Abstract
Background and Purpose
Interventions are effective in promoting health behavior change to the extent that (a) intervention strategies modify targets (i.e., mechanisms of action), and (b) modifying targets leads to changes in behavior. To complement taxonomies that characterize the variety of strategies used in behavioral interventions, we outline a new principle that specifies how strategies modify targets and thereby promote behavior change. We distinguish two dimensions of targets—value (positive vs. negative) and accessibility (activation level)—and show that intervention strategies operate either by altering the value of what people think, feel, or want (target change) or by heightening the accessibility of behavior-related thoughts, feelings, and goals (target activation).
Methods and Results
We review strategies designed to promote target activation and find that nudges, cue-reminders, goal priming, the question-behavior effect, and if-then planning are each effective in generating health behavior change, and that their effectiveness accrues from heightened accessibility of relevant targets. We also identify several other strategies that may operate, at least in part, via target activation (e.g., self-monitoring, message framing, anticipated regret inductions, and habits).
Conclusions
The Activation Vs. Change Principle (AVCP) offers a theoretically grounded and parsimonious means of distinguishing among intervention strategies. By focusing on how strategies modify targets, the AVCP can aid interventionists in deciding which intervention strategies to deploy and how to combine different strategies in behavioral trials. We outline a research agenda that could serve to further enhance the design and delivery of interventions to promote target activation.
Keywords: Health behavior change, Interventions, Strategies, Techniques, Taxonomy, Theory
Intervention strategies promote health behaviors by changing people’s minds (i.e., modifying what people think, feel, or want) or by cueing people’s minds to change (i.e., activating cognitions, affect, or goals).
To meet the public health goals specified nationally [1] and globally [2], there is a growing demand for health behavior interventions that are effective and efficient and can be taken to scale. Strategies are needed that can increase vaccination rates, reduce the onset of tobacco use, and help people initiate and maintain healthy patterns of eating and physical activity, to name but a few vexing challenges. Within the toolbox of behavior change strategies, investigators could, for instance, choose to distribute messages that instill confidence about engaging in a new pattern of behavior, post graphic images that illustrate the consequences of not taking action, modify the context in which the behavior is enacted, provide prompts that link the opportunity and the intention to act, or offer incentives that reinforce a new behavior. A number of efforts have been made to organize and label available strategies [3–7]. These typologies emphasize the content of different strategies, focusing on what the intervention strategy is comprised of and how the strategy is instantiated (e.g., provide information vs. encouragement vs. instruction; prompt intention formation vs. self-monitoring; alter position, presentation, or size of stimuli), and the dimensions that characterize these contents (e.g., scheduled vs. natural consequences [7]; properties vs. placement of stimuli [5]; self- vs. other-deployed [4, 6]). These typologies help to specify the scope of strategies available and enable clear communication about which strategies have been used to promote behavior change. However, in deciding which strategies to use in an intervention, investigators will want to know not only what each strategy is (i.e., what tools are in the toolbox) but also how each strategy operates (i.e., what each tool is designed to do). What do strategies do to promote behavior change?
Intervention strategies are effective to the extent that they engage a target that, in turn, elicits changes in behavior [8, 9]. Targets are typically psychological constructs that serve as the mechanism(s) of action and explain the impact of intervention strategies on behavior change. For instance, feedback strategies can promote exercise performance by increasing self-efficacy (i.e., self-efficacy is a target of the strategy [10];). Given the critical link between intervention strategies and targets, there is growing interest in organizing intervention strategies not only in terms of their content but also with respect to the targets they can be designed to engage. Ongoing efforts such as the Human Behavior Change Project (www.humanbehaviourchange.org) [11, 12] and the Science of Behavior Change program (www.scienceofbehaviorchange.org) [9] have generally focused on mapping which targets a strategy engages to promote behavior change (e.g., risk perceptions, attitudes, self-efficacy). Here we expand on this approach to consider what feature of the target the intervention strategy engages, or how the strategy modifies the target. We distinguish two features of targets: Strategies can promote health behaviors by altering the value of what people think, feel, or want (target change) or by altering the degree to which the relevant thought, feeling, or goal comes to mind (target activation).
To see this distinction, imagine that intervention strategies were needed to increase regular handwashing to prevent infection with a novel virus and perceived risk of infection was identified as a key target for intervention. What needs to be done to the target (i.e., perceived risk) to promote behavior change? Do we need to increase people’s perception of risk (i.e., change the value of what people think and feel about the possibility of infection) or do we need to bring the risk perceptions they already hold to mind at critical junctures (i.e., activate what people already think and feel about the possibility of infection)? If the former is the case, investigators might develop a persuasive message regarding the relevant risk factors, whereas if the latter is the case, investigators might rely on a brief image in a suitable location that can serve as a reminder. Both of these strategies are designed to engage the same target (risk perceptions); they differ in what the respective strategy does to the target (i.e., change risk perception vs. activate risk perception). We propose that target activation vs target change can serve as a key organizing principle underlying intervention strategies. This principle is focused on what intervention strategies are designed to do to targets (i.e., activate vs. change), and thus can provide investigators with a taxonomy that illuminates when and why particular intervention strategies warrant implementing, rather than what the strategy involves or how it is implemented (e.g., brief vs. intensive interventions, in-person vs. online delivery).
Unpacking Target Engagement: Modification of Different Dimensions of Targets
Mechanistic approaches to the design and evaluation of behavior change interventions [8, 9, 13–15] have emphasized that the effectiveness of an intervention strategy rests on two underlying processes: an intervention strategy’s ability to modify the hypothesized mechanisms of action and the ability of these mechanisms to affect change in behavior. Target engagement is the process of modifying specified targets using particular intervention strategies. But what does it mean to modify a target? Our intuitive conception of “changing people’s minds” and the fact that targets typically are measured via self-reports suggest that target change involves increasing or decreasing scores on the relevant dimension. That is, change refers to modifying the value of targets such that participants who receive the intervention have, for example, more favorable attitudes, more supportive norms, higher self-efficacy, and stronger intentions compared to control participants. Target engagement in this analysis involves maximizing the value of targets (their direction and intensity) to support healthful choices and energize behavior change.
