Abstract
Clinically, it is highly challenging to promote recovery in patients with acute liver failure (ALF) and acute-on-chronic liver failure (ACLF). Despite recent advances in understanding the underlying mechanisms of ALF and ACLF, standard medical therapy remains the primary therapeutic approach. Liver transplantation (LT) is considered the last option, and in several cases, it is the only intervention that can be lifesaving. Unfortunately, this intervention is limited by organ donation shortage or exclusion criteria such that not all patients in need can receive a transplant. Another option is to restore impaired liver function with artificial extracorporeal blood purification systems. The first such systems were developed at the end of the 20th century, providing solutions as bridging therapy, either for liver recovery or LT. They enhance the elimination of metabolites and substances that accumulate due to compromised liver function. In addition, they aid in clearance of molecules released during acute liver decompensation, which can initiate an excessive inflammatory response in these patients causing hepatic encephalopathy, multiple-organ failure, and other complications of liver failure. As compared to renal replacement therapies, we have been unsuccessful in using artificial extracorporeal blood purification systems to completely replace liver function despite the outstanding technological evolution of these systems. Extracting middle to high-molecular-weight and hydrophobic/protein-bound molecules remains extremely challenging. The majority of the currently available systems include a combination of methods that cleanse different ranges and types of molecules and toxins. Furthermore, conventional methods such as plasma exchange are being re-evaluated, and novel adsorption filters are increasingly being used for liver indications. These strategies are very promising for the treatment of liver failure. Nevertheless, the best method, system, or device has not been developed yet, and its probability of getting developed in the near future is also low. Furthermore, little is known about the effects of liver support systems on the overall and transplant-free survival of these patients, and further investigation using randomized controlled trials and meta-analyses is needed. This review presents the most popular extracorporeal blood purification techniques for liver replacement therapy. It focuses on general principles of their function, and on evidence regarding their effectiveness in detoxification and in supporting patients with ALF and ACLF. In addition, we have outlined the basic advantages and disadvantages of each system.
Keywords: Liver failure, Transplantation, Blood purification, Liver replacement therapy, Artificial extracorporeal systems, Transplant-free survival
Core Tip: Elimination of liver toxins during liver failure is a highly difficult and complex process and demands a combination of multiple methods. Although the evolution of artificial extracorporeal systems is remarkable, it is still insufficient to meet the current therapeutic demands. Several methods and circuits are available, each one with different features, advantages, and disadvantages. There is an urgent need for more research, randomized controlled trials, and evidence. Implementation of protocols combining the available techniques in response to each patient’s special needs is probably the key to personalized treatment, as bridging therapy either to recovery or to liver transplantation.
INTRODUCTION
Artificial extracorporeal blood purification techniques offer the possibility of liver replacement therapy (LRT) in patients with acute liver failure (ALF) and acute-on-chronic liver failure (ACLF). Artificial liver support systems (LSSs) can efficiently remove cytokines and a wide variety of hepatotoxic metabolites, including ammonia, fatty acids, bilirubin, bile acids, and amino acids[1]. The removal of cytokines using LSSs has been shown to intervene in the immunologic processes occurring during ALF and ACLF. Thus, these system-based therapies are considered immunomodulatory interventions, with their widespread implementation in treating both septic patients and those with liver failure. An increasing number of studies are being conducted to evaluate the role of the immune system in the pathophysiology of liver failure, which presents certain features that differentiate ACLF from ALF. More specifically, ACLF is a clinical syndrome that is characterized by the acute decompensation of chronic, pre-existing liver disease, usually led by a precipitating event, such as an underlying infection and is often accompanied by multiorgan failure (MOF) and high mortality. The basis of the pathophysiological mechanisms in ACLF is the hyperinflammatory state, which is triggered by factors called pathogen- and damage-associated molecular patterns (PAMPs and DAMPs)[2]. On the other hand, ALF represents a life-threatening condition that is usually the result of an offending agent, such as medications or viral infections in patients without pre-existing liver disease. It is characterized by an overwhelming systemic inflammatory response, hepatocyte necrosis and accumulation of bile acids and ammonia, which can lead to permanent liver damage, encephalopathy and cerebral edema[3,4].
The production of toxins and vasoactive agents by intestinal bacteria and the accumulation of these molecules due to the diminished liver detoxification capacity play a significant role in the pathophysiology of liver failure[5]. The accumulation of these toxins induces complications of liver failure, such as increased intracranial pressure (ammonia) and hepatic encephalopathy (HE) (ammonia and amino acids). Furthermore, it is associated with increased mortality, especially in patients with high levels of bilirubin[6]. Therefore, the removal of all these deleterious molecules can protect patients from a wide variety of complications and dangers, thereby exerting beneficial effects.
Although progress has made these modalities very effective in removing their target molecules, whether this improves overall survival (OS), transplant-free survival (TFS) or even short-term survival, as bridging to liver transplantation (LT) is a question that remains to be answered. Nevertheless, except for plasma exchange (PE) therapy, none of these systems has resulted in favorable outcomes such as those mentioned in randomized controlled studies (RCTs), and only a few studies have systematically investigated these issues. This is largely attributed to complex liver physiology. Because each method individually has a narrow spectrum of toxin removal, a combination of methods is used in the majority of cases. The clinical condition of patients with ALF and ACLF is highly complex and is constantly changing, demanding adaptation to the modality applied; thus, only a combination that fits the specific clinical condition can be used. In addition, concerns exist about the loss of antibiotics and functional molecules such as albumin during these therapies, whereas cytokine removal is non-selective for most of these systems, leading to an imbalance between the levels of pro- and anti-inflammatory mediators, with unpredictable clinical effects.
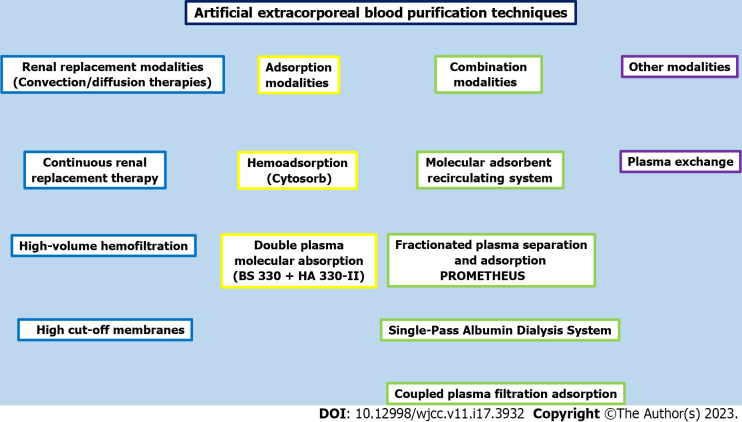
The present review outlines the principles of function and the applications of the most popular and widely available artificial extracorporeal systems for LRT (Figure 1). It describes their methods of detoxification, major advantages and disadvantages, their practice in patients with liver failure, and their effect on patients’ survival.
Figure 1.
Most popular available blood purification methods with artificial extracorporeal systems for liver replacement therapy.
RENAL REPLACEMENT MODALITIES (CONVECTION/DIFFUSION THERAPIES)
Continuous renal replacement therapy
Apart from liver dysfunction, patients with ALF and ACLF often present with decompensation of functions of other organs, including the kidneys, with relative rates reaching up to 70%[7]. Renal replacement therapy (RRT) is often necessary in these patients either due to concomitant renal failure or due to a liver indication, in most cases hyperammonemia. Hyperammonemia is a common metabolic disorder, which is associated with cerebral edema and elevated intracranial pressure, especially in patients with ALF and rarely in those with ACLF. In fact, due to the serious complications associated with hyperammonemia, mainly regarding HE and cerebral edema[8], prompt initiation of RRT is indicated even in the absence of renal failure, when this serious metabolic derangement is present at these patients[8,9]. Although no specific cut-off for the initiation of RRT exists based solely on this indication, the majority of the studies suggest it’s initiation when the value of ammonia is thrice greater than the upper limit of normal, or greater than 200 µmoles/L or when the patient shows severe encephalopathy[9].
Nowadays, continuous RRT (CRRT) is preferred over intermittent hemofiltration or peritoneal dialysis in ALF and ACLF due to its well-documented advantages in critically ill patients, mostly related to hemodynamic stability[10,11]. In addition, it can be used in complicated cases of refractory to medical treatment hepatorenal syndrome (HRS)[12]. It presents a more favorable and safe profile regarding changes in osmolality and their effect on intracranial pressure/brain edema, contributing to the maintenance of cerebral homeostasis[10]. CRRT aids in maintaining a circulatory, acid-base, and electrolyte balance during the pro-, peri-, and post-LT periods[10,13]. It exerts beneficial effects on other complications of liver failure, such as HE[14]. Moreover, it facilitates the control of fluid balance, avoidance of volume overload, and deterioration of peripheral edemas-ascites due to third-space fluid loss[12,15]. In several cases, especially in pediatric patients, it is combined with PE therapy and has produced good results[16,17].
It can remove water-soluble, small- and medium-sized molecules (mostly urea, creatinine, phosphorus, and ammonia). Furthermore, it extracts cytokines non-selectively and, in the majority of cases, to a lower degree compared to hemoperfusion[18,19]. However, it is unable to remove albumin-bound molecules.
It is inexpensive and widely available almost in every intensive care unit (ICU) or high-dependency unit (HDU), whereas its side effects are few and primarily catheter-related.
Although the effect of CRRT therapy on survival has been randomly studied, there exist a few reports on its beneficial short-term effects[14,20] thus improving the possibility for LT.
High-volume hemofiltration
High-volume hemofiltration (HVHF) therapy is characterized by high effluent rates and is performed either continuously or intermittently. Although its limits differ significantly among studies, relative rates can be as high as 50 mL/kg/h to 70 mL/kg/h (continuous treatment) and 100 mL/kg/h to 120 mL/kg/h (intermittent treatment)[21,22]. It represents an interesting alternative to conventional RRT because it can more effectively remove medium-sized and water-soluble molecules and cytokines with a wide range of molecular weights, from 5 kDa to 60 kDa using convection for removing solutes. Increased ultrafiltration rates also enhance the elimination of ammonia[23,24], which is of utmost importance for patients with ALF and ACLF. Furthermore, high ultrafiltration rates allow the filters to perform some degree of adsorption, targeting molecules with molecular weight above the threshold of the filter membrane and thereby expanding the range of cytokines and substance removal[25].
This last feature has an associated disadvantage, which is the undesirable loss of molecules and substances with functional or beneficial properties, including albumin[26,27], nutrients, and antibiotics[25]. However, the technique can be used to remove a small degree of albumin-bound metabolites, primarily uremic toxins[28].
