Abstract
Purpose
To assess clinical outcomes of patients who have undergone surgical repair of radial meniscal tears with reinforced suture bar (rebar) technique augmented with bone marrow aspirate concentrate.
Methods
This is a retrospective study of a single fellowship-trained sports medicine surgeon's experience on all patients who underwent a reinforced repair (rebar) of a radial meniscus tear from November 2016 to 2018, with a minimum of 12-month follow-up. Lysholm scores, IKDC (International Knee Documentation Committee) Subjective Knee Form scores, and Tegner scale were collected postoperatively at periods for at least 1 year and retrospectively studied.
Results
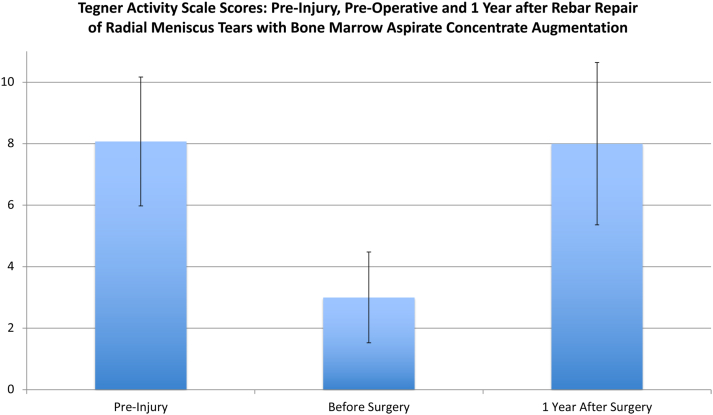
Patients were followed for an average of 36.3 ± 25.0 months [range: 12.0-69.0 months]. Pain scores improved from 6.1 ± 2.1 to 0.4 ± 1.4 at 1 year (P < .001). IKDC Subjective Knee Form scores improved from 63 ± 26 to 90 ± 13 (P = .021). Lysholm scores improved from 64 ± 28 to 94 ± 9 (P = .025). Based on a calculated minimal clinical important difference (MCID) of 1.5, 100% of patients had improvement above the MCID. In addition, 88% of patients had a 1-year IKDC Subjective Knee Form score above the patient acceptable symptomatic state. Preoperative Tegner activity scale improved from 3 ± 1.5 to 8 ± 2.6 (P = .007). Patients returned to their preinjury activity with little difference in the Tegner activity scale when we compared preinjury and 1-year postoperative (8.1 ± 1.3 vs 8.0 ± 2.6 respectively, P = .317).
Conclusions
The rebar repair technique for radial meniscus tears, with bone marrow aspirate concentrate augmentation, showed improved outcomes in both pain and function at minimum follow-up of 12 months. Patients were able to return to a high preinjury activity level by 1 year, and 100% of patients had improvement above the MCID and 88% met patient acceptable symptomatic state.
Level of Evidence
Level IV, therapeutic case series.
The meniscus serves a complex and vital role in the biomechanics of a healthy knee. It is an important stabilizer of the knee, while distributing load and serving as a shock absorber. It also serves to lubricate and distribute nourishment within the joint. With nearly 500,000 meniscus tears occurring in the United States each year, meniscus surgery has become one of the most frequently performed orthopaedic procedures.1 As a result of these numbers, numerous treatment options exist depending on the nature of the meniscal pathology.1, 2, 3
Radial meniscus tears can be particularly difficult to treat. Radial tears occur perpendicular to the circumferential fibers of the meniscus, partially or completely transecting the meniscus. With discontinuity of these circumferential fibers, radial meniscus tears significantly impair the normal function of the meniscus to absorb hoop stress and distribute tibiofemoral loading.4 Contact points across the tibiofemoral joint are then significantly altered, which may lead to articular cartilage degeneration and early-onset osteoarthritis.5, 6, 7 Historically, many radial meniscus tears were treated with meniscectomy.8 Unfortunately, without restoration of the meniscus’s ability to absorb hoop stresses and distribute load, many authors have found meniscectomy to provide undesirable outcomes.6,9 Accordingly, there has been increasing evidence focused on meniscus preservation and repair, especially in younger patients.6 With this emerging knowledge, there has been an increase in the number of meniscal repair surgeries performed in recent years.10,11
Treatment of radial meniscal tears are further complicated by technical and biological challenges. Goals of meniscal repair include an appropriate reduction and stabilization of the torn meniscus, which allows for healing and restoration of biomechanical function. At least a portion of many radial tears include the avascular white–white zone of the meniscus, which is known for its poor healing potential.10,11 This has led some surgeons to add augmented biologics such as fibrin clot or bone marrow–derived fibrin clot.12, 13, 14 As surgical technology continues to evolve, the optimal suture configuration to achieve our goals in meniscal repair are still under investigation. Horizontal mattresses, oblique sutures, reinforcing sutures, all-inside repairs, and transtibial tunnel repairs have been studied to assess patient outcomes, tear displacement after loading, overall load-to-failure, and other mechanical characteristics.15, 16, 17, 18
A previous biomechanical investigation demonstrated a significant improvement in load-to-failure using a novel technique, reinforced suture bar (rebar) repair, compared to standard parallel and cross stitch configurations.17,19 This study demonstrated a decrease in failures due to suture cut out.17 The purpose of this study was to assess clinical outcomes of patients who have undergone surgical repair of radial meniscal tears with the reinforced suture bar (rebar) technique augmented with BMAC (bone marrow aspirate concentrate). Our hypothesis was that patients would have improved functional outcomes and lower pain 1 year after rebar repair for radial meniscus tears with BMAC augmentation.
