Abstract
Purpose
To evaluate the relationship between patient resilience and patient-reported outcome measures (PROMS) after primary anterior cruciate ligament (ACL) reconstruction.
Methods
Patients who underwent an ACL reconstruction by a single surgeon between January 2012 and June 2020 were identified by an institutional query using Current Procedural Terminology codes. Patients were included if they (1) underwent a primary ACL reconstruction and (2) had a minimum of 2 years’ follow-up. Data were retrospectively collected regarding demographics, surgical details, visual analog scale (VAS) scores, and 12-item short form survey (SF-12) scores. Resilience scores were obtained via the Brief Resilience Scale questionnaire. Stratification into low (LR), normal (NR), and high resilience (HR) was based on standard deviation from mean Brief Resilience Scale score to determine differences in PROMS between groups.
Results
One-hundred eighty-seven patients were identified by the institutional query. Of the 187 patients, 180 met inclusion criteria. Seven patients underwent revision ACL reconstruction and were excluded from the study. One-hundred three patients (57.2%) completed the postoperative questionnaire and were included. Patients in the NR group and HR group had significantly greater postoperative SF-12 scores (P < .001) and lower postoperative VAS pain scores (P < .001) when compared with those of the LR group. This trend was again shown with breakdown of the SF-12 into physical and mental aspects, each of which were significantly greater in either the NR group or HR group when compared with the LR group (P < .001). Overall, 97.9% and 99.0% of patients had changes in their SF-12 total and VAS pain scores respectively that exceeded the minimal clinically important difference for the cohort.
Conclusions
Patients with lower resilience scores have worse PROMs and increased pain than patients with greater resilience at a minimum of 2-year follow-up after ACL reconstruction.
Level of Evidence
Level IV, prognostic case series.
The anterior cruciate ligament (ACL) functions to resist anterolateral displacement of the tibia on the femur and is one of the most commonly injured structures of the knee. Despite the robust literature that exists regarding satisfaction and surgical outcomes after ACL reconstruction, there is little information regarding patient-reported outcome measures (PROMs) and the effect that psychological factors may have on these PROMS.
Historically, much of the literature regarding outcomes after ACL reconstruction has centered on patients’ physical factors, such as age, medical comorbidities, and body mass index with inferior outcomes demonstrated in smokers and those with elevated body mass index.1 More recently, there has been a transition to evaluating psychosocial health, which has a significant impact on both patient satisfaction and postoperative outcomes after a variety of orthopaedic procedures.2, 3, 4 The psychological aspects of recovery play a critical role in functional outcomes and issues related to “emotional disturbance, motivation, self-esteem, locus of control, and self-efficacy which can have profound effects on patients’ compliance, athletic identity, and readiness to return to sport.”5 A more well-rounded appreciation and understanding of these psychological concepts is critical to optimizing the treatment and outcomes of patients undergoing ACL reconstruction, which continue to have varied postoperative outcomes despite stable fixation. One of the more underappreciated psychometric factors that has garnered significant attention recently is “resilience” and its influence on postoperative recovery. Previous studies relating to arthroscopic surgery about the knee and shoulder have shown that patients with elevated resilience scores had superior postoperative functional outcome scores when compared with patients with low resilience.6, 7, 8 Knowing this, patient resilience may serve as a key facet to better understand varied outcomes despite reproducible, stable fixation strategies for ACL tears. In addition, resilience could serve as a key clinical stratification tool to understanding positive as well as suboptimal outcomes in patients undergoing surgical intervention. Recent literature has demonstrated that resilience is not significantly associated with return to sport; however, there has been no evaluation of the interplay of patient resilience and PROMs.9 The purpose of this study is to evaluate the relationship between patient resilience and PROMS after primary ACL reconstruction. Our hypothesis was that patients with low resilience scores would have inferior PROMs compared with their counterparts with normal and high resilience.