The method has been used primarily for inborn urea cycle disorders[29], in combination with PE, for children[30,31] and for adults with liver failure and hyperammonemia[23,24]. Further research is warranted to explore the possibility of more widespread applications, as it is inexpensive and effective, can be performed in every ICU or HDU, and requires no special equipment. Only prescription dosing and familiarization with the modality are sufficient to allow the proper use of HVHF in patients with ALF and ACLF[30].
High cut-off membranes
High cut-off (HCO) membranes represent an evolution in RRT in clearing middle molecular weight substances and cytokines. Their median pore radius is approximately 0.01 µm, providing a cut-off of 60 KDa, which is close to that of normally functioning glomeruli[32]. This property enhances the removal of uremic toxins that are either protein-bound or of middle molecular weight but also results in loss of albumin when these membranes are used. Cytokine removal is also augmented with HCO membranes. Examples of cytokines removed by these membranes include interleukin (IL)-8, IL-6, and tumor necrosis factor-alpha (TNF-α)[33].
These membranes present interesting prospects for treating patients with ALF and ACLF due to the extent and quality of cytokines and toxin removal that they offer[34,35]; however, this hypothesis must be further tested and evaluated.
ADSORPION MODALITIES
Adsorption therapies are administered either by direct hemoperfusion or by plasma separation and subsequent plasma perfusion[19]. In addition, these therapies can be applied either as stand-alone or in combination with other extracorporeal modalities such as a CRRT circuit[36] or an extracorporeal membrane oxygenation (ECMO) device[37], which further improve their utility. They can successfully eliminate albumin-bound toxins and cytokines[19,37] with less complexity and more cost-effectiveness as compared to the Molecular adsorbent recirculating system (MARS) and the Fractionated plasma separation and Adsorption (FPSA)-Prometheus. These characteristics enhance their attractiveness for further research as promising options for patients with liver failure.
Hemadsorption
Direct hemoperfusion (Cytosorb): Small-scale studies have been conducted on Cytosorb hemoperfusion. It consists of a synthetic membrane with biocompatible polystyrene beads that have a large surface area and can remove molecules up to 55 kDa[38-40]. It was initially used for cytokine adsorption in sepsis and other hyperinflammatory conditions such as burns, pancreatitis, and hemophagocytic lymphohistiocytosis, where it is known to produce a beneficial effect by alleviating the excessive inflammatory response. IL-6 has been identified as a potential target of Cytosorb treatment[19,39,40].
Acute liver dysfunction presents with similar immunologic disorders, which forms the basis for the introduction of hemoadsorption in liver diseases. In cases of liver failure, drug-induced cholestasis, and acute alcoholic hepatitis, Cytosorb has been reported to be effective in reducing the levels of plasma bilirubin, ammonia, bile acids, and C-reactive protein (CRP) by altering the immune response in patients with high levels of proinflammatory cytokines[3,19,39,40].
Cytosorb is often paired with other extracorporeal therapies, such as continuous venovenous hemofiltration or ECMO, particularly in the ICU setting[39]. The literature reports several case series on patients with coronavirus disease-19 on ECMO, where encouraging results were obtained following the use of Cytosorb. In contrast, other trials have not reported any benefits in terms of mortality, vasopressor requirement, and organ dysfunction[1,19].
The advantages of Cytosorb include its high safety profile and ease of use. Cytosorb is mostly effective at around 12 h of use, with a blood flow rate of 150 mL/min to 500 mL/min, with the effect continuing up to 24 h[19]. Its adverse effects include the removal of beneficial substances, such as anti-inflammatory cytokines or medications, and thrombocytopenia[3,41].
Although Cytosorb appears to be a promising therapeutic method and serves as a bridge to transplantation in patients with ALF or ACLF, the literature reports limited evidence; large prospective data or results of RCTs are still missing[39-41]. In addition, conflicting results have been reported in several existing trials. For instance, a study by Scharf et al[42] demonstrated that the reduction in IL-6 in seriously ill patients was insignificantly different in patients treated with and without Cytosorb. The indications and endpoints of Cytosorb treatment, the effect on mortality, and risk stratification in terms of which patients would benefit from its use remain to be elucidated in large controlled, and adequately powered studies[19,42].
Plasma-perfusion after plasma separation
Double plasma molecular absorption system (DPMAS)-(BS 330 + HA 330-II): Another artificial LSS is double plasma molecular absorption system (DPMAS), which uses a neutral macroporous resin (HA 330-II) and an anion-exchange resin (BS 330). Toxic plasma is separated and cleansed by perfusion over the two hemoperfusion columns and subsequently recirculated to the body[43]. This combination efficiently removes macromolecules, medium-sized molecules, and toxins bound to plasma proteins, bilirubin, bile acids, ammonia, phenol, mercaptan, and inflammatory molecules. Thus, it potentially improves prognosis in patients with liver failure. In addition, the system requires no plasma or fluid replacement during treatment. It has been reported that DPMAS can reduce the levels of total bilirubin to more than 40%[43-45].
The advantages of this method include reduced risk for anaphylactic reactions, which are common in PE therapy, as it is a well-tolerated treatment. A major disadvantage of DPMAS is its inability to supplement for albumin and coagulation factors, correlating with the non-selective adsorption of the columns. This results in a significant loss of these molecules, coagulation disorders, and bleeding complications. To overcome these issues, DPMAS has been used in combination with PE; studies have reported that combined techniques substantially improved survival rates[43,44]. Because DPMAS is a new achievement, there are limited data on the effectiveness of DPMAS, derived from studies with small sample size. Larger, prospective trials are required to assess the exact efficacy, risk benefits, and outcomes[43,45,46].
COMPINATION MODALITIES
MARS
Another artificial liver replacement system for albumin dialysis is MARS. It can remove albumin-bound molecules and decrease the plasma concentrations of bilirubin, ammonia, creatinine, urea, and cytokines in patients with liver failure[47-49].
The system comprises a blood compartment, an albumin compartment, and a “renal” compartment. Its circuit allows the passage of molecules < 50 kDa and the extraction of albumin-bound toxins. Blood is passed through an albumin-high-flux dialysis membrane with adsorbent columns, and the albumin-bound molecules are released[47,49] and are then removed through the diffusion process[5]. The requirement for continuous albumin infusion is mitigated by the recirculation of albumin dialysate[47,49]. Afterward, traditional dialysis is performed to remove the toxins from the dialysate.
Moreover, MARS can modify the inflammatory response related to liver failure and its consequences, such as the development of systemic inflammatory response syndrome and MOF. It can efficiently remove certain proinflammatory cytokines, such as TNF-α, IL-6, and IL-1β, as well as certain anti-inflammatory cytokines, such as IL-10. In addition, treatment with MARS is associated with hemodynamic and clinical improvement in cases of portal hypertension, HE, refractory pruritus, Wilson’s disease, and drug-induced liver injury[47-49].
The majority of patients with liver failure develop bleeding disorders and have impaired hemostasis, leading to hemorrhagic complications. Therefore, anticoagulation regimens in MARS are highly significant. The most widely used anticoagulant is unfractionated heparin. In addition, no anticoagulation vs regional anticoagulation with citrate has been studied. Another significant aspect of MARS is that it eliminates certain antibiotics, particularly the low protein-bound antibiotics, such as quinolones and meropenem. Such cases require careful dose adjustments and therapeutic drug monitoring[47,49].
Limited data exist on the clinical outcomes of MARS in retrospective, uncontrolled trials with conflicting results. The benefits mostly include the treatment of HE and improved hemodynamics[47,49]. In addition, it has been reported to be beneficial in ALF in severely ill patients[49]. Although direct cost from its use is high, and it is performed exclusively in special reference centers, when combined with standard medical therapy it was found even more cost-effective than standard medical therapy alone, highlighting the need for more precise and holistic estimation of total cost and benefit drawn by these therapies[50]. Further RCTs are required to elucidate the potential effects on mortality and any added benefits of MARS on disease outcomes and define the clinical and laboratory profiles of patients who would benefit from such intervention. Currently, MARS remains another appealing option for bridging to transplantation in patients with liver failure.
FPSA-Prometheus
Prometheus is a kind of LSS introduced at the end of the 20th century[51]. Its functioning is based on an integration of plasma separation, albumin dialysis, adsorption, and high-flux hemodialysis. The system consists of a 250-kDa albumin-permeable filter, a neutral resin adsorber, an anion-exchange column, and a high-flux hemofilter. Patient’s albumin passes through the 250-kDa filter, thus leading to reduction of the plasma concentration of albumin. The blood subsequently is detoxified as it passes through the adsorber, the column, and the hemofilter, following which the purified blood is returned to the patient.
This combination allows the elimination of both water-soluble and albumin-bound toxins and drugs. Prometheus significantly reduces the levels of bilirubin, with studies reporting a better performance than MARS in removing highly albumin-bound substances such as unconjugated bilirubin[52-55]. Although a recent, well-designed meta-analysis reported lack of efficient clearance of ammonia and creatinine by the Prometheus system[2], other studies support reverse findings[52,53,55,56]. Moreover, Prometheus effectively eliminates bile acids[52,55], even better than MARS[53,54]. Urea[2,56] and amino acids[57], implicated in the pathogenesis of HE, have been found to be adequately removed. This has been shown to result in significant improvement in HE[57] in these patients, and several case reports have found the same[58].
The results regarding the clearance of cytokines have been conflicting, with certain studies reporting reduced levels of cytokines[59], whereas others do not[2,60].
Other indications, including refractory pruritus and HRS, have been studied with encouraging results for Prometheus[61,62].
Prometheus has a good safety profile and good hemodynamic tolerance, although no improvement in the hemodynamic parameters was observed as compared to MARS[54]. Moreover, it has been used to treat severely ill patients. No major adverse effects have been recorded after decades of use, apart from a few reports regarding catheter-related, primarily septic complications[63], technical issues such as clotting of the circuit[64], and others such as thrombocytopenia[65].
The impact of Prometheus on OS and TFS is unclear because of lack of available data, whereas results regarding the survival rate of patients with HRS as a whole are conflicting[12,66]. However, these therapies can simultaneously improve patient’s compromised renal and liver function by removing cytokines implicated in the worsening of renal function and HRS[12,62].
Although several research groups have been unable to demonstrate the OS benefits of using Prometheus[2,67], subgroup analyses have revealed a favorable effect on patients with more severe liver disease [Model for End-Stage Liver Disease (MELD) score > 30] and in patients with type 1 HRS[67]. Novel, well-designed, preferably RCTs are required to reach reliable conclusions regarding the use of these systems.