Methods
A retrospective review was completed on all meniscus repairs performed by a single fellowship-trained surgeon using Current Procedural Terminology codes 29882 and 29883 from November 2016 to November 2018 after institutional review board approval (STUDY00001235). Inclusion criteria were radial meniscus tears repaired with a rebar technique. Exclusion criteria were patients with grade 3 or 4 chondromalacia, fractures, associated root avulsions, parrot beak tears (any radial tears that also had a longitudinal tear component), patients with less than 12 months of follow-up, and repairs not done with adjunctive BMAC using the BioCue system (Biomet, Warsaw, IN). Demographic data were reviewed via a chart review and concomitant procedures such as anterior cruciate ligament (ACL) surgery were recorded.
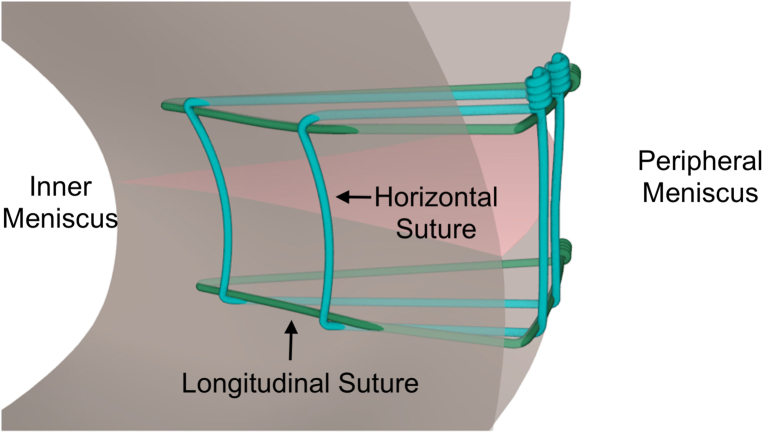
This technique is an arthroscopic reinforced suture repair performed in a standard inside-out fashion (Figs 1 and 2).17,19 The standard technique used four 2-0 nonabsorbable sutures, which are attached to meniscus needles (FiberWire; Arthrex, Naples, FL). Needle cannulas are then used to pass the needles (ZoneNavigator; Arthrex). The rebar repair consists of 2 vertical sutures, the reinforcement, and 2 parallel horizontal sutures (Fig 1). Two parallel vertical sutures are first placed on each side of the radial tear. Two additional sutures are then placed perpendicular to and crossing the radial tear, in juxtaposition to the vertical reinforcing sutures.19
Fig 1.
Illustration of an over-top view of a left lateral meniscus radial meniscus tear repair with a reinforced technique (rebar). The bottom of the figure is anterior. There are 2 parallel vertical sutures in dark green to act as reinforcing sutures. There are also 2 perpendicular horizontal sutures in blue juxtaposed to the reinforcing vertical sutures. The completed rebar repair is visualized with sutures tied on the capsular side.17,19
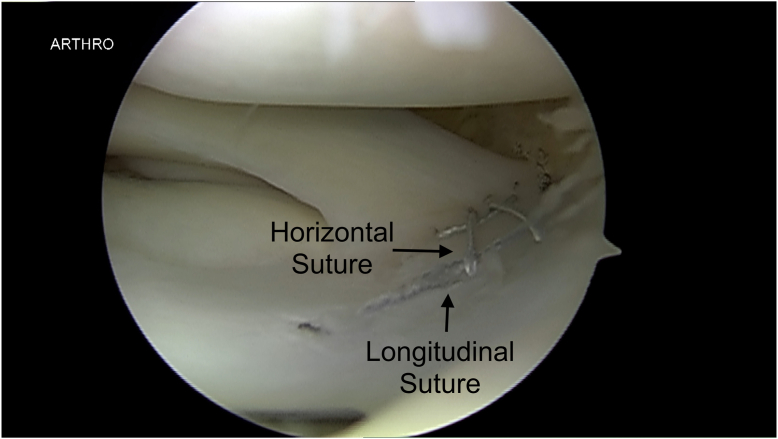
Fig 2.
Arthroscopic view through an anterolateral portal of a left knee lateral meniscus. The rebar repair has been completed. There are 2 parallel vertical sutures placed with 2 perpendicular sutures juxtaposed to the reinforcing vertical sutures.
For posterior based tears, a variation of this technique was done with all-inside devices (FAST-FIX 360; Smith & Nephew, Memphis, TN).