Methods
Following institutional review board approval (institutional review board no. G22008), a query was run to identify all patients who underwent ACL reconstruction for acute, traumatic, ACL tears from January 2012 to June 2020. Patients were included in the study if they (1) underwent a primary ACL reconstruction and (2) had a minimum of 2 years’ follow-up. Exclusion criteria consisted of (1) underwent revision ACL reconstruction, (2) did not meet the minimum of 2 years’ follow-up, (3) refused to fill out the questionnaire, or (4) were unable to be reached to fill out the questionnaire. Patients included in this study all underwent primary, arthroscopically assisted ACL reconstruction with various grafts including bone–patellar tendon–bone autograft, hamstring autograft, quadriceps tendon autograft, and allograft. Patient demographic data, prospectively collected preoperative visual analog score (VAS) pain (0-100 scale), and preoperative 12-item short form survey (SF-12) scores were recorded for each patient from chart review.
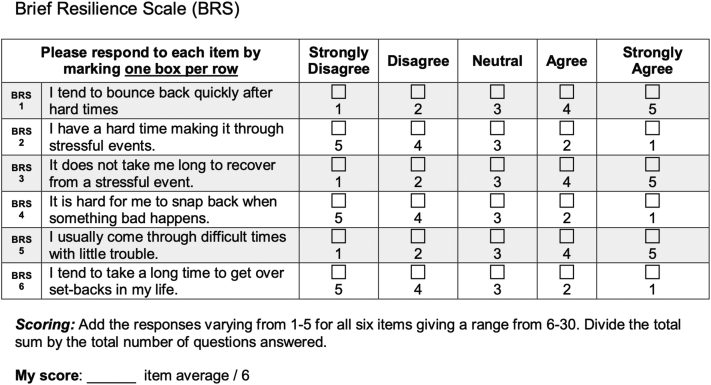
A postoperative survey was sent to all patients who met our inclusion criteria via secure Research Electronic Data Capture (REDCap). Those patients unable to be contacted via e-mail were followed up with a telephone interview. The survey included both consent for the patients agreeing to participate in the study itself, the Brief Resilience Scale (BRS), postoperative SF-12 questionnaire, and postoperative VAS pain score. The BRS is a 6-item Likert questionnaire with a mixture “of positively and negatively worded items,” that has been shown to be an accurate and reproducible means for measuring an individual’s level of resilience and is shown in Figure 1.10,11 All operative procedures were performed by a single sports medicine fellowship-trained orthopaedic surgeon (S.M.) at a single institution. All revision cases were excluded from analysis.
Fig 1.
Brief Resilience Scale (BRS) questionnaire.
Statistical Analysis
Statistical analysis on around patients being stratified based on resilience. Three groups were created: high resilience (HR), normal resilience (NR), and low resilience (LR) based on standard deviation from the mean. One standard deviation below the mean equated to LR group whereas one standard deviation above the mean placed patients into the HR group. Resilience scores between these 2 data points yielded a NR. Data analyses were performed with JMP Pro, Version 16.2.0 (SAS Institute Inc., Cary, NC). Statistical significance of differences between NR and LR patients or between HR and LR patients were estimated by t-tests. In addition, distribution-based cohort-specific minimal clinically important difference (MCID) values were calculated based off of standard deviations.12 Lastly, a post-hoc power analysis was completed.13
Results
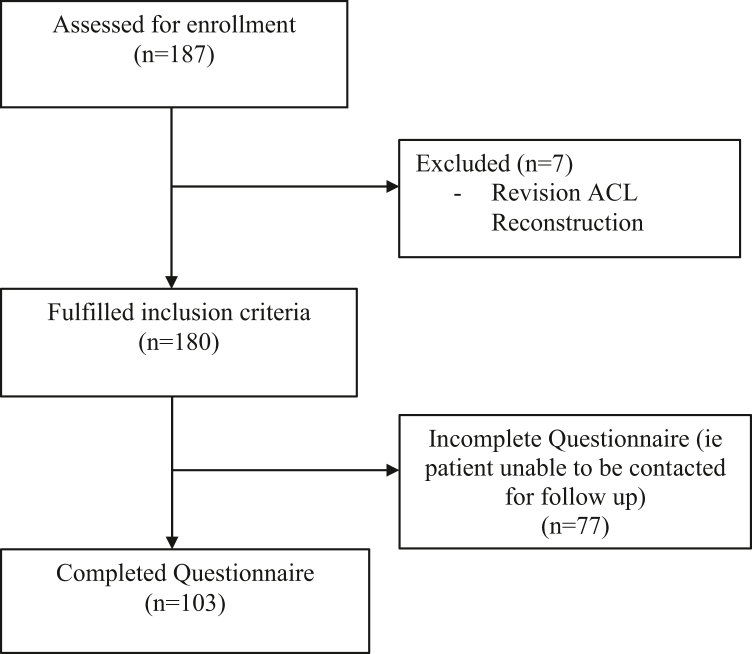