Value is but one feature of a target that can be modified, however. Even extremely positive attitudes and intentions may not be acted upon unless these targets are accessible in working memory (i.e., activated) when the opportunity to initiate the behavior arises. The frequency and recency with which a target is activated determine target accessibility (how quickly the relevant target is retrieved from memory) and its impact on subsequent behavior [16]. The cognitive architecture supporting this activation process is described in models of semantic memory (see ref [17] for review). For instance, in spreading activation models, concepts are represented by localized nodes, and relations between these nodes are stored in network links. Exposure to a cue retrieves a concept from memory, activating its internal representation, which, in turn, spreads to associated concepts; the residual activation facilitates subsequent retrieval of the concept. Activating concepts also leads to a decreased hemodynamic response in neuroimaging studies; with the specific brain regions that are implicated depending upon the type of stimulus and how the stimulus is processed (see refs [18, 19] for reviews).
The idea that value and accessibility are separable features of targets is consistent with Fazio’s MODE model [20]. According to this model, how well attitudes predict behavior depends on both the value of the attitude (how favorable is the person’s evaluation of the behavior), and the accessibility of that evaluation. Attitude accessibility is typically measured by response latencies to attitude questions; the faster participants respond, the more activated is the relevant evaluation in working memory. When an attitude towards a behavior is both favorable and accessible, then behavioral performance is likely, whereas performance is less likely when the attitude is unfavorable or accessibility is low. This prediction is supported by meta-analyses of both observational studies that measured attitude accessibility [21] and experiments that manipulated attitude accessibility [22]. Value and accessibility are not only features of attitudes but also characterize the variety of thoughts, feelings, and goals that form targets for behavior change strategies [21, 23, 24].
Figure 1 indicates how intervention strategies influence value and accessibility as separate features of target change. Strategies can modify target value (Strategy A in Fig. 1) or they can modify target accessibility (Strategy B in Fig. 1) and different intervention strategies may be better suited to modifying value vs heightening accessibility. For instance, consider the following five targets that are specified by multiple health behavior theories: risk perceptions, attitudes, norms, self-efficacy, and intentions [8]. For each of these targets, experimental evidence has shown that when interventions are able to increase scores on these constructs (i.e., modify their value), these changes lead to changes in health behaviors [25–27]. In the case of risk perceptions, interventions that offer visual feedback appear to increase the value of this target among smokers [28]. Yet, placing graphic warnings on cigarette packs does not modify the valence or value of smokers’ risk perceptions for adverse outcomes [29] but rather increases the accessibility of the risk perceptions smokers already hold (see ref [23]., Study 1). A recent trial of graphic pack warnings observed significant increases in smoking restraint over the course of the intervention but no change in the level of risk perceptions. Consistent with the idea that pack warnings activate pre-existing risk perceptions, perceived risk measured at the outset of the study predicted subsequent restraint among participants who had health warnings on their packs whereas no such associations were observed for controls. Repeatedly encountering pack warnings didn’t change how smokers perceived the risks posed by smoking but did render those perceptions more powerful predictors of behavior (ref [23]., Study 2).
Fig. 1.
Intervention strategies can modify two dimensions of targets: value or accessibility.
Different strategies also appear to be effective in modifying the value vs. accessibility of attitudes, norms, self-efficacy, and intentions. Whereas persuasive communications proved effective in changing the favorability of dietary attitudes [30], an intervention that involved merely completing a survey about diet (vs. no survey) increased the accessibility of pre-existing dietary attitudes and led to changes in eating behavior (question-behavior effect [31];). A social influence intervention that “promoted modeling by informal leaders at the wards and … setting norms” (p. 467) led to improved rates of hand hygiene among nurses [32]. However, merely placing an image of two male eyes over a gel dispenser (thereby activating injunctive norms about hand hygiene) almost doubled hand hygiene rates in a hospital setting [33]. Providing vicarious mastery experiences (e.g., the opportunity to observe others successfully perform the behavior) increases people’s ratings of their self-efficacy [34] and, in turn, their behavior [26], but behavior change can also accrue from activating perceptions of self-efficacy when they are needed—by forming an if-then plan to “ignore my worries and tell myself: I can do it!” at a critical juncture during a test [35]. Finally, various strategies have proven effective in strengthening health-related behavioral intentions [27]. However, as research on prospective memory has shown, “forgetting of intentions in demanding situations is rapid” (ref [36], p. 147). Intervention strategies designed to activate intentions in situ, such as phone call reminders of intentions to take antiretroviral medication [37] or if-then plans to remember one’s dieting goal among restrained eaters [38], have proven effective in changing health behaviors, without the need to change the value of participants’ intentions. In sum, target engagement involves more than the colloquial, “changing people’s minds;” thoughts, feelings, and goals that favor health behavior performance must also be activated at the opportune moment. Value and accessibility are discriminable dimensions of target change and different intervention strategies may be suited to changing vs. activating targets.