The bone marrow was obtained from a trocar inserted into the femoral notch and 25 cc was withdrawn into a mixture of 5 cc of anticoagulant citrate dextrose. After 15 minutes of centrifugation, 3 to 5 cc of BMAC was injected into the radial meniscus tear after final tying of the sutures and the repair was completed.
All patients received a standardized postoperative rehabilitation protocol. Patients wore a hinged knee brace for 6 weeks and were toe-touch weight bearing with crutches. Patients did physical therapy 2 times per week for range of motion and quadriceps sets. After 6 weeks, patients were advanced to full weight-bearing with basic closed chain exercises. After 4 months, patients were cleared for full-duty work or sports participation. Patients receiving an ACL reconstruction were not cleared until 9 months after surgery. Patients had a physical examination and clinical assessment at their postoperative visits and had incision checks at 1 and 2 weeks’ postoperative and physical examination tests at the follow-up intervals consisting of range of motion evaluation, knee effusion evaluation, and meniscus testing with McMurray’s test before work or sport clearance.
Preoperative pain, Lysholm, International Knee Documentation Committee (IKDC) Subjective Knee Form Score, and Tegner activity scale were collected in person by a physician assistant or resident physician, as well as postoperative scores at 1-week, 2-week, 6-week, 3-month, 6-month, and 12-month intervals.20, 21, 22 A subgroup analysis of outcomes was performed by categorizing patients who had concomitant ACL reconstruction and those who did not. Preinjury Tegner activity scale was also included for comparison. Pain was evaluated at rest using the Wong-Baker scale of 0-10 for subjective pain assessment.
Statistical Analysis
Based on a previous statistical analysis of radial meniscus repairs with a preoperative Tegner activity scale of 4 ± 0.7 and postoperative Tegner scale of 6.1 ± 1.3, the number needed to reach a power of 0.8 was 5.23 Minimal clinical importance difference (MCID) was calculated by 0.5 × standard deviation of the improvement of pain. The patient acceptable symptomatic state (PASS) used was 69 for the IKDC Subjective Knee Form score based on previous literature.24 As the data were determined to be nonparametric, preoperative and postoperative metrics were compared using a Wilcoxon signed rank test.
Results
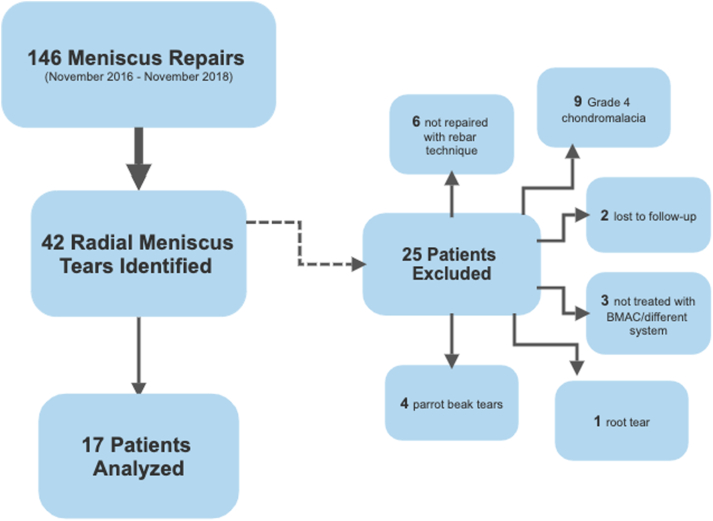
During the 2-year inclusion period, there were 146 meniscus repairs performed. After review of operative notes, there were 42 radial meniscus repairs identified. Six were excluded due to not being repaired with a rebar technique, 9 for grade 4 chondromalacia, 1 root tear, 4 parrot peak tears, 2 that were not treated with adjunctive BMAC, and 1 treated with a different BMAC system. Two repairs were lost to follow-up. This yielded 17 repairs in 17 patients for final inclusion (see Fig 3); 11 were male and 6 were female. Average time to follow-up was 36.3 months ± 25.0 [range: 12.0-69.0]. The average age of the patients was 23 ± 14 [range: 12-67]. Six (35%) of these patients had tears located on the medial meniscus, whereas 11 (65%) patients had lateral meniscus tears. Five of the lateral radial meniscus repairs had concomitant medial meniscus repairs and 1 of the medial radial repairs had a concomitant lateral meniscus repair. Also, there were 10 (61.1%) right knees repaired and 7 (38.9%) left knees repaired. Based on the location of the tear, different techniques were used with the same reinforced suture configuration. Eight (44.4%) patients had inside-out repairs for a mid-body tear; 8 (50%) had all-inside for posterior tears, and 1 (5.5%) had outside in for an anterior tear. Six (33.3%) of the patients had concomitant anterior cruciate ligament reconstruction performed at the same time as meniscal repair (Table 1). Other concomitant procedures were 1 loose body removal, 1 lateral collateral ligament reconstruction, and 1 chondroplasty.
Fig 3.