Single-pass albumin dialysis system
Single-pass albumin dialysis (SPAD) is an alternative to MARS and Prometheus modality of LRT for albumin dialysis. It is an inexpensive, widely available, simple technique that requires only a simple CRRT machine and exogenous albumin. Although an HCO filter has been reported to be used[68]; in most cases, a high-flux hemofilter is used as a dialyzer. The albumin-containing dialysate flows opposite to the blood in the filter, extracting the hydrophobic substances from the saturated albumin of the blood to the dialysate, which is subsequently disposed. Although this technique efficiently eliminates albumin-bound toxins, it causes a significant loss of albumin, which is a major disadvantage of the method.
Another important issue that needs attention is that dialysate’s ideal albumin concentration and flow rate are not standardized. Different values have been proposed by various studies, whereas commercial albumin-containing CRRT fluids are not provided by companies and should be prepared before use, thereby increasing the workload on nurses. Recent suggestions to improve these issues include using a 3% albumin solution at the dialysate, 700 mL/h to 1000 mL/h dialysate flow rate, and constructing instructions for easy preparation of bags containing 3% albumin[24].
SPAD can effectively remove bilirubin, bile acids, and other albumin-bound toxins, and the hemofilter simultaneously removes small-sized, water-soluble toxins.
Metabolic disarrangements (elevated lactate/low calcium levels) and loss of antibiotics have been reported. Therefore, close monitoring of patients is highly essential for early detection and treatment[24,69].
The SPAD method has been reported to effectively remove bilirubin[69-71], bile acids (although less effectively than MARS)[69], urea, and creatinine (although less effectively than MARS)[69-71]. It has been used in ALF patients with Wilson’s disease[72], for elevated bilirubin levels following acute hepatitis A[73], liver failure, and HE in pediatric patients[74], and HRS[75]. Because the majority of these studies are either case reports or case series, more research, preferably RCTs, is warranted to describe the effect of SPAD on OS and TFS and other liver-related outcomes.
Coupled plasma filtration adsorption
Coupled plasma filtration adsorption (CPFA) was developed during the 1990s. It uses a combination of adsorption (resin cartridge) and convection (CRRT) in the same circuit. Thus, it is different from other adsorption therapies (Cytosorb and DPMAS), where CRRT is an alternative option and not a prerequisite. Another characteristic of the method is plasma separation, performed by a plasma filter. It is the first step of the procedure before adsorption. Plasma is subsequently cleared from albumin-bound substances and mediators through the cartridge. Finally, the passage through a hemofilter removes water-soluble substances. Thus, the method has several advantages. Slow plasma passage from the resin allows better interaction and adsorption of substances, whereas the absence of blood cells, especially platelets, prevents clotting during the passage of the separated plasma through the cartridge[76]. Moreover, it incurs minimal or no loss of significant molecules such as albumin and coagulation factors and does not require the replacement of the patient’s plasma. Compared to other methods of removal of albumin-bound toxins (MARS, Prometheus, Cytosorb, PE), CPFA is less expensive. However, CPFA cannot be performed in patients with septic shock due to associated potential harm[19,77].
The available literature reports that CPFA can effectively remove bilirubin, tryptophan, phenols[78,79], bile acids[79], and cytokines[80]. It has been used for liver indications such as ALF and ACLF[81,82], after LT[83], in hypoxic hepatitis[84], and combined with PE therapy for ALF due to Wilson’s disease[85]. Future studies are required to elucidate its role as an LRT.
OTHER MODALITIES
Plasma exchange
Plasma exchange (PE) is the LRT with the highest proven beneficial effects on patient outcomes. Recent meta-analyses[2], guidelines and RCTs[11,86] have reported beneficial outcomes for 3-mo OS and TFS, respectively, especially for patients with early initiation of the treatment and not undergoing LT and same results come from well-designed reviews, regarding 1- and 3-mo survival in nontransplanted patients[87]. The effect is more pronounced when high-volume PE (the replacement of thrice the patient’s estimated plasma volume) is performed[86-88], whereas standard-volume PE has demonstrated good results in certain sub-groups of patients with liver failure[89,90].
The circuit consists of a plasma filter, with pore sizes approximately 0.2 µm (far larger than those of hemofilter[32], thus allowing the extraction of larger molecular weight proteins, including antibodies, immune complexes, paraproteins, and lipoproteins[91,92]). In addition, it consists of a replacement solution containing plasma and/or albumin. The process separates plasma substances from whole blood and replacement with plasma and/or albumin follows, thereby exchanging the patient’s plasma with that of healthy donors. The method allows the removal of cytokines, albumin-bound and water-soluble toxins, and the replacement of plasma proteins, including clotting factors that are severely diminished in patients with liver failure[93]. However, it cannot effectively eliminate small and medium molecular weight water-soluble molecules. Simultaneous CRRT could be necessary for patients with concomitant renal failure[31,94]. The immunomodulatory effects of PE therapy have been outstanding, as evident from its benefits reported for other indications such as chronic inflammatory demyelinating polyneuropathy, myasthenia gravis, multiple myeloma, Guillain-Barre syndrome, and thrombotic thrombocytopenic purpura. These advantages make PE treatment of choice for suppressing the inflammatory cascade of liver failure, whereas substitution of clotting factors offers the advantage of correcting coagulation disorders often observed in these patients. In addition, it has been shown that PE reduces vasopressor requirements and ammonia levels and improves HE. It exerts no effect on intracranial pressure elevation[93]. However, it is an expensive method, primarily due to the use of significant quantities of fresh frozen plasma (the circuit for PE does not have a significant cost). Furthermore, it could induce the side effects associated with the use of blood products, such as allergic reactions, transfusion-related acute lung injury, the transmission of infectious diseases and hypocalcemia. Apart from CRRT, it is frequently combined with other modalities, such as DPMAS[43-45].
NEW SYSTEMS AND METHODS UNDER RESEARCH
Carbalive and Dialive
Bacterial translocation remains one of the major causes for disease-related morbidity and mortality in patients with ACLF. An established method of prevention is the use of oral antibiotics, which are poorly absorbed by the gastrointestinal tract, however this approach comes with increased resistance and cost. CARBALIVE is a novel, non-antibiotic related intervention, which is under investigation. It consists of a microporous carbon absorbent, which is orally administered and removes bacterial endotoxins from the bowel, thus preventing the harmful consequences of inflammation, which usually accompanies bacterial translocation. Recent trials revealed positive preliminary results in patients with decompensated cirrhosis, while CARBALIVE seems to be safe and well tolerated. Another novel option for endotoxin removal and bridging to transplant in patients with ACLF is DIALIVE. It represents a dual filtration system. One filter removes toxin products from bloodstream and the other one removes and replaces albumin. Preliminary results are promising in terms of safety and tolerability. Data for both of these two modalities still need to be validated in larger randomized clinical trials[95].
DISCUSSION
Pathophysiologically, liver failure is regulated by immune-mediated reactions, mainly consisting of overproduction of proinflammatory cytokines, that results in a cascade of excessive inflammatory response[2]. As most of LRT systems were found to perform cytokine clearance, their application has been studied as to how it affects the dysregulation of the immune system by reducing cytokine levels and alleviating the catastrophic consequences of immune system over-activation. There are two main issues that must be further elucidated: (1) Studies regarding the effectiveness of the LRT systems to reduce cytokine levels have given conflicting results[42,60]. This can be attributed to the heterogeneity of the amount and type of pro- and anti-inflammatory cytokines produced in patients with liver failure. In several cases, the overproduction of cytokines has been reported to overcome the elimination capacity of the LSS[60]; and (2) LRT systems eliminate both pro- and anti-inflammatory cytokines[42], resulting in non-predictable and simultaneous suppression and activation of the immune system respectively. The clinical impact of the effect of LRT systems on the imbalance between pro- and anti-inflammatory mediators in liver failure remains unclear, and further studies are warranted in this field.
Table 1 lists the different characteristics of all modalities discussed in this review, including costs, complexity, applicability, and methods of toxin clearance. The attempted comparison of costs and complexity of these modalities is preliminary and arbitrary and could differ between different centers and countries. Their extent of applicability is based on whether these methods can be performed in any ICU or HDU (broad), or in ICUs and HDUs with particular experience, knowledge, and equipment (medium), or, finally, in special reference centers for LRT (limited).
Table 1.
Comparison of basic characteristics of artificial liver support systems
|
System
|
Detoxification methods
|
Cost
|
Complexity
|
Applicability
|
Detoxification capacity/range
|
Impaction OS/TFS
|
Main characteristics
|
| Continuous renal replacement therapy | Diffusion, convection | Low | Low | Broad (all ICUs, HDUs) | Restricted (water-soluble, low and medium molecular weight substances, mainly ammonia, cytokines) | Few data, no RCTs | Simple, no removal of albumin-bound toxins |
| High-volume hemofiltration | Convection | Low | Low | Broad (all ICUs, HDUs) | Restricted (water-soluble, low and medium molecular weight substances, mainly ammonia, cytokines), but more effectively than CRRT | Few data, no RCTs | Simple, better removal of low and medium sized molecules and cytokines than low-volume. No significant removal of albumin-bound toxins, loss of albumin, nutrients |
| High cut-off membranes | Diffusion, convection | Low | Low | Broad (all ICUs, HDUs) | Middle molecules up to 60 kDa, protein-bound uremic toxins, cytokines (IL-8, IL-6, and TNF-α) | Few data, no RCTs | Simple, removal of protein-bound-medium sized uremic toxins cytokines. No removal of other albumin bound toxins, loss of albumin |
| Direct hemoperfusion (Cytosorb) | Adsorption | Medium to high | Medium | Medium (ICUs, HDUs with experience) | Molecules up to 55 kDa, bilirubin, ammonia, bile acids, IL-6, CRP | Few data, no RCTs | Simple, removal of albumin bound toxins, bilirubin, bile acids, cytokines. Needs more literature |
| Double plasma molecular absorption system | Plasma separation, adsorption | Medium | Medium | Medium (ICUs, HDUs with experience) | Macromolecules, medium-sized plasma protein bound molecules and toxins, bilirubin, inflammatory molecules | Few data, no RCTs | Simple, removal of albumin bound toxins, bilirubin, bile acids, cytokines; needs more literature |
| Molecular adsorbent recirculating system | Albumin dialysis-diffusion, adsorption, convection | High | High | Limited (special centers) | Albumin-bound molecules < 50 kDa, water-soluble substances, Cytokines (TNF-α, IL-6, IL-1β, and IL-10) | Not found/not found | With available literature, removal of albumin-bound toxins; complex, expensive, limited access, uses exogenous albumin |
| Fractionated plasma separation and Adsorption-PROMETHE-US | Plasma separation, albumin dialysis-diffusion, adsorption, convection | High | High | Limited (special centres) | Broad (albumin-bound toxins, water-soluble substances of a wide range of molecular weight, cytokines) | Not found/not found | With available literature, removal of albumin-bound toxin; complex, expensive, limited access |
| Single-pass albumin dialysis | Albumin dialysis-diffusion, convection | Medium | Low | Broad (all ICUs, HDUs) | Albumin-bound substances (bilirubin, bile acids), small-sized (< 500 Da) water-soluble toxins | Few data, no RCTs | Simple, removal of albumin-bound substances, water soluble toxins; high cost of exogenous albumin, metabolic disarrangements |
| Coupled plasma filtration adsorption | Plasma separation, adsorption, convection | Medium | Medium | Medium (ICUs, HDUs with experience) | Albumin-bound molecules and toxins (bilirubin, tryptophan, phenols, bile acids), cytokines, water soluble toxins | Few data, no RCTs | Simple, removal of albumin-bound toxins, bilirubin, bile acids, cytokines; needs more literature |
| Plasma exchange | Separation of plasma substances, replacement with FFP | Medium to high, mainly due to the FFP | Medium | Medium (ICUs, HDUs with experience) | Broad (removal of cytokines, albumin-bound and water-soluble toxins, antibodies, immune complexes, lipoproteins) | Beneficial (RCTs and guidelines) | Effective with available literature from RCTs, replaces plasma proteins, clotting factors; expensive, need, cost and complications of blood products |
OS: Overall survival; TFS: Transplant-free survival; ICUs: Intensive care units; HDUs: High dependency units; RCTs: Randomized controlled trials; FFP: Fresh frozen plasma; TNF-α: Tumor necrosis factor-alpha; IL: Interleukin; kDa: Kilodalton; CRP: C-reactive protein.
