Abstract
Introduction
This scoping review takes stock of the social and behavior change theories that have underpinned tobacco interventions tailored to sexual and/or gender minority (SGM) people and reflects on the need to target contextually based drivers of SGM tobacco use inequities.
Aims and Methods
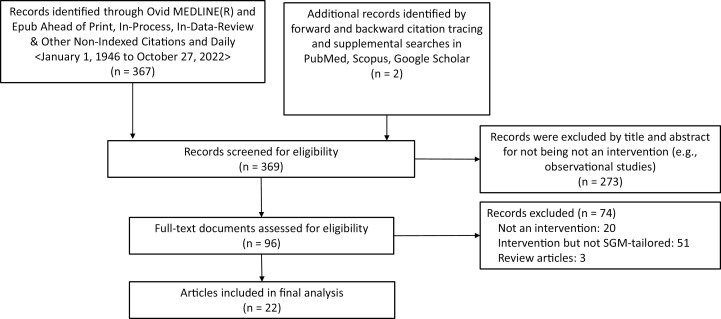
Data sources were Medline (Ovid), Scopus, PubMed, and Google Scholar (January 01, 1946 to October 27, 2022). Peer-reviewed publications in English from anywhere in the world describing SGM-tailored tobacco cessation and/or prevention interventions were independently identified by a librarian and screened by the first and third authors. Three hundred and sixty-seven articles were extracted; an additional two were found by hand searching. A total of 369 articles were assessed for eligibility. Exclusion criteria were: Not an intervention, review article, not SGM-tailored, or tobacco-focused. We documented the intervention name, intervention components, theoretical frameworks cited in reference to intervention design and/or implementation, and evaluation outcomes. All authors provided input on theoretical framework categorization.
Results
We identified 22 publications corresponding to 15 unique interventions. Individual-level behavior change theories (ie, those focusing on within-person behavior change processes) were the most prominent. Among these, the Transtheoretical Model was the most frequently utilized, while Social Inoculation Theory, Theory of Reasoned Action, and Theory of Psychological Reactance were also employed. A minority of interventions referenced frameworks that more explicitly engaged with SGM people’s social contexts, namely, Theory of Diffusion of Innovations and Minority Stress Model.
Conclusions
Future SGM-tailored tobacco interventions should leverage both the strengths of individual-level behavior change theories and those of frameworks that understand tobacco use inequities as indivisible from place, context, and policy.
Implications
This scoping review describes the theoretical underpinnings of sexual and/or gender minority (SGM)-tailored tobacco interventions published in the peer-review literature in English. It reflects on the need for greater utilization of social and behavior change theoretical frameworks that can engage with unique drivers of SGM tobacco use and barriers to cessation.
Introduction
Persistently high tobacco use rates among sexual and/or gender minority (SGM) groups1–3 have roots in the social, political, and physical environments that SGM people live in and the ways in which tobacco use is linked to interacting with and negotiating these environments as a socially minoritized person.4–9 For example, studies from predominantly English-speaking countries have attributed tobacco use among SGM individuals to cope with experiences of social minority stress, including internalized homophobia, fear of rejection, harassment, and violence.4,5,10–17 Tobacco use has also been described by SGM individuals as a way to symbolically resist oppression by engaging in a “counterculture” practice.18,19 The tobacco industry capitalizes on the motives that many SGM people report for using tobacco and has long promoted tobacco use among SGM groups with targeted tobacco marketing campaigns.20–24 Consequently, pro-tobacco norms are prevalent within SGM social networks, and tobacco use is highly visible within SGM-oriented media and spaces.19,25–29 Promoting health equity for SGM groups through tobacco-free living must be done in a way that can address these unique drivers of use at the individual, network, community, and ecological levels, as well as the barriers that SGM people have to access tobacco cessation assistance30,31 and the preference SGM people have expressed for tailored and culturally relevant intervention approaches.32–35
There has been an increase in tailored tobacco cessation and prevention interventions for SGM people in the past decade,36–38 although early tobacco control efforts for SGM communities began at least in the early 1990s.39 These efforts have been concentrated in the United States; as of 2017, 79% of SGM-tailored tobacco cessation interventions originated in the United States.37 The modest but growing body of scholarly evidence on SGM-tailored tobacco interventions presents an opportunity to take stock of the social and behavior change theories that have underpinned these intervention efforts thus far. It also provides an opportunity to consider how theories that have been employed in other health behavior change fields may be leveraged to further engage with drivers of SGM tobacco use that are perpetuated within person-environment interactions.
Following Glanz et al,40,41 social and behavior change theories each offer “a systematic way of understanding events, behaviors and/or situations”.40 They consist of “a set of interrelated concepts, definitions, and propositions that explain or predict events or situations by specifying relations among variables”.40 Increasing evidence suggests that public health and health-promoting interventions that are informed by social and behavior change theories are more effective than those lacking an explicit theoretical base.40,42–44 Moreover, the particular set of factors that a social and/or behavior change theory relies upon to explain or predict health behavior (eg, affect, knowledge, attitudes, social networks, culture, and geography) also appears to influence the effectiveness of the interventions informed by that theory.40,45,46 For example, interventions that focus on individual-level processes of behavior change will influence different factors related to smoking than interventions that also account for the social and physical environments of smoking behavior and smoking cessation.
Although prior reviews of SGM-tailored tobacco interventions exist,36–38 none have specifically examined the social and behavior change theories that have underpinned these interventions. To address this gap in the literature, we conducted a scoping review with the objective of assessing the theoretical influences driving the current direction of the scientific field of SGM-tailored tobacco intervention design and implementation. We limit our scoping review to publications that have gone through the peer-review process, which is meant to improve the scientific accuracy and quality of published reports.47
Methods
We conducted a scoping review of peer-reviewed articles published in English from anywhere in the world that described SGM-tailored tobacco cessation and prevention interventions and identified any theoretical frameworks referenced therein. A comprehensive Ovid MEDLINE search was performed by a health sciences librarian (SC) for the time period of January 1, 1946 (database inception) to October 27, 2022. The full electronic search strategy for Ovid MEDLINE is provided in Supplementary Appendix A. This yielded 367 unique records. Two (2) additional unique records were identified by the first and third author with forward and backward citation tracking (ie, hand searching) and supplemental searches in Scopus, PubMed, and Google Scholar with the keywords “sexual and gender minorities”, OR “LGB,*” AND “smoking cessation”, OR “tobacco intervention”.