One-hundred eighty-seven patients were identified who underwent ACL reconstruction during the study period. Ultimately, 103 patients had complete data (were able to be contacted and completed the entirety of the survey) and were included in this study, for an inclusion rate of 57.2% (Fig. 2). The remaining 77 patients were either unable to be contacted via telephone or e-mail, or they declined to participate in the study. The mean BRS score for included patients was 21.9 (standard deviation = 4.1) with a range between 11 and 28 of a total possible 30 points. After statistical analysis, 20 patients were greater than one standard deviation below the mean and made up the LR group (n = 20, BRS: mean = 15.0, range 11-17). Similarly, those within one standard deviation of the mean accounted for the NR group (n = 66, BRS: mean = 22.8, range 18-25). Lastly, the subset of patients greater than one standard deviation above the mean for BRS score became the HR group (n = 17, BRS: mean = 26.6, range 26-28). The stratification employed for determining LR, NR, and HR groups was based on the previously described method employed by Dombrowsky et al.14 There were no significant differences in demographic data including patient age or sex across the 3 resilience groups (Table 1).
Fig 2.
Patient flow diagram showing the selection of the study sample. (ACL, anterior cruciate ligament.)
Table 1.
Patient Demographics Stratified According to Resilience
| Total | Low Resilience (LR) | Normal Resilience (NR) | High Resilience (HR) | P Value | |
|---|---|---|---|---|---|
| n | 103 | 20 | 66 | 17 | |
| BRS score | 21.9 (4.1) | 15.0 (1.8) | 22.8 (2.0) | 26.6 (0.7) | <.001 |
| Age at surgery, y | 31.1 (10.1) | 32.7 (11.1) | 31.4 (9.8) | 28.2 (10.1) | .370 |
| Sex | |||||
| Male | 63 (61.2%) | 10 (50.0%) | 41 (62.1%) | 12 (70.6%) | .425 |
| Female | 40 (38.8%) | 10 (40.0%) | 25 (37.9%) | 5 (29.4%) | .425 |
NOTE. Those values listed in parentheses without percentages are standard deviations for the data set. Those values listed in parentheses with percentages is the mean for the data set. P values <.05 in bold were deemed significant.
BRS, Brief Resilience Score.
Preoperative data demonstrated that those individuals with NR and HR had greater SF-12 Total scores of 73.5 and 78.0, respectively (P = .380 and P = .070). When the subscores of the SF-12 Total were further analyzed, it showed that patients in the NR and HR groups had significantly greater preoperative SF-12 mental component scores when compared with patients in the LR group (P < .001 and P < .001, respectively). Those patients in the NR group had an average preoperative SF-12 mental score of 46.2, whereas the HR group had an average of 51.8. This contrasts with the LR group, which had a preoperative SF-12 mental significantly lower with a mean of 40.8 (P < .001). SF-12 data are shown in Table 2.
Table 2.
