Abstract
Background: Helicobacter pylori (H. pylori) is significantly linked to various diseases that seriously impact human health, such as gastric ulcers, chronic gastritis and gastric adenocarcinoma. Methods: The compositional shifts in bacterial communities of the orointestinal axis were surveyed pre/post-eradication of H. pylori. In total, 60 samples, including stool and salivary specimens, were collected from 15 H. pylori-positive individuals (HPP) before beginning and 2 months after receiving the eradication therapy. The V3-V4 regions of the 16S rRNA gene were sequenced using MiSeq. Results: Overall, oral microbiomes were collectively more diverse than the gut microbiomes (Kruskal–Wallis; p = 3.69 × 10−5). Notably, the eradication of H. pylori was associated with a significant reduction in the bacterial diversity along the orointestinal axis (Wilcoxon rank sum test; p = 6.38 × 10−3). Interestingly, the oral microbiome of HPP showed a positive correlation between Proteobacteria and Fusobacteria, in addition to a significant predominance of Streptococcus, in addition to Eubacterium_eligens, Haemophilus, Ruminococcaceae, Actinomyces and Staphylococcus. On the other hand, Fusobacterium, Veillonella, Catenibacterium, Neisseria and Prevotella were significantly enriched upon eradication of H. pylori. Generally, Bacteroidetes and Fusobacteria positively coexisted during H. pylori infection along the orointestinal axis (r = 0.67; p = 0.0006). The eradication of H. pylori was positively linked to two distinctive orotypes (O3 and O4). Orotype O4 was characterized by a robust abundance of Veillonella and Fusobacteria. The gut microbiomes during H. pylori infection showed a remarkable predominance of Clostridium_sensu_stricto_1 and Escherichia_Shigella. Likewise, Bifidobacterium and Faecalibacterium were significantly enriched upon eradication of H. pylori. Conclusions: Finally, the impact of eradication therapy clearly existed on the representation of certain genera, especially in the oral microbiome, which requires particular concern in order to counteract and limit their subsequent threats.
Keywords: orointestinal axis, gut microbiota, Helicobacter pylori eradication, 16S rRNA gene
1. Introduction
Helicobacter pylori (H. pylori) is a gram-negative bacterium that is found in the gastric mucosa [1]. H. pylori is acquired during the early life stage, and the infection continues throughout the patients’ whole lives [2,3,4]. Half of the world’s population is infected with H. pylori which causes gastric diseases such as chronic atrophic gastritis, superficial gastritis and peptic and duodenal ulcers [5]. Moreover, diseases outside the gastrointestinal tract, such as iron deficiency anemia and idiopathic thrombocytopenic purpura, were found to occur due to H. pylori infection, which indicated a correlation between H. pylori infection and diseases outside the gastrointestinal tract [6,7]. International Agency for Research on Cancer has classified H. pylori as a class I carcinogen [8]. Several studies have revealed that the earlier the eradication of H. pylori, the lower will be the probability of gastric cancer [9,10]. That’s why, in some countries, such as Japan and Korea, nationwide eradication therapy has been applied. This is considered as a primary prevention method to treat gastric cancer disease [11,12].
The majority of oral bacteria species are not easily cultured in vitro via traditional cultivation methods, but it requires advanced high-throughput molecular techniques [13]. It has been reported that H. pylori was found in the oral cavity as a result of stomach reflux. The oral cavity acts as a reservoir for H. pylori bacteria [14], and there are various routes for H. pylori transmission between individuals which include both gastro-oral and fecal-oral methods in contaminated food and water [14]. Regarding the oral and gut microbiota, it might originate from different parts of the digestive tract, which includes the bacterial passage from the oral cavity and esophagus to colonize the gastric mucosa or through reflux from the duodenum. There was a microbial similarity detected between gastric juice and the oral cavity [15].
H. pylori infection has been detected to result in dysbiosis of gastric and intestinal microbiota, which is a factor in diseases associated with H. pylori [16]. However, to state whether H. pylori infection is more harmful than useful for gastrointestinal microbiota is yet unclear [17]. Various studies have evaluated the influence of H. pylori eradication on the gut microbiome. After the H. pylori eradication treatment, it was discovered that the bacterial diversity decreased significantly. Therefore, it is important to investigate the impacts of eradication treatment changes on the gut microbiota composition to ensure the maintenance of microbiome homeostasis [18,19,20,21]. Interestingly, one study found that gut microbiota perturbations in several subjects remained for up to 4 years after eradication treatment [22]. The gut microbiota plays an essential role concerning human health, and any imbalance of this microbiota is linked to different diseases [13,14].
The H. pylori eradication effect on the oral and gut microbiota of adults is still not completely investigated. There were few studies investigating H. pylori’s relationship with the microbial community in the oral microbiome, although it was discovered that it passes via saliva [14]. Furthermore, the compositional shifts in the orointestinal axis microbiome that accompany the eradication of H. pylori are not significantly explored yet. Thus, this study targeted to dissect the underlying changes in the orointestinal axis microbiome upon eradication treatment.
2. Material and Methods
2.1. Ethics Statement
This study was approved by the Ethics Committee at the Faculty of Pharmacy, Suez Canal University, Egypt (reference number: 202009PHDH1). The present study was performed following the principles of the Declaration of Helsinki. Written informed consent was obtained from the patients involved in the study.
2.2. Patient Recruitment and Sample Collection
Participants were enrolled at outpatient clinics of the Internal Medicine Department, Al Mabarrah Health Insurance Hospital, Zagazig, Egypt. Patients were diagnosed as H. pylori-positive individuals (HPP) by positive H. pylori stool antigen test and urea breath test (C13-UBT) [23]. The successful eradication of H. pylori was confirmed by a negative H. pylori stool antigen test 2 months after completing the eradication treatment [18]. Two stool samples and 2 saliva specimens were collected from participants upon HPP diagnosis and 2 months after receiving the eradication therapy [24]. The experimental design was based on comparisons of our 4 study groups (Supplementary Figure S1).
The included subjects had good oral hygiene in such a way that they regularly brushed their teeth twice daily for 3 minutes each time [14]. Patients with any of the following criteria were excluded from this study: (1) previous eradication treatment, (2) allergy to any drugs included in this study, (3) previous gastric surgery, (4) the coexistence of severe concomitant illness, (5) pregnant or lactating women, (6) antibiotics, proton pump inhibitor, or probiotics administration during the past 8 weeks, (7) the existence of dental carious and oral abscesses, (8) the presence of any untreated cavitated carious lesions, (9) periodontal disease or periodontal pockets ≥ 4 mm, (10) patients suffering from any systemic diseases such as hypertension, diabetes, or cardiopathy, (11) smoker patients [14,18,25]. The recruited patients received a triple eradication regimen which included clarithromycin (500 mg), omeprazole (20 mg) and amoxicillin (500 mg) for 14 days [25].
Stool samples were collected freshly in a sterile stool plastic container, while saliva samples were collected using a sterile cotton oral swab. Saliva sample collection was carried out in the morning 2 hours after eating [14].
2.3. Genomic DNA Extraction
Genomic DNA of saliva and stool samples were extracted using a Qiagen DNeasy power soil kit (cat. No 12888-100) as recommended by the manufacturer. Oral and stool samples were evaluated by measuring the samples’ absorbance values at 260 and 280 nm. This was performed using a Nanodrop ND-1000 spectrophotometer (ND-1000; Thermo Scientific, Waltham, MA, USA) [26].
2.4. Polymerase Chain Reaction (PCR) Amplification and Sequencing of the 16S rRNA Amplicon
The extracted DNA was amplified by PCR targeting the hypervariable region (V3-V4) of the bacterial 16S rRNA. The V3-V4 hypervariable region of the 16S rRNA gene was amplified using Forward Primer 5′ TCGTCGGCAGCGTCAGATGTGTATAAGAGACAGCCTACGGGNGGCWGCAG and Reverse Primer 5 GTCTCGTGGGCTCGGAGATGTGTATAAGAGACAGGACTACHVGGGTATCTAATCC. The Illumina adapters in those primers are underlined [26]. Sequencing of PCR amplicons was performed at IGA Technology Services (Udine, Italy) on an Illumina MiSeq platform according to the manufacturer’s instructions (Illumina, San Diego, CA, USA) [26,27].
2.5. Bioinformatics and Data Analysis of 16S rRNA Gene Sequencing
The preprocessing of raw 16S rRNA sequences was performed by inputting raw reads in the Quantitative Insights Into Microbial Ecology 2 platform (QIIME2) [28]. The classification of 16S rRNA reads to representative reads was based on Amplicon Sequence Variants (ASVs). Trimming and filtering out, denoising and outputting high-resolution representative ASVs were achieved using DADA2 plugged in QIIME2 (Phred quality ≥19, maximum of two expected errors per read = 2, truncation length 270 and 210 for forward and reverse reads, respectively) [29]. Pre-trained RDP’s naive Bayesian classifier was employed for the taxonomy assignment of ASVs against SILVA reference sequences (V138) [30] at 97% sequence similarity [31].