Figure 1, below, displays the article identification and selection process that was followed by the first and third authors. Inclusion criteria were any peer-reviewed work published in the English language (January 1, 1946 to October 27, 2022) describing or reporting the outcomes of an intervention tailored to reduce, prevent, or stop tobacco use among SGM populations. By “interventions” we mean behavioral interventions, pharmacotherapy, clinical approaches, communication and media campaigns, public policy, and combinations thereof. By “tobacco”, we mean any nicotine-containing product other than U.S. Food and Drug Administration-approved medications for tobacco cessation (eg, nicotine replacement therapy). By SGM-tailored, we mean enhanced and/or informed intervention approaches for SGM populations that specifically take into account characteristics shared by SGM people. We endorse the term “tailored” over “targeted” because of the connotations of violence in the latter term.48 Exclusion criteria were: (1) literature reviews or other work that does not report primary research on an SGM-tailored tobacco intervention, (2) non-peer-reviewed work, and (3) formative work to inform future SGM-tailored tobacco intervention design. Ultimately, we identified 22 articles for inclusion in the final analysis that described or reported on outcomes of a total of 15 unique SGM-tailored tobacco interventions.
Figure 1.
Identification and selection.
The first author read the articles included for final analysis (n = 22) in full and recorded the following dimensions for each article:
Intervention name (or concise intervention description if not named).
Main intervention delivery components (eg, group counseling, 7-week program, began with an educational focus, and shifted to a social support focus in later weeks).
Any social and/or behavior change theories referenced in the article (eg, Diffusion of Innovations).
Evaluation components (eg, sample size, use of comparison or control group, primary outcome measures).
All authors provided input on decisions regarding how to describe and categorize the theories underpinning each intervention.
Findings
Table 1 summarizes the social and behavior change theoretical frameworks underpinning peer-review published SGM-tailored tobacco interventions. Frameworks are grouped by the theories that informed them and listed in order of most to least cited. Five interventions were not linked to a specific theory in their corresponding publication(s), or, they mentioned concepts that were likely related to specific theoretical underpinnings, but did not make this explicit (eg, “psychosocial treatment”; “cognitive behavioral program”).49–51 Several interventions were linked to multiple theories. Multiple articles associated with the same intervention are included in the table as cases were found where all the theories that informed the intervention were not listed exhaustively in any one publication associated with that intervention.
Table 1.
Theoretical Frameworks Informing Sexual and/or Gender Minority (SGM)-tailored Tobacco Interventions Published in the Peer-reviewed Literature (n = 15 Unique Interventions; January 1, 1946 to October 27, 2022)
| Social and/or behavioral theory | # Interventions | Intervention name(s) and main intended outcome | Corresponding peer-reviewed publication(s) |
|---|---|---|---|
| Unspecified theoretical framework | |||
| No explicit theoretical framework | 5 | Queer Quit -Cigarette smoking cessation Project Exhale -Cigarette smoking cessation Freedom from Smokinga -Cigarette smoking cessation Location-based media campaign for lesbian and bisexual women -Promote cigarette smoking cessation and awareness of state quitline Smoking cessation for gay men -Cigarette smoking cessation |
Dickson-Spillmann et al. 2014 Matthews, Conrad, et al. 2013 Matthews, Li et al. 2013 Caldwell et al. 2022 Harding et al. 2004 |
| Individual-level theories of behavior | |||
| Transtheoretical Model | 3 | The Last Drag -Cigarette smoking cessation Courage to Quita -Cigarette smoking cessation The Put It Out Project -Cigarette smoking cessation |
Eliason et al. 2012 Walls and Wisneski 2011 Williams et al. 2020 Matthews et al. 2014 Matthews, Steffen et al. 2019 Vogel et al. 2020 Vogel et al. 2019 |
| Theory of Reasoned Action or Theory of Planned Behavior b | 3 | This Free Life -Change beliefs about cigarette smoking This Free Life + local Social Branding -Increase intentions to quit cigarette smoking Truth Campaigna -Increase support for tobacco control policies and anti-tobacco industry sentiments |
Guillory et al. 2021 Crankshaw et al. 2022 Navarro et al. 2019 Hinds et al. 2021 Beckerley et al. 2022 Skurka et al. 2021 |
| Social Inoculation Theory | 2 | This Free Life -Change beliefs about cigarette smoking Truth Campaigna -Increase support for tobacco control policies and anti-tobacco industry sentiments |
Guillory et al. 2021 Crankshaw et al. 2022 Navarro et al. 2019 Hinds et al. 2021 Skurka et al. 2021 |
| Theory of Psychological Reactance | 2 | This Free Life -Change beliefs about cigarette smoking Truth Campaigna -Increase support for tobacco control policies and anti-tobacco industry sentiments |
Guillory et al. 2021 Crankshaw et al. 2022 Navarro et al. 2019 Hinds et al. 2021 Skurka et al. 2021 |
| Health Belief Model | 1 | Courage to Quita -Cigarette smoking cessation |
Matthews et al. 2014 Matthews, Steffen et al. 2019 |
| Relational Frame Theory | 1 | Empowered, Queer, Quitting, and Living (EQQUAL) -Cigarette smoking cessation |
Heffner et al. 2021 |
| Self-Determination Theory | 1 | Proactive Outreach Lettera -Increase uptake of state quitline cigarette smoking cessation services |
Matthews, Breen et al. 2019 |
| Theories of social context and behavior | |||
| Diffusion of Innovations Theory | 3 | CRUSH -Reduce cigarette smoking prevalence Break Up -Reduce cigarette smoking prevalence This Free Life + local Social Branding -Increase intentions to quit cigarette smoking |
Fallin et al. 2015 Plant et al. 2017 Beckerley et al. 2022 |
| Minority Stress Model | 1 | Courage to Quita -Cigarette smoking cessation |
Matthews et al. 2014 |
aIndicates an SGM-tailored version of the intervention.
bUsually classified together under the Reasoned Action Approach umbrella52.
The main intended outcome of each intervention is noted in italics beneath the intervention name. As observed in Table 1, the majority of interventions focused on cigarette smoking cessation, with a minority focusing on beliefs, norms, and/or intentions related to cigarettes. Nicotine-containing products other than cigarettes (eg, e-cigarettes, smokeless tobacco) were not targeted. As an exception, one intervention53 aimed to encourage support for tobacco control policies and anti-tobacco industry sentiment rather than focusing on cigarettes specifically.
