Abstract
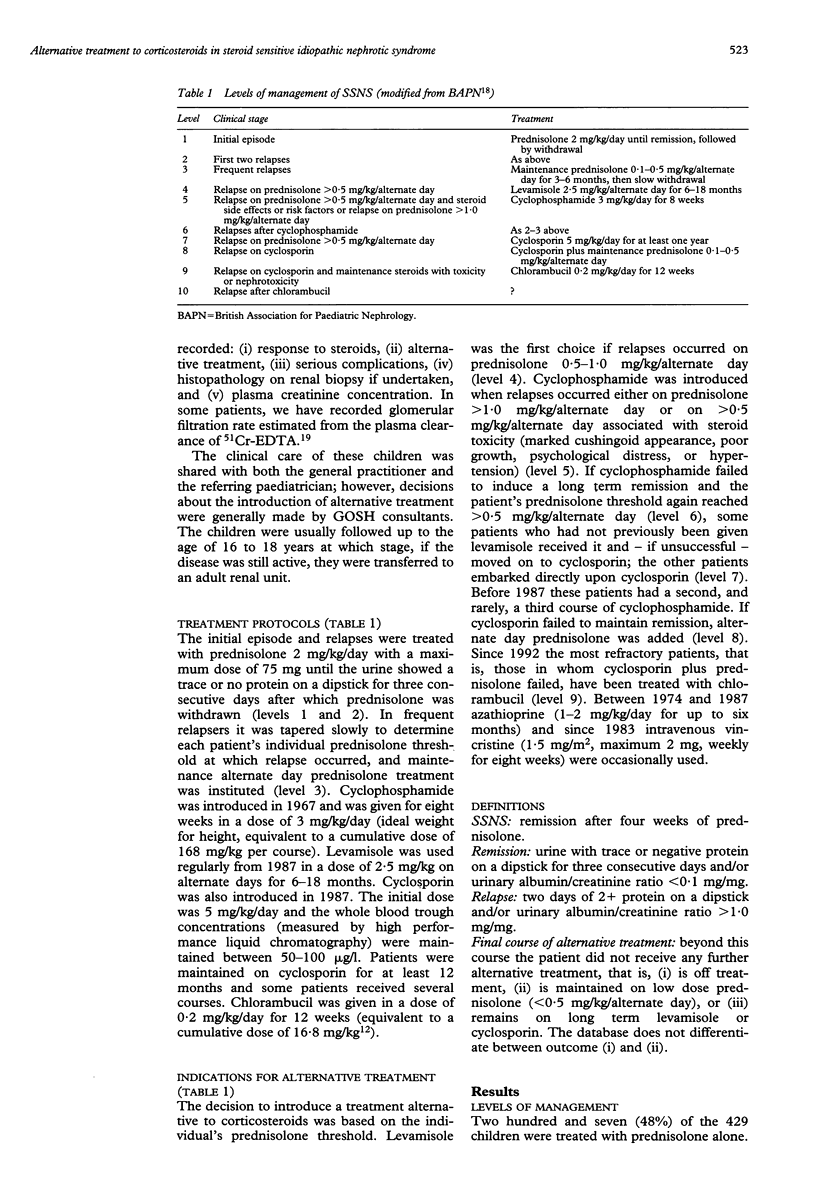
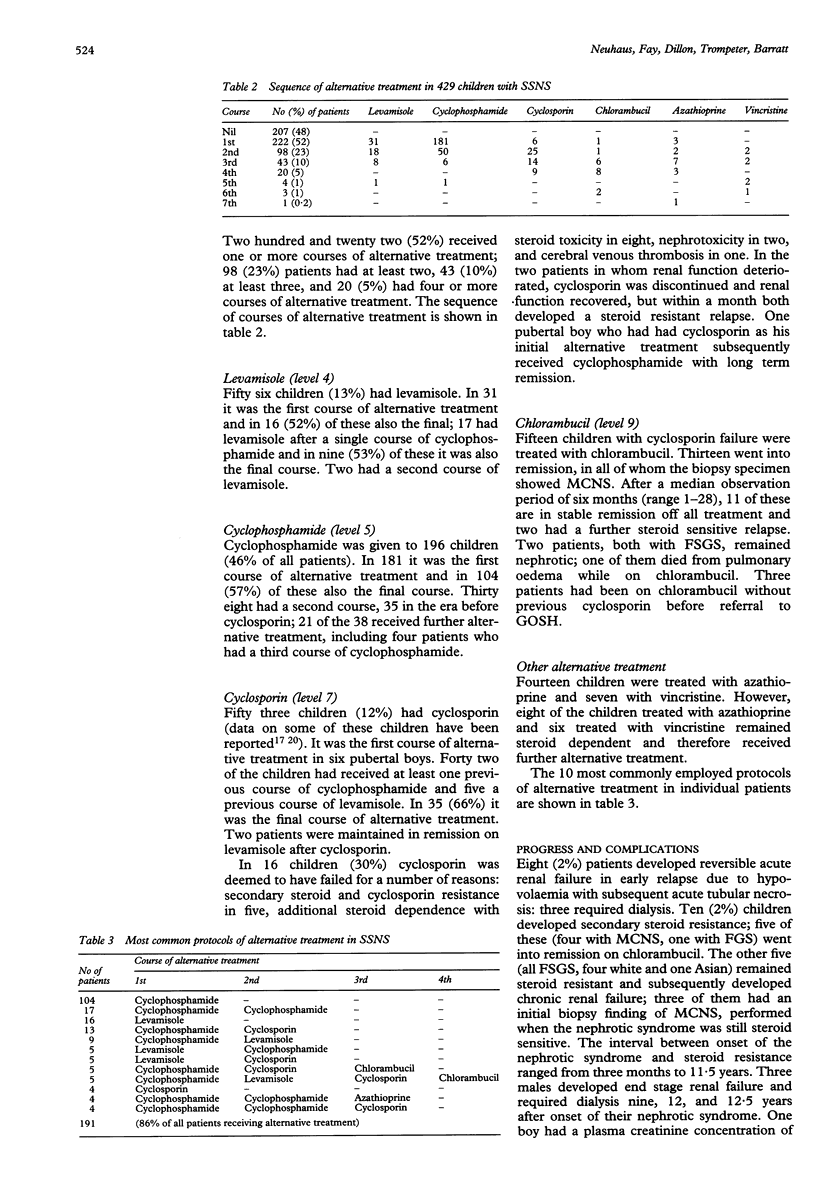
A review was undertaken of the use of alternative immunosuppressive treatment in addition to corticosteroids in a cohort of 429 children with steroid sensitive nephrotic syndrome (SSNS) treated between 1980 and 1994. Two hundred and twenty two children (52%) received at least one course of alternative treatment, 98 (23%) two, and 43 (10%) three. Cyclophosphamide was administered to 196 children (46%); in 181 it was the first course of alternative treatment and in 104 (57%) of those it was also the last ('final course'). Levamisole was given to 56 children (13%) and cyclosporin to 53 (12%). Fifteen children in whom cyclosporin failed were treated with chlorambucil. A few patients received azathioprine or vincristine. Ten children developed secondary steroid resistance, of whom five progressed to chronic renal failure. Acute complications included reversible renal failure, septicaemia, peritonitis, convulsions, and cerebral thrombosis. There were three deaths. It is concluded that half of the referred children with SSNS were deemed to require at least one course of alternative immunosuppressive treatment, and that side effects of the treatment and complications of SSNS are infrequent but occasionally fatal.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baluarte H. J., Hiner L., Gruskin A. B. Chlorambucil dosage in frequently relapsing nephrotic syndrome: a controlled clinical trial. J Pediatr. 1978 Feb;92(2):295–298. doi: 10.1016/s0022-3476(78)80030-4. [DOI] [PubMed] [Google Scholar]
- Barratt T. M., Bercowsky A., Osofsky S. G., Soothill J. F. Cyclophosphamide treatment in steroid-sensitive nephrotic syndrome of childhood. Lancet. 1975 Jan 11;1(7898):55–58. doi: 10.1016/s0140-6736(75)91068-5. [DOI] [PubMed] [Google Scholar]
- Bogdanović R., Banićević M., Cvorić A. Pituitary-gonadal function in women following cyclophosphamide treatment for childhood nephrotic syndrome: long-term follow-up study. Pediatr Nephrol. 1990 Sep;4(5):455–458. doi: 10.1007/BF00869819. [DOI] [PubMed] [Google Scholar]
- Bogdanović R., Banićević M., Cvorić A. Testicular function following cyclophosphamide treatment for childhood nephrotic syndrome: long-term follow-up study. Pediatr Nephrol. 1990 Sep;4(5):451–454. doi: 10.1007/BF00869818. [DOI] [PubMed] [Google Scholar]