QIIME2 scripts were run on the entire dataset to identify the patterns of microbial diversity that were associated with the orointestinal axis microbiome. The statistical significance of shifts in bacterial diversity along the orointestinal axis was elucidated using the nonparametric Wilcoxon rank-sum test and the Kruskal–Wallis rank-sum test. The resulting p-values were adjusted using the false discovery rate method (FDR) [32]. Inter-community features (alpha diversity) were identified using observed species and the Shannon diversity index. The similarities between the studied microbiomes were assessed by applying unweighted and weighted UniFrac distance matrices on the generated ASVs. The significance of the clustering of the studied groups was assessed using Permutational Multivariate Analysis of Variance (PRERMANOVA)(Adonis R, package Vegan) [33].
To define the differentially represented genera that drove the shifts in microbiomes, DESeq2 was applied to all genera in the dataset (FDR-corrected p-value < 0.05) [34]. The Correlations between bacterial taxa at different taxonomic levels were assessed by applying Spearman correlation distance (r ≥ ±0.6, p ≤ 0.05) on the dominant taxa (mean relative abundance ≥1.37; R package, Hamsic) [35]. Furthermore, the enterotyping approach was employed to identify the genera that stratify the microbiomes into distinct clusters [36]. Likewise, the taxon that was detected in all of the samples belonging to one site was considered a core taxon for that site. The linear discriminant analysis (LDA) effective size (LEfSe) was performed to define the potential biomarkers associated with each site at sampling (LDA scores >3.0, α = 0.05) [37].
2.6. Data Availability
This study of 16S rRNA raw sequences has been submitted in NCBI bioproject under accession number PRJNA901020 (http://www.ncbi.nlm.nih.gov/bioproject/901020 accessed on 11 June 2023) and biosamples (SAMN31721358:SAMN31721717) and accessed on 11 June 2023. The sequences are available at the NCBI Sequence Read Archive (SRA) under accession numbers (SRR22293484:SRR22293543).
3. Results
3.1. Characteristics of Patients and Data
In total, sixty saliva and stool specimens were derived from 15 H. pylori-positive adults pre/post eradication of H. pylori (eight females and seven males; age: mean ± SD; 47.2 ± 15.15 years). Overall, 2,424,317 raw reads were inputted to Qiime2 and generated 1,912,721 reads (78.89% of all raw reads; median length = 446 bp) which were obtained by merging forward and reverses reads, quality checking, removing low-quality reads and potential chimeric sequences that were used in downstream analyses.
3.2. Distinct Taxonomic Profiles Accompany the Pre/Post-Eradication of H. pylori Infection along the Orointestinal Axis
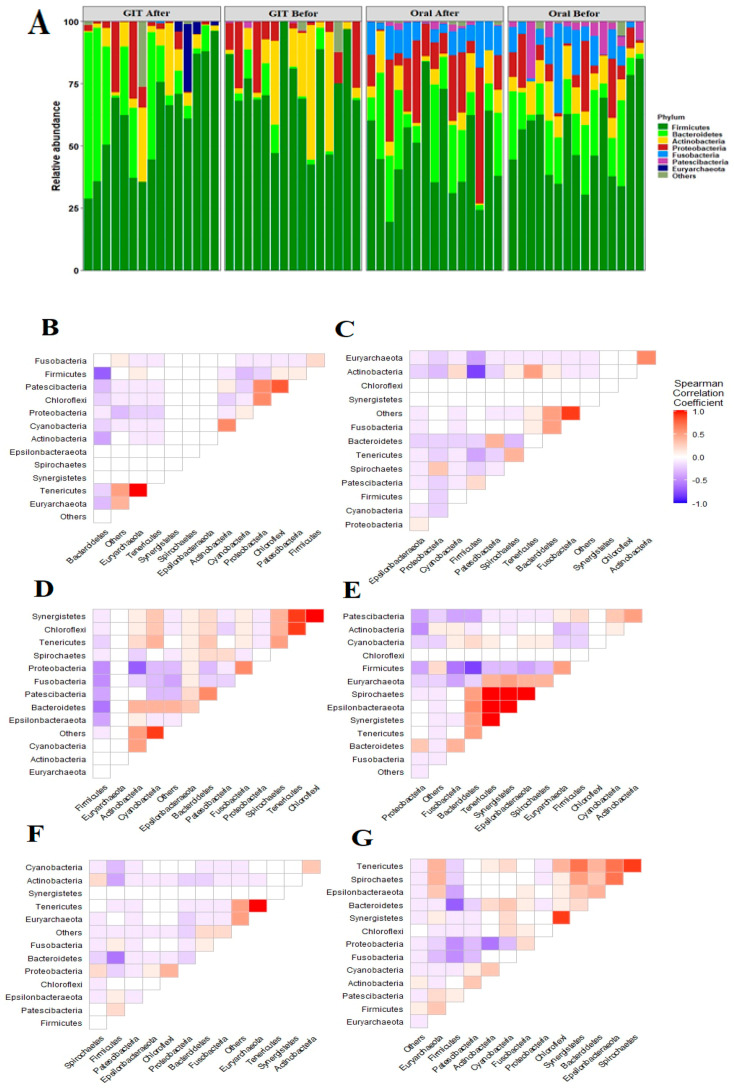
In total, 8846 ASVs were assigned to the corresponding taxonomy in the SILVA database. The overall taxonomy profile of the studied groups was composed of 26 phyla, 42 classes, 97 orders, 247 families, 643 genera and 1358 species. The most abundant phyla across the oral specimens were Firmicutes (50.4%), Bacteroidetes (16.9%), Proteobacteria (12.6%), Fusobacteria (8.8%), Actinobacteria (7.4%) and Patescibacteria (3.3%) (Figure 1A). Regarding stool samples, Firmicutes showed significantly variable proportions in relation to the treatment (68.28% and 47.98% for pre- and post-eradication therapy, respectively; Kruskal–Wallis: p = 6.17 × 10−4). In addition, Proteobacteria and Actinobacteria were enriched during H. pylori infections (13.91% and 9.57%, respectively) in comparison to the post-eradication period (7.52 and 5.82%, respectively).
Figure 1.
Phylum level analysis of oral and gut microbiota. (A) Bar charts illustrated the relative abundance of the major phyla in the oral and gut microbiome before and after eradication therapy of subjects. The X-axis represents the relative abundance. The Y- axis defined the study groups. Corrplots, based on the Spearman correlation coefficient, highlight the association between the main phyla: (B,C) represent the association between dominant phyla in oral microbiomes pre/post eradication of H. pylori. (D,E) define the correlation between the main phyla of gut microbiomes before and after receiving the treatment. (F,G) illustrate the association between the major phyla in the microbiomes of the orointestinal axis during and after the eradication of H. pylori.
Interestingly, Proteobacteria and Bacteroidetes showed variable proportions between either the two sites or sampling events, whereas Proteobacteria in the oral microbiome existed with a relatively diminished abundance before the treatment and was subsequently overrepresented upon eradication of H. pylori. Bacteroidetes was in contrast to Proteobacteria in both sites with enriched proportion in gut microbiome upon eradication of H. pylori. Furthermore, Bacteroidetes and Fusobacteria were positively correlated during H. pylori infection along the orointestinal axis (r = 0.67; p = 0.0006). Remarkably, Firmicutes and Bacteroidetes negatively coexisted in all the studied groups and along the orointestinal axis (Figure 1).
3.3. H. pylori Infections Are Positively Linked with Diverse Orointestinal axis Microbiomes
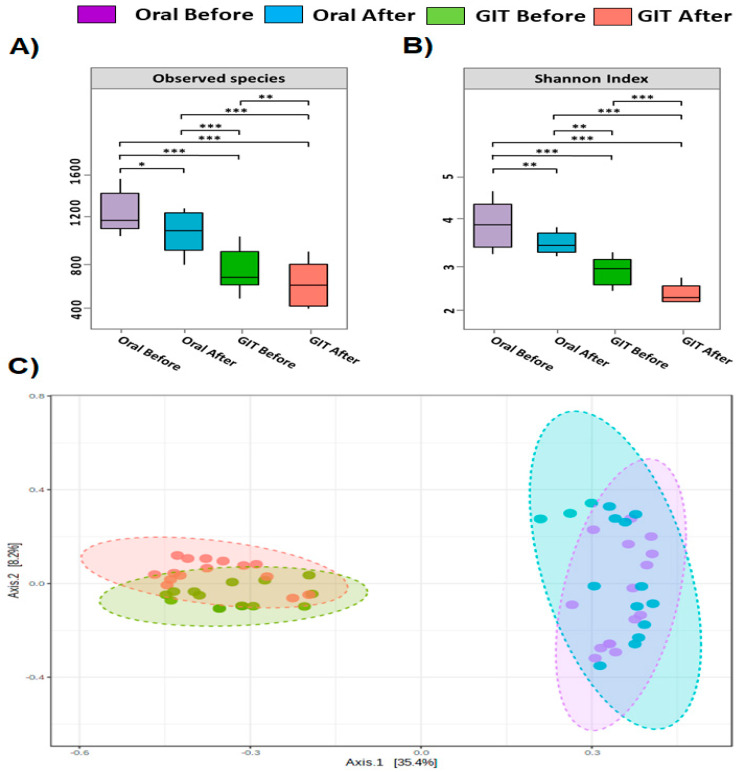
Bacterial diversity analyses in terms of alpha and beta diversity were measured using the entire dataset (Figure 2). Of note, the eradication of H. pylori exhibited a distinct reduction in the bacterial diversity along the orointestinal axis in contrast to HPP (Kruskal–Wallis; p = 3.69 × 10−5; Figure 2A,B). Also, oral microbiota was significantly more diverse than gut microbiomes regardless of the H. pylori infection (Wilcoxon rank sum test; p = 6.38 × 10−3). Furthermore, the overall taxonomic composition showed anatomical and disease-based clustering of samples (Figure 2C; PERMANOVA; 13.728; R-squared: 0.42378; p-value: 0.001).