Preoperative Versus Postoperative Results for SF-12 Scores (0-100)
| Brief Resilience Score (BRS) Groups | |||||||
|---|---|---|---|---|---|---|---|
| Low Resilience (LR) (Ref) N = 20 |
Normal Resilience (NR), N = 66 |
High Resilience (HR), N = 17 |
|||||
| Mean (SD) | Mean (SD) | t | P Value | Mean (SD) | t | P Value | |
| SF-12 Physical | |||||||
| Preoperative | 29.7 (3.7) | 30.8 (3.7) | 1.20 | .232 | 29.7 (3.3) | –0.00 | .998 |
| Postoperative | 39.9 (5.5) | 51.1 (6.1) | 7.89 | <.001 | 54.9 (2.3) | 8.21 | <.001 |
| ΔSF-12 Physical | 10.2 (6.5) | 20.3 (7.0) | 6.18 | <.001 | 25.3 (2.8) | 7.14 | <.001 |
| SF-12 Mental | |||||||
| Preoperative | 40.8 (4.2) | 46.2 (6.0) | 3.86 | <.001 | 51.8 (3.8) | 6.10 | <.001 |
| Postoperative | 48.1 (3.5) | 54.8 (4.2) | 6.79 | <.001 | 58.6 (2.8) | 8.20 | <.001 |
| ΔSF-12 Mental | 7.3 (5.7) | 8.9 (6.7) | 1.01 | .313 | 6.8 (3.9) | –0.24 | .812 |
| SF-12 Total | |||||||
| Preoperative | 70.5 (7.0) | 73.5 (14.3) | 0.88 | .380 | 78.5 (13.9) | 1.83 | .070 |
| Postoperative | 88.0 (8.2) | 105.9 (9.0) | 8.49 | <.001 | 113.5 (4.6) | 9.37 | <.001 |
| ΔSF-12 Total | 17.5 (10.8) | 29.2 (9.8) | 4.83 | <.001 | 31.9 (4.7) | 4.56 | <.001 |
| Power | 0.99 | 1.00 | |||||
NOTE. Those values listed in parentheses without percentages are SDs for the data set. P values <.05 in bold were deemed significant.
SD, standard deviation; SF-12, 12-item short form survey.
Preoperative VAS pain scores did not significantly differ among the 3 groups (P = .217 when LR compared with NR and P = .098 when LR compared with HR). However, postoperative VAS pain scores showed a statistically significant difference. Those individuals in the HR and NR contingents had a lower average VAS pain score at 6.9 (P < .001) and 15.7 (P < .003), respectively, than individuals in the LR group who had a mean postoperative VAS pain score of 28.5. VAS pain scores are tabulated in Table 3.
Table 3.
Preoperative Versus Postoperative Results for VAS Pain Scores (0-100)
| Brief Resilience Score (BRS) | |||||||
|---|---|---|---|---|---|---|---|
| VAS Pain |
Low (N = 20) |
Normal (N = 66) |
High (N = 17) |
||||
| Scores | Mean (SD) | Mean (SD) | t | P Value | Mean (SD) | t | P Value |
| Preoperative | 74.2 (13.9) | 69.3 (15.8) | –1.24 | .217 | 65.7 (21.4) | –1.67 | .097 |
| Postoperative | 28.5 (8.4) | 15.7 (10.3) | –5.39 | <.001 | 6.9 (5.1) | –7.03 | <.001 |
| ΔVAS Pain | –45.8 (16.1) | –53.8 (16.7) | –1.79 | .077 | -58.8 (21.0) | –2.27 | .025 |
| Power | 0.44 | 0.74 | |||||
NOTE. Those values listed in parentheses without percentages are standard deviations for the data set.
VAS, visual analog scale.
MCID values are tabulated in Table 4. As shown, the MCID for SF-12 Physical form yielded a result of 4.0 with 95.1% of the patient cohort reaching a change in score that was clinically significant (P < .001). Similarly, for the SF-12 Mental component, an MCID of 3.1 was demonstrated with nearly 82% of the cohort demonstrating a clinically significant change (P < .001). When the SF-12 total score was evaluated, the MCID was shown to be 5.3, with nearly 98% of patients in the study reaching a clinically important difference (P < .001). Lastly, VAS pain scores demonstrated an MCID of 8.8 with nearly 100% (99%) of the cohort demonstrated a significant difference (P < .001).