Costs included in Table 1 mainly regard direct costs from the use of each method, not including the expenses that emerge from the rest of the support that these patients require. However, indirect costs from ICU/HDU hospitalization that represent a significant burden worldwide[96], including albumin supplementation, antibiotic administration for hospital-acquired infections (a very frequent complication for these patients) and maintenance of the above-mentioned expensive health-care facilities, are not included. On the other hand, keeping these patients alive until LT is available while reducing their morbidity and mortality is another parameter that must be taken into consideration. Of note, there are studies that find these therapies cost-effectively superior to standard medical therapy alone[50]. Thus, the exact balance between cost and effectiveness of application of these methods remains to be elucidated.
A key point to this approach is to detect patients that may benefit at a significant degree from LRT and apply these methods accordingly. Use of appropriate biomarkers, in the context of compatible clinical picture, could serve as a tool for distinguishing those patients and identify the most appropriate method for them, offering a personalized approach to the treatment of ALF and ACLF. Such biomarkers are under intense study in sepsis and COVID-19. The measurement of endotoxin levels with an endotoxin activity assay for initiation of polymyxin B hemoperfusion and measurements of CRP, IL-6 or ferritin for initiation of Cytosorb therapy are relative examples[97,98]. However, such biomarkers have not been identified for ALF and ACLF yet, and their identification presents a challenging target for future research. Alternatively, certain sub-groups of patients, such as those that are more severely ill[49], those with more severe liver disease (MELD score > 30) or with type 1 HRS[67], and those with early initiation of treatment, that will not undergo LT[11] have been found to receive more favorable effect from LRT, and treating these sub-groups preferably is a reasonable approach for achieving cost-effective use of the LRT systems. Nevertheless, proper validation of indications and application of suitable tools for identifying these patients represent fields for thorough future research.
Table 2 summarizes in tabular form data from a selection of the studies that were included in this review, with the main key points that were drawn by each study, while Table 3 (adapted with modifications from a recent study regarding expert consensus recommendations for the majority of currently available LSSs[99]) highlights advantages, disadvantages, side effects, complications and contraindications of LSSs.
Table 2.
Selected data from available guidelines, systematic reviews, meta-analyses or clinical studies included in this review
|
Ref.
|
Type of study
|
Modality-ies studied
|
Summary of key points of each study
|
| [2] | Systematic review/meta-analysis | LRT systems | Liver failure pathophysiology involves immune system over-activation and overproduction of proinflammatory cytokines, resulting in multiple-organ failure; reducing cytokine levels and thus correcting the dysregulation of the immune system is the pathophysiologic base of the application of LRT systems |
| Plasma exchange | The best currently available LRT system in ACLF regarding 3-mo OS | ||
| [9] | Review | Continuous renal replacement therapy | It has indication for initiation of when ammonia is more than × 3 the uln, or more than 200 µmoles/L or when severe encephalopathy occurs |
| [10] | Review | Continuous renal replacement therapy | It has a role in the maintenance of circulatory, acid-base, and electrolyte balance during the pro-, peri-, and post-LT periods. It facilitates control of fluid balance and avoidance of volume overload/of peripheral edemas-ascites in patients with ALF and ACLF |
| [11] | Guidelines | Plasma exchange | It improves transplant-free survival in ALF, and modulates immune dysregulation; patients with early treatment initiation that will not undergo LT may benefit most |
| [19] | Review | Adsorption therapies | They are delivered either by direct hemoperfusion or by plasma separation and subsequent plasma perfusion |
| Direct hemoperfusion (Cytosorb) | It reduces levels of plasma bilirubin, ammonia, bile acids, and C-reactive protein and alters the immune response by absorbing proinflammatory cytokines; IL-6 has been identified as one of its main therapeutic targets; it presents high safety profile and easy application; indications, endpoints, effect on mortality and detection of which patients receive benefit from its use remain to be elucidated | ||
| [24] | Review | Single-pass albumin dialysis | Dialysate’s ideal albumin concentration and flow rate are not standardized while there are no commercially available albumin-containing Continuous renal replacement therapy fluids. Metabolic disarrangements and loss of antibiotics have been observed |
| [30] | Clinical study | High-volume hemofiltration | An inexpensive and effective method that can be performed in every ICU or HDU, requiring no special equipment. Increased ultrafiltration rates enhance the elimination of ammonia |
| [35] | Clinical study | High Cut-off membranes | Cytokine and toxin removal by these membranes may represent a promising intervention in ALF and ACLF |
| [36] | Review | Adsorption therapies | They are delivered either as stand-alone or in combination with other extracorporeal modalities; the evidence to support their routine use is still conflicting and insufficient. May be of utmost benefit when applied early in the course, for an adequate duration, and frequently repeated until hemodynamic stability is achieved; they require carefully monitoring of drug levels, supplemented with additional doses as needed |
| [38] | Review | Adsorption therapies | They have been used with positive effects in chronic dialysis and chronic liver disease |
| Direct hemoperfusion (Cytosorb) | Ιt removes molecules up to 55 kDa | ||
| [43] | Systematic review/meta-analysis | Double plasma molecular absorption system | It combines two resins that remove macromolecules, medium-sized molecules, and toxins bound to plasma proteins, bilirubin, bile acids, ammonia, phenol, mercaptan, and inflammatory molecules |
| [44] | Clinical study | Double plasma molecular absorption system | It is frequently combined with Plasma exchange therapy, to overcome loss of for albumin and coagulation factors, with promising results on survival rates |
| [48] | Randomized controlled study | Molecular adsorbent recirculating system | It removes albumin-bound molecules and decreases the plasma concentrations of bilirubin, ammonia, creatinine, urea, and cytokines. It has good safety profile |
| [49] | Review | Molecular adsorbent recirculating system | Recirculation of albumin dialysate restricts albumin loss; under certain circumstances and indications, it has been associated with hemodynamic and clinical improvement at patients with liver disease; dose adjustments and therapeutic drug monitoring, especially for low protein-bound antibiotics, is required |
| [50] | Clinical study | Molecular adsorbent recirculating system | Expensive method, application in selected centers, but when compared to standard medical therapy alone it was found more cost-effective |
| [52,57] | Review, Clinical study | PROMETHEUS | It performs albumin dialysis. It removes bilirubin, ammonia, creatinine, bile acids, amino acids, cytokines and is associated with a small reduction in plasma concentration of albumin; it was associated with improvement in HE |
| [54] | Randomized controlled study | PROMETHEUS | It presents good safety profile and good hemodynamic tolerance |
| [67] | Randomized controlled study | PROMETHEUS | Favorable effect on patients’ subgroups such as those with more severe liver disease (MELD score > 30) and with type 1 HRS |
| [69] | Randomized controlled study | Single-pass albumin dialysis | It is inexpensive, apart from the cost of albumin, and requires no special center for its application; it performs albumin dialysis and removes bilirubin, bile acids, urea and creatinine |
| [76] | Review | Coupled plasma filtration adsorption | It combines plasma separation, adsorption and convection, with no loss of albumin or coagulation factors; it can effectively remove bilirubin, tryptophan, phenols, bile acids, cytokines |
| [77] | Randomized controlled study | Coupled plasma filtration adsorption | It cannot be performed in patients with septic shock |
| [87] | Review | Plasma exchange | It improves 1- and 3-mo survival in nontransplanted patients. More pronounced effect and high level of evidence for high volume plasma exchange |
| [93] | Review | Plasma exchange | It removes cytokines and albumin-bound toxins, and replaces plasma proteins; it effectively suppresses the inflammatory cascade of liver failure, while substituting clotting factors and correcting coagulation disorders; relatively expensive, it presents transfusion related side effects and cost |
LRT: Liver replacement therapy; OS: Overall survival; ALF: Acute liver failure; ACLF: Acute-on-chronic liver failure; uln: Upper limit of normal; LT: Liver transplantation; IL: interleukin; ICU: Intensive care unit; HDU: High Dependency Unit; kDa: Kilodalton; MELD: Model for end-stage liver disease; HRS: Hepatorenal syndrome; HE: Hepatic encephalopathy.
Table 3.
