Abstract
Objective
To reduce unwitnessed inpatient falls on the neurology services floor at an academic medical center by 20% over 15 months.
Patients and Methods
A 9-item preintervention survey was administered to neurology nurses, resident physicians, and support staff. Based on survey data, interventions targeting fall prevention were implemented. Providers were educated during monthly in-person training sessions regarding the use of patient bed/chair alarms. Safety checklists were posted inside each patient’s room reminding staff to ensure that bed/chair alarms were on, call lights and personal items were within reach, and patients’ restroom needs were addressed. Preimplementation (January 1, 2020, to March 31, 2021) and postimplementation (April 1, 2021, to June 31, 2022) rates of falls in the neurology inpatient unit were recorded. Adult patients hospitalized in 4 other medical inpatient units not receiving the intervention served as a control group.
Results
Rates of falls, unwitnessed falls, and falls with injury all decreased after intervention in the neurology unit, with rates of unwitnessed falls decreasing by 44% (2.74 unwitnessed falls per 1000 patient-days before intervention to 1.53 unwitnessed falls per 1000 patient-days after intervention; P=.04). Preintervention survey data revealed a need for education and reminders on inpatient fall prevention best practices given a lack of knowledge on how to operate fall prevention devices, driving the implemented intervention. All staff reported significant improvement in operating patient bed/chair alarms after intervention (P<.001).
Conclusion
A collaborative, multidisciplinary approach focusing on provider fall prevention education and staff checklists is a potential technique to reduce neurology inpatient fall rates.
Inpatient falls are a serious health care safety and quality-of-care issue, accounting for the most common adverse event reported in hospital settings.1 Approximately 30% of falls result in morbidity, and 6% of falls result in serious injuries, including death.2 Inpatient falls are also associated with increased hospital length of stay and total hospital expenses.1 In fact, the Centers for Medicare and Medicaid Services have reduced reimbursement rates to hospitals for patients who experience preventable complications, such as falls during their stay.3
At our academic medical center, coinciding with the start of the coronavirus disease 2019 (COVID-19) pandemic, the rate of falls on the inpatient neurology services floor increased by 44% from 2019 to 2020, with a corresponding increase in unwitnessed inpatient falls from 44% to 58% in the respective years. Similarly, the rate of falls in 4 nonneurologic medical floor units at our center increased by 31% from 2019 to 2020, although unwitnessed inpatient falls in these units decreased slightly from 43% to 37% over the respective years. It is well known that neurologic patients are at increased risk of falls given the neurologic deficits that often accompany their disease processes and that frequently specialized patient precautions and hospital care are required to prevent complications such as falls.4, 5, 6 A multimodal approach to fall prevention is often required for these patients and requires not only hospital staff but also hospital visitors, including patient caregivers, given the extra layer of supervision that visitors often provide to patients.7 During the early stages of the COVID-19 pandemic, visitors had restricted access to hospitals worldwide in order to reduce the spread of the virus.8 These restrictions have been shown to negatively affect patient health, well-being, and provision of care and have potentially contributed to increases in patient falls, particularly in the neurologic disease population.8 Several recent studies have reported increased rates of inpatient falls in association with the COVID-19 pandemic in various health care centers, suggesting that limited caregiver support due to visitor restrictions may play a significant role in this regard.9, 10, 11, 12 The change in patient safety outcomes at our institution in correlation with the early stages of the pandemic made reducing inpatient neurology fall rates a priority at our center.
Prior research has shown that a multidisciplinary approach to fall prevention best practices in a neurology service can be successful.13 Other studies have emphasized how brief educational sessions for hospital staff can also improve fall rates.14, 15, 16 The current study hypothesized that a multidisciplinary and educational intervention for resident physicians, nurses, and patient care assistants would reduce the inpatient fall rates in our neurology services unit. The specific aim of the study was to reduce unwitnessed inpatient falls on the neurology services floor by 20% over 15 months because unwitnessed falls were more frequently associated with more severe morbidity.
Patients and Methods
Standard Protocol Approvals, Registrations, and Patient Consents
This study was approved by the Mayo Clinic Institutional Review Board and nursing data review leadership. All participants voluntarily participated in the anonymous survey.
