Abstract
Chronic traumatic anterior shoulder instability can be defined as recurrent trauma-associated shoulder instability requiring the assessment of three anatomic lesions: a capsuloligamentous and/or labral lesion; anterior glenoid bone loss and a Hill–Sachs lesion.
Surgical treatment is generally indicated. It remains controversial how risk factors should be evaluated to decide between a soft-tissue, free bone-block or Latarjet-type procedure.
Patient risk factors for recurrence are age; hyperlaxity; competitive, contact and overhead sports. Trauma-related factors are soft tissue lesions and most importantly bone loss with implications for treatment.
Different treatment options are discussed and compared for complications, return to sports parameters, short- and long-term outcomes and osteoarthritis.
Arthroscopic Bankart and open Latarjet procedures have a serious learning curve. Osteoarthritis is associated with the number of previous dislocations as well as surgical techniques.
Latarjet-type procedures have the lowest rate of dislocation recurrence and if performed correctly, do not seem to increase the risk of osteoarthritis.
Keywords: shoulder, instability, dislocation, Latarjet, Bankart, remplissage, bone block, bone grafting, arthroscopic stabilization
Introduction
Chronic traumatic anterior shoulder instability can be defined as recurrent instability having required glenohumeral reduction and being associated with a bony (Hill–Sachs or glenoid) or capsuloligamentous and labral lesion (Bankart and variants or humeral avulsion of glenohumeral ligament (HAGL)). Recurrent episodes may include further dislocations, symptomatic subluxations or apprehension. The clinical assessment, imaging and injury patterns were previously described in detail by Provencher et al. (1). It is caused by three anatomical lesions: (i) a capsulo-ligamentous and labral lesion; (ii) anterior glenoid bone loss and (iii) a Hill–Sachs lesion. They need to be assessed to decide on the surgical strategy (2). It is also important to assess patient risk factors (age, hyperlaxity and sports profile) (3). Proven risk factors for recurrence are as follows: young age < 20–25 years; bone loss; competitive, contact and overhead sports; as well as hyperlaxity associated with structural traumatic lesions (3). There is continuous international debate as to the indications for different treatment options, such as arthroscopic Bankart repair (4, 5, 6, 7, 8, 9, 10, 11, 12) with and without remplissage; free bone block procedures and coracoid transfer surgery (13, 14) with its most standardized technique, the Latarjet–Patte procedure modified by Walch (15). The purpose of this article is to review the current literature about risk assessment and prevention of recurrence, treatment options, their complications, return to sports (RTS) parameters, short- and long-term outcomes and rates of osteoarthritis.
Options for surgical treatment
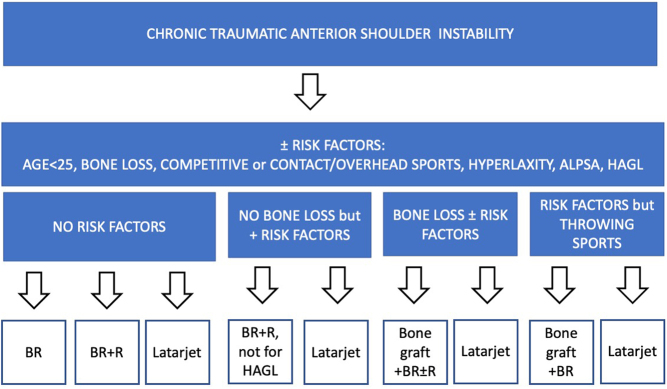
Indications for the following established surgical techniques according to risk factors and patient profile are shown in the flowchart in Fig. 1.
Figure 1.
Flowchart for indications of established surgical techniques according to risk factors and patient profile.
Arthroscopic Bankart repair with capsular shift (BR)
The arthroscopic technique is performed by releasing the capsuloligamentous complex and freshening up the insertion of the labrum. Capsule and labrum are then repaired with suture anchors to create an anatomical reconstruction (16). Lateral patient positioning has been reported to be advantageous for the performance and results of BR in a recent systematic review (17). The MOON shoulder group reported that surgeons using the lateral position for BR more frequently placed anchors in the inferior glenoid and at the 6-o'clock position, which are recognized as important to achieve a satisfactory repair (18). The MOON shoulder group also reported in their prospective study for anterior shoulder instability that the majority of patients (75.5%, 426 of 564) underwent BR as their surgical treatment (19).
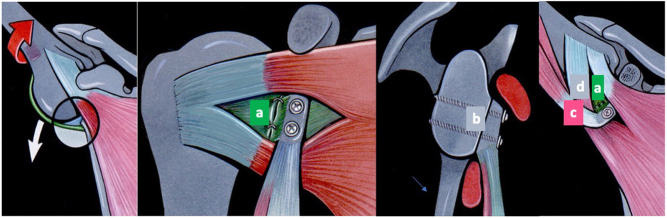
According to recent surveys, 90% of surgeons would use BR as the initial repair procedure in Germany, the Netherlands and Great Britain (20, 21, 22). When surgery was indicated, arthroscopic Bankart repair was the treatment of choice for 93% of survey participants in 2016 compared to 66% in a survey in 2001. For BR, knotless anchors were preferred by 72% of surgeons. For glenoid bone loss, only 46% of participants performed a glenoid bone augmentation procedure despite evidence of higher failure rates. For young patients with a first shoulder dislocation, the majority of survey participants listed arthroscopic BR as their first choice. High patient satisfaction and RTS have been documented after BR (7), but there is evidence of a high recurrent dislocation rate over time (Fig. 2) associated with risk factors (4, 11, 12).
Figure 2.
Recurrence of any instability as published by Gerber’s group (12).
Arthroscopic Bankart with Hill–Sachs remplissage (BR+R)
Wolf described the arthroscopic remplissage as a solution for the difficult problem of an engaging Hill–Sachs lesion by adding a Hill–Sachs remplissage procedure to a standard arthroscopic Bankart repair. The postero-superior capsule and the infraspinatus tendon are anchored and sutured in the Hill–Sachs lesion which is transformed into an extra-articular lesion preventing it from engaging at the antero-inferior glenoid rim (23).
A systematic review in 2020 compared BR+R with bone block augmentation (Latarjet) in patients with bipolar bone loss (24). In selected studies reporting 10–15% of mean glenoid bone loss, there was an increased rate of recurrent instability for BR+R (6.1–13.2%) compared to bony augmentation (0–8.2%). The recorded complication rate was lower in the BR+R group compared to bony augmentation. The authors conclude that BR+R should be reserved for engaging Hill–Sachs lesions (off-track) associated with glenoid bone loss of less than 10%.
A meta-analysis in 2018 concluded that isolated BR was significantly inferior to BR+R for recurrence of instability and redislocation. The authors were unable to comment on the postoperative range of motion (2).
In a retrospective cohort study, Feng et al. found a significantly higher RTS (100 vs 84.2%) and a return to the same level of sport rate (77.8 vs 50%) for patients who underwent arthroscopic Bankart repair with the addition of a remplissage procedure compared to patients with a Bankart repair alone (25). In 2020, Mac Donald et al. reported the results of a randomized controlled trial comparing arthroscopic Bankart repair with or without a remplissage for patients with a Hill–Sachs lesion of any size with glenoid bone loss of less than 15%, with a minimum follow-up of 2 years (26). Adding a remplissage significantly decreased the risk for recurrent dislocation from 18 to 4%.
Hurley et al. published a systematic review and meta-analysis showing lower rates of recurrent instability for BR+R over BR alone in patients with a Hill–Sachs lesion and subcritical glenoid bone loss. A significantly lower rate of complications was noted for the BR+R procedure compared to the Latarjet procedure (27). Analysis of the four studies included in Hurley’s meta-analysis reporting on the open Latarjet procedure revealed no difference in complication rates for the studies by Abouelsoud and Abdelrehman (28) and Bah et al. (29). Significant higher complication rates for the open Latarjet procedure were retrospectively reported for a Latarjet cohort of patients operated on by multiple fellowship-trained shoulder surgeons (30) and a second retrospective cohort (n = 35) of an open Latarjet–Patte technique from Korea without specification of the surgical experience and Latarjet expertise of the surgeons (31). Bah et al. compared patients with chronic instability and significant Hill–Sachs lesions treated with either BR+R or an open Latarjet procedure. There was no significant difference in recurrent instability but decreased external rotation (ER) and increased residual pain in the Bankart + Remplissage group (29). Therefore, BR + Remplisage is not recommended in throwers requiring maximal ER. Significant reduction of ER with the arm at side (ER1) and 90° abduction of the arm (ER2) was also found by Randelli et al. after adding an arthroscopic remplissage, but without influencing the patient’s sporting activity (32).
There is evidence that the addition of a remplissage increases the stability, reducing the risk of recurrence after an arthroscopic Bankart repair. Return to any sport and return to the same level of sport are also higher with the addition of a remplissage. There may be increased post-operative pain and stiffness with decreased rotation. When comparing BR+R to the Latarjet procedure, some authors recorded a lower number of postoperative complications for BR+R, but this may be biased by experience and expertise with the Latarjet procedure.