Advantages, disadvantages, side effects, complications and contraindications, with intended population to treat, for each liver support system (adapted with modifications from[99])
|
Method
|
Advantages
|
Disadvantages-side effects- complications-contraindications
|
Intended population
|
| Plasma exchange | Easy operation, broad-spectrum rapid, and efficient removal of various toxins, supplementation of fresh frozen plasma, shorter treatment time, acceptable patient tolerance | Higher treatment cost, poor clearance of water-soluble toxins, aggravation of hepatic encephalopathy, plasma allergy, risk of infection associated with blood products, water and sodium retention after treatment | Patients with hepatic failure, hyperbilirubinemia, cryoglobulinemia, Guillain-Barré syndrome, thrombotic thrombocytopenic purpura, myasthenia gravis |
| Continuous renal replacement therapy | Hemodynamic stability in critically ill patients, maintenance of cerebral homeostasis, inexpensive and widely available | Unable to remove albumin-bound molecules | Critically ill patients, patients with refractory hepatorenal syndrome |
| High-volume hemofiltration | More effective removal of medium-sized and water-soluble molecules and cytokines; enhances the elimination of ammonia | Undesirable loss of molecules and substances with functional or beneficial properties, including albumin, nutrients, and antibiotics | Patients with ALF and ACLF, inborn urea cycle disorders, in children and adults with liver failure and hyperammonemia |
| High cut-off membranes | Removal of uremic toxins | Loss of albumin | Patients with ALF and ACLF |
| Direct hemoperfusion (Cytosorb) | Reduces the levels of plasma bilirubin, ammonia, bile acids, and C-reactive protein, high safety profile and ease of use | Higher treatment cost Removal of beneficial substances, such as anti-inflammatory cytokines or medications, and thrombocytopenia | Patients with liver failure, drug-induced cholestasis, and acute alcoholic hepatitis; bridge to transplantation in patients with ALF or ACLF |
| Double plasma molecular absorption system | Rapid removal of bilirubin, inflammatory mediators without requiring exogenous plasma | Inability to replenish coagulation factors; hypotension is likely to occur during the initial treatment period | Patients with liver failure, hyperbilirubinemia, hepatic encephalopathy, perioperative treatment of liver transplantation |
| Molecular adsorbent recirculating system | Effective removal of protein-bound and water-soluble toxins, excellent biocompatibility, relatively safe | Markedly expensive and complex, cannot supplement coagulation factors | Patients with acute severe liver injury or liver failure |
| Fractionated plasma separation and Adsorption-PROMETHEUS | Elimination of both water-soluble and albumin-bound toxins and drugs, good safety profile and good hemodynamic tolerance | Markedly expensive and complex, lack of efficient clearance of ammonia and creatinine | Patients with hepatic encephalopathy, hepatorenal syndrome |
| Single-pass albumin dialysis | Inexpensive, widely available, simple technique, effectively removes bilirubin, bile acids, and other albumin-bound toxins | Significant loss of albumin, metabolic disarrangements and loss of antibiotics | Patients with ALF, Wilson’s disease, acute hepatitis A, liver failure, hepatic encephalopathy, hepatorenal syndrome |
| Coupled plasma filtration adsorption | Removes medium and small molecular weight water-soluble toxins and is capable of volume regulation and renal support | Higher equipment requirements, higher treatment cost | Patients with liver failure, renal insufficiency, hyperammonemia, rhabdomyolysis, burns, severe autoimmune diseases, poisoning |
LSS: Liver support system; ALF: Acute liver failure; ACLF: Acute-on-chronic liver failure.
It is worth noting that the impact from the application of LSSs on OS and TFS remains unclear because of the lack of data, especially from RCTs. The majority of the studies have limited sample sizes and present methodological issues, especially the risk of bias. Properly designed, double-blind, RCTs with efficient statistical analysis and adequate sample size to achieve statistical power must be performed by experienced researchers. In order to draw reliable conclusions, enrollment should be done on the basis of discrete inclusion criteria, comparing groups of equal severity and comparable comorbidities, with separate study of patients with ALF and those with ACLF, as these entities have differences in pathophysiology, clinical presentation and prognosis.
Choice of study outcomes is also challenging. The most commonly used include OS, TFS, all-cause mortality, liver-related mortality, improvement of HE, HRS or other complications of liver failure[2,100]. Nevertheless, the majority of patients with ALF and ACLF are severely ill and present MOF, with high rates of mortality, making it difficult to prove the beneficial effects of any of these interventions. In order to overcome this obstacle, other endpoints, such as short-term survival as bridging to LT, have been proposed[66], however LT is not offered as an immediate or future option to most of these patients. Thus, proper identification of other suitable endpoints is demanded. Simple to use and interesting endpoints to consider could be the reduction of ACLF-grades, the reduction of MELD score and estimators of patients’ quality of life; the latter is increasingly being used in other circumstances, such as at patients after LT and could present an interesting alternative for assessing the impact of LRT on patients’ health status.
At this point of time artificial LRT systems mostly serve as bridging therapies towards LT. Factors including cost, lack of available evidence and complexity restrict their applicability. However, the introduction of new systems like DIALIVE, CARBALIVE, and new methods like adsorption therapies (their cost is lower compared to previous systems and gets lower over time, they are simple in use and can be widely available, they have a wide range of clearance of molecules and toxins) and the evolution of technology along with the evidence acquired regarding already available systems and techniques (MARS, prometheus, and PE therapy) give the perspective for more widespread use of LRT. The goal for LRT should be its application at every patient with ALF or ACLF that will benefit from it, regardless of the presence or absence of exclusion criteria for LT, and regardless of any anticipated delay for LT. Ideally, the experience from RRT should be adapted, where technological progress and cost deterioration from widespread use have made RRT widely available, practically for every patient that needs it.
CONCLUSION
LRT is a constantly evolving and widely offered therapeutic approach for patients with ALF and ACLF. Different systems and methods described in this review can efficiently detoxify all toxins and molecules implicated in the pathophysiology of ALF and ACLF and responsible for the associated complications. Amongst the available LRT systems, certain modalities are neither expensive nor highly sophisticated and can be applied almost in every ICU or HDU supporting this category of extremely complicated patients. Although these systems have not yet gained a strong position among treatment guidelines regarding patients with liver failure, this is probably due to the poor quality of available evidence. Recent meta-analyses have reported promising results[100,101], indicating the need for further research and more RCTs. Another challenge for clinicians treating these patients is to decide the appropriate method, correct initiation time, and parameters of the prescribed therapy for these patients. In addition, the majority of them are critically ill, with coagulation disorders and liver complications (HE, HRS, ascites, hyperammonemia, and elevated intracranial pressure). Considering the restricted available literature on these systems, these decisions need to be made prudently and more research is warranted in this field. Nevertheless, standard medical therapy for liver failure has probably reached its peak; LT is lifesaving but not easily accessible and demands lifelong immunosuppression. Thus, LRT represents a highly promising alternative offering new potentials for treating ALF and ACLF in the future, improving the survival of these patients either toward recovery of liver function or as support for impaired liver function until LT becomes available. Options, including the use of combinations of different methods, application of multiple methods in a patient according to the phase of the disease and the toxins to be removed, and adoption by centers of LRT protocols have already been described[24,102]. Such options could probably be ideal for treating these highly complicated patients. We believe that as technology and knowledge evolve, the future of these systems will witness major advancements.
ACKNOWLEDGEMENTS
This paper is dedicated to the memory of Tilemachos Zafeiridis (1974-2021), an exceptional doctor. Two years after his premature death, we remember his exceptional character and honor his contribution to his patients and co-workers.
Footnotes
Conflict-of-interest statement: The authors declare having no conflicts of interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: February 27, 2023
First decision: April 10, 2023
Article in press: May 12, 2023
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ferrarese A, Italy; Manrai M, India S-Editor: Chen YL L-Editor: A P-Editor: Zhao S
Contributor Information
Panagiotis Papamichalis, Intensive Care Unit, General Hospital of Larissa, Larissa 41221, Thessaly, Greece. ppapamih@med.uth.gr.
Katerina G Oikonomou, Intensive Care Unit, General Hospital of Larissa, Larissa 41221, Thessaly, Greece.
Asimina Valsamaki, Intensive Care Unit, General Hospital of Larissa, Larissa 41221, Thessaly, Greece.
Maria Xanthoudaki, Intensive Care Unit, General Hospital of Larissa, Larissa 41221, Thessaly, Greece.
Periklis Katsiafylloudis, Intensive Care Unit, General Hospital of Larissa, Larissa 41221, Thessaly, Greece.
Evangelia Papapostolou, Intensive Care Unit, General Hospital of Larissa, Larissa 41221, Thessaly, Greece.
Apostolia-Lemonia Skoura, Department of Transfusion Medicine, University Hospital of Larissa, Larissa 41110, Thessaly, Greece.
Michail Papamichalis, Department of Cardiology, University Hospital of Larissa, Larissa 41110, Thessaly, Greece.
Marios Karvouniaris, Intensive Care Unit, AHEPA University Hospital, Thessaloniki 54636, Greece.
Antonios Koutras, 1st Department of Obstetrics and Gynecology, General Hospital of Athens “ALEXANDRA”, National and Kapodistrian University of Athens, Athens 11528, Greece.
Eleni Vaitsi, Intensive Care Unit, General Hospital of Larissa, Larissa 41221, Thessaly, Greece.
Smaragdi Sarchosi, Department of Anesthesiology, University Hospital of Larissa, Larissa 41110, Thessaly, Greece.
Antonios Papadogoulas, Intensive Care Unit, General Hospital of Larissa, Larissa 41221, Thessaly, Greece.
Dimitrios Papadopoulos, Intensive Care Unit, General Hospital of Larissa, Larissa 41221, Thessaly, Greece.
