Abstract
Benzofuran and 1,3,4-oxadiazole are privileged and versatile heterocyclic pharmacophores which display a broad spectrum of biological and pharmacological therapeutic potential against a wide variety of diseases. This article reports in silico CADD (computer-aided drug design) and molecular hybridization approaches for the evaluation of the chemotherapeutic efficacy of 16 S-linked N-phenyl acetamide moiety containing benzofuran-1,3,4-oxadiazole scaffolds BF1–BF16. This virtual screening was carried out to discover and assess the chemotherapeutic efficacy of BF1–BF16 structural motifs as Mycobacterium tuberculosis polyketide synthase 13 (Mtb Pks13) enzyme inhibitors. The CADD study results revealed that the benzofuran clubbed oxadiazole derivatives BF3, BF4, and BF8 showed excellent and remarkably significant binding energies against the Mtb Pks13 enzyme comparable with the standard benzofuran-based TAM-16 inhibitor. The best binding affinity scores were displayed by 1,3,4-oxadiazoles-based benzofuran scaffolds BF3 (−14.23 kcal/mol), BF4 (−14.82 kcal/mol), and BF8 (−14.11 kcal/mol), in comparison to the binding affinity score of the standard reference TAM-16 drug (−14.61 kcal/mol). 2,5-Dimethoxy moiety-based bromobenzofuran-oxadiazole derivative BF4 demonstrated the highest binding affinity score amongst the screened compounds, and was higher than the reference Pks13 inhibitor TAM-16 drug. The bindings of these three leads BF3, BF4, and BF8 were further confirmed by the MM-PBSA investigations in which they also exhibited strong bindings with the Pks13 of Mtb. Moreover, the stability analysis of these benzofuran-1,3,4-oxadiazoles in the active sites of the Pks13 enzyme was achieved through molecular dynamic (MD) simulations at 250 ns virtual simulation time, which indicated that these three in silico predicted bio-potent benzofuran tethered oxadiazole molecules BF3, BF4, and BF8 demonstrated stability with the active site of the Pks13 enzyme.
Keywords: benzofuran-1,3,4-oxadiazole; tuberclosis; Pks13 inhibitor; molecular docking; MM-PBSA; MD simulations; ADMET study; SAR
1. Introduction
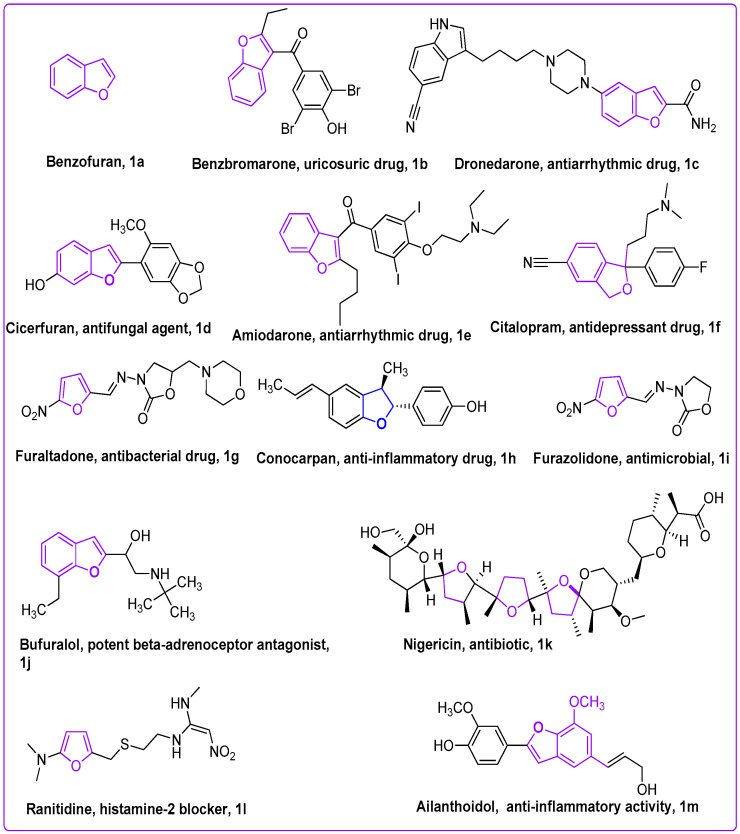
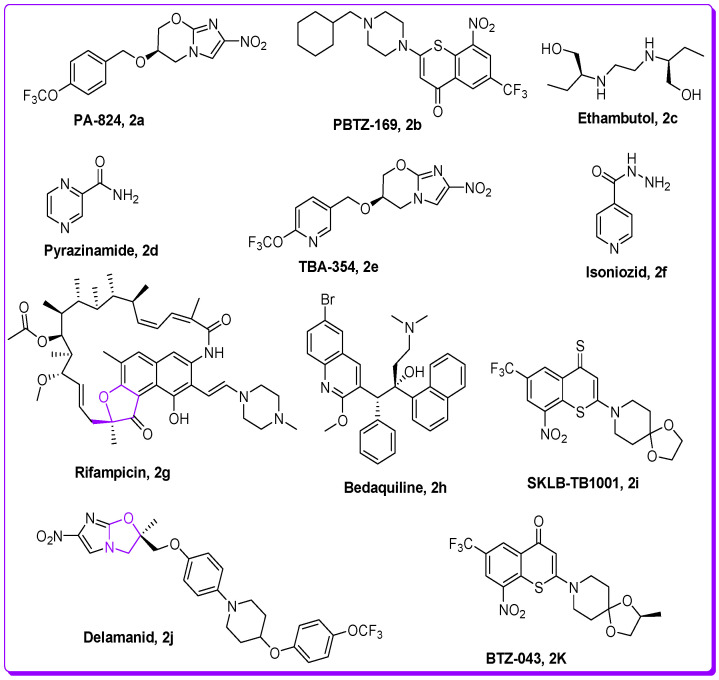
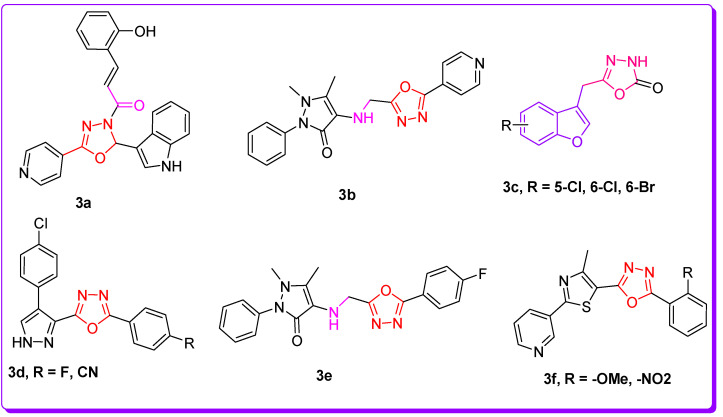
TB (tuberculosis) is among the deadliest transmittable infectious lung disease caused by Mycobacterium tuberculosis (Mtb). The global TB report 2018 described that Mtb is the leading cause of single infectious disease [1]. TB and its percentage are higher than human immunodeficiency virus (HIV) and AIDS. Amongst the infectious diseases after HIV, TB is a global health issue, being the second major cause of death across the world. In today’s world, antibiotic resistance is a major global problem in curing contagious microbial diseases (CMD) caused by deadly microbes [2,3]. The drug-resistant TB is a major health concern of today’s scientific community due to its resistance against the first-line drug rifampicin (RR-TB) [4,5]. To counter multi-drug resistance (MDR) and pan-drug resistance bacteria resulting from the development of mutagenicity [4,5,6,7,8], novel wide spectrum chemotherapeutic agents are urgently necessitated. It is imperative to discover novel anti-tuberculosis chemotherapeutic agents to stop resistance in Mtb strains, and ideally cure the disease in a shorter time [4,5,6,7,8,9,10]. There is an urgent demand and necessity for the designing, discovery, and development of novel curative candidates active against all forms of Mtb [8,9,10,11,12,13]. Heterocycles-based ring systems such as quinoxalines, coumarins, benzothiazoles, benzoxazoles, thiadiazoles, benzofurans, and oxadiazoles, etc., constitute a powerful backbone of different chemotherapeutic agents with a wide spectrum of biological activities in medicine, pharmacology, and pharmaceutics [14,15,16,17,18,19,20,21]. Benzofuran (Figure 1) is a five-membered oxygen containing a fused heterocyclic compound first synthesized by Perkin in 1870 [22]. Benzofuran moiety is an important structural unit of many of the natural and synthetic derivatives (Figure 1) displaying a versatile array of biological activities against a wide variety of diseases, such as anti-cancer, hemolytic, thrombolytic [23], anti-microbial [24], anti-tuberculosis [25,26], anti-Alzheimer’s [27,28], inflammation inhibitory activity [29], anti-parasitic [30], anti-viral [31], analgesic, anti-pyretic [32], anti-bacterial [33], anti-hyperglycemic [34], and anti-oxidant activities [33,35]. On the other hand, 1,3,4-oxadiazole scaffolds showed a broad spectrum of pharmacological applications; for example, anti-Alzheimer’s [36], anti-neoplastic [37], anti-viral [38], anti-cancer [39], FAK inhibitors [40], anti-fungal [41], anti-inflammatory [42], anti-bacterial [43] and anti-tubular activities [44]. The benzofuran-oxadiazoles also exhibited anti-lung cancer, human tyrosinase inhibitors, anti-HepG-2, anti-hemolytic, and anti-thrombotic activities [24,45]. The different marketed anti-TB drugs are listed in Figure 2, while potent anti-TB bioactive compounds with oxadiazole and furan cores are depicted in Figure 3 [46,47,48,49,50,51,52].
Figure 1.
Structures of natural and synthetic furan scaffolds 1a–1m.
Figure 2.
Structures of commercially available anti-TB drugs in market.
Figure 3.
Structures of oxadiazole and benzofuran-based anti-TB scaffolds.
