Abstract
This study aimed to provide a national estimate of the prevalence of the high risk of autism spectrum disorder (ASD) and their determinants. A national screening survey was conducted for 41,640 Egyptian children aged 1 to 12 years in two phases. Tools used were Vineland's Adaptive Behavior Scales, Modified Checklist for Autism in Toddlers, Gilliam Autism Rating scale, and Denver II Developmental screening test. The overall prevalence of children at high risk of ASD was 3.3% (95% CI:3.1%–3.5%). Children living without mothers in homes, suffered from convulsions (AOR = 3.67; 95%CI:2.8–4.8), a history of cyanosis after birth (AOR = 1.87; 95% CI:1.35–2.59) or history of LBW babies (AOR = 1.53; 95% CI:1.23–1.89) carried higher odds of being at high risk of ASD.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-023-04977-5.
Keywords: Autism spectrum disorder, Egyptian national prevalence, Socio-demographic, Epidemiological characteristics, Perinatal
Introduction
According tothe Diagnostic and Statistical Manual of Mental Disorders (5th edition) (DSM-5) criteria, autism spectrum disorder (ASD) is defined as a group of neurodevelopmental disorders characterized by early-onset and persistent impaired social interaction, communication, and restricted/repetitive behavior and interest [22, 43, 96]. Having a child with ASD is accompanied by a great burden of care on family members; physically, emotionally, and financially [7, 57].
The Global Burden of Disease Study estimated ASD prevalence and years living with disability among the common six prevalent developmental disabilities in children under the age of five years [73]. The prevalence of ASD has increased considerably in the last two decades, reaching around 1–2% of the general population due to greater recognition and knowledge of the disease [12].
Around 52 million children with ASD were recorded worldwide in 2010, with a prevalence of 7.6 per 1000 [88]. In 2018, the Centers for Disease Control and Prevention (CDC) reported that nearly 1 in 59 children had ASD. In 2020, that number increased to 1 in 44 children [19]. The most recent data from Europe and the United States show a significant increase in the measured prevalence of autism over the last two decades from 0.48 to 3.13 percent [66]. However, research on ASD prevalence in Arab countries was limited to high-income countries; Systematic meta-analysis in these countries revealed wide variations, Oman, the United Arab of Emirates, Saudi Arabia, Bahrain, Kuwait, and Qatar [1, 8]. Meanwhile, there is a shortage of data concerning ASD prevalence in developing Arab countries. Generally speaking, the great variation in the prevalence of ASD estimates that was found in Arab countries was due to the variation in the study methods, age of participants, case ascertainment approaches, and diagnostic tools used as there is no standardized method for screening of ASD until now which is considered a challenging situation. Due to the same reasons, studies in Egypt estimated great variability of ASD prevalence ranging from 5.4/1000 [102] to 33.6% [85]. At the same time, studies in Egypt were limited to, confined areas, facility-based, and with a limited sample size [41, 102].
Till now, the causes and risk factors of ASD are not well known with many operational risk factors; prenatal, perinatal, and environmental [87, 97]. Even though, there is growing evidence that ASD has become a public health problem in many countries. Such findings indicated that autism has to be perceived as an important problem that deserves to be in the light spot for policymakers to allow delivery of targeted services, especially in developing countries where access to therapeutic effective services is either limited or not existed. Early detection of ASD is crucial for prompt and early intervention to achieve significant improvement in behavioral performance and the intellectual abilities of children with ASD.
This study aimed at providing a national screening estimate of children who are at high risk of ASD among Egyptian children aged 1 to 12 years with integration of their developmental level based on reliable screening tools used during two phases. The study identified the possible determinants of the at high risk of ASD that are related to sociodemographic, epidemiological, maternal, and child health status.
Methodology
Study type, design, and setting
The current study was both community and facility based, represented a part of a national Egyptian survey for estimation of the prevalence of autism spectrum disorder among children aged 1 to 12 years. This survey included four phases. Phase one was a household community based survey planned for detection of children with deviated development and potentially suspicious for autism. In phase two, these children were referred to maternal and child health centers and screened for ASD using ASD screening tools. Diagnosis of ASD was confirmed in phase three using DSM-5 criteria and CARS. Children with confirmed diagnosis of ASD were assessed for intellectual functions and adaptive behavior in phase four.
The current study reported results of the first and second phases to detect the at high risk of autism, meanwhile confirmed cases with autism and their characteristics will be published in another manuscript. It was a cross-sectional national screening study which was done in two phases. The study was conducted in 8 Governorates representing all geographic regions of Egypt according to their population density. The whole study was conducted over 24 months starting from December 2017 till December 2019.
Target group
The study targeted parents or caregivers with their children aged 12 months up to 12 years at the visited houses.
Inclusion and exclusion criteria
Any child in the age range of 12 months to 12 years whether previously identified as having ASD or with typical or deviated development according to [15, 99], whose parents accepted to participate was included in the study. The response rate of acceptance for participation was 100%.
Exclusion criteria: Children with known or previously diagnosed with genetic disorders (e.g., Down syndrome, Turner syndrome, or fragile-X syndrome) as assessed by a clinical genetics team from the National Research Centre of Egypt. The validated WHO ten-question screening tool with their probes was explained to the household for detecting any disability that is affecting hearing, vision, movement, learning, thinking, or social relationships whether for children or their parents [24, 70].
The researchers ensured that all children with detected disabilities or delay other than autism were enrolled in rehabilitation programs by the Ministry of Health. Those with autism were referred for management to the outpatients' clinics of Children with Special Needs and clinic of Clinical Genetics Department of the National Research Centre of Egypt.
Sampling frame and cluster preparation
Three sampling frames were chosen in three stages; the first sampling frame used was the comprehensive list of the governorates in Egypt according to the enumeration census from the Central Agency for Public Mobilization and Statistics (Central Agency for Public Mobilization and Statistics (CAPMS) [20]. In the first stage, a representative sample of 8 governorates was selected to represent the main geographic areas in Egypt including; One urban (Cairo), three Upper Egypt (Fayoum, Assuit, and, Aswan), three Lower Egypt (Damietta, Dakahlia, and, Gharbia) and One border -Frontier- (Marsa Matrouh). In the second stage, a representative sample of cities and local units were selected from each governorate. In this selection process, each governorate was divided into three categories according to its human development scores, namely low, medium, and high [10, 26]. One city for urban areas and a local unit for rural areas were selected from each category for each governorate. In the third stage, for urban areas, the selected cities were divided into city blocks then choosing one or two blocks for surveying. For the rural areas, one or two villages were selected from the selected local units (according to population size). A total of 45-blocks ensured both the adequate sample size and heterogenicity of data collected. In this stage, households in the selected cities and villages blocks were screened. The sample was allocated to be proportional to the size of large governorates. While governorates with relatively small populations were assigned to arbitrary sample sizes with adjusting weights during the analysis of the data.
Survey sample size
The sample size calculation is based on the estimated prevalence of ASD which was 1% as indicated from the previously stated survey studies in Arab countries [85]. Taking this prevalence into consideration ensured the largest sample size at a level of accuracy set at 0.0049 (margin of error), confidence limit of 95%, and the least reliable of the questionnaires used for detecting Autism was 80%. Accordingly, targeting 40,000 children were expected to ensure data accuracy for the provision of estimates of the prevalence of ASD [44]. The actual number obtained was 41,640 from 22,026 surveyed houses along 45 blocks from the eight targeted governorates.
Study instruments
Autism spectrum disorder is characterized by sorts of delay and deviation in the development of social, communication, and cognitive functions, which begin in the first years of life. Autism spectrum disorder has a varied range of syndrome expression and its diagnosis presents actual challenges [94]. In the current study assessment of the targeted children was done on two levels.
5.1First phase screening
This phase was a screening phase carried out at the household level. It was directed to parents/caregivers of children in the age range of 12 months to 12 years. Due to lack of professional specialists for ASD screening of the enormous number of children (41,460 children), and lack of registration of developmentally delayed children in Egypt, the research team preferred to use the Arabic version of Vineland Adaptive Behavior Scales, (VABSA) [6] for assessment in the first phase screening. The main output of this phase was children with deviated development or aberrant behavior who potentially had one of the neurodevelopmental disorders among which ASD was suspected. Through face-to-face interviews with the parents or caregivers, three parts of a household-developed questionnaire were fulfilled.
The first part of the household questionnaire
Collected information on housing and sociodemographic characteristics including age, sex, birth order, number of siblings, maternal age, residence, and parental education and occupation [10, 26, 31].
The second part of the questionnaire
collected information about the epidemiological, maternal, and neonatal risk factors for autism that were identified before [37].
The third part of the questionnaire
Included adaptive behavior assessment using VABS.
The Vineland Adaptive Behavior Scales (VABS) is one of the most commonly used measures of parent-reported adaptive behavior for individuals from birth through adulthood [92]. It measures adaptive functioning across four domains: Communication, Daily Living Skills, Socialization and Motor Skills. It supports diagnosis of intellectual and developmental disabilities, autism, and developmental delay [42]. The measured four domains integrated eleven subdomains. For example, the subdomains of socialization domain inscribe interpersonal relationships, play and leisure time, and coping skills which are greatly impacted in children with ASD. A number of old and recent studies suggested the usefulness of VABS as a well-standardized, normative assessment instrument for verifying autistic social dysfunction [95, 34, 90, 30, 83].
The Vineland survey form, which is administered in 15–20 min by a trained interviewer, was used in this study. The mean of the adaptive behavior composite score is 100 with SD of 15. A delay in specific domain is considered if the score of that domain is 2 SD below the mean (< 70). The VABS survey form demonstrated high reliability coefficient ranging from 0.83 to 0.94 across all domains [92]. Discovered children with low scores (< 70) on VABS suggesting developmental delay were referred to maternal and child health centers and screened for ASD using ASD screening tools.
5.2Second phase screening
In this phase the referred children were screened for ASD according to their ages. Either with the Modified checklist for autism in toddlers-revised [68, 76] for children aged 1–3 years. Or with (Gilliam Autism Rating scale (GARS-2) for children aged 3–12 years [82]. Denver II Developmental screening test (DDST) was used for developmental assessment and developmental regression of children up to 6 years [33]. The output of this phase was to find out the children who were scored positive for autism according to M-Chat, and GARS-2.
The M-CHAT is a parent-completed questionnaire that includes items from the CHAT that cover a broader range of signs and a wider age range (16–30 months). The sensitivity of the M-CHAT was reported to be as high as 85%, but specificity is low around 40%. Parents were asked in more detail about symptoms identified by the first phase questionnaire. This interview increases the specificity of the M-CHAT and is highly recommended. If the total score of M-CHAT was 0–2, The child has screened negative. Rescreening is needed at 24 months if the child is younger than 2 years old. If the total Score was 3–7: The child is at moderate risk, and at a score of 8–20 the child is at high risk. In cases of moderate and high-risk individuals, the child should be referred for diagnostic evaluation and early intervention. In the current study, the child was referred for diagnostic evaluation by the NRC consultants when the total score was 3 or more [56].