Figure 2.
Bacterial diversity measurements of orointestinal axis microbiomes. Alpha diversity indices of gut microbiomes illustrated in (A) and (B) panels: Box plots define the bacterial diversity in terms of richness (the number of observed species) and evenness (Shannon diversity index). The X-axis defines the study groups, and the Y-axis denotes the alpha diversity indices. The line in each box indicates the median, the boxes define the interquartile range (IQR) between the 25th and 75th percentile, and the whisker delimits the range. The nonparametric Wilcoxon rank-sum test was employed to identify the statistical significance of pairwise comparisons. Significant differences were indicated with either * (p < 0.05), ** (p < 0.01) or *** (p < 0.001). (C) panel represented PCoA two-dimensional graph of oral and gut microbial community membership before and after eradication therapy (axis 1 = 35.4%; axis 2 = 8.2%). Colors represented the four groups based on before and after treatment. Purple- and blue-colored balls resembled oral samples before and after treatment, respectively. Green- and pink-colored balls resembled stool samples before and after treatment, respectively. Ellipses indicate significant clustering according to site and treatment at (p-value < 0.001, PERMANOVA).
3.4. Orointestinal Axis Microbiomes Have Potential Biomarkers and Microbial Signatures for Pre/Post Eradication of H. pylori
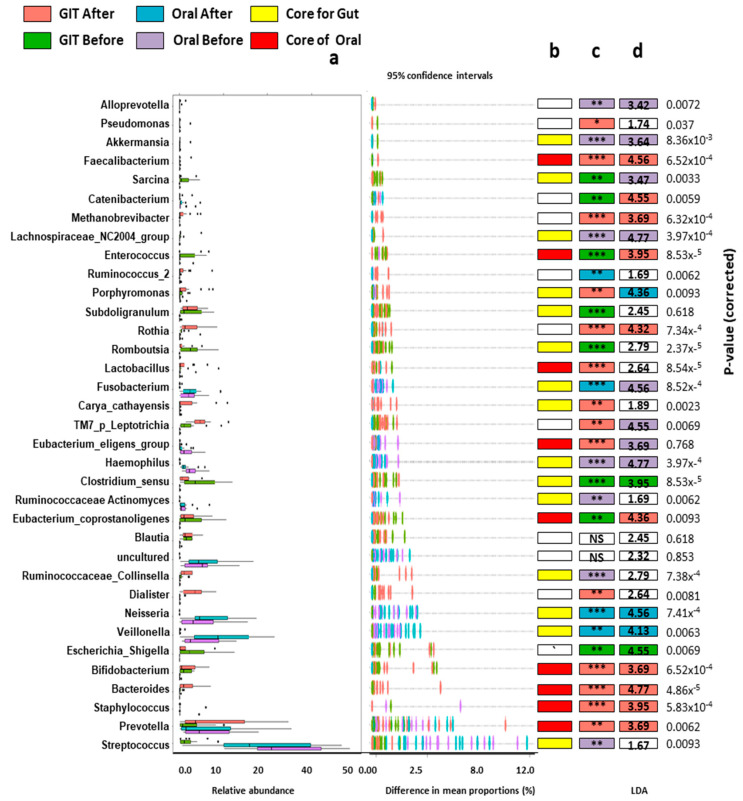
Differentially abundant genera were identified by applying DESEQ2 to all genera in the studied samples (Figure 3). The orointestinal axis microbiomes before the treatment were characterized by the over-representation and positive coexistence of Staphylococcus and Enterococcus (r = 0.086; p = 0.001). On the other hand, the eradication of H. pylori was accompanied by an overrepresentation of Rothia, Romboutsia, Lactobacillus, TM7_p_Lleptotichia, Clostridium_sensu, Blautia, Eubacterium_coprostangolins and Bifidobacterium. Interestingly, the saliva and gut microbiomes were manifested with apparent proportions of certain genera, which could be considered as a biological signature (biomarker) for either the site or the treatment. Regarding oral microbiomes, the H. pylori infection was distinguished by an over predominance of Eubacterium_eligens, Ruminococcaceae_Actinomyces, Enterococcus, Haemophilus and Staphylococcus. The post-eradication of H. pylori showed an enriched abundance of Catenibacterium, Rothia, Lactobacillus, Fusobacterium and Veillonella, in addition to the notable predominance of Prevotella.
Figure 3.
The genus level-based analysis of gut microbiomes associated with the orointestinal axis. (a) Box plots denote the relative abundance and differences in mean proportions with 95% confidence intervals. (b) The colored boxes describe the core genera of gut and oral microbiomes. (c) DESEQ2 was implemented to identify the significantly represented genera between the studied groups. The significant differences were represented either * (p < 0.05), ** (p < 0.01) or *** (p < 0.001). (d) LEfSe was performed to define the Candidate biomarkers for the studied groups, and the numbers indicate LDA scores.
On the other side, the gut microbiome of HPP displayed a prominent representation of Clostridium_sensu_stricto_1, Pseudomonas, Sarcina, Romboutsia, Lactobacillus, Eubacterium_ coprostangolins, Blautia, Bifidobacterium and Streptococcus. On the contrary, Faecalibacterium, Catenibacterium, Methanobrevibacter, Porphyromonas, Rothia, Carya_cathayensis, Dialiaster, Bacteroides and Prevotella increased in abundance after eradication.
3.5. Enterotype and Orotypes of Pre/Post H. pylori Infection
To define the main driver of the orointestinal axis, enterotype analysis was applied to all samples. The term orotype was introduced as being synonymous with the oral cluster. The dominance of Streptococcus, Prevotella, Neisseria, Clostridium_sensu_stricto_1 and Viellonella distinctly clustered the microbiomes to sex enterotypes (Table 1). Oral microbiomes showed a remarkable clustering of samples to four orotypes that mainly were based on the classification of pre/post-eradication of H. pylori to two orotypes for each event.
Table 1.
Enterotypes of Oro-intestinal axis microbiomes.