- Brodehl J., Brandis M., Helmchen U., Hoyer P. F., Burghard R., Ehrich J. H., Zimmerhackl R. B., Klein W., Wonigeit K. Cyclosporin A treatment in children with minimal change nephrotic syndrome and focal segmental glomerulosclerosis. Klin Wochenschr. 1988 Nov 15;66(22):1126–1137. doi: 10.1007/BF01727848. [DOI] [PubMed] [Google Scholar]
- Callis L., Nieto J., Vila A., Rende J. Chlorambucil treatment in minimal lesion nephrotic syndrome: a reappraisal of its gonadal toxicity. J Pediatr. 1980 Oct;97(4):653–656. doi: 10.1016/s0022-3476(80)80035-7. [DOI] [PubMed] [Google Scholar]
- Chantler C., Barratt T. M. Estimation of glomerular filtration rate from plasma clearance of 51-chromium edetic acid. Arch Dis Child. 1972 Aug;47(254):613–617. doi: 10.1136/adc.47.254.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coovadia H. M., Adhikari M. Outcome of childhood minimal-change disease. Lancet. 1989 May 27;1(8648):1199–1200. doi: 10.1016/s0140-6736(89)92774-8. [DOI] [PubMed] [Google Scholar]
- Elzouki A. Y., al-Nassar K., al-Ali M., Malik G., Elsharie F., Jaiswal O. P. Sister chromatid exchange analysis in monitoring chlorambucil therapy in primary nephrotic syndrome of childhood. Pediatr Nephrol. 1991 Jan;5(1):59–61. doi: 10.1007/BF00852847. [DOI] [PubMed] [Google Scholar]
- Feehally J., Kendell N. P., Swift P. G., Walls J. High incidence of minimal change nephrotic syndrome in Asians. Arch Dis Child. 1985 Nov;60(11):1018–1020. doi: 10.1136/adc.60.11.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorensek M. J., Lebel M. H., Nelson J. D. Peritonitis in children with nephrotic syndrome. Pediatrics. 1988 Jun;81(6):849–856. [PubMed] [Google Scholar]
- Grupe W. E., Makker S. P., Ingelfinger J. R. Chlorambucil treatment of frequently relapsing nephrotic syndrome. N Engl J Med. 1976 Sep 30;295(14):746–749. doi: 10.1056/NEJM197609302951402. [DOI] [PubMed] [Google Scholar]
- Haws R. M., Baum M. Efficacy of albumin and diuretic therapy in children with nephrotic syndrome. Pediatrics. 1993 Jun;91(6):1142–1146. [PubMed] [Google Scholar]
- Hoyer P. F., Gonda S., Barthels M., Krohn H. P., Brodehl J. Thromboembolic complications in children with nephrotic syndrome. Risk and incidence. Acta Paediatr Scand. 1986 Sep;75(5):804–810. doi: 10.1111/j.1651-2227.1986.tb10294.x. [DOI] [PubMed] [Google Scholar]