Individual-level behavior change theories—meaning those that focus on explaining within-person processes of behavior change—were the most prominent. Among these, the most utilized theory was the Transtheoretical Model, cited in the articles describing three interventions.54–59 This framework delineates a process in which individuals move through various “stages of readiness” for behavior change, from pre-contemplation to sustained termination of smoking.60 SGM-tailored interventions have “stage-matched” their engagement with participants according to where they fall on the theorized behavior change continuum.56,57 One intervention cited the health belief model,58,61 which purports that a person’s belief in the personal threat of tobacco-related harm, and the extent to which they believe that abstaining from tobacco use will benefit them, will predict tobacco cessation motivation and outcomes.62 Another study used relational frame theory,63 which underpins acceptance and commitment therapy, to support SGM smoking cessation.63 Acceptance and commitment therapy focuses on building psychological flexibility—defined as a willingness to experience uncomfortable thoughts, feelings, and physical sensations without attempting to change them—and having clarity of one’s values to act in a way that is in service of those values.63,64 Self-determination Theory,65 cited as informing one intervention,66 emphasizes the importance of competence, relatedness, and autonomy in the successful achievement of goal-directed behavior, like smoking cessation.
SGM-tailored tobacco interventions have also utilized public education media campaigns that deliver counter-tobacco industry messaging.53,67–71 While the publications describing these SGM-tailored interventions may not explicitly cite theory, Hersey et al72 argue that the influence of these types of anti-tobacco campaigns on the beliefs, attitudes, and behaviors of those exposed to messaging is best explained by Social Inoculation Theory,73 Theory of Reasoned Action,74 and Theory of Psychological Reactance.75 Social Inoculation Theory explains how exposing people to small “doses” of tobacco industry marketing alongside delegitimizing arguments can protect them from being persuaded by subsequent exposure to tobacco marketing. The Theory of Reasoned Action focuses on attitudes and intentions toward a behavior; if anti-tobacco industry messaging can shift beliefs about the tobacco industry, it may also shift attitudes about and intentions to use tobacco products and, therefore, tobacco use. The Theory of Psychological Reactance posits that the perception of a threat to one’s freedom to act or not act produces an experience of reactance that motivates the individual to regain their threatened or lost freedom. There is evidence that campaigns that portray the tobacco industry as manipulating the public for their own gain may arouse psychological reactance against the tobacco industry and its products.76
A minority of SGM-tailored tobacco interventions (3 out of 12) referenced frameworks that more explicitly engage with the social contexts of SGM people. Fallin et al,77 Plant et al,78 and Beckerley et al71 described local social branding or social marketing campaigns. These were community-level approaches to behavior change based on the Diffusion of Innovations Theory.79 This theory focuses on the importance of social networks in the spread, maintenance, and demise of behaviors and attitudes within a population and emphasizes the role of certain influential group members in promoting or discouraging the uptake of the behavior or attitudes within the rest of the group. These interventions used commercial marketing strategies that were culturally tailored to SGM to try to shift pro-tobacco norms within SGM social networks and spaces by using anti-tobacco messaging, branded events in lesbian and gay bars, and recruitment of influential SGM community members to endorse the intervention’s anti-tobacco message.
Matthews et al55 work describing an SGM-tailored intervention was unique in that its conceptual framework explicitly integrated individual-level as well as SGM-specific cultural and psychosocial factors that may influence tobacco use and tobacco cessation outcomes for SGM people. Individual-level factors were drawn from the Health Belief Model and the Transtheoretical Model, while interpersonal and community-level factors were derived from the Minority Stress Model.80 This model explains how stigma, prejudice, and discrimination create a hostile and stressful social environment, which in turn causes mental health problems and maladaptive coping behaviors, like tobacco use, for SGM individuals.80 This intervention’s conceptual framework integrated predictors of cessation that are both generic as well as those that are specific to SGM groups. “Individually-mediated predictors of cessation” included perceived benefits of cessation, self-efficacy for quitting, and stage of readiness. “Cultural factors” were also accounted for, such as identification with SGM community, as well as “psychosocial factors”, namely, general stress (eg, number of stressful life events) and minority-specific stress (eg, internalized homophobia). In practice, these factors were addressed in group counseling sessions by discussing SGM determinants of tobacco use (eg, SGM social norms, SGM industry targeting) and SGM health and weight concerns. Finally, while Caldwell et al81 practice note did not provide an explicit theoretical basis for the intervention, it described a contextually engaged approach to a smoking cessation messaging campaign in Western North Carolina. The digital approach used cell phone locations and marketing profiles to deliver tailored smoking cessation messages to LB women while they were in the vicinity of a location known to be frequented by LB women in the area.
It would be ideal to assess the relative success of different theoretical approaches across SGM-tailored tobacco interventions, however, we found that the current body of peer-reviewed intervention outcomes is difficult to compare. Intervention delivery approaches have been heterogeneous, including in-person group sessions,54,59 online interventions,56,63 video ad campaigns, outreach letters,66 and hybrid digital, venue, and event-based social marketing campaigns.77,78 Publications reported a broad range of evaluation designs from cross-sectional pre- and post-intervention surveys within selected geographical areas67,68,77,78 to assessment of within-subject outcomes post-intervention,49–51,54–56,58,59 qualitative assessment of intervention acceptability,66,70 and use of single arm trials49,50,53,59,63 versus those with comparison and/or control groups.53,56,58,67,68,82
Four interventions’ effects were evaluated with randomized control or comparison group design. These likely offer53 the most reliable insights into theory-informed SGM-tailored tobacco intervention effectiveness to date.53,55,56,58,67,68 These were: (1) an SGM-tailored version of Courage to Quit,55,58 a group-based smoking cessation intervention delivered in SGM-serving health care centers that drew from the Transtheoretical Model, the Health Belief Model, and the Minority Stress Model, (2) the Put It Out Project,82 a group-based smoking cessation intervention delivered on social media that drew from the Transtheoretical Model, (3) This Free Life,67,68 a national digital ad campaign designed to promote anti-tobacco norms and behaviors that drew from the Theory of Psychological Reactance, the Theory of Reasoned Action, and Social Inoculation Theory,82 and (4) an SGM-tailored version of the Truth Campaign,53 a national anti-tobacco industry video ad campaign designed to promote anti-tobacco norms and behaviors, which also drew from the Theory of Psychological Reactance, the Theory of Reasoned Action, and Social Inoculation Theory. Outcomes from these four interventions showed mixed results, and are summarized below.