Research Methodology
This pre-post quality improvement study was performed at a tertiary academic medical hospital (Saint Marys Hospital, one of Mayo Clinic’s hospitals in Rochester, Minnesota). A quality improvement work group consisting of staff and resident physicians, nurses, and support staff (patient care assistants) was established in early 2021 with the goal of decreasing the number of unwitnessed inpatient falls. The intervention group comprised adult patients with neurologic diseases hospitalized in the neurology inpatient unit. Adult patients hospitalized in 4 other medical inpatient units (general internal medicine, gastroenterology, and pulmonary services) who did not receive our intervention served as the control group.
An anonymous survey was developed, with 7 questions assessing respondent confidence in fall prevention best practices as well as respondent opinion on the importance of fall prevention education using ordinal data via a Likert-style 5-point scale rated from strongly disagree (1) to strongly agree (5). There were also 2 qualitative free-response questions to assess respondent insight into risk factors associated with increased falls and ideas regarding interventions that could reduce the patient fall rate in the neurology services unit. The survey was administered in February 2021 and July 2021 (3 months after intervention) to all resident physicians, nursing staff, and patient support staff working in the neurology inpatient unit at our hospital. Survey completion was voluntary for all eligible respondents.
From the knowledge gaps and opportunities for improvement identified in the initial survey result data, a 15-minute monthly educational session was developed and lead by nursing and support staff to train physicians on the proper use of inpatient bed and chair alarms. Educational sessions started in April 2021 and recurred every 4 weeks to correspond with the start of new resident rotations. All resident physicians were expected to attend the educational sessions that were held during protected teaching times in the morning before daily rounds. Senior neurology residents, which included quality improvement team members, helped communicate with nursing leadership to plan sessions and to ensure that junior residents were consistently attending.
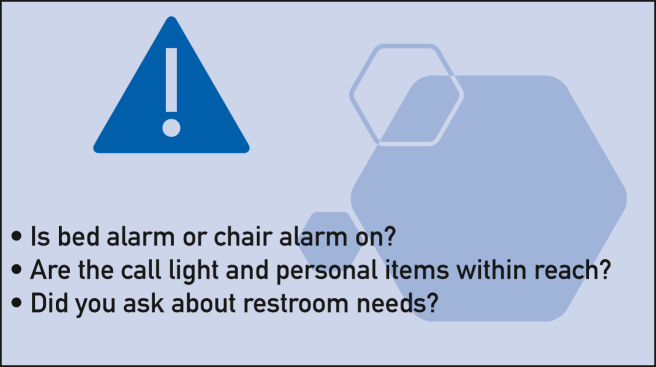
The 15-minute interactive sessions took place in an empty patient room in the neurology unit. At the beginning of the session, patient factors contributing to fall risk were discussed. Strategies to decrease fall risk were emphasized, including proper use of bed and chair alarms, placing the call light within reach, and addressing patients’ personal needs. This was followed by demonstration of bed/chair alarm use as well as time for resident practice and questions. A patient safety checklist was also created, printed on bright yellow paper, and posted inside each neurology patient’s room reminding staff before they left the room to ensure that bed and charm alarms were on, call lights and personal items were within reach, and patients’ restroom needs were addressed (Figure).
Figure.
Patient safety checklist.
Preimplementation (January 1, 2020, to March 31, 2021) and postimplementation (April 1, 2021, to June 31, 2022) rates of falls in the neurology inpatient unit were determined using an established institutional process. Data from this system are reported quarterly as number of falls per 1000 patient-days. In this system, a fall is defined as a fall to the floor, including instances when a member of the health care team helps guide or ease the patient to the floor. Patient days are derived from hospital administrative data, which do not include patient-specific information. The combined rates of falls from the 4 other medical units that did not receive our intervention were also determined using the same process during the same time frames. Additional measures collected included patient discharge volumes per quarter and Hester Davis Scale scores in the respective units. The Hester Davis Scale served as a validated fall risk assessment tool, incorporating factors such as patient age, last known date of fall, mobility, medications, mental status, toileting needs, volume/electrolyte status, communication ability, and behaviors, with combined scores greater than 15 suggesting a high fall risk.17 Our interventions were implemented beginning April 1, 2021.
For data analysis, the rate of falls in the inpatient neurology unit served as the primary outcome, with further delineation of unwitnessed fall rates and rates of falls with injury also recorded. Because falls are overall rare events compared with the number of patient admissions, the number of falls over time was assumed to follow a Poisson distribution. Ratios of 2 Poisson rates using preintervention and postintervention rates of falls in the neurology inpatient unit and the combined rates of falls in the 4 control medical inpatient units during the same time frames were tested using the test approach described by Lehmann and Romano.18 Preintervention vs postintervention patient discharge volumes and Hester Davis Scale scores were compared using unpaired t-tests.
