| Kitamura et al., 201318 | Level IV, case series | ACLR, MCLR | 16 | ROM, AP laxity, valgus laxity, pivot shift, IKDC evaluation, Lysholm score | Mean flexion loss of 2.5 ± 2.6° Mean side-to-side difference in AP laxity at 20° of flexion was 1.5 ± 1.7 mm Mean side-to- side difference in AP laxity at 70° of flexion was 3.3 ± 4.8 mm Mean side-to-side difference of valgus instability at 20° of flexion was 0.9 ± 1.9 mm Overall IKDC grade A: 8, grade B: 8 IKDC valgus instability grade A: 13, grade B: 3 Lysholm score of 95.3 ± 3.9 |
All patients completed 2-y follow-up | 55 |
| Koga et al., 201119 | Level IV, case series | ACLR, MCL Repair | 14 | ROM, Valgus laxity | Less than 5° of extension and 10° of flexion deficits in all patients Valgus laxity at 0° of flexion negative in 13, +1 in 1 Valgus laxity at 30° of flexion negative in 8, +1 in 5, +2 in 1 |
All patients completed 2-y follow-up | 50 |
| Millett et al., 200420 | Level IV, case series | ACLR, NSx MCL | 12 | Valgus and rotational instability, Lysholm score, Tegner activity score | No valgus or rotational instability in any patient Lysholm score of 94.6 Tegner score of 8.4 |
45.6 mo (24-98 mo) | 42 |
| Noyes et al., 199521 | Level IV, case series | ACLR, MCL repair (2 patients had MCLR) | 34 (14 M, 20 F) | AP and valgus laxity, subjective rating, return to sport, hamstring and quadriceps muscle strength | 22 had <3 mm, 7 had 3-5.5 mm of AP displacement at 89 N 16 had <3 mm, 11 had >3 mm of AP displacement at 134 N 33 had 0-3 mm medial joint opening at 5° and 25° of flexion 19 reported good or excellent results 50% decreased level of sport participation 21 <20% deficit in quadriceps strength 23 <20% deficit in hamstring strength |
69 mo (24-107 mo) | 55 |
| Shelbourne et al., 199222 | Level IV, case series | ACLR, NSx MCL | 68 | ROM, Valgus laxity, AP laxity, subjective instability, return to sport, isokinetic testing | 69 patients with full ROM, 9 MUA for flexion loss and 5 scar resection for extension loss All had firm endpoints by valgus stress testing at 30° of flexion Mean of 2 mm difference in side-to-side AP laxity 96% without instability events 66% returned to prior level of competition 100% experienced return of strength |
2.3 y (1-5 y) | 61 |
| Shirakura et al., 200023 | Level IV, case series | NSx ACL, MCL repair | 14 (6 M, 8 F) | Valgus stress tests, Lysholm score, Tegner activity score, activity level, radiographic exam | 1 positive valgus stress test at 0° flexion and 9 positive valgus stress test at 30° of flexion Lysholm score 98.5 Tegner activity score of 5.2 11 of 12 patients in competitive or recreational activity postop 5 degenerative changes on postoperative imaging |
67.6 mo ± 30.1 mo | 54 |
| Yoshiya et al., 200524 | Level IV, case series | ACLR, MCLR | 12 (10 M, 2 F) | Valgus laxity, sagittal laxity, IKDC evaluation | 12 patients with normal or nearly normal ROM 12 patients with valgus laxity side-to-side difference <2 mm 10 patients with AP laxity <6 mm 11 patients with normal or nearly normal symptoms |
27 mo (24-28 mo) | 51 |
| Zhang et al., 201425 | Level IV, case series | ACLR, MCLR | 21 | ROM, valgus laxity, AP laxity, anteromedial rotatory instability, IKDC evaluation, return to activity | 95% full ROM Mean side-to-side AP laxity difference at 20° of flexion 0.8 ± 0.9 mm Mean medial joint opening of 0.80 ± 0.96 mm No anteromedial rotatory instability IKDC score of 87.7 ± 8.2 90% returned to preinjury activity level |
40 mo (26-61 mo) | 58 |
ACLR, anterior cruciate ligament reconstruction; AP, anteroposterior; F, female; HSS, Hospital for Special Surgery; IKDC, International Knee Documentation Committee; KOOS, Knee Injury and Osteoarthritis Outcome Score; M, male; MCL, medial collateral ligament; MCLR, medial collateral ligament reconstruction; MUA, manipulation under anesthesia; NSx, nonsurgical; ROM, range of motion.