The prospective randomized design used to evaluate the SGM-tailored version of Courage to Quit against a non-tailored version of Courage to Quit55,58 found no differences between treatment groups in the primary outcome of biochemically verified smoking quit rates or in secondary outcomes but did find that the tailored version was more highly rated on acceptability than the non-tailored version (ie, program effectiveness, intervention techniques, treatment manual, being targeted to the needs of SGM individuals who smoke).
The Put It Out Project’s56 primary outcome, biochemically verified smoking abstinence, did not differ significantly between the randomized tailored and non-tailored Facebook treatment groups. However, secondary outcomes did show that the group receiving the tailored intervention was more likely than the non-tailored group to self-report smoking abstinence at 3- and 6 months and was more likely to report reduced smoking at 3 months (but not at 6 months). No difference between tailored and non-tailored groups was observed with regards to making a quit attempt during treatment or movement between the Transtheoretical Model’s stages of change (ie, pre-contemplation, contemplation, preparation, and action or maintenance).
Counter-industry tobacco advertisements from the Truth Campaign were tailored to target either SGM individuals or black individuals.53 These were evaluated with a web-based, between-subjects experimental design in which participants were randomized to watch different types of ads.53 The evaluation concluded that there was little evidence that the targeted counter-industry ads were especially influential in increasing support for tobacco control policies or counter-industry beliefs for either of their respective intended groups, but that the ads may have evoked anger among participants toward the tobacco industry regardless of the audience targeted.
Finally, the final evaluation of his Free Life,67 a primarily digital campaign designed to change tobacco-related beliefs among SGM young adults, compared end-of-campaign awareness, receptivity to, and effect of campaign exposure on tobacco-related beliefs in 24 treatment and control markets. The evaluation concluded that the campaign had modest overall effects, with high campaign awareness and receptivity but only a small effect on beliefs involving social aspects of smoking.56
Discussion
Overall, individual-level theories of behavior change have dominated the design and implementation of SGM-tailored tobacco interventions as described in the peer-reviewed literature. These frameworks have value for addressing important within-person factors related to SGM-tailored tobacco interventions. For example, the focus on strengthening generalizable emotion regulation skills via acceptance and commitment therapy may be particularly relevant to supporting tobacco cessation for socially minoritized groups because it can increase resilience to minority stressors that help drive high SGM tobacco use rates.63 However, individual-level theories may not adequately engage with drivers of SGM tobacco use that reside within the person-environment relationship. As exceptions, some engagement has been made with the role of social networks in SGM tobacco use and cessation, as well as social minority stressors unique to SGM people that may exacerbate tobacco use and impede cessation. Building on Matthews et al. explicit integration of individual-level theories of behavior change with the Minority Stress Model,55 we advocate for more utilization of theoretical frameworks that account for multi-level factors relevant to SGM-tailored tobacco prevention and cessation.
There is increasing acknowledgment of the need for greater engagement with and more sophisticated conceptualizations of “context” in health behavior and health equity research,83,84 including tobacco-related research.3,85–93 Socio-ecological frameworks have been employed in tobacco use inequities research and tobacco control efforts,3,91–93 but this scoping review found that they have yet to be used to explicitly inform tobacco prevention and cessation intervention approaches for SGM people. The socio-ecological model has long accounted for five levels of influence on health behavior: Intrapersonal, interpersonal (including dyadic-level influences), organizational, community, and public policy.45 The social context of health promotion is known to impact the target health behavior as well as how health interventions are received, play out, and make an impact.94 For example, Williams et al.95 reflected on a failed attempt to implement a San Francisco-based SGM-tailored tobacco intervention in SGM communities in South Central Texas, reporting the need to address local social, cultural, and political factors when adapting and implementing existing interventions for different regions.
From a theoretical perspective, thoroughly taking context into account would mean moving beyond the typical social psychological conceptualization of “context” as the individual’s immediate internal state and location in space and time (ie, “situational triggers” of behavior) to understanding context through disciplinary lenses like those of anthropology, sociology, and human and cultural geography. These disciplinary approaches to context are underutilized in public health and health promotion research and account for the relational, dynamic, and transformative interactions between individuals and their everyday contexts. They consider social relations that are embedded in the rules, values, and resources of social structures and contexts,83 as well as the importance of neighborhood and ecological factors on health behavior96 that are determined by place-based practices and place-based regulation.86
A reorientation toward context in SGM-tailored tobacco intervention design, implementation, and evaluation can stimulate context-related questions that may be important for tobacco prevention and cessation outcomes. For example, how do area-level characteristics where SGM people live, such as levels of structural stigma which vary by state,97 interplay with how SGM people experience smoking and quitting? And, how can these contextual factors be addressed in an intervention approach to support SGM people’s smoking cessation experiences and outcomes? What additional pathways for intervention are available within place-based regulation and practices? How can public health efforts better support and reward SGM organizational policies that reject tobacco industry co-optation of LGBTQ+ Pride celebration spaces and run more tobacco-free Pride events?98 How can tobacco interventions influence policies and practices in nightlife spaces where SGM people have long been targeted by tobacco industry marketing and tobacco use practices are prevalent?26 Importantly, how can SGM-tailored tobacco interventions be designed and implemented in partnership with SGM communities such that SGM individuals are involved in multi-level efforts to support health equity and well-being in their own communities?