Gilliam Autism Rating Scale (GARS-2) although could be used for verification of autism diagnosis it was used as screening for children aged 3–12 years who have severe behavioral problems that may be indicative of autism. GARS-2 is a 42-item norm-referenced screening tool to help professionals identify ASD. The GARS-2 gathers information about specific characteristics typically noted in children with autism spectrum disorders in three subscales (Stereotyped Behaviors, Communication, and Social Interaction) and it contains a developmental history. The Autism Index is calculated by first calculating the raw scores of each subscale and then converting them into derived standard scores. Scores of 85 or higher on the Autism Index indicate that an individual is likely to have autism. Scores of 70 to 84 indicate that an individual may have autism, and any score of 69 or less suggests that it is unlikely that the individual has autism [35]. In the current study, nurses were instructed to refer children to consultants once the autism index was 70 or more to avoid missing probable cases.
Denver II Developmental Screening Test (DDST): This test is a screening measure to identify possible developmental delays in children ages birth through six years. Screening includes four developmental areas: personal-social, fine-motor adaptive, language, and gross motor. There is one form for all ages. The test includes direct child assessment and parent report, and takes 10–20 min to complete. Each item is scored as passed, failed, or refused. DDST is a norm-referenced test. Items that can be completed by 75% of children but are failed by the examined child are called cautions; items that can be completed by 90% of children but are failed by the examined child are referred to as delays. The test is interpreted as Normal, Suspect, or Untestable according to the number of items upon which the child scores below or within the expected age range [33]. The sensitivity and specificity of this test are 0.83 and 0.43 respectively [36]. In the current study, all children interpreted as Suspect or Untestable were referred to specialized physicians in the health care centers of the Ministry of Health and Population (MOHP) and NRC team to ascertain the results of screening test.
Survey implementation
Before the implementation of phase one and two, condensed training sessions about how to conduct the relevant used questionnaires in a standardized way were done. Both phases were done under the supervision of specialized team members.
Phase one of the survey was conducted by the pre-trained 64 social workers (average 6/governorate) under the supervision of a collaborative team from the Cairo Demographic Center (CDC) with professional team members from the National Research Centre of Egypt (NRC).
The range of the targeted houses per governorate was from 1960–4170 (S table-1). Each social worker targeted an average of 6 houses per day for an average of 5 months. The implementation of both phase one and phase two was conducted over one year in a simultaneous way along the geographical areas of the eight randomly selected governorates. A pilot study was performed on 80 participants (10/governorate) to ensure the validity of the questionnaire items through revising and modifying difficulty- understood items or language and then re-introduced them.
In this phase, Vineland Adaptive Behavior survey form was administered by the social workers who have properly trained on this questionnaire. It was reported that, a psychologist, social worker, or other professional who has appropriate training in interview techniques can complete these forms [72].
Before starting implementation of phase II, 208 selected nurses were trained by specialized consultants (26 per each governorate) to ensure using the screening tests for autism and development and calculate the score. This number was chosen for covering 45-blocks of Shiaka and villages (within 24 Kism in urban areas and 21 markaz in rural areas) to ensure heterogeneity of the data collected (S table-1). For suspicious children who did not attend the health facilities, outreach visits by the trained nurses were scheduled for meeting the children and undergoing reliable tests. Moreover, recognized children with suspected developmental delays and/or autism were confirmed by specialized physicians in the health care centers of the Ministry of Health and Population (MOHP) and NRC to ascertain the results of the 2nd screening phase.
In this phase the well-trained nurses administered 3 psychological tests:
The M-CHAT and Denver Developmental screening tests (DDST). Administration of these tests usually does not need a specialist and can be administered by individuals who have trained to proficiency [16, 38, 56]. Nurses were directed to refer children to consultants when the DDST was interpreted as suspect or untestable and when the child had a score of 3 or more on M-CHAT.
Gilliam Autism Rating Scale (GARS-2), although administration of this test needs a professional individual, it was administered by the well-trained nurses who have received extensive training and were closely supervised by qualified consultants and supervisors. Nurses were instructed to refer children to consultants once the autism index was 70 or more to avoid missing probable cases. (The child is likely to be diagnosed with autism at scores of 85 or more).
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 22.0 software (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). All data were represented by percentages and comparisons between groups were done using crude odds ratios and 95% confidence intervals (CI) were calculated in comparison between DDs and children without delays. Probability values (p) < 0.05 were regarded as statistically significant. Logistic regression analysis was done to assess the contribution of each independent variable to predict the odds of ASD based on the values of the independent variables (risk factors for ASD) by using the Adjusted odds ratio [93]. A significant association is considered if the 95% CI does not include the value of 1.0, and a cutoffp-value of less than 0.05 is used for all tests of statistical significance in this study.
Results
Table 1 shows the socio-demographic characteristics and perinatal problems of the study population. The parents or the caregivers of 41,640 children in the age range 1–12 years were participated in the study. Children were slightly insignificantly higher in rural than urban communities. They were equally distributed among social classes. They were distributed among the randomly selected governorates according to their population size. The surveyed boys were insignificantly slightly higher than girls (51.5% versus 48.5% respectively). Half of the children were in the age group 6 to 12 years (48.8%). The least percentage of children were in the age group 1- < 3 years (20.1%). 95.8% of children above 6 years went to school. The mean age at which mothers gave birth was 26.06 ± 6.13 years and their current mean age was 32.04 ± 6.81 years. Regarding education levels, almost half of mothers and fathers completed their higher school degrees (44.7% and 44.2% respectively). Most of the mothers were unemployed (84.8%). Houses without mothers were 0.7% versus 4.6% without fathers. Among the perinatal conditions, the presence of a history of neonatal jaundice after birth was the most prevalent (26.5%) followed by a history of difficult labor (14.6%). 0.9% of houses had mothers who were physically or mentally disabled and 4.3% had twins. History of LBW was reported among 4.4% versus 1% with a history of premature delivery.
Table 1.
Characteristics of the study population
| Socio-demographic characteristics | Surveyed children n = (41,640) |
|---|---|
| N (%) | |
| Locality (Urban/ Rural) | |
| Urban | 19,422 (46.6%) |
| Rural | 22,218 (53.4%) |
| Social class | |
| Low | 13,586 (32.6%) |
| Middle | 13,887 (33.4%) |
| High | 14,167 (34.0%) |
| Geographical Distribution | |
| Cities | 6919 (16.6%) |
| Lower Egypt | 15,892 (38.2%) |
| Upper Egypt | 14,344 (34.5%) |
| Frontier | 4485 (10.8%) |
| Mean no of households ± SD | 4.97 ± 1.281 |
| Sex | |
| Surveyed boys | 21,437 (51.5%) |
| Surveyed girls | 20,203 (48.5%) |
| Age | |
| 1- < 3 years | 8383 (20.1%) |
| 3- < 6 years | 12,933 (31.1%) |
| 6–12 years | 20,324 (48.8%) |
| School attendance statusa (n = 20,332) | |
| Child goes to school | 19,470 (95.8%) |
| Does not go to school | 858 (4.2%) |
| Mean Mother age at giving birth ± SD | 26.06 ± 6.13 |
| Mean Current maternal age ± SD | 32.04 ± 6.81 |
| Mothers Education | |
| Illiterate/ below high school | 16,046 (38.5%) |
| High School | 18,609 (44.7%) |
| University or higher | 6674 (16.0%) |
| Fathers Education | |
| Illiterate/ below high school | 14,666 (35.2%) |
| High School | 18,390 (44.2%) |
| University or higher | 6662 (16.0%) |
| Mothers´ work | |
| Employed | 6014 (14.4%) |
| Unemployed | 35,315 (84.8%) |
| Presence of mothers or fathers | |
| No father in the HH | 1922 (4.6%) |
| No mother in the HH | 299 (0.7%) |
| Prenatal, natal and neonatal problems | |
| History of Premature delivery (< 37 weeks gestation) | 413 (1%) |
| History of Low birth weight (LBW) (< 2500 g) | 1848 (4.4%) |
| Children with history of jaundice after birth | 11,028 (26.5%) |
| Children with history of cyanosis after birth | 546 (1.3%) |
| Children with history of any convulsions after birth | 675 (1.6%) |
| Children kept in an incubator for more than two days | 3078 (7.4%) |
| Children with history of meningitis after birth | 378 (0.9%) |
| Twins | 1774 (4.3%) |
| Mothers have any health problem during pregnancyb | 2770 (6.6%) |
| Difficult laborc | 6092 (14.6%) |
| Disabled mothersd | 373 (0.9%) |
aof children aged 6 -12 years,
bMothers having complications during pregnancy such as gestational diabetes, hypertension, iron deficiency anemia, anxiety, depression, or infection [18]
cDifficult labor refers to prolongation in the duration of labor, especially in the first stage of labor. It can be a contributor to maternal mortality and morbidity if unrecognized or untreated [13]
ddisabled mother: physically or mentally disabled; Hearing, Vision, Mental, Movement, Speech [99, 100]
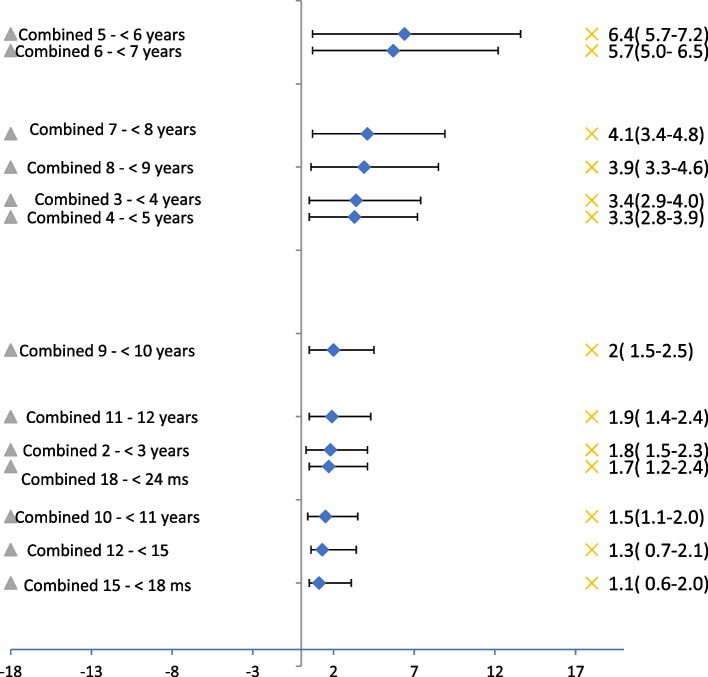
Age and sex-specific estimates of ASD appeared in Figs. 1 and 2 respectively. Group-specific prevalence was highest for the age group 5- < 6 years (6.4%, 95% CI: 5.7%–7.2%) followed by age group 6- < 7 (5.7%, 95% CI: 5.0%–6.5%) as shown in Fig. 1.
Fig. 1.