Paired sample t-tests were performed on quantitative survey data to assess for difference in mean responses before and after the educational intervention. We assessed the impact on the whole sample and by individual role (resident physician, nurse, and support staff). Free-response survey data were analyzed by the quality improvement team members by assigning codes to repetitive ideas. Each free response was then coded to each idea. The team members then agreed on mutually identified patterns and refined them until a consensus was reached.
All statistical analyses were performed on BlueSky Statistics (version 7.40, using R version 3.6.3). P values less than .05 were considered statistically significant.
Data Availability
Anonymized data not published within this article will be made available by request from any qualified investigator.
Results
Rates of falls for the neurology inpatient unit and 4 combined medical inpatient units before and after our intervention are summarized in Table 1. Rates of falls, unwitnessed falls, and falls with injury all decreased after our intervention in the neurology inpatient unit, with rates of unwitnessed falls decreasing by 44% after intervention (2.74 unwitnessed falls per 1000 patient-days before intervention to 1.53 unwitnessed falls per 1000 patient-days after intervention; P=.04). In contrast, the combined rate of falls and falls with injury in the 4 other medical units that did not receive our intervention indicated no statistically significant change during the same time frame, and the rate of unwitnessed falls indicated a statistically significant increase during the same time period (0.93 unwitnessed falls per 1000 patient-days to 1.38 unwitnessed falls per 1000 patient-days; P=.03). Mean patient discharge volumes did not significantly differ in both the neurology and medical units before and after intervention. Mean Hester Davis Scale scores in both the neurology and medical units increased minimally, without statistical significance, over the time period of the study.
Table 1.
Rates of Falls, Discharge Volumes, and Hester Davis Scale Scores Before and After Implementation of a Multidisciplinary Quality Improvement Initiative in the Neurology Inpatient Unit
| Before intervention January 1, 2020, to March 31, 2021 |
After intervention April 1, 2021, to June 30, 2022 |
P value | |
|---|---|---|---|
| Neurology unit | |||
| Falls per 1000 patient-days (95% CI) | 5.11 (3.96-6.49) | 3.60 (2.69-4.73) | 0.07a |
| Unwitnessed falls per 1000 patient-days (95% CI) | 2.74 (1.92-3.80) | 1.53 (0.96-2.31) | 0.04a |
| Falls with injury per 1000 patient-days (95% CI) | 1.45 (0.87-2.26) | 1.04 (0.58-1.71) | 0.42a |
| Mean patient discharge volume per quarter (SD) | 508 (70.7) | 517 (28.4) | 0.79b |
| Mean patient Hester Davis Scale score (SD) | 17 (1.8) | 19 (0.9) | 0.07b |
| Medical unitc | |||
| Falls per 1000 patient-days (95% CI) | 2.90 (2.46-3.40) | 2.71 (2.31-3.17) | 0.58a |
| Unwitnessed falls per 1000 patient-days (95% CI) | 0.93 (0.69-1.23) | 1.38 (1.10-1.72) | 0.03a |
| Falls with injury per 1000 patient-days (95% CI) | 0.61 (0.41-0.86) | 0.80 (0.59-1.07) | 0.27a |
| Mean patient discharge volume per quarter (SD) | 1483 (168.7) | 1399 (108.9) | 0.38b |
| Mean patient Hester Davis Scale score (SD) | 17 (1.6) | 19 (0.5) | 0.08b |
Poisson test. Significant (P<.05) differences are emboldened.
t-test.
Four inpatient medical units (general internal medicine, gastroenterology, and pulmonary services) comprising adult patients who did not receive our intervention.
Table 2 summarizes the thematic qualitative free-response data from preintervention surveys. The 2 consensus risk factors for falls identified by the quality improvement team based on survey responses were alarm detection devices and the specific neurologic patient population. Alarm detection devices were reported to have malfunctioned due to either a technical issue with the device or the providers not understanding how to work the device. The neurologic patient population was cited as being impulsive, with change in mental status thought to be secondary to their underlying neurologic disease. Interventions that were thought to help reduce falls were largely recommendations for physician education through formal training on fall prevention and reminders, such as checklists.
Table 2.