Empowerment Theory is one approach that may be especially effective in multi-level, community-engaged control efforts among socially minoritized groups, like SGM people, because it links individual well-being to the larger social and political environment.99 Empowerment Theory-informed approaches have not been used in SGM-tailored tobacco interventions, but have been found to be feasible, acceptable, and efficacious among SGM communities for HIV and STI prevention100,101 and are increasingly used in youth-tailored tobacco interventions.102–104 At the individual level, efforts to exert control are central to empowerment; empowering processes often involve participation with others to achieve goals, efforts to gain access to resources, and opportunities to gain a critical understanding of one’s sociopolitical environment.99,105 Individual empowerment outcomes may include perceptions of personal control, a proactive approach to life, and a critical understanding of the sociopolitical environment.106
For SGM individuals, SGM-related activism, and community-building participation are linked to empowering outcomes, including experiences of more meaning in life, greater community connectedness (sense of community caring), coping resources that buffer negative consequences of minority stress, and overall positive psychological functioning.107 Minority Stress-guided80 research on SGM people shows that as levels of coping and social support increase, so does engagement in health-promoting lifestyles and decreased health risk behaviors.108 For SGM individuals who smoke, adaptive coping strategies,109,110 social support,110 smoking abstinence self-efficacy,111 and internalized SGM stigma112 may influence tobacco use and cessation behaviors, suggesting that empowerment activities may indirectly support tobacco cessation among SGM. When integrated with individual-level behavioral frameworks, such as those outlined above, empowering approaches to SGM-tailored tobacco interventions may be particularly effective in places with high levels of SGM stigma that exacerbate tobacco and other substance use inequities among SGM people.9 Hatzenbuehler and Pachankis, in particular, documented the impact of SGM stigma operating at multiple levels (eg, individual, structural) on SGM individuals’ tobacco and other substance use.4,5,9,97,113,114 For example, the presence or absence of state-level policies that provide equal opportunities for heterosexual and sexual minority individuals and the valence of state-aggregated attitudes toward sexual minority people interacts with gay-related rejection sensitivity to predict tobacco and alcohol use for young sexual minority men.9
Tobacco intervention efforts that aim to address tobacco-related inequities for SGM people are building momentum. Now is an opportune time to take stock and reflect on the constraints and capacities offered by the frameworks used thus far to design interventions, and to consider integrating the strengths of individual-level behavior change frameworks with those that can explain the phenomenon of tobacco use as situated within the social, political, and physical environments of minoritized people. This can lay the foundation for an empowerment-focused intervention—an approach that has not yet been developed or evaluated for SGM tobacco cessation, despite its adoption as an effective means of promoting health equity in other areas.100–103,115–119 Considering the limited success of previous SGM-tailored treatments that have been largely grounded in individual-level theories of behavior change, a foundational shift may be what is needed to move the field forward.
A final observation from these scoping review findings is the lack of focused targeting of nicotine-containing products other than combustible cigarettes in SGM-tailored tobacco interventions. SGM groups have high rates of poly-tobacco product use as well as dual use of nicotine-containing products with other substances (eg, cannabis, alcohol).120–124 Future intervention development should target multiple substance use among SGM groups and utilize frameworks that offer well-defined conceptualizations of multiple substance use practices.90,125–127
There are some limitations to the current scoping review. This review did not include non-peer-reviewed (gray) literature on SGM-tailored tobacco interventions which may include theoretical underpinnings not described in the peer-reviewed literature, nor did it provide a meta-analysis of intervention design and outcomes. As a larger number of robustly validated SGM-tailored intervention outcomes are reported in the peer-reviewed literature (eg, randomized control trials) future meta-analysis of intervention outcomes because of the low number of studies that would provide data suitable for such an analysis. This should include an assessment of the degree to which focusing on broader contextual-level factors rather than individual-level factors could be more effective for SGM tobacco prevention and cessation.
Conclusion
To conclude, at least two lessons may be gleaned from this scoping review of SGM-tailored tobacco prevention and cessation interventions: (1) The thinking that informs culturally tailored tobacco interventions for SGM people and other minoritized groups is currently driven almost exclusively by individual-level theories and (2) existing SGM-tailored interventions have had limited success in improving outcomes over non-tailored interventions. Future work to understand tobacco use inequities as indivisible from place, context, and policy may be useful for improving prevention and cessation outcomes. Working in partnership with SGM communities to address environmentally rooted drivers of SGM tobacco inequities, especially in places with high levels of SGM stigma, may be a way to enact positive change at the level of SGM individuals as well as their social and physical contexts.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Contributor Information
Julia McQuoid, Department of Family and Preventive Medicine and TSET Health Promotion Research Center, University of Oklahoma Health Sciences Center, 655 Research Parkway, Suite 400, Oklahoma City, OK, USA.
Arturo Durazo, Health Sciences Research Institute and Nicotine & Cannabis Policy Center, University of California, Merced, Merced, CA, USA.
Evan Mooney, Department of Family and Preventive Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA.
Jaimee L Heffner, Cancer Prevention Program, Public Health Sciences Division, Fred Hutchinson Cancer Center, Seattle, WA, USA.
Andy S L Tan, Annenberg School for Communication, University of Pennsylvania, Philadelphia, PA, USA.
Amanda Y Kong, Department of Family and Preventive Medicine and TSET Health Promotion Research Center, University of Oklahoma Health Sciences Center, 655 Research Parkway, Suite 400, Oklahoma City, OK, USA.
Shari Clifton, Health Sciences Library and Information Management, Graduate College, Robert M. Bird Health Sciences Library, University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA.
Elizabeth Horn, Freedom Oklahoma, Oklahoma City, OK, USA.
Funding
JM, AYK, and EM’s work on this manuscript was funded by the Oklahoma Tobacco Settlement Endowment Trust (TSET) Grant R23-12 and NCI Cancer Center Support Grant P30CA225520 awarded to the Stephenson Cancer Center.
Declaration of Interests
Dr. Heffner has received research support from Pfizer. Dr. Kong serves as a paid expert consultant in litigation against tobacco companies.
Author Contributions
JM conceived and planned the work and drafted the manuscript. The JM, SC, and EM conducted the scoping review by identifying and screening publications. JM, AD, EM, JLH, ASLT, AYK, and EH all provided input on decisions regarding how to describe and categorize the theories underpinning each intervention and reviewed the final manuscript.
(Note: References 100-127 are available as Supplementary Appendix B.)