References
- 1.Valsamaki A, Xanthoudaki M, Oikonomou KG, Vlachostergios PJ, Papadogoulas A, Katsiafylloudis P, Voulgaridi I, Skoura AL, Komnos A, Papamichalis P. Prevention, diagnostic evaluation, management and prognostic implications of liver disease in critically ill patients with COVID-19. World J Clin Cases. 2023;11:514–527. doi: 10.12998/wjcc.v11.i3.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ocskay K, Kanjo A, Gede N, Szakács Z, Pár G, Erőss B, Stange J, Mitzner S, Hegyi P, Molnár Z. Uncertainty in the impact of liver support systems in acute-on-chronic liver failure: a systematic review and network meta-analysis. Ann Intensive Care. 2021;11:10. doi: 10.1186/s13613-020-00795-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tomescu D, Popescu M, David C, Sima R, Dima S. Haemoadsorption by CytoSorb® in patients with acute liver failure: A case series. Int J Artif Organs. 2021;44:560–564. doi: 10.1177/0391398820981383. [DOI] [PubMed] [Google Scholar]
- 4.Scharf C, Liebchen U, Paal M, Becker-Pennrich A, Irlbeck M, Zoller M, Schroeder I. Successful elimination of bilirubin in critically ill patients with acute liver dysfunction using a cytokine adsorber and albumin dialysis: a pilot study. Sci Rep. 2021;11:10190. doi: 10.1038/s41598-021-89712-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matar AJ, Subramanian R. Extracorporeal Liver Support: A Bridge to Somewhere. Clin Liver Dis (Hoboken) 2021;18:274–279. doi: 10.1002/cld.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.López-Velázquez JA, Chávez-Tapia NC, Ponciano-Rodríguez G, Sánchez-Valle V, Caldwell SH, Uribe M, Méndez-Sánchez N. Bilirubin alone as a biomarker for short-term mortality in acute-on-chronic liver failure: an important prognostic indicator. Ann Hepatol. 2013;13:98–104. [PubMed] [Google Scholar]
- 7.Tujios SR, Hynan LS, Vazquez MA, Larson AM, Seremba E, Sanders CM, Lee WM Acute Liver Failure Study Group. Risk factors and outcomes of acute kidney injury in patients with acute liver failure. Clin Gastroenterol Hepatol. 2015;13:352–359. doi: 10.1016/j.cgh.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Redant S, Beretta-Piccoli X, Mugisha A, Attou R, Kaefer K, De Bels D, Tolwani A, Honoré PM. Hyperammonemia, the Last Indication of High-Volume Hemodiafiltration in Adult and Children: A Structured Review. Blood Purif. 2019;48:330–335. doi: 10.1159/000501390. [DOI] [PubMed] [Google Scholar]
- 9.Gupta S, Fenves AZ, Hootkins R. The Role of RRT in Hyperammonemic Patients. Clin J Am Soc Nephrol. 2016;11:1872–1878. doi: 10.2215/CJN.01320216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davenport A. Is there a role for continuous renal replacement therapies in patients with liver and renal failure? Kidney Int Suppl. 1999:S62–S66. [PubMed] [Google Scholar]
- 11.European Association for the Study of the Liver; Clinical practice guidelines panel; Wendon, J; Panel members; Cordoba J, Dhawan A, Larsen FS, Manns M, Samuel D, Simpson KJ, Yaron I; EASL Governing Board representative; Bernardi M. EASL Clinical Practical Guidelines on the management of acute (fulminant) liver failure. J Hepatol. 2017;66:1047–1081. doi: 10.1016/j.jhep.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 12.Bera C, Wong F. Management of hepatorenal syndrome in liver cirrhosis: a recent update. Therap Adv Gastroenterol. 2022;15:17562848221102679. doi: 10.1177/17562848221102679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang HB, Xu Y, Zhou H, Zhu Y, Qin JP. Intraoperative Continuous Renal Replacement Therapy During Liver Transplantation: A Meta-Analysis. Liver Transpl. 2020;26:1010–1018. doi: 10.1002/lt.25773. [DOI] [PubMed] [Google Scholar]
- 14.Cardoso FS, Gottfried M, Tujios S, Olson JC, Karvellas CJ US Acute Liver Failure Study Group. Continuous renal replacement therapy is associated with reduced serum ammonia levels and mortality in acute liver failure. Hepatology. 2018;67:711–720. doi: 10.1002/hep.29488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hansard PC, Manning RA, Haseeb MA, Salwen MJ. Hepatorenal syndrome: resolution of ascites by continuous renal replacement therapy in an alcoholic coinfected with hepatitis B, C, and human immunodeficiency viruses. Ann Clin Lab Sci. 2006;36:96–100. [PubMed] [Google Scholar]
- 16.Sanchez AP, Ward DM, Cunard R. Therapeutic plasma exchange in the intensive care unit: Rationale, special considerations, and techniques for combined circuits. Ther Apher Dial. 2022;26 Suppl 1:41–52. doi: 10.1111/1744-9987.13814. [DOI] [PubMed] [Google Scholar]
- 17.Tufan Pekkucuksen N, Sigler KE, Akcan Arikan A, Srivaths P. Tandem plasmapheresis and continuous kidney replacement treatment in pediatric patients. Pediatr Nephrol. 2021;36:1273–1278. doi: 10.1007/s00467-020-04769-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buonanno P, Servillo G, Vargas M. Continuous renal replacement and removal of inflammatory mediators in sepsis: Still an open debate. Asian J Surg. 2021;44:1431. doi: 10.1016/j.asjsur.2021.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ricci Z, Romagnoli S, Reis T, Bellomo R, Ronco C. Hemoperfusion in the intensive care unit. Intensive Care Med. 2022;48:1397–1408. doi: 10.1007/s00134-022-06810-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong LP, Blackley MP, Andreoni KA, Chin H, Falk RJ, Klemmer PJ. Survival of liver transplant candidates with acute renal failure receiving renal replacement therapy. Kidney Int. 2005;68:362–370. doi: 10.1111/j.1523-1755.2005.00408.x. [DOI] [PubMed] [Google Scholar]
- 21.Clark E, Molnar AO, Joannes-Boyau O, Honoré PM, Sikora L, Bagshaw SM. High-volume hemofiltration for septic acute kidney injury: a systematic review and meta-analysis. Crit Care. 2014;18:R7. doi: 10.1186/cc13184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Honore PM, Joannes-Boyau O, Boer W, Collin V. High-volume hemofiltration in sepsis and SIRS: current concepts and future prospects. Blood Purif. 2009;28:1–11. doi: 10.1159/000210031. [DOI] [PubMed] [Google Scholar]
- 23.Slack AJ, Auzinger G, Willars C, Dew T, Musto R, Corsilli D, Sherwood R, Wendon JA, Bernal W. Ammonia clearance with haemofiltration in adults with liver disease. Liver Int. 2014;34:42–48. doi: 10.1111/liv.12221. [DOI] [PubMed] [Google Scholar]
- 24.Ronco C, Reis T. Continuous renal replacement therapy and extended indications. Semin Dial. 2021;34:550–560. doi: 10.1111/sdi.12963. [DOI] [PubMed] [Google Scholar]
- 25.Rimmelé T, Kellum JA. High-volume hemofiltration in the intensive care unit: a blood purification therapy. Anesthesiology. 2012;116:1377–1387. doi: 10.1097/ALN.0b013e318256f0c0. [DOI] [PubMed] [Google Scholar]
- 26.Canaud B. Recent advances in dialysis membranes. Curr Opin Nephrol Hypertens. 2021;30:613–622. doi: 10.1097/MNH.0000000000000744. [DOI] [PubMed] [Google Scholar]
- 27.Ahrenholz PG, Winkler RE, Michelsen A, Lang DA, Bowry SK. Dialysis membrane-dependent removal of middle molecules during hemodiafiltration: the beta2-microglobulin/albumin relationship. Clin Nephrol. 2004;62:21–28. doi: 10.5414/cnp62021. [DOI] [PubMed] [Google Scholar]
- 28.van Gelder MK, Abrahams AC, Joles JA, Kaysen GA, Gerritsen KGF. Albumin handling in different hemodialysis modalities. Nephrol Dial Transplant. 2018;33:906–913. doi: 10.1093/ndt/gfx191. [DOI] [PubMed] [Google Scholar]
- 29.Lai YC, Huang HP, Tsai IJ, Tsau YK. High-volume continuous venovenous hemofiltration as an effective therapy for acute management of inborn errors of metabolism in young children. Blood Purif. 2007;25:303–308. doi: 10.1159/000106102. [DOI] [PubMed] [Google Scholar]
- 30.Chevret L, Durand P, Lambert J, Essouri S, Balu L, Devictor D, Tissieres P. High-volume hemofiltration in children with acute liver failure*. Pediatr Crit Care Med. 2014;15:e300–e305. doi: 10.1097/PCC.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 31.Trepatchayakorn S, Chaijitraruch N, Chongsrisawat V, Chanakul A, Kongkiattikul L, Samransamruajkit R. Therapeutic Plasma Exchange with Continuous Renal Replacement Therapy for Pediatric Acute Liver Failure: A Case Series from Thailand. Indian J Crit Care Med. 2021;25:812–816. doi: 10.5005/jp-journals-10071-23896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gondouin B, Hutchison CA. High cut-off dialysis membranes: current uses and future potential. Adv Chronic Kidney Dis. 2011;18:180–187. doi: 10.1053/j.ackd.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 33.Naka T, Haase M, Bellomo R. 'Super high-flux' or 'high cut-off' hemofiltration and hemodialysis. Contrib Nephrol. 2010;166:181–189. doi: 10.1159/000314871. [DOI] [PubMed] [Google Scholar]
- 34.Dominik A, Stange J, Pfensig C, Borufka L, Weiss-Reining H, Eggert M. Reduction of elevated cytokine levels in acute/acute-on-chronic liver failure using super-large pore albumin dialysis treatment: an in vitro study. Ther Apher Dial. 2014;18:347–352. doi: 10.1111/1744-9987.12146. [DOI] [PubMed] [Google Scholar]
- 35.Weidhase L, Haussig E, Haussig S, Kaiser T, de Fallois J, Petros S. Middle molecule clearance with high cut-off dialyzer versus high-flux dialyzer using continuous veno-venous hemodialysis with regional citrate anticoagulation: A prospective randomized controlled trial. PLoS One. 2019;14:e0215823. doi: 10.1371/journal.pone.0215823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ankawi G, Xie Y, Yang B, Xie P, Ronco C. What Have We Learned about the Use of Cytosorb Adsorption Columns? Blood Purif. 2019;48:196–202. doi: 10.1159/000500013. [DOI] [PubMed] [Google Scholar]
- 37.Akil A, Ziegeler S, Reichelt J, Rehers S, Abdalla O, Semik M, Fischer S. Combined Use of CytoSorb and ECMO in Patients with Severe Pneumogenic Sepsis. Thorac Cardiovasc Surg. 2021;69:246–251. doi: 10.1055/s-0040-1708479. [DOI] [PubMed] [Google Scholar]