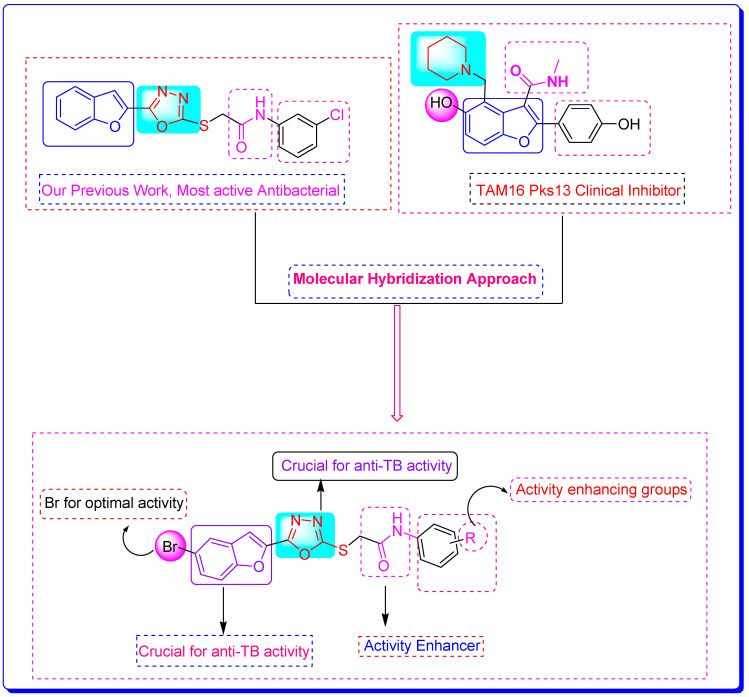
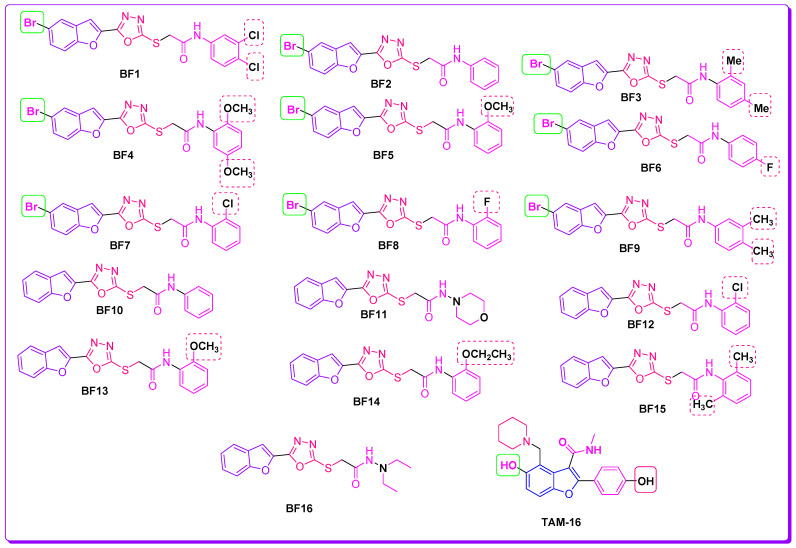
The previous work reported on benzofuran-oxadiazoles as anti-microbial agents by our research group and the current comprehensive literature study (Figure 4) [17,42,43,44,45,46,47,48,49,50,51,52] is the basis of the rationale to discover novel benzofuran-appended oxadiazole structural hybrids as anti-TB drug candidates with the help of different in silico techniques.
Figure 4.
Rational design of benzofuran-1,3,4-oxadiazole derivatives BF1–BF16 as anti-tuberculosis agents [24,46,47].
2. Results and Discussion
2.1. Evalaution of Anti-Mtb Potenial of Benzofurans-1,3,4-Oxadiazoles Using Computational Approaches
Mycobacterium Tuberculosis
Benzofuran-1,3,4-oxadiazoles BF1–BF16 [23,45,52] were evaluated for their anti-Mtb potential using computational approaches. Tuberculosis is a bacterial disease that predominantly affects the lungs and is caused by Mycobacterium tuberculosis [53]. Even though macrophages are crucial to the host immune system because they identify and eliminate potential intruders (pathogens), Mtb has developed several tactics that allow it to live and proliferate inside these lung macrophages, which are the main host cells for Mtb infection [54]. It is one of the prevalent causes of death worldwide, particularly in people who have also been infected by other pathogenic viruses and have viral infections. The existing TB treatment regimens take between six and nine months to complete, which makes it difficult for patients to adhere to them, which causes multi-drug resistant TB, which is essentially resistant to antibacterial drug treatments [55]. Hence, new potential anti-TB chemotherapeutics need to be designed and developed to overcome the MDR problem by targeting novel pathways and enzymes involved in bacterial growth, with new modes of action to lessen the likelihood of a relapse of the TB infection when existing medications are no longer reliable [5,6,13].
Intensive research has been put into finding new Mtb targets and their inhibitors that can stop the spread of this bacterial pathogen and mitigate its drug resistance [6,13,56]. Similarly, an important class of enzymes known as polyketide synthases (Pks) has not been explored as a therapeutic target for microbial infection. The Pks are enzymes that produce mycolic acids, which are essential for the survival and pathogenicity of Mtb [57]. More than 20 (Pks) enzymes are a part of various multi-enzyme complexes that work together to produce mycolic acid in Mtb [58]. These Pks13-derived lipid metabolites (mycolic acids) are important constituents of Mtb’s distinctively sophisticated and lipid-rich cell wall [59], which has been suggested as a way for it to live in hostile environments in host macrophages while also providing an inherent resistance to numerous anti-microbial medications [60]. As it is recognized that these mycolic acids, a feature of the genus mycobacterium, are essential for the survival of this pathogen, disruption of this important biosynthesis pathway is a promising drug target for TB mitigation [59,60].
One of the important enzymes of the Pks enzyme family is Pks13, which is responsible for the condensation of two fatty acid chains into α-alkyl β-ketoacyl, a primary precursor of the mycolates. Therefore, Pks13 is a crucial enzyme for mycobacterial survival, making it a desirable new target for the pursuit of possible anti-tuberculosis drug candidates [61]. Research has been going on to identify drugs targeting this Pks13 enzyme, and several benzofuran-based scaffold-carrying compounds have been identified as potent repressive agents of Pks13 using structure-based drug design techniques [17,42,43,62]. These novel benzofurans oxadiazoles BF1–16 had strong anti-Pks13 activity in various investigational models [46,63]. Moreover, benzofuran-based compounds have also been identified to target other vital enzymes of Mtb [64]. Taking into account these potent inhibitory activities of benzofuran-based compounds against Mycobacterium tuberculosis, we will evaluate the potential anti-Mtb activities of our synthesized compounds (BF1 to BF16) in this study by utilizing computer-aided drug discovery techniques (CADD) by targeting the important Pks13 enzyme of Mtb.
2.2. Molecular Docking Investigations of BF1–BF16 against the Pks13 Enzyme
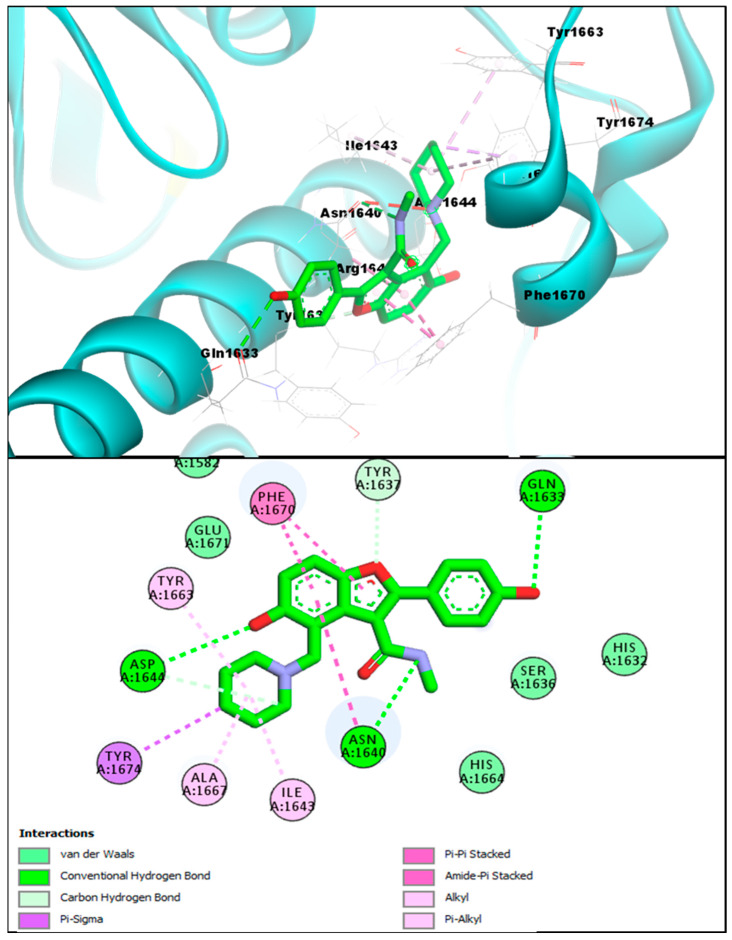
The in silico molecular docking approach was utilized to screen the 1,3,4-oxadiazole based benzofuran compounds via MOE (molecular operating environment) against the Pks13 of Mtb, and these results were compared with the co-crystallized inhibitor (TAM-16) of Pks13.The standard reference benzofuran TAM-16 inhibitor of anti-Mtb displayed an excellent binding affinity score (−14.61 kcal/mol) due to its strong binding interaction with the Pks13 enzyme active site (which is involved in the Mtb mycolic acid biosynthesis). The conformation analysis of the interaction of TAM-16 inhibitor with the active site pocket of Pks13 indicated that the TAM-16 inhibitor interacts with multiple amino acids residues (ASP1644, ASN1640, and GLN1633). The TAM-16 inhibitor made different multiple conventional and carbon-hydrogen-type hydrogen bonds with different amino acids of the active site. In the analysis, the Pks13 and TAM-16 protein-ligand complex demonstrated several other Pi-Pi and Amide-Pi Stacked-type molecular interactions. In addition, other types of molecular interactions—such as Alkyl, Pi-Alkyl, and Pi-Sigma interactions, which stabilize a compound inside a pocket—were also observed with the ILE1643, TYR1663, ALA1667, and TYR1674 between the Pks13 and the TAM-16 inhibitor. Furthermore, researchers that first discovered TAM-16 against Pks13 have stated that it exerts its inhibitory action by obstructing access to the Pks13 active site, which houses the catalytic triad (Ser1533, Asp1560, and His1699); in this study, it can be seen that TAM-16 also occupied the active site pocket and blocked access to these residues, as seen in Figure 5.
Figure 5.
TAM-16 inhibitor (upper panel) 3D pose (obtained through molecular docking) with the Pks13 interacting residues labeled, and its 2D interactive pose (lower panel) with the Pks13 enzyme.