References
- 1. Drope J, Liber AC, Cahn Z, et al. Who’s still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA Cancer J Clin. 2018;68(2):106–115. [DOI] [PubMed] [Google Scholar]
- 2. King BA, Dube SR, Tynan MA. Current tobacco use among adults in the United States: findings from the National Adult Tobacco Survey. Am J Public Health. 2012;102(11):e93–e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee JGL, Griffin GK, Melvin CL. Tobacco use among sexual minorities in the USA, 1987 to May 2007: a systematic review. Tob Control. 2009;18(4):275–282. [DOI] [PubMed] [Google Scholar]
- 4. Hatzenbuehler ML, Jun H-J, Corliss HL, Austin SB. Structural stigma and cigarette smoking in a prospective cohort study of sexual minority and heterosexual youth. Ann Behav Med. 2013;47(1):48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hatzenbuehler ML, Keyes KM, Hamilton A, Hasin DS. State-level tobacco environments and sexual orientation disparities in tobacco use and dependence in the USA. Tob Control. 2014;23(e2):e127–e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Soneji S, Knutzen KE, Tan ASL, et al. Online tobacco marketing among US adolescent sexual, gender, racial, and ethnic minorities. Addict Behav. 2019;95:189–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fallin A, Neilands TB, Jordan JW, Ling PM. Secondhand smoke exposure among young adult sexual minority bar and nightclub patrons. Am J Public Health. 2014;104(2):e148–e153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wintemberg J, McElroy JA, Ge B, Everett KD. Can smoke-free policies reduce tobacco use disparities of sexual and gender minorities in Missouri? Nicotine Tob Res. 2017;19(11):1308–1314. [DOI] [PubMed] [Google Scholar]
- 9. Pachankis JE, Hatzenbuehler ML, Starks TJ. The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Soc Sci Med. 2014;103:67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McQuoid J, Thrul J, Ozer E, Ramo D, Ling PM. Tobacco use in the sexual borderlands: the smoking contexts and practices of bisexual young adults. Health Place. 2019;58:102069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Antin TMJ, Hunt G, Sanders E. The “here and now” of youth: the meanings of smoking for sexual and gender minority youth. Harm Reduct J. 2018;15(1):30–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blosnich J, Lee JGL, Horn K. A systematic review of the aetiology of tobacco disparities for sexual minorities. Tob Control. 2013;22(2):66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bennett K, Ricks JM, Howell BM. “It’s just a way of fitting in:” tobacco use and the lived experience of lesbian, gay, and bisexual Appalachians. J Health Care Poor Underserved. 2014;25(4):1646–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gruskin EP, Byrne KM, Altschuler A, Dibble SL. Smoking it all away: influences of stress, negative emotions, and stigma on lesbian tobacco use. J LGBT Health Res. 2008;4(4):167–179. [DOI] [PubMed] [Google Scholar]
- 15. Youatt EJ, Johns MM, Pingel ES, Soler JH, Bauermeister JA. Exploring young adult sexual minority women’s perspectives on LGBTQ smoking. J LGBT Youth. 2015;12(3):323–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ylioja T, Cochran G, Woodford MR, Renn KA. Frequent experience of LGBQ microaggression on campus associated with smoking among sexual minority college students. Nicotine Tob Res. 2018;20(3):340–346. [DOI] [PubMed] [Google Scholar]
- 17. Livingston NA, Flentje A, Heck NC, Szalda-Petree A, Cochran BN. Ecological momentary assessment of daily discrimination experiences and nicotine, alcohol, and drug use among sexual and gender minority individuals. J Consult Clin Psychol. 2017;85(12):1131–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sanders E, Antin T, Hunt G, Young M. Is smoking queer? Implications of California tobacco denormalization strategies for queer current and former smokers. Deviant Behav. 2020;41(4):497–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Upson D, Reid C, Dakota R, et al. Exploring factors that influence tobacco use and cessation among Lesbian, gay, bisexual, transgender and queer youth in New Mexico. Am J Respir Crit Care Med. 2009;179:A3746. [Google Scholar]
- 20. Goebel K. Lesbian and gays face tobacco targeting. Tob Control. 1994;3(1):65–67. [Google Scholar]
- 21. Smith EA, Malone RE. The outing of Philip Morris: advertising tobacco to gay men. Am J Public Health. 2003;93(6):988–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Washington HA. Burning love: big tobacco takes aim at LGBT youths. Am J Public Health. 2002;92(7):1086–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stevens P, Carlson LM, Hinman JM. An analysis of tobacco industry marketing to lesbian, gay, bisexual, and transgender (lgbt) populations: strategies for mainstream tobacco control and prevention. Health Promot Pract. 2004;5(3_suppl):129S–34S. [DOI] [PubMed] [Google Scholar]
- 24. Smith EA, Thomson K, Offen N, Malone RE. “If you know you exist it’s just marketing poison”: meanings of tobacco industry targeting in the lesbian, gay, bisexual, and transgender community. Am J Public Health. 2008;98(6):996–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lee JG, Agnew-Brune CB, Clapp JA, Blosnich JR. Out smoking on the big screen: tobacco use in LGBT movies, 2000–2011. Tob Control. 2014;23(e2):e156–e158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Leibel K, Lee JGL, Goldstein AO, Ranney LM. Barring intervention? Lesbian and gay bars as an underutilized venue for tobacco interventions. Nicotine Tob Res. 2011;13(7):507–511. [DOI] [PubMed] [Google Scholar]
- 27. Valentine G, Skelton T. Finding oneself, losing oneself: the lesbian and gay “scene” as a paradoxical space. Int J Urban Reg Res. 2003;27(4):849–866. [Google Scholar]
- 28. Jannat-Khah DP, Dill LJ, Reynolds SA, Joseph MA. Stress, socializing, and other motivations for smoking among the lesbian, gay, bisexual, transgender, and queer community in New York City. Am J Health Promot. 2018;32(5):1178–1186. [DOI] [PubMed] [Google Scholar]
- 29. Remafedi G. Lesbian, gay, bisexual, and transgender youths: who smokes, and why? Nicotine Tob Res. 2007;9(Suppl_1):S65–S71. [DOI] [PubMed] [Google Scholar]
- 30. Burns EK, Deaton EA, Levinson AH. Rates and reasons: disparities in low intentions to use a state smoking cessation quitline. Am J Health Promot. 2011;25(5_suppl):S59–S65. [DOI] [PubMed] [Google Scholar]
- 31. Levinson AH, Hood N, Mahajan R, Russ R.. Smoking cessation treatment preferences, intentions, and behaviors among a large sample of Colorado gay, lesbian, bisexual, and transgendered smokers. Nicotine Tob Res. 2012;14(8):910–918. [DOI] [PubMed] [Google Scholar]