| Oral Before | Oral After | Gut Before | Gut After | ||
|---|---|---|---|---|---|
| O1 | O2 | O3 | O4 | G1 | G2 |
| Streptococcus | Streptococcus | Streptococcus | Neisseria | Clostridium_sensu_stricto_1 | Prevotella |
| Neisseria | Fusobacterium | Neisseria | Prevotella | Escherichia_Shigella | Bacteroides |
| Ruminococcaceae Actinomyces | Haemophilus | Fusobacterium | Veillonella | Bifidobacterium | Bifidobacterium |
| Eubacterium_eligens_group | Enterococcus | Prevotella | Fusobacterium | Enterococcus | Lactobacillus |
| Porphyromonas | Neisseria | Rothia | Streptococcus | Subdoligranulum | Romboutsia |
| Prevotella | Prevotella | Ruminococcaceae Actinomyces | Ruminococcaceae Actinomyces | Ruminococcaceae_Collinsella | Sarcina |
| Bifidobacterium | Veillonella | Streptococcus | Staphylococcus | Prevotella | Escherichia_Shigella |
| Veillonella | Staphylococcus | Haemophilus | Eubacterium_coprostanoligenes | Blautia | |
| Staphylococcus | Romboutsia | ||||
3.6. Bidirectional Association between Microbiomes, Either Anatomical Sites or the Disease State
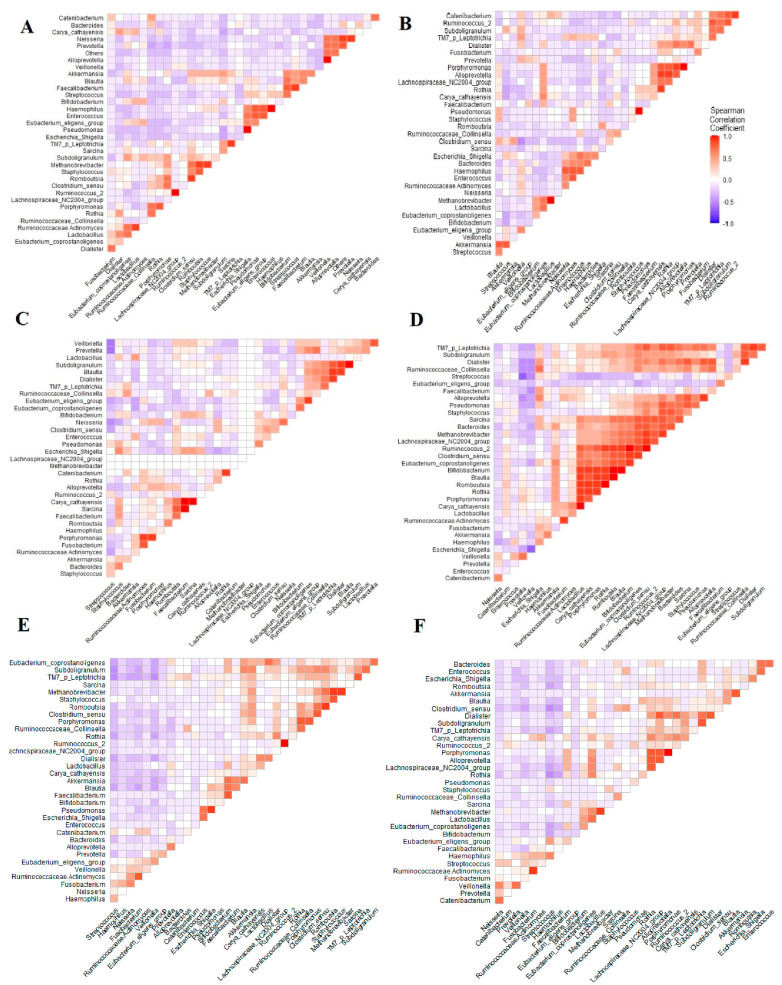
Correlations between oral and gut microbiome before and after eradication at genus taxonomic levels were assessed to infer the coexistence of the dominant genera at the two sites and along the orointestinal axis (Figure 4). Regarding the orointestinal axis, fusobacterium was negatively correlated to Clostridium_sensu_stricto_1. Oppositely, Streptococcus was positively correlated to Clostridium_sensu_stricto_1. Interestingly, combining the oral and saliva microbiomes in pre/post-H. pylori infection revealed that Clostridium_sensu_stricto_1 was significantly linked to a cluster of genera, including Romboutsia, Porphyromonas and Rothia.
Figure 4.
Corrplots based on the Spearman correlation coefficient highlighting the association between the dominant genera: (A,B) demonstrate the association between the dominant genera in oral microbiomes pre/post eradication of H. pylori. (C,D) define the correlation between the main genera of gut microbiomes before and after receiving the treatment. (E,F) represent the association between the major genera in the microbiomes of the orointestinal axis during and after the eradication of H. pylori.
4. Discussion
Helicobacter pylori (H. pylori) is significantly linked to various diseases that seriously impact human health, such as gastric ulcer, chronic gastritis and gastric adenocarcinoma. H. pylori is frequently accompanied by pathophysiological perturbations in the gastric environment, which in turn reshape the microbiota of the orointestinal axis. In this study, we carried out a self-comparison study before and after eradication treatment of salivary and fecal samples to compare oral and gut microbiome composition at the same point in time. It has been shown in a few studies that H. pylori can be transmitted by oral-oral or fecal-oral methods [38]. It was detected that sharing of food, tableware and even kisses could play a role in the transmission of H. pylori. There were a number of previous studies that revealed the existence of H. pylori in saliva [39]. Since those bacteria found in the plaque adhere to the gums, therefore, it is more logical to examine the saliva rather than examining the dental plaque in this study. Previous research has suggested the benefits of H. pylori eradication to prevent gastric cancer and the recrudescence of peptic ulcers. Thus, the impact of antibiotics and proton pump inhibitors on the gut microbiome has focused more attention [9,25].
To date, the H. pylori eradication therapy regimen involves dual therapy, triple therapy and quadruple therapy [40,41]. Triple therapy stays the standard guideline of the European Helicobacter and Microbiota Study Group in areas where clarithromycin resistance is low [42]. EGené et al. study revealed that triple and quadruple therapies were nearly equivalent in effectiveness, compliance and even side effects when administrated to patients suffering from H. pylori infection as a first line of treatment [43]. The administration of triple therapy and its rate of success ranges from 80–85% [44]. Furthermore, the eradication therapy of H. pylori was recently linked to short-term and long-term (less than 6 months) alterations in the gut microbiota of treated individuals (52.3% of cases) [45,46].
The oral samples demonstrated that the relative abundance of Firmicutes, Actinobacteria and Patescibacteria declined following treatment while the relative abundance of Bacteroidetes, Fusobacteria and Proteobacteria increased. On the other hand, regarding stool samples which elucidated that the relative abundance of Firmicutes, Actinobacteria, Proteobacteria, Verrucomicrobia and Patescibacteria decreased after treatment, whereas the relative abundance of Bacteroidetes, Euryarchaeota and Cyanobacteria increased. Gao et al. [16] and Hold and Hansen [47] reported in their studies that H. pylori infection lowered colon acidity leading to a decrease in the relative abundance of Bacteroidetes while Firmicutes and Proteobacteria increased in their relative abundance. Their results were in line with our current study. Various studies demonstrated that H. pylori infection lowers the Actinobacteria abundance [48], as represented in our study, but on the contrary, He et al. [17] reported an increase.
Although Proteobacteria is regarded as a natural inhabitant of the intestine, it constitutes a small part of a healthy microbiome [25]. There was a conflict in the results of the relative abundance of Proteobacteria in salivary and fecal samples in the collected samples, as salivary samples showed an enriched abundance of Proteobacteria after eradication therapy while fecal samples revealed a decrease in their relative abundance. The increase in the Proteobacteria relative abundance in oral samples after eradication therapy might be due to the inhibitory effect of H. pylori eradication on commensal bacteria. Some studies suggested that increased Proteobacteria prevalence in microbial communities can be a possible sign of risk disease and dysbiosis [49].
Overall, oral microbiomes were collectively more diverse than the gut microbiomes. Notably, the eradication of H. pylori was associated with a significant reduction in bacterial diversity along the orointestinal axis. This finding was consistent with previous studies that reported a notable reduction in bacterial diversity upon eradication of H. pylori which could be attributed to the impact of reshaping the gut microbiome as a result of the eradication of H. pylori and the used therapy such as proton pump inhibitor and antibiotics which in turn could manipulate the oral microbiome [14,17,18,19,22,25,27,48,50,51,52,53,54].
Furthermore, the anatomical site-dependent compositional and structural patterns of orointestinal axis microbiomes were clearly manifested in the current study. Beta diversity analysis based on the Bray–Curtis index indicated that the community structure of salivary microbiota before and after eradication therapy was different, and this observation was consistent with Ji et al. finding [14]. Both salivary and fecal samples pre and post-treatment appeared to cluster according to treatment and site, suggesting that H. pylori infection may affect oral and GIT bacterial communities. Obvious separation by the PCoA and PERMANOVA analysis before and after H. pylori eradication therapy clarified that eradication therapy altered the oral and gut microbiome to some extent.
Porphyromonas gingivalis (P. gingivalis) is one of the bacteria which plays a role in gut diseases and periodontitis in the oral cavity. P. gingivalis induced the tight junction proteins depression causing changes in the gut microbiota [55]. In our findings, P. gingivalis was found to be overrepresented after eradication therapy in oral and stool samples which means that H. pylori greatly affects its existence. P. gingivalis was closely related to dysbiosis of the oral-gut axis microbiome. H. pylori eradication was associated with Porphyromonas overrepresentation which must be taken into consideration.
Staphylococcus aureus (S. aureus) colonizes the anterior nares [56], that’s why their existence in the oral cavity is reasonable but at the same time controversial [57]. It is not obvious whether S. aureus plays a portion in the ecology of the healthy normal oral flora or not [58]. Various research has indicated that the oral cavity acts as a reservoir for S. aureus in immunosuppressed patients [57]. S. aureus infections may cause oral diseases like periodontitis and dental caries [59]. Not only this, but it might also cause systemic diseases such as chronic kidney disease, heart disease, Crohn’s disease and orofacial granulomatosis [60,61,62]. In addition, oral S. aureus has been observed as a causative factor in infective endocarditis [63]. Interestingly, S. aureus relative abundance in our study decreased after eradication treatment indicating the influence of eradication on the oral microbiome and the shift in the community composition.
Streptococcus, Enterococcus and Bifidobacterium are probiotics found in the gastrointestinal tract which provide health benefits to the host [64,65,66,67]. Safe strains of Enterococcus are regarded as probiotics in the human gut [68]. These genera were found to have lower abundance in the orointestinal axis after eradication therapy. Overall, H. pylori eradication was revealed to affect and change the abundance of the previously mentioned probiotics in the Oro-intestinal axis microbiome. Previous studies have explained that probiotics supplementation can reduce the changes and imbalance in the gut microbiome due to antibiotics [69,70]. Probiotics supplementation in eradication therapy can decrease dysbiosis and the adverse effects of treatment [18].