Preintervention Free-Response Consensus Themes of all Responses From the Surveya
| Free response 1. Please list any risk factors you think are associated with the recent increase in patient falls. | |
|---|---|
| Representative themes | Representative quotes |
| Devices | “Service getting patients up by themselves and shutting alarms off, and then leaving the patient alone.” “Malfunctioning equipment (ie, patients being able to sit on the edge of the bed without alarms going off, etc.)” “Some risk factors include people forgetting to turn on the bed alarm, video monitoring missing patients trying to get up, and not putting all 4 side rails up for patients who continuously try to get out of bed.” |
| Patient population | “The greatest risk factor is the patient population that we service. Patients are confused and need close monitoring to reduce falls.” “Impulsive patients and bed alarms not going off (eg, if not plugged into the wall).” “Impulsivity of patients.” |
| Free response 2. Please summarize any ideas and/or interventions you think would help reduce inpatient falls. | |
|---|---|
| Representative themes | Representative quotes |
| Education | “Educating the physicians on how to operate bed alarms, chair alarms, and call light access with reminder signs.” “Education on plugging bed into wall/how to set alarms and how to use chair alarm.” “Educate service physician teams on alerting nursing and getting the patient up with trained staff.” |
| Reminders | “Check list of important items to remember to check to prevent falls when leaving a patient’s room.” “Some people forget to turn on bed alarm and chair alarm.” “Find a way to remind staff of alarms more often.” |
Note that free-response questions were administered with the quantitative survey questions.
Table 3 highlights results of the 7 Likert-style questions from both the preintervention and postintervention surveys. A total of 72 respondents, including 36 nurses, 24 resident physicians, and 12 patient support staff, completed the preintervention survey, with a 49% overall response rate out of total sent. The postintervention survey (3 months later) was completed by 59 participants, including 31 nurses, 12 resident physicians, and 16 patient support staff, with a 38% overall response rate.
Table 3.
Results of Paired t-Tests With Preintervention and Postintervention Means and SDs for the Full Sample and by Health care Provider Role From the Surveya
| Full sample | Before |
After |
P value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Q1: I am confident in my knowledge of the current institutional best practices in place to reduce inpatient falls. | 4.1 (1.1) | 4.4 (0.8) | .05 |
| Q2: I am confident in my ability to operate the inpatient bed alarms. | 4.5 (1.1) | 4.8 (0.8) | .08 |
| Q3: I am confident in my ability to operate the inpatient chair alarms. | 4.1 (1.5) | 4.7 (0.8) | .005 |
| Q4: Before leaving a patient’s room, how often do you assess whether the bed alarm/chair alarm is on? | 4.2 (1.1) | 4.6 (0.6) | .004 |
| Q5: Before leaving the patient’s room, how often do you assess whether the call light is within the patient’s reach? | 4.5 (0.9) | 4.6 (0.6) | .24 |
| Q6: Education on fall prevention best practices will increase (or has increased) my confidence in reducing inpatient falls. | 4.5 (0.9) | 4.3 (0.9) | .17 |
| Q7: Education on operating the inpatient bed alarms and chair alarms will improve (or has improved) my ability to operate the inpatient bed alarms and chair alarms. | 3.6 (1.1) | 4.4 (0.8) | <.001 |
| Residents | Before |
After |
P value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Q1: I am confident in my knowledge of the current institutional best practices in place to reduce inpatient falls. | 2.6 (1.0) | 4.1 (1.2) | .006 |
| Q2: I am confident in my ability to operate the inpatient bed alarms. | 3.0 (1.3) | 4.5 (1.2) | .02 |
| Q3: I am confident in my ability to operate the inpatient chair alarms. | 1.5 (0.9) | 4.3 (1.1) | <.001 |
| Q4: Before leaving a patient’s room, how often do you assess whether the bed alarm/chair alarm is on? | 2.3 (1.1) | 4.0 (0.7) | .001 |
| Q5: Before leaving the patient’s room, how often do you assess whether the call light is within the patient’s reach? | 3.3 (1.3) | 4.0 (0.6) | .82 |
| Q6: Education on fall prevention best practices will increase (or has increased) my confidence in reducing inpatient falls. | 4.8 (0.5) | 4.8 (0.5) | 1.00 |
| Q7: Education on operating the inpatient bed alarms and chair alarms will improve (or has improved) my ability to operate the inpatient bed alarms and chair alarms. | 4.6 (0.5) | 4.8 (0.4) | .92 |