Free bone block procedures
Resch’s group from Salzburg, Austria, popularized the J-bone graft (33) for anatomical glenoid reconstruction in recurrent posttraumatic anterior shoulder dislocation with bone loss (34, 35, 36, 37). The J-graft is harvested from the iliac crest. A shoulder arthrotomy and tenotomy of the subscapularis tendon are followed by an osteotomy 5 mm medial to the glenoid rim, angled 30° to the glenoid plane with a 15 mm wide chisel prior to impacting the J-graft into the crevice offering primary stability in most cases (94%) without an additional screw (33). Moroder et al. published the long-term follow-up (minimum of 15 years) of 35 shoulders with excellent stability (1 dislocation), but 23% of patients had persistent apprehension. There was no instability arthropathy in 24 shoulders (69%), mild arthropathy in 23%, moderate arthropathy in 6% and severe arthropathy in 1 shoulder. A randomized controlled trial did not show a clinically relevant difference between a standardized open Latarjet procedure and the J-bone graft technique for a short follow-up time of a minimum of 2 years (38).
Scheibel et al. published on the arthroscopic reconstruction of glenoid bone loss with autologous iliac crest bone grafting, bioabsorbable screw fixation and labral as well as capsuloligamentous anchor repair (39). Mid- to long-term results with a minimum follow-up of 5 years showed recurrence of instability in 14% of patients, one recurrent dislocation (7%) and an average subjective shoulder value (SSV) of 87%. The same procedure with allograft showed a recurrence of glenoid bone loss of 14% after 1 year due to massive graft resorption associated with apprehension in 30% of patients and recurrence of instability in 10% of patients (40). So far, the arthroscopic autologous technique has not been shown to provide any advantage in instability symptoms and recurrence over open bone transfer procedures. Frank et al. reported similar clinical outcomes for their technique using fresh distal tibial allograft to a Latarjet procedure in a cohort study of 100 patients (41).
Latarjet–Patte with Walch’s technique
After 40 years of clinical practice with over 4000 procedures and publication of excellent long-term outcomes for different patient cohorts, the open Latarjet–Patte with Walch’s technique can be considered the most standardized of Latarjet procedures (15, 42, 43, 44, 45, 46).
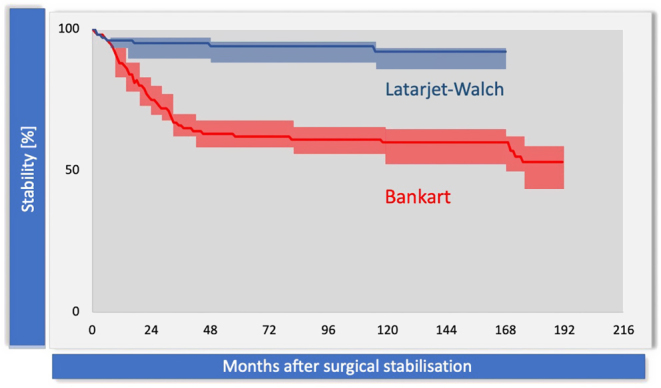
The procedure consists of a subscapularis split and coracoid transfer, which is placed flat on the anterior surface of the scapula with its broad flattened under surface and fixed with two screws (Fig. 3) (15). The coracoacromial ligament stump is repaired to the vertical anterior capsulotomy in ER of the arm. The procedure is intricate and has been standardized and broken up into key maneuvers and key stages (47) to prevent complications as several studies and a systematic review have shown an increased complication rate of non-standardized Latarjet–type procedures with variable techniques (48).
Figure 3.
Latarjet–Patte with Walch’s technique and stabilizing mechanisms. (A) Capsular repair to CAL. (B) Bone augmentation. (C) Sling effect by the conjoint tendon. (D) Hammock effect by the lower subscapularis.
Postoperative stability is attributed to a triple effect first described by Patte (49, 50):
Bone augmentation by the coracoid process (Fig. 3B),
Sling effect by the conjoint tendon and hammock effect (Fig. 3C and D) of the lower portion of the subscapularis and
Capsular repair with the coracoacromial ligament stump (Fig. 3A).
The procedure was modified by Walch who used a subscapularis split and two screws allowing for rotationally stable fixation of the bone block and immediate postoperative range of motion in ER (42). How the labrum and capsule are handled is subject to continuous debate (15). A capsular shift and labral repair are not required (51). Capsular repair to the glenoid or directly to the bone block has been advocated but may reduce ER (52, 53). Some authors prefer additional repair of the labrum to assure that the graft is extra-articular, combined with a capsular repair to the coracohumeral ligament (54). Several authors have shown that subscapularis function does not show a clinically important alteration after a Latarjet with subscapularis split (55, 56).
In 2000, Walch published a recurrent dislocation rate of 1% in a series of 126 patients with a 3-year follow-up (42). In 2011, the same recurrence rate for dislocations of 1% in over 2000 patients was reported for his patients (15). The RTS rate was 83%. Good or excellent satisfaction was reported for 98% of patients who self-rated their results. According to the modified Rowe score, 76% of patients achieved good or excellent results.
Gerber’s group used the Latarjet technique described by Walch (42) and reported a 1% dislocation recurrence (Fig. 2) at a minimum follow-up of 6 years (12). Gerber’s patients were equally satisfied as Walch’s patients with an SSV of 96.8 and 98%, respectively, and it has been shown that these results can be reproduced after fellowship training and meticulous standardization of the technique (47).
Procedure-specific complications
Bankart repair is frequently associated with a low short-term complication rate associated with mostly arthroscopic, cannula-based interventions with minimal risk for hematoma formation and infection. The surgical technique is widespread; however, low and correct anchor placement and low suture passage are technically demanding. It is therefore not surprising that the rate of osteoarthritis after BR is not inferior to other techniques (57), which is sometimes associated with ‘anchor arthropathy’ (Fig. 4A) due to a higher number of anchors, too far medialized drilling or proud anchors and suture material (58). Further complications include recurrent dislocations requiring revisions, especially in patients with risk factors (young age, bone loss and sports profile) (3, 13), leading to increased bone loss (59) and/or instability arthropathy (60) and inferior results after revision (61). Remplissage in addition to BR has been reported to reduce ER as an expected complication (29, 32). It should therefore not be used in throwing athletes.
Figure 4.
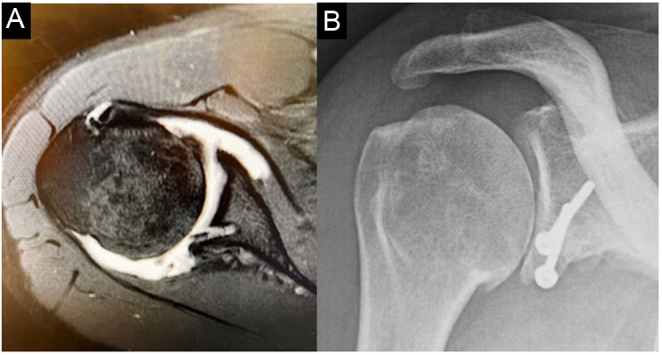
(A/B) ‘Anchor arthropathy’ (A) and arthropathy related to lateral Latarjet overhang (B).
Free bone block procedures can be performed with auto- or allograft. Graft resorption is a concern for allograft procedures (40) and the iliac-crest autograft is associated with donor-side morbidity (38). Placement of the graft is demanding. Since there are no additional sling and hammock effects, too much graft medialization can be associated with symptomatic instability and too much lateralization with the development of arthritis.
A systematic review of complications and re-operations after open and arthroscopic Latarjet and Bristow–Latarjet procedures was conducted by two sports medicine centers and published by Griesser and colleagues in 2013, including 45 studies. They included procedures with different modifications of coracoid transfer and found an overall complication rate of 30% (48). Over 1900 shoulders were included. The re-dislocation rate was 2.9%, the subluxation rate 5% and the re-operation rate 7% (removal of hardware making up 2.5% of the 7%). Mild loss of ER was common (mean loss: 11.7° for the open technique). Infection and hematoma formation were both below 1%. Bone block complications made up 14.1% (fracture: 1.5%; lysis: 3.2%; fibrous union: 9.4%). Neurovascular complications were seen in 1.8% and subscapularis rupture in less than 1%. These more serious complications have led some surgeons to avoid Latarjet procedures in favor of BR in patients at lower risk of recurrence.
The standardized Latarjet–Patte procedure modified by Walch provides a reliable strategy to prevent complications such as loss of ER, subscapularis impairment, bone block and neurovascular complications (47). Mizuno and colleagues published the long-term outcome of Walch’s technique with a minimium follow-up of 18 years (mean: 20 years). The rate of dislocation recurrence was 2.9%, as well as the rate of recurrent subluxations (overall instability rate: 5.9% at 20 years) and the mean subjective shoulder value ranged between 82 and 92%. The development of osteoarthritis was mild if at all present if the bone block was positioned correctly without lateral overhang and screws parallel to the glenoid articular surface (43). The lateral coracoid overhang has been associated with more advanced osteoarthritis (Fig. 4B), as reported previously by Hovelius et al. (61, 62).