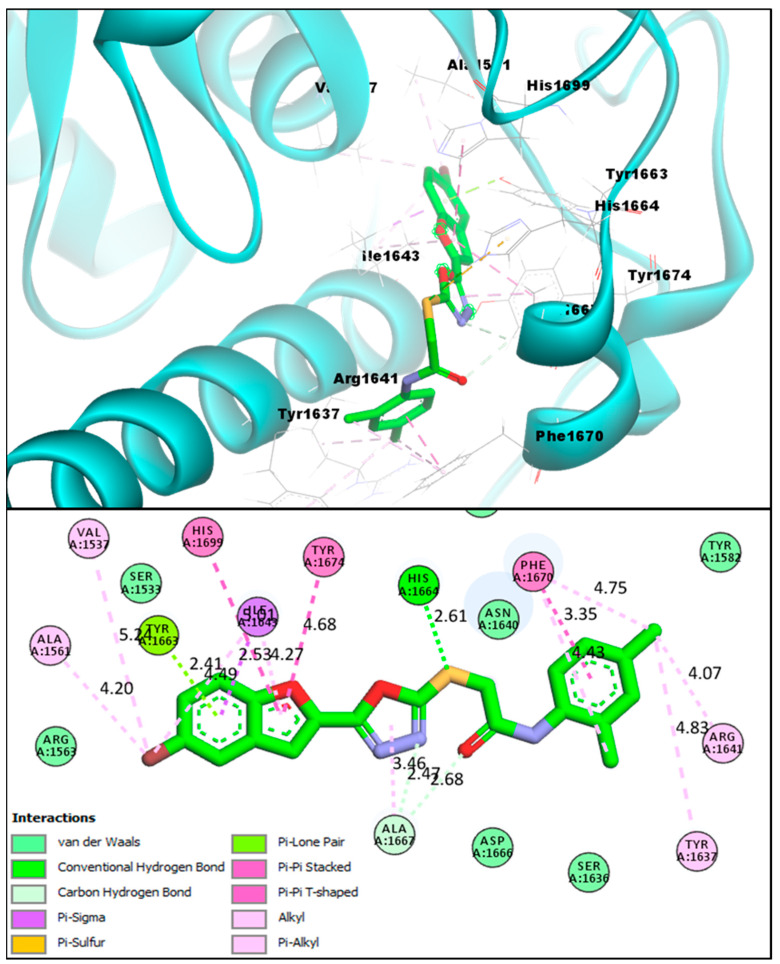
The afforded benzofuran molecules demonstrated strong binding affinities and robust interactions with the Pks13 enzyme active site in comparison to the benzofuran-based TAM-16 reference standard inhibitor. Out of the 16 novel synthesized analogs BF1 to BF16, three of them, BF3, BF4, and BF8 showed similar affinities to that of TAM-16 with the Mtb Pks13 enzyme. The conformation analysis of the pose and binding affinity of benzofuran-appended 1,3,4-oxadiazole derivative BF3 showed the binding affinity score (−14.23 kcal/mol) with the Pks13 active site due to the multiple molecular interactions with the Pks13 receptor residues. The benzofuran ring of the derivative BF3 demonstrated hydrogen bonds of conventional and carbon-hydrogen types with TYR1663, along with an H-bond between the HIS1664 and the sulphur atom. Moreover, other interactions such as Pi-Pi T-shaped (With the HIS1699 catalytic residue), Pi-Pi Stacked, Pi-Sigma and Alkyl were present, as were Pi-Alkyl interactions between the benzofuran ring and the Pks13. Several of the Pks13 receptor residues also made Van der Waals and Pi-Lone Pair molecular interactions with this compound; they are graphically presented in Figure 6.
Figure 6.
BF3 compound’s 3D pose (upper panel) interacting receptor residues are labeled, and its 2D interactive pose (lower panel) with the Pks13 enzyme.
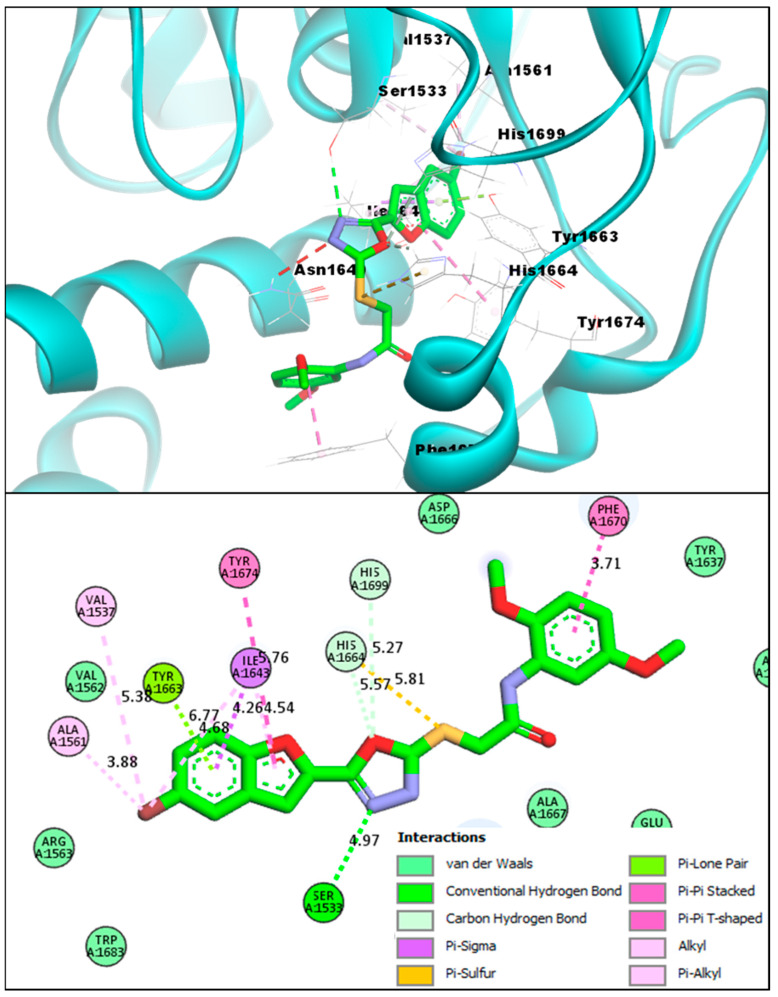
During the molecular docking studies, compound BF4 also showed a strong binding affinity score with the Pks13 active site (−14.82 kcal/mol) as compared to the TAM-16 binding affinity, which was (−14.61 kcal/mol) with the Pks13 enzyme; BF4 showed relatively stronger binding to the active site of the target protein. Furthermore, the interaction analysis of BF4 and the Pks13 protein complexes showed that BF4 directly interacted with the catalytic residues (Ser1533 and His1699), which are directly involved in the mycolic acid synthesis and are essential to the Pks13 activity. The benzofuran BF4 blocked access to these catalytic residues by interacting similarly to the TAM-16 inhibitor, as mentioned in previous paragraphs. It can be seen in Figure 7 that BF4 was able to engage the HIS1699 catalytic residue via a carbon-hydrogen-type hydrogen bonding with the oxygen atom of the oxadiazole ring. This oxadiazole ring’s nitrogen atom also engaged the other important catalytic residue (SER1533) by forming a conventional hydrogen bond. Furthermore, the benzofuran moiety of BF4 also made multiple molecular contacts, as was previously seen in the BF3 and Pks13 complex, and formed a hydrogen bond with the TYR1663, a Pi-Sigma interaction with the ILE1643, and multiple stabilizing interactions with Alkyl, Pi-Alkyl, Pi-Pi T-shaped and Pi-Pi Stacked; these Pi-Sulfur and Pi-Sigma interactions were also present in BF4 and the Pks13 complex.
Figure 7.
BF4 compound’s 3D pose (upper panel) interacting receptor residues are labeled, and its 2D interactive pose (lower panel) with the Pks13 enzyme.
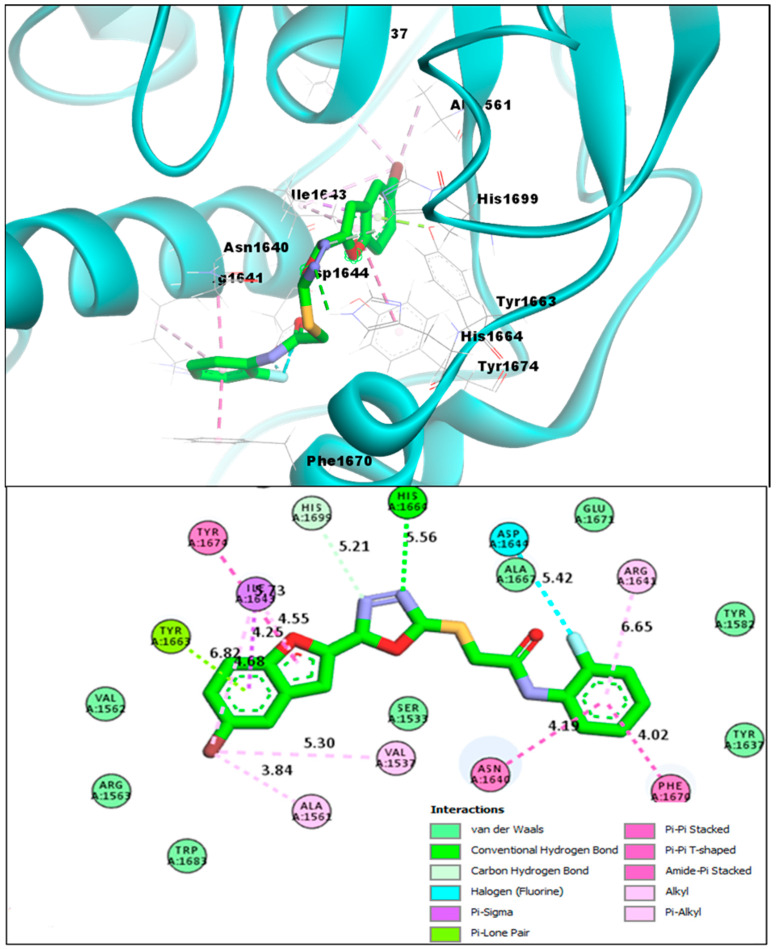
The third novel benzofuran BF8 also showed comparable binding affinity in comparison to that of TAM-16, and was able to bind to the Pks13 active site with a binding affinity score of −14.11 kcal/mol. It also directly engaged one of the crucial catalytic residues HIS1699 with its oxadiazole ring’s nitrogen atom via a conventional H-bond. Moreover, the benzofuran moiety of BF8 also showed stable molecular interactions of multiple types with the Pks13 receptor residues, and the TYR1663 made an H-bond with the bromine atom of this ring and made Alkyl and Pi-Alkyl interactions, as previously seen in the other benzofurans. In addition, other molecular interactions, i.e., Pi-Pi T-shaped, Pi-Pi Stacked-type, Amide-Pi Stacked, Pi-Sigma, and interactions of fluorine on the phenyl ring of BF8 with the ASP1644 of Pks13 receptor were also seen in BF8 and the Pks13 protein complex, as seen in Figure 8.