Table 4.
Minimal Clinically Important Difference in PROM Scores
| Mean (SD) | P Value | MCID | % of Cohort | |
|---|---|---|---|---|
| SF-12 Physical | 19.2 (7.9) | <.001 | 4.0 | 95.1% |
| SF-12 Mental | 8.2 (6.1) | <.001 | 3.1 | 81.6% |
| SF-12 Total | 27.2 (10.6) | <.001 | 5.3 | 98.0% |
| VAS | -53.0 (17.7) | <.001 | 8.8 | 99.0% |
NOTE. Those values listed in parentheses without percentages are standard deviations for the data set.
“Mean” indicates the mean PROM improvement score; “% of Cohort” indicates the percentage of patients with improvement scores greater than MCID.
MCID, minimal clinically important difference; PROM, patient-reported outcome measures; SD, standard deviation, SF-12, 12-item short form survey; VAS, visual analog scale.
Discussion
Our study demonstrated that patients with low resilience scores had significantly worse PROMs, postoperative pain, and overall patient satisfaction when compared with patients with normal or high resilience scores after ACL reconstruction. There was no significant difference between those individuals in the NR and HR groups when compared over the same aforementioned variables. Although most orthopaedic literature focuses on the physical components of a patient, these results highlight the validity of psychologic contributions to optimal patient outcomes. Arthroscopic surgeons performing ACL reconstructions must consider these patient characteristics throughout the perioperative time period to appropriately counsel and discuss potential outcomes with their patients. This study exhibits that resilience may be used as a tool to help physicians guide treatment and educate patients on what to expect after surgery.
Although the BRS is not specific to orthopaedic surgery, even elective surgery is considered a “stressful event.”15 Other studies have assessed the effect of resilience scores on patient outcomes after different types of orthopedic procedures.8,11,14,16,17 Low resilience scores have been directly correlated to worse PROMs, pain scores, and satisfaction after total knee arthroplasty, total shoulder arthroplasty, and reverse total shoulder arthroplasty.11,14,16 Outcome scores were reported up to 14 points lower for patients with low resilience when compared with patients with high resilience in reverse total shoulder arthroplasty, whereas patients with low resilience undergoing total shoulder arthroplasty scored as many as 30 to 40 points lower on traditional outcome scales. Similar results were seen in shoulder and knee arthroscopy.6,8 Active-military patients with high resilience undergoing shoulder and knee arthroscopy procedures not only demonstrated better early postoperative outcomes but also demonstrated faster return to duty after their surgeries. A critical difference of the current study in comparison with the aforementioned literature is the duration of follow-up with a minimum of 2 years after surgical intervention. Similar to the previously discussed studies, outcomes after ACL reconstruction were significantly diminished in the LR cohort when compared with the NR and HR populations, respectively. Interestingly, there was no significant difference among the patients with normal and high resilience. The lack of significant difference among the NR and HR groups may demonstrate that there is a threshold of resilience and after achieving this level one does not incur a statistically significant benefit in PROMS, postoperative pain, or overall satisfaction. Despite the lack of statistically significant difference, the clinical importance of improved patient resilience should not be lost. Although the values did not reach statistical significance, there was a trend for those patients in the HR cohort to have a larger change in their VAS pain scores and SF-12 physical scores with overall similar changes in their total SF-12 scores. Importantly, regardless of resilience score, the vast majority of patients had change in their total SF-12 scores and VAS pain scores significantly greater than the MCID (98.0% and 99.0%, respectively.) Resilience offers a measure of the biopsychosocial assets that military personnel and athletes can harness to bounce back from the injury, surgery, and rehabilitation.6,8,18
ACL tears can be detrimental to an athlete’s career and life. This can be shown by the preoperative SF-12 scores being significantly lower than postoperative scores. Although there was a significant difference in SF-12 scores among the LR cohort when compared with their NR and HR counterparts, VAS scores preoperatively did not demonstrate a significant difference. The lack of difference in preoperative VAS pain scores echoes the pain and discomfort associated with acute anterior cruciate ligamentous disruption regardless of one’s level of resilience. Commonly, there is a significant hemarthrosis in the acute setting that can cause significant pain until swelling is decreased.19 This contrasts with previously reported data in orthopaedic patients that showed individuals with decreased