- 32. Schwappach DLB. Queer Quit: gay smokers’ perspectives on a culturally specific smoking cessation service. Health Expect. 2009;12(4):383–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schwappach DLB. Smoking behavior, intention to quit, and preferences toward cessation programs among gay men in Zurich, Switzerland. Nicotine Tob Res. 2008;10(12):1783–1787. [DOI] [PubMed] [Google Scholar]
- 34. Bruce Baskerville N, Wong K, Shuh A, et al. A qualitative study of tobacco interventions for LGBTQ+ youth and young adults: overarching themes and key learnings. BMC Public Health. 2018;18(1):155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ramo DE, Meacham M, Thrul J, Belohlavek A, Sarkar U, Humfleet G. Exploring identities and preferences for intervention among LGBTQ+ young adult smokers through online focus groups. J Adolesc Health. 2019;64(3):390–397. [DOI] [PubMed] [Google Scholar]
- 36. Lee JG, Matthews AK, McCullen CA, Melvin CL. Promotion of tobacco use cessation for lesbian, gay, bisexual, and transgender people: a systematic review. Am J Prev Med. 2014;47(6):823–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Berger I, Mooney-Somers J. Smoking cessation programs for Lesbian, gay, bisexual, transgender, and intersex people: a content-based systematic review. Nicotine Tob Res. 2017;19(12):1408–1417. [DOI] [PubMed] [Google Scholar]
- 38. Baskerville NB, Dash D, Shuh A, et al. Tobacco use cessation interventions for lesbian, gay, bisexual, transgender and queer youth and young adults: a scoping review. Prev Med Rep. 2017;6:53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Offen N, Smith EA, Gordon B. Early history of LGBT tobacco control: CLASH at 25. Tob Control. 2016;25(5):502–503. [DOI] [PubMed] [Google Scholar]
- 40. Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31(1):399–418. [DOI] [PubMed] [Google Scholar]
- 41. Glanz K, Rimer BK, Viswanath KEHBT.. Health Behavior: Theory, Research, and Practice. 5th ed. San Francisco: Jossey-Bass; Wiley; 2015. [Google Scholar]
- 42. Ammerman AS, Lindquist CH, Lohr KN, Hersey J. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: a review of the evidence. Prev Med. 2002;35(1):25–41. [DOI] [PubMed] [Google Scholar]
- 43. Legler J, Meissner HI, Coyne C, Breen N, Chollette V, Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiol Biomarkers Prev. 2002;11(1):59–71. [PubMed] [Google Scholar]
- 44. Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673–693. [DOI] [PubMed] [Google Scholar]
- 45. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–377. [DOI] [PubMed] [Google Scholar]
- 46. Sallis JF, Owen N, Fisher E. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, eds. Health Behavior: Theory, Research, and Practice. 5th ed. John Wiley & Sons; 2015:43–64. [Google Scholar]
- 47. Jefferson T, Alderson P, Wager E, Davidoff F. Effects of editorial peer review: a systematic review. JAMA. 2002;287(21):2784–2786. [DOI] [PubMed] [Google Scholar]
- 48. Kreuter MW, Lukwago SN, Bucholtz DC, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30(2):133–146. [DOI] [PubMed] [Google Scholar]
- 49. Matthews AK, Li CC, Kuhns LM, Tasker TB, Cesario JA. Results from a community-based smoking cessation treatment program for LGBT smokers. J Environ Public Health. 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dickson-Spillmann M, Sullivan R, Zahno B, Schaub MP. Queer quit: a pilot study of a smoking cessation programme tailored to gay men: Maria Dickson-Spillmann. Eur J Public Health 2014;24(suppl_2):cku161-058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Matthews AK, Conrad M, Kuhns L, Vargas M, King AC. Project Exhale: preliminary evaluation of a tailored smoking cessation treatment for HIV-positive African American smokers. AIDS Patient Care STDS. 2013;27(1):22–32. [DOI] [PubMed] [Google Scholar]
- 52. Fishbein M, Ajzen I.. Predicting and Changing Behavior: The Reasoned Action Approach. 1st ed. New York: Psychology Press; 2009. doi: 10.4324/9780203838020. [DOI] [Google Scholar]
- 53. Skurka C, Wheldon CW, Eng N. Targeted truth: an experiment testing the efficacy of counterindustry tobacco advertisements targeted to black individuals and sexual and gender minority individuals. Nicotine Tob Res. 2021;23(9):1542–1550. [DOI] [PubMed] [Google Scholar]
- 54. Eliason MJ, Dibble SL, Gordon R, Soliz GB. The Last Drag: an evaluation of an LGBT-specific smoking intervention. J Homosex. 2012;59(6):864–878. [DOI] [PubMed] [Google Scholar]
- 55. Matthews AK, McConnell EA, Li C-C, Vargas MC, King A. Design of a comparative effectiveness evaluation of a culturally tailored versus standard community-based smoking cessation treatment program for LGBT smokers. BMC Psychol. 2014;2(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Vogel EA, Ramo DE, Meacham MC, Prochaska JJ, Delucchi KL, Humfleet GL. The Put It Out Project (POP) Facebook intervention for young sexual and gender minority smokers: outcomes of a pilot, randomized, controlled trial. Nicotine Tob Res. 2020;22(9):1614–1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Vogel EA, Belohlavek A, Prochaska JJ, Ramo DE. Development and acceptability testing of a Facebook smoking cessation intervention for sexual and gender minority young adults. Internet Interv. 2019;15:87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Matthews AK, Steffen AD, Kuhns LM, et al. Evaluation of a randomized clinical trial comparing the effectiveness of a culturally targeted and nontargeted smoking cessation intervention for lesbian, gay, bisexual, and transgender smokers. Nicotine Tob Res. 2019;21(11):1506–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Walls NE, Wisneski H. Evaluation of smoking cessation classes for the lesbian, gay, bisexual, and transgender community. J Soc Serv Res. 2011;37(1):99–111. [Google Scholar]
- 60. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. [DOI] [PubMed] [Google Scholar]
- 61. Matthews AK, Hotton A, Aranda F, et al. Predictors of readiness to quit among a diverse sample of sexual minority male smokers. J Health Disparities Res Pract. 2014;7(5):9. [Google Scholar]
- 62. Bakan AB, Erci B. Comparison of the effect of trainings based on the transtheoretical model and the health belief model on nurses’ smoking cessation. Int J Caring Sci. 2018;11(1):213–224. [Google Scholar]
- 63. Heffner JL, Watson NL, Serfozo E, et al. An avatar-led digital smoking cessation program for sexual and gender minority young adults: intervention development and results of a single-arm pilot trial. JMIR Form Res. 2021;5(7):e30241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1–25. [DOI] [PubMed] [Google Scholar]
- 65. Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. [DOI] [PubMed] [Google Scholar]