Figure 8.
BF8 compound’s 3D pose (upper panel), the interacting receptor residues are labeled, and its 2D interactive pose (lower panel) with the Pks13 enzyme.
An overview of the binding affinity scores of the studied bromo-substituted benzofuran-1,3,4-oxadiazoles BF1–BF9 and the interactive residues engaged by these compounds in the active pocket of the Pks13 enzyme are presented in Table 1; while the bromo-unsubstituted benzofuran-1,3,4-oxadiazole structural hybrids BF10–BF16 that showed less binding affinity scores with the Pks13 enzyme are presented in the Supplementary Table S1.
Table 1.
The molecular docking profile of bromobenzofuran-oxadiazoles BF1–BF9 against Pks13.
| Compounds | Binding Affinities | Interacting Residues of Pks13 | Interaction Types |
|---|---|---|---|
| BF1 | −12.93 kcal/mol | ILE1643, TYR1663, HIS1632, HIS1699, ALA1667, TYR1674, | Carbon-Hydrogen Bond, Van der Waals, Pi-Pi T-Shaped, Pi-Alkyl, and Alkyl. |
| BF2 | −12.71 kcal/mol | ASN1640, ILE1643, TYR1637, TYR1663, HIS1632, ALA1667, TYR1674, PHE1670 | C-Hydrogen Bond, Van der Waals, Pi-Pi T-Shaped, Pi-Pi Stacked, and Alkyl. |
| BF3 | −14.23 kcal/mol | VAL1537, ALA1561, PHE1637, ARG1641, ILE1643, TYR1663, HIS1664, ALA1667, PHE1670, TYR1674, HIS1699 | Conventional H-bond, C-Hydrogen Bond, Van der Waals, Pi-Pi T-Shaped, Pi-Alkyl, Pi-Lone pair, Pi-Sulfur, Pi-Sigma, and Pi-Pi Stacked |
| BF4 | −14.82 kcal/mol | VAL1537, SER1533, ALA1561, VAL1537, TYR1674, ILE1643, PHE1670, ALA1667 | Conventional H-bond, C-Hydrogen Bond, Van der Waals, Pi-Pi T-Shaped, Pi-Alkyl, Pi-Lone pair, Pi-Sulfur, Pi-Sigma, and Pi-Pi Stacked |
| BF5 | −12.31 kcal/mol | ALA1561, TYR1663, ILE1643, HIS1664, TYR1674, ALA1667 | C-Hydrogen Bond, Van der Waals, Pi-Pi T-Shaped, Pi-Alkyl, Pi-Lone pair, and Alkyl. |
| BF6 | −11.89 kcal/mol | SER1533, ALA1667, ALA1561, TYR1663, ILE1643, HIS1664, GLN1633, TYR1674 | Conventional H-bond, C-Hydrogen Bond, Van der Waals, Pi-Pi T-Shaped, Pi-Alkyl, Pi-Lone pair, Halogen, and Alkyl. |
| BF7 | −12.23 kcal/mol | HIS1632, TYR1637, ILE1643, TYR1663, ALA1667, PHE1670, TYR1674 | Carbon-Hydrogen Bond, Van der Waals, Pi-Pi Stacked, Pi-Alkyl, and Alkyl. |
| BF8 | −14.11 kcal/mol | VAL1537, ALA1561, TYR1663, ASN1640, ILE1643, PHE1670, ARG1641, ASP1644, HIS1664 | Conventional H-bond, C-Hydrogen Bond, Van der Waals, Pi-Pi T-Shaped, Pi-Alkyl, Pi-Lone pair, Amide-Pi Stacked |
| BF9 | −13.44 kcal/mol | ILE1643, ALA1667, PHE1670, VAL1562, HIS1699, TYR1674, TYR1637 | Conventional H-bond, C-Hydrogen Bond, Van der Waals, Pi-Pi T-Shaped, Pi-Pi Stacked, Pi-Alkyl, and Alkyl |
| TAM-16 (Standard) | −14.61 kcal/mol | SER1533, GLN1633, ASN1640, ASP1644, ILE1643, TYR1663, ALA1667, PHE1670, TYR1674 | Conventional H-bond, C-Hydrogen Bond, Van der Waals, Pi-Pi Stacked, Pi-Alkyl, Amide Pi-Stacked, Pi-Sigma, and Alkyl |
2.3. Structure-Activity Relationship (SAR) of Bromobenzofuran-1,3,4-Oxadiazoles BF3, BF4, and BF8
The analysis of the structure-activity relationship (SAR) of the novel 5-bromobenzofuran-oxadiazole compounds BF1–BF9 revealed that the simple benzofuran moiety containing oxadiazole molecules BF10–BF16 showed less binding affinity towards the Pks13 enzyme active site as compared to the 5-bromo moiety-based benzofuran-oxadiazoles. Among the 5-bromobenzofuran-oxadiazole compounds, BF3 and BF8 compounds having methyl (-CH3) and highly electronegative atom fluorine on the phenyl rings (Figure 9) displayed comparable binding affinities with reference to the benzofuran TAM-16 standard Pks13 inhibitor. Meanwhile, the 2,5-dimehoxy functionality containing the BF4 molecule demonstrated stronger binding affinities due to stable conformation, alignments, robust interactions, and direct bindings to the catalytic residues of Pks13 active site pocket compared to the standard TAM-16 inhibitor, which only blocked access to the Pks13 of Mtb active site pocket residues. Overall, the SAR study of all B1–BF9 predicted that phenyl position 2 of the N-phenyl acetamide fragment is more active in comparison to other positions in the S-alkylated 5-bromobenzofuran-oxadiazoles tethered N-phenyl acetamides BF1–BF9. These findings suggest that the in silico identified compounds can be effective novel anti-Mtb agents, and may help tackle the resistant strains of Mtb and reduce the treatment times if used in combinatorial therapy against Mycobacterium tuberculosis infections.
Figure 9.
Structural data of benzofuran-1,3,4-oxadiazole derivatives BF1–BF16 and TAM-16 inhibitor.
2.4. ADMET and Drug-Likeness Studies of Benzofuran-1,3,4-Oxadiazoles BF1–BF16
The ADMET and drug likeness studies of novel benzofuran clubbed 1,3,4-oxadiazole compounds BF1–BF9 are already reported by Irfan et al. [23,45,52]). In this study, ADMET and drug likeness studies of benzofuran oxadiazoles BF10–BF16 (Supplementary Tables S2 and S3) were carried out in order to check their profile in comparison to previously reported derivatives BF1–BF9. In general, benzofuran oxadiazoles BF1–BF16 showed good human intestinal absorptions and were classified as HIA+ based on pharmacokinetics and ADMET analysis. The novel benzofuran-appended 1,3,4-oxadiazoles demonstrated acceptable lipophilic (iLogP) characteristics and good Log S (ESOL) water solubility values. Additionally, they were not P-gp protein substrates (P-glycoprotein, or P-gp, is a transporter protein of cell membranes that controls the efflux of substances and medications from cells). Studies on metabolism have revealed that these substances are CYP450 3A4 substrates, which means that after these drug-like compounds have completed their task inside the body, the CYP450 3A4 can easily biotransform these substances inside the liver before sending them to the excretory organs for excretion from the body. These novel compounds were also non-inhibitors of the renal-OCT proteins (transporter proteins), which are crucial in the detoxifying/excretion of exogenous chemicals/drugs from the body. The toxicity investigations of these substances also revealed that they are not carcinogenic, non-AMES toxic, do not affect or inhibit the ThERG II ion channel that regulates cardiac action potential repolarization, and are non-interferers in its regular operation. According to these studies, just like BF1–BF9, the derivatives under study BF10–BF16 had shown favorable ADMET properties compared to the standard TAM-16, which shows that these compounds, if utilized, would pose no significant health hazards to its subjects upon administration.
Moreover, the drug-likeness investigations involving identifying these compounds’ physicochemical properties and medicinal chemistry showed that these BF1–BF9 and BF10–BF16 compounds had an excellent topological surface area (TPSA), acceptable molecular weight values, and good synthetic accessibility scores. These benzofuran BF1–BF9 and BF10–BF16 compounds followed the drug-likeness rules, such as Pfizer and Lipinski’s drug rules. These compounds also showed no PAINS alerts, and along with this, they also followed the Golden Triangle rule and had good bioavailability scores (greater than 0.10). ADMET and drug-likeness data of BF10–BF16 along with the reference compound TAM-16 are presented in the Supplementary Tables S2 and S3, respectively.