Flow chart illustrating the reasons for including and excluding patients for this study. (BMAC, bone marrow aspirate concentrate.)
Table 1.
Demographics, Laterality, Technique, and Concomitant Procedures for All Patients Included in the Study
| n | |
|---|---|
| Sex | |
| Male | 11 |
| Female | 6 |
| Laterality meniscus | |
| Medial | 6 |
| Lateral | 11 |
| Laterality knee | |
| Right | 10 |
| Left | 7 |
| Technique | |
| All inside | 8 |
| Inside-out | 8 |
| Outside- in | 1 |
| Associated ACLR | |
| With ACLR | 6 |
| Without ACLR | 11 |
| Age, y | |
| Mean | 23 [range: 12-67] |
| SD | 14 |
ACLR, anterior cruciate ligament reconstruction; SD, standard deviation.
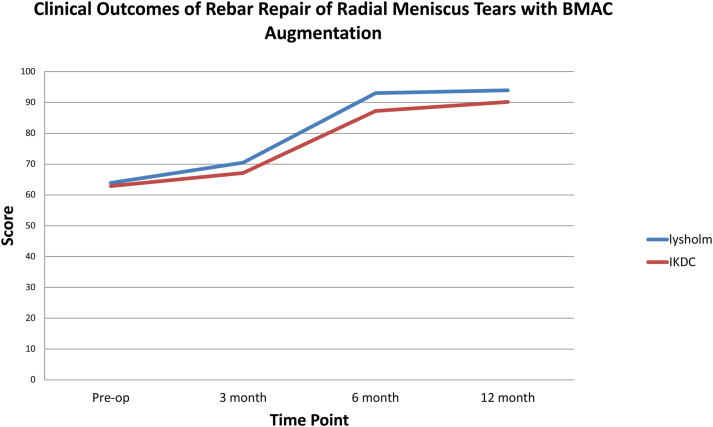
Overall, pain and functional scores improved after 1 year (Table 2). Pain scores improved from 6.1 ± 2.1 to 0.4 ± 1.4 at 1 year (P < .001). IKDC Subjective Knee Form scores improved from 63 ± 26 to 90 ± 13 (P = .021) (Fig 4). Lysholm scores improved from 64 ± 28 to 94 ± 9 (P = .025) (Fig 4). Based on a calculated MCID of 1.5, 100% of patients had improvement above the MCID. In addition, 88% of patients had a 1-year IKDC Subjective Knee Form score above the PASS.
Table 2.
Short-term outcomes of Radial Meniscus Repair With Rebar Technique and Adjuvant BMAC
| Preoperative |
3 Months’ Postoperative |
6 Months’ Postoperative |
12 Months’ Postoperative |
P Value∗ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | ||
| Pain | 6.2 | 2.1 | [5.9 - 6.5] | 1.2 | 1.5 | [1 - 1.5] | 0.1 | 0.3 | [0 - 0.1] | 0.4 | 1.3 | [0.1 - 0.6] | <.001 |
| Lysholm | 63.9 | 28 | [59.5 - 68.3] | 70.6 | 21.8 | [67.1 - 74] | 92.6 | 11.3 | [90.8 - 94.4] | 93.9 | 8.6 | [92.6 - 95.3] | .025 |
| IKDC | 62.9 | 26 | [58.7 - 67] | 67 | 22.4 | [63.4 - 70.6] | 88.3 | 11.9 | [86.4 - 90.2] | 90.2 | 13.2 | [88.1 - 92.3] | .021 |
BMAC, bone marrow aspirate concentrate; CI, confidence interval; IKDC, International Knee Documentation Committee Subjective Knee Form score; SD, standard deviation.
Preoperative vs 12-month postoperative.
Fig 4.
Outcomes after rebar radial meniscus repair augmented with bone marrow aspirate concentrate. International Knee Documentation Committee (IKDC) Subjective Knee Form score and Lysholm, increased over a 1-year postoperative period (P = .002 and P < .001, respectively). (BMAC, bone marrow aspirate concentrate.)
Preoperative Tegner activity scale improved from a mean of 3.0 ± 1.5 to 8 ± 2.6 (P = .007) (Fig 4). Patients returned to their preinjury activity level with no difference in the Tegner activity scale when comparing preinjury and 1-year postoperative (8.1 ± 1.3 vs 8.0 ± 2.6 respectively, (P = .317) (Fig 5). There was no difference in outcomes between male and female patients for pain, IKDC Subjective Knee Form score, Lysholm, and Tegner at the final follow-up (P = .48, = .41, = .06, and = .76, respectively). Range of motion was 1.9 ± 5.1 to 120.4 ± 51.4° preoperatively and 0.0 ± 0.0 to 130.4 ± 12.3° at final follow-up. There was no significant difference in preoperative versus final follow-up extension or flexion (P = .210 and P = .117, respectively).
Fig 5.