Reconstruction of the ACL and MCL
Five studies examined outcomes after ACL and MCL reconstruction.9,11,18,24,25 Grafts used for MCL reconstruction included tibialis anterior allograft,9 Achilles tendon allograft,25 iliotibial band autograft or allograft,11 and hamstring tendon autograft.18,24 These studies demonstrate restoration of anteroposterior (AP) and valgus stability after MCL reconstruction, improved anteromedial rotatory stability compared with MCL repair in one study,9 with high rates of return to activity and minimal loss of range of motion. Finally, patients with a tibial-sided injury were more likely to require MCL reconstruction in one study.11
Dong et al.9 randomized 32 patients to ACLR combined with either anatomic ligament repair (ALR) of the MCL or triangular ligament reconstruction of the MCL. For evaluation of anteromedial rotatory instability, the Slocum test was carried out. Rotatory instability was lower after triangular ligament reconstruction (3 patients, 9.4%) than after ALR (11 patients, 34.4%). Nearly all patients gained full motion and an IKDC sports participation grade of A or B, but 2 patients who underwent ALR underwent a second surgery for ongoing valgus instability and 4 patients who underwent ALR required revision ACLR.
Nakamura et al.11 compared ACLR with ACLR and MCL reconstruction. All patients had at least 6 weeks of bracing before surgery, and those with residual valgus at time of ACLR underwent concurrent MCL surgery (5 reconstruction, 1 repair). The mean side-to-side difference in the medial joint opening among the patients who had ACLR and MCL repair was 6.6 mm (range 5-12 mm) at 30° of knee flexion. In total, 11 of 12 patients with isolated femoral insertion injury regained valgus stability before ACLR and all 5 patients with type III MCL lesions had diffuse injury patterns extending from the femoral attachment site over the joint line required MCL reconstruction. No tibial insertion site lesions were examined. Postoperative knee stability and function were similar in the 2 groups.
Three case series included 49 total patients who underwent ACL and MCL reconstruction.18,24,25 The mean side-to-side difference in valgus laxity ranged from 0.5 mm to 0.9 mm after reconstruction.18,24,25 Zhang et al.25 reported a reduction in anteromedial rotatory instability from 15 (71%) patients preoperatively to zero postoperatively. Full or nearly full range of motion was achieved postoperatively in almost all patients. Kitamura et al.18 and Yoshiya et al.24 reported that 100% and 91.7% of their patients had normal or nearly normal postoperative IKDC knee function, respectively. Zhang et al.25 found that 90.5% of patients returned to their preinjury level of activity.
ACL Reconstruction, MCL Repair
Five studies examined outcomes after ACL reconstruction combined with MCL repair.8, 9, 10,12,13 Outcomes after MCL repair were similar to outcomes after nonoperative treatment of the MCL. Proximal injuries that underwent repair had more difficulty regaining full extension than distal injuries.
Halinen et al.8,10 performed 2 randomized-controlled trials of ACLR and MCL repair versus ACLR alone. Postoperatively, the ACL-only group had greater valgus laxity than the ACL/MCL group (7.6 mm vs 6.3 mm, P = .024) but the side-to-side difference was not significant. The ACL-only group regained full flexion earlier than the ACL/MCL group, but most patients regained full motion in both groups with a maximum of 13° flexion loss in one patient at final follow-up. Functional scores were similar in both groups postoperatively and no ACL re-tears occurred in either group.
Westermann et al.13 also compared ACLR with or without surgical treatment of the MCL in a multicenter study group; 14 underwent MCL repair, 2 were reconstructed, and 11 MCL injuries were treated nonoperatively in a hinged brace. The location of the MCL tear was not associated with MCL treatment decision. Both groups had similar improvements in their IKDC and Knee Injury and Osteoarthritis Outcome Score, but scores in the ACL/MCL group were observed to be lower both pre- and post-operatively than the ACL-only group although it was found not to be statistically significant. Notably, the Marx activity rating scale was comparable at time zero with a statistically significant decrease in Marx score at 2-year follow-up (P = .04) for the ACL/MCL repair group compared with the ACL-only group. The authors concluded that the study results might have been more influenced by the severity of injuries in each group than by the treatment choice itself.