| Nurses | Before |
After |
P value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Q1: I am confident in my knowledge of the current institutional best practices in place to reduce inpatient falls. | 4.4 (0.8) | 4.6 (0.5) | .18 |
| Q2: I am confident in my ability to operate the inpatient bed alarms. | 4.7 (0.8) | 4.9 (0.3) | .28 |
| Q3: I am confident in my ability to operate the inpatient chair alarms. | 4.6 (1.1) | 4.8 (0.4) | .20 |
| Q4: Before leaving a patient’s room, how often do you assess whether the bed alarm/chair alarm is on? | 4.6 (0.6) | 4.7 (0.4) | .26 |
| Q5: Before leaving the patient’s room, how often do you assess whether the call light is within the patient’s reach? | 4.8 (0.5) | 4.7 (0.5) | .45 |
| Q6: Education on fall prevention best practices will increase (or has increased) my confidence in reducing inpatient falls. | 4.3 (1.1) | 3.9 (0.9) | .27 |
| Q7: Education on operating the inpatient bed alarms and chair alarms will improve (or has improved) my ability to operate the inpatient bed alarms and chair alarms. | 3.2 (1.0) | 4.2 (0.7) | <.001 |
| Support staff | Before |
After |
P value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Q1: I am confident in my knowledge of the current institutional best practices in place to reduce inpatient falls. | 4.7 (0.5) | 4.3 (1.2) | .31 |
| Q2: I am confident in my ability to operate the inpatient bed alarms. | 5.0 (0) | 4.7 (1.2) | .34 |
| Q3: I am confident in my ability to operate the inpatient chair alarms. | 4.9 (0.3) | 4.7 (1.2) | .71 |
| Q4: Before leaving a patient’s room, how often do you assess whether the bed alarm/chair alarm is on? | 4.7 (0.5) | 4.7 (0.5) | 1.00 |
| Q5: Before leaving the patient’s room, how often do you assess whether the call light is within the patient’s reach? | 4.8 (0.5) | 4.9 (0.3) | .34 |
| Q6: Education on fall prevention best practices will increase (or has increased) my confidence in reducing inpatient falls. | 4.8 (0.5) | 4.4 (0.9) | .31 |
| Q7: Education on operating the inpatient bed alarms and chair alarms will improve (or has improved) my ability to operate the inpatient bed alarms and chair alarms. | 4.1 (0.8) | 4.5 (0.9) | .14 |
Significant (P<.05) differences are emboldened.
Likert-style scale rated from (1) strongly disagree to (5) strongly agree for Q1-3 and Q6 and Q7, and assessing frequency from (1) never to (5) always for Q4 and Q5.
Q, question.
There was a significant postintervention change in survey responses for the whole sample for questions 3, 4, and 7. That is, respondents reported improved frequency and confidence in operating patient alarm devices, such as bed and chair alarms, and they also reported that education on fall prevention techniques improved their ability to operate these alarms. When assessing the impact of intervention on responses by health care provider role, we found that resident physicians had a more robust change, with positive postintervention responses to 4 questions (questions 1-4, for all, P=.024 to <.001). There was a significant change in response to question 7 for nurses (P<.001). There was no difference between preintervention and postintervention responses for the support staff. All significant postintervention survey responses were positive, suggesting that there was benefit from the intervention.
Discussion
Falls in the inpatient setting remain a significant cause of morbidity and highly use inpatient resources. Among neurologic patients, this is ever more important given the increased risk of falls secondary to associated neurologic deficits.4, 5, 6,19 In fact, several studies have highlighted the significantly increased fall risk that neurologic patients face compared with age-matched controls and how falls can further neurologic morbidity and hinder progress toward recovery.20, 21, 22, 23 The current study addressed the increased inpatient fall rate in our hospital’s neurology services unit through a collaborative, interdisciplinary educational intervention. Throughout the COVID-19 pandemic, given visitor restrictions to the hospitals to reduce the spread of the virus, there was an increased need of and reliance on technology to assist providers caring for patients in the hospital setting.24 Our preliminary survey data indicated that providers did not feel comfortable using fall prevention technology, such as bed and chair alarms, and required increased education and reminders for regular use of these items.