- 66. Matthews AK, Breen E, Veluz-Wilkins A, et al. Adaptation of a proactive smoking cessation intervention to increase Tobacco Quitline Use by LGBT smokers. Prog Community Health Partnersh. 2019;13(5):71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Crankshaw E, Gaber J, Guillory J, et al. Final evaluation findings for this free life, a 3-year, multi-market tobacco public education campaign for gender and sexual minority young adults in the United States. Nicotine Tob Res. 2021;24(1):109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Guillory J, Crankshaw E, Farrelly MC, et al. LGBT young adults’ awareness of and receptivity to the This Free Life tobacco public education campaign. Tob Control. 2021;30(1):63–70. [DOI] [PubMed] [Google Scholar]
- 69. Navarro MA, Hoffman L, Crankshaw EC, Guillory J, Jacobs S. LGBT identity and its influence on perceived effectiveness of advertisements from a LGBT Tobacco Public Education Campaign. J Health Commun. 2019;24(5):469–481. [DOI] [PubMed] [Google Scholar]
- 70. Hinds JT, Chow S, Loukas A, Perry CL. Reactions to targeted tobacco control messaging: transgender and gender diverse young adult perspectives. Drug Alcohol Depend. 2021;218:108440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Beckerley S, Fernandez P, Matter C, Wagner D, Tate B, Jordan J. This free life campaign: increasing intention to quit among LGBTQ+ young adult nondaily smokers in Minneapolis. Tob Use Insights. 2022;15:1179173X221133978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Hersey JC, Niederdeppe J, Evans WD, et al. The theory of “truth”: How counterindustry campaigns affect smoking behavior among teens. Health Psychol. 2005;24(1):22–31. [DOI] [PubMed] [Google Scholar]
- 73. Pfau M, Parrott R.. Persuasive Communication Campaigns. Boston: Allyn and Bacon; 1993. [Google Scholar]
- 74. Fishbein M, Ajzen I.. Belief, Attitude, Intention, and Behavior. Reading, MA: Addison Wesley; 1975. [Google Scholar]
- 75. Brehm SS, Brehm JW.. Psychological Reactance: A Theory of Freedom and Control. New York: Academic Press; 1981. [Google Scholar]
- 76. Malone RE, Grundy Q, Bero LA. Tobacco industry denormalisation as a tobacco control intervention: a review. Tob Control. 2012;21(2):162–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Fallin A, Neilands TB, Jordan JW, Ling PM. Social branding to decrease Lesbian, gay, bisexual, and transgender young adult smoking. Nicotine Tob Res. 2015;17(8):983–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Plant A, Montoya JA, Tyree R, et al. The break up: evaluation of an anti-smoking educational campaign for Lesbians, gays, and bisexuals in Los Angeles County. J Health Commun. 2017;22(1):29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Rogers E. Diffusion of Innovations. 4th ed. New York: THE FREE PRESS; 1995. [Google Scholar]
- 80. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Caldwell KK, Staples AH, Bnadad L, Lee JG.. Promoting smoking cessation among Lesbian and bisexual women: lessons learned from a location-based media campaign in Western North Carolina. Health Promot Pract. 2022:15248399221083833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Vogel EA, Thrul J, Humfleet GL, Delucchi KL, Ramo DE. Smoking cessation intervention trial outcomes for sexual and gender minority young adults. Health Psychol. 2019;38(1):12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Burke NJ, Joseph G, Pasick RJ, Barker JC. Theorizing social context: rethinking behavioral theory. Health Educ Behav. 2009;36(5_suppl):55S–70S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Frohlich KL, Corin E, Potvin L. A theoretical proposal for the relationship between context and disease. Sociol Health Illn. 2001;23(6):776–797. [Google Scholar]
- 85. Barnett R, Moon G, Pearce J, et al. Smoking Geographies: Space, Place and Tobacco. Chichester, West Sussex: John Wiley & Sons; 2017. [Google Scholar]
- 86. Pearce J, Barnett R, Moon G. Sociospatial inequalities in health-related behaviours: pathways linking place and smoking. Prog Hum Geogr. 2012;36(1):3–24. [Google Scholar]
- 87. McQuoid J. Engaging with drug, set, and setting to understand nicotine use experiences and practices. In: Hunt G, Antin T, Frank VA, eds. Routledge Handbook of Intoxicants and Intoxication. London: Routledge; In Press. pp. 261–271. [Google Scholar]
- 88. Frohlich KL, Potvin L, Chabot P, Corin E. A theoretical and empirical analysis of context: neighbourhoods, smoking and youth. Soc Sci Med. 2002;54(9):1401–1417. [DOI] [PubMed] [Google Scholar]
- 89. Poland B, Frohlich K, Haines RJ, Mykhalovskiy E, Rock M, Sparks R. The social context of smoking: the next frontier in tobacco control? Tob Control. 2006;15(1):59–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Blue S, Shove E, Carmona C, Kelly MP. Theories of practice and public health: understanding (un) healthy practices. Crit Public Health. 2016;26(1):36–50. [Google Scholar]
- 91. Salihu HM, Wilson RE, King LM, Marty PJ, Whiteman VE. Socio-ecological model as a framework for overcoming barriers and challenges in randomized control trials in minority and underserved communities. Int J MCH AIDS. 2015;3(1):85–95. [PMC free article] [PubMed] [Google Scholar]
- 92. Davies ME. Developing community resilience through grassroot initiatives: comparing culturally adapted substance use prevention programs directed towards indigenous youth in Canada. Indonesia J Soc Sci. 2022;5(2):687–703. [Google Scholar]
- 93. Han G, Son H. A systematic review of socio-ecological factors influencing current e-cigarette use among adolescents and young adults. Addict Behav. 2022;135:107425. [DOI] [PubMed] [Google Scholar]
- 94. Poland B, Frohlich KL, Cargo M. Context as a fundamental dimension of health promotion program evaluation. In: Potvin L, McQueen DV, Hall M, de Salazar L, Anderson LM, Hartz ZM, eds. Health Promotion Evaluation Practices in the Americas. New York, NY: Springer; 2008:299–317. 10.1007/978-0-387-79733-5_17. [DOI] [Google Scholar]
- 95. Williams RD Jr, Housman JM, McDonald JD. If we build it, will they come? Challenges of adapting and implementing a smoking cessation program for the LGBTQ community in Southcentral Texas. Health Promot Pract. 2020;21(1_suppl):118S–123S. [DOI] [PubMed] [Google Scholar]
- 96. Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Hatzenbuehler ML, Jun HJ, Corliss HL, Austin SB. Structural stigma and cigarette smoking in a prospective cohort study of sexual minority and heterosexual youth. Ann Behav Med. 2014;47(1):48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Spivey JD, Lee JGL, Smallwood SW. Tobacco policies and alcohol sponsorship at lesbian, gay, bisexual, and transgender pride festivals: time for intervention. Am J Public Health. 2018;108(2):187–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Perkins DD, Zimmerman MA. Empowerment theory, research, and application. Am J Community Psychol. 1995;23(5):569–579. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.