Robins et al.12 examined a series of patients who underwent ACLR with MCL repair, grouped based on the location of MCL injury. 13 MCL injuries were proximal to the joint line and 7 were distal. Distal injuries recovered full extension (116 vs 200 days) and full flexion (160 vs 204 days) more quickly than proximal injuries. Distal injuries also had significantly greater maximum flexion (138° vs 130°) at final follow-up. 5 patients with proximal injuries required additional surgery to achieve full range of motion.
ACL Reconstruction, MCL Repair With Allograft Augmentation
Two studies examined outcomes after ACL reconstruction combined with MCL repair with allograft augmentation,19,21 Outcomes after MCL repair were similar to outcomes after nonoperative treatment of the MCL, although some patients who underwent repair in these studies required additional allograft augmentation because of poor quality MCL tissue.
Koga et al.19 found that 7 of 14 patients who underwent ACLR with MCL repair required allograft augmentation of the MCL because intraoperative valgus stability was insufficient after MCL repair. When comparing MCL repair to non-operative management, this study did not show any differences with respect to subjective function of the knee postoperative stability, return to activities, Lysholm score and overall IKDC evaluation. Rather, range of motion and muscle power were better in the nonoperatively treated group.
Noyes et al.21 examined ACLR with MCL repair (26% femoral, 53% tibial, 21% midsubstance) and found that 2 of 34 patients required allograft augmentation due to the quality of remaining MCL tissue. 31 of 33 previously active patients returned to sport but only 8 (23%) returned to their prior level of activity.
ACL Reconstruction, Nonoperative Management of the MCL
Eight studies examined outcomes after ACLR and nonoperative management of the MCL.2,8,10,11,13,15,20,22 These studies are small and not comparative with other treatment strategies, but the largest study reported that approximately 20% of patients had postoperative valgus laxity regardless of timing of treatment.
Petersen et al.2 compared early (<21 days) versus late (10-12 weeks) ACL reconstruction with nonsurgical MCL treatment. 20% of early treatment and 23.3% of late treatment patients had a positive postoperative valgus stress test. Patients who underwent early surgery were more likely to have flexion and extension deficits in the early postoperative period but not at final follow-up (mean 22 months). Lysholm scores were significantly higher in the late ACLR group.
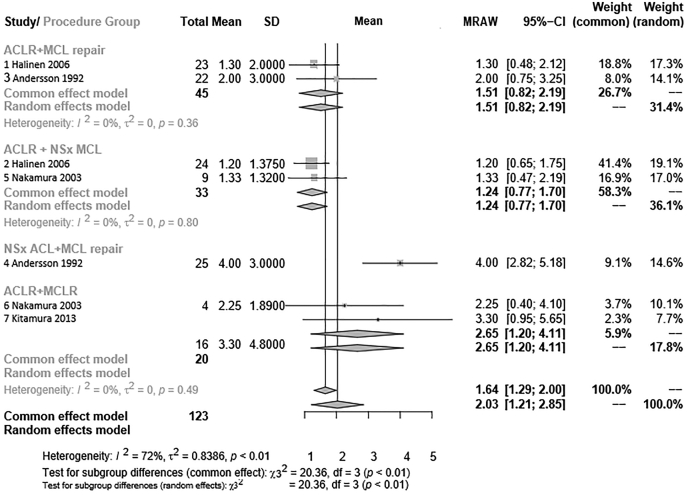
Three case series included a total of 94 patients after isolated ACLR and nonoperative MCL treatment. All three studies reported that valgus and AP laxity were adequately restored in their patients15,20,22 (Fig 2). Shelbourne and Porter22 found that average final range of motion was nearly normal, but 9 patients required manipulation under anesthesia for flexion deficits and 5 patients required scar excision for extension deficits. 95% of patients treated nonoperatively returned to their pre-injury level of sport in one study,22 and no ruptures of the ACL graft were reported in any of the studies.
Fig 2.