Several studies have examined methods to improve inpatient fall rates and have included patient monitoring devices,25 bedside sitters,26 a fall prevention safety checklist,27 medication supplementation such as vitamin D,28 patient and staff education,14, 15, 16 and individualized patient fall prevention plans.29 These interventions have resulted in varying success rates in reducing inpatient falls likely because fall prevention is a complex problem that often requires a multimodal approach.7 Interestingly, a recent meta-analysis analyzing several different types of fall prevention interventions identified that the only intervention to yield a significant improvement result was education.30
From the preintervention survey data, we found that resident physicians reported the least confidence with fall prevention strategies, with lower mean survey responses to questions 1 through 5 (Table 3), compared with support staff and nurses. These data suggested that an intervention targeting resident physicians would likely be most beneficial. The free-response data indicated that providers did not feel comfortable using fall prevention technology, such as bed and chair alarms, and required increased education and reminders for regular use of these items. Therefore, brief monthly educational sessions designed to teach physicians how to use the technology available to our hospital for fall prevention, such as patient bed and chair alarms, were implemented in addition to fall prevention checklists.
The postintervention survey data were clear. The average score for all participants in most questions increased after intervention. In fact, questions 3, 4, and 7 found statistically significant increases after intervention, suggesting that our fall prevention strategy through educational sessions targeted to the resident physicians as well as reminder checklists targeted to all staff was an effective tool for improving fall prevention at our institution. Interestingly, when each individual group’s scores were calculated, the resident physicians had the highest number of questions (4 questions) with statistically significant improvement after intervention, followed by nurses (1 question) and support staff (0 questions). It is plausible that nurses and support staff are better trained in fall prevention best practices in association with their positions, particularly given their higher preintervention confidence score on the survey compared with that of their physician colleagues. These data suggest that interventions in fall prevention in the hospital setting should target physicians because there seems to be limited training in the physician population. A previous study performed at our own institution also supports increasing physician engagement in fall prevention as an effective way to improve inpatient fall risk.13
Most impressive was the decreased rate of inpatient falls that occurred. The primary goal of the study was ultimately to decrease unwitnessed patient falls by 20% over the selected time. Our results found a decrease in the overall rate of falls and the rate of falls with injury and, in particular, a 44% decrease in unwitnessed falls in the neurology inpatient unit, far exceeding our initial goal. Although the absolute number of falls is low, falls lead to significant morbidity and even mortality, especially among patients with neurologic conditions.31 Previous epidemiologic studies on inpatient falls cite on average 6 falls per 1000 days in inpatient neurology services.32 A recent study with data from 8 hospitals reported that inpatient falls were associated with approximately $36,000 in cost increases per fall and that an intervention targeting fall reduction led to a reduced financial burden of $14,600 in net costs per 1000 patient-days.33
These results show that a collaborative, multidisciplinary intervention that involves simple strategies, such as brief education sessions as well as reminder checklists, improves inpatient falls. The rates of falls in 4 other medical units did not show similar changes during the same time frames, suggesting that the reduced rate of falls in the neurology inpatient unit was not simply due to increased institutional awareness of fall risk and prevention. Patient discharge volumes and Hester Davis Scale scores remained similar during the study period, suggesting that shifts in risk factors for falls or changes in patient volumes did not account for the differences observed after intervention. Additionally, fall rates decreased in the neurology unit but did not similarly decrease in the control medical units, and hospital-wide visitor policies changed throughout the study time frame as the pandemic unfolded, indicating that our results were not simply due to relaxation of visitor restrictions. Our results remained durable throughout 15 months despite the heterogeneous nature of resident physicians rotating through our services, highlighting that such a model is feasibly generalizable and could be implemented not only throughout different departments at our own institution but also potentially in other hospitals. Similar collaborations between nursing staff and inpatient providers at other institutions could work to identify major patient fall risk factors via survey and subsequently implement strategies for prevention, namely focused on education. This strategy could be applied to academic hospitals, community hospitals, neurology units, and other medical units. A multidisciplinary approach with a focus on education proved to be most effective at our institution.
Limitations to the study include a small sample size and low survey response over time, especially resident physician response on the postintervention survey (with half the number of respondents compared with that for the preintervention survey). It is possible that responses might have been biased toward residents who were most engaged in the intervention, which is certainly a significant limitation. There is also likely a wide variation in the training that hospital staff receive across departments and institutions regarding fall prevention, which could potentially skew data if some staff receive more training than others. Future directions include expanding this model to include other departments at our own institution as well as potential other neurology departments at other institutions. Transitions between the inpatient and outpatient setting, or vice versa, and targeted fall prevention education in the outpatient setting remain further areas of study as well.
Conclusion
A collaborative, interdisciplinary educational endeavor between physicians, nurses, and support staff focusing on education and reminder checklists is an effective way to reduce inpatient fall rate as well as improve fall prevention confidence among neurology hospital floor staff. This work can hopefully be continued and used as a model for fall prevention throughout other departments at our institution and potentially health care systems worldwide.