Risk factors for recurrence after surgery
Age
Young age has been known to be one of the most important risk factors for recurrent instability after capsuloligamentous soft tissue procedures to treat chronic traumatic instability (63, 64, 65, 66, 67). However, no age cut-off was defined until Balg and Boileau studied risk factors for recurrence in 2007 (3). They used an age cut-off of less than 20 years, which was highly significant for the difference in dislocation rates in the two age groups (P = 0.001). After a mean follow-up of 31 months (24-52) 8.3% (n = 8 of 96) of patients older than 20 years dislocated again compared to 31.4% (n = 11 of 35) of patients who were younger than 20 years. In recent years, there has been more and more evidence underlining the high recurrence rates in younger patients under the age of 20. In 2017, 143 patients operated on with an arthroscopic Bankart repair in a center of excellence and showed a recurrence rate of 18.2% for all patients and 39.1% for patients below the age of 20 years with a minimum follow-up of 10 years (7). Long-term arthroscopic Bankart outcomes of 186 shoulders (minimum follow-up 10 years) from a university center in Finland showed a dislocation recurrence rate of 30% for all patients and 54% for patients 20 years of age or younger (4).
A recent study of 100 patients with a mean follow-up of 8.3 years of Zeifang’s group in Heidelberg reported overall recurrence rates after arthroscopic Bankart repair of 22% (10). Of the observed recurrences, 86% were seen in patients below the age of 30 years. This study may indicate that 20 years of age as a cut-off could be too low for attributing an increased or decreased recurrence risk related to the patient’s age.
A systematic review of surgical instability treatment in pediatric patients concluded that arthroscopic Bankart repair surgery has the highest recurrence rate of at least 24% (68). The Latarjet procedure was underrepresented (n = 26). The authors concluded that given the high recurrence rate without surgery in this age group, it may be reasonable to perform surgery after first-time dislocation, particularly in patients with other risk factors.
In 2022, Kukkonen et al. published the first high-level evidence randomized trial of 95 patients comparing modern arthroscopic BR with or without remplissage vs open Latarjet procedures in young males (mean age 21 years; 16–25) with short-term follow-up of 2 years (69). There was a significant difference in the redislocation rate in young males in favor of open Latarjet procedures (2% vs 21%; P = 0.006). This is the strongest comparative evidence between open Latarjet surgery and arthroscopic Bankart repair to date.
The largest series of 46 skeletally immature patients (age range 13–17) operated with the Latarjet procedure by Walch with a median follow-up of 6.6 years was published in 2020 (44). The mean SSV was 95%, 98% of patients were satisfied, 75% of patients returned to the same level of sports, 20% had mild postoperative pain, 24% had subjective apprehension, 4% re-dislocated and 9% had postoperative arthritis at long-term follow-up. Hyperlaxity, female gender and large or deep Hill–Sachs lesions were associated with persistent apprehension.
Sports profile
The instability severity index (ISIS) score uses two preoperative risk criteria for sports (3): ‘type of sport – contact or forced overhead’ and ‘degree of sports participation – competitive’.
Certain sports are associated with an increased risk of recurrence after arthroscopic Bankart repair (63, 66, 70, 71). A high risk for shoulder dislocations in general has been reported for not only contact sports like rugby, American and Australian football, handball, basketball, soccer and martial arts, wrestling, but also sports with risks of falls such as skateboarding, snowboarding, skiing, overhead sports and throwing (72, 73).
The criterion ‘type of sport’ as a criterion in the ISIS score has been attributed 1 point for an increased risk if characterized as ‘contact sports and forced overhead’ (3). This variable, however, was not significant (P = 0.310) in the ISIS study. Competitive sports level has been associated with a higher recurrence rate after Bankart repairs (71) and is the second risk criterion of the sports profile in the ISIS score. It has been attributed 1 point on the score (3). The variable was statistically significant (P = 0.031).
Hyperlaxity
Hyperlaxity has been associated with bilateral shoulder instability and has been shown to increase the risk of recurrent shoulder instability (63, 74, 75). In the ISIS score, it has been attributed 1 point for either anterior or inferior hyperlaxity tested with the Walch–Coudane test (76) or Gagey test (77).
Critical soft tissue lesions
An anterior labroligamentous periostal sleeve avulsion (78) leads to a medialization and scarring of the labrum associated with decreased ER in 90° of abduction (79) and has been found to be associated with an increased risk of recurrence after arthroscopic Bankart repair (80, 81). The increased risk of failure of an arthroscopic capsulolabral repair may be associated with abundant capsular length after reduction and repair of the labrum.
Humeral avulsion of glenohumeral ligament (HAGL) lesions are present in a small number of cases with anterior glenohumeral instability (<10%). Arthroscopic (82) and open repair (83) have been reported with good outcomes. Some high-level athletes did not return to the preinjury level after arthroscopic repair (82). The Latarjet procedure is effective for the treatment of HAGL lesions (84).
Bone loss
Traditionally, the Latarjet procedure was reserved for patients with ‘critical bone loss’ following recurrent shoulder dislocations (85). The most reproducible and accurate techniques to measure glenoid bone loss are the Barchilon method and Giles method, with the latter requiring adjustment for overestimation bias (86). Many researchers have tried to define the amount of glenoid bone loss at which a Latarjet procedure is required. Over time, this threshold has been decreasing – partly due to the high recurrence rate seen with arthroscopic soft tissue procedures and the comparatively high success of bony procedures.
In 1998, a clinical study by Bigliani et al. classified glenoid rim lesions. They recommended that bone defects involving greater than 25% of the glenoid width required a coracoid transfer, with anything smaller having a soft tissue procedure (34). Burkhart et al. defined a significant glenoid bone defect as one in which the arthroscopic appearance of the glenoid was that of an ‘inverted pear’, where the inferior glenoid had a smaller diameter than the superior glenoid (16). In their study published in 2000, they demonstrated a 67% recurrence rate in these patients treated with an arthroscopic Bankart repair.
In a biomechanical study on cadaveric shoulders, Itoi et al. determined that an osseous defect with a width that is at least 21% of the glenoid length resulted in instability after Bankart repair (87). It also limited the range of ER of the shoulder because of the over-tensioning of the capsule caused by closing the gap between the detached capsule and the glenoid rim. Further biomechanical studies by Yamamoto et al. 2009 (88) and 2010 (89) showed that a defect length of 20 and 19% was critical corresponding to 26 and 25% of glenoid width, respectively.
Critical bone loss was thus thought to be in the range of 20–25% bone loss of the width of the glenoid. Clinical studies, however, started to report poor outcomes with smaller amounts of bone loss which they termed sub-critical bone loss. Shaha et al. reported worse Western Ontario Shoulder Instability (WOSI) scores and higher failure rates in patients with greater than 13.5% bone loss (90). Yamamoto et al. similarly demonstrated lower WOSI scores in patients with 17–25% compared to those with less than 17% of bone loss (91). Shin et al. reviewed 166 patients who underwent arthroscopic Bankart repair for recurrent anterior shoulder instability (92). They determined that 17.3% was the cut-off point of glenoid bone loss which predicted surgical failure during follow-up for more than 2 years.
Rather than having a defined cut-off for bone loss in which a shoulder becomes unstable, a biomechanical study by Gerber et al. demonstrated that there is a continuous, inverse relationship between bone loss and dislocation resistance (Fig. 5) (35). They found that an antero-inferior glenoid rim defect that measures half the diameter of the glenoid fossa decreases the dislocation resistance to 70% of the value of an intact joint.
Figure 5.
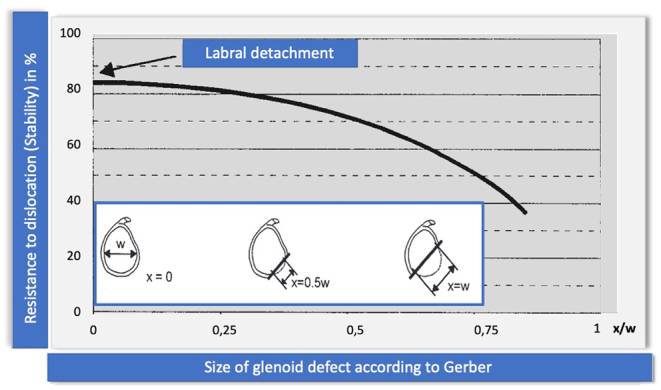
Inversed relationship: bone loss and dislocation resistance according to Gerber & Nyffeler (35).
Yamamoto et al. introduced the concept of the glenoid track to evaluate which Hill–Sachs lesions engage with the glenoid (93). With the arm elevated whilst in maximum ER and maximum horizontal extension, the contact zone of the glenoid on the humeral head is termed the glenoid track. If the Hill–Sachs lesion extends over the medial margin of the glenoid track (an off-track lesion, Fig. 6), there is a risk of engagement and dislocation. Kurokowa et al. found the prevalence of an off-track lesion to be 7% in a series of 100 consecutive patients with anterior instability (94). All cases with an engaging Hill–Sachs lesion had a large bony defect of the glenoid. There were two types of engaging Hill–Sachs lesions: a large and wide type and a narrow but medially located type. A follow-up study by Yamamoto et al. further subdivided on-track or non-engaging lesions into those with peripheral track lesions (Hill–Sachs occupancy > 75%) and those with central-track lesions (Hill–Sachs occupancy < 75%) (95). They found the former had significantly worse WOSI scores in a cohort of 50 patients treated with arthroscopic Bankart repair.
Figure 6.