Forest plot for studies that reported mean anteroposterior laxity. (ACLR, anterior cruciate ligament reconstruction; CI, confidence interval; MCL, medial collateral ligament; MCLR, medial collateral ligament reconstruction; MRAW, raw mean difference; NSx, nonsurgical; SD, standard deviation)
Nonoperative Management of the ACL, MCL Reconstruction
Frolke et al.16 examined 22 patients after nonoperative treatment of the ACL with MCL reconstruction at an average of 7 days postinjury and found that nonoperative ACL treatment led to ongoing AP knee laxity. All patients had less than 5 mm of medial joint opening postoperatively but 16 patients continued to have at least 6 mm of AP laxity at 25° and 70° of flexion and had a 2+ pivot shift exam. Only 42% of patients reported normal outcomes on postoperative IKDC evaluation.
Nonoperative Management of the ACL, MCL Repair
Andersson and Gillquist14 examined functional outcomes after MCL repair with either augmented ACL repair or nonsurgical treatment of the ACL and reported significantly lower Lysholm scores in the MCL-only group compared with the ACL/MCL group. Shirakura et al.23 reported on a series of patients who underwent nonoperative ACL treatment with MCL repair. Both studies found improvement in valgus laxity but ongoing AP laxity compared with the contralateral knee. Return to activity was poor in both studies; 29%14and 40%23 of patients returned to competitive activities after nonoperative ACL treatment, while 50% of patients who underwent ACL repair and MCL repair returned to sport in the study from Andersson and Gillquist.14 Both studies concluded that surgical management of the ACL is the primary driver of improved outcomes, regardless of MCL treatment.
Nonoperative Management of the ACL and MCL
Jokl et al.17 examined 28 patients at an average of 3 years after nonoperative management of the ACL and MCL and found a high rate of secondary knee injury. In total, 68% of patients reported a return to their previous level of activity, but of the 19 patients who returned to sports, 6 had a secondary injury during the study period. Four had meniscus injuries that required surgery and two had recurrent MCL injuries.
ACLR With MCL Treated Operatively Versus ACLR With MCL Treated Nonoperatively
Halinen et al.8 directly compared patients with combined ACL and grade III MCL injury who underwent either operative or nonoperative treatment of the MCL. They found that the nonoperative treatment of the MCL led to results similar to those obtained with operative treatment, with respect to subjective function of the knee, postoperative stability, ROM, muscle power, return to activities, Lysholm score, and overall IKDC evaluation. In contrast, Nakamura et al.11 found that all of the patients diagnosed by magnetic resonance imaging with grade II injuries were successfully treated nonoperatively, and all those for whom nonoperative treatment was unsuccessful had grade III injuries.
Postoperative Outcomes
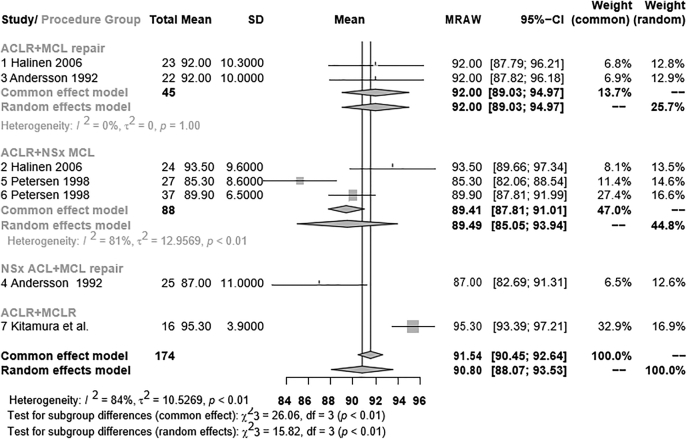
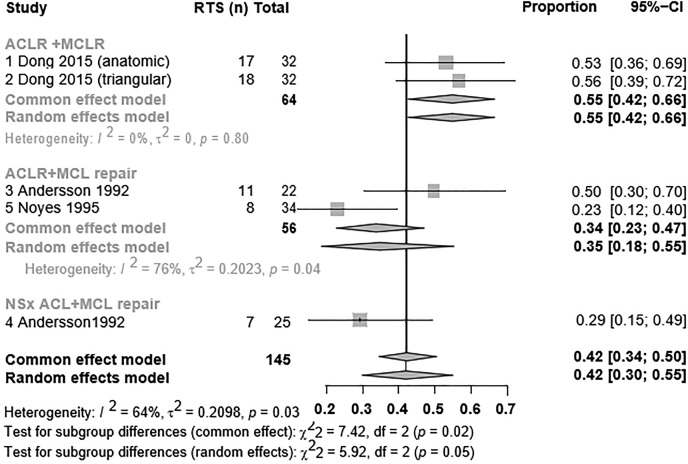
Forest plots were created to illustrate the results of the various procedural groups. In total, three sets of outcomes (AP laxity, Lysholm, and return to previous level of sport) were reported. The data showed significant heterogeneity in all of the studies evaluated (Fig 2, Fig 3, Fig 4). AP laxity was reported in 4 studies with 7 procedural groups (n = 123 patients) 8,11,14,18 (Fig 2). Lysholm score was also reported in 4 studies with 7 procedural subgroups (n = 174 patients). There was significant heterogeneity found amongst included studies that reported Lysholm score.2,8,14,18 (Fig 3). Return to sport was evaluated in 3 studies and 5 procedural subgroups (n = 145). Heterogeneity was also significant amongst these studies9,14,21 (Fig 4).