Behavioral Medicine’s Toolbox of Strategies to Promote Target Engagement
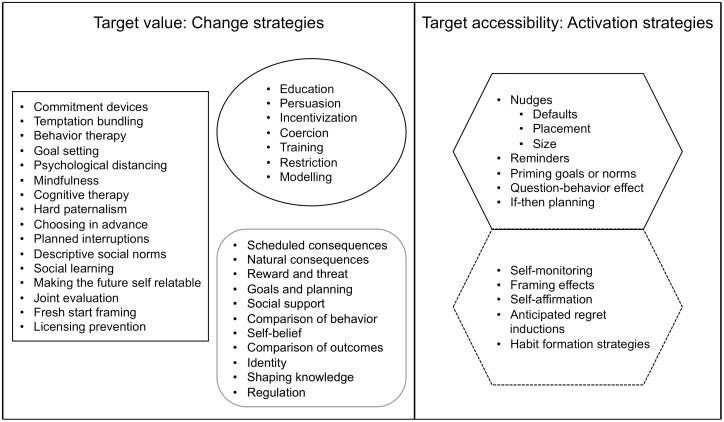
Figure 2 offers an overview of intervention strategies that have been identified in prior typologies but differentiates between strategies that focus on target change and those that focus on target activation. Change strategies (left panel) come from three, partially overlapping, typologies: Duckworth et al.’s analysis of strategies to reduce self-control failures [39], Michie et al.’s Behavior Change Wheel [40], and Michie et al.’s Behavior Change Techniques Taxonomy (BCTTv1 [7];). Each of these change strategies is designed to modify either the desirability of an outcome (e.g., commitment devices, temptation bundling, hard paternalism, persuasion, incentivization, coercion, scheduled and natural consequences, reward, and threat) or the feasibility of acting (e.g., behavior therapy, social learning, licensing prevention, modeling, social support, regulation). As target change has been the prevailing approach to specifying and testing behavioral interventions, an analysis of these strategies is not the focus of the present paper. There are numerous reviews of intervention strategies designed to change target value [34, 41, 42] as well as meta-analytic evidence that experimentally elicited changes in the value of constructs such as attitudes, norms, self-efficacy, risk perceptions, and intentions lead to changes in behavior of meaningful magnitude (ds = 0.38, 0.36, 0.47, 0.25, and 0.36, respectively; refs [25–27]).
Fig. 2.
Intervention strategies modify the value or accessibility of targets via change or activation strategies. Note. Change strategies are from Duckworth et al. (2019) [right-angled rectangle], The Behavior Change Wheel (Michie et al., 2011) [oval] and the Behavior Change Technique Taxonomy (v1) (Michie et al., 2013) [rounded rectangle]. Activation strategies [solid and dotted hexagons] come from Duckworth et al. (2019), Michie et al. (2011, 2013), the TIPPME taxonomy (Hollands et al., 2017), and reviews of specific strategies (Finitsis et al., 2014; Gollwitzer & Sheeran, 2006; Harkin et al., 2016; Papies, 2016; Wilding et al., 2016).
The activation strategies in Fig. 2 (right panel) were extracted from the Duckworth and Michie taxonomies or from the TIPPME taxonomy [5] as well as reviews of specific strategies [37, 43–46]. In each case, the strategy is thought to operate by modifying the accessibility of people’s behavior-related thoughts, feelings, or goals. We focus here on synthesizing strategies that researchers in behavioral medicine can use to activate targets and to illustrate how seemingly different intervention strategies are united by a focus on modifying target accessibility. Below, we illustrate the effectiveness of these strategies in promoting health behavior change and outline evidence indicating that target activation forms the mechanism of action in each case.
Setting defaults.
Thaler and Sunstein [47] defined nudges as “simple changes in the presentation of choice alternatives that make the desired choice the easy, automatic or default choice.” Defaults are a type of nudge that involves setting a course of action that will unfold unless the person actively chooses otherwise. One classic default study concerned opting in vs. opting out of registering as an organ donor [48]. When registration was the default and people had to opt out of becoming a donor, registration rates were dramatically higher compared to a condition wherein participants had to opt-in to become a donor. Setting defaults also has positive effects on flu vaccination [49], use of sit-stand desks [50], and vegetable consumption [51]. Meta-analysis showed an effect of d+ = 0.68 across k = 58 tests of default interventions [52].
Although defaults and other nudges have been widely used, surprisingly little research has examined their underlying mechanisms of action [53]. The most compelling account to date comes from Suri and colleagues [54, 55]. In a behavioral experiment that involved viewing one of two images, Suri and Gross [54] observed the classic default effect: Participants chose to view an aversive, default image on 71% of trials even though debriefing indicated that 100% of participants knew they could have switched to viewing a neutral image and pilot research indicated that participants overwhelmingly preferred the neutral image to the aversive default. However, when a red border was placed around the neutral image option, participants selected that option on 50% of trials.
Why did the red border attenuate the default effect? In Higgin’s [56] classic treatment of the concepts of salience, attention, and knowledge activation, salience is construed as a feature of the stimulus and the sequence is as follows: “Salience … impact[s] subsequent responses by influencing which features of a stimulus event receive attention, and this in turn will influence which stored knowledge units are likely to be activated in the immediate situation” (p. 158). In line with this account, neither salience nor attention are the proximal mechanisms of switching vs. default behavior but rather it is the particular knowledge units that are activated by the red border. Simulations of Suri and Gross’s findings [57] based on the Interactive Activation and Competition (IAC; ref [55]) model indicated that these knowledge units concerned the switch option and the relation between the switch option and the relevant action unit (pressing the button to switch images) – the red border activated the opportunity to switch which, in turn, activated the relevant behavioral schemata and led to the observed shift in participants’ choices [55]. Thus, setting defaults appears to modify behavior, not by altering the value of the different options, but by failing to activate alternatives to the pre-set option.
Altering stimulus position.
Research on position has predominantly focused on food choice and finds that “foods that are more proximate, or closer to the individual, are consumed in greater quantities” (ref [58], p. 175). For instance, placing healthy foods near the cash register increased the purchase of those foods [59], whereas placing unhealthy snacks further away from participants reduced consumption [60] (see refs [61, 62] for systematic reviews). Although there appears to be no direct test of the mechanisms underlying the proximity effect, there is evidence consistent with an activation-based explanation. First, how much fruit and chocolate “looked irresistible” influenced consumption in a study that varied the proximity of these food items, whereas perceived effort to obtain the food items was not [63]. Second, the proximity effect is not influenced by the availability of cognitive resources [64] which might be expected if effortful, evaluative processing was involved. Third, Garnet et al [65]. observed that placing healthy options near the cafeteria entrance increased the selection of a healthy meal, but only when this was the sole option that could activate relevant eating goals (i.e., when alternative meal options were placed at least 1.5 m away). When the more vs. less healthy options were close together (< 1 m) and competing goals could be activated by the different options, the proximity effect disappeared.