The metabolites of the bacteria perform the function of signaling between the gut microbiome and the host. From these bacterial metabolites, there are short-chain fatty acids (SCFAs) which are regarded as the most abundant microbial metabolites. SCFAs are generated by anaerobic gut bacteria through the fermentation of complex carbohydrates which weren’t digested and absorbed in the small intestine [71]. The bacteria that belong to the Firmicutes phylum are able to ferment carbohydrates into SCFAs that increase the intestinal barrier function [72]. There are several functions of these metabolites, such as increasing the junctions’ level in the gastrointestinal tract, preventing inflammations and decreasing mucosal permeability, which are triggered through cytokines [73]. The decrease in the level of SCFAs is related to changes in the host’s health and metabolism [74].
We observed an increase in Bacteroides and Faecalibacterium genera post-H. pylori eradication in stool samples which are categorized as bacteria-producing SCFAs. Bacteroides genera are considered a dominant member of the gut microbiome which participates in the metabolism of carbohydrates and the synthesis of conjugated linoleic acid. In addition, it exerts anti-atherogenic, anti-diabetic, anti-obesogenic and anti-hyperlipidemic effects as well as immunomodulatory properties [75]. Another genus that is highly abundant in the healthy individual colon is the Faecalibacterium genus which plays an important role in producing energy for colonocytes and mediating anti-inflammatory action [23,76]. Lin et al. study [77] stated that Faecalibacterium produces butyrate, which is one of the main short-chain fatty acids found in the gut microbiota. It was found that patients with metabolic and intestinal disorders (for instance, irritable bowel syndrome and inflammatory bowel disease) had decreased levels of the Faecalibacterium genus, which could be considered a biomarker of a healthy intestine [76,78,79]. Thus, Bacteroides and Faecalibacterium genera are considered beneficial bacteria [25]. In this line of thought, we could conclude that the higher abundance of Bacteroides and Faecalibacterium post-eradication was due to compensatory and protective mechanisms.
On the other hand, there are detrimental bacteria as well in the GIT, such as Escherichia-Shigella. However, Escherichia-Shigella relative abundance was increased during H. pylori infection. The overgrowth of Escherichia-Shigella can be associated with dysbiosis of the gut flora leading to serious diseases such as non-alcoholic fatty liver disease, acute necrotizing pancreatitis and inflammatory bowel disease [80,81]. Added to this, Escherichia-Shigella are resistant to a broad range of antibiotics which can spread genes of resistance to both commensal and pathogenic bacteria through horizontal gene transfer [82,83].
Prevotella is a common colonizer of the oral-gut microbiome [84]. This study reported that Prevotella genus relative abundance increased in association with H. pylori eradication leading to orointestinal axis microbiota remodeling. The H. pylori infection affected the growth of Prevotella, but the mechanism still needed to be explored.
Clostridium_sensu_stricto_1 is an opportunistic pathogen that causes intestinal inflammation and lowers the content of SCFAs [85]. In our study, we found that Clostridium_sensu_stricto_1 negatively correlated with fusobacterium and SCFAs, and positively correlated with streptococcus during H. pylori infection, which indicated that it might be concerned with the manifestation of changes and shifts in the orointestinal axis microbiota. Clostridium_sensu_stricto_1 was found to be overrepresented during H. pylori that might occur as a result of compensatory mechanisms.
Our result concerning oral samples showed an augment in Fusobacterium abundance after H. pylori eradication. This genus is pathogenic bacteria that cause infective endocarditis, pneumonia, systemic infections, liver abscess and meningitis [86,87]. It was stated that an increase in Fusobacterium abundance was associated with oral cancer and colorectal cancer [88,89]. Lavelle and Sokol’s study as well indicated that Fusobacterium increased in patients suffering from irritable bowel syndrome (IBS) and was rarely found in healthy persons [90]. Added to this, it can trigger colitis through disruption of the epithelial barrier and results in causing inflammation [91]. It is worth mentioning that elevated Fusobacterium abundance post-eradication may be related to higher oral cancer risk. Therefore, monitoring Fusobacterium relative abundance post-H. pylori eradication is to be considered necessary.
Interestingly, the Veillonella genus was detected to be overrepresented post-H. pylori eradication in salivary samples. Veillonella causes oral diseases such as periodontic and endodontic diseases in humans [92]. Added to this, Veillonella plays a critical role in atherosclerosis and cardiovascular disease development [93]. Thus, it is essential to take into account the elevated abundance level of Veillonella after eradication and its possible effects on human health.
This is the first study in Egypt and the Middle East to demonstrate oral and gut microbiota alterations defining the orointestinal axis as a result of H. pylori infection in a group of patients to investigate the relationship between two different sites before and after eradication therapy. Our results indicated that eradication of H. pylori infection could change the salivary and gut microbiota composition. To the best of our knowledge, this is the premier prospective study to illustrate H. pylori‘s post-eradication impact on orointestinal axis microbiota in Egyptian individuals. On the other hand, the limitations of the present study include the slightly limited sample size and tracking the patterns of orointestinal axis microbiomes at different periods after the eradication of H. pylori to infer the required time for recovery of microbiomes. Also, exploring the overall functional potential of the orointestinal axis microbiome during and after the eradication of H. pylori might provide evidence about the crosstalk between the microbiome and H. pylori.
5. Conclusions
H. pylori is positively associated with collective shifts in microbiomes along the orointestinal axis, which were obviously reshaped upon receiving eradication therapy. The microbiomes along the orointestinal axis during H. pylori infections potentially either protect or implicate the underlying protective or pathogenic mechanisms. Furthermore, the overall intra-microbial relations potentially counteract the predominance of pathogenic residents, in addition to compensatory and recovery mechanisms against the subsequent harmful pathophysiological impacts of H. pylori and the dominant pathogenic competitors. The eradication of H. pylori results in substantial changes in the oral and gut microbiome, which resulted in the robust predominance of harmful bacteria such as Fusobacterium. Finally, the present study provides new insight into the shifts in the oral microbiome that accompany the eradication of H. pylori and an alert about the required interventions in order to frustrate the enrichment of pathogenic bacteria during post-H. pylori transience. Further future prospective investigations and sequencing of the whole metagenome might be required to provide a deeper insight into the taxonomic and functional profile of the oral and gut microbiota.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/pathogens12060832/s1: The study design. A total of 60 salivary and stool samples collected from 15 participants; 15 oral samples before eradication (OB); 15 oral samples after eradication (OA); 15 stool samples before eradication (SB); 15 stool samples after eradication (SA).
Author Contributions
Conceptualization: M.A., S.S., A.A. and M.R.; Methodology: S.A.T. and M.S.; Software: M.R., M.S. and S.A.T.; Formal Analysis: M.R., M.S. and S.A.T.; Preparation of Figures and Tables: M.R. and S.A.T.; Writing—Original Draft Preparation, Reviewing, Editing and Revision: S.A.T., M.A., S.S., A.A., S.S.A.T., A.A., M.S. and M.R. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was approved by the Ethics Committee at the Faculty of Pharmacy, Suez Canal University, Egypt (reference number: 202009PHDH1). The present study was performed following the principles of the Declaration of Helsinki. Written informed consent was obtained from the patients involved in the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
This study of 16S rRNA raw sequences have been submitted in NCBI bioproject under accession number PRJNA901020 (http://www.ncbi.nlm.nih.gov/bioproject/901020) and biosamples (SAMN31721358:SAMN31721717) and accessed on 11 June 2023. The sequences are available at the NCBI Sequence Read Archive (SRA) under accession numbers (SRR22293484:SRR22293543).