- Hulton S. A., Jadresic L., Shah V., Trompeter R. S., Dillon M. J., Barratt T. M. Effect of cyclosporin A on glomerular filtration rate in children with minimal change nephrotic syndrome. Pediatr Nephrol. 1994 Aug;8(4):404–407. doi: 10.1007/BF00856512. [DOI] [PubMed] [Google Scholar]
- Hulton S. A., Neuhaus T. J., Dillon M. J., Barratt T. M. Long-term cyclosporin A treatment of minimal-change nephrotic syndrome of childhood. Pediatr Nephrol. 1994 Aug;8(4):401–403. doi: 10.1007/BF00856511. [DOI] [PubMed] [Google Scholar]
- Ingulli E., Gonzalez R., Rajpoot D., Tejani A. Nephrotic syndrome: from toddlers to twenties. Lancet. 1989 Mar 25;1(8639):674–674. doi: 10.1016/s0140-6736(89)92180-6. [DOI] [PubMed] [Google Scholar]
- Koskimies O., Vilska J., Rapola J., Hallman N. Long-term outcome of primary nephrotic syndrome. Arch Dis Child. 1982 Jul;57(7):544–548. doi: 10.1136/adc.57.7.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis M. A., Baildom E. M., Davis N., Houston I. B., Postlethwaite R. J. Nephrotic syndrome: from toddlers to twenties. Lancet. 1989 Feb 4;1(8632):255–259. doi: 10.1016/s0140-6736(89)91266-x. [DOI] [PubMed] [Google Scholar]
- Mehls O., Andrassy K., Koderisch J., Herzog U., Ritz E. Hemostasis and thromboembolism in children with nephrotic syndrome: differences from adults. J Pediatr. 1987 Jun;110(6):862–867. doi: 10.1016/s0022-3476(87)80397-9. [DOI] [PubMed] [Google Scholar]
- Schlesinger E. R., Sultz H. A., Mosher W. E., Feldman J. G. The nephrotic syndrome. Its incidence and implications for the community. Am J Dis Child. 1968 Dec;116(6):623–632. [PubMed] [Google Scholar]
- Sharples P. M., Poulton J., White R. H. Steroid responsive nephrotic syndrome is more common in Asians. Arch Dis Child. 1985 Nov;60(11):1014–1017. doi: 10.1136/adc.60.11.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tejani A. Morphological transition in minimal change nephrotic syndrome. Nephron. 1985;39(3):157–159. doi: 10.1159/000183363. [DOI] [PubMed] [Google Scholar]
- Tejani A., Suthanthiran M., Pomrantz A. A randomized controlled trial of low-dose prednisone and ciclosporin versus high-dose prednisone in nephrotic syndrome of children. Nephron. 1991;59(1):96–99. doi: 10.1159/000186526. [DOI] [PubMed] [Google Scholar]
- Trompeter R. S., Lloyd B. W., Hicks J., White R. H., Cameron J. S. Long-term outcome for children with minimal-change nephrotic syndrome. Lancet. 1985 Feb 16;1(8425):368–370. doi: 10.1016/s0140-6736(85)91387-x. [DOI] [PubMed] [Google Scholar]