- 38.Ronco C, Bellomo R. Hemoperfusion: technical aspects and state of the art. Crit Care. 2022;26:135. doi: 10.1186/s13054-022-04009-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dhokia VD, Madhavan D, Austin A, Morris CG. Novel use of Cytosorb™ haemadsorption to provide biochemical control in liver impairment. J Intensive Care Soc. 2019;20:174–181. doi: 10.1177/1751143718772789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ocskay K, Tomescu D, Faltlhauser A, Jacob D, Friesecke S, Malbrain M, Kogelmann K, Bogdanski R, Bach F, Fritz H, Hartjes A, Kortgen A, Soukup J, Utzolino S, van Tellingen M, Träger K, Schumacher U, Brunkhorst FM, Molnar Z. Hemoadsorption in 'Liver Indication'-Analysis of 109 Patients' Data from the CytoSorb International Registry. J Clin Med. 2021;10 doi: 10.3390/jcm10215182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sekandarzad A, Weber E, Prager EP, Graf E, Bettinger D, Wengenmayer T, Supady A. Cytokine adsorption in patients with acute-on-chronic liver failure (CYTOHEP)-a single center, open-label, three-arm, randomized, controlled intervention trial. Trials. 2022;23:222. doi: 10.1186/s13063-022-06139-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scharf C, Schroeder I, Paal M, Winkels M, Irlbeck M, Zoller M, Liebchen U. Can the cytokine adsorber CytoSorb(®) help to mitigate cytokine storm and reduce mortality in critically ill patients? A propensity score matching analysis. Ann Intensive Care. 2021;11:115. doi: 10.1186/s13613-021-00905-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bai W, Yao C, Mao D, Wu J, Wang K, Wei H, Huang Z, Shi Q, Wang N. The Clinical Efficacy of Double Plasma Molecular Absorption System Combined with Plasma Exchange in the Treatment of Acute-on-Chronic Liver Failure: A Systematic Review and Meta-Analysis. J Healthc Eng. 2022;2022:3139929. doi: 10.1155/2022/3139929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yao J, Li S, Zhou L, Luo L, Yuan L, Duan Z, Xu J, Chen Y. Therapeutic effect of double plasma molecular adsorption system and sequential half-dose plasma exchange in patients with HBV-related acute-on-chronic liver failure. J Clin Apher. 2019;34:392–398. doi: 10.1002/jca.21690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guo X, Wu F, Guo W, Zhang J, Yang Y, Lu Y, Yin C, Fan H, Xu J, Liao M. Comparison of plasma exchange, double plasma molecular adsorption system, and their combination in treating acute-on-chronic liver failure. J Int Med Res. 2020;48:300060520932053. doi: 10.1177/0300060520932053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xu W, Li Y, Wang L, Gao H, Chen J, Yuan J, Ouyang Y, Gao Y, Li J, Li X, Peng L. Efficacy and safety of combination treatment of double plasma molecular adsorption system and low volume plasma exchange for patients with hepatitis B virus related acute-on-chronic liver failure: a multicentre randomised controlled clinical trial. BMJ Open. 2021;11:e047690. doi: 10.1136/bmjopen-2020-047690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kumar Mandal A, Garlapati P, Tiongson B, Gayam V. Liver Assist Devices for Liver Failure. 2021. [cited 15 Jan 2023]. Available from: [DOI]
- 48.Bañares R, Nevens F, Larsen FS, Jalan R, Albillos A, Dollinger M, Saliba F, Sauerbruch T, Klammt S, Ockenga J, Pares A, Wendon J, Brünnler T, Kramer L, Mathurin P, de la Mata M, Gasbarrini A, Müllhaupt B, Wilmer A, Laleman W, Eefsen M, Sen S, Zipprich A, Tenorio T, Pavesi M, Schmidt HH, Mitzner S, Williams R, Arroyo V RELIEF study group. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: the RELIEF trial. Hepatology. 2013;57:1153–1162. doi: 10.1002/hep.26185. [DOI] [PubMed] [Google Scholar]
- 49.García Martínez JJ, Bendjelid K. Artificial liver support systems: what is new over the last decade? Ann Intensive Care. 2018;8:109. doi: 10.1186/s13613-018-0453-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kantola T, Mäklin S, Koivusalo AM, Räsänen P, Rissanen A, Roine R, Sintonen H, Höckerstedt K, Isoniemi H. Cost-utility of molecular adsorbent recirculating system treatment in acute liver failure. World J Gastroenterol. 2010;16:2227–2234. doi: 10.3748/wjg.v16.i18.2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Falkenhagen D, Strobl W, Vogt G, Schrefl A, Linsberger I, Gerner FJ, Schoenhofen M. Fractionated plasma separation and adsorption system: a novel system for blood purification to remove albumin bound substances. Artif Organs. 1999;23:81–86. doi: 10.1046/j.1525-1594.1999.06292.x. [DOI] [PubMed] [Google Scholar]
- 52.Krisper P, Stadlbauer V, Stauber RE. Clearing of toxic substances: are there differences between the available liver support devices? Liver Int. 2011;31 Suppl 3:5–8. doi: 10.1111/j.1478-3231.2011.02588.x. [DOI] [PubMed] [Google Scholar]
- 53.Evenepoel P, Laleman W, Wilmer A, Claes K, Kuypers D, Bammens B, Nevens F, Vanrenterghem Y. Prometheus versus molecular adsorbents recirculating system: comparison of efficiency in two different liver detoxification devices. Artif Organs. 2006;30:276–284. doi: 10.1111/j.1525-1594.2006.00215.x. [DOI] [PubMed] [Google Scholar]
- 54.Laleman W, Wilmer A, Evenepoel P, Elst IV, Zeegers M, Zaman Z, Verslype C, Fevery J, Nevens F. Effect of the molecular adsorbent recirculating system and Prometheus devices on systemic haemodynamics and vasoactive agents in patients with acute-on-chronic alcoholic liver failure. Crit Care. 2006;10:R108. doi: 10.1186/cc4985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Santoro A, Faenza S, Mancini E, Ferramosca E, Grammatico F, Zucchelli A, Facchini MG, Pinna AD. Prometheus system: a technological support in liver failure. Transplant Proc. 2006;38:1078–1082. doi: 10.1016/j.transproceed.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 56.Grodzicki M, Kotulski M, Leonowicz D, Zieniewicz K, Krawczyk M. Results of treatment of acute liver failure patients with use of the prometheus FPSA system. Transplant Proc. 2009;41:3079–3081. doi: 10.1016/j.transproceed.2009.08.024. [DOI] [PubMed] [Google Scholar]
- 57.Rifai K, Das A, Rosenau J, Ernst T, Kretschmer U, Haller H, Fliser D, Manns MP. Changes in plasma amino acids during extracorporeal liver support by fractionated plasma separation and adsorption. Artif Organs. 2010;34:166–170. doi: 10.1111/j.1525-1594.2009.00763.x. [DOI] [PubMed] [Google Scholar]
- 58.Piechota M. Hepatic encephalopathy in the course of alcoholic liver disease--treatment options in the intensive care unit. Anaesthesiol Intensive Ther. 2014;46:34–36. doi: 10.5603/AIT.2014.0007. [DOI] [PubMed] [Google Scholar]
- 59.Rocen M, Kieslichova E, Merta D, Uchytilova E, Pavlova Y, Cap J, Trunecka P. The effect of Prometheus device on laboratory markers of inflammation and tissue regeneration in acute liver failure management. Transplant Proc. 2010;42:3606–3611. doi: 10.1016/j.transproceed.2010.07.103. [DOI] [PubMed] [Google Scholar]
- 60.Stadlbauer V, Krisper P, Aigner R, Haditsch B, Jung A, Lackner C, Stauber RE. Effect of extracorporeal liver support by MARS and Prometheus on serum cytokines in acute-on-chronic liver failure. Crit Care. 2006;10:R169. doi: 10.1186/cc5119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rifai K, Hafer C, Rosenau J, Athmann C, Haller H, Peter Manns M, Fliser D. Treatment of severe refractory pruritus with fractionated plasma separation and adsorption (Prometheus) Scand J Gastroenterol. 2006;41:1212–1217. doi: 10.1080/00365520600610154. [DOI] [PubMed] [Google Scholar]
- 62.Rifai K, Ernst T, Kretschmer U, Hafer C, Haller H, Manns MP, Fliser D. The Prometheus device for extracorporeal support of combined liver and renal failure. Blood Purif. 2005;23:298–302. doi: 10.1159/000086552. [DOI] [PubMed] [Google Scholar]
- 63.Rifai K, Ernst T, Kretschmer U, Haller H, Manns MP, Fliser D. Removal selectivity of Prometheus: a new extracorporeal liver support device. World J Gastroenterol. 2006;12:940–944. doi: 10.3748/wjg.v12.i6.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rifai K, Ernst T, Kretschmer U, Bahr MJ, Schneider A, Hafer C, Haller H, Manns MP, Fliser D. Prometheus--a new extracorporeal system for the treatment of liver failure. J Hepatol. 2003;39:984–990. doi: 10.1016/s0168-8278(03)00468-9. [DOI] [PubMed] [Google Scholar]
- 65.Dethloff T, Tofteng F, Frederiksen HJ, Hojskov M, Hansen BA, Larsen FS. Effect of Prometheus liver assist system on systemic hemodynamics in patients with cirrhosis: a randomized controlled study. World J Gastroenterol. 2008;14:2065–2071. doi: 10.3748/wjg.14.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nadim MK, Kellum JA, Davenport A, Wong F, Davis C, Pannu N, Tolwani A, Bellomo R, Genyk YS ADQI Workgroup. Hepatorenal syndrome: the 8th International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2012;16:R23. doi: 10.1186/cc11188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kribben A, Gerken G, Haag S, Herget-Rosenthal S, Treichel U, Betz C, Sarrazin C, Hoste E, Van Vlierberghe H, Escorsell A, Hafer C, Schreiner O, Galle PR, Mancini E, Caraceni P, Karvellas CJ, Salmhofer H, Knotek M, Ginès P, Kozik-Jaromin J, Rifai K HELIOS Study Group. Effects of fractionated plasma separation and adsorption on survival in patients with acute-on-chronic liver failure. Gastroenterology. 2012;142:782–789.e3. doi: 10.1053/j.gastro.2011.12.056. [DOI] [PubMed] [Google Scholar]
- 68.Piscitani L, Di Vito R, Tunno M, Bonomini M. Successful use of single-pass albumin dialysis in the correction of severe hyperbilirubinemia in a case of acute hepatitis E. Ther Apher Dial. 2023;27:278–283. doi: 10.1111/1744-9987.13909. [DOI] [PubMed] [Google Scholar]
- 69.Sponholz C, Matthes K, Rupp D, Backaus W, Klammt S, Karailieva D, Bauschke A, Settmacher U, Kohl M, Clemens MG, Mitzner S, Bauer M, Kortgen A. Molecular adsorbent recirculating system and single-pass albumin dialysis in liver failure--a prospective, randomised crossover study. Crit Care. 2016;20:2. doi: 10.1186/s13054-015-1159-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sauer IM, Goetz M, Steffen I, Walter G, Kehr DC, Schwartlander R, Hwang YJ, Pascher A, Gerlach JC, Neuhaus P. In vitro comparison of the molecular adsorbent recirculation system (MARS) and single-pass albumin dialysis (SPAD) Hepatology. 2004;39:1408–1414. doi: 10.1002/hep.20195. [DOI] [PubMed] [Google Scholar]