Potential Competing Interests
The authors report no competing interests.
Acknowledgments
We would like to thank all members of the Mayo Clinic Neurology Quality Committee for helping coordinate this project.
Supplemental Online Material
References
- 1.Bates D.W., Pruess K., Souney P., Platt R. Serious falls in hospitalized patients: correlates and resource utilization. Am J Med. 1995;99(2):137–143. doi: 10.1016/s0002-9343(99)80133-8. [DOI] [PubMed] [Google Scholar]
- 2.Fields J., Alturkistani T., Kumar N., et al. Prevalence and cost of imaging in inpatient falls: the rising cost of falling. Clinicoecon Outcomes Res. 2015;7:281–286. doi: 10.2147/CEOR.S80104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenthal M.B. Nonpayment for performance? Medicare's new reimbursement rule. N Engl J Med. 2007;357(16):1573–1575. doi: 10.1056/NEJMp078184. [DOI] [PubMed] [Google Scholar]
- 4.Thurman D.J., Stevens J.A., Rao J.K., Quality Standards Subcommittee of the American Academy of Neurology Practice parameter: assessing patients in a neurology practice for risk of falls (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2008;70(6):473–479. doi: 10.1212/01.wnl.0000299085.18976.20. [DOI] [PubMed] [Google Scholar]
- 5.Tamm A., Siddiqui M., Shuaib A., et al. Impact of stroke care unit on patient outcomes in a community hospital. Stroke. 2014;45(1):211–216. doi: 10.1161/STROKEAHA.113.002504. [DOI] [PubMed] [Google Scholar]
- 6.Ramirez-Zamora A., Tsuboi T. Hospital management of Parkinson disease patients. Clin Geriatr Med. 2020;36(1):173–181. doi: 10.1016/j.cger.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Tzeng H.M., Yin C.Y. Using family visitors, sitters, or volunteers to prevent inpatient falls. J Nurs Adm. 2007;37(7-8):329–334. doi: 10.1097/01.nna.0000285116.68313.c1. [DOI] [PubMed] [Google Scholar]
- 8.Hugelius K., Harada N., Marutani M. Consequences of visiting restrictions during the COVID-19 pandemic: an integrative review. Int J Nurs Stud. 2021;121 doi: 10.1016/j.ijnurstu.2021.104000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kwok Y.T., Lam M.S. Using human factors and ergonomics principles to prevent inpatient falls. BMJ Open Qual. 2022;11(1) doi: 10.1136/bmjoq-2021-001696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lombardi J., Strobel S., Pullar V., Senthil P., Upadhye S., Khemani E. Exploring changes in patient safety incidents during the COVID-19 pandemic in a Canadian regional hospital system: a retrospective time series analysis. J Patient Saf. 2022;18(6):e1014–e1020. doi: 10.1097/PTS.0000000000000991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liang S.C., Wei P.C., Ma H.L., Hsiao S.H. Higher fall rate of admitted patients during the ongoing COVID-19 epidemic: is it coincidence or not? J Patient Saf. 2021;17(1):e45–e46. doi: 10.1097/PTS.0000000000000794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arafa M., Nesar S., Abu-Jabeh H., Jayme M.O.R., Kalairajah Y. COVID-19 pandemic and hip fractures: impact and lessons learned. Bone Jt Open. 2020;1(9):530–540. doi: 10.1302/2633-1462.19.BJO-2020-0116.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hunderfund A.N., Sweeney C.M., Mandrekar J.N., Johnson L.M., Britton J.W. Effect of a multidisciplinary fall risk assessment on falls among neurology inpatients. Mayo Clin Proc. 2011;86(1):19–24. doi: 10.4065/mcp.2010.0441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ott L.D. The impact of implementing a fall prevention educational session for community-dwelling physical therapy patients. Nurs Open. 2018;5(4):567–574. doi: 10.1002/nop2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee D.R., Lo J.C., Tran H.N. Don’t fall for that: a residency curricular innovation about fall prevention. Perm J. 2020;24:19–058. doi: 10.7812/TPP/19.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DiGerolamo K.A., Chen-Lim M.L. An educational intervention to improve staff collaboration and enhance knowledge of fall risk factors and prevention guidelines. J Pediatr Nurs. 2021;57:43–49. doi: 10.1016/j.pedn.2020.10.027. [DOI] [PubMed] [Google Scholar]