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Brown L.M. Helicobacter pylori: Epidemiology and routes of transmission. Epidemiol. Rev. 2000;22:283–297. doi: 10.1093/oxfordjournals.epirev.a018040. [DOI] [PubMed] [Google Scholar]
- 2.Goh K.L., Chan W.K., Shiota S., Yamaoka Y. Epidemiology of Helicobacter pylori infection and public health implications. Helicobacter. 2011;16((Suppl. S1)):1–9. doi: 10.1111/j.1523-5378.2011.00874.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zamani M., Ebrahimtabar F., Zamani V., Miller W.H., Alizadeh-Navaei R., Shokri-Shirvani J., Derakhshan M.H. Systematic review with meta-analysis: The worldwide prevalence of Helicobacter pylori infection. Aliment. Pharmacol. Ther. 2018;47:868–876. doi: 10.1111/apt.14561. [DOI] [PubMed] [Google Scholar]
- 4.Yuan C., Adeloye D., Luk T.T., Huang L., He Y., Xu Y., Ye X., Yi Q., Song P., Rudan I. The global prevalence of and factors associated with Helicobacter pylori infection in children: A systematic review and meta-analysis. Lancet Child Adolesc. Health. 2022;6:185–194. doi: 10.1016/S2352-4642(21)00400-4. [DOI] [PubMed] [Google Scholar]
- 5.Waskito L.A., Salama N.R., Yamaoka Y. Pathogenesis of Helicobacter pylori infection. Helicobacter. 2018;23((Suppl. S1)):e12516. doi: 10.1111/hel.12516. [DOI] [PubMed] [Google Scholar]
- 6.Franchini M., Cruciani M., Mengoli C., Pizzolo G., Veneri D. Effect of Helicobacter pylori eradication on platelet count in idiopathic thrombocytopenic purpura: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2007;60:237–246. doi: 10.1093/jac/dkm195. [DOI] [PubMed] [Google Scholar]
- 7.Choe Y.H., Kim S.K., Son B.K., Lee D.H., Hong Y.C., Pai S.H. Randomized placebo-controlled trial of Helicobacter pylori eradication for iron-deficiency anemia in preadolescent children and adolescents. Helicobacter. 1999;4:135–139. doi: 10.1046/j.1523-5378.1999.98066.x. [DOI] [PubMed] [Google Scholar]
- 8.Wang F., Meng W., Wang B., Qiao L. Helicobacter pylori-induced gastric inflammation and gastric cancer. Cancer Lett. 2014;345:196–202. doi: 10.1016/j.canlet.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 9.Leung W.K., Wong I.O.L., Cheung K.S., Yeung K.F., Chan E.W., Wong A.Y.S., Chen L., Wong I.C.K., Graham D.Y. Effects of Helicobacter pylori Treatment on Incidence of Gastric Cancer in Older Individuals. Gastroenterology. 2018;155:67–75. doi: 10.1053/j.gastro.2018.03.028. [DOI] [PubMed] [Google Scholar]
- 10.Doorakkers E., Lagergren J. Helicobacter pylori eradication treatment and the risk of gastric adenocarcinoma in a Western population. Gut. 2018;67:2092–2096. doi: 10.1136/gutjnl-2017-315363. [DOI] [PubMed] [Google Scholar]
- 11.Kowada A. Cost-effectiveness of Helicobacter pylori screening followed by eradication treatment for employees in Japan. Epidemiol. Infect. 2018;146:1834–1840. doi: 10.1017/S095026881800208X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bae S.E., Choi K.D. The effect of eradication of Helicobacter pylori on gastric cancer prevention in healthy asymptomatic populations. Helicobacter. 2018;23:e12464. doi: 10.1111/hel.12464. [DOI] [PubMed] [Google Scholar]
- 13.Ciric L., Pratten J., Wilson M., Spratt D. Development of a novel multi-triplex qPCR method for the assessment of bacterial community structure in oral populations. Environ. Microbiol. Rep. 2010;2:770–774. doi: 10.1111/j.1758-2229.2010.00183.x. [DOI] [PubMed] [Google Scholar]
- 14.Ji Y., Liang X., Lu H. Analysis of by high-throughput sequencing: Helicobacter pylori infection and salivary microbiome. BMC Oral Health. 2020;20:84. doi: 10.1186/s12903-020-01070-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuan Z., Xiao S. The impact of Helicobacter pylori infection, eradication therapy, and probiotics intervention on gastric microbiota in young adults. Helicobacter. 2021;26:e12848. doi: 10.1111/hel.12848. [DOI] [PubMed] [Google Scholar]
- 16.Gao J.-J., Zhang Y., Gerhard M., Mejias-Luque R., Zhang L., Vieth M., Ma J.-L., Bajbouj M., Suchanek S., Liu W.-D., et al. Association Between Gut Microbiota and Helicobacter pylori-Related Gastric Lesions in a High-Risk Population of Gastric Cancer. Front. Cell. Infect. Microbiol. 2018;8:00202. doi: 10.3389/fcimb.2018.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He C., Peng C., Wang H., Ouyang Y., Zhu Z., Shu X., Zhu Y., Lu N. The eradication of Helicobacter pylori restores rather than disturbs the gastrointestinal microbiota in asymptomatic young adults. Helicobacter. 2019;24:e12590. doi: 10.1111/hel.12590. [DOI] [PubMed] [Google Scholar]
- 18.Hsu P.I., Pan C.Y., Kao J.Y., Tsay F.W., Peng N.J., Kao S.S., Wang H.M., Tsai T.J., Wu D.C. Helicobacter pylori eradication with bismuth quadruple therapy leads to dysbiosis of gut microbiota with an increased relative abundance of Proteobacteria and decreased relative abundances of Bacteroidetes and Actinobacteria. Helicobacter. 2018;23:e12498. doi: 10.1111/hel.12498. [DOI] [PubMed] [Google Scholar]
- 19.Liou J.M., Chen C.C., Chang C.M., Fang Y.J., Bair M.J., Chen P.Y., Chang C.Y., Hsu Y.C., Chen M.J., Chen C.C., et al. Long-term changes of gut microbiota, antibiotic resistance, and metabolic parameters after Helicobacter pylori eradication: A multicentre, open-label, randomised trial. Lancet. Infect. Dis. 2019;19:1109–1120. doi: 10.1016/S1473-3099(19)30272-5. [DOI] [PubMed] [Google Scholar]
- 20.Zamani M., Alizadeh-Tabari S., Zamani V., Shokri-Shirvani J., Derakhshan M.H. Worldwide and Regional Efficacy Estimates of First-line Helicobacter pylori Treatments: A Systematic Review and Network Meta-Analysis. J. Clin. Gastroenterol. 2022;56:114–124. doi: 10.1097/MCG.0000000000001641. [DOI] [PubMed] [Google Scholar]
- 21.Lee Y.C., Dore M.P., Graham D.Y. Diagnosis and Treatment of Helicobacter pylori Infection. Annu. Rev. Med. 2022;73:183–195. doi: 10.1146/annurev-med-042220-020814. [DOI] [PubMed] [Google Scholar]
- 22.Jakobsson H.E., Jernberg C., Andersson A.F., Sjölund-Karlsson M., Jansson J.K., Engstrand L. Short-term antibiotic treatment has differing long-term impacts on the human throat and gut microbiome. PLoS ONE. 2010;5:e9836. doi: 10.1371/journal.pone.0009836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yanagi H., Tsuda A., Matsushima M., Takahashi S., Ozawa G., Koga Y., Takagi A. Changes in the gut microbiota composition and the plasma ghrelin level in patients with Helicobacter pylori-infected patients with eradication therapy. BMJ Open Gastroenterol. 2017;4:e000182. doi: 10.1136/bmjgast-2017-000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen H., Jiang W. Application of high-throughput sequencing in understanding human oral microbiome related with health and disease. Front. Microbiol. 2014;5:508. doi: 10.3389/fmicb.2014.00508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou Y., Ye Z., Wang Y., Huang Z., Zheng C., Shi J., Tang W., Zhang P., Wang S., Huang Y. Long-term changes in the gut microbiota after triple therapy, sequential therapy, bismuth quadruple therapy and concomitant therapy for Helicobacter pylori eradication in Chinese children. Helicobacter. 2021;26:e12809. doi: 10.1111/hel.12809. [DOI] [PubMed] [Google Scholar]
- 26.Tawfik S.A., Azab M.M., Ahmed A.A.A. Illumina MiSeq Sequencing for Preliminary Analysis of Microbiome Causing Primary Endodontic Infections in Egypt. Int. J. Microbiol. 2018;2018:2837328. doi: 10.1155/2018/2837328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou Y., Ye Z., Lu J., Miao S., Lu X., Sun H., Wu J., Wang Y., Huang Y. Long-term changes in the gut microbiota after 14-day bismuth quadruple therapy in penicillin-allergic children. Helicobacter. 2020;25:e12721. doi: 10.1111/hel.12721. [DOI] [PubMed] [Google Scholar]
- 28.Callahan B.J., McMurdie P.J., Rosen M.J., Han A.W., Johnson A.J., Holmes S.P. DADA2: High-resolution sample inference from Illumina amplicon data. Nat. Methods. 2016;13:581–583. doi: 10.1038/nmeth.3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ramadan M., Solyman S., Yones M., Abdallah Y., Halaby H., Hanora A. Skin Microbiome Differences in Atopic Dermatitis and Healthy Controls in Egyptian Children and Adults, and Association with Serum Immunoglobulin E. Omics A J. Integr. Biol. 2019;23:247–260. doi: 10.1089/omi.2019.0011. [DOI] [PubMed] [Google Scholar]