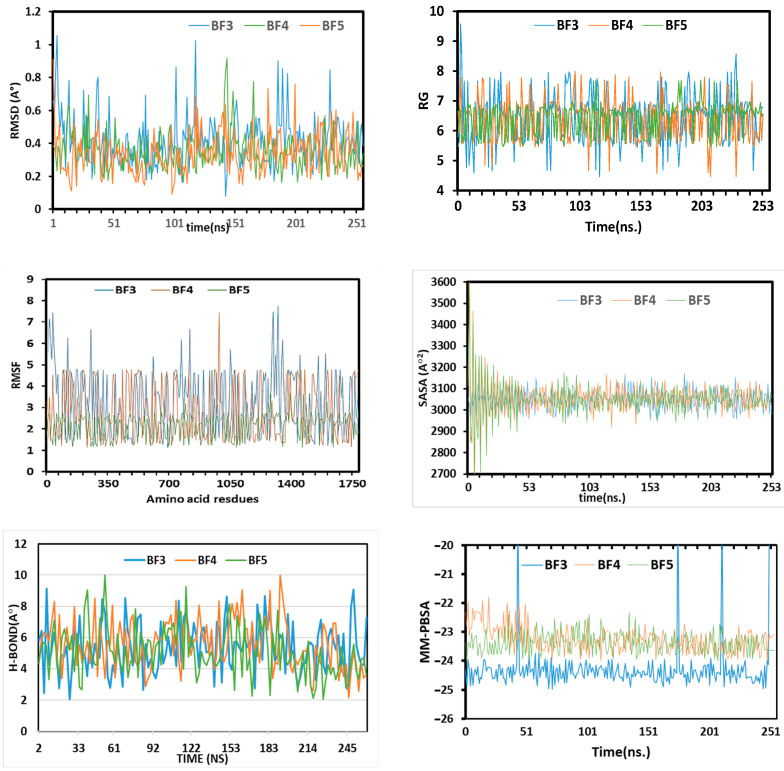
2.5. MD Simulations Study of Benzofuran-1,3,4-oxadiazoles BF3, BF4, and BF8
The variation and stability of the in silico predicted bioactive benzofuran-1,3,4-oxadiazoles BF3, BF4, and BF8 were studied by applying the C-alpha atoms root means square deviation (RMSD) approach. The three complexes displayed the initial upper phase, which resulted in the flexible behavior depicted in Figure 10. At the 25 ns simulation time, the complexes reached a steady state and the complexes retained stability until the simulations’ last segment. On the other hand, BF3 had fluctuations at 150 ns, 180 ns, and 230 ns. The higher RMSD for BF3 than other compounds demonstrates how these complexes are more adaptable than the other molecules, BF4 and BF8. The analyzed complexes were defined as having a stable comparative characteristic because their RMSD was below 2.5 during the simulation. The SASA simulation (solvent-accessible-surface-area) was carried out on complexes BF3, BF4, and BF8. The SASA simulation approach was utilized to study the variation of the complexes’ topology, which showed that higher SASA reflected the extent of the surface volumes, while the elongated nature defined the lower SASA, as shown in Figure 9. Their stability was proved by the steady-state for BF3, BF4, and BF8 after 48 ns and the low fluctuation degree for SASA profiles along the simulated trajectories. Additionally, each complex had SASA degrees that were roughly comparable, and the interaction over BF3, BF4, and BF8 compounds described these protein complexes in their compact form. The BF3, BF4, and BF8 complexes were analyzed for radius-gyration (RG) and trajectories. The trajectories demonstrated the flexibility and degree of mobility. The complexes BF3, BF4, and BF8 RG steady degree appeared at 7 ns.
Figure 10.
The molecular dynamics simulation trajectories from 250-ns simulation time.
To assess the flexibility of the residues of amino acids, the root-means-square-fluctuations (RMSF) were likewise also explored (Figure 10). The high Firmness of BF4 and BF8 complexes was demonstrated by their low RMSF values of 2.5 Å, but the relative flexibility of the back-bone of amino acid residues in the BF3 complex was demonstrated by its growing RMSF value of 6Å. Additionally, the small variations in the RMSD of BF3, BF4, and BF8 systems demonstrated loops variations in Mtb Pks13, which are naturally flexible. These RMSD variations correspond to enzyme structure adaptations in order to strongly engage the compounds at the binding site, as suggested by the H-bonding pattern. [65,66].
The H-bond played an important role in identifying the stability of the interaction-strength in the ligand and protein. The in silico predicted bioactive BF3, BF4, and BF8 have constant H-bonds range between 2 and 10 in the simulation process. The changing H-bond between the ligand-enzyme may suggest that the conformation around the ligands inside the binding site change through simulation. Overall, simulations supported the high stability of all protein-ligand complexes.
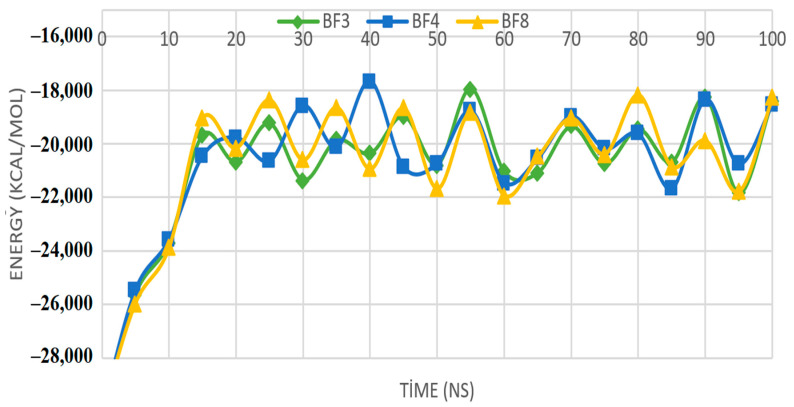
2.6. MM-PBSA Investigations of the Most In Silico Bioactive Benzofuran-1,3,4-oxadiazoles
Deciphering intermolecular interactions and energies at different nanoseconds are important to unveil microscopic information important for guiding stable docked complexes. This in turn ensures the selection of compounds that can inhibit the receptor enzyme. Although the ligand molecules are pretty flexible in the calculations, the Pks13 protein does not have this flexibility. In Molecular Mechanics-Poisson-Boltzmann surface area (MM-PSBA) calculations, the interaction between the ligand and Pks13 protein is done at the ns level. Both the ligand molecule and the Pks13 protein have flexibility in calculations of MM-PSBA. The interaction occurring in these calculations were examined every 10 ns, and the energy change is given in Figure 11.
Figure 11.
Display of Gibbs free energy values of protein and ligand molecules at ten ns intervals.
The generated graph displays the binding free energy variations and changes for each interval of ten (ns), along with standard deviations (±) given in Table 2. The high affinity bromobenzofuran-1,3,4-oxadiazole binders to Mtb Pks13 were BF3, BF4, and BF8 molecules, which were then compared to one another. Using this comparison, calculations were performed to support the (MM-PBSA) method’s estimation of the bonding’s free energies. The relevant parameters’ negative values signify stronger binding [67]. According to calculations using equation-1, the average values of Gibbs free energies are −31.4 kcal/mol for Pks13+BF3, −48.8 for Pks13+BF4, and −41.5 for Pks13+BF8. It can be seen in Table 2 that at each ns, the compounds showed robust strong intermolecular interactions energy. This further demonstrates the formation of high stable complexes and the strong binding of the compounds to the Mtb Pks13 enzyme. However, as standard deviation values are moderate to high, further extensive calculations are needed to validate the energy values. In light of these results, it can be seen that the free energy values of these three molecules show that they may possess better repressive properties against the important Mtb Pks13 enzyme.
Table 2.
The binding free energy changes and deviations in each ten (ns) interval. The energy values are presented in kcal/mol.
| Nanoseconds | Pks13+BF3 | Pks13+BF4 | Pks13+BF8 |
|---|---|---|---|
| 10 | −59.4 ± 149.6 | −956.2 ± 586.2 | −87.8 ± 235.6 |
| 20 | −135.2 ± 235.5 | −105.3 ± 387.4 | −508.9 ± 245.1 |
| 30 | −95.8 ± 269.3 | −912.3 ± 189.3 | −354.2 ± 245.3 |
| 40 | −570.3 ± 684.2 | −245.3 ± 245.6 | −150.8 ± 250.4 |
| 50 | −856.2 ± 345.6 | −856.3 ± 409.8 | −750.4 ± 150.6 |
| 60 | −135.2 ± 248.6 | −301.7 ± 204.8 | −723.3 ± 523.6 |
| 70 | −486.3 ± 367.3 | −501.1 ± 193.5 | −685.8 ± 351.2 |
| 80 | −648.8 ± 385.2 | −1101.3 ± 497.6 | −289.7 ± 487.5 |
| 90 | −329.2 ± 301.2 | −687.5 ± 260.1 | −350.4 ± 293.7 |
| 100 | −300.8 ± 283.2 | −423.4 ± 305.3 | −145.8 ± 354.6 |
3. Materials and Methods
3.1. Chemistry
All the benzofuran-oxadiazole structural motifs BF1–16 were afforded, and their characterization data were published by Irfan et al. [23,45,52]. The structures of benzofuran-1,3,4-oxadiazoles BF1–BF16 along with the TAM-16 standard reference inhibitor structure are given in Figure 11.
3.2. Molecular Docking of Benzofuran-1,3,4-oxadiazoles BF1–BF16
The protein PDB structure of the target enzyme Pks13 of Mycobacterium tuberculosis was achieved from the RCSB to carry out the molecular docking study (computational research) [68] website with the PDB Identifier (5V3Y) [62]. The molecular docking study of sixteen novel benzofuran-1,3,4-oxadiazoles was carried out with MOE (Ver-2009.10) software [69]. The first step was the preparation of protein structure of the Pks13 enzyme by removing water molecules and heteroatoms from the protein PDB structure with the help of Biovia DS [70] software for molecular docking study. The Chem-draw professional (Ver-16) software [71] (by PerkinElmer Informatics) was used to draw the structures of benzofuran-1,3,4-oxadiazole ligands BF1–BF16 and saved in the mol format for further studies. Before docking, the ligand structures were loaded in the MOE, and their energy was minimized via the MMFF94x forcefield, and the partial charges were also added to the ligand structures. Using the Triangle Matcher placement strategies, the compounds were docked in the binding pocket and scored by the Dock module using the London-dG scoring function of MOE. The protein PDB was opened in MOE, and was 3D-protonated using the Amber99-ff. The active site of the Pks13 was located and selected using the Site Finder function of MOE. The ligand-protein interaction was viewed using the software Biovia DS Studio (Ver-2017) [72].
3.3. ADMET and Drug-Likeness Investigations of Benzofuran-1,3,4-oxadiazoles
The ADME and drug-likeness studies of benzofuran-1,3,4-oxadiaole compounds were carried out by utilizing the Swissadme (Ver-1) [73] and ADMET lab (Ver-2.0) [74] online web-servers, while for the toxicity investigations, the ADMETSAR (Ver-1.0) [75,76] online server was utilized.
3.4. MD Simulation Study of the Most In Silico Bioactive BF3, BF4, and BF8 Derivatives
The MD Simulations of the most in silico predicted biologically active benzofuran-1,3,4-oxadiazole BF3, BF4, and BF8 scaffolds were performed by GROMACS. Using GROMACS (Ver-2021) and the Linux 5.4 package, MD simulation of the protein-ligand complexes was carried out. The ligand topologies were created using the PRODRG server, and the GROMOS96 forcefield was used as the force field for proteins. Simple point charge (SPC) water molecules in a rectangular box were used to solvate each complex. Na + and Cl + ions were added to electrically make the simulation system neutral, whereas salt concentrations of 0.15 mol/L were set in each system. All solvated complexes underwent energy minimization for 5000 steps using the steepest descent method. Different productions were run in the MD simulation, including the constant number of particle, pressure, and temperature (NPT) series and the constant number of particle, volume, and temperature (NVT) series. For the simulation, a V-rescale thermostat and a Parrinello-Rahman barostat were chosen, and the NVT and NPT series were conducted at 300 K and 1 atm for 300 ps. Finally, the production run was completed after 250 ns at 300 K. [77,78].