Fig 3.
Forest plot for studies that reported mean postoperative Lysholm score. (ACLR, anterior cruciate ligament reconstruction; CI, confidence interval; MCL, medial collateral ligament; MCLR, medial collateral ligament reconstruction; MRAW, raw mean difference; NSx, nonsurgical; SD, standard deviation)
Fig 4.
Forest plot for studies that reported mean return to previous level of sport. (ACLR, anterior cruciate ligament reconstruction; CI, confidence interval; MCL, medial collateral ligament; MCLR, medial collateral ligament reconstruction; NSx, nonsurgical; RTS, return to sport.)
Discussion
The results of our review suggest that those that undergo an MCL reconstruction have high rates of return to sport with low risk of recurrent valgus instability. Restoration of valgus stability can be expected after reconstruction of the ACL with or without surgical management of the MCL, although special attention should be given to grade III tibial-sided or midsubstance injuries. Triangular MCL reconstruction more effectively restores anteromedial rotatory instability when compared with MCL repair. When surgery is indicated, the quality of MCL tissue and stability at time of surgery should be given particular attention if a repair is chosen.
While concurrent tears of the ACL and MCL are a common pattern of multiligamentous knee injury, treatment of these injuries can be challenging because of the wide range of options and limited high-quality outcome data available in the literature. Reconstruction of the ACL has been established as the standard of care in these injuries, as in isolated injuries, because of the persistent instability and risk for secondary meniscal and chondral injuries that follow non-operative treatment of an ACL tear.17 This has been suggested consistently in previous studies as well as the results of the current systematic review, and therefore the primary focus of this review is the treatment of the concurrent MCL injuries.
Various treatment options have been published for the treatment of full-thickness MCL injuries, including nonoperative management in a brace, MCL repair at the site of injury, and MCL reconstruction. The indications, techniques, and outcomes of each of these options have been widely variable in the literature, and thus there is not a clear or consistent algorithm that has been used to aid in decision-making. Previous studies and systematic reviews have described an initial approach to treatment, which includes a period of nonoperative treatment in a brace to provide valgus stability to the knee while the MCL heals and full range of motion can be obtained before ACLR. At the time of ACLR, valgus stability can be assessed at 0 and 30 degrees either clinically and/or with stress radiographs, and those patients who have ongoing valgus laxity are those who ultimately require surgical treatment of the MCL. Nakamura et al.11 demonstrated that patients with isolated femoral insertion injuries are most likely to regain valgus stability with nonoperative treatment, and patients with injury throughout the rest of the ligament are much more likely to require additional stabilization.