resilience scores had elevated preoperative pain levels and worse preoperative functional scores.17,20 Although ACL reconstruction is not a life-saving procedure, it is often required for patients to return-to-sport or return to preinjury activities effectively. Patients who choose ACL reconstruction over nonsurgical treatment for ACL tears report superior outcomes for knee symptoms and function, and in knee-specific and health-related quality of life.20 Undergoing this operation does not come without concern. Rigorous pre- and postoperative rehabilitation for 6 to 12 months is necessary for a successful surgical outcome.21, 22, 23 Patients face physical and psychologic barriers during the perioperative period, as well as when eventually returning to sport. Self-esteem levels and locus of control had significant relationships with functional test performance after ACL reconstruction.5 Patients who eventually returned to sport had significantly greater levels of self-esteem than those who did not return to sport.4 Depression, anxiety, mood, self-efficacy, catastrophizing, and kinesiophobia have also all been identified as factors hindering patients returning to sport after ACL reconstruction. Promising results have been shown for interventions aimed at addressing patients’ psychological obstacles.4,24,25
The physiological, psychological, social, and medicolegal factors that influence recovery are part of a biopsychosocial model that describes these complex interactions. Being cognizant of patient resilience and other psychosocial entities that may affect outcomes when not optimized is an important facet of holistic care in these patients undergoing ACL reconstruction. Studies have shown that with intervention such as cognitive-based therapy, resilience is thought to be a modifiable trait.26 Psychoeducation, cognitive-based therapy, and physical therapy or occupational therapy have been proposed to potentially improve patient resilience, as well as postoperative pain, anxiety, and depression.17,27,28 With multiple studies exhibiting a direct correlation between patients with low resilience and poor surgical outcomes, further investigation is warranted on preoperative screening and potential modifiable factors of resilience before and after orthopaedic surgeries to optimize outcomes. Whether resilience in the orthopaedic patient is truly a modifiable factor is yet to be fully understood; however, the interplay that low patient resilience has on inferior reported outcomes has been shown in multiple orthopaedic studies and is similarly demonstrated in the current study.
Limitations
This study is not without limitations. First, this was a retrospective study. Because data were used that was originally collected for other purposes, not all relevant information was available for every patient. Second, patients were recruited by convenience sampling and thus are prone to selection bias and may not represent the general population. In addition, the BRS was administered postoperatively and may have contributed to patients’ responses to the questionnaire. The BRS questionnaire was not administered to patients at the same postoperative date since the study period ran over a number of years, which could introduce recall bias into the study population. Patients with a perceived worse surgical outcome may have reported inferior BRS data. Of the 180 patients who met inclusion criteria, only 57.2% were available for administration of questionnaires. Given the response rate of the study, population transfer bias and nonresponder bias may be present in the remaining cohort. This study was also subject to recall bias, as PROMs were subjected and, at minimum, 2 years postoperative from their procedure. Confounding factors for negative outcomes were also not analyzed such as other medical comorbidities or baseline mental health illnesses. Anxiety, depression, substance abuse, and compliance with postoperative protocol may have influenced our data. Graft selection/type could contribute to donor-site morbidity and/or increased postoperative pain, potentially confounding the current data. Varied graft selection (which was based on available literature at the index procedure date) in the setting of this single-surgeon study could introduce confounding bias to this study’s findings. Further study should consider stratification based on graft type. Given the vast number of patient-reported outcome scores, VAS pain and SF-12 may not be as “knee-centric” as other scores. However, these aforementioned outcome scores are widely used and accepted in the literature as proxies for pain and functionality. Further study may consider the use of outcome scores focused on knee pathology, such as the Knee Injury and Osteoarthritis Outcome Score or the Tegner/Lysholm Knee Scoring Scale. Finally, this study was conducted using a single surgeon, and future data should be analyzed using multiple institutions and evaluated patients with combined injuries such as associated cartilaginous damage.