- 17.Hester A.L., Davis D.M. Validation of the Hester Davis Scale for fall risk assessment in a neurosciences population. J Neurosci Nurs. 2013;45(5):298–305. doi: 10.1097/JNN.0b013e31829d8b44. [DOI] [PubMed] [Google Scholar]
- 18.Lehmann E.L., Romano J.P. Springer; 2006. Testing Statistical Hypotheses. [Google Scholar]
- 19.Benson C., Lusardi P. Neurologic antecedents to patient falls. J Neurosci Nurs. 1995;27(6):331–337. doi: 10.1097/01376517-199512000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Heikkilä A, Lehtonen L, Junttila K. Fall rates by specialties and risk factors for falls in acute hospital: a retrospective study. J Clin Nurs. Published online December 7, 2022. https://doi.org/10.1111/jocn.16594 [DOI] [PubMed]
- 21.Koç Z., Memiş A., Sağlam Z. Prevalence, etiology and risk factors for falls in neurological patients admitted to the hospital in northern Turkey. Acta Clin Croat. 2020;59(2):199–208. doi: 10.20471/acc.2020.59.02.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Czernuszenko A., Członkowska A. Risk factors for falls in stroke patients during inpatient rehabilitation. Clin Rehabil. 2009;23(2):176–188. doi: 10.1177/0269215508098894. [DOI] [PubMed] [Google Scholar]
- 23.Stolze H., Klebe S., Zechlin C., Baecker C., Friege L., Deuschl G. Falls in frequent neurological diseases—prevalence, risk factors and aetiology. J Neurol. 2004;251(1):79–84. doi: 10.1007/s00415-004-0276-8. [DOI] [PubMed] [Google Scholar]
- 24.Thomas K.A.S., O’Brien B.F., Fryday A.T., et al. Developing an innovative system of open and flexible, patient-family-centered, virtual visiting in ICU during the COVID-19 pandemic: a collaboration of staff, patients, families, and technology companies. J Intensive Care Med. 2021;36(10):1130–1140. doi: 10.1177/08850666211030845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cournan M., Fusco-Gessick B., Wright L. Improving patient safety through video monitoring. Rehabil Nurs. 2018;43(2):111–115. doi: 10.1097/RNJ.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 26.Greeley A.M., Tanner E.P., Mak S., Begashaw M.M., Miake-Lye I.M., Shekelle P.G. Sitters as a patient safety strategy to reduce hospital falls: a systematic review. Ann Intern Med. 2020;172(5):317–324. doi: 10.7326/M19-2628. [DOI] [PubMed] [Google Scholar]
- 27.Johnston M., Magnan M.A. Using a fall prevention checklist to reduce hospital falls: results of a quality improvement project. Am J Nurs. 2019;119(3):43–49. doi: 10.1097/01.NAJ.0000554037.76120.6a. [DOI] [PubMed] [Google Scholar]
- 28.Cameron I.D., Gillespie L.D., Robertson M.C., et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2012;12:CD005465. doi: 10.1002/14651858.CD005465.pub3. [DOI] [PubMed] [Google Scholar]
- 29.Spano-Szekely L., Winkler A., Waters C., et al. Individualized fall prevention program in an acute care setting: an evidence-based practice improvement. J Nurs Care Qual. 2019;34(2):127–132. doi: 10.1097/NCQ.0000000000000344. [DOI] [PubMed] [Google Scholar]
- 30.Morris M.E., Webster K., Jones C., et al. Interventions to reduce falls in hospitals: a systematic review and meta-analysis. Age Ageing. 2022;51(5):afac077. doi: 10.1093/ageing/afac077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cumbler E.U., Simpson J.R., Rosenthal L.D., Likosky D.J. Inpatient falls: defining the problem and identifying possible solutions. Part I: an evidence-based review. Neurohospitalist. 2013;3(3):135–143. doi: 10.1177/1941874412470665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hitcho E.B., Krauss M.J., Birge S., et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19(7):732–739. doi: 10.1111/j.1525-1497.2004.30387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dykes P.C., Curtin-Bowen M., Lipsitz S., et al. Cost of inpatient falls and cost-benefit analysis of implementation of an evidence-based fall prevention program. JAMA Health Forum. 2023;4(1) doi: 10.1001/jamahealthforum.2022.5125. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Anonymized data not published within this article will be made available by request from any qualified investigator.