Screening plot per age distributed according to the highest prevalence/age, the overall prevalence among children aged 1–12 years (Combined sex) = 3.3% (95% CL: 3.1%-3.5%), Population Survey
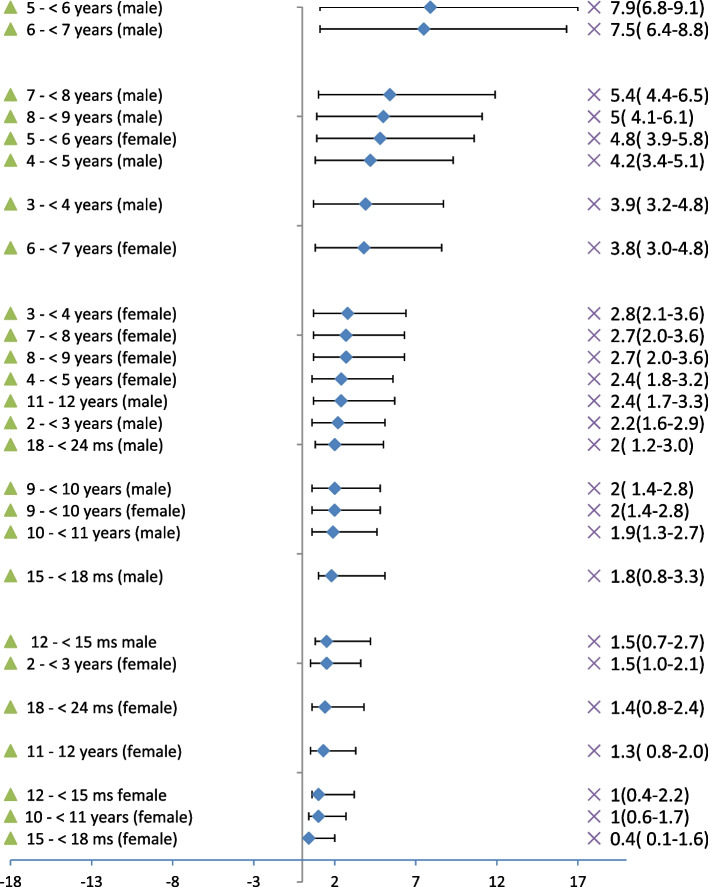
Fig. 2.
Screening plot per sex distributed according to the highest prevalence/sex, COR males/Females = 1.72 (95% CL: 1.53–1.92), Population Survey
The prevalence of ASD among boys was almost double that of the girls for these two specific age groups (COR = 1.70, 95% CI: 1.32%–2.19% & COR = 2.06, 95% CI: 1.54%–4.88% respectively) as shown in Fig. 2.
Summing the prevalence of the at high risk of ASD among children aged 1–12 years was 3.3% (95% CI: 3.1%–3.5%). The prevalence of the at high risk of ASD among boys aged 1–12 years was 4.1% (95% CI: 3.4%–4.8%) versus 2.4% (95% CI: 1.7%–3.3%) among girls in the same age group. Having a child at high risk of ASD was likely to be found among boys one and three-quarters times that of girls in the age range 1–12 years (COR 1.72, 95% CI: 1.53%–1.92%).
Table 2 shows the odds of having features of autism among surveyed children according to the socio-demographic and child characteristics. Having at high risk of ASD was higher among children belonging to the middle class than belonging to either the high and low classes (COR 1.53, 95% CI: 1.34–1.73 & COR 1.72, 95% CI: 1.51–1.97 respectively). Living in urban communities was associated with significantly increased odds of at high risk for ASD than living in rural (COR = 1.71, 95% CI: 1.53–1.91). Living in Lower Egypt or in Frontiers significantly decreased the odds of at high risk of ASD than living in cities by more than 60% (COR = 0.39, CI: 0.34–0.44 & COR = 0.36, CI: 0.29–0.45 respectively).
Table 2.
Odds of having at high risk of Autism among surveyed children according to the sociodemographic and child characteristics
| sociodemographic and child characteristicsa |
All ASD (n = 1370) n(%) |
Boys (n = 879) n(%) |
Girls n = 491 n(%) |
COR (95% CI) All versus Healthy |
|---|---|---|---|---|
| Locality (Urban/ Rural) | ||||
| Urban (19,422) | 815 (4.2) | 513(2.65) | 302(1.6) |
Urban/ rural 1.71* (1.53–1.91) |
| Rural (22,218) | 555 (2.5) | 366(1.65) | 189(0.85) | |
| Social class | ||||
| Low (13,586) | 351 (2.6) | 243 (1.8) | 108(0.8) |
Middle vs. low 1.72(1.51–1.97)** |
| Middle (13,887) | 607 (4.4) | 361 (2.6) | 246 (1.8) |
Middle vs. high 1.53(1.34–1.73)** |
| High (14,167) | 412 (2.9) | 275 (1.9) | 137(1.0) |
low vs. high 0.89(0.766–1.02) |
| Geographical Distribution | ||||
| Cities (6919) | 462 (6.7) | 285(4.1) | 177(2.6) |
Lower vs Cities 0.39 (0.34–0.44)** |
| Lower Egypt (15,892) | 428 (2.7) | 264(1.7) | 164(1.0) |
lower vs. Frontiers 1.07 (0.87–1.32) |
| Upper Egypt (14,344) | 367 (2.6) | 251(1.7) | 116(0.9) |
upper vs. Frontiers 1.02(.82–1.26) |
| Frontier (4485) | 113 (2.5) | 79(1.8) | 34(0.7) |
Frontiers vs cities 0.36(0.29–0.45)** |
| Age category | ||||
| 1- < 3 years (8383) | 137 (1.6) | 86 (1.0) | 51 (0.6) |
3- < 6 years vs. 1- < 3 2.77(2.29–3.34)** |
| 3- < 6 years (12,933) | 568 (4.4) | 360(2.8) | 208(1.6) |
3- < 6 years vs. 6–12 years 1.46(1.21–1.52)** |
| 6–12 years (20,324 | 665 (3.3) | 433(2.1) | 232(1.2) |
6-12 years vs. 1- < 3 years 0.99 (0.89–1.1) |
| School attending statusb (n = 20,332) | ||||
| 1. Child goes to school (19,470) | 1247 (6.4) | 790 (4.1) | 457 (2.3) |
2 vs 1 5.2 (4.43–6.17)** |
| 2. Does not go to school (858) | 123 (14.3) | 89(10.4) | 34(3.9) | |
apercent was calculated out of rows
bof children aged 6 -12 years
*p-value significant at < 0.05
**p-value highly sig at < 0.01
Children aged 3 – < 6 years were the most likely to be at high risk of ASD with the highest prevalence (4.4%) with significantly twice and three quarters more odds than those of the age group 1- < 3 years (COR = 2.7, CI: 2.29–3.34) and one and a half more odds than children aged 6–12 years (COR = 1.46, CI: 1.21–1.52).
Non-school attendance was significantly five times more among children with at high risk of ASD (COR = 5.2, 95% CI: 4.43–6.17) than non-autistic children.
Concerning the odds of having at high risk of ASD among surveyed children according to the maternal and paternal characteristics (Table 3), the age of mothers who gave birth above 35 years was associated with significantly increased odds of ASD than mothers giving birth below 18 years by one and a half-time (COR = 1.57, 95% CI: 1.13–2.18).
Table 3.
Odds of having at high risk of Autism among surveyed children according to the maternal and paternal characteristics
|
maternal and paternal characteristicsa N = 41,640 |
All ASD (n = 1370) n(%) |
Boys (n = 879) n(%) |
Girls n = 491 n(%) |
COR (95% CI) All versus Healthy |
|---|---|---|---|---|
| Mother age at giving birth | ||||
| < 18 (1976) | 50 (2.5) | 38(1.9) | 12(0.6) |
> 35 vs. < 18 1.57(1.13–2.18)* |
| 18 to < 35 (35,958) | 1167 (3.2) | 752(2.1) | 415(1.1) |
18- < 35 vs. < 18 1.29(0.97–1.72) |
| > 35 (3407) | 133 (3.9) | 80(2.9) | 53(1.7) |
18- < 35 vs. > 35 .83(0.69–1.0) |
| No mother (299) | 20 (6.7) | 9(3.0) | 11(3.7) |
No mother vs. mother at home 2.04 (1.29–3.23)** |
| Current Mothers Age | ||||
| < 35 (n = 36,344) | 1179 (3.2) | 761(2.0) | 418(1.2) |
= > 35 vs. < 35 1.08(0.97–1.21) |
| = > 35 (n = 5296) | 191 (3.6) | 118(2.2) | 73(1.4) | |
| Mothers Education | ||||
| 1. Illiterate/ Read & write to Prep (16,046) | 580 (3.6) | 369(2.2) | 211(1.4) |
3 vs. 1 0.66(0.55–0.79)** |
| 2. High School & technical (18,609) | 628 (3.4) | 416(2.2) | 212(1.2) |
2 vs. 1 0.90(0.80–1.01) |
| 3. University or higher (6674) | 142 (2.1) | 85(1.2) | 57(0.9) |
2 vs. 3 1.59(1.32–1.9)* |
| Fathers Education | ||||
| 1. Illiterate/ Read & write to Prep (14,666) | 569 (3.9) | 377(2.6) | 192(1.3) |
3 vs. 1 0.61(0.51–0.72)* |
| 2. High School & technical (18,390) | 569 (3.0) | 367(2.0) | 202(1.0) |
2 vs. 1 0.75(0.67–0.85)* |
| 3. University or higher (6662) | 133 (2.0) | 77(1.2) | 56(0.8) |
2 vs. 3 1.55(1.28–1.8)* |
| 4. No father at home (1922) | 99 (5.2) | 58(3.0) | 41(2.2) |
No Father vs. Father at home 1.61(1.3–1.98)* |
| Mothers´ work | ||||
| 1. Work (paid-unpaid-her own) (n = 6014) | 196 (3.3) | 121 (2.0) | 75 (1.3) |
COR 2 vs 1 1.00(0.86–1.17) |
| 2. Unemployed (35,315) | 1154 (3.3) | 749(2.1) | 405 (1.2) | |
apercent was calculated out of rows
*p-value significant at < 0.05
**p-value highly sig at < 0.01
Children with mothers or fathers who had higher education were less likely to have at high risk of ASD, especially those who had a college or greater education level with a fewer odds of a range from 25 to 39% than lower grades of education. The influence of higher paternal education was higher than that of maternal education. Mothers’ work or current age did not show any association with having at high risk of ASD.
Whereas living without mothers was associated with two times increased odds for at high risk of ASD (COR = 2.04, 95% CI: 1.29–3.23) than living with mothers. Living without fathers carries significantly one and a half odds for at high risk of ASD than the presence of fathers (COR = 1.61, 95% CI: 1.30–1.98).
The odds of having at high risk of ASD among surveyed children according to all the studied medical perinatal history problems were shown in Table 4. All the studied medical histories for both mothers and children were risk factors for at high risk of ASD. The odds for at high risk of ASD are largely affected by the type of medical perinatal history.
Table 4.