Conclusions
Patients with lower resilience scores have worse PROMs and increased pain than patients with higher resilience at a minimum of 2-year follow up after ACL reconstruction.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.MOON Knee Group. Spindler K.P., Huston L.J., et al. Ten-year outcomes and risk factors after anterior cruciate ligament reconstruction: A MOON longitudinal prospective cohort study. Am J Sports Med. 2018;46:815–825. doi: 10.1177/0363546517749850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Riediger W., Doering S., Krismer M. Depression and somatisation influence the outcome of total hip replacement. Int Orthop. 2010;34:13–18. doi: 10.1007/s00264-008-0688-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sinikallio S., Aalto T., Airaksinen O., et al. Depression is associated with poorer outcome of lumbar spinal stenosis surgery. Eur Spine J. 2007;16:905–912. doi: 10.1007/s00586-007-0349-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma A.K., Elbuluk A.M., Gkiatas I., Kim J.M., Sculco P.K., Vigdorchik J.M. Mental health in patients undergoing orthopaedic surgery: Diagnosis, management, and outcomes. JBJS Rev. 2021;9(7) doi: 10.2106/JBJS.RVW.20.00169. [DOI] [PubMed] [Google Scholar]
- 5.Christino M.A., Fantry A.J., Vopat B.G. Psychological aspects of recovery following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2015;23:501–509. doi: 10.5435/JAAOS-D-14-00173. [DOI] [PubMed] [Google Scholar]
- 6.Drayer N.J., Wallace C.S., Yu H.H., et al. High resiliency linked to short-term patient reported outcomes and return to duty following arthroscopic knee surgery. Mil Med. 2020;185:112–116. doi: 10.1093/milmed/usz180. [DOI] [PubMed] [Google Scholar]
- 7.Chavez T.J., Garvey K.D., Collins J.E., Lowenstein N.A., Matzkin E.G. Resilience as a predictor of patient satisfaction with nonopioid pain management and patient-reported outcome measures after knee arthroscopy. Arthroscopy. 2020;36:2195–2201. doi: 10.1016/j.arthro.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Shaha J.S., Shaha S.H., Bottoni C.R., Song D.J., Tokish J.M. Preoperative resilience strongest predictor of postoperative outcome following an arthroscopic Bankart repair. Orthop J Sports Med. 2017;5 (3_suppl 3) [Google Scholar]
- 9.Zhang J.K., Barron J., Arvesen J., Israel H., Kim C., Kaar S.G. Effect of patient resilience and the Single Assessment Numeric Evaluation (SANE) score on return to sport following anterior cruciate ligament reconstruction surgery. Arch Bone Joint Surg. 2021;9:512–518. doi: 10.22038/abjs.2021.48823.2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: Assessing the ability to bounce back. Int J Behav Med. 2008;15:194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 11.Tokish J.M., Kissenberth M.J., Tolan S.J., et al. Resilience correlates with outcomes after total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:752–756. doi: 10.1016/j.jse.2016.12.070. [DOI] [PubMed] [Google Scholar]
- 12.Simovitch R., Flurin P.H., Wright T., Zuckerman J.D., Roche C.P. Quantifying success after total shoulder arthroplasty: The minimal clinically important difference. J Shoulder Elbow Surg. 2018;27:298–305. doi: 10.1016/j.jse.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Cohen J. Ed 2. Routledge; Oxfordshire, UK: 2013. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 14.Dombrowsky A.R., Kirchner G., Isbell J., et al. Resilience correlates with patient reported outcomes after reverse total shoulder arthroplasty. Orthop Traumatol Surg Res. 2021;107 doi: 10.1016/j.otsr.2020.102777. [DOI] [PubMed] [Google Scholar]