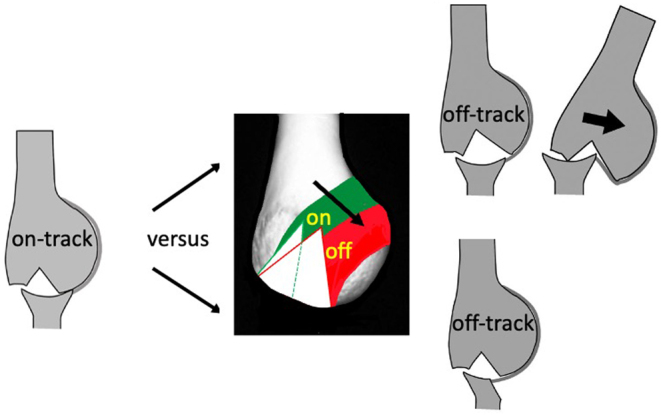
The glenoid-track concept.
The instability severity index score (ISIS) developed by Balg and Boileau has gained popularity for determining which patients are best suited to a Latarjet procedure (3). Radiographic analysis has been simplified to a Hill–Sachs lesion present on an anteroposterior radiograph of the shoulder in ER and/or loss of the inferior glenoid contour. Each of these findings is worth 2 points, and the developers of the score recommend performing a Latarjet in all patients with a score equal to or greater than 4 (13). Some researchers argue that the ISIS scoring system has a low sensitivity, with a high false-negative rate, because radiographs alone cannot consistently identify humeral and/or glenoid bone loss (96). To compensate for this inaccuracy, the cut-off score for a Latarjet has been reduced over time from equal to or greater than 7 to equal to or greater than 4 (97). Di Giacomo et al. developed a modification of the ISIS score which uses 3D computed tomography imaging to incorporate the on-track/off-track concept (96). They found that when the ISIS scoring and plain radiograph parameters were used, there was a two-fold increase in recommending a Latarjet vs the novel scoring criteria. The novel score, however, does require advanced imaging and sophisticated analysis, which is often not suited to everyday clinical practice.
Patient satisfaction after surgery
A recent study by Hurley of first-time dislocators did not show any difference in patient satisfaction in athletes treated with Bankart repair for lower risk patients vs the open Latarjet for patients with risk factors, at short-term follow-up (minimum 2 years) (98). A second study by the same group comparing the same procedures for patients with recurrent dislocation showed a significant superiority of the open Latarjet procedure for recurrence of instability (1.6 vs 16.1%; P = 0.009) (99). The Rowe score was significantly superior in the Latarjet group (P = 0.008). Both studies are limited by the short follow-up, and differences may increase over time in favor of Latarjet procedures.
In a benchmark study on long-term outcomes, Gerber’s group from Zurich compared state-of-the-art arthroscopic Bankart repairs with a capsular shift in lateral position with double-traction (271 shoulders) vs Latarjet procedures with Walch’s technique (94 shoulders) (12). They also compared patient satisfaction in a subset of patients with successful Bankart procedures with those who had successful Latarjet procedures without any instability in both groups. Recurrent instability was graded into apprehension, subluxation and redislocation. For patients without any instability in the context of successful outcomes, the subjective shoulder value was significantly higher (0.002) for patients with Latarjet procedures (91%) compared to patients with Bankart repair procedures (87%).
RTS parameters and instability
Laboute et al. reported on RTS after arthroscopic Bankart repair and open Latarjet surgery (100). RTS was significantly more frequent among sports people undergoing Latarjet procedures, for both training (P = 0.031) and competition (P = 0.038), and was also significantly more rapid for training (P = 0.034) with a mean time to return to training of 5.1 months after Latarjet procedures vs 6.4 months after Bankart procedures. The risk of recurrence was significantly higher for Bankart procedures (17.9%; P < 0.001) compared to Latarjet procedures (2%).
Gowd et al. reported on RTS of 66 patients with combined bone loss treated with a Latarjet procedure, and of those 35 patients were revision cases of failed Bankart repairs (59). RTS was possible for 90% of patients. A reduced amount of humeral bone loss was associated with significantly (P = 0.026) better RTS rates and RTS levels. Inversely, increased humeral bone loss was associated with limitations in throwing and the ability to return to the injury level. ER hyperlaxity is needed in overhead throwing athletes on the dominant side, in order to RTS. These patients will not do well with an arthroscopic Bankart and remplissage, which has been demonstrated to decrease ER (101, 102, 103).
Soccer
Walch’s group reported on the results and RTS in 28 shoulders of soccer players after the Latarjet procedure (88% professional or semi-professional) with a mean follow-up of 7 years (46). The rate of RTS was 96%, the mean time to RTS was 8 months (5 months for goalkeepers) and 71% reached the same level. There was one recurrent dislocation. Eight goalkeepers’ shoulders were treated. Pain and discomfort when throwing the ball were reported in 17% of the goalkeeper’s shoulders. Apprehension was recorded in 12.5% of players.
Stirma et al. reported on 10 professional soccer players between 16 and 28 years of age (mean 22.9) with a mean follow-up of 40.6 months operated with a Latarjet procedure (104). The RTS rate was 100%, the mean time to RTS was 93.5 days and all players returned to professional soccer with zero events of recurrent dislocation or subluxation.
Rugby
Rossi et al. compared RTS of 80 BR and 50 consecutive Latarjet procedures in competitive rugby players with glenoid bone loss of less than 20% with a mean follow-up of 40 months (105). The RTS rate at the previous level was 92% without a significant difference between the procedures. There was a significant difference in instability recurrence (20 vs 4%) and reoperation rate (16 vs 4%) in favor of the Latarjet procedure.
Neyton et al. reported on the Latarjet procedure in 37 shoulders of rugby players (41% professional) with a minimum follow-up of 5 years (45). RTS was 68% but only one player stopped because of the shoulder and all returned to sports activity. RTS time in professional players was 3 months for training and 4 months for competition. There was no recurrence of dislocation. The mean SSV was 90% and the mean Rowe score was 93%. Mild arthritis was seen in 30% but no moderate or severe arthritis.
Australian football
In Australian football, a sport heavy in collision and overhead activity, RTS of 8 weeks has been reported for the Latarjet procedure after radiological confirmation of bony healing (106). The group of Hoy published recently on RTS of professional Australian football players (58 stabilizations) after a modified extracapsular Latarjet with anchors (n = 32) or BR (n = 26) (107). Percentage RTS and time for professional Australian football was 93.1% (6.8 months; in season 16.9 weeks in 75%) for the Bankart cohort and 96.9% (7.3 months; in season 18.8 weeks in 71%) for the Latarjet cohort. RTS time was influenced by the rehab schedule and may have been influenced by the capsular repair of the glenoid in Latarjet patients. There was a significant difference in instability recurrence, with 19% for the Bankart cohort and 0% for the Latarjet cohort. The cohorts were subject to selection bias with increased instability severity in the Latarjet group.
Revision of failed instability surgery
In 2020, Lau et al. performed a systematic review of revision surgery after failed instability surgery including 1110 revision cases over several studies (90). The weighted mean instability recurrence was 3.8% after Latarjet revisions (n = 245), 13.4% after open repair (n = 260), 16% after arthroscopic Bankart revisions (n = 531), 20.8% after a bone block revisions (n = 72) and 31% after capsular reconstruction (n = 35). Additional revision surgery was performed in 23% of cases after capsular reconstruction, 9% after BR and 9% after open repair compared to 0.02% after Latarjet revision cases. The data underline that recurrent instability is a problem in instability revision surgery if not performed by a Latarjet procedure, which outperformed all other techniques.
The same authors performed a systematic review of RTS after instability revision surgery including 564 revision cases over 18 studies (108). For arthroscopic revision, the RTS rate was 88% (n = 153), for open revision 91.5% (n = 153), for Latarjet revisions 88.1% (n = 149) and for bone block revisions 73.8% (n = 65). The mean weighted time to RTS was 7.8 months for arthroscopic revisions (4 studies) and 5.2 months for Latarjet revisions. Davey et al. reported a significantly (P < 0.0001) lower RTS rate in athletes treated with a Latarjet for a previously failed repair compared to athletes without previous instability surgery (109). Werthel et al. published significantly worse functional outcomes (P < 0.001) and pain (P = 0.01) in Latarjet procedures for failed BR compared to primary Latarjet procedures (61).
The aforementioned studies demonstrate that primary Latarjet may be a better option in at-risk patients. The strategy of trying a primary arthroscopic Bankart repair with revision Latarjet surgery for failures may be doing patients a disservice.
Osteoarthritis and instability arthropathy
Hovelius et al. have shown that recurrence of instability, older age at the time of dislocation, high-energy sports and alcoholism are risk factors for arthropathy (60). He also examined the occurrence of arthropathy after the Bristow–Latarjet procedure. Suboptimal bone block position was associated with a higher arthropathy rate (17%) compared to 2–4 mm coracoid placement medially to the glenoid rim (8%) (62).
Mizuno reported the long-term follow-up (mean: 20 years) of Walch’s patients with a mean age of 29.4 years at surgery (61). Of 60 shoulders with no arthritis prior to surgery, 12 shoulders (20%) showed arthritis at the final follow-up. Of eight shoulders with preoperative arthritis, only four shoulders showed progressive arthritis after the Latarjet procedure (50%). Arthritis was mild in 20.6% of cases (stages 1 and 2) and moderate in 8% of cases (stage 3). No severe stage 4 arthritis was seen. Risk factors for arthritis were older age at surgery, high-energy sports and lateral overhang of the transferred coracoid process.