Tegner activity level after rebar radial meniscus repair augmented with bone marrow aspirate concentrate. Preinjury Tegner, before surgery and 1 year after surgery. Tegner scores improved significantly before and 1 year after surgery (P = .007). There was no significant difference in preinjury and 1-year postsurgery Tegner scores (P = .317).
A subgroup analysis was performed comparing the outcomes of patients with concomitant ACL reconstruction. Patients with rebar repair without ACL reconstruction had 1-year pain score of 0.67 ± 1.78, IKDC Subjective Knee Form score of 89 ± 15, Lysholm of 93 ±10, and Tegner of 7.6 ± 2.9, whereas rebar repair with ACL reconstruction had a 1-year pain score of 0 ± 0, IKDC Subjective Knee Form score of 91 ± 11, Lysholm of 96 ± 6, and Tegner of 9 ± 0. There was no significant difference between the rebar repair 1-year outcomes with or without ACL reconstruction for the pain scores, IKDC Subjective Knee Form score, Lysholm and Tegner scores (P = 1.000, P = .892, P = .892, and P = .317 respectively) (Table 3). The preoperative extension was 1.9 ± 5.1° and final extension was 0 ± 0. The preoperative flexion was 120.4 ± 51.4 and postoperative was 130.4 ± 12.3. There was no difference in preoperative versus postoperative extension or flexion (P = .21 and P = .12, respectively). During follow-up, 2 patients were found on palpation to have symptomatic postoperative effusions and were treated successfully with aspirations. There were no reoperations.
Table 3.
Rebar Repair Patient-Reported Outcomes 1-Year Postoperatively With or Without ACLR
| Meniscus Repair With ACLR | Meniscus Repair Without ACLR | P Value | |
|---|---|---|---|
| Pain | 0.0 ± 0.0 | 0.5 ± 1.8 | 1.000 |
| IKDC | 91.2 ± 11.2 | 89.6 ± 14.8 | .892 |
| Lysholm | 95.8 ± 6.1 | 82.8 ± 9.9 | .892 |
| Tegner | 9.0 ± 0.0 | 8.0 ± 3.0 | .317 |
ACLR, anterior cruciate ligament reconstruction; IKDC, International Knee Documentation Committee Subjective Knee Form score.
Discussion
Our study demonstrates favorable outcomes with the rebar repair technique for radial meniscus tears, showing improved IKDC Subjective Knee Form score, Lysholm, and Tegner activity scale outcomes from preoperative scores. Our study supports the idea that treating the meniscus with an appropriate technique for radial meniscus tears aids in meniscal healing which could have implications in preventing future knee degeneration. Patients were able to return to their preinjury level of activity with decreased pain by the 1-year follow-up appointment.
It has been demonstrated that patients with meniscal repairs, when compared with partial meniscectomy, have better outcomes in terms of functionality, Lysholm scores, KOOS scores, radiographic degeneration, and activity levels.25, 26, 27, 28 In a systematic review, Salata et al. and Paxton et al. also reported better Lysholm scores in those patients that were treated with repair rather than meniscectomy.29,30 Paxton et al.30 found that 100% of patients undergoing meniscal repair had excellent Lysholm scores versus only 54.2% who underwent partial meniscectomy. Salata et al.29 performed a systematic review, which reported that lateral meniscectomy was associated with the poorest post-operative outcomes when considering knee function, activity level, repeat surgeries, and instability when compared to medial meniscectomy. Meniscal absence, particularly the lateral meniscus, is known to significantly increase contact stresses across the joint; this leads to increased probability of osteoarthritis and poor outcomes associated with meniscectomy.4,29,31,32 Furthermore, a systematic review demonstrated superior radiographic and long-term subjective outcomes with complete meniscal repair.30 Although it has become accepted that meniscal preservation improves clinical outcomes, meniscal repair can be technically challenging. This can be especially true with repairs of radial meniscus tears, which subject the suture repair to significant stress leading to a continued search of the optimal repair technique for returning patients to their pre-injury level of performance.