Odds of having at high risk of Autism among surveyed children according to the medical perinatal history problems and postnatal child problems
|
Perinatal and postnatal problemsa N = 41,640 |
All ASD (n = 1370) n(%) |
Boys (n = 879) n(%) |
Girls n = 491 n(%) |
COR (95% CI) All versus Healthy |
|---|---|---|---|---|
| Maternal problems | ||||
| Disabled mothers (apparent disability) (n = 373) | 26 (7.0) | 12 (3.1) | 14 (3.9) |
7.77 (5.9–10.1)** |
| Mothers having any health problem during pregnancy (n = 2770) | 215 (7.8) | 140 (5.1) | 75 (2.7) |
2.75 (2.36–3.20) ** |
| Difficult labor (n = 6092) | 309 (5.1) | 195 (3.2) | 114 (1.9) |
1.74 (1.53–1.98) * |
| Perinatal problems | ||||
| Child suffer from any convulsions (n = 675) | 132 (19.6) | 89(13.2) | 43(6.4) |
7.80 (6.40–9.51) ** |
| Child suffer from cyanosis after birth (n = 546) | 91(16.7) | 55(10.1) | 36(6.6) |
6.23 (4.94–7.85) ** |
| Child suffer from meningitis (n = 378) | 49 (13) | 29(7.7) | 20(5.3) |
4.50 (3.32–6.12) ** |
| Twins (n = 1774) | 57 (3.2) | 39 (2.2) | 18(1.0) |
3.75 (3.18–4.41) ** |
| Child born less than 7 months (preterm delivery) (n = 413) | 41 (9.9) | 29 (7.0) | 12 (2.9) |
3.31 (2.39–4.59) ** |
| LBW (less than 2.5 kg at birth) (n = 1848) | 156 (8.4) | 94 (5.1) | 62(3.3) |
2.93 (2.46–3.49) * |
| Child kept in an incubator for more than two days (n = 3078) | 241 (7.8) | 150(4.9) | 91(2.9) |
2.82 (2.44–3.25) * |
| Child suffer from jaundice after birth (n = 11,028) | 524 (4.8) | 343(3.1) | 181(1.7) |
1.76 (1.57–1.96)* |
apercent was calculated out of rows
*p-value significant at < 0.05
**p-value highly sig at < 0.01
Mothers with apparent physical or mental disabilities carried the highest odds for the at high risk of ASD among the other maternal problems (COR = 7.77, 95% CI: 5.9–10.1). Whereas, children with a history of cyanosis after birth (COR = 6.23, 95% CI: 4.94–7.85) or convulsions (COR = 7.8, 95% CI: 6.40–9.51) or had a history of meningitis after birth (COR = 4.50, 95% CI: 3.32–6.12) were the most of postnatal child problems for carrying the highest odds for the at high risk of ASD than being a healthy child.
The odds of presenting features of Autism among surveyed children according to sex were shown in Table 5. Three presenting features of Autism were significantly observed to be higher among boys with at high risk of ASD than among girls. Behavioral/Emotional expression problems were significantly two times higher among boys with at high risk of ASD than among girls with at high risk of ASD (COR = 1.96, CI: 1.32–2.91). Whereas, Reduced peer interaction and insistence of children to play with the same thing the same way were significantly more than one and a half times higher among boys with at high risk of ASD than among girls with at high risk of ASD (COR = 1.64, CI: 1.22–2.21 & COR = 1.61, CI: 1.17- 2.19). The odds of having poor to limited comprehension/Limited language/nonverbal, speech difficulties, learning, and academic performance difficulties were insignificantly higher among boys than girls.
Table 5.
Odds of presenting features of Autism among surveyed children according to sex
| Presenting features of Autisma |
All ASD (n = 1370) n(%) |
Boys (n = 879) n(%) |
Girls n = 491 n(%) |
COR (95% CI) between boys and girls |
|---|---|---|---|---|
|
Child does not usually express joy when seeing parents (Behavioral/Emotional expression problems) (n = 257) |
150 (58.4) | 115 (44.7) | 35 (13.7) | 1.96 (1.32–2.91)** |
|
Child does not play with mates and do not socialize (Reduced peer interaction) (n = 450) |
262 (58.2) | 191 (42.4) | 71 (15.8) | 1.64 (1.22–2.21)** |
|
Child insists to play with the same thing the same way (n = 431) |
238 (55.2) | 173 (40.1) | 65 (15.1) | 1.61 (1.17- 2.19)** |
|
Child is beyond his/her mates in comprehension (Poor to limited comprehension/Limited language/nonverbal) (n = 886) |
379 (42.8) | 252 (28.4) | 127 (14.4) | 1.15 (0.89–1.48) |
|
Child is beyond his/her mates in speech (Speech Difficulties) (n = 1627) |
671 (42.0) | 455 (28.0) | 216 (14.0) | 1.37 (0.31–1.71) |
|
Child is beyond mates in school (if he/she is in school)b (learning and academic performance difficulties) (n = 544) |
149 (27.4) | 101 (18.6) | 48 (8.8) | 1.9 (0.83–1.72) |
apercent was calculated out of rows
bcalculated out of school aged children (6–12 years)
**p-value highly sig at < 0.01
Twenty four significant variables associated with children who screened + ve for at high risk of ASD versus those who screened negative of the healthy population were entered into a multivariate logistic regression using the enter selection procedure (Table 6). The odds of being at high risk of autism increased significantly with being males by almost one and three-quarters times that being females (AOR = 1.70, 95%, CI:1.51–1.92).
Table 6.
Multivariate Logistic regression model for predictor ASD
| Parameters | Screen + ve ASD total Vs. Screen -ve ASD total | ||
|---|---|---|---|
| Wald | OR | CI | |
| Age | .051 | 1.00 | 0.98- 1.02 |
| Sex | 75.95 | 1.70 | 1.51–1.92* |
| No of households | 2.51 | 0.95 | 0.89- 1.01 |
| Locality (rural) | 4.902 | 0.84 | 0.73–0.98* |
| Social level (Middle Vs. Low) | 5.708 | 1.76 | 1.52–2.03* |
| Social level (High to low) | 58.10 | 1.20 | 1.03–1.40* |
| Residency (Lower to cities) | 68.38 | 0.47 | 0.39–0.56* |
| Residency (Upper to cities) | 1.87 | 0.98 | 0.96–1.08 |
| Residency (Frontiers to cities) | 46.94 | 0.46 | 0.35–0.56* |
| Maternal age at birth | .080 | 1.00 | 0.99–1.01 |
| Maternal University and above to less | 10.54 | 0.66 | 0.52–0.85* |
| Paternal University and above to less | 13.37 | 0.64 | 0.51–0.82* |
| School attending status (not)a | 4.43 | 1.22 | 0.92–1.28 |
| Maternal work status (working) | 1.31 | 0.90 | 0.75–1.08 |
| Mothers have any health problems during pregnancy | 34.74 | 1.74 | 1.45 – 2.10* |
| Difficult labor | 6.96 | 1.24 | 1.06–1.45* |
| Disabled mothers | 4.78 | 1.35 | 0.92–1.50 |
| Less than 7 months (preterm delivery) | 1.90 | 0.89 | 0.98–1.94 |
| LBW (less than 2.5 kg at birth) | 14.80 | 1.53 | 1.23–1.89* |
| Children suffer from jaundice after birth | 7.26 | 1.20 | 1.05–1.37* |
| Children suffer from cyanosis after birth | 14.38 | 1.87 | 1.35–2.59* |
| Children suffer from any convulsions | 89.01 | 3.67 | 2.80- 4.80* |
| Children kept in an incubator for more than two days | 16.62 | 1.47 | 1.22–1.76* |
| Child suffer from meningitis | .223 | 0.9 | 0.58–1.40 |
| Constant | 138.96 | 0.043 | |
*p-value significant at < 0.05
**p-value highly sig at < 0.01
aof children aged 6 -12 years
The neonatal problems related predictors for at high risk of ASD in order were: Children with a history of any convulsions increased the odds of autism by almost four times compared to those not having convulsions (AOR = 3.67; 95% CI: 2.8–4.8), children with a history of cyanosis after birth (AOR = 1.87; 95% CI: 1.35–2.59), history of LBW babies (AOR = 1.53; 95% CI: 1.23–1.89). Children kept in an incubator for more than two days (AOR = 1.47; 95% CI: 1.22–1.76) were associated with increased odds of being at high risk of autism by nearly one and a half times compared to healthy and full-term born children.
Maternal predictors were having either a history of health problems during pregnancy or a history of difficult labor. They increased the odds to be at high risk of autism by one and half times compared to healthy mothers (AOR = 1.74; 95%, CI: 1.45–2.10 & AOR = 1.74; 95%, CI:1.45–2.10). Maternal factors are not age-specific predictors.
The protective factors that decrease the odds to be at high risk of autism included: being resident in a rural locality with a decrease in the odds to be at high risk of autism by 15% compared to being resident in urban communities (AOR = 0.84, 95%, CI: 0.73 – 0.98), maternal and paternal education with university or above degree decrease the odds to be at high risk of autism by approximately 40% compared of being with less degree of education (AOR = 0.66, 95%, CI: 0.52 – 0.85 & AOR = 0.64, 95%, CI: 0.51– 0.82 respectively). Being resident in frontiers or in Lower Egypt decreases the odds of being at high risk of autism by almost 50% compared to being resident in cities (AOR = 1.5, 95%, CI: 1.09 – 2.06).
Discussion
ASD is a complex developmental disorder that causes a burden to affected children and their families. Early detection and intervention lead to a better prognosis with decreased psychological and economic burdens on the families and society. According to Leo Kanner, the first prevalence estimate of ASD was reported in 1966 to be 4.5 per 10,000 people among children aged 8 to 10 in the United States [51]. Meanwhile, there is a consensus perception about the increase in ASD prevalence worldwide over the last decade. This perception may be attributed to the increased public awareness and better diagnostic services [4], earlier autism diagnosis, and/ or the discovery of therapeutic targets [88]. Accordingly, the current study focused on screening to detect the at high risk of autism with their risk factors. This step is important at the primary health care level to detect suspicious cases for early management. The current study was both a community and facility-based screening study for detecting children at high risk for ASD and determining the risk factors among 41,640 children aged 1–12 years.
There is a growing increase in ASD prevalence worldwide. However, the prevalence is variable in different countries; in the USA, 1 in 59 children had ASD [12] and in the UK, the prevalence of ASD was 1.1% [102]. Few researchers have looked at the national prevalence of ASD among Arab countries as estimated by a recent systematic scoping review [2] with the reported lesser prevalence of ASD than that reported among the developed countries. In Arab countries, it is reported that there is a wide range in prevalence of ASD from 0.014 to 4.7% [2]. The estimate was 2.9 per 1000 in the United Arab Emirates [102], 1.4 per 10,000 in Oman, 4.3 per 10,000 in Bahrain, and 1/167 in Saudi Arabia [5, 81]. The estimated variations in ASD prevalence between countries were mainly attributed to the methodological tools used for the autism diagnosis. It is well known that the confirmation of ASD diagnosis is usually done by specialized clinicians using both DSM5 (Diagnostic and Statistical Manual of Mental Disorders (DSM-5), [23] and CARS [84]. Accordingly, the terminology used for defining autism prevalence should be very precise according to the used tool for diagnosis. Another contributing factor to the detected variation was the targeted age group differences between studies as well as the level at which the study was conducted; whether at the community or facility level.
Few studies were done in Egypt to detect either the prevalence of the at high risk of Autism or ASD confirmed cases; mostly clinic-based, typically with small sample sizes, and were not representative of the whole country. Although ASD is frequently underdiagnosed or misdiagnosed in Egypt [2], existing studies were suggestive that ASD is a prevalent disorder in Egypt. The majority of prevalence studies in Egypt included samples from specialized units or hospitals and were related to the confined age group as a target group. The main objective of the current study was reporting the real situation of children at high risk of ASD as a national screening estimate through two screening phases. The first phase was a community-based one through using Vineland Adaptive Behavior Scales to detect children suspicious for autism. The second screening phase was a facility-based for reporting the prevalence of the high risk of ASD among the referred suspicious children aged 1–12 years using the M-CHAT for children aged 1–3 years, GARS-2 for children 3–12 years. In addition, Denver II Developmental screening test for children up to 6 years was used to confirm developmental delay detected in phase I screening and documenting possible developmental regression that is affected because of autism. The current study estimated the prevalence of the at high risk for autism to be 3.3% (95% CI: 3.1%–3.5%). This estimate was in accordance with two facility-based Egyptian studies. The first study investigated 500 children aged from 3 to 12 years in one Egyptian governorate according to GARS-2 and showed the prevalence of ASD to be 3.4% [11]. The other Egyptian screening study was done in kindergartens on 3722 preschool children and estimated that 2.8% of children were at high risk for ASD according to Modified Check List for Toddlers/Revised (M-CHAT-R) [102].