When surgical treatment is necessary, the optimal choice of procedure is less clear and is the focus of the newer studies published in the last 10 years. Five new studies with 142 total patients were included in this review; 2 of these focused on MCL reconstruction, 2 focused largely on MCL repair, and 1 was a randomized controlled study of MCL reconstruction and repair. Dong et al.9 directly compared MCL repair with MCL reconstruction, and found that in 64 patients with a mean follow-up of 34 months there was no significant difference in clinical or radiographic valgus laxity between the two treatments. At follow-up, the incidence of anteromedial rotational instability in the MCL reconstruction group decreased significantly compared with that in the repair group (P < .05). Notably, the technique for MCL reconstruction in this study was a triangular ligament reconstruction with a posterior limb that serves to reconstruct the posterior-oblique ligament, and therefore the improvement in rotational instability may not be reproduced by other MCL reconstruction techniques that do not incorporate this posterior-oblique ligament limb. Another important finding was that 2 patients in the repair group and no patients in the reconstruction group required revision surgery for ongoing valgus laxity. Koga et al.19 did not directly compare outcomes between patients who underwent MCL reconstruction and MCL repair, but they did note that nearly one half of the patients in their series undergoing MCL repair required allograft augmentation of the MCL for continued valgus laxity in the operating room. The findings of these studies demonstrate the importance of evaluating MCL tissue quality and stability in the operating room if MCL repair is chosen, as this is a potential downside of attempted MCL repair instead of reconstruction.
Return to previous level of sport is another important goal of ACL and MCL treatment, and the most recent studies included in this review found that at least 85% to 90% of patients who underwent combined ACL and MCL reconstruction returned to their previous level of sport. Dong et al.9 found that 87.5% of MCL repair and 90.6% of MCL reconstruction patients had returned to their normal or near-normal level of sports, and Yoshiya et al.24 and Kitamura et al.18 found at least 90% of patients had normal or nearly normal knees on IKDC evaluation after MCL reconstruction. One important concept highlighted by Westermann et al.13 is that not all combined ACL and MCL injuries are equal, even those that are grade III injuries. Their study included patients in the MOON study group who underwent ACL reconstruction with either repair or non-operative treatment of the MCL injury. Patients in both groups had similar overall improvements in multiple domains of patient-reported outcome scores; however, the preoperative and postoperative scores in the MCL repair group were lower than in the non-operative MCL group,13 including Knee Injury and Osteoarthritis Outcome Score sports/recreation and knee-related quality of life scores. They pointed out that these findings are likely related to a difference in the severity of the initial injury, which led to patients with more severe injuries and greater laxity undergoing MCL repair than those who underwent nonoperative MCL treatment. This highlights the major challenge in evaluating nonrandomized studies of combined ACL and MCL injuries, as most are likely limited by selection bias and patients who undergo operative treatment likely tend to have more severe injuries. Future randomized studies may help to further elucidate the true differences between treatment types and help to further define the indications for each treatment.
Range of motion after combined ACL and MCL injuries has been frequently discussed in the literature, as patients with these injuries often have difficulty regaining full motion compared with patients with isolated ACL injuries, particularly those with proximal injuries. Halinen et al.10 demonstrated that patients randomized to MCL repair took longer to regain full motion than those randomized to nonoperative MCL treatment and were more likely to lack full flexion at final follow-up. Even with an improved understanding of the importance of motion after MCL injuries, the recent studies continue to identify patients who require additional surgery to restore full motion. Dong et al.9 identified 1 patient from the MCL reconstruction group who required an additional knee stiffness release procedure to restore full motion, and, although not significantly different, Westermann et al.13 identified 3 patients who required reoperation for arthrofibrosis in the ACL-MCL treatment group versus 1 patient in the nonoperative MCL and ACLR group. It may also be noteworthy to mention that there were no ACL failures in the nonoperative MCL group which obscures the relative impact of persistent valgus instability with a combined injury. These studies continue to highlight the importance of early mobilization and aggressive therapy in all patients with MCL injuries, but particularly those who undergo surgical treatment of the MCL.
Finally, Dong et al.9 found that 4 patients in their MCL repair group required revision ACL surgery during the follow-up period compared with none in the MCL reconstruction group. Although this was not necessarily statistically significant, it is an important finding that is worthy of future study. Most studies of combined ACL and MCL injuries are not powered to find significant differences in ACL reinjury rates based on the treatment of the MCL injury, and the follow-up time of most of these studies is also not long enough to detect many recurrent injuries. Because of these limitations, it is unknown how treatment choices for concurrent MCL injuries affect ACL reconstruction outcomes, but further study may help to identify the ideal MCL treatment choices for patients at high risk of ACL graft tear. Evident from the results of this review, and supporting the need for this study, is that various management strategies have been reported to date and a consensus within the literature is unclear.