Haklar et al.33 performed a study examining clinical results of patients undergoing radial meniscus tear repairs with 2 horizontal sutures using an inside-out repair. Five patients were followed postoperatively for an average of 31 months with clinical and magnetic resonance imaging (MRI) assessments taken. The results of the study revealed that all 5 patients were able to return to their preinjury level of activity and that the menisci were fully healed at the repair sites, as assessed with MRI. The mean Lysholm scores in that study were all improved from preoperative period to final postoperative follow-up (from 61.8 to 94.2; P = .029).33
Previous studies have evaluated the biomechanics and healing of this rebar repair mechanism and those similar to it.17,34, 35, 36, 37, 38 Nakata et al.35 and Tsujii et al.36 studied a reinforced repair similar to the rebar repair technique. Nakata et al.35 showed improved symptoms and decreased complaints of tibiofemoral joint symptoms at the 18-month follow-up with a success rate of 89%.35 This study used a fibrin clot similar to augmentation of BMAC. Although their study had a larger sample size and longer follow-up, they also included both radial and flap tears representing a more heterogenous group of tears. Also, 66% of patients showed complete healing on postoperative arthroscopic evaluation, and 28% had partial meniscal healing. Tsujii et al.36 performed second look arthroscopy on 18 consecutive patients with a similar technique finding 61% achieved full or partial healing, with more satisfactory results in patient whose tears extended into the vascular zone of the meniscus.35
Feltz et al.37 described a very similar repair technique with suture tapes for radial meniscus tears. This group employed use of suture tape in addition to the rebar technique, which aimed to decrease cutout of sutures during repair. The authors emphasized the need to consider meniscal collagen fiber orientation, illustrating that vertical sutures placed perpendicular to the collagen fibers seemed to reduce suture pull out.37
A study that used a novel technique referred to as the H-plasty for lateral meniscus posterior root tears used a similar backup suture repair method as in the rebar technique.37 This technique only uses one horizontal stich as compared with the rebar technique, which uses 2 stitches. The study reported an average increase in both the Lysholm score and the IKDC Subjective Knee Form score in patients from the preoperative period to the final postoperative appointment, with a minimum follow-up of 18 months. Respectively the Lysholm score increased from an average of 65.2 ± 4.5 to 93.3 ± 1.0 (P < .001) and the IKDC Subjective Knee Form score increased from 57.3 ± 9.9 to 83.2 ± 6.4 (P = .004). In total, 38 of the 47 patients underwent a second look arthroscopy at a minimum of 14 months postoperative showing complete healing of all meniscal root tears with satisfactory tension. The authors concluded that this backup suture repair technique showed improved clinical outcomes and a high rate of healing demonstrated on MRI.39
Using the rebar technique, all patients returned to their preinjury level of activity but were unable to obtain imaging to confirm complete healing in our patients due to the retrospective nature of this study. However, use of MRI for evaluation of meniscal tears has been reported only as sensitive as 92% for medial meniscal tears and 80% for lateral tears such that reimaging for healing is not well established.32 We also did not perform routine second-look arthroscopy at any interval during the study.
Radial meniscus tear repairs are challenging from a biomechanical viewpoint, but they also may be difficult to heal due to biologic reasons.12,40 Some surgeons have reported on various adjuvant treatments to augment repair of the avascular zone of the meniscus, such as fibrin clots or bleeding that occurs from ACL tunnels.12,13,40 These studies have demonstrated successful healing of these avascular areas both clinically and through imaging. All the patients in our study received adjuvant BMAC injected at the location of the tear, which may have also contributed to the successful outcomes.
ACL reconstructions have been associated with improved meniscal healing rates when performed in the same setting as meniscal repair.39 Our study included 6 of 17 patients who underwent ACL reconstruction in the same setting of rebar meniscal repair. Although it is felt that the release of growth factors in the synovial fluid are increased with ACL reconstructions,40 we did use BMAC for each patient, which is standard in our institution for meniscal repairs, to improve local biology for optimum healing. After subgroup analysis, we found no difference in outcomes with and without ACL reconstruction. Although this comparison is likely underpowered, similar outcomes with or without ACL reconstruction may be due to the use of BMAC in all patients in our study. Milliron et al.41 performed a meta-analysis looking at healing rate and patient reported outcomes of repair of radial meniscus tears. Multiple repair techniques were used, 7 of the studies assessed healing using second-look arthroscopy and found complete healing in 60-100%, and no healing evident in on 0- 13%.41 Patient-reported measures were also assessed in study from Milliron et al.,41 showing very promising result for patient reported outcomes for radial repair, including visual analog scale, IKDC Subjective Knee Form score, and Tegner activity scale scores.
Limitations
Limitations of our study include the study size, lack of comparison group and length of follow-up. Our study used a minimum follow-up of 12 months, which is under the length of time for meniscal repair failure to become evident. Also, due to our study being a retrospective case series, we had no comparison group. Other limitations include lack of independent assessment and lack of assessment of healing.
Conclusions
The rebar repair technique for radial meniscus tears, with BMAC augmentation, showed improved outcomes in both pain and function at minimum follow-up of 12 months. Patients were able to return to a high preinjury activity level by 1 year and 100% of patients had improvement above the MCID and 88% met PASS.