The current study reported that the highest prevalence was for the age group 5- < 6 years (6.4%, 95% CI: 5.7%–7.2%) followed by age group 6- < 7 years (5.7%, 95% CI: 5.0%–6.5%). The study revealed also that children aged 3 – < 6 years were the most likely to be diagnosed with ASD (4.4%). This was in accordance with another study which found that the most common age of presentation was between 2–5 years of age [103]. This finding supports the crucial recommendation for the early detection of ASD in preschool children [49, 54]. Unfortunately, the majority of children with ASD do not obtain a diagnosis until they reach school age. The fact that many physicians- especially in rural communities- have insufficient awareness of the diagnosis of ASD resulted in a delay in referral of the at-risk children to ASD specialists, another reason was the lack of awareness of mothers about the developmental milestones until their children reach school age [86]. This values the importance of screening at the community level to provide a real situation for ASD problems.
The present study's finding of having that ASD among boys was one and three-quarters times more than that of girls in the age range 1–12 years (OR 1.72, 95% CI: 1.53%–1.92%) was in parallel with many studies that revealed a higher frequency of ASD among males than females with a ratio of 2:1 [3], 3:1 [11, 51], or 4:1 [50, 67]. Results of different studies have been contradictory. When screening the entire population using gold standard assessments, current estimates suggest around 3 males receive an autism diagnosis for every female. However, in clinical samples who have already received an autism diagnosis, that ratio is higher at over four males to each female [50]. In individuals with intellectual disability, the ratio is closer to 2:1 [101].
One of the first signs of ASD is delayed speech. However, the presence of speech before the age of five is the most powerful predictor of better improvement of ASD symptoms [69]. The odds of having speech difficulties, learning, and academic performance difficulties were insignificantly higher among boys than girls in the current study (COR = 1.37, CI: 0.31–1.71). Our results reported three presenting features of autism to be significantly higher among the at-risk boys than among the at-risk girls for ASD. Behavioral and emotional expression problems were significantly associated with nearly two times higher odds of ASD risk among boys than among girls (COR = 1.96, CI: 1.32–2.91). Whereas, reduced peer interaction and insistence of children to play with the same thing the same way carried significantly more than one and a half times higher odds among boys than among girls with at risk of ASD (COR = 1.64, CI: 1.22–2.21 & COR = 1.61, CI: 1.17- 2.19). Our study comes in agreement with Yousef and his colleagues [102] who reported behavioral disturbance, significant developmental and speech delay among ASD patients, also with another Egyptian study that was done by El-Baz and his colleagues who proved that ASD is associated with developmental delay, speech defect, psychological disorders, and intellectual and learning disabilities [28, 40, 45, 102]. Alshaban and his coworkers [8] reported that 75.1% of children with ASD had language delays for words, 91.4% for phrase speaking, and 19.4% had developmental regression. They also reported that 19.4% of children had persistent deficiencies in expressive language and 14.0% in peer interactions.
There have been not enough evaluations on sex differences by ASD end phenotypes to date. However, some researchers reported that males with ASD are more likely than females to suffer from repetitive behaviors and have limited interests [17, 39, 78]. The odds of having poor to limited comprehension or limited language or nonverbal difficulties were insignificantly higher among boys than girls in the present study. This finding was also similar to other researchers who found no significant differences between males and females with ASD in communication, comprehension difficulties, or language skills [71, 89, 91].
ASD risk factors have yet to be properly defined [102]. The current study identified the determinants of children who were at high risk for ASD that are related to socio-demographic, epidemiological, maternal, and child health status. Cultural aspects of ASD remain understudied. Saudi Arabia and Lebanon provided the majority of the studies and declared no association between ASD and socioeconomic status [25, 32]. Investigating the association between parental socioeconomic status and risk of ASD is important to be clarified as it could provide insight into the etiology of ASDs, which is still largely not understood [75]. Some investigators have found a strong link between ASD and urbanity (i.e., a higher risk of autism in urban than rural districts) [48, 77, 98]. Our results revealed the same and reported that living in Lower Egypt or in Frontiers significantly decreased the odds at risk of ASD than living in urban cities by more than 60% (OR = 0.39, CI: 0.34–0.44 & OR = 0.36, CI: 0.29–0.45 respectively). Moreover, the at-risk of ASD was significantly higher among the middle class than in both the high and low classes (OR 1.53, 95% CI: 1.34–1.73 & OR 1.72, 95% CI: 1.51–1.97 respectively). Many studies implicated the role of the socioeconomic status of parents in the early diagnosis of ASD as a low socioeconomic class may delay taking medical advice and this could lead to the child not being probably diagnosed [53, 54]. However, in the current study the association between the middle class and the risk of ASD could be attributed to the lack of functional role of the parents especially mothers. The majority of mothers belonging to the middle class are working for a long time, seldom communicating with their children (play, talk or teach things) being overwhelmed by the home duties, besides their limited awareness about children's developmental milestones. Most of children belonging to the middle class have been constrained for screens for prolonged periods of time. A recent study showed that longer durations of screen time among 1-year-old boys was significantly associated with ASD at 3 years old [47]. On the other hand, women belonging to the low social class leave their children to play outside the home with their peers or mates which had a positive impact on the improvement of their cognitive and social skills. Whereas, children belonging to the high class often regularly attend a preschool education program that enhances children's communication skills.
Systematic review studies revealed that advanced paternal and maternal age has been associated with the risk for autism [52, 55, 74].
When looking at the odds of having ASD, mothers who were over 35 years old at the time of birth carried one-and-a-half- higher odds of risk for ASD compared to mothers who were under 18 years old (OR = 1.57, 95 percent CI: 1.13–2.18) in the current study.
The present study revealed that children with mothers or fathers who had higher education were less likely to be associated with a risk of ASD, especially those who had a college or greater education level with a fewer odds of a ranging from 25 to 39% than lower grades of education indicating that education serves as a protective factor. This could be supported by many Egyptian studies which concluded that awareness of the mothers regarding developmental milestones [27, 64, 79] and their children feeding practices [61] increased with the attainment of maternal education.
Unfortunately, this finding was in contrast with other Egyptian studies for which the majority of ASD children's moms were university graduates [29, 102], A Saudi Arabian study discovered also a high educational level of ASD children's moms [9]. Such variability in the mentioned studies could be attributed to the selection criteria with the exclusion of illiterate parents and those of a low education level from participating due to their negligence in filling the checklist questionnaire. These studies declared their selection as one of their studies’ limitations.
Until now no obvious causes for ASD could be fully understood, no single factor is responsible for the development of ASD but some multifactorial determinants seem to operate in the development of this disorder. On looking up predictors of the at high risk for ASD, prenatal and postnatal insults showed a significant impact. Children with a history of convulsions were associated with increased odds of being at high risk for autism by almost four times compared to those not having convulsions (AOR = 3.67; 95% CI: 2.8–4.8). It has been estimated that between 15 to 47% of people with ASD have epilepsy in early childhood [46].
Meanwhile, children with a history of cyanosis after birth or with a history of LBW or those who were kept in an incubator for more than two days or with a history of LBW babies were associated with increased odds to be at high risk for ASD by nearly one and a half times compared to healthy and full-term born children. The history of maternal health problems during pregnancy or difficult labor was associated with increased odds to be at high risk of ASD by one and half times compared to healthy mothers (AOR = 1.74; 95%, CI:1.45–2.10 & AOR = 1.74; 95%, CI:1.45–2.10). This finding supports other studies that affirmed the significant implication of perinatal insults for the development of ASD [11, 14]. Our study supports the recommendation that policymakers have to be concerned with the provision of services mainly during the perinatal period. In Egypt, community and health facilities based interventions had a great impact on reducing maternal and neonatal adverse outcomes [65, 58].
Strengths
Our study has some important strengths. To the best of our knowledge, this study is considered to be the first study to investigate the prevalence and predictors for children who are at high risk of ASD at a national level with a very large sample size of Egyptian children aged 1–12 years and as a representative to Egypt. Accordingly, we could make it easy to generalize our findings. The use of two phases for screening using reliable screening tools is a strength. Our study also was the first that determined sex-specific estimates and predictors of ASD.
Limitations
The lack of studying the environmental variability in the demographic status of the participating children is a weakness of this study. Environmental factors such as industrially emitted heavy metals, chemicals, bacterial, and viral infections may all play a role in ASD. The documented impact of environmental education and awareness-raising at the community level in Egypt in having a profound effect on knowledge attainment was proved [62, 63]. Out of limitation was studying the influence of childhood malnutrition which may be risk factors for ASD, especially the impact of school feeding programs on improving children’s growth and development was documented also in Egypt [60, 80]. The last-mentioned two factors are limited to be investigated during screening studies because of the long time required for filling the related questionnaires.
Conclusion and recommendation
In this paper, we focused on the whole community to determine the prevalence of children who are at high risk of ASD among 41,640 children aged 1 to 12 years in Egypt through community-based national screening. This study was conducted among 8 Governorates representing all geographic regions of Egypt. The survey highlighted the most important contribution to the need for community-driven data to detect the risk and the protective determinants of ASD in general and among sex which when neglected can lead to a severe degree of ASD that could impact not only the life of the children but the whole family. Most of the detected determinants were preventable factors indicating that the educational and rehabilitation fields are far beyond the medical ones. Thus identifying the prevalence and the risk factors for the high risk of ASD is a step toward implementing surveillance for the at-risk of autism which is drastically needed for creating awareness among health care workers and caregivers. Neglecting to study the extent of the problem of the spread of autism makes more burdens on the families and the governments and helps in increasing the rate of disabilities.
The study findings necessitate prompt actions of local health and educational systems to be appropriately equipped to support affected children and their families optimally. Local health units should be provided with multidisciplinary teams including developmental and behavioral pediatrician, psychiatrist, psychologist, speech therapist, physiotherapist and social worker for early detection, proper diagnosis and management of these children. In addition, efforts must be taken to reduce the uncertainty around the proper estimates of this lifelong disorder. These efforts may include; screening of all children for ASD at ages 9, 18 and 24 months, along with regular developmental surveillance during vaccination visits, screening of preschool and school age children for ASD on admission to kindergarten and primary schools and consistent courses for primary physicians, school teachers, and kindergarten supervisors about early warning signs of ASD.
Supplementary Information
Additional file 1: S Table-1. (List of the targeted Households (HH) according to the governorates, locality and sociodemographic status for screening of at high risk autism among children aged 1-12 years).
Additional file 2: S Table-2. Raw data (XLSX) that are anonymous.