Manipulating stimulus size
Perhaps the most extensively researched size nudge is the “portion-size effect” (PSE [66];), in which the amount people eat is shaped by the amount they are given to eat in a sitting. One meta-analysis estimated that a 100% increase in portion size leads to a 35% increase in consumption (d+ = 0.45, k = 88 [67]). Importantly, people fail to compensate later for excess consumption due to larger portion sizes. Marchiori et al. [67] argued that the implicit activation of an exaggerated norm or reference point in situ underlies the PSE; this activated norm then serves as an anchor that people fail to adjust for (cf. ref [68]). The idea is that the proffered portion size doesn’t change people’s general standards of how much food it is appropriate to eat (i.e., no target change), but, rather, it generates an accessible norm (i.e., target activation). Consistent with this analysis, Machiori et al. observed that activating a large portion norm led to greater estimated consumption, and activating a small portion norm reduced estimated consumption, compared to a control condition where a norm was not activated (see also ref [69]).
Providing cue-reminders.
One frequently adduced reason for failing to perform health behaviors (e.g., take prescribed medication, get vaccinated) is “forgetting” [43]. Accordingly, multiple trials have tested cue-reminders (e.g., computer prompts, text messages, signs, bracelets) as strategies to activate goals and promote health behavior performance. Meta-analyses indicate that cue-reminders are effective for a variety of behaviors (e.g., alcohol consumption, diet, adherence to treatment; vaccinations) and samples (community members, patients, and healthcare providers) [37, 70–72](d+ = 0.32, k = 6 [71];). Classic research in cognitive psychology explains these cue-reminder effects in terms of a feature of prospective memory termed “goal neglect” [73]. Duncan et al [73]. observed that almost one-fifth of their healthy participants did not follow a key requirement on a computerized task despite (a) understanding the task requirement, and (b) reporting afterwards that they could identify when the appropriate moment to act had occurred: “The data suggest that … the process of goal activation fails in some subjects... the relevant task requirement ‘slips the subject’s mind.’” However, “as soon as a verbal prompt was given … complete neglect was often replaced with almost immediate and complete success” (p. 274). Thus, cue-reminders promote intention realization not because they increase the value of the intention to act, but rather because the intention is activated at the critical juncture.
Health goal activation.
Incidental features of the environment have been shown to affect behavior through the unobtrusive activation of mental representations (e.g., goals, norms; see ref [24]). The relevance of activating mental representations in efforts to change health behaviors was demonstrated in seminal studies by Papies et al. [74–76]. Environmental cues designed to prime the goal of weight control (e.g., a poster in a shop doorway, a flyer for a low-fat recipe, mention of low-calorie options on a menu, presence of dieting magazines) were shown to influence eating behavior, even though the relevant cues were incidental and unobtrusive. Similar effects have been obtained for other behaviors including hand hygiene [33] and physical activity [24] (see refs [44, 77] for reviews). In a meta-analysis, d+ was .41 across k = 15 tests of health priming [78]. Because the environmental cues relate to goals that people already hold [79], they are understood to operate through the activation of people’s pre-existing goals [44].
The question-behavior effect strategy.
The question-behavior effect (QBE) is the phenomenon whereby randomizing participants to answer questions about a behavior (e.g., intentions or attitudes) leads to increased performance of that behavior compared to participants who were not asked those questions. The QBE has been used to improve rates of vaccination [80], blood donation [81, 82], and colorectal cancer screening [83] and has been observed to both increase health-protective behaviors and reduce health-risk behaviors [46]. A meta-analysis of 94 tests showed an effect size of d+ = 0.14 [84]. How does answering a set of survey questions affect people’s behavior? Research has shown that completing the survey does not change the favorability of participants’ attitudes, norms, or intentions concerning the behavior [85]; but rather activates either people’s attitudes towards the behavior [31] or a personal or social norm that potentiates dissonance about not performing the behavior [46].
If-then planning.
If-then plans or implementation intentions [43, 86] are an established tool for managing obstacles that threaten the performance of health behaviors (e.g., forgetting to act, falling prey to unwanted thoughts and feelings). If-then plans are so-named because they have the format, If [opportunity/obstacle] occurs, then I will [respond in this way]! If-then planning has proven effective in promoting medication adherence [87], physical activity [88], teen pregnancy prevention [89], and cancer screening [90] among many other health behaviors. In a meta-analysis of meta-analyses of implementation intention interventions, d+ was .54 [91]. If-then plans operate not by changing the favorability of people’s intentions to act, but by increasing the accessibility of two targets [92]. First, the opportunity or obstacle specified in the if-part of the plan becomes highly activated [92, 93] which means people can quickly and accurately detect their moment to act [94]. Second, the specified opportunity/obstacle activates the response spelled out in the then-part of the plan [92, 93]. The development of a strong association between the cue (in the if-part of the plan) and response (in the plan’s then-part) means that the response is initiated swiftly and effortlessly when the cue is encountered [43], and rates of performance of health behaviors are thereby enhanced [91].
Other intervention strategies that appear to involve target change may rely on target activation.
Several prominent intervention strategies including self-monitoring, framing effects, anticipated regret inductions, and habit formation, may also operate wholly or in part through target activation (see the dotted hexagon in Fig. 2). However, the manner in which, and the evidence about how, target activation operates through these strategies are less well-developed. Self-monitoring strategies are designed to bring discrepancies between actual and desired patterns of health behavior to mind [45]. However, discrepancies on their own do not appear to motivate behavioral responses; rather, discrepancies only lead to instrumental action when the relevant goal is accessible [95].