This review demonstrates the need for additional studies of the management of full-thickness ACL tears with concomitant grade III MCL tears, as very few randomized trials currently exist. Another growing area of interest is suture augmentation with MCL repair or reconstruction, with ongoing studies of this technique that were not included in this review because they did not meet inclusion criteria, but are an interesting area of future study.
Limitations
By definition, the quality of systematic reviews are limited by the level of evidence of the studies that they include. In this review, only 4 of the 19 studies are randomized trials,8, 9, 10,14 and 2 of these Level I trials included the same patient population and were treated as one study.8,10 In addition, the variability of surgical techniques and inclusion criteria within each treatment category, as well as high variability in outcome reporting, prevented aggregation of data for meta-analysis and created significant challenges in the comparison of different treatment methods.
Conclusions
High rates of return to sport with low risk of recurrent valgus instability have been demonstrated after MCL reconstruction, and triangular MCL reconstruction can more effectively restore anteromedial rotatory instability compared with MCL repair. Restoration of valgus stability can be common after reconstruction of the ACL with or without surgical management of the MCL, although patients with grade III tibial-sided or mid-substance injuries were less likely to regain valgus stability with nonoperative treatment than femoral-sided injuries.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Cox C.L., Spindler K.P. Multiligamentous knee injuries—surgical treatment algorithm. N Am J Sports Phys Ther. 2008;3:198–203. [PMC free article] [PubMed] [Google Scholar]
- 2.Petersen W., Laprell H. Combined injuries of the medial collateral ligament and the anterior cruciate ligament: Early ACL reconstruction versus late ACL reconstruction. Arch Orthop Trauma Surg. 1999;119:258–262. doi: 10.1007/s004020050405. [DOI] [PubMed] [Google Scholar]
- 3.Lucidi G.A., Agostinone P., Grassi A., et al. Do clinical outcomes and failure rates differ in patients with combined ACL and grade 2 MCL tears versus isolated ACL tears? A prospective study with 14-year follow-up. Orthop J Sports Med. 2022;10 doi: 10.1177/23259671211047860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smyth M.P., Koh J.L. A review of surgical and nonsurgical outcomes of medial knee injuries. Sports Med Arthrosc Rev. 2015;23:e15–e22. doi: 10.1097/JSA.0000000000000063. [DOI] [PubMed] [Google Scholar]
- 5.Hewett T.E., Myer G.D., Ford K.R., et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 6.Svantesson E., Hamrin Senorski E., Alentorn-Geli E., et al. Increased risk of ACL revision with non-surgical treatment of a concomitant medial collateral ligament injury: A study on 19,457 patients from the Swedish National Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc. 2019;27:2450–2459. doi: 10.1007/s00167-018-5237-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant J.A., Tannenbaum E., Miller B.S., Bedi A. Treatment of combined complete tears of the anterior cruciate and medial collateral ligaments. Arthroscopy. 2012;28:110–122. doi: 10.1016/j.arthro.2011.08.293. [DOI] [PubMed] [Google Scholar]
- 8.Halinen J., Lindahl J., Hirvensalo E., Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: A prospective randomized study. Am J Sports Med. 2006;34:1134–1140. doi: 10.1177/0363546505284889. [DOI] [PubMed] [Google Scholar]
- 9.Dong J., Wang X.F., Men X., et al. Surgical treatment of acute grade III medial collateral ligament injury combined with anterior cruciate ligament injury: Anatomic ligament repair versus triangular ligament reconstruction. Arthroscopy. 2015;31:1108–1116. doi: 10.1016/j.arthro.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Halinen J., Lindahl J., Hirvensalo E. Range of motion and quadriceps muscle power after early surgical treatment of acute combined anterior cruciate and grade-III medial collateral ligament injuries: A prospective randomized study. J Bone Joint Surg Am. 2009;91:1305–1312. doi: 10.2106/JBJS.G.01571. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura N., Horibe S., Toritsuka Y., Mitsuoka T., Yoshikawa H., Shino K. Acute grade III medial collateral ligament injury of the knee associated with anterior cruciate ligament tear: The usefulness of magnetic resonance imaging in determining a treatment regimen. Am J Sports Med. 2003;31:261–267. doi: 10.1177/03635465030310021801. [DOI] [PubMed] [Google Scholar]