Acknowledgements
The authors express their deep appreciation to the Ministry of Health and Population’s (MOHP) staff who contributed to the provision of the consultation to referred cases with developmental disabilities. Special thanks to all caregivers and, parents in their communities, who gave their time and provided valuable information to make the implementation of the current study possible.
Abbreviations
- AOR
Adjusted Odds Ratio
- ASD
Autism Spectrum Disorder
- CAPMS
Central Agency for Public Mobilization and Statistics
- CARS
The Childhood Autism Rating Scale
- CDC
Centers for Disease Control and Prevention
- CI
Confidence Interval
- COR
Crude Odds Ratio
- DDs
Developmental delays
- DDST
Denver II Developmental Screening Test
- DSM-5
Diagnostic and Statistical Manual of Mental Disorders (5th edition)
- ERF
Economic Research Forum
- GARS-2
Gilliam Autism Rating Scale
- LBW
Low Birth Weight
- M-CHAT-R/F
Modified Checklist for Autism in Toddlers-Revised
- MOHP
Ministry of Health and Population
- NRC
National Research Centre of Egypt
- SD
Standard Deviation
- SPSS
Statistical Package for the Social Sciences
- UK
United Kingdom
- USA
United States of America
- VABSA
Arabic version of Vineland Adaptive Behavior Scales
- WHO
World Health Organization
Authors’ contributions
Conceptualization: AMM, EMS and ERA; Data curation: RMS, AE, MME, DAN,MAS, IRE, HME, SIS, TMR, GAA, LAE, DME, SMS, NAI and EAA; Formal analysis: MAH, RMS, AMAand EE; Funding Acquisition: AMM and ZK; Investigation: RMS, AE, MME, DAN, MAS, IRE, HME, SIS, TMR, GAA, LAE, DME, SMS NAI and EAA; Methodology: AMM, MAH, EMS,ERA,AMA, ZK, HME, NAE, HYB and EMD; Project Administration: AMM, AMA, ZK, NAE, HYB and EMD; Resources: AMM, ZK, and HYB; Software: AMM, MAH, EMS, RMS, AMA, ZK,HMEand EE; Supervision: AMM, EMS, AMA, ERA, RIB, SMS, NAI, NAE, HYB and EMD; Validation: MAH, AMA, ZK, HME, SIS, TMR, GAA, LAE, DMEand EE; Visualization: RMS, DAN, AE, MME, MAS, IRE, HME, SIS, TMR, GAA, LAE, DME, SMS, NAI and EAA, Writing – original draft: EAA and RMS; Writing – review & editing: AMM and EMS. All authors read and approved the final manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This study was conducted through a project titled “National Prevalence Survey for Autism Spectrum Disorders (ASD): Assessing its Epidemiological Pattern and Risk Factors” under the leadership of Prof. Ammal Mokhtar Metwally and Prof. Zeinab Khader (Principal Investigators). The project was supported financially by Academy of Scientific Research and Technology (Egypt), project ID Number”13893″. The funder had no role in the design of the study, collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and analyzed during the current study are anonymous and are fully available without restriction as S Table-2 Raw data (XLSX).
Declarations
Ethics approval and consent to participate
The study was approved by the Ministry of Health and Population (MOHP) and the Medical Research Ethics Committee of the National Research Centre with an ethical registration approved number: 17034. Written informed consent was taken from the parents or guardians of all children enrolled in the study (mothers/or fathers/ or any caregivers). A right thumbprint was used as a signature for participants who were unable to write. For any caregivers under the age of 18, parental or legal guardian consent was obtained. The study was fully voluntary. Participants were well informed about their rights to withdraw at any time. Data was collected in a confidential manner, and it was de-identified, de-linked, and stored in a safe location. The conduct of the study complied with the International Ethical Guidelines for Biomedical Research Involving Human Subjects [21], and that information disclosure “Making sure patients understand” was guaranteed according to the recommendations of the Egyptian patients and guardians’ perception about clinical informed consent as a preferred purpose for IC practices [59].
Consent for publication
Non applicable.
Competing interests
All authors report no conflict of interest. “No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ammal M. Metwally, Email: ammal_mok@yahoo.com
Mona A. Helmy, Email: drmonaadel81@gmail.com
Ebtissam M. Salah El-Din, Email: ebtissam2006@yahoo.com
Rehan M. Saleh, Email: rehansaleh@yahoo.com
Ehab R. Abdel Raouf, Email: ehabragaa@gmail.com
Ali M. Abdallah, Email: a.abdallah@aswu.edu.eg
Zeinab Khadr, Email: zeinabk@aucegypt.edu.
Amal Elsaied, Email: omar_elsaeid_amal@yahoo.com.
Mostafa M. El-Saied, Email: mostafa_gaballah2000@yahoo.com
Randa I. Bassiouni, Email: randabass@hotmail.com
Dina A. Nagi, Email: dinanagi@live.com
Manal A. Shehata, Email: dr_manalabdelkader@hotmail.com
Inas R. El-Alameey, Email: inasno@hotmail.com
Hazem M. El-Hariri, Email: dochzm@gmail.com
Somia I. Salama, Email: somaia2721199@hotmail.com
Thanaa M. Rabah, Email: thanarabah@yahoo.com
Ghada A. Abdel-Latif, Email: dr.ghada237@gmail.com
Lobna A. El Etreby, Email: lobnaeletreby@hotmail.com
Dalia M. Elmosalami, Email: dodacambo@yahoo.com
Samia M. Sami, Email: samosam1190@yahoo.com
Eman Eltahlawy, Email: eman.eltahlawy@gmail.com.
Nihad A. Ibrahim, Email: nihad_amer@yahoo.com
Nahed A. Elghareeb, Email: elghareebnahed2016@gmail.com
Hala Y. Badawy, Email: badawihala29@gmail.com
Eman M. Dewdar, Email: emandewdar7@gmail.com
Engy A. Ashaat, Email: nogy80@hotmail.com
References
- 1.Afifi M. Mental health publications from the Arab world cited in PubMed. East Mediterr Health J. 2015;11(3):319–328. [PubMed] [Google Scholar]
- 2.Alallawi B, Hastings P, Gray G. A systematic scoping review of social, educational, and psychological research on individuals with autism spectrum disorder and their family members in Arab countries and cultures. Rev J Autism Dev Disord. 2020;7:364–382. doi: 10.1007/s40489-020-00198-8. [DOI] [Google Scholar]
- 3.Al-Farsi YM, Al-Sharbati MM, Al-Farsi OA, Al-Shafaee MS, Brooks DR, Waly MI. Brief report: prevalence of autistic spectrum disorders in the sultanate of Oman. J Autism Dev Disord. 2010;41(6):821–825. doi: 10.1007/s10803-010-1094-8. [DOI] [PubMed] [Google Scholar]
- 4.Al-Mamri W, Idris A, Dakak S, Al-Shekaili M, Al-Harthi Z, Alnaamani A, Alhinai F, Jalees S, Al Hatmi M, El-Naggari M, Islam M. Revisiting the prevalence of autism spectrum disorder among Omani children: a multicentre study. Sultan Qaboos University Medical Journal. 2019;19(4):e305–e309. doi: 10.18295/squmj.2019.19.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Almandil N, Alkuroud D, AbdulAzeez S, AlSulaiman A, Elaissari A, Borgio J. Environmental and genetic factors in autism spectrum disorders: special emphasis on data from Arabian studies. Int J Environ Res Public Health. 2019;16:E658. doi: 10.3390/ijerph16040658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alotibi, B. (2004). The Vineland Adaptive Behavior Scales – The Saudi version. Arabian Journal of Special Education, 5.
- 7.Al-Salehi SM, Al-Hifthy EH, Ghaziuddin M. Autism in Saudi Arabia: Presentation, clinical correlates and comorbidity. Transculture Psychiatry. 2009;46:340–347. doi: 10.1177/1363461509105823. [DOI] [PubMed] [Google Scholar]
- 8.Alshaban F, Aldosari M, Al-Shammari H, El-Hag S, Ghazal I, Tolefat M, &, , et al. Prevalence and correlates of autism spectrum disorder in Qatar: a national study. J Child Psychol Psychiatry. 2019;60(12):1254–1268. doi: 10.1111/jcpp.13066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alsulaimani A, Helmy F, Abdel Wahab M. Risk factors of autism: a Saudia study. Inernational Journal of Science and Research. 2014;3(10):1200–1210. [Google Scholar]
- 10.Assad, R. &Krafft, C. (2012). The structure and evolution of employment in Egypt“1998–2012”, Economic Research Forum (ERF) – working paper 805, Egypt. 10.1093/acprof:oso/9780198737254.003.0002
- 11.Auf K, Al-Nagar E, Al-Gendy R, Abd El-Raouf E. Screening of autism spectrum disorder by using Gilliam autism rating scale in a sample of Egyptian children attending Bab Al Shareya University Hospital. AL-Azhar J Pediatrics. 2020;23(4):1259–1277. [Google Scholar]
- 12.Baio J, Wiggins L, Christensen D, Maenner M, Daniels J, Warren Z, &, , et al. Prevalence of at risk autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 Sites, United States. Mmwr Surveillance Summaries Journal. 2018;67:1–23. doi: 10.15585/mmwr.ss6706a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boatin AA, Eckert LO, Boulvain M, Grotegut C, Fisher BM, King J, Berg M, Adanu R, Reddy U, Waugh J, Gupta M, Kochhar S, Kenyon S, Brighton Collaboration Dysfunctional Labor Working Group. Electronic address: contact@brightoncollaboration.org Dysfunctional labor: Case definition & guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine. 2017;35(4):6538–6545. doi: 10.1016/j.vaccine.2017.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bölte S, Girdler S, Marschik P. The contribution of environmental exposure to the etiology of autism spectrum disorder. Celullular and Molecular Life Sciences. 2019;76(7):1275–1297. doi: 10.1007/s00018-018-2988-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown KA, Parikh S, Patel DR. Understanding basic concepts of developmental diagnosis in children. Translational Pediatrics. 2020;9(S1):S9–S22. doi: 10.21037/tp.2019.11.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cadman D, Chambers LW, Walter SD, Feldman W, Smith K, Ferguson R. The usefulness of the Denver Developmental Screening Test to predict kindergarten problems in a general community population. Am J Public Health. 1984;74(10):1093–1097. doi: 10.2105/AJPH.74.10.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carter AS, Black DO, Tewani S, Connolly CE, Kadlec MB, Tager-Flusberg H. Sex differences in toddlers with autism spectrum disorders. J Autism Dev Disord. 2007;37(1):86–97. doi: 10.1007/s10803-006-0331-7. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention (2015). Pregnancy complications. Available at http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregcomplications.htm
- 19.Centers for Disease Control and Prevention . Data and statistics on autism spectrum disorder. Atlanta, Georgia, United States: Center for Disease Control and Prevention, 2020; 2020. [Google Scholar]
- 20.Central Agency for Public Mobilization and Statistics (CAPMS) (2017). http//www.capmas.gov.eg.