Acknowledgments
The authors acknowledge Baraa Shihadeh for the preparation of this manuscript.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Engler I.D., Moradian J.R., Pockros B.M., Schirmeister C.M., Richmond J.C., Salzler M.J. Patient-reported outcomes of meniscal repair and meniscectomy in patients 40 years of age and older show similar good results. Knee Surg Sports Traumatol Arthrosc. 2021;29:2911–2917. doi: 10.1007/s00167-020-06299-5. [DOI] [PubMed] [Google Scholar]
- 2.Garrett WE. American Board of Orthopaedic Surgery Practice of the Orthopaedic Surgeon: Part-II, certification examination case mix. J Bone Joint Surg Am. 2006;88:660. doi: 10.2106/JBJS.E.01208. [DOI] [PubMed] [Google Scholar]
- 3.Kim S., Bosque J., Meehan J.P., Jamali A., Marder R. Increase in outpatient knee arthroscopy in the United States: A comparison of national surveys of ambulatory surgery, 1996 and 2006. J Bone Joint Surg. 2011;93:994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 4.Ode G.E., Van Thiel G.S., McArthur S.A., et al. Effects of serial sectioning and repair of radial tears in the lateral meniscus. Am J Sports Med. 2012;40:1863–1870. doi: 10.1177/0363546512453291. [DOI] [PubMed] [Google Scholar]
- 5.Mcdermott I.D., Amis A.A., Biomechanics O., Engineering M. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88:1549–1556. doi: 10.1302/0301-620X.88B12.18140. [DOI] [PubMed] [Google Scholar]
- 6.Abrams G.D., Frank R.M., Gupta A.K., Harris J.D., McCormick F.M., Cole B.J. Trends in meniscus repair and meniscectomy in the United States, 2005-2011. Am J Sports Med. 2013;41:2333–2339. doi: 10.1177/0363546513495641. [DOI] [PubMed] [Google Scholar]
- 7.Baratz M.E., Fu F.H., Mengato R. Meniscal tears: The effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 8.Jeong H.J., MD, Lee S.H., MD, Ko, CS, MD Meniscectomy. Knee Surg Relat Res. 2012;24:129–136. doi: 10.5792/ksrr.2012.24.3.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beaufils P., Pujol N. Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res. 2017;103:S237–S244. doi: 10.1016/j.otsr.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Henning C.E., Lynch M.A., Clark J.R. Vascularity for healing of meniscus repairs. Arthrosc J Arthrosc Relat Surg. 1987;3:13–18. doi: 10.1016/s0749-8063(87)80004-x. [DOI] [PubMed] [Google Scholar]
- 11.Fox A.J.S., Wanivenhaus F., Burge A.J., Warren R.F., Rodeo S.A. The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin Anat. 2015;28:269–287. doi: 10.1002/ca.22456. [DOI] [PubMed] [Google Scholar]
- 12.Van Trommel M.F., Simonian P.T., Potter H.G., Wickiewicz T.L. Arthroscopic meniscal repair with fibrin clot of complete radial tears of the lateral meniscus in the avascular zone. Arthrosc J Arthrosc Relat Surg. 1998;14:360–365. doi: 10.1016/s0749-8063(98)70002-7. [DOI] [PubMed] [Google Scholar]
- 13.Hashimoto Y., Nishino K., Orita K., et al. Biochemical characteristics and clinical result of bone marrow–derived fibrin clot for repair of isolated meniscal injury in the avascular zone. Arthrosc J Arthrosc Relat Surg. 2022;38:441–449. doi: 10.1016/j.arthro.2021.05.026. [DOI] [PubMed] [Google Scholar]
- 14.Muckenhirn K.J., Kruckeberg B.M., Cinque M.E., et al. Arthroscopic inside-out repair of a meniscus bucket-handle tear augmented with bone marrow aspirate concentrate. Arthrosc Tech. 2017;6:e1221–e1227. doi: 10.1016/j.eats.2017.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhatia S., Civitarese D.M., Turnbull T.L., et al. A novel repair method for radial tears of the medial meniscus. Am J Sports Med. 2016;44:639–645. doi: 10.1177/0363546515615565. [DOI] [PubMed] [Google Scholar]
- 16.Branch E.A., Milchteim C., Aspey B.S., et al. Biomechanical comparison of arthroscopic repair constructs for radial tears of the meniscus. Am J Sports Med. 2015;43:2270–2276. doi: 10.1177/0363546515591994. [DOI] [PubMed] [Google Scholar]
- 17.Massey P., McClary K., Parker D., Barton R.S., Solitro G. The rebar repair for radial meniscus tears: a biomechanical comparison of a reinforced suture repair versus parallel and cross-stitch techniques. J Exp Orthop. 2019;6:38. doi: 10.1186/s40634-019-0206-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stender Z.C., Cracchiolo A.M., Walsh M.P., Patterson D.P., Wilusz M.J., Lemos S.E. Radial tears of the lateral meniscus-two novel repair techniques: A biomechanical study. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118768086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Massey P.A., McClary K., Sanders N., Myers M., Barton R.S., Solitro G. Rebar repair of radial meniscus tears: A reinforced suture technique. Arthrosc Tech. 2020;9:e953–e957. doi: 10.1016/j.eats.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garra G., Singer A.J., Domingo A., Thode H.C. The Wong-Baker Pain FACES scale measures pain, not fear. Pediatr Emerg Care. 2013;29:17–20. doi: 10.1097/PEC.0b013e31827b2299. [DOI] [PubMed] [Google Scholar]