- 30.Quast C., Pruesse E., Yilmaz P., Gerken J., Schweer T., Yarza P., Peplies J., Glöckner F.O. The SILVA ribosomal RNA gene database project: Improved data processing and web-based tools. Nucleic Acids Res. 2013;41:D590–D596. doi: 10.1093/nar/gks1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Q., Garrity G.M., Tiedje J.M., Cole J.R. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl. Environ. Microbiol. 2007;73:5261–5267. doi: 10.1128/AEM.00062-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benjamini Y., Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B Stat. Methodol. 1995;57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 33.Anderson M.J. A new method for non-parametric multivariate analysis of variance. Australas Ecol. 2001;26:32–46. [Google Scholar]
- 34.Love M.I., Huber W., Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harrell F.E., Dupont C.J.R.P.V. Hmisc: Harrell Miscellaneous. Volume 3. The R Foundation; Vienna, Austria: 2008. p. 437. R Package Version. [Google Scholar]
- 36.Arumugam M., Raes J., Pelletier E., Le Paslier D., Yamada T., Mende D.R., Fernandes G.R., Tap J., Bruls T., Batto J.-M. Enterotypes of the human gut microbiome. Nature. 2011;473:174–180. doi: 10.1038/nature09944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Segata N., Izard J., Waldron L., Gevers D., Miropolsky L., Garrett W.S., Huttenhower C. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12:R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bui D., Brown H.E., Harris R.B., Oren E. Serologic Evidence for Fecal-Oral Transmission of Helicobacter pylori. Am. J. Trop. Med. Hyg. 2016;94:82–88. doi: 10.4269/ajtmh.15-0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yee J.K. Helicobacter pylori colonization of the oral cavity: A milestone discovery. World J. Gastroenterol. 2016;22:641–648. doi: 10.3748/wjg.v22.i2.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O’Connor A., Liou J.M., Gisbert J.P., O’Morain C. Review: Treatment of Helicobacter pylori Infection 2019. Helicobacter. 2019;24((Suppl. S1)):e12640. doi: 10.1111/hel.12640. [DOI] [PubMed] [Google Scholar]
- 41.Liu C., Wang Y. The status and progress of first-line treatment against Helicobacter pylori infection: A review. Ther. Adv. Gastroenterol. 2021;14:1756284821989177. doi: 10.1177/1756284821989177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Malfertheiner P., Megraud F., O’Morain C.A., Gisbert J.P. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017;66:6–30. doi: 10.1136/gutjnl-2016-312288. [DOI] [PubMed] [Google Scholar]
- 43.Gené E., Calvet X., Azagra R., Gisbert J.P. Triple vs. quadruple therapy for treating Helicobacter pylori infection: A meta-analysis. Aliment. Pharmacol. Ther. 2003;17:1137–1143. doi: 10.1046/j.1365-2036.2003.01566.x. [DOI] [PubMed] [Google Scholar]
- 44.Tang B., Tang L., Huang C., Tian C., Chen L., He Z., Yang G., Zuo L., Zhao G., Liu E., et al. The Effect of Probiotics Supplementation on Gut Microbiota After Helicobacter pylori Eradication: A Multicenter Randomized Controlled Trial. Infect. Dis. Ther. 2021;10:317–333. doi: 10.1007/s40121-020-00372-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shin C.M., Kim N., Park J.H., Lee D.H. Changes in Gastric Corpus Microbiota With Age and After Helicobacter pylori Eradication: A Long-Term Follow-Up Study. Front. Microbiol. 2020;11:621879. doi: 10.3389/fmicb.2020.621879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sung J.J.Y., Coker O.O., Chu E., Szeto C.H., Luk S.T.Y., Lau H.C.H., Yu J. Gastric microbes associated with gastric inflammation, atrophy and intestinal metaplasia 1 year after Helicobacter pylori eradication. Gut. 2020;69:1572–1580. doi: 10.1136/gutjnl-2019-319826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hold G.L., Hansen R. Impact of the Gastrointestinal Microbiome in Health and Disease: Co-evolution with the Host Immune System. Curr. Top. Microbiol. Immunol. 2019;421:303–318. doi: 10.1007/978-3-030-15138-6_12. [DOI] [PubMed] [Google Scholar]
- 48.Martín-Núñez G.M., Cornejo-Pareja I., Coin-Aragüez L., Roca-Rodríguez M.D.M., Muñoz-Garach A., Clemente-Postigo M., Cardona F., Moreno-Indias I., Tinahones F.J. H. pylori eradication with antibiotic treatment causes changes in glucose homeostasis related to modifications in the gut microbiota. PLoS ONE. 2019;14:e0213548. doi: 10.1371/journal.pone.0213548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shin N.R., Whon T.W., Bae J.W. Proteobacteria: Microbial signature of dysbiosis in gut microbiota. Trends Biotechnol. 2015;33:496–503. doi: 10.1016/j.tibtech.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 50.Abeles S.R., Ly M., Santiago-Rodriguez T.M., Pride D.T. Effects of Long Term Antibiotic Therapy on Human Oral and Fecal Viromes. PLoS ONE. 2015;10:e0134941. doi: 10.1371/journal.pone.0134941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mishiro T., Oka K., Kuroki Y., Takahashi M., Tatsumi K., Saitoh T., Tobita H., Ishimura N., Sato S., Ishihara S., et al. Oral microbiome alterations of healthy volunteers with proton pump inhibitor. J. Gastroenterol. Hepatol. 2018;33:1059–1066. doi: 10.1111/jgh.14040. [DOI] [PubMed] [Google Scholar]
- 52.Gotoda T., Takano C., Kusano C., Suzuki S., Ikehara H., Hayakawa S., Andoh A. Gut microbiome can be restored without adverse events after Helicobacter pylori eradication therapy in teenagers. Helicobacter. 2018;23:e12541. doi: 10.1111/hel.12541. [DOI] [PubMed] [Google Scholar]
- 53.Olekhnovich E.I., Manolov A.I., Samoilov A.E., Prianichnikov N.A., Malakhova M.V., Tyakht A.V., Pavlenko A.V., Babenko V.V., Larin A.K., Kovarsky B.A., et al. Shifts in the Human Gut Microbiota Structure Caused by Quadruple Helicobacter pylori Eradication Therapy. Front. Microbiol. 2019;10:1902. doi: 10.3389/fmicb.2019.01902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wu L., Wang Z., Sun G., Peng L., Lu Z., Yan B., Huang K., Yang Y. Effects of anti-H. pylori triple therapy and a probiotic complex on intestinal microbiota in duodenal ulcer. Sci. Rep. 2019;9:12874. doi: 10.1038/s41598-019-49415-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hsu P.I., Pan C.Y., Kao J.Y., Tsay F.W., Peng N.J., Kao S.S., Chen Y.H., Tsai T.J., Wu D.C., Tsai K.W. Short-term and long-term impacts of Helicobacter pylori eradication with reverse hybrid therapy on the gut microbiota. J. Gastroenterol. Hepatol. 2019;34:1968–1976. doi: 10.1111/jgh.14736. [DOI] [PubMed] [Google Scholar]
- 56.Chen X., Wang N., Wang J., Liao B., Cheng L., Ren B. The interactions between oral-gut axis microbiota and Helicobacter pylori. Front. Cell Infect. Microbiol. 2022;12:914418. doi: 10.3389/fcimb.2022.914418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kearney A., Kinnevey P., Shore A., Earls M., Poovelikunnel T.T., Brennan G., Humphreys H., Coleman D.C. The oral cavity revealed as a significant reservoir of Staphylococcus aureus in an acute hospital by extensive patient, healthcare worker and environmental sampling. J. Hosp. Infect. 2020;105:P396–P589. doi: 10.1016/j.jhin.2020.03.004. [DOI] [PubMed] [Google Scholar]
- 58.Zaatout N. Presence of non-oral bacteria in the oral cavity. Arch. Microbiol. 2021;203:2747–2760. doi: 10.1007/s00203-021-02300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blomqvist S., Leonhardt Å., Arirachakaran P., Carlen A., Dahlén G. Phenotype, genotype, and antibiotic susceptibility of Swedish and Thai oral isolates of Staphylococcus aureus. J. Oral Microbiol. 2015;7:26250. doi: 10.3402/jom.v7.26250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Merghni A., Ben Nejma M., Hentati H., Mahjoub A., Mastouri M. Adhesive properties and extracellular enzymatic activity of Staphylococcus aureus strains isolated from oral cavity. Microb. Pathog. 2014;73:7–12. doi: 10.1016/j.micpath.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 61.Simões-Silva L., Ferreira S., Santos-Araujo C., Tabaio M., Pestana M. Oral Colonization of Staphylococcus Species in a Peritoneal Dialysis Population: A Possible Reservoir for PD-Related Infections? Can. J. Infect. Dis. Med. Microbiol. 2018;2018:5789094. doi: 10.1155/2018/5789094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zuanazzi D., Souto R., Mattos M.B., Zuanazzi M.R., Tura B.R., Sansone C., Colombo A.P. Prevalence of potential bacterial respiratory pathogens in the oral cavity of hospitalised individuals. Arch. Oral Biol. 2010;55:21–28. doi: 10.1016/j.archoralbio.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 63.Gibson J., Wray D., Bagg J. Oral staphylococcal mucositis: A new clinical entity in orofacial granulomatosis and Crohn’s disease. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000;89:171–176. doi: 10.1067/moe.2000.101810. [DOI] [PubMed] [Google Scholar]