- 71.Kortgen A, Rauchfuss F, Götz M, Settmacher U, Bauer M, Sponholz C. Albumin dialysis in liver failure: comparison of molecular adsorbent recirculating system and single pass albumin dialysis--a retrospective analysis. Ther Apher Dial. 2009;13:419–425. doi: 10.1111/j.1744-9987.2009.00760.x. [DOI] [PubMed] [Google Scholar]
- 72.Collins KL, Roberts EA, Adeli K, Bohn D, Harvey EA. Single pass albumin dialysis (SPAD) in fulminant Wilsonian liver failure: a case report. Pediatr Nephrol. 2008;23:1013–1016. doi: 10.1007/s00467-008-0761-x. [DOI] [PubMed] [Google Scholar]
- 73.Seoung WL, Woo CJ, Su HK, Jin WL, Joon HS, Moon-Jae K. The Use of Single-pass Albumin Dialysis to Correct Severe Hyperbilirubinemia in Acute Hepatitis A: A Case Report. Korean J Nephrol. 2010;29:260–264. [Google Scholar]
- 74.Holle J, Gratopp A, Balmer S, Varnholt V, Henning S, Bufler P, Müller D, Rosenfeld L. Single-Pass Albumin Dialysis in the Treatment of Children with Liver Failure. Blood Purif. 2020;49:55–62. doi: 10.1159/000502938. [DOI] [PubMed] [Google Scholar]
- 75.Rahman E, Al Suwaida AK, Askar A. Single pass albumin dialysis in hepatorenal syndrome. Saudi J Kidney Dis Transpl. 2008;19:479–484. [PubMed] [Google Scholar]
- 76.La Manna G, Donati G. Coupled Plasma Filtration Adsorption: A Multipurpose Extracorporeal Detoxification Therapy. Blood Purif. 2018;46:228–238. doi: 10.1159/000490234. [DOI] [PubMed] [Google Scholar]
- 77.Garbero E, Livigni S, Ferrari F, Finazzi S, Langer M, Malacarne P, Meca MCC, Mosca S, Olivieri C, Pozzato M, Rossi C, Tavola M, Terzitta M, Viaggi B, Bertolini G GiViTI. High dose coupled plasma filtration and adsorption in septic shock patients. Results of the COMPACT-2: a multicentre, adaptive, randomised clinical trial. Intensive Care Med. 2021;47:1303–1311. doi: 10.1007/s00134-021-06501-3. [DOI] [PubMed] [Google Scholar]
- 78.Harm S, Falkenhagen D, Hartmann J. Pore size--a key property for selective toxin removal in blood purification. Int J Artif Organs. 2014;37:668–678. doi: 10.5301/ijao.5000354. [DOI] [PubMed] [Google Scholar]
- 79.Donati G, Angeletti A, Gasperoni L, Piscaglia F, Croci Chiocchini AL, Scrivo A, Natali T, Ullo I, Guglielmo C, Simoni P, Mancini R, Bolondi L, La Manna G. Detoxification of bilirubin and bile acids with intermittent coupled plasmafiltration and adsorption in liver failure (HERCOLE study) J Nephrol. 2021;34:77–88. doi: 10.1007/s40620-020-00799-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tetta C, Cavaillon JM, Schulze M, Ronco C, Ghezzi PM, Camussi G, Serra AM, Curti F, Lonnemann G. Removal of cytokines and activated complement components in an experimental model of continuous plasma filtration coupled with sorbent adsorption. Nephrol Dial Transplant. 1998;13:1458–1464. doi: 10.1093/ndt/13.6.1458. [DOI] [PubMed] [Google Scholar]
- 81.Donati G, Capelli I, Croci Chiocchini AL, Natali N, Scrivo A, La Manna G. Coupled Plasma Filtration Adsorption Application for Liver and Thyroid Toxins. Contrib Nephrol. 2017;190:31–42. doi: 10.1159/000468909. [DOI] [PubMed] [Google Scholar]
- 82.Ullo I, Zappulo F, Bini C, Bruno P, Scrivo A, Donati G, Bolondi L, Piscaglia F, Simoni P, La Manna G. Coupled plasma filtration and adsorption (CPFA) for extracorporeal detoxification during acute and acute on-chronic liver failure. Blood Purif . 2017;44:182. [Google Scholar]
- 83.Maggi U, Nita G, Gatti S, Antonelli B, Paolo R, Como G, Messa P, Rossi G. Hyperbilirubinemia after liver transplantation: the role of coupled plasma filtration adsorption. Transplant Proc. 2013;45:2715–2717. doi: 10.1016/j.transproceed.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 84.Caroleo S, Rubino AS, Tropea F, Bruno O, Vuoto D, Amantea B, Renzulli A. Coupled plasma filtration adsorption reduces serum bilirubine in a case of acute hypoxic hepatitis secondary to cardiogenic shock. Int J Artif Organs. 2010;33:749–752. [PubMed] [Google Scholar]
- 85.Zhang Y, Li L, Zhang X, Xu W, Guo Q, Zhou J. Plasmapheresis Combined with Continuous Plasma Filtration Adsorption Rescues Severe Acute Liver Failure in Wilson's Disease before Liver Transplantation. Blood Purif. 2019;47:120–125. doi: 10.1159/000493909. [DOI] [PubMed] [Google Scholar]
- 86.Larsen FS, Schmidt LE, Bernsmeier C, Rasmussen A, Isoniemi H, Patel VC, Triantafyllou E, Bernal W, Auzinger G, Shawcross D, Eefsen M, Bjerring PN, Clemmesen JO, Hockerstedt K, Frederiksen HJ, Hansen BA, Antoniades CG, Wendon J. High-volume plasma exchange in patients with acute liver failure: An open randomised controlled trial. J Hepatol. 2016;64:69–78. doi: 10.1016/j.jhep.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 87.Tan EX, Wang MX, Pang J, Lee GH. Plasma exchange in patients with acute and acute-on-chronic liver failure: A systematic review. World J Gastroenterol. 2020;26:219–245. doi: 10.3748/wjg.v26.i2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lim H, Kang Y, Park S, Koh H. Effectiveness of High-Volume Therapeutic Plasma Exchange for Acute and Acute-on-Chronic Liver Failure in Korean Pediatric Patients. Pediatr Gastroenterol Hepatol Nutr. 2022;25:481–488. doi: 10.5223/pghn.2022.25.6.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mao W, Ye B, Lin S, Fu Y, Chen Y. Prediction value of model for end-stage liver disease scoring system on prognosis in the acute on chronic liver failure patients with plasma exchange treatment. ASAIO J. 2010;56:475–478. doi: 10.1097/MAT.0b013e3181e6bf13. [DOI] [PubMed] [Google Scholar]
- 90.Xiao LL, Xu XW, Huang KZ, Zhao YL, Zhang LJ, Li LJ. Artificial Liver Support System Improves Short-Term Outcomes of Patients with HBV-Associated Acute-on-Chronic Liver Failure: A Propensity Score Analysis. Biomed Res Int. 2019;2019:3757149. doi: 10.1155/2019/3757149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gashti CN. Membrane-based Therapeutic Plasma Exchange: A New Frontier for Nephrologists. Semin Dial. 2016;29:382–390. doi: 10.1111/sdi.12506. [DOI] [PubMed] [Google Scholar]
- 92.Redant S, De Bels D, Ismaili K, Honoré PM. Membrane-Based Therapeutic Plasma Exchange in Intensive Care. Blood Purif. 2021;50:290–297. doi: 10.1159/000510983. [DOI] [PubMed] [Google Scholar]
- 93.Chris-Olaiya A, Kapoor A, Ricci KS, Lindenmeyer CC. Therapeutic plasma exchange in liver failure. World J Hepatol. 2021;13:904–915. doi: 10.4254/wjh.v13.i8.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen YY, Li H, Xu BY, Zheng X, Li BL, Wang XB, Huang Y, Gao YH, Qian ZP, Liu F, Lu XB, Shang J, Wang SY, Zhang YH, Meng ZJ Chinese Chronic Liver Failure (CLIF) Consortium. Plasma Exchange-Based Non-bioartificial Liver Support System Improves the Short-Term Outcomes of Patients With Hepatitis B Virus-Associated Acute-on-Chronic Liver Failure: A Multicenter Prospective Cohort Study. Front Med (Lausanne) 2021;8:779744. doi: 10.3389/fmed.2021.779744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Caraceni P, Abraldes JG, Ginès P, Newsome PN, Sarin SK. The search for disease-modifying agents in decompensated cirrhosis: From drug repurposing to drug discovery. J Hepatol. 2021;75 Suppl 1:S118–S134. doi: 10.1016/j.jhep.2021.01.024. [DOI] [PubMed] [Google Scholar]
- 96.Prinja S, Bahuguna P, Duseja A, Kaur M, Chawla YK. Cost of Intensive Care Treatment for Liver Disorders at Tertiary Care Level in India. Pharmacoecon Open. 2018;2:179–190. doi: 10.1007/s41669-017-0041-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dellinger RP, Bagshaw SM, Antonelli M, Foster DM, Klein DJ, Marshall JC, Palevsky PM, Weisberg LS, Schorr CA, Trzeciak S, Walker PM EUPHRATES Trial Investigators. Effect of Targeted Polymyxin B Hemoperfusion on 28-Day Mortality in Patients With Septic Shock and Elevated Endotoxin Level: The EUPHRATES Randomized Clinical Trial. JAMA. 2018;320:1455–1463. doi: 10.1001/jama.2018.14618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ruiz-Rodríguez JC, Molnar Z, Deliargyris EN, Ferrer R. The Use of CytoSorb Therapy in Critically Ill COVID-19 Patients: Review of the Rationale and Current Clinical Experiences. Crit Care Res Pract. 2021;2021:7769516. doi: 10.1155/2021/7769516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chen Y, Han T, Duan Z Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Clinical application of artificial liver and blood purification: expert consensus recommendations. Hepatol Int. 2023;17:4–17. doi: 10.1007/s12072-022-10430-8. [DOI] [PubMed] [Google Scholar]
- 100.Alshamsi F, Alshammari K, Belley-Cote E, Dionne J, Albrahim T, Albudoor B, Ismail M, Al-Judaibi B, Baw B, Subramanian RM, Steadman R, Galusca D, Huang DT, Nanchal R, Al Quraini M, Yuan Y, Alhazzani W GUIDE Group. Extracorporeal liver support in patients with liver failure: a systematic review and meta-analysis of randomized trials. Intensive Care Med. 2020;46:1–16. doi: 10.1007/s00134-019-05783-y. [DOI] [PubMed] [Google Scholar]
- 101.Bañares R, Ibáñez-Samaniego L, Torner JM, Pavesi M, Olmedo C, Catalina MV, Albillos A, Larsen FS, Nevens F, Hassanein T, Schmidt H, Heeman U, Jalan R, Moreau R, Arroyo V. Meta-analysis of individual patient data of albumin dialysis in acute-on-chronic liver failure: focus on treatment intensity. Therap Adv Gastroenterol. 2019;12:1756284819879565. doi: 10.1177/1756284819879565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Akcan Arikan A, Srivaths P, Himes RW, Tufan Pekkucuksen N, Lam F, Nguyen T, Miloh T, Braun M, Goss J, Desai MS. Hybrid Extracorporeal Therapies as a Bridge to Pediatric Liver Transplantation. Pediatr Crit Care Med. 2018;19:e342–e349. doi: 10.1097/PCC.0000000000001546. [DOI] [PubMed] [Google Scholar]