3.5. MM-PBSA Binding Free Energy Calculations of the Most In Silico Bioactive BF3, BF4, and BF8 Derivatives
Molecular mechanics Poisson-Boltzmann surface area (MM-PBSA) calculations of molecules were made with molecular dynamic calculations. The different types of binding free energies, i.e., Van der Waals, electrostatic, kinetic, and potential energy changes of the studied BF3, BF4, and BF8 molecules were determined for these calculations. In addition, this study examined the interactions between BF3, BF4, and BF8 molecules and the 5V3Y protein, which is the Pks13 protein. These interaction energies were investigated at 100 ns. As a result of the interaction of the three molecules studied with the protein, the values of the binding free energy change were calculated. This calculation is given in Equation (1).
| (1) |
In the above equation, gives the total binding free energy value between the ligand and the Pks13 protein. , , and values in the equation are the values of the ligand molecule, Pks13 receptor protein, and complex molecule, respectively [79].
4. Conclusions
In conclusion, the novel series of sixteen benzofuran-1,3,4-oxadiazoles BF1–BF16 was evaluated for their therapeutic inhibitory effect on Mtb Pks13 enzyme by applying various in silico approaches, such as molecular docking, MM-PBSA, pharmacokinetics, ADMET, and molecular dynamic simulations. The results of the CADD approach indicated that three in silico predicted lead compounds such as the 2,4-dimethyl moiety containing BF3, 2,5-dimethoxy moiety-based BF4, and 2-flouro moiety containing BF8 displayed excellent in silico anti-TB chemotherapeutic potential due to the strong interaction with the active site of the Pks13 enzyme and the greater stability of these complexes in comparison to the standard reference benzofuran drug TAM-16. The conformational pose and binding affinity analysis of BF3, BF4, and BF8 showed that these derivatives bind to the Pks13 active site with a binding affinity score of −14.23 kcal/mol, −14.82 kcal/mol, and of −14.11 kcal/mol, respectively, in comparison with the standard reference TAM-16 (−14.61 kcal/mol). The BF4 bromobenzofuran-1,3,4-oxadiazole showed higher binding affinity −14.82 kcal/mol than the reference Pks13 inhibitor TAM-16 (−14.61 kcal/mol), which was further confirmed by the MM-PBSA calculations and the MD simulations studies. The ADMET studies of all the screened bromobenzofuran-oxadiazole structural hybrids demonstrated a high degree of drug-likeness profile. Overall, it is seen that the bromobenzofuran-1,3,4-oxadiazole BF4 derivative has a more stable total binding free energy value against the 5V3Y protein. On the basis of different in silico techniques, 2,5-dimethoxy phenyl-substituted bromobenzofuran-1,3,4-oxdiazole BF4 is a more in silico predicted effective reagent than TAM-16, so this in silico bioactive BF4 can be a future lead anti-TB chemotherapeutic candidate after further in vitro and in vivo evaluations, which would be necessary to establish its chemotherapeutic efficacy against Mtb.
Acknowledgments
Authors acknowledge the Government college university Faisalabad for research facilities provided to carry out this research work.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ph16060829/s1. Binding affinities of benzofuran-1,3,4-oxadiazole BF10–16 are present in the supplementary Table S1; ADMET and drug-likeness data is depicted in Tables S2 and S3, respectively.
Author Contributions
Conceptualization, A.F.Z. and A.I.; methodology, A.I.; software, S.F., B.T., M.H.A., A.A.E. and S.A.; validation, S.F., B.T. and M.H.A.; formal analysis, S.F., R.J. and M.H.A.; investigation, R.J. and A.I.; resources, S.A.A.-H.; data curation, S.A.A.-H. and R.J.; writing—original draft preparation, A.I.; writing—review and editing, A.I., S.F., R.N., A.F.Z. and M.E.A.Z.; Visualization, A.I. and S.F; supervision, A.F.Z.; project administration, A.F.Z. and M.E.A.Z. funding acquisition, S.A.A.-H. and M.E.A.Z. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article and Supplementary material.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was supported by the Deanship of Scientific Research, Imam Mohammad Ibn Saud Islamic University, Saudi Arabia.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.WHO . Global Tuberculosis Report 2018. WHO; Geneva, Switzerland: 2018. [(accessed on 8 May 2023)]. pp. 1–277. Available online: https://apps.who.int/iris/handle/10665/274453. [Google Scholar]
- 2.Espinal M.A. The Global Situation of MDR-TB. Proc. Tuberc. 2003;83:44–51. doi: 10.1016/S1472-9792(02)00058-6. [DOI] [PubMed] [Google Scholar]
- 3.WHO . Global Tuberculosis Report 2022. WHO; Geneva, Switzerland: 2022. pp. 1–68. [Google Scholar]
- 4.Prasad R., Gupta N., Banka A. Multidrug-resistant tuberculosis/rifampicin-resistant tuberculosis: Principles of management. Lung India. 2018;35:78–81. doi: 10.4103/lungindia.lungindia_98_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sotgiu G., Migliori G.B. Facing Multi-Drug Resistant Tuberculosis. Pulm. Pharmacol. Ther. 2015;32:144–148. doi: 10.1016/j.pupt.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 6.Aspatwar A., Kairys V., Rala S., Parikka M., Bozdag M., Carta F., Supuran C.T., Parkkila S. Mycobacterium Tuberculosis β-Carbonic Anhydrases: Novel Targets for Developing Antituberculosis Drugs. Int. J. Mol. Sci. 2019;20:5153. doi: 10.3390/ijms20205153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaul G., Kapoor E., Dasgupta A., Chopra S. Management of multidrug-resistant tuberculosis in the 21st century. Drugs Today. 2019;55:215–224. doi: 10.1358/dot.2019.55.3.2927587. [DOI] [PubMed] [Google Scholar]
- 8.Saxena A.K., Singh A. Mycobacterial tuberculosis Enzyme Targets and their Inhibitors. Curr. Top. Med. Chem. 2019;19:337–355. doi: 10.2174/1568026619666190219105722. [DOI] [PubMed] [Google Scholar]
- 9.Harding E. WHO Global Progress Report on Tuberculosis Elimination. Lancet. Respir. Med. 2020;8:19. doi: 10.1016/S2213-2600(19)30418-7. [DOI] [PubMed] [Google Scholar]
- 10.Tsai Y.-P. Effectiveness of Tuberculosis Case Management. J. Microbiol. Immunol. Infect. 2015;48:S121. doi: 10.1016/j.jmii.2015.02.427. [DOI] [Google Scholar]
- 11.Zumla A., Nahid P., Cole S.T. Advances in the Development of New Tuberculosis Drugs and Treatment Regimens. Nat. Rev. Drug Discov. 2013;12:388–404. doi: 10.1038/nrd4001. [DOI] [PubMed] [Google Scholar]
- 12.Chimeh R.A., Gafar F., Pradipta I.S., Akkerman O.W., Hak E., Alffenaar J.W.C., van Boven J.F.M. Clinical and Economic Impact of Medication Non-Adherence in Drug-Susceptible Tuberculosis: A Systematic Review. Int. J. Tuberc. Lung Dis. 2020;24:811–819. doi: 10.5588/ijtld.19.0754. [DOI] [PubMed] [Google Scholar]
- 13.Wang X., Dowd C.S. The Methylerythritol Phosphate Pathway: Promising Drug Targets in the Fight against Tuberculosis. ACS Infect. Dis. 2018;4:278–290. doi: 10.1021/acsinfecdis.7b00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hiremathad A., Patil M.R., Chethana K.R., Chand K., Santos M.A., Keri R.S. Benzofuran: An Emerging Scaffold for Anti-microbial Agents. RSC Adv. 2015;5:96809–96828. doi: 10.1039/C5RA20658H. [DOI] [Google Scholar]
- 15.Xu Z., Zhao S., Lv Z., Feng L., Wang Y., Zhang F., Bai L., Deng J. Benzofuran Derivatives and Their Anti-Tubercular, Antibacterial Activities. Eur. J. Med. Chem. 2019;162:266–276. doi: 10.1016/j.ejmech.2018.11.025. [DOI] [PubMed] [Google Scholar]
- 16.Gill C., Jadhav G., Shaikh M., Kale R., Ghawalkar A., Nagargoje D., Shiradkar M. Clubbed [1,2,3] Triazoles by Fluorine Benzimidazole: A Novel Approach to H37Rv Inhibitors as a Potential Treatment for Tuberculosis. Bioorganic Med. Chem. Lett. 2008;18:6244–6247. doi: 10.1016/j.bmcl.2008.09.096. [DOI] [PubMed] [Google Scholar]
- 17.Irfan A., Sabeeh I., Umer M., Naqvi A.Z., Fatima H., Yousaf S., Fatima Z. A Review On The Therapeutic Potential of Quinoxaline Derivatives. World J. Pharm. Res. 2017;6:47–68. [Google Scholar]
- 18.Rubab L., Afroz S., Ahmad S., Hussain S., Nawaz I., Irfan A., Batool F., Kotwica-Mojzych K., Mojzych M. An Update on Synthesis of Coumarin Sulfonamides as Enzyme Inhibitors and Anticancer Agents. Molecules. 2022;27:1604. doi: 10.3390/molecules27051604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Irfan A., Batool F., Irum S., Ullah S., Umer M., Shaheen R., Chand A.J. A Therapeutic Journey Of Sulfonamide Derivatives As Potent Anti-Cancer Agents: A Review. WJPR. 2018;7:257–270. [Google Scholar]
- 20.Aziz H., Zahoor A.F., Shahzadi I., Irfan A. Recent Synthetic Methodologies Towards the Synthesis of Pyrazoles. Polycycl. Aromat. Compd. 2019;41:698–720. doi: 10.1080/10406638.2019.1614638. [DOI] [Google Scholar]