There is a large literature on the impact of health message framing on behavior (see refs [96, 97] for reviews). Although message framing may alter the value of risk perceptions or attitudes and thereby affect behavior, target accessibility may be needed to explain how framing generates such changes in risk perceptions and attitudes. For instance, a prominent explanation of framing effects is “accessibility bias” [98] which proposes that framing alters the accessibility of different considerations (e.g., losses vs. gains, utility vs. pleasure) and exerts a predictable influence on attitudes, decisions, and actions. From this perspective, message framing may alter behavior at least in part by activating a subset of people’s thoughts and feelings about a behavior rather than changing those targets.
Anticipated regret inductions (see ref [99] for meta-analysis)—that invite people to consider how much they would regret it if they failed to perform a health behavior—do not change the degree to which people feel regret but rather activate consideration of regret at the critical moment. For instance, Abraham and Sheeran [100] randomized participants either to report how much they would regret not exercising and then indicate their exercise intentions, or to report their exercise intentions and then rate their anticipated regret. Even though participants anticipated the same level of regret in both conditions, activating anticipated regret prior to intention formation led to stronger intentions to exercise. Finally, although self-reported habit strength could seem to involve value, habits are associations in memory between particular cues (e.g., times, places, people) and behavioral responses [101]. Encountering the cue activates its mental representation which, in turn, activates the representation of behavior via the process of spreading activation. The strength of the mental associations underlying habits is thus a function of how quickly the cue activates the relevant response due to repeated and consistent execution of responses to the cue in the past [102]. Habit-based interventions have proven effective at improving diet [103] and exercise [104], and may be especially valuable for promoting the maintenance of new behaviors [105].
One key reason why it is difficult to specify whether the accessibility or value of targets underlies how a strategy affects behavior is that randomized trials typically include measures of target value (e.g., self-report scales), but rarely include the indices needed to measure target accessibility (e.g., reaction times). Thus, intervention strategies could have changed and activated targets in many trials, but measurement practices meant that variation in target accessibility was missed. Given that most assessments are now conducted online, and software can record both the speed and value of responses, future studies should endeavor to determine whether the shift in target accessibility, target value, or synergy between these target dimensions explains the impact of intervention strategies on health behavior change.
The Role of Target Activation in Health-Risk Behavior
Whereas discussion has so far focused on intervention strategies that behavioral medicine researchers and practitioners could use to promote health behaviors, it is important to acknowledge that target activation is also relevant to understanding the performance of unhealthy behaviors. Many of the factors that promote unhealthy behavior operate by activating thoughts, feelings, or goals that favor these behaviors. For example, Harris et al. [106] showed that food advertising can directly prime food consumption. Exposure to snack food ads increased snack consumption in both adults and children (by 45%) even though the available snacks were not the same as those advertised. Importantly, consumption was “not related to reported hunger or other conscious influences” (p. 404). Other research has observed similar effects on alcohol consumption [107, 108] and demonstrated that exposure to “anti-smoking” public service announcements (PSAs) sponsored by the tobacco industry actually elicited smoking behavior, unlike a PSA from a nonprofit tobacco control organization [109].
The implication is that behavioral medicine researchers should not only make use of target activation strategies to promote health-protective behaviors but also develop and use strategies that can counter the target activation strategies that engender health risks. Several strategies could be useful in this regard, including imposing restrictions on the availability of unhealthy products through bans or other regulations, counter-marketing, and if-then planning. He et al [110]. analyzed data from 77 countries and estimated that banning point-of-sale displays for tobacco products led to a reduction in adult daily smoking of ~7%. Counter-marketing campaigns involve “exposing motives and undermining marketing practices of producers” to reduce demand for tobacco, alcohol, and unhealthy food (ref [111], p. 119). For instance, teaching 8th graders to construe healthy eating as a way to “stick it to the man” led to a 9% reduction in the sugar content of food choices [112]. Finally, if it is not feasible to implement restrictive regulation or counter-marketing strategies, if-then planning has proven effective in abolishing the impact of activation strategies on health behaviors [113, 114].
Intervention Strategies May Engage Multiple Targets or Target Dimensions
Although different intervention strategies appear to be effective in promoting changes in target activation and target value, intervention strategies need not necessarily engage just one target or target dimension. For instance, mental contrasting [115] is an imagery exercise that involves juxtaposing the desired outcomes of performing health behaviors and obstacles that stand in the way of performance and has proven effective in promoting health behaviors (see ref [116] for a meta-analysis). One study with sedentary, low-income men observed that writing about, first, the best outcomes of increased activity and, second, the biggest obstacle standing in one’s way led to increased physical activity over 6 months [117]. Mental contrasting engenders shifts in both target value (e.g., increased energization, more negative evaluation of obstacles, enhanced goal commitment) and target activation (e.g., increased accessibility of desired outcomes, desired outcomes prime obstacles, and obstacles prime means to overcome obstacles) (see ref [118] for a review of mechanisms underlying mental contrasting). Thus, while we have focused on intervention strategies with relatively discreet targets and target dimensions in Fig. 1, it is important to recognize that certain strategies could be powerful precisely because they engage multiple targets and target dimensions.
Implications of Distinguishing Target Activation vs. Target Change
Identifying activation vs. change as a key principle underlying strategies to promote health behavior change has implications for both the conceptualization and conduct of behavioral medicine interventions. First, categorizing strategies based on how they engage targets provides a parsimonious conceptual structure for the myriad change techniques that are available. This structure complements previous taxonomies [5, 7, 40] that focused on classifying the content of different strategies (e.g., scheduled vs. natural consequences; altering properties vs. placement of stimuli), and can easily accommodate the inclusion of new and emerging intervention strategies.
