Sir,
We present the case of a 48-year-old woman with a history of diffuse cutaneous systemic sclerosis (SSc) with prominent salt and pepper changes. In August 2015, she was diagnosed with SSc based on proximal skin thickening, Raynaud’s phenomenon with digital ulcers, abnormal nailfold capillary changes (giant capillaries and hemorrhages), esophageal dysmotility, and calcinosis. At the time of diagnosis, she also developed proximal muscle weakness and creatine kinase (CK) was elevated to 600 IU/L. She was prescribed prednisone and mycophenolate mofetil (MMF), which she intermittently took from 2015-2017. She was referred to our Center by November 2018 for progressive muscle weakness and skin tightening and was not on any therapy. On skin examination, her modified Rodnan skin score (mRSS) was 17 and she had prominent salt and pepper like changes on the anterior chest, forehead, and posterior neck. Muscle strength exam revealed proximal muscle weakness with neck flexors of 2/5, bilateral arm abductors 3/5, and hip flexors 2/5 on MRC scale. The remainder of the examination was unremarkable. CK was 142 IU/L. SSc specific antibodies were negative. Myositis panel was positive for U3-RNP (anti-fibrillarin). She underwent electromyography (EMG) which demonstrated severe non-irritable myopathy and bilateral thigh muscle magnetic resonance imaging (MRI-T2/STIR) demonstrated muscle edema. She declined muscle biopsy. Based on active skin disease and severe myopathy, MMF was initiated in December 2018 but ultimately discontinued due to gastrointestinal side effects. Intravenous immunoglobulin (IVIG) was started in March 2020 and within 4 months, she had improvement of her proximal muscle weakness. By November 2020, she developed inflammatory arthritis and was started on tofacitinib 11mg XR daily. Three months thereafter, in January 2021, she reported improvement in inflammatory arthritis, skin tightening, and hypopigmentation. On follow-up examination in August 2021, she had significant improvement of the salt and pepper changes of the skin (Figure 1). Interestingly, there was also improvement of the mRSS (17 points to 8 points) and muscle strength (2/5 to 4+/5 in proximal muscles). Janus kinase (JAK) inhibitors such as tofacitinib have been reported to be efficacious in treating diffuse SSc and dermatomyositis in early phase clinical trials (1, 2). Bariticinitb has also been reported to be efficacious in the treatment of refractory arthritis in a patient with diffuse SSc (3). Recently, topical ruxolitinib was approved for the treatment of non-segmental vitiligo (4).
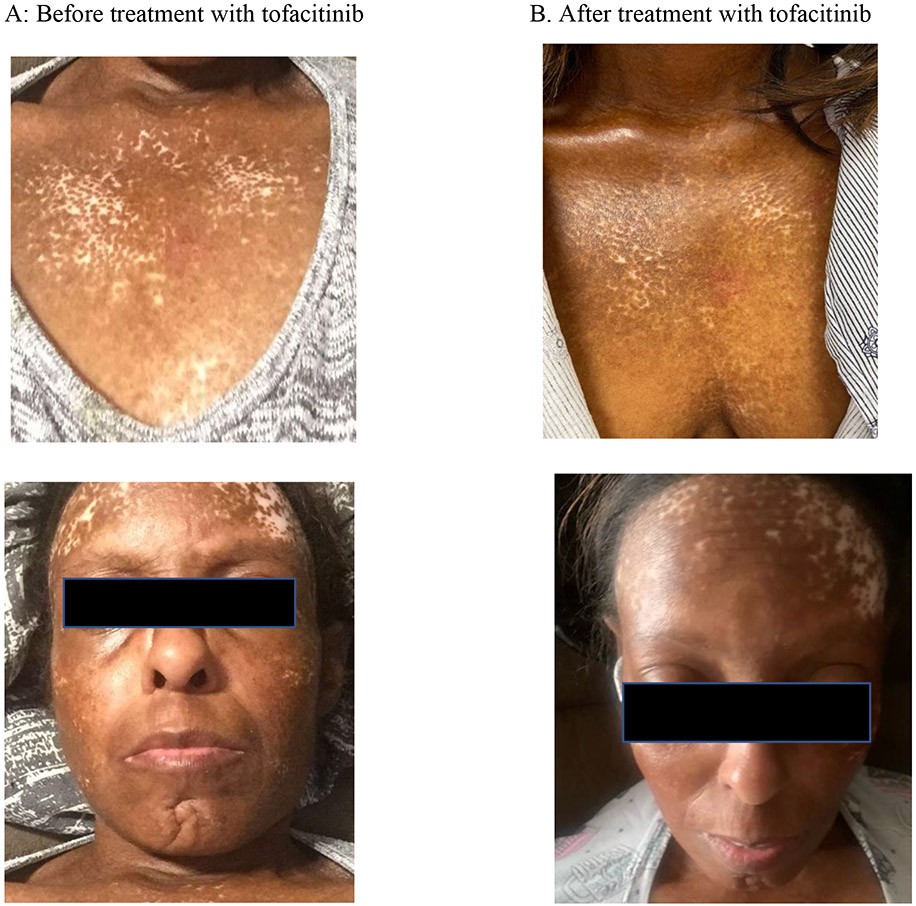
Fig. 1.