- 12.Robins A.J., Newman A.P., Burks R.T. Postoperative return of motion in anterior cruciate ligament and medial collateral ligament injuries: The effect of medial collateral ligament rupture location. Am J Sports Med. 1993;21:20–25. doi: 10.1177/036354659302100104. [DOI] [PubMed] [Google Scholar]
- 13.Westermann R.W., Spindler K.P., Huston L.J., et al. Outcomes of grade III medial collateral ligament injuries treated concurrently with anterior cruciate ligament reconstruction: A multicenter study. Arthroscopy. 2019;35:1466–1472. doi: 10.1016/j.arthro.2018.10.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andersson C., Gillquist J. Treatment of acute isolated and combined ruptures of the anterior cruciate ligament: A long-term follow-up study. Am J Sports Med. 1992;20:7–12. doi: 10.1177/036354659202000103. [DOI] [PubMed] [Google Scholar]
- 15.Ballmer P.M., Ballmer F.T., Jakob R.P. Reconstruction of the anterior cruciate ligament alone in the treatment of a combined instability with complete rupture of the medial collateral ligament: A prospective study. Arch Orthop Trauma Surg. 1991;110:139–141. doi: 10.1007/BF00395795. [DOI] [PubMed] [Google Scholar]
- 16.Frölke J.P., Oskam J., Vierhout P.A. Primary reconstruction of the medial collateral ligament in combined injury of the medial collateral and anterior cruciate ligaments. Short-term results. Knee Surg Sports Traumatol Arthrosc. 1998;6:103–106. doi: 10.1007/s001670050081. [DOI] [PubMed] [Google Scholar]
- 17.Jokl P., Kaplan N., Stovell P., Keggi K. Non-operative treatment of severe injuries to the medial and anterior cruciate ligaments of the knee. J Bone Joint Surg Am. 1984;66:741–744. [PubMed] [Google Scholar]
- 18.Kitamura N., Ogawa M., Kondo E., Kitayama S., Tohyama H., Yasuda K. A novel medial collateral ligament reconstruction procedure using semitendinosus tendon autograft in patients with multiligamentous knee injuries: Clinical outcomes. Am J Sports Med. 2013;41:1274–1281. doi: 10.1177/0363546513485716. [DOI] [PubMed] [Google Scholar]
- 19.Koga H., Muneta T., Yagishita K., Ju Y.J., Sekiya I. Surgical management of grade 3 medial knee injuries combined with cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2011;20:88–94. doi: 10.1007/s00167-011-1541-x. [DOI] [PubMed] [Google Scholar]
- 20.Millett P.J., Pennock A.T., Sterett W.I., Steadman J.R. Early ACL reconstruction in combined ACL–MCL injuries. J Knee Surg. 2004;17:94–98. doi: 10.1055/s-0030-1248204. [DOI] [PubMed] [Google Scholar]
- 21.Noyes F.R., Barber-Westin S.D. The treatment of acute combined ruptures of the anterior cruciate and medial ligaments of the knee. Am J Sports Med. 1995;23:380–391. doi: 10.1177/036354659502300402. [DOI] [PubMed] [Google Scholar]
- 22.Shelbourne K.D., Porter D.A. Anterior cruciate ligament-medial collateral ligament injury: Nonoperative management of medial collateral ligament tears with anterior cruciate ligament reconstruction. A preliminary report. Am J Sports Med. 1992;20:283–286. doi: 10.1177/036354659202000308. [DOI] [PubMed] [Google Scholar]
- 23.Shirakura K., Terauchi M., Katayama M., Watanabe H., Yamaji T., Takagishi K. The management of medial ligament tears in patients with combined anterior cruciate and medial ligament lesions. Int Orthop. 2000;24:108–111. doi: 10.1007/s002640000119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoshiya S., Kuroda R., Mizuno K., Yamamoto T., Kurosaka M. Medial collateral ligament reconstruction using autogenous hamstring tendons: Technique and results in initial cases. Am J Sports Med. 2005;33:1380–1385. doi: 10.1177/0363546504273487. [DOI] [PubMed] [Google Scholar]
- 25.Zhang H., Sun Y., Han X., et al. Simultaneous reconstruction of the anterior cruciate ligament and medial collateral ligament in patients with chronic ACL-MCL lesions: A minimum 2-year follow-up study. Am J Sports Med. 2014;42:1675–1681. doi: 10.1177/0363546514531394. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.