- 21.Council for International Organizations of Medical Science (CIOMS)–A nongovernmental organization in official relations with WHO . International Ethical Guidelines for Biomedical Research Involving Human Subjects. Geneva: CIOMS; 2016. p. 2016. [Google Scholar]
- 22.David SI. Treatment of aggression in adults with autism spectrum disorder: a review. Harv Rev Psychiatry. 2021;29(1):35–80. doi: 10.1097/HRP.0000000000000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diagnostic and Statistical Manual of Mental Disorders (DSM-5) Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association (APA), 2013; 2013. [Google Scholar]
- 24.Durkin MS, Davidson LL, Desai P, Hasan ZM, Khan N, Shrout PE, &, , et al. Validity of the ten questions screened for childhood disability: results from population-based studies in Bangladesh, Jamaica, and Pakistan. Epidemiology. 1994;5(3):283–289. doi: 10.1097/00001648-199405000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Eapen V, Mabrouk A, Zoubeidi T, Yunis F. Prevalence of pervasive developmental disorders in preschool children in the UAE. J Trop Pediatr. 2007;53(3):202–205. doi: 10.1093/tropej/fml091. [DOI] [PubMed] [Google Scholar]
- 26.Economic Research Forum (ERF) and CAPMAS . “Egypt Labor Market Panel Survey (ELMPS) of 2012”, Egypt. 2012. [Google Scholar]
- 27.El Din EMS, Rabah TM, Metwally AM, Nassar MS, Elabd MA, Shalaan A, Kandeel W, El Etreby LA, Shaaban SY. Potential risk factors of developmental cognitive delay in the first two years of life. Open Access Macedonian Journal of Medical Sciences. 2019;7(12):2024–2030. doi: 10.3889/oamjms.2019.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.El-Baz F, Ismael N, el-Din S. Risk factors for autism: An Egyptian study. The Egyptian Journal of Medical Human Genetic. 2011;12(1):31–38. doi: 10.1016/j.ejmhg.2011.02.011. [DOI] [Google Scholar]
- 29.Elwardany S, Ibrahim H, Askar G, Bayomi S. Risk factors for autistic spectrum disorders at Assiut City. J Educ Pract. 2013;4(28):14757. [Google Scholar]
- 30.Farmer, C.A., Swineford, L., Swedo, S.E. & Thurm, A. (2018). Classifying and characterizing the developmental and adaptive behavior in a naturalistic longitudinal study of young children with autism. Journal of neurodevelopmental disorders, 10(1). 10.1186/s11689-017-9222-9. [DOI] [PMC free article] [PubMed]
- 31.Filmer, D. & Pritchett, L. (2001). Estimating wealth effects without expenditure data- or tears: An application to educational enrollment in states of India. Demography, 38(1), 15–132. Retrieved from http://www.Jstor.org/stable/3088292. [DOI] [PubMed]
- 32.Fombonne E, Du Mazaubrun C, Cans C, Grandjean H. Autism and associated medical disorders in a French epidemiological survey. J Am Acad Child Adolesc Psychiatry. 1997;36:1561–1569. doi: 10.1016/S0890-8567(09)66566-7. [DOI] [PubMed] [Google Scholar]
- 33.Frankenburg WK, Dodds J, Archer P, Shapiro H, Bresnick B. The Denver II: A major revision and restandardization of the Denver developmental screening test. Pediatrics. 1992;89:91–97. doi: 10.1542/peds.89.1.91. [DOI] [PubMed] [Google Scholar]
- 34.Gilham JE, Carter AS, Volkmar FR, Sparrow SS. Toward a developmental operational definition of autism. J Autism Dev Disord. 2000;30:269–278. doi: 10.1023/A:1005571115268. [DOI] [PubMed] [Google Scholar]
- 35.Gilliam J. GARS-2: Gilliam Autism Rating Scale-Second Edition. PRO-ED: Austin; 2006. [Google Scholar]
- 36.Glascoe FP, Byrne KE, Ashford LG, Johnson KL, Chang B, Strickland B. Accuracy of the Denver II in developmental screening. Pediatrics. 1992;89:1221–1225. doi: 10.1542/peds.89.6.1221. [DOI] [PubMed] [Google Scholar]
- 37.Guinchat V, Thorsen P, Laurent C, Cans C, Bodeau N, Cohen D. Pre-, peri- and neonatal risk factors for autism were identified and included in the survey Pre-, peri- and neonatal risk factors for autism. Acta Obstetricia and Gynecologica Scandinavica. 2012;91(3):287–300. doi: 10.1111/j.1600-0412.2011.01325.x. [DOI] [PubMed] [Google Scholar]
- 38.Hansen, R. (2013). Denver Development Screening Test (DDST). In: Volkmar, F.R. (eds) Encyclopedia of Autism Spectrum Disorders. Springer, New York. 10.1007/978-1-4419-1698-3_613
- 39.Hattier MA, Matson JL, Tureck K, Horovitz M. The effects of gender and age on repetitive and/or restricted behaviors and interests in adults with autism spectrum disorders and intellectual disability. Res Dev Disabil. 2011;32(6):2346–2351. doi: 10.1016/j.ridd.2011.07.028. [DOI] [PubMed] [Google Scholar]
- 40.Herbert MR, Harris GJ, Adrien KT, Zeigler DA, Markis N, Kennedy DN, &, , et al. Abnormal asymmetry in language association cortex in autism. Ann Neurol. 2002;52(5):588–596. doi: 10.1002/ana.10349. [DOI] [PubMed] [Google Scholar]
- 41.Hussein H, Taha G. Autism spectrum disorders. Middle East Current Psychiatry. 2013;20(3):106–116. doi: 10.1097/01.XME.0000430433.49160.a4. [DOI] [Google Scholar]
- 42.Icabone, D.G. (1999). Vineland Adaptive Behavior Scales. Assessment for Effective Intervention, 24(1–4). 10.1177/153450849902401-423.
- 43.Ismail, S., Abo Senna, A., Behiry, E., Ashaat, E., Zaki, M., Ashaat, N. & Salah, D. (2019). Study of C677T variant of methylene tetrahydrofolatereductase gene in autistic spectrum disorder Egyptian children. American Journal of Medical Genetics, 1–5. [DOI] [PubMed]
- 44.Jones SR, Carley S, Harrison M. An introduction to power and sample size estimation. Emergency Medical Journal. 2003;20:453–458. doi: 10.1136/emj.20.5.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kinnear, D., Rydzewska, E., Dunn, K., Hughes McCormack, L, Melville, C., Henderson, A. & Cooper, S. (2020). The relative influence of intellectual disabilities and autism on sensory impairments and physical disability: A whole country cohort of 5.3 million children and adults. Journal of Applied Research in Intellectual Disabilities, 33(5), 1059–1068. 10.1111/jar.12728, PMCID:PMC8641374. [DOI] [PMC free article] [PubMed]
- 46.Ko C, Kim N, Kim E, Song D, Cheon K. The effect of epilepsy on autistic symptom severity assessed by the social responsiveness scale in children with autism spectrum disorder. Behav Brain Functions. 2016;12(20):1–9. doi: 10.1186/s12993-016-0105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kushima M, Kojima R, Shinohara R, Horiuchi S, Otawa S, Ooka T, et al. Association between screen time exposure in children at 1 year of age and autism spectrum disorder at 3 years of age: the Japan environment and children's study. JAMA Pediatr. 2022;176(4):384–391. doi: 10.1001/jamapediatrics.2021.5778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lai DC, Tseng YC, Hou YM, Guo HR. Gender and geographic differences in the prevalence of autism spectrum disorders in children: analysis of data from the national disability registry of Taiwan. Res Dev Disabil. 2012;33:909–915. doi: 10.1016/j.ridd.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 49.Levy SE, Mandell DS, Merhar S, Ittenbach RF, Pinto-Martin JA. Use of complementary and alternative medicine among children recently diagnosed with autistic spectrum disorder. J Dev Behav Pediatr. 2003;24:418–423. doi: 10.1097/00004703-200312000-00003. [DOI] [PubMed] [Google Scholar]
- 50.Loomes R, Hull L, Mandy WPL. What is the maleto-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466–474. doi: 10.1016/j.jaac.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 51.Lotter V. Epidemiology of autism conditions in young children. Soc Psychiatry. 1966;1:124–135. doi: 10.1007/BF00584048. [DOI] [Google Scholar]
- 52.Lyall K, Song L, Botteron K, Croen L, Dager S, Fallin M, Hazlett H, Kauffman E, et al. The association between parental age and autism-related outcomes in children at high familial risk for autism. Autism Research. 2020;13(6):998–1010. doi: 10.1002/aur.2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mandell D, Listerud J, Levy S, Pinto-Martin J. Race differences in the age at diagnosis among Medicaid-eligible children with autism. J Am Acad Child Adolesc Psychiatry. 2002;41:1447–1453. doi: 10.1097/00004583-200212000-00016. [DOI] [PubMed] [Google Scholar]
- 54.Mandell, D., ScD, Novak, M. & Zubritsky, C. (2005). Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics, 116(6), 1480–1486. 10.1542/peds.2005-0185. [DOI] [PMC free article] [PubMed]
- 55.McGrath JJ, Petersen L, Agerbo E, Mors O, Mortensen PB, Pedersen CB. A comprehensive assessment of parental age and psychiatric disorders. JAMA Psychiat. 2014;71:301–309. doi: 10.1001/jamapsychiatry.2013.4081. [DOI] [PubMed] [Google Scholar]
- 56.M-CHAT™ - Autism Screening. (n.d.) Avilable at https://mchatscreen.com.