Favard’s group evaluated osteoarthritis after modified Latarjet procedures with capsular repair directly to the side of the bone block to make it extra-articular in 58 shoulders with a minimum follow-up of 10 years (range: 10-15 years). The rate of mild osteoarthritis was 8.3%. The authors concluded that the extra-articular technique may reduce the development of osteoarthritis, but the results are comparable to Walch’s cases without lateral graft overhang with much longer follow-up (52).
The long-term results of BR with radiographs after 9–12 years (n = 38) showed moderate-to-severe arthritis in 36.8% of investigated shoulders (n = 14) (9). Ernstbrunner et al. compared long-term results at 8–18 years (mean: 13.2 years) of BR in lateral position with open Latarjet procedures in patients over 40 years of age (110). There was a significantly higher re-dislocation and subluxation rate in BR shoulders (P = 0.037) and a significantly lower final SSV (86% vs 91%; P = 0.011). There were no significant differences in final advanced arthropathy (16 vs 14; P = 0.334). There is no evidence for differences in osteoarthritis rates between BR and the Latarjet, as long as there are no technical errors (anchor placement and lateral graft overhang).
Conclusions
There is increasing evidence from long-term studies that in patients with risk factors, BR has higher failure rates than BR+R, BR with bone grafts and the Latarjet procedure. Patients at the highest risk of failure are young patients and those with bone loss. The amount of bone loss deemed significant continues to decrease. All surgeries have satisfactory rates of RTS across all sports, as well as high patient satisfaction. Recurrence rates, however, are higher in BR and RTS may be quicker with the Latarjet. Instability arthropathy is associated with the number of previous dislocations as well as surgical technique. Latarjet procedures do not seem to increase the risk of osteoarthritis if the bone block is not lateralized.
ICMJE conflict of interest statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
No funding was received for this research.
Author contribution statement
All authors prepared parts of the manuscript and reviewed the whole manuscript.
References
- 1.Provencher MT Midtgaard KS Owens BD & Tokish JM. Diagnosis and management of traumatic anterior shoulder instability. Journal of the American Academy of Orthopaedic Surgeons 202129e51–e61. ( 10.5435/JAAOS-D-20-00202) [DOI] [PubMed] [Google Scholar]
- 2.Camus D Domos P Berard E Toulemonde J Mansat P & Bonnevialle N. Isolated arthroscopic Bankart repair vs. Bankart repair with “remplissage” for anterior shoulder instability with engaging Hill-Sachs lesion: A meta-analysis. Orthopaedics and Traumatology, Surgery and Research 2018104803–809. ( 10.1016/j.otsr.2018.05.011) [DOI] [PubMed] [Google Scholar]
- 3.Balg F & Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. Journal of Bone and Joint Surgery. British Volume 2007891470–1477. ( 10.1302/0301-620X.89B11.18962) [DOI] [PubMed] [Google Scholar]
- 4.Flinkkilä T Knape R Sirniö K Ohtonen P & Leppilahti J. Long-term results of arthroscopic Bankart repair: minimum 10 years of follow-up. Knee Surgery, Sports Traumatology, Arthroscopy 20182694–99. ( 10.1007/s00167-017-4504-z) [DOI] [PubMed] [Google Scholar]
- 5.Vermeulen AE Landman EBM Veen EJD Nienhuis S & Koorevaar CT. Long-term clinical outcome of arthroscopic Bankart repair with suture anchors. Journal of Shoulder and Elbow Surgery 201928e137–e143. ( 10.1016/j.jse.2018.09.027) [DOI] [PubMed] [Google Scholar]
- 6.Marquardt B Witt KA Götze C Liem D Steinbeck J & Pötzl W. Long-term results of arthroscopic Bankart repair with a bioabsorbable tack. American Journal of Sports Medicine 2006341906–1910. ( 10.1177/0363546506290404) [DOI] [PubMed] [Google Scholar]
- 7.Aboalata M Plath JE Seppel G Juretzko J Vogt S & Imhoff AB. Results of arthroscopic Bankart repair for anterior-inferior shoulder instability at 13-year follow-up. American Journal of Sports Medicine 201745782–787. ( 10.1177/0363546516675145) [DOI] [PubMed] [Google Scholar]
- 8.Komnos GA Banios K Liantsis A Alexiou K Varitimidis S Bareka M & Hantes ME. Results of arthroscopic Bankart repair in recreational athletes and laborers: A retrospective study with 5 to 14 years of follow-up. Orthopaedic Journal of Sports Medicine 201972325967119881648. ( 10.1177/2325967119881648) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ono Y Dávalos Herrera DA Woodmass JM Lemmex DB Carroll MJ Yamashita S Thornton GM & Lo IK. Long-term outcomes following isolated arthroscopic Bankart repair: a 9- to 12-year follow-up. JSES Open Access 20193189–193. ( 10.1016/j.jses.2019.05.002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Panzram B Kentar Y Maier M Bruckner T Hetto P & Zeifang F. Mid-term to long-term results of primary arthroscopic Bankart repair for traumatic anterior shoulder instability: a retrospective study. BMC Musculoskeletal Disorders 202021 191. ( 10.1186/s12891-020-03223-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van der Linde JA van Kampen DA Terwee CB Dijksman LM Kleinjan G & Willems WJ. Long-term results after arthroscopic shoulder stabilization using suture anchors: an 8- to 10-year follow-up. American Journal of Sports Medicine 2011392396–2403. ( 10.1177/0363546511415657) [DOI] [PubMed] [Google Scholar]
- 12.Zimmermann SM Scheyerer MJ Farshad M Catanzaro S Rahm S & Gerber C. Long-term restoration of anterior shoulder stability: A retrospective analysis of arthroscopic Bankart repair versus open latarjet procedure. Journal of Bone and Joint Surgery. American Volume 2016981954–1961. ( 10.2106/JBJS.15.01398) [DOI] [PubMed] [Google Scholar]
- 13.Bessière C Trojani C Carles M Mehta SS & Boileau P. The open latarjet procedure is more reliable in terms of shoulder stability than arthroscopic Bankart repair. Clinical Orthopaedics and Related Research 20144722345–2351. ( 10.1007/s11999-014-3550-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frank RM Thon SG Tokish JM Cole BJ McCarty EC Romeo AA & Provencher CMT. Management of shoulder instability in 2020: what, when, and how. Instructional Course Lectures 2021703–22. [PubMed] [Google Scholar]
- 15.Young AA Maia R Berhouet J & Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. Journal of Shoulder and Elbow Surgery 201120(2)(Supplement) S61–S69. ( 10.1016/j.jse.2010.07.022) [DOI] [PubMed] [Google Scholar]
- 16.Burkhart SS & Beer JFD. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 200016677–694. ( 10.1053/jars.2000.17715) [DOI] [PubMed] [Google Scholar]
- 17.Frank RM Saccomanno MF McDonald LS Moric M Romeo AA & Provencher MT. Outcomes of arthroscopic anterior shoulder instability in the beach chair versus lateral decubitus position: a systematic review and meta-regression analysis. Arthroscopy 2014301349–1365. ( 10.1016/j.arthro.2014.05.008) [DOI] [PubMed] [Google Scholar]
- 18.Baron JE, Duchman KR, Hettrich CM, Glass NA, Ortiz SF, MOON Shoulder Group. Baumgarten KM, Bishop JY, Bollier MJ, Bravman JT, et al. Beach chair versus lateral decubitus position: differences in suture anchor position and number during arthroscopic anterior shoulder stabilization. American Journal of Sports Medicine 2021492020–2026. ( 10.1177/03635465211013709) [DOI] [PubMed] [Google Scholar]
- 19.Bishop JY, Hidden KA, Jones GL, Hettrich CM, Wolf BR. & MOON Shoulder Group. Factors influencing Surgeon’s choice of procedure for anterior shoulder instability: A multicenter prospective cohort study. Arthroscopy 2019352014–2025. ( 10.1016/j.arthro.2019.02.035) [DOI] [PubMed] [Google Scholar]
- 20.Balke M Shafizadeh S Bouillon B & Banerjee M. Management of shoulder instability: the current state of treatment among German orthopaedic surgeons. Archives of Orthopaedic and Trauma Surgery 20161361717–1721. ( 10.1007/s00402-016-2553-2) [DOI] [PubMed] [Google Scholar]
- 21.Berendes TD Pilot P Nagels J Vochteloo AJH & Nelissen RGHH. Survey on the management of acute first-time anterior shoulder dislocation amongst Dutch public hospitals. Archives of Orthopaedic and Trauma Surgery 2015135447–454. ( 10.1007/s00402-015-2156-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chong M Karataglis D & Learmonth D. Survey of the management of acute traumatic first-time anterior shoulder dislocation among trauma clinicians in the UK. Annals of the Royal College of Surgeons of England 200688454–458. ( 10.1308/003588406X117115) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolf EM & Pollack ME. Hill-Sachs “Remplissage”: an arthroscopic solution for the engaging Hill-Sachs lesion (SS-32). Arthroscopy 200420e14–e15. ( 10.1016/j.arthro.2004.02.033) [DOI] [PubMed] [Google Scholar]