Second, the Activation Vs. Change Principle (AVCP) offers a basis for categorizing intervention strategies grounded on strategies’ mechanism of action. The AVCP embraces the importance of target engagement for promoting behavior change but extends this analysis to encompass two distinct dimensions of targets that strategies can engage—value and accessibility. Doing so highlights the fact that initiatives to address behavioral problems sometimes require people to change what they think and feel and other times require people to call to mind the thoughts and feelings they already hold. The premise that target activation underlies the effectiveness of certain intervention strategies builds on evidence from decades of research in social and cognitive psychology on the importance of concept accessibility [16, 20]. Organizing strategies in terms of their underlying mechanism of action also renders visible similarities between intervention strategies that initially seem very different. For instance, risk communications and incentives focus on the level of disease threat and the value of the preventive behavior, respectively, but both strategies can be used to strengthen intentions to take one’s medication (i.e., to promote target change). People could form if-then plans long before they are prescribed medication or telephone reminders could be initiated at the precise moment that medication should be taken, but if-then planning and cue-reminders can both be used to activate medication intentions at the critical juncture. Activation vs. change thus offers a principled way to demarcate intervention strategies—based on their action on targets rather on conceptual similarities or where, when, how, for how long, or by whom they are delivered.
Third, distinguishing between target activation and target change strategies can also support interventionists as they make decisions about which strategies to deploy. The AVCP foregrounds the question, does the intervention need to change people’s minds or cue people’s minds? Too often, interventions are predicated on the default assumption that the value of people’s thoughts, feelings, and goals needs to be increased when scores on these constructs may already strongly favor the behavioral performance [87, 90]. The starting point for intervention development should thus involve consideration of the behavior-relevant thoughts, feelings, and goals of the focal sample, rather than top-down selection from a menu of strategies. If participants already are motivated and able to perform a behavior, then the issue may be what target needs to be activated to secure the behavioral performance—is goal neglect the problem, or does the person need to be able to respond more quickly and effectively to obstacles? If goal neglect is the problem, then interventionists could deploy a nudge, cue-reminder, or the question-behavior effect. If handling obstacles is the issue, then if-then plans should be a helpful strategy [43]. However, if participants lack motivation or ability, then these targets will first need to be changed. Nudges, if-then plans, or other target activation strategies will not be effective if the value of these targets does not favor performing the behavior [119, 120]. To engage motivation, interventionists will need to consider what are the targets antecedent to motivation that should be changed (e.g., risk perceptions, attitudes, norms) and consider what features of ability (e.g., resources, opportunities, co-operation, skills, self-efficacy) form the target in order to engage ability. Thus, the AVCP implies that identifying the target and target dimension that need to be engaged is the crucial first step for intervention development; the selection of the intervention strategy follows from that step, informed by how effectively and efficiently the strategy can modify the target in relation to the focal sample and behavior.
The AVCP also has implications for combining intervention strategies. If people are failing to act despite being motivated and able to do so, then investing in target change could waste resources that would be better spent on target activation strategies. Relatedly, investment in target activation would be wasteful if people are not motivated to perform the behavior to begin with. However, in the case of samples with low motivation and ability, it could be worthwhile to invest in efforts that promote both target change and target activation—to ensure that changes to these targets are activated at the critical moment and become translated effectively into action. The AVCP thus suggests that strategies that engage different dimensions of the same target could prove effective. For instance, persuasive communications that change eating goals (e.g., “One meat-free day a week is good for your health because ….”) that are accompanied by signs that activate this eating goal in restaurants or stores (“Is today your meat-free day?”) could be more effective than either the persuasive communication or sign on its own. It is also possible that one target needs to be changed (e.g., an increase in motivation) but another target needs to be activated (e.g., an if-then plan is needed to activate self-efficacy at the moment of acting; see ref [35]). The AVCP offers interventionists a way to think about these issues and may thus provide a typology that is aligned with their needs.
Leveraging the Distinction Between Target Activation and Target Change: Opportunities and Challenges
Although the AVCP offers insights about when interventions should aim to promote target activation vs. target change, much remains to be learned about the conditions that regulate the effectiveness of modifying these target dimensions (e.g., when, for whom, and for what behaviors). The Operating Conditions Framework (OCF [121];) is designed to support investigators as they pursue questions regarding the personal and situational factors that facilitate or inhibit the impact of an intervention strategy. According to the OCF, an intervention’s effectiveness is predicated on its ability to engage a specified mechanism of action (i.e., target engagement) and the degree to which change in the target elicits change in behavior (i.e., target validity). A review of the evidence concerning interventions designed to engage target value (e.g., risk perceptions, attitudes, intentions) indicated that remarkably little is known about the conditions that determine whether interventions engage target value or whether changing target value leads to behavior change [121].
To date, tests of conditions that regulate the effectiveness of interventions to promote target activation are both rare and idiosyncratic. There is evidence that priming effects are more pronounced following an inflammatory reaction to vaccination [122], when interventions eschew multiple cues that could activate competing targets [65], and when people attribute activated concepts to their own thoughts and not to environmental cues [123]. Similarly, evidence suggests that if-then planning is especially effective for people with weak executive control resources [124] or mental health problems [125]. However, the evidence to date concerning target engagement is piecemeal and not yet systematized. There is also a paucity of research on factors that could regulate the degree to which an activated target will impact the behavioral outcome (target validity). The availability of resources, psychological or material, may be critical as these conditions facilitate action [126]. For instance, the impact of reminders designed to activate the goals of using a condom [127] or getting vaccinated [70], likely depends upon the ease with which one can obtain condoms or schedule a vaccination.
Programs of research are needed to spell out the operating conditions for target activation strategies—what makes people receptive to interventions that promote target accessibility, and what influences the likelihood that accessible targets get translated into action. For example, there is emerging evidence that depression is associated with reduced goal activation [128–130] and that goal activation may play a role in executive dysfunction [131]; a pattern of findings that may mitigate the effect of strategies designed to promote target activation. However, additional research is needed to clarify the role of individual-level (e.g., stress, socioeconomic status, psychiatric illness [132];) and structural-level factors (e.g., discrimination, inequality, neighborhood resources, access to health care facilities) and their implications for the magnitude of target activation effects. According to Funder and Ozer’s guidelines [133], the effect sizes for the activation strategies reviewed here ranged from very small for the question-behavior effect (d+ = 0.14 [84];) to medium-large for if-then planning (d+ = 0.54 [91]). However, a key insight of the OCF is that heterogeneity of intervention effects is the norm rather than the exception and average d-values mask considerable variability in interventions’ impact. This variability demands theoretical and empirical explication [121].