- 64.Carmona I.T., Diz Dios P., Scully C. An update on the controversies in bacterial endocarditis of oral origin. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002;93:660–670. doi: 10.1067/moe.2002.122338. [DOI] [PubMed] [Google Scholar]
- 65.Martinović A., Cocuzzi R. Streptococcus thermophilus: To Survive, or Not to Survive the Gastrointestinal Tract, That Is the Question! Nutrients. 2020;12:2175. doi: 10.3390/nu12082175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen J., Chen X., Ho C.L. Recent Development of Probiotic Bifidobacteria for Treating Human Diseases. Front. Bioeng. Biotechnol. 2021;9:770248. doi: 10.3389/fbioe.2021.770248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fijan S. Microorganisms with claimed probiotic properties: An overview of recent literature. Int. J. Environ. Res. Public Health. 2014;11:4745–4767. doi: 10.3390/ijerph110504745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jung J.H., Cho I.K., Lee C.H., Song G.G., Lim J.H. Clinical Outcomes of Standard Triple Therapy Plus Probiotics or Concomitant Therapy for Helicobacter pylori Infection. Gut Liver. 2018;12:165–172. doi: 10.5009/gnl17177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bazireh H., Shariati P., Azimzadeh Jamalkandi S., Ahmadi A., Boroumand M.A. Isolation of Novel Probiotic Lactobacillus and Enterococcus Strains From Human Salivary and Fecal Sources. Front. Microbiol. 2020;11:597946. doi: 10.3389/fmicb.2020.597946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Oh B., Kim B.S., Kim J.W., Kim J.S., Koh S.J., Kim B.G., Lee K.L., Chun J. The Effect of Probiotics on Gut Microbiota during the Helicobacter pylori Eradication: Randomized Controlled Trial. Helicobacter. 2016;21:165–174. doi: 10.1111/hel.12270. [DOI] [PubMed] [Google Scholar]
- 71.Wang Z.J., Chen X.F., Zhang Z.X., Li Y.C., Deng J., Tu J., Song Z.Q., Zou Q.H. Effects of anti-Helicobacter pylori concomitant therapy and probiotic supplementation on the throat and gut microbiota in humans. Microb. Pathog. 2017;109:156–161. doi: 10.1016/j.micpath.2017.05.035. [DOI] [PubMed] [Google Scholar]
- 72.Nogal A., Valdes A.M. The role of short-chain fatty acids in the interplay between gut microbiota and diet in cardio-metabolic health. Gut Microbes. 2021;13:1–24. doi: 10.1080/19490976.2021.1897212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yap T.W., Gan H.M., Lee Y.P., Leow A.H., Azmi A.N., Francois F., Perez-Perez G.I., Loke M.F., Goh K.L., Vadivelu J. Helicobacter pylori Eradication Causes Perturbation of the Human Gut Microbiome in Young Adults. PLoS ONE. 2016;11:e0151893. doi: 10.1371/journal.pone.0151893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nicholson J.K., Holmes E., Kinross J., Burcelin R., Gibson G., Jia W., Pettersson S. Host-gut microbiota metabolic interactions. Science. 2012;336:1262–1267. doi: 10.1126/science.1223813. [DOI] [PubMed] [Google Scholar]
- 75.Cani P.D., Bibiloni R., Knauf C., Waget A., Neyrinck A.M., Delzenne N.M., Burcelin R. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes. 2008;57:1470–1481. doi: 10.2337/db07-1403. [DOI] [PubMed] [Google Scholar]
- 76.Rivière A., Selak M., Lantin D., Leroy F., De Vuyst L. Bifidobacteria and Butyrate-Producing Colon Bacteria: Importance and Strategies for Their Stimulation in the Human Gut. Front. Microbiol. 2016;7:979. doi: 10.3389/fmicb.2016.00979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sokol H., Pigneur B., Watterlot L., Lakhdari O., Bermúdez-Humarán L.G., Gratadoux J.J., Blugeon S., Bridonneau C., Furet J.P., Corthier G., et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl. Acad. Sci. USA. 2008;105:16731–16736. doi: 10.1073/pnas.0804812105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lin H.V., Frassetto A., Kowalik E.J., Jr., Nawrocki A.R., Lu M.M., Kosinski J.R., Hubert J.A., Szeto D., Yao X., Forrest G., et al. Butyrate and propionate protect against diet-induced obesity and regulate gut hormones via free fatty acid receptor 3-independent mechanisms. PLoS ONE. 2012;7:e35240. doi: 10.1371/journal.pone.0035240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li T.H., Qin Y., Sham P.C., Lau K.S., Chu K.M., Leung W.K. Alterations in Gastric Microbiota After H. Pylori Eradication and in Different Histological Stages of Gastric Carcinogenesis. Sci. Rep. 2017;7:44935. doi: 10.1038/srep44935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Miquel S., Martín R., Rossi O., Bermúdez-Humarán L.G., Chatel J.M., Sokol H., Thomas M., Wells J.M., Langella P. Faecalibacterium prausnitzii and human intestinal health. Curr. Opin. Microbiol. 2013;16:255–261. doi: 10.1016/j.mib.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 81.Shen F., Zheng R.D., Sun X.Q., Ding W.J., Wang X.Y., Fan J.G. Gut microbiota dysbiosis in patients with non-alcoholic fatty liver disease. Hepatobiliary Pancreat. Dis. Int. 2017;16:375–381. doi: 10.1016/S1499-3872(17)60019-5. [DOI] [PubMed] [Google Scholar]
- 82.Pascal V., Pozuelo M., Borruel N., Casellas F., Campos D., Santiago A., Martinez X., Varela E., Sarrabayrouse G., Machiels K., et al. A microbial signature for Crohn’s disease. Gut. 2017;66:813–822. doi: 10.1136/gutjnl-2016-313235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Holt K.E., Wertheim H., Zadoks R.N., Baker S., Whitehouse C.A., Dance D., Jenney A., Connor T.R., Hsu L.Y., Severin J., et al. Genomic analysis of diversity, population structure, virulence, and antimicrobial resistance in Klebsiella pneumoniae, an urgent threat to public health. Proc. Natl. Acad. Sci. USA. 2015;112:E3574–E3581. doi: 10.1073/pnas.1501049112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shaikh S., Fatima J., Shakil S., Rizvi S.M., Kamal M.A. Antibiotic resistance and extended spectrum beta-lactamases: Types, epidemiology and treatment. Saudi J. Biol. Sci. 2015;22:90–101. doi: 10.1016/j.sjbs.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Könönen E., Gursoy U.K. Oral Prevotella Species and Their Connection to Events of Clinical Relevance in Gastrointestinal and Respiratory Tracts. Front. Microbiol. 2022;12:798763. doi: 10.3389/fmicb.2021.798763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hu C., Niu X., Chen S., Wen J., Bao M., Mohyuddin S.G., Yong Y., Liu X., Wu L., Yu Z., et al. A Comprehensive Analysis of the Colonic Flora Diversity, Short Chain Fatty Acid Metabolism, Transcripts, and Biochemical Indexes in Heat-Stressed Pigs. Front. Immunol. 2021;12:717723. doi: 10.3389/fimmu.2021.717723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nørskov-Lauritsen N. Classification, identification, and clinical significance of Haemophilus and Aggregatibacter species with host specificity for humans. Clin. Microbiol. Rev. 2014;27:214–240. doi: 10.1128/CMR.00103-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chaucer B., Smith N., Beatty D., Yadav M. Multiple Hepatic Abscess from Parvimonas micra: An Emerging Gastrointestinal Microbe. ACG Case Rep. J. 2018;5:e70. doi: 10.14309/crj.2018.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McIlvanna E., Linden G.J., Craig S.G., Lundy F.T., James J.A. Fusobacterium nucleatum and oral cancer: A critical review. BMC Cancer. 2021;21:1212. doi: 10.1186/s12885-021-08903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hsieh Y.Y., Tung S.Y., Pan H.Y., Chang T.S., Wei K.L., Chen W.M., Deng Y.F., Lu C.K., Lai Y.H., Wu C.S., et al. Fusobacterium nucleatum colonization is associated with decreased survival of helicobacter pylori-positive gastric cancer patients. World J. Gastroenterol. 2021;27:7311–7323. doi: 10.3748/wjg.v27.i42.7311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lavelle A., Sokol H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 2020;17:223–237. doi: 10.1038/s41575-019-0258-z. [DOI] [PubMed] [Google Scholar]
- 92.Liu H., Hong X.L., Sun T.T., Huang X.W., Wang J.L., Xiong H. Fusobacterium nucleatum exacerbates colitis by damaging epithelial barriers and inducing aberrant inflammation. J. Dig. Dis. 2020;21:385–398. doi: 10.1111/1751-2980.12909. [DOI] [PubMed] [Google Scholar]
- 93.Mashima I., Nakazawa F. The interaction between Streptococcus spp. and Veillonella tobetsuensis in the early stages of oral biofilm formation. J. Bacteriol. 2015;197:2104–2111. doi: 10.1128/JB.02512-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This study of 16S rRNA raw sequences have been submitted in NCBI bioproject under accession number PRJNA901020 (http://www.ncbi.nlm.nih.gov/bioproject/901020) and biosamples (SAMN31721358:SAMN31721717) and accessed on 11 June 2023. The sequences are available at the NCBI Sequence Read Archive (SRA) under accession numbers (SRR22293484:SRR22293543).