- 24.Gouveia K Abidi SK Shamshoon S Gohal C Madden K Degen RM Leroux T Alolabi B & Khan M. Arthroscopic Bankart repair with remplissage in comparison to bone block augmentation for anterior shoulder instability with bipolar bone loss: a systematic review. Arthroscopy 202137706–717. ( 10.1016/j.arthro.2020.08.033) [DOI] [PubMed] [Google Scholar]
- 25.Feng S Chen M Chen J Li H Chen J & Chen S. Patient outcomes and fear of returning to sports after arthroscopic Bankart repair with remplissage. Orthopaedic Journal of Sports Medicine 2021923259671211001775. ( 10.1177/23259671211001775) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacDonald P, McRae S, Old J, Marsh J, Dubberley J, Stranges G, Koenig J, Leiter J, Mascarenhas R, Prabhakar S, et al. Arthroscopic Bankart repair with and without arthroscopic infraspinatus remplissage in anterior shoulder instability with a Hill-Sachs defect: a randomized controlled trial. Journal of Shoulder and Elbow Surgery 2021301288–1298. ( 10.1016/j.jse.2020.11.013) [DOI] [PubMed] [Google Scholar]
- 27.Hurley ET Toale JP Davey MS Colasanti CA Pauzenberger L Strauss EJ & Mullett H. Remplissage for anterior shoulder instability with Hill-Sachs lesions: a systematic review and meta-analysis. Journal of Shoulder and Elbow Surgery 2020292487–2494. ( 10.1016/j.jse.2020.06.021) [DOI] [PubMed] [Google Scholar]
- 28.Abouelsoud MM & Abdelrahman AA. Recurrent anterior shoulder dislocation with engaging Hill–Sachs defect: remplissage or Latarjet? European Orthopaedics and Traumatology 20156151–156. ( 10.1007/s12570-015-0313-3) [DOI] [Google Scholar]
- 29.Bah A Lateur GM Kouevidjin BT Bassinga JYS Issa M Jaafar A & Beaudouin E. Chronic anterior shoulder instability with significant Hill-Sachs lesion: arthroscopic Bankart with remplissage versus open Latarjet procedure. Orthopaedics and Traumatology, Surgery and Research 201810417–22. ( 10.1016/j.otsr.2017.11.009) [DOI] [PubMed] [Google Scholar]
- 30.Yang JS Mehran N Mazzocca AD Pearl ML Chen VW & Arciero RA. Remplissage versus modified latarjet for off-track Hill-Sachs lesions with subcritical glenoid bone loss. American Journal of Sports Medicine 2018461885–1891. ( 10.1177/0363546518767850) [DOI] [PubMed] [Google Scholar]
- 31.Cho NS Yoo JH & Rhee YG. Management of an engaging Hill–Sachs lesion: arthroscopic remplissage with Bankart repair versus Latarjet procedure. Knee Surgery, Sports Traumatology, Arthroscopy 2016243793–3800. ( 10.1007/s00167-015-3666-9) [DOI] [PubMed] [Google Scholar]
- 32.Randelli PS Compagnoni R Radaelli S Gallazzi MB Tassi A & Menon A. Arthroscopic remplissage is safe and effective: clinical and magnetic resonance results at a minimum 3 years of follow-up. Journal of Orthopaedics and Traumatology 202223 5. ( 10.1186/s10195-021-00624-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Auffarth A Schauer J Matis N Kofler B Hitzl W & Resch H. The J-bone graft for anatomical glenoid reconstruction in recurrent posttraumatic anterior shoulder dislocation. American Journal of Sports Medicine 200836638–647. ( 10.1177/0363546507309672) [DOI] [PubMed] [Google Scholar]
- 34.Bigliani LU Newton PM Steinmann SP Connor PM & Mcllveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. American Journal of Sports Medicine 19982641–45. ( 10.1177/03635465980260012301) [DOI] [PubMed] [Google Scholar]
- 35.Gerber C & Nyffeler RW. Classification of glenohumeral joint instability. Clinical Orthopaedics and Related Research 200240065–76. ( 10.1097/00003086-200207000-00009) [DOI] [PubMed] [Google Scholar]
- 36.Itoi E Lee SB Berglund LJ Berge LL & An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. Journal of Bone and Joint Surgery. American Volume 20008235–46. ( 10.2106/00004623-200001000-00005) [DOI] [PubMed] [Google Scholar]
- 37.Montgomery WH Wahl M Hettrich C Itoi E Lippitt SB & Matsen FA. Anteroinferior bone-grafting can restore stability in osseous glenoid defects. Journal of Bone and Joint Surgery. American Volume 2005871972–1977. ( 10.2106/JBJS.D.02573) [DOI] [PubMed] [Google Scholar]
- 38.Moroder P Schulz E Wierer G Auffarth A Habermeyer P Resch H & Tauber M. Neer Award 2019: latarjet procedure vs. iliac crest bone graft transfer for treatment of anterior shoulder instability with glenoid bone loss: a prospective randomized trial. Journal of Shoulder and Elbow Surgery 2019281298–1307. ( 10.1016/j.jse.2019.03.035) [DOI] [PubMed] [Google Scholar]
- 39.Scheibel M Kraus N Diederichs G & Haas NP. Arthroscopic reconstruction of chronic anteroinferior glenoid defect using an autologous tricortical iliac crest bone grafting technique. Archives of Orthopaedic and Trauma Surgery 20081281295–1300. ( 10.1007/s00402-007-0509-2) [DOI] [PubMed] [Google Scholar]
- 40.Boehm E Minkus M Moroder P & Scheibel M. Massive graft resorption after iliac crest allograft reconstruction for glenoid bone loss in recurrent anterior shoulder instability. Archives of Orthopaedic and Trauma Surgery 2020140895–903. ( 10.1007/s00402-020-03380-z) [DOI] [PubMed] [Google Scholar]
- 41.Frank RM Romeo AA Richardson C Sumner S Verma NN Cole BJ Nicholson GP & Provencher MT. Outcomes of latarjet versus distal tibia allograft for anterior shoulder instability repair: a matched cohort analysis. American Journal of Sports Medicine 2018461030–1038. ( 10.1177/0363546517744203) [DOI] [PubMed] [Google Scholar]
- 42.Walch G & Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Techniques in Shoulder and Elbow Surgery 20001256–261. ( 10.1097/00132589-200001040-00008) [DOI] [Google Scholar]
- 43.Mizuno N Denard PJ Raiss P Melis B & Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. Journal of Shoulder and Elbow Surgery 2014231691–1699. ( 10.1016/j.jse.2014.02.015) [DOI] [PubMed] [Google Scholar]
- 44.Domos P Chelli M Lunini E Ascione F Bercik MJ Neyton L Godeneche A & Walch G. Clinical and radiographic outcomes of the open Latarjet procedure in skeletally immature patients. Journal of Shoulder and Elbow Surgery 2020291206–1213. ( 10.1016/j.jse.2019.09.039) [DOI] [PubMed] [Google Scholar]
- 45.Neyton L Young A Dawidziak B Visona E Hager JP Fournier Y & Walch G. Surgical treatment of anterior instability in rugby union players: clinical and radiographic results of the Latarjet-Patte procedure with minimum 5-year follow-up. Journal of Shoulder and Elbow Surgery 2012211721–1727. ( 10.1016/j.jse.2012.01.023) [DOI] [PubMed] [Google Scholar]
- 46.Cerciello S Edwards TB & Walch G. Chronic anterior glenohumeral instability in soccer players: results for a series of 28 shoulders treated with the Latarjet procedure. Journal of Orthopaedics and Traumatology 201213197–202. ( 10.1007/s10195-012-0201-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bauer S Coron C Lannes X Walch G & Blakeney WG. Open Latarjet-Patte procedure for anterior shoulder stabilization: critical steps and pearls for the Walch technique. Video Journal of Sports Medicine 20214 1. ( 10.1177/26350254211014201) [DOI] [Google Scholar]
- 48.Griesser MJ Harris JD McCoy BW Hussain WM Jones MH Bishop JY & Miniaci A. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. Journal of Shoulder and Elbow Surgery 201322286–292. ( 10.1016/j.jse.2012.09.009) [DOI] [PubMed] [Google Scholar]
- 49.Giles JW Boons HW Elkinson I Faber KJ Ferreira LM Johnson JA & Athwal GS. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. Journal of Shoulder and Elbow Surgery 201322821–827. ( 10.1016/j.jse.2012.08.002) [DOI] [PubMed] [Google Scholar]
- 50.Yamamoto N Muraki T An KN Sperling JW Cofield RH Itoi E Walch G & Steinmann SP. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. Journal of Bone and Joint Surgery. American Volume 2013951390–1397. ( 10.2106/JBJS.L.00777) [DOI] [PubMed] [Google Scholar]
- 51.Sahu D. Capsular repair is not an important part of the Latarjet-Walch procedure. Journal of Shoulder and Elbow Surgery 20210. Available at: https://www.jshoulderelbow.org/article/S1058-2746(21)00808-9/abstract. [DOI] [PubMed] [Google Scholar]
- 52.Bouju Y Gadéa F Stanovici J Moubarak H & Favard L. Shoulder stabilization by modified Latarjet-Patte procedure: results at a minimum 10 years’ follow-up, and role in the prevention of osteoarthritis. Orthopaedics and Traumatology, Surgery and Research 2014100(4)(Supplement) S213–S218. ( 10.1016/j.otsr.2014.03.010) [DOI] [PubMed] [Google Scholar]