Studies should also be directed towards understanding the durability of target activation effects. Although question-behavior effects have been observed over one year [82] and if-then planning engendered behavior change over two years [89], most tests of activation strategies involve immediate or short-term follow-ups. Although it might seem safe to assume that a health goal prime or text reminder will instigate behavior each time it is encountered, there are important empirical questions about the time course of activation effects, the potential for cue habituation, the diversity of cues that could be effective, and the impact of participants becoming aware of the potential influence of cues that warrant investigation [134]. A research agenda that prioritizes not only specifying the mechanism by which an intervention strategy operates (i.e., target activation vs. target change), but also the conditions under which those strategies operate could provide investigators with the guidance they need to optimize their efforts to promote health behavior change.
The content of this paper was informed by discussions at the 2015 meeting (Low-Touch Interventions: Implications for Health Behavior Change) of the National Cancer Institute’s Cognitive, Affective and Social Processes in Health Research (CASPHR) workgroup. The research reported in this paper was undertaken while Jerry Suls was at the National Cancer Institute.
Contributor Information
Paschal Sheeran, Department of Psychology and Neuroscience, University of North Carolina at Chapel Hill, Chapel Hill, USA; Lineberger Comprehensive Cancer Center, Chapel Hill, NC, USA.
Jerry Suls, Center for Personalized Health, Institute of Health System Science, Feinstein Institutes for Medical Research, Northwell Health, New York, NY, USA.
Angela Bryan, Department of Psychology and Neuroscience, University of Colorado Boulder, Boulder, CO, USA.
Linda Cameron, Psychological Sciences, School of Social Sciences, University of California, Merced, Merced CA, USA.
Rebecca A Ferrer, Behavioral Research Program, National Cancer Institute, Bethesda, MD, USA.
William M P Klein, Behavioral Research Program, National Cancer Institute, Bethesda, MD, USA.
Alexander J Rothman, Department of Psychology, University of Minnesota, Minneapolis, MN, USA.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards The authors declare that there are no conflicts of interest with respect to this paper.
Authors’ Contributions Paschal Sheeran led the conceptualization, project administration, supervision, writing—original draft, and writing—reviewing and editing. Jerry Suls, Angela Bryan, Linda Cameron, Rebecca Ferrer, and William Klein each contributed to the conceptualization and writing—reviewing and editing. Alex Rothman co-led the conceptualization, writing—original draft, and writing—review and editing.
Transparency Statement This is a theoretical paper that did not involve data collection from human participants. Thus, there is no study or analytic plan to register and no data or materials that can be made available.
References
- 1. Healthy People 2030 2020. Available at https://health.gov/healthypeople.
- 2. World Health Organization 2020. Available at https://www.who.int/initiatives/sdg3-global-action-plan.
- 3. Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008; 27(3):379–387. [DOI] [PubMed] [Google Scholar]
- 4. Duckworth AL, Gendler TS, Gross JJ. Situational strategies for self-control. Perspect Psychol Sci. 2016; 11(1):35–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hollands GJ, Bignardi G, Johnston M, et al. The TIPPME intervention typology for changing environments to change behaviour. Nat Hum Behav. 2017; 1(8):1–9. [Google Scholar]
- 6. Knittle K, Heino M, Marques MM, et al. The compendium of self-enactable techniques to change and self-manage motivation and behaviour v.1.0. Nat Hum Behav. 2020; 4(2):215–223. [DOI] [PubMed] [Google Scholar]
- 7. Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013; 46(1):81–95. [DOI] [PubMed] [Google Scholar]
- 8. Sheeran P, Klein WM, Rothman AJ. Health behavior change: moving from observation to intervention. Annu Rev Psychol. 2017; 68:573–600. [DOI] [PubMed] [Google Scholar]
- 9. Nielsen L, Riddle, M, King, JW. The NIH Science of Behavior Change Implementation Team. The NIH science of behavior change program: transforming the science through a focus on mechanisms of change. Behav Res Ther. 2018; 101:3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Escarti A, Guzman JF. Effects of feedback on self-efficacy, performance, and choice in an athletic task. J Appl Sport Psychol. 1999; 11(1):83–96. [Google Scholar]
- 11. Johnston M, Rothman AJ, de Bruin M, Kelly MP, Connell LE. From theory-inspired to theory-based interventions: a protocol for developing and testing a methodology for linking behaviour change techniques to theoretical mechanisms of action. Ann Behav Med. 2018; 52:501–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Connell Bohlen LE, Johnston DW, Rothman AJ, et al. Online tool for linking behavior change techniques and mechanisms of action based on triangulation of findings from literature synthesis and expert consensus. Transl Behav Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Collins LM. Optimization of Behavioral, Biobehavioral, and Biomedical Interventions: The Multiphase Optimization Strategy (MOST). New York: Springer; 2018. [Google Scholar]
- 14. Adler N, Naar-King S, Reynolds KD, Charlson, M.E. From ideas to efficacy: the ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 2015; 34:971–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Michie S, Carey RN, Johnston M, et al. From theory-inspired to theory-based interventions: a protocol for developing and testing a methodology for linking behaviour change techniques to theoretical mechanisms of action. Ann Behav Med. 2018; 52(6):501–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Higgins ET. Accessibility Theory. Handbook of Theories of Social Psychology. Vol. 1. Los Angeles, CA: Sage; 2012. p. 75–96. [Google Scholar]