- 21.Irfan A., Batool F., Ahmad S., Ullah R., Sultan A., Sattar R., Nisar B., Rubab L. Recent trends in the synthesis of 1,2,3-thiadiazoles. Phosphorus Sulfur Silicon Relat. Elem. 2019;194:1098–1115. doi: 10.1080/10426507.2019.1633323. [DOI] [Google Scholar]
- 22.Irfan A., Faisal S., Ahmad S., Al-Hussain S.A., Javed S., Zahoor A.F., Parveen B., Zaki M.E.A. Structure-Based Virtual Screening of Furan-1,3,4-Oxadiazole Tethered N-phenylacetamide Derivatives as Novel Class of hTYR and hTYRP1 Inhibitors. Pharmaceuticals. 2023;16:344. doi: 10.3390/ph16030344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Irfan A., Faiz S., Rasul A., Zafar R., Zahoor A.F., Kotwica-Mojzych K., Mojzych M. Exploring the Synergistic Anticancer Potential of Benzofuran–Oxadiazoles and Triazoles: Improved Ultrasound-and Microwave-Assisted Synthesis, Molecular Docking, Hemolytic, Thrombolytic and Anticancer Evaluation of Furan-Based Molecules. Molecules. 2022;27:1023. doi: 10.3390/molecules27031023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Faiz S., Zahoor A.F., Ajmal M., Kamal S., Ahmad S., Abdelgawad A.M., Elnaggar M.E. Design, Synthesis, Antimicrobial Evaluation, and Laccase Catalysis Effect of Novel Benzofuran–Oxadiazole and Benzofuran–Triazole Hybrids. J. Heterocycl. Chem. 2019;56:2839–2852. doi: 10.1002/jhet.3674. [DOI] [Google Scholar]
- 25.Bhargava S., Rathore D. Synthetic Routes and Biological Activities of Benzofuran and Its Derivatives: A Review. Lett. Org. Chem. 2017;14:381–402. doi: 10.2174/1570178614666170321125853. [DOI] [Google Scholar]
- 26.Nevagi R.J., Dighe S.N., Dighe S.N. Biological and Medicinal Significance of Benzofuran. Eur. J. Med. Chem. 2015;97:561–581. doi: 10.1016/j.ejmech.2014.10.085. [DOI] [PubMed] [Google Scholar]
- 27.Hiremathad A., Chand K., Tolayan L., Rajeshwari, Keri R.S., Esteves A.R., Cardoso S.M., Chaves S., Santos M.A. Hydroxypyridinone-Benzofuran Hybrids with Potential Protective Roles for Alzheimer’s Disease Therapy. J. Inorg. Biochem. 2018;179:82–96. doi: 10.1016/j.jinorgbio.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 28.Goyal D., Kaur A., Goyal B. Benzofuran and Indole: Promising Scaffolds for Drug Development in Alzheimer’s Disease. ChemMedChem. 2018;13:1275–1299. doi: 10.1002/cmdc.201800156. [DOI] [PubMed] [Google Scholar]
- 29.Zeni G., Lüdtke D.S., Nogueira C.W., Panatieri R.B., Braga A.L., Silveira C.C., Stefani H.A., Rocha J.B.T. New Acetylenic Furan Derivatives: Synthesis and Anti-Inflammatory Activity. Tetrahedron Lett. 2001;42:8927–8930. doi: 10.1016/S0040-4039(01)01984-0. [DOI] [Google Scholar]
- 30.Thévenin M., Thoret S., Grellier P., Dubois J. Synthesis of Polysubstituted Benzofuran Derivatives as Novel Inhibitors of Parasitic Growth. Bioorganic Med. Chem. 2013;21:4885–4892. doi: 10.1016/j.bmc.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Zhong M., Peng E., Huang N., Huang Q., Huq A., Lau M., Colonno R., Li L. Discovery of Novel Potent HCV NS5B Polymerase Non-Nucleoside Inhibitors Bearing a Fused Benzofuran Scaffold. Bioorganic Med. Chem. Lett. 2018;28:963–968. doi: 10.1016/j.bmcl.2018.01.029. [DOI] [PubMed] [Google Scholar]
- 32.Xie Y.S., Kumar D., Bodduri V.D.V., Tarani P.S., Zhao B.X., Miao J.Y., Jang K., Shin D.S. Microwave-Assisted Parallel Synthesis of Benzofuran-2-Carboxamide Derivatives Bearing Anti-Inflammatory, Analgesic and Antipyretic Agents. Tetrahedron Lett. 2014;55:2796–2800. doi: 10.1016/j.tetlet.2014.02.116. [DOI] [Google Scholar]
- 33.Rangaswamy J., Kumar H.V., Harini S.T., Naik N. Functionalized 3-(Benzofuran-2-Yl)-5-(4-Methoxyphenyl)-4,5-Dihydro-1H-Pyrazole Scaffolds: A New Class of Antimicrobials and Antioxidants. Arab. J. Chem. 2017;10:S2685–S2696. doi: 10.1016/j.arabjc.2013.10.012. [DOI] [Google Scholar]
- 34.Singh F.V., Chaurasia S., Joshi M.D., Srivastava A.K., Goel A. Synthesis and in Vivo Antihyperglycemic Activity of Nature-Mimicking Furanyl-2-Pyranones in STZ-S Model. Bioorganic Med. Chem. Lett. 2007;17:2425–2429. doi: 10.1016/j.bmcl.2007.02.036. [DOI] [PubMed] [Google Scholar]
- 35.Simonetti S.O., Larghi E.L., Bracca A.B.J., Kaufman T.S. Angular Tricyclic Benzofurans and Related Natural Products of Fungal Origin. Isolation, Biological Activity and Synthesis. Nat. Prod. Rep. 2013;30:941–969. doi: 10.1039/c3np70014c. [DOI] [PubMed] [Google Scholar]
- 36.Mei W., Ji S., Xiao W., Wang X., Jiang C., Ma W., Zhang H., Gong J., Guo Y. Synthesis and Biological Evaluation of Benzothiazol-Based 1,3,4-Oxadiazole Derivatives as Amyloid β-Targeted Compounds against Alzheimer’s Disease. Mon. fur Chem. 2017;148:1807–1815. doi: 10.1007/s00706-017-1993-x. [DOI] [Google Scholar]
- 37.Nieddu V., Pinna G., Marchesi I., Sanna L., Asproni B., Pinna G.A., Bagella L., Murineddu G. Synthesis and Antineoplastic Evaluation of Novel Unsymmetrical 1,3,4-Oxadiazoles. J. Med. Chem. 2016;59:10451–10469. doi: 10.1021/acs.jmedchem.6b00468. [DOI] [PubMed] [Google Scholar]
- 38.Calcagno A., D’Avolio A., Bonora S. Pharmacokinetic and Pharmacodynamic Evaluation of Raltegravir and Experience from Clinical Trials in HIV-Positive Patients. Expert Opin. Drug Metab. Toxicol. 2015;11:1167–1176. doi: 10.1517/17425255.2015.1056732. [DOI] [PubMed] [Google Scholar]
- 39.Bondock S., Adel S., Etman H.A., Badria F.A. Synthesis and Antitumor Evaluation of Some New 1,3,4-Oxadiazole-Based Heterocycles. Eur. J. Med. Chem. 2012;48:192–199. doi: 10.1016/j.ejmech.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 40.Sun J., Ren S.Z., Lu X.Y., Li J.J., Shen F.Q., Xu C., Zhu H.L. Discovery of a Series of 1,3,4-Oxadiazole-2(3H)-Thione Derivatives Containing Piperazine Skeleton as Potential FAK Inhibitors. Bioorganic Med. Chem. 2017;25:2593–2600. doi: 10.1016/j.bmc.2017.03.038. [DOI] [PubMed] [Google Scholar]
- 41.Prakash O., Kumar M., Kumar R., Sharma C., Aneja K.R. Hypervalent Iodine(III) Mediated Synthesis of Novel Unsymmetrical 2,5-Disubstituted 1,3,4-Oxadiazoles as Antibacterial and Antifungal Agents. Eur. J. Med. Chem. 2010;45:4252–4257. doi: 10.1016/j.ejmech.2010.06.023. [DOI] [PubMed] [Google Scholar]
- 42.Akhter M., Husain A., Azad B., Ajmal M. Aroylpropionic Acid Based 2,5-Disubstituted-1,3,4-Oxadiazoles: Synthesis and Their Anti-Inflammatory and Analgesic Activities. Eur. J. Med. Chem. 2009;44:2372–2378. doi: 10.1016/j.ejmech.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 43.Janardhanan J., Chang M., Mobashery S. The Oxadiazole Antibacterials. Curr. Opin. Microbiol. 2016;33:13–17. doi: 10.1016/j.mib.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahsan M.J., Samy J.G., Khalilullah H., Nomani M.S., Saraswat P., Gaur R., Singh A. Molecular Properties Prediction and Synthesis of Novel 1,3,4-Oxadiazole Analogues as Potent Antimicrobial and Antitubercular Agents. Bioorg. Med. Chem. Lett. 2011;21:7246–7250. doi: 10.1016/j.bmcl.2011.10.057. [DOI] [PubMed] [Google Scholar]
- 45.Irfan A., Zahoor A.F., Rasul A., Al-Hussain S.A., Faisal S., Ahmad S., Noor R., Muhammed M.T., Zaki M.E.A. BTEAC Catalyzed Ultrasonic-Assisted Synthesis of Bromobenzofuran-Oxadiazoles: Unravelling Anti-HepG-2 Cancer Therapeutic Potential through In Vitro and In Silico Studies. Int. J. Mol. Sci. 2023;24:3008. doi: 10.3390/ijms24033008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wilson C., Ray P., Zuccotto F., Hernandez J., Aggarwal A., Mackenzie C., Caldwell N., Taylor M., Huggett M., Mathieson M., et al. Optimization of TAM16, a Benzofuran That Inhibits the Thioesterase Activity of Pks13; Evaluation toward a Preclinical Candidate for a Novel Antituberculosis Clinical Target. J. Med. Chem. 2022;65:409–423. doi: 10.1021/acs.jmedchem.1c01586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Verma S.K., Verma R., Verma S., Vaishnav Y., Tiwari S.P., Rakesh K.P. Anti-Tuberculosis Activity and Its Structure-Activity Relationship (SAR) Studies of Oxadiazole Derivatives: A Key Review. Eur. J. Med. Chem. 2021;209:112886. doi: 10.1016/j.ejmech.2020.112886. [DOI] [PubMed] [Google Scholar]
- 48.Makane V.B., Krishna V.S., Krishna E.V., Shukla M., Mahizhaveni B., Misra S., Chopra S., Sriram D., Azger Dusthackeer V.N., Rode H.B. Novel 1,3,4-Oxadiazoles as Antitubercular Agents with Limited Activity against Drug-Resistant Tuberculosis. Future Med. Chem. 2019;11:499–510. doi: 10.4155/fmc-2018-0378. [DOI] [PubMed] [Google Scholar]
- 49.Desai N.C., Somani H., Trivedi A., Bhatt K., Nawale L., Khedkar V.M., Jha P.C., Sarkar D. Synthesis, Biological Evaluation and Molecular Docking Study of Some Novel Indole and Pyridine Based 1,3,4-Oxadiazole Derivatives as Potential Antitubercular Agents. Bioorgan. Med. Chem. Lett. 2016;26:1776–1783. doi: 10.1016/j.bmcl.2016.02.043. [DOI] [PubMed] [Google Scholar]