- 53.Kleiner MT Payne WB McGarry MH Tibone JE & Lee TQ. Biomechanical comparison of the latarjet procedure with and without capsular repair. Clinics in Orthopedic Surgery 2016884–91. ( 10.4055/cios.2016.8.1.84) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zumstein MA & Raniga S. The Role of Capsular Repair in Latarjet Procedures: Commentary on an article by Yoshiaki Itoigawa, MD, PhD, et al. “Repairing the Capsule to the Transferred Coracoid Preserves External Rotation in the Modified Latarjet Procedure.” Journal of Bone and Joint Surgery 201698e75. [DOI] [PubMed] [Google Scholar]
- 55.Elkousy H Gartsman GM Labriola J O’Connor DP & Edwards TB. Subscapularis function following the latarjet coracoid transfer for recurrent anterior shoulder instability. Orthopedics 201033 802. ( 10.3928/01477447-20100924-08) [DOI] [PubMed] [Google Scholar]
- 56.Azizi S Urbanschitz L Bensler S Lenz CG Borbas P & Eid K. Structural and functional results of subscapularis and conjoint tendon after latarjet procedure at 8-year average follow-up. American Journal of Sports Medicine 202250321–326. ( 10.1177/03635465211061599) [DOI] [PubMed] [Google Scholar]
- 57.Plath JE Aboalata M Seppel G Juretzko J Waldt S Vogt S & Imhoff AB. Prevalence of and risk factors for dislocation arthropathy: radiological long-term outcome of arthroscopic Bankart repair in 100 shoulders at an average 13-year follow-up. American Journal of Sports Medicine 2015431084–1090. ( 10.1177/0363546515570621) [DOI] [PubMed] [Google Scholar]
- 58.Franceschi F Papalia R Del Buono A Vasta S Maffulli N & Denaro V. Glenohumeral osteoarthritis after arthroscopic Bankart repair for anterior instability. American Journal of Sports Medicine 2011391653–1659. ( 10.1177/0363546511404207) [DOI] [PubMed] [Google Scholar]
- 59.Gowd AK Liu JN Polce EM Agarwalla A Garcia GH Nicholson GP Cole BJ Romeo AA & Verma NN. Return to sport following Latarjet glenoid reconstruction for anterior shoulder instability. Journal of Shoulder and Elbow Surgery 2021302549–2559. ( 10.1016/j.jse.2021.04.020) [DOI] [PubMed] [Google Scholar]
- 60.Hovelius L Saeboe M & Award Neer. Arthropathy after primary anterior shoulder dislocation--223 shoulders prospectively followed up for twenty-five years. Journal of Shoulder and Elbow Surgery 200818339–347. ( 10.1016/j.jse.2008.11.004) [DOI] [PubMed] [Google Scholar]
- 61.Werthel JD, Sabatier V, Schoch B, Amsallem L, Nourissat G, Valenti P, Kany J, Deranlot J, Solignac N, Hardy P, et al. Outcomes of the latarjet procedure for the treatment of chronic anterior shoulder instability: patients with prior arthroscopic Bankart repair versus primary cases. American Journal of Sports Medicine 20204827–32. ( 10.1177/0363546519888909) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hovelius L Sandström B & Saebö M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: Study II—the evolution of dislocation arthropathy. Journal of Shoulder and Elbow Surgery 200615279–289. ( 10.1016/j.jse.2005.09.014) [DOI] [PubMed] [Google Scholar]
- 63.Lafosse L Iserin A Kempf JF & Hardy P. Arthroscopic treatment of chronic anterior shoulder instability. Revue de Chirurgie Orthopédique et Reparatrice de l’Appareil Moteur 200086(Supplement 1) 106–109. [PubMed] [Google Scholar]
- 64.Gartsman GM Roddey TS & Hammerman SM. Arthroscopic treatment of anterior-inferior glenohumeral instability. Two to five-year follow-up. Journal of Bone and Joint Surgery. Am. 200082-A991–1003. ( 10.2106/00004623-200007000-00011) [DOI] [PubMed] [Google Scholar]
- 65.Kandziora F Jäger A Bischof F Herresthal J Starker M & Mittlmeier T. Arthroscopic labrum refixation for post-traumatic anterior shoulder instability: suture anchor versus transglenoid fixation technique. Arthroscopy 200016359–366. ( 10.1016/s0749-8063(0090079-3) [DOI] [PubMed] [Google Scholar]
- 66.Pagnani MJ Warren RF Altchek DW Wickiewicz TL & Anderson AF. Arthroscopic shoulder stabilization using transglenoid sutures. A four-year minimum followup. American Journal of Sports Medicine 199624459–467. ( 10.1177/036354659602400409) [DOI] [PubMed] [Google Scholar]
- 67.Bacilla P Field LD & Savoie FH. Arthroscopic Bankart repair in a high demand patient population. Arthroscopy 19971351–60. ( 10.1016/s0749-8063(9790209-7) [DOI] [PubMed] [Google Scholar]
- 68.Shanmugaraj A Chai D Sarraj M Gohal C Horner NS Simunovic N Athwal GS & Ayeni OR. Surgical stabilization of pediatric anterior shoulder instability yields high recurrence rates: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy 202129192–201. ( 10.1007/s00167-020-05913-w) [DOI] [PubMed] [Google Scholar]
- 69.Kukkonen J, Elamo S, Flinkkilä T, Paloneva J, Mäntysaari M, Joukainen A, Lehtinen J, Lepola V, Holstila M, Kauko T, et al. Arthroscopic Bankart versus open Latarjet as a primary operative treatment for traumatic anteroinferior instability in young males: a randomised controlled trial with 2-year follow-up. British Journal of Sports Medicine 202256327–332. ( 10.1136/bjsports-2021-104028) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Torchia ME Caspari RB Asselmeier MA Beach WR & Gayari M. Arthroscopic transglenoid multiple suture repair: 2 to 8 year results in 150 shoulders. Arthroscopy 199713609–619. ( 10.1016/s0749-8063(9790189-4) [DOI] [PubMed] [Google Scholar]
- 71.Roberts SN Taylor DE Brown JN Hayes MG & Saies A. Open and arthroscopic techniques for the treatment of traumatic anterior shoulder instability in Australian rules football players. Journal of Shoulder and Elbow Surgery 19998403–409. ( 10.1016/s1058-2746(9990067-8) [DOI] [PubMed] [Google Scholar]
- 72.Twomey-Kozak J Whitlock KG O’Donnell JA Anakwenze OA & Klifto CS. Shoulder dislocations among high school-aged and college-aged athletes in the United States: an epidemiologic analysis. JSES International 20215967–971. ( 10.1016/j.jseint.2021.06.006) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Martetschläger F & Imhoff AB. Shoulder dislocation in athletes. Current therapy concepts. Der Orthopade 201443236–243. ( 10.1007/s00132-013-2146-5) [DOI] [PubMed] [Google Scholar]
- 74.O’Driscoll SW & Evans DC. Contralateral shoulder instability following anterior repair. An epidemiological investigation. Journal of Bone and Joint Surgery. British Volume 199173941–946. ( 10.1302/0301-620X.73B6.1955441) [DOI] [PubMed] [Google Scholar]
- 75.Kempf JF Lacaze F & Hila A. Anterior instability and hyperlaxity of the shoulder. Revue de Chirurgie Orthopédique et Reparatrice de l’Appareil Moteur 200086(Supplement 1) 132–137. [PubMed] [Google Scholar]
- 76.Coudane H Walch G & Sebesta A. Chronic anterior instability of the shoulder in adults. Methodology. Revue de Chirurgie Orthopédique et Reparatrice de l’Appareil Moteur 200086(Supplement 1) 94–95. [PubMed] [Google Scholar]
- 77.Gagey OJ & Gagey N. The hyperabduction test. Journal of Bone and Joint Surgery. British Volume 20018369–74. ( 10.1302/0301-620x.83b1.10628) [DOI] [PubMed] [Google Scholar]
- 78.Neviaser TJ. The anterior labroligamentous periosteal sleeve avulsion lesion: a cause of anterior instability of the shoulder. Arthroscopy 1993917–21. ( 10.1016/s0749-8063(0580338-x) [DOI] [PubMed] [Google Scholar]
- 79.Deutsch A Ramsey ML & Williams GR. Loss of passive external rotation at 90 degrees abduction is predictive of a medially healed Bankart lesion. Arthroscopy 200622710–715. ( 10.1016/j.arthro.2006.02.008) [DOI] [PubMed] [Google Scholar]
- 80.Ozbaydar M Elhassan B Diller D Massimini D Higgins LD & Warner JJP. Results of arthroscopic capsulolabral repair: Bankart lesion versus anterior labroligamentous periosteal sleeve avulsion lesion. Arthroscopy 2008241277–1283. ( 10.1016/j.arthro.2008.01.017) [DOI] [PubMed] [Google Scholar]