On the left is a 48-year-old female before treatment with severe skin hypopigmentation and hyperpigmentation appearing with salt and pepper changes on her anterior chest, forehead, and face. After 8 months of treatment with tofacitinib, the right panel shows regimentation of affected skin in anterior chest, right anterior forehead, and cheeks.
Salt and pepper changes of the skin in SSc are thought to be due to areas of depigmentation where the perifollicular pigmentation remains intact. The proposed autoimmune mechanism is that the melanocytes in the perifollicular areas are spared (5) because the perifollicular sites have a better capillary system that can warm the perifollicular skin which further enables melanogenesis and thus pigmentation for these areas (6). The pathogenesis is thought to be similar to that of vitiligo where the JAK/STAT pathway has been implicated. JAKs transcribe cytokine-mediated signals which lead to activation of STAT1 and result in CXCL10 transcription (thought to be elevated in vitiligo patients) where JAK inhibitors, like tofacitinib, block cytokine signaling to induce re-pigmentation (7, 8). While our patient was on combination therapy with tofacitinib and IVIG, the improvement was clearly evident 3 months after initiation of tofacitinib. To our knowledge, this case is the first report of significant improvement in pigmentation after treatment with tofacitinib in diffuse SSc. However, it should be noted that the pigment change may have also occurred due to changes in disease control rather than direct effects of the tofacitinib. Nonetheless, JAK inhibitors may be a promising therapeutic agent for the treatment of salt and pepper depigmentation in patients with diffuse cutaneous SSc.
Funding.
J.J. Paik is supported in part by K23AR073927.
Footnotes
Competing interests: none declared.
References
- 1.KHANNA D, NAGARAJA V, KOENIG A et al. : Tofacitinib in early diffuse cutaneous systemic sclerosis- results of phase I/II investigator iniviated, double blind randomized placebo-controlled trial [abstract]. Arthritis Rheumatol 2019; Accessed November 23, 2021. [Google Scholar]
- 2.PAIK JJ, CASCIOLA-ROSEN L, SHIN JY et al. : Study of Tofacitinib in Refractory Dermatomyositis (STIR): An open label pilot study of 10 patients. Arthritis Rheumatol 2021; 73: 858–65. 10.1002/art.41602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.BOLETO G, CREN J-B, AVOUAC J, ALLANORE Y: Successful treatment with baricitinib of refractory arthritis in a patient with severe diffuse cutaneous systemic sclerosis-rheumatoid arthritis overlap syndrome. Clin Exp Rheumatol 2021; 39 (Suppl. 131): S163–4. 10.55563/clinexprheumatol/gu1ac8 [DOI] [PubMed] [Google Scholar]
- 4.FDA approves topical treatments addressing repigmentation in vitiligo in patients aged 12 and older. Available from: https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-topical-treatment-addressing-repigmentation-vitiligo-patients-aged-12-and-older [Google Scholar]
- 5.VARGA J, DENTON CP, WIGLEY FM, KUWANA M: Scleroderma: from pathogenesis to comprehensive management. New York, Springer, 2011. 10.1007/978-3-319-31407-5 [DOI] [Google Scholar]
- 6.VIJAYARAJU D, PRAKASH G, YOGANANDH T, SUBRAMANIAN SR, RAMKUMAR S: Salt and Pepper Pigmentation - Skin Manifestation of Systemic Sclerosis. J Assoc Physicians India 2015; 63: 70. [PubMed] [Google Scholar]
- 7.RASHIGHI M, HARRIS JE: Interfering with the IFN-γ/CXCL10 pathway to develop new targeted treatments for vitiligo. Ann Transl Med 2015; 3: 343. 10.3978/j.issn.2305-5839.2015.11.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.SEARLE T, AL-NIAIMI F, ALI FR: Vitiligo: an update on systemic treatments. Clin Exp Dermatol 2021; 46: 248–58. 10.1111/ced.14435 [DOI] [PubMed] [Google Scholar]