- 50.Chobe S.S., Kamble R.D., Patil S.D., Acharya A.P., Hese S.V., Yemul O.S., Dawane B.S. Green Approach towards Synthesis of Substituted Pyrazole-1,4-Dihydro,9-Oxa, 1,2,6,8-Tetrazacyclopentano[b]Naphthalene-5-One Derivatives as Antimycobacterial Agents. Med. Chem. Res. 2013;22:5197–5203. doi: 10.1007/s00044-013-0487-6. [DOI] [Google Scholar]
- 51.Dhumal S.T., Deshmukh A.R., Bhosle M.R., Khedkar V.M., Nawale L.U., Sarkar D., Mane R.A. Synthesis and Antitubercular Activity of New 1,3,4-Oxadiazoles Bearing Pyridyl and Thiazolyl Scaffolds. Bioorganic Med. Chem. Lett. 2016;26:3646–3651. doi: 10.1016/j.bmcl.2016.05.093. [DOI] [PubMed] [Google Scholar]
- 52.Irfan A., Zahoor A.F., Kamal S., Hassan M., Kloczkowski A. Ultrasonic-Assisted Synthesis of Benzofuran Appended Oxadiazole Molecules as Tyrosinase Inhibitors: Mechanistic Approach through Enzyme Inhibition, Molecular Docking, Chemoinformatics, ADMET and Drug-Likeness Studies. Int. J. Mol. Sci. 2022;23:10979. doi: 10.3390/ijms231810979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marimani M., Ahmad A., Duse A. The Role of Epigenetics, Bacterial and Host Factors in Progression of Mycobacterium Tuberculosis Infection. Tuberculosis. 2018;113:200–214. doi: 10.1016/j.tube.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 54.Ryndak M.B., Laal S. Mycobacterium tuberculosis Primary Infection and Dissemination: A Critical Role for Alveolar Epithelial Cells. Front. Cell. Infect. Microbiol. 2019;9:299. doi: 10.3389/fcimb.2019.00299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abdoli A., Falahi S., Kenarkoohi A. COVID-19-Associated Opportunistic Infections: A Snapshot on the Current Reports. Clin. Exp. Med. 2022;22:327–346. doi: 10.1007/s10238-021-00751-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Oh S., Park Y., Engelhart C.A., Wallach J.B., Schnappinger D., Arora K., Manikkam M., Gac B., Wang H., Murgolo N., et al. Discovery and Structure-Activity-Relationship Study of N-Alkyl-5-Hydroxypyrimidinone Carboxamides as Novel Antitubercular Agents Targeting Decaprenylphosphoryl-β-D-Ribose 2′-Oxidase. J. Med. Chem. 2018;61:9952–9965. doi: 10.1021/acs.jmedchem.8b00883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mohanty D., Sankaranarayanan R., Gokhale R.S. Fatty Acyl-AMP Ligases and Polyketide Synthases Are Unique Enzymes of Lipid Biosynthetic Machinery in Mycobacterium tuberculosis. Tuberculosis. 2011;91:448–455. doi: 10.1016/j.tube.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 58.Singh S., Singh D., Hameed S., Fatima Z. Biology of Mycobacterial Lipids. Academic Press; Cambridge, MA, USA: 2022. An Overview of Mycolic Acids. Structure–function–classification, biosynthesis, and beyond; pp. 1–25. [DOI] [Google Scholar]
- 59.Maitra A., Munshi T., Healy J., Martin L.T., Vollmer W., Keep N.H., Bhakta S. Cell Wall Peptidoglycan in Mycobacterium tuberculosis: An Achilles’ Heel for the TB-Causing Pathogen. FEMS Microbiol. Rev. 2019;43:548–575. doi: 10.1093/femsre/fuz016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Howard N.C., Marin N.D., Ahmed M., Rosa B.A., Martin J., Bambouskova M., Sergushichev A., Loginicheva E., Kurepina N., Rangel-Moreno J., et al. Mycobacterium tuberculosis Carrying a Rifampicin Drug Resistance Mutation Reprograms Macrophage Metabolism through Cell Wall Lipid Changes. Nat. Microbiol. 2018;3:1099–1108. doi: 10.1038/s41564-018-0245-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wellington S., Hung D.T. The Expanding Diversity of Mycobacterium tuberculosis Drug Targets. ACS Infect. Dis. 2018;4:696–714. doi: 10.1021/acsinfecdis.7b00255. [DOI] [PubMed] [Google Scholar]
- 62.Aggarwal A., Parai M.K., Shetty N., Wallis D., Woolhiser L., Hastings C., Dutta N.K., Galaviz S., Dhakal R.C., Shrestha R., et al. Development of a Novel Lead That Targets M. Tuberculosis Polyketide Synthase 13. Cell. 2017;170:249–259.e25. doi: 10.1016/j.cell.2017.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Çınaroğlu S.S., Timuçin E. Insights into an Alternative Benzofuran Binding Mode and Novel Scaffolds of Polyketide Synthase 13 Inhibitors. J. Mol. Model. 2019;25:130. doi: 10.1007/s00894-019-4010-y. [DOI] [PubMed] [Google Scholar]
- 64.He Y., Xu J., Yu Z.H., Gunawan A.M., Wu L., Wang L., Zhang Z.Y. Discovery and Evaluation of Novel Inhibitors of Mycobacterium Protein Tyrosine Phosphatase B from the 6-Hydroxy-Benzofuran-5-Carboxylic Acid Scaffold. J. Med. Chem. 2013;56:832–842. doi: 10.1021/jm301781p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lokhande K.B., Shrivastava A., Singh A. In silico discovery of potent inhibitors against monkeypox’s major structural proteins. J. Biomol. Struct. Dyn. 2023;25:1–16. doi: 10.1080/07391102.2023.2183342. [DOI] [PubMed] [Google Scholar]
- 66.Nagare S., Lokhande K.B., Swamy K.V. Docking and simulation studies on cyclin D/CDK4 complex for targeting cell cycle arrest in cancer using flavanone and its congener. J. Mol. Model. 2023;29:90. doi: 10.1007/s00894-023-05496-6. [DOI] [PubMed] [Google Scholar]
- 67.Gupta M.K., Vemula S., Donde R., Gouda G., Behera L., Vadde R. In-Silico Approaches to Detect Inhibitors of the Human Severe Acute Respiratory Syndrome Coronavirus Envelope Protein Ion Channel. J. Biomol. Struct. Dyn. 2021;39:2617–2627. doi: 10.1080/07391102.2020.1751300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Burley S.K., Berman H.M., Bhikadiya C., Bi C., Chen L., Di Costanzo L., Christie C., Dalenberg K., Duarte J.M., Dutta S., et al. RCSB Protein Data Bank: Biological Macromolecular Structures Enabling Research and Education in Fundamental Biology, Biomedicine, Biotechnology and Energy. Nucleic Acids Res. 2019;47:D464–D474. doi: 10.1093/nar/gky1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vilar S., Cozza G., Moro S. Medicinal Chemistry and the Molecular Operating Environment (MOE): Application of QSAR and Molecular Docking to Drug Discovery. Curr. Top. Med. Chem. 2008;8:1555–1572. doi: 10.2174/156802608786786624. [DOI] [PubMed] [Google Scholar]
- 70.Faisal S., Lal Badshah S., Kubra B., Sharaf M., Emwas A.H., Jaremko M., Abdalla M. Computational Study of SARS-CoV-2 Rna Dependent Rna Polymerase Allosteric Site Inhibition. Molecules. 2022;27:223. doi: 10.3390/molecules27010223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Accelrys Software Inc . Discovery Studio Modeling Environment, Release 3.5. Accelrys Software Inc.; San Diego, CA, USA: 2012. [Google Scholar]
- 72.Mills N. ChemDraw Ultra 10.0 CambridgeSoft, 100 CambridgePark Drive, Cambridge, MA 02140. Www.Cambridgesoft.Com. Commercial Price: $1910 for Download, $2150 for CD-ROM; Academic Price: $710 for Download, $800 for CD-ROM. J. Am. Chem. Soc. 2006;128:13649–13650. doi: 10.1021/ja0697875. [DOI] [Google Scholar]
- 73.Daina A., Michielin O., Zoete V. SwissADME: A Free Web Tool to Evaluate Pharmacokinetics, Drug-Likeness and Medicinal Chemistry Friendliness of Small Molecules. Sci. Rep. 2017;7:42717. doi: 10.1038/srep42717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Xiong G., Wu Z., Yi J., Fu L., Yang Z., Hsieh C., Yin M., Zeng X., Wu C., Lu A., et al. ADMETlab 2.0: An Integrated Online Platform for Accurate and Comprehensive Predictions of ADMET Properties. Nucleic Acids Res. 2021;49:W5–W14. doi: 10.1093/nar/gkab255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.GFYang H., Lou C., Sun L., Li J., Cai Y., Wang Z., Li W., Liu G., Tang Y. AdmetSAR 2.0: Web-Service for Prediction and Optimization of Chemical ADMET Properties. Bioinformatics. 2019;35:1067–1069. doi: 10.1093/bioinformatics/bty707. [DOI] [PubMed] [Google Scholar]
- 76.Cheng F., Li W., Zhou Y., Shen J., Wu Z., Liu G., Lee P.W., Tang Y. AdmetSAR: A Comprehensive Source and Free Tool for Assessment of Chemical ADMET Properties. J. Chem. Inf. Model. 2012;52:3099–3105. doi: 10.1021/ci300367a. [DOI] [PubMed] [Google Scholar]
- 77.Jo S., Kim T., Iyer V.G., Im W. CHARMM-GUI: A web-based graphical user interface for CHARMM. J. Comput. Chem. 2008;29:1859–1865. doi: 10.1002/jcc.20945. [DOI] [PubMed] [Google Scholar]
- 78.Lee J., Cheng X., Swails J.M., Yeom M.S., Eastman P.K., Lemkul J.A., Wei S., Buckner J., Jeong J.C., Qi Y., et al. CHARMM-GUIInput Generator for NAMD, GROMACS, AMBER, OpenMM, and CHARMM/OpenMM Simulations Using the CHARMM36Additive Force Field. J. Chem. Theory Comput. 2016;12:405–413. doi: 10.1021/acs.jctc.5b00935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Aktaş A., Tüzün B., Aslan R., Sayin K., Ataseven H. New Anti-Viral Drugs for the Treatment of COVID-19 Instead of Favipiravir. J. Biomol. Struct. Dyn. 2021;39:7263–7273. doi: 10.1080/07391102.2020.1806112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is contained within the article and Supplementary material.