- 81.Verweij LPE van Spanning SH Grillo A Kerkhoffs GMMJ Priester-Vink S & van Deurzen DFP. Age, participation in competitive sports, bony lesions, ALPSA lesions, > 1 preoperative dislocations, surgical delay and ISIS score > 3 are risk factors for recurrence following arthroscopic Bankart repair: a systematic review and meta-analysis of 4584 shoulders. Knee Surgery, Sports Traumatology, Arthroscopy 2021294004–4014. ( 10.1007/s00167-021-06704-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grundshtein A Kazum E Chechik O Dolkart O Rath E Bivas A & Maman E. Arthroscopic repair of humeral avulsion of glenohumeral ligament lesions: outcomes at 2-year follow-up. Orthopaedic Journal of Sports Medicine 2021923259671211004968. ( 10.1177/23259671211004968) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Davey MS Hurley ET Gaafar M Delaney R & Mullett H. Clinical outcomes in patients with humeral avulsion glenohumeral ligament lesions in the setting of anterior shoulder instability: a retrospective comparative study. American Journal of Sports Medicine 202250327–333. ( 10.1177/03635465211063917) [DOI] [PubMed] [Google Scholar]
- 84.Agneskirchner JD & Lafosse L. Transfer of the coracoid process in recurrent anterior instability of the shoulder joint. The arthroscopic Latarjet procedure. Operative Orthopadie und Traumatologie 201426296–306. ( 10.1007/s00064-011-0052-8) [DOI] [PubMed] [Google Scholar]
- 85.Reider B. Placing the latarjet in context. American Journal of Sports Medicine 20204817–20. ( 10.1177/0363546519892245) [DOI] [PubMed] [Google Scholar]
- 86.Arenas-Miquelez A Dabirrahmani D Sharma G Graham PL Appleyard R Bokor DJ Read JW Piper K & Raniga S. What is the most reliable method of measuring glenoid bone loss in anterior glenohumeral instability? A cadaveric study comparing different measurement techniques for glenoid bone loss. American Journal of Sports Medicine 2021493628–3637. ( 10.1177/03635465211041386) [DOI] [PubMed] [Google Scholar]
- 87.Itoi E Yamamoto N Kurokawa D & Sano H. Bone loss in anterior instability. Current Reviews in Musculoskeletal Medicine 2013688–94. ( 10.1007/s12178-012-9154-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yamamoto N Itoi E Abe H Kikuchi K Seki N Minagawa H & Tuoheti Y. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. American Journal of Sports Medicine 200937949–954. ( 10.1177/0363546508330139) [DOI] [PubMed] [Google Scholar]
- 89.Yamamoto N Muraki T Sperling JW Steinmann SP Cofield RH Itoi E & An KN. Stabilizing mechanism in bone-grafting of a large glenoid defect. Journal of Bone and Joint Surgery. American Volume 2010922059–2066. ( 10.2106/JBJS.I.00261) [DOI] [PubMed] [Google Scholar]
- 90.Shaha JS Cook JB Song DJ Rowles DJ Bottoni CR Shaha SH & Tokish JM. Redefining “critical” bone loss in shoulder instability: functional outcomes worsen with “subcritical” bone loss. American Journal of Sports Medicine 2015431719–1725. ( 10.1177/0363546515578250) [DOI] [PubMed] [Google Scholar]
- 91.Yamamoto N Kawakami J Hatta T & Itoi E. Effect of subcritical glenoid bone loss on activities of daily living in patients with anterior shoulder instability. Orthopaedics and Traumatology, Surgery and Research 20191051467–1470. ( 10.1016/j.otsr.2019.08.015) [DOI] [PubMed] [Google Scholar]
- 92.Shin SJ Kim RG Jeon YS & Kwon TH. Critical value of anterior glenoid bone loss that leads to recurrent glenohumeral instability after arthroscopic Bankart repair. American Journal of Sports Medicine 2017451975–1981. ( 10.1177/0363546517697963) [DOI] [PubMed] [Google Scholar]
- 93.Yamamoto N Itoi E Abe H Minagawa H Seki N Shimada Y & Okada K. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. Journal of Shoulder and Elbow Surgery 200716649–656. ( 10.1016/j.jse.2006.12.012) [DOI] [PubMed] [Google Scholar]
- 94.Kurokawa D Yamamoto N Nagamoto H Omori Y Tanaka M Sano H & Itoi E. The prevalence of a large Hill-Sachs lesion that needs to be treated. Journal of Shoulder and Elbow Surgery 2013221285–1289. ( 10.1016/j.jse.2012.12.033) [DOI] [PubMed] [Google Scholar]
- 95.Yamamoto N Shinagawa K Hatta T & Itoi E. Peripheral-track and central-track hill-Sachs lesions: A new concept of assessing an on-track lesion. American Journal of Sports Medicine 20204833–38. ( 10.1177/0363546519886319) [DOI] [PubMed] [Google Scholar]
- 96.Di Giacomo G Peebles LA Pugliese M Dekker TJ Golijanin P Sanchez A & Provencher MT. Glenoid track instability management score: radiographic modification of the instability severity index score. Arthroscopy 20203656–67. ( 10.1016/j.arthro.2019.07.020) [DOI] [PubMed] [Google Scholar]
- 97.Rosenberg SI Padanilam SJ Pagni BA Tjong VK & Sheth U. A lower Instability Severity Index score threshold may better predict recurrent anterior shoulder instability after arthroscopic Bankart repair: a systematic review. Journal of ISAKOS: Joint Disorders and Orthopaedic Sports Medicine 20216295–301. ( 10.1136/jisakos-2020-000584) [DOI] [PubMed] [Google Scholar]
- 98.Hurley ET Davey MS Montgomery C O’Doherty R Gaafar M Pauzenberger L & Mullett H. Arthroscopic Bankart repair versus open latarjet for first-time dislocators in athletes. Orthopaedic Journal of Sports Medicine 2021923259671211023803. ( 10.1177/23259671211023803) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hurley ET Davey MS Montgomery C O’Doherty R Gaafar M Pauzenberger L & Mullett H. Arthroscopic Bankart repair versus open latarjet for recurrent shoulder instability in athletes. Orthopaedic Journal of Sports Medicine 2021923259671211023801. ( 10.1177/23259671211023801) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Laboute E Hoffmann R Bealu A Ucay O & Verhaeghe E. Recurrence and return to sport after surgery for shoulder instability: arthroscopic Bankart versus Latarjet procedure. JSES International 20215609–615. ( 10.1016/j.jseint.2021.04.007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Merolla G Paladini P Di Napoli G Campi F & Porcellini G. Outcomes of arthroscopic Hill-Sachs remplissage and anterior Bankart repair: a retrospective controlled study including ultrasound evaluation of posterior capsulotenodesis and infraspinatus strength assessment. American Journal of Sports Medicine 201543407–414. ( 10.1177/0363546514559706) [DOI] [PubMed] [Google Scholar]
- 102.Boileau P O’Shea K Vargas P Pinedo M Old J & Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. Journal of Bone and Joint Surgery. American Volume 201294618–626. ( 10.2106/JBJS.K.00101) [DOI] [PubMed] [Google Scholar]
- 103.Haviv B Mayo L & Biggs D. Outcomes of arthroscopic “remplissage”: capsulotenodesis of the engaging large Hill-Sachs lesion. Journal of Orthopaedic Surgery and Research 20116 29. ( 10.1186/1749-799X-6-29) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Stirma GA Lima EBS Chaves DH Belangero PS Andreoli CV & Ejnisman B. Latarjet procedure on anterior shoulder instability in professional soccer players. Acta Ortopédica Brasileira 20202884–87. ( 10.1590/1413-785220202802225433) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rossi LA Tanoira I Gorodischer T Pasqualini I & Ranalletta M. Recurrence and revision rates with arthroscopic Bankart repair compared with the latarjet procedure in competitive rugby players with glenohumeral instability and a glenoid bone loss <20. American Journal of Sports Medicine 202149866–872. ( 10.1177/0363546520988154) [DOI] [PubMed] [Google Scholar]
- 106.Murphy M Stockden M Withers K Breidahl W & Charlesworth J. Eight-week return to play following latarjet shoulder reconstruction in an Australian football player: a case report. Journal of Sport Rehabilitation 201928283–287. ( 10.1123/jsr.2017-0194) [DOI] [PubMed] [Google Scholar]
- 107.Perret M Warby S Brais G Hinse S Hoy S & Hoy G. Return to professional Australian rules football after surgery for traumatic anterior shoulder instability. American Journal of Sports Medicine 2021493066–3075. ( 10.1177/03635465211029022) [DOI] [PubMed] [Google Scholar]
- 108.Lau BC Pineda LB Johnston TR Gregory BP Wu M Fletcher AN Ledbetter L & Riboh JC. Return to play after revision anterior shoulder stabilization: A systematic review. Orthopaedic Journal of Sports Medicine 202192325967120982059. ( 10.1177/2325967120982059) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Davey MS Hurley ET O’Doherty R Stafford P Delahunt E Gaafar M Pauzenberger L & Mullett H. Open latarjet procedure in athletes following failed prior instability surgery results in lower rates of return to play. Arthroscopy 2021372412–2417. ( 10.1016/j.arthro.2021.03.062) [DOI] [PubMed] [Google Scholar]
- 110.Ernstbrunner L De Nard B Olthof M Beeler S Bouaicha S Gerber C & Wieser K. Long-term results of the arthroscopic Bankart repair for recurrent anterior shoulder instability in patients older than 40 years: a comparison with the open latarjet procedure. American Journal of Sports Medicine 2020482090–2096. ( 10.1177/0363546520931090) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a