- 21.Briggs K.K., Kocher M.S., Rodkey W.G., Steadman J.R. Reliability, validity, and responsiveness of the Lysholm Knee Score and Tegner activity scale for patients with meniscal injury of the knee. J Bone Joint Surg. 2006;88:698–705. doi: 10.2106/JBJS.E.00339. [DOI] [PubMed] [Google Scholar]
- 22.Higgins L.D., Taylor M.K., Park D., et al. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Joint Bone Spine. 2007;74:594–599. doi: 10.1016/j.jbspin.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 23.Rosner B. Cengage learning; 2015. Fundamentals of biostatistics. [Google Scholar]
- 24.Maheshwer B., Wong S.E., Polce E.M., et al. Establishing the minimal clinically important difference and patient-acceptable symptomatic state after arthroscopic meniscal repair and associated variables for achievement. Arthroscopy. 2021;37:3479–3486. doi: 10.1016/j.arthro.2021.04.058. [DOI] [PubMed] [Google Scholar]
- 25.Barber-Westin S.D., Noyes F.R. Clinical healing rates of meniscus repairs of tears in the central-third (red-white) zone. Arthroscopy. 2014;30:134–146. doi: 10.1016/j.arthro.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Stein T., Mehling A.P., Welsch F., Von Eisenhart-Rothe R., Jäger A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38:1542–1548. doi: 10.1177/0363546510364052. [DOI] [PubMed] [Google Scholar]
- 27.Xu C., Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: The more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015;23:164–170. doi: 10.1007/s00167-013-2528-6. [DOI] [PubMed] [Google Scholar]
- 28.Lutz C., Dalmay F., Ehkirch F.P., et al. Meniscectomy versus meniscal repair: 10 years radiological and clinical results in vertical lesions in stable knee. Orthop Traumatol Surg Res. 2015;101:S327–S331. doi: 10.1016/j.otsr.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 29.Salata M.J., Gibbs A.E., Sekiya J.K. A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med. 2010;38:1907–1916. doi: 10.1177/0363546510370196. [DOI] [PubMed] [Google Scholar]
- 30.Paxton E.S., Stock M.V., Brophy R.H. Meniscal repair versus partial meniscectomy: A systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27:1275–1288. doi: 10.1016/j.arthro.2011.03.088. [DOI] [PubMed] [Google Scholar]
- 31.Krause W.R., Pope M.H., Johnson R.J., Wilder D.G. Mechanical changes in the knee after meniscectomy. J Bone Joint Surg Am. 1976;58:599–604. [PubMed] [Google Scholar]
- 32.Peña E., Calvo B., Martinez M.A., Palanca D., Doblaré M. Why lateral meniscectomy is more dangerous than medial meniscectomy. A finite element study. J Orthop Res. 2006;24:1001–1010. doi: 10.1002/jor.20037. [DOI] [PubMed] [Google Scholar]
- 33.Haklar U., Kocaoglu B., Nalbantoglu U., Tuzuner T., Guven O. Arthroscopic repair of radial lateral menicus tear by double horizontal sutures with inside-outside technique. Knee. 2008;15:355–359. doi: 10.1016/j.knee.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 34.Milchteim C., Branch E.A., Maughon T., Hughey J., Anz A.W. Biomechanical comparison of parallel and crossed suture repair for longitudinal meniscus tears. Orthop J Sports Med. 2016;4(4) doi: 10.1177/2325967116640263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nakata K, Kanamoto T, Mae T, et al. New technique of arthroscopic meniscus repair in radial tears [published online January 1, 2012]. Sports Inj Prev Diagn Treat Rehabil. https://doi.org/10.1007/978-3-642-15630-4_41/COVER.
- 36.Tsujii A., Amano H., Tanaka Y., et al. Second look arthroscopic evaluation of repaired radial/oblique tears of the midbody of the lateral meniscus in stable knees. J Orthop Sci. 2018;23:122–126. doi: 10.1016/j.jos.2017.09.023. [DOI] [PubMed] [Google Scholar]
- 37.Feltz K., Brown A., Hanish S., Gan Y., Ma R. An arthroscopic-assisted radial meniscal tear repair using reinforced suture tape rebars and suture tapes. Arthrosc Tech. 2021;10:e1395–e1401. doi: 10.1016/j.eats.2021.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakanishi Y., Hoshino Y., Nagamune K., et al. Radial meniscal tears are best repaired by a modified “cross” tie-grip suture based on a biomechanical comparison of 4 repair techniques in a porcine model. Orthop J Sports Med. 2020;8(7) doi: 10.1177/2325967120935810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Z.Z., Zhou Y.F., Luo H., et al. A novel surgical technique for arthroscopic repair of type II posterior lateral meniscal root tear. Knee. 2020;27:1560–1566. doi: 10.1016/j.knee.2020.07.100. [DOI] [PubMed] [Google Scholar]
- 40.Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy. 2000;16:822–829. doi: 10.1053/jars.2000.19434. [DOI] [PubMed] [Google Scholar]
- 41.Milliron E.M., Magnussen R.A., A. Cavendish P., P. Quinn J., DiBartola A.C., Flanigan D.C. Repair of radial meniscus tears results in improved patient-reported outcome scores: A systematic review. Arthrosc Sports Med Rehabil. 2021;3:e967–e980. doi: 10.1016/j.asmr.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.