- 15.Odom-Forren J., Reed D.B., Rush C. Postoperative distress of orthopedic ambulatory surgery patients. AORN J. 2017;105:464–477. doi: 10.1016/j.aorn.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Magaldi R.J., Staff I., Stovall A.E., Stohler S.A., Lewis C.G. Impact of resilience on outcomes of total knee arthroplasty. J Arthroplasty. 2019;34:2620–2623.e1. doi: 10.1016/j.arth.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 17.Otlans P.T., Szukics P.F., Bryan S.T., Tjoumakaris F.P., Freedman K.B. Resilience in the orthopaedic patient. J Bone Joint Surg Am. 2021;103:549–559. doi: 10.2106/JBJS.20.00676. [DOI] [PubMed] [Google Scholar]
- 18.Barcia A.M., Shaha J.S., Tokish J.M. The resilient athlete: Lessons learned in the military. Sports Med Arthrosc Rev. 2019;27:124–128. doi: 10.1097/JSA.0000000000000234. [DOI] [PubMed] [Google Scholar]
- 19.Spindler K.P., Wright R.W. Anterior cruciate ligament tear. N Engl J Med. 2008;359:2135–2142. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ardern C.L., Sonesson S., Forssblad M., Kvist J. Comparison of patient-reported outcomes among those who chose ACL reconstruction or non-surgical treatment. Scand J Med Sci Sports. 2017;27:535–544. doi: 10.1111/sms.12707. [DOI] [PubMed] [Google Scholar]
- 21.Carter H.M., Littlewood C., Webster K.E., Smith B.E. The effectiveness of preoperative rehabilitation programmes on postoperative outcomes following anterior cruciate ligament (ACL) reconstruction: A systematic review. BMC Musculoskelet Disord. 2020;21:647. doi: 10.1186/s12891-020-03676-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kruse L.M., Gray B., Wright R.W. Rehabilitation after anterior cruciate ligament reconstruction: A systematic review. J Bone Joint Surg Am. 2012;94:1737–1748. doi: 10.2106/JBJS.K.01246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Risberg M.A., Holm I. The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: A randomized controlled clinical trial with 2 years of follow-up. Am J Sports Med. 2009;37:1958–1966. doi: 10.1177/0363546509335196. [DOI] [PubMed] [Google Scholar]
- 24.Brand E., Nyland J. Patient outcomes following anterior cruciate ligament reconstruction: The influence of psychological factors. Orthopedics. 2009;32:335. doi: 10.3928/01477447-20090502-01. [DOI] [PubMed] [Google Scholar]
- 25.Ashton M.L., Kraeutler M.J., Brown S.M., Mulcahey M.K. Psychological readiness to return to sport following anterior cruciate ligament reconstruction. JBJS Rev. 2020;8 doi: 10.2106/JBJS.RVW.19.00110. [DOI] [PubMed] [Google Scholar]
- 26.Masten A.S. Resilience in developing systems: Progress and promise as the fourth wave rises. Dev Psychopathol. 2007;19:921–930. doi: 10.1017/S0954579407000442. [DOI] [PubMed] [Google Scholar]
- 27.Lim K.K., Matchar D.B., Tan C.S., et al. The association between psychological resilience and physical function among older adults with hip fracture surgery. J Am Med Dir Assoc. 2020;21:260–266.e2. doi: 10.1016/j.jamda.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 28.Yi-Frazier J.P., Smith R.E., Vitaliano P.P., et al. A person-focused analysis of resilience resources and coping in diabetes patients. Stress Health. 2010;26:51–60. doi: 10.1002/smi.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.