- 57.Mendoza RL. The economics of autism in Egypt. Am J Econ Bus Admin. 2010;2:12–19. [Google Scholar]
- 58.Metwally AM, Abdel-Latif GA, Mohsen A, El Etreby L, Elmosalami D, Saleh RM, et al. Strengths of community and health facilities based interventions in improving women and adolescents’ care seeking behaviors as approaches for reducing maternal mortality and improving birth outcome among low income communities of Egypt. BMC Health Service Research. 2020;20:592. doi: 10.1186/s12913-020-05412-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Metwally AM, Amer HA, Salama HI, Abd El Hady SI, Alam RR, Aboulghate A, et al. Egyptian patients’/guardians’ experiences and perception about clinical informed consent and its purpose: Cross sectional study. PLoS ONE. 2021;16(6):e0252996. doi: 10.1371/journal.pone.0252996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Metwally AM, El-Sonbaty MM, El Etreby LA, Salah El-Din EM, Abdel Hamid N, Hussien HA, Hassanin AM & Monir ZM. (2020c). Impact of national Egyptian school feeding program on growth, development, and school achievement of school children. World Journal of Pediatrics, 16, 393–400. /10.1007/s12519-020-00342-8. [DOI] [PubMed]
- 61.Metwally, A.M., Hanna, C., Galal ,Y.S., Saleh, R.M., Ibrahim, N.A. &Labib, N.A. (2020a). Impact of nutritional health education on knowledge and practices of mothers of anemic children in El Othmanyia village – Egypt. Open Access Macedonian Journal of Medical Sciences, 8(E), 458–65. Available from: https://oamjms.eu/index.php/mjms/article/view/4570
- 62.Metwally AM, Ibrahim NA, Saad A, Abu el-Ela MH. Improving the roles of rural women in health and environmental issues. Int J Environ Health Res. 2006;16(2):133–44. doi: 10.1080/09603120500539208. [DOI] [PubMed] [Google Scholar]
- 63.Metwally AM, Saad A, Ibrahim NA, Emam HM, El-Etreby LA. Monitoring progress of the role of integration of environmental health education with water and sanitation services in changing community behaviors. Int J Environ Health Res. 2007;17(1):61–74. doi: 10.1080/09603120600937856. [DOI] [PubMed] [Google Scholar]
- 64.Metwally AM, Salah El-Din EM, Shehata MA, Shaalan A, El Etreby LA, Kandeel WA, et al. Early life predictors of socio-emotional development in a sample of Egyptian infants. PLoS ONE. 2016;11(7):e0158086. doi: 10.1371/journal.pone.0158086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Metwally AM, Saleh RM, El-Etreby LA, Salama SI, Aboulghate A, Amer HA, &, , et al. Enhancing the value of women’s reproductive rights through community based interventions in Upper Egypt governorates: a randomized interventional study. Int J Equity Health. 2019;18:146. doi: 10.1186/s12939-019-1042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Micai, M., Ciaramella, A., Salvitti, T., Fulceri, F., Fatta, L., Poustka, L. & et al. (2021). Autistic adult health and professional perceptions of it: Evidence from the ASDEU project. Front Psychiatry, 12, 614102. Published online 2021 May 28. 10.3389/fpsyt.2021.614102, PMCID: PMC8193054. [DOI] [PMC free article] [PubMed]
- 67.Mo K, Sadoway T, Bonato S, Ameis S, Anagnostou E, Lerch J, Taylor M, Lai M. Sex/gender differences in the human autistic brains: a systematic review of 20 years of neuroimaging research. Neuroimage Clinical. 2021;32:102811. doi: 10.1016/j.nicl.2021.102811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Modified checklist for autism in toddlers-revised with follow-up (M-CHAT-R/F) Arabic version Translated by: Dr. Mona Fathelbab, Prof. Suaad Moussa, 2014. 2014. [Google Scholar]
- 69.Mody M, Belliveau J. Speech and language impairments in autism: insights from behavior and neuroimaging. North Am J Med Science (Boston) 2013;5(3):157–161. doi: 10.7156/v5i3p157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mung'ala-Odera V, Meehan R, Njuguna P, Mturi N, Alcock K, Carter JA, et al. Validity and reliability of the 'Ten Questions' questionnaire for detecting moderate to severe neurological impairment in children aged 6–9 years in rural Kenya. Neuroepidemiology. 2004;23(1–2):67–72. doi: 10.1159/000073977. [DOI] [PubMed] [Google Scholar]
- 71.Nicholas JS, Charles JM, Carpenter LA, King LB, Jenner W, Spratt EG. Prevalence and characteristics of children with autism-spectrum disorders. Ann Epidemiol. 2008;18(2):130–136. doi: 10.1016/j.annepidem.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 72.National Research Council (US) Committee on Disability Determination for Mental Retardation. In: Reschly DJ, Myers TG, Hartel CR, editors. Mental Retardation: Determining Eligibility for Social Security Benefits. Washington (DC): National Academies Press (US); Chapter 4, The Role of Adaptive Behavior Assessment; 2002. [PubMed] [Google Scholar]
- 73.Olusanya BO, Davis AC, Wertlieb D, Boo N-Y, Nair MKC, Halpern R, Kuper H, Breinbauer C, De Vries PJ, Gladstone M, et al. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Global Health. 2018;6:e1100–e1121. doi: 10.1016/S2214-109X(18)30309-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Parner ET, Baron-Cohen S, Lauritsen MB, Jørgensen M, Schieve LA, Yeargin Allsopp M, et al. Parental age and autism spectrum disorders. Ann Epidemiol. 2012;22:143–150. doi: 10.1016/j.annepidem.2011.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rai D, Lewis G, Lundberg M, Araya R, Svensson A, Dalman C, Carpenter P, Magnusson C. Parental socioeconomic status and risk of offspring autism spectrum disorders in a Swedish population-based study. J Am Acad Child Adolesc Psychiatry. 2012;51(5):467–476.e6. doi: 10.1016/j.jaac.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 76.Robins DL, Casagrande K, Barton M, Chen CM, Dumont-Mathieu T, Fein D. Validation of the modified checklist for Autism in toddlers, revised with follow-up (M-CHAT-R/F) Pediatrics. 2014;133(1):37–45. doi: 10.1542/peds.2013-1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rosenberg RE, Daniels AM, Law JK, Law PA, Kaufmann WE. Trends in autism spectrum disorder diagnoses: 1994–2007. J Autism Dev Disord. 2009;39:1099–1111. doi: 10.1007/s10803-009-0723-6. [DOI] [PubMed] [Google Scholar]
- 78.Rubenstein E, Wiggins L, Lee L. A review of the differences in developmental, psychiatric, and medical endophenotypes between males and females with autism spectrum disorder. J Dev Phys Disabil. 2015;27(1):119–139. doi: 10.1007/s10882-014-9397-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Salah El-Din EM, Elabd MA, Nassar MS, Metwally AM, Abdellatif GA, Rabah TM, et al. The interaction of social, physical and nutritive factors in triggering early developmental language delay in a sample of Egyptian children. Open Access Macedonian Journal of Medical Sciences. 2019;7(17):2767–2774. doi: 10.3889/oamjms.2019.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Salah EM, Khalifa AG, Metwally AM, et al. The impact of school snacks on cognitive function of primary school children in Egypt. J Appl Sci Res. 2012;8(12):5639–5650. [Google Scholar]
- 81.Salhia H, Al-Nasser L, Taher L, Al-Khathaami A, El-Metwally A. Systemic review of the epidemiology of autism in Arab Gulf countries. Neurosciences (Riyadh) 2014;19:291–296. [PMC free article] [PubMed] [Google Scholar]
- 82.Samadi SA, McConkey R. The utility of the Gilliam autism rating scale for identifying Iranian children with autism. Disabil Rehabil. 2014;36(6):452–456. doi: 10.3109/09638288.2013.797514. [DOI] [PubMed] [Google Scholar]
- 83.Saulnier CA, Klaiman C. Assessment of adaptive behavior in autism spectrum disorder. Psychol Sch. 2022;59(7):1419–1429. doi: 10.1002/pits.22690. [DOI] [Google Scholar]
- 84.Schopler E, Reichler RJ, DeVellis RF, Daly K. Toward objective classification of childhood autism: Childhood autism rating scale (CARS) J Autism Dev Disord. 1980;10(1):91–103. doi: 10.1007/BF02408436. [DOI] [PubMed] [Google Scholar]
- 85.SeifEldin A, Habib D, Noufal A, Farrag S, Bazaid K, Al-Sharbati M, et al. Use of M-CHAT for a multinational screening of young children with autism in the Arab countries. Int Rev Psychiatry. 2008;20(3):281–289. doi: 10.1080/09540260801990324. [DOI] [PubMed] [Google Scholar]
- 86.Shah K. What do medical students know about autism. Autism. 2001;5:127–133. doi: 10.1177/1362361301005002003. [DOI] [PubMed] [Google Scholar]
- 87.Shelton J, Hertz-Picciotto I, Pessah I. Tipping the balance of autism risk: potential mechanisms linking pesticides and autism. Environ Health Perspect. 2012;120:944–951. doi: 10.1289/ehp.1104553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shuid A, Jayusman P, Shuid N, Ismail J, Nor N, Mohamed I. Association between viral infections and risk of autistic disorder: an overview. Int J Environ Res Public Health. 2021;18(6):2817. doi: 10.3390/ijerph18062817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sipes M, Matson JL, Worley JA, Kozlowski AM. Gender differences in symptoms of autism spectrum disorders in toddlers. Res Autism Spectrum Disord. 2011;5(4):1465–1470. doi: 10.1016/j.rasd.2011.02.007. [DOI] [Google Scholar]
- 90.Slentz, K.L., Early, D.M & McKenna, M. (2008). A guide to assessment in early childhood: infancy to age eight. Superintendent of Public Instruction. [Olympia, Wash.], Washington State Office of Superintendent of Public Instruction 2008. http://www.digitalarchives.wa.gov/ViewRecordMedia.aspx?RID=6EA736E930FE301DC888E3D5D153F6D8.
- 91.Solomon M, Miller M, Taylor SL, Hinshaw SP, Carter CS. Autism symptoms and internalizing psychopathology in girls and boys with autism spectrum disorders. J Autism Dev Disord. 2012;42(1):48–59. doi: 10.1007/s10803-011-1215-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sparrow SS, Balla DA, Cicchetti DV. Vineland adaptive behavior scales. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- 93.SPSS IBM Corp . IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: SPSS IBM Corp; 2016. [Google Scholar]
- 94.Volkmar F, Siegel M, Woodbury-Smith M, King B, McCracken J, State M. American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Quality Issues (CQI). Practice parameter for the assessment and treatment of children and adolescents with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2014;53(2):237–257. doi: 10.1016/j.jaac.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 95.Volkmar FR, Sparrow SS, Goudreau D, Cicchetti DV, Paul R, Cohen DJ. Social deficits in autism: An operational approach using the Vineland Adaptive Behavior Scales. J Am Acad Adolesc Psychiatry. 1987;26(2):156–161. doi: 10.1097/0000483-198703000-00005. [DOI] [PubMed] [Google Scholar]
- 96.Warrier V, Greenberg D, Weir E, Buckingham C, Smith P, Lai M, Allison C, Baron-Cohen S. Elevated rates of autism, other neurodevelopmental and psychiatric diagnoses, and autistic traits in transgender and gender-diverse individuals. Nat Commun. 2020;11:3959. doi: 10.1038/s41467-020-17794-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Weir E, Allison C, Warrier V, Baron-Cohen S. Increased prevalence of non-communicable physical health conditions among autistic adults. Autism. 2021;25(3):681–694. doi: 10.1177/1362361320953652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Williams JG, Higgins JP, Brayne CE. Systematic review of prevalence studies of autism spectrum disorders. Arch Dis Child. 2006;91:8–15. doi: 10.1136/adc.2004.062083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.World Health Organization . International Classification of Functioning, Disability and Health (ICF) external icon. Geneva: WHO; 2001. [Google Scholar]
- 100.World Health Organization . International Classification of Functioning, Disability and Health, Version for children and Youth (ICF-CY) Geneva: WHO; 2007. [Google Scholar]
- 101.Yeargin-Allospp M, Rice C, Karapurkar T, Doernberg N, Boyle C, Murphy C. Prevalence of autism in a US metropolitan area. J Am Med Assoc. 2003;289(1):49–55. doi: 10.1001/jama.289.1.49. [DOI] [PubMed] [Google Scholar]
- 102.Yousef AM, Roshdy EH, Abdel Fattah NR, Said RM, Atia MM, Hafez EM, Mohamed AE. Prevalence and risk factors of autism spectrum disorders in preschool children in Sharkia, Egypt: a community-based study. Middle East Current Psychiatry. 2021;28:1–14. doi: 10.1186/s43045-021-00114-8. [DOI] [Google Scholar]
- 103.Zeglam A, Maouna A. Is there a need for a focused health care service for children with autistic spectrum disorders? A keyhole look at this problem in Tripoli. Libya Autism. 2011;16(4):337–339. doi: 10.1177/1362361310393535. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: S Table-1. (List of the targeted Households (HH) according to the governorates, locality and sociodemographic status for screening of at high risk autism among children aged 1-12 years).
Additional file 2: S Table-2. Raw data (XLSX) that are anonymous.
Data Availability Statement
The datasets used and analyzed during the current study are anonymous and are fully available without restriction as S Table-2 Raw data (XLSX).