- 17. McNamara TP, Holbrook J. Sematic Memory and Priming. In: Weiner IB, Healy AF, Procto RW, eds. Handbook of Psychology. Vol. 4. New York: Wiley; 2003. [Google Scholar]
- 18. Henson RNA. Neuroimging studies of priming. Prog Neurobiol. 2003; 70:53–81. [DOI] [PubMed] [Google Scholar]
- 19. Conca FB, Cappa SF, Catricalà E. The multidimensionality of abstract concepts: a systematic review. Neurosci Biobehav Rev. 2021; 127:474–491. [DOI] [PubMed] [Google Scholar]
- 20. Fazio RH. Multiple processes by which attitudes guide behavior: the MODE model as an integrative framework. Adv Exp Social Psych. 1990; 23:75–109. [Google Scholar]
- 21. Cooke RS, Sheeran P. Moderation of cognition-intention and cognition-behaviour relations: a meta-analysis of properties of variables from the theory of planned behaviour. Br J Social Psych. 2004; 43(2):159–186. [DOI] [PubMed] [Google Scholar]
- 22. Glasman LR, Albarracín D. Forming attitudes that predict future behavior: a meta-analysis of the attitude-behavior relation. Psychol Bull. 2006; 132(5):778–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Avishai A, Brewer NT, Mendel JR, Sheeran P. Expanding the analysis of mechanisms of action in behavioral interventions: cognitive change versus cognitive activation. Psychology and Health, in press. Doi:10.1080/08870446.2021.1969021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sheeran P, Gollwitzer PM, Bargh JA. Nonconscious processes and health. Health Psychol. 2013; 32(5):460–473. [DOI] [PubMed] [Google Scholar]
- 25. Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull. 2014; 140(2):511–543. [DOI] [PubMed] [Google Scholar]
- 26. Sheeran P, Maki A, Montanaro E, et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis. Health Psychol. 2016; 35(11):1178–1188. [DOI] [PubMed] [Google Scholar]
- 27. Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006; 132(2):249–268. [DOI] [PubMed] [Google Scholar]
- 28. Benton JS, Deaton C, Harvie M. Can communicating personalised disease risk promote healthy behaviour change? A systematic review of systematic reviews. Ann Behav Med. 2017; 51(5):718–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT. Pictorial cigarette pack warnings: a meta-analysis of experimental studies. Tob Control. 2016; 25(3):341–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lagström, H, Angle, S, Hakanen, M, Aromaa, M, Simell, O. Parental eating attitudes and indicators of healthy eating in a longitudinal randomized dietary intervention trial (the STRIP study). Public Health Nutr. 2011; 14(11):2065–2073. [DOI] [PubMed] [Google Scholar]
- 31. Wood C, Conner M, Sandberg T, Godin G, Sheeran P. Why does asking questions change health behaviours? The mediating role of attitude accessibility. Psychol Health. 2014; 29(4):390–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Grol R, Donders R, Hulscher M, van Achterberg T. Impact of a team and leaders-directed strategy to improve nurses’ adherence to hand hygiene guidelines: a cluster randomised trial. Int J Nurs Stud. 2013; 50(4):464–474. [DOI] [PubMed] [Google Scholar]
- 33. King D, Vlaev I, Everett-Thomas R, Fitzpatrick M, Darzi A, Birnbach DJ. “Priming” hand hygiene compliance in clinical environments. Health Psychol. 2016; 35(1):96–101. [DOI] [PubMed] [Google Scholar]
- 34. Ashford S, Edmunds J, French DP. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br J Health Psychol. 2010; 15(Pt 2):265–288. [DOI] [PubMed] [Google Scholar]
- 35. Thürmer JL, McCrea SM, Gollwitzer PM. Regulating self-defensiveness: if–then plans prevent claiming and creating performance handicaps. Motivation Emotion. 2013; 37(4):712–725. [Google Scholar]
- 36. Einstein GO, McDaniel MA, Williford CL, Pagan JL, Dismukes R. Forgetting of intentions in demanding situations is rapid. J Exp Psychol: Appl. 2003; 9(3):147–162. [DOI] [PubMed] [Google Scholar]
- 37. Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS One. 2014; 9(2):e88166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. van Koningsbruggen GM, Stroebe W, Papies EK, Aarts H. Implementation intentions as goal primes: boosting self-control in tempting environments. Eur J Social Psychol. 2011; 41(5):551–557. [Google Scholar]
- 39. Duckworth AL, Milkman KL, Laibson D. Beyond willpower: strategies for reducing failures of self-control. Psychol Sci Public Interest. 2019; 19(3):102–129. [DOI] [PubMed] [Google Scholar]
- 40. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011; 6:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hagger M, Cameron L, Hamilton K, Hankonen N, Lintunen T, eds. The Handbook of Behavior Change. Cambridge, UK: Cambridge University Press; 2020. [Google Scholar]
- 42. Ntoumanis NN, Prestwich A, Quested E, et al. A meta-analysis of self-determination theory-informed intervention studies in the health domain: effects on motivation, health behavior, physical, and psychological health. Health Psychol Rev. 2020; 4:1–31. [DOI] [PubMed] [Google Scholar]
- 43. Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Social Psychol. 2006; 38:69–119. [Google Scholar]
- 44. Papies EK. Health goal priming as a situated intervention tool: how to benefit from nonconscious motivational routes to health behaviour. Health Psychol Rev. 2016; 10(4):408–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Harkin B, Webb TL, Chang BP, et al. Does monitoring goal progress promote goal attainment? A meta-analysis of the experimental evidence. Psychol Bull. 2016; 142(2):198–229. [DOI] [PubMed] [Google Scholar]
- 46. Wilding S, Conner M, Prestwich A, Lawton R, Sheeran P. Using the question-behavior effect to change multiple health behaviors: an exploratory randomized controlled trial. J Exp Soc Psychol. 2019; 81:53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Thaler RH, Sunstein, CR. Nudge: Improving Decisions About Health, Wealth, and Happiness. Yale: Yale University Press; 2008. [Google Scholar]
- 48. Johnson EJ, Goldstein D. Do defaults save lives? Science. 2003; 302:1338–1339. [DOI] [PubMed] [Google Scholar]
- 49. Chapman GB, Li M, Colby H, Yoon H. Opting in vs opting out of influenza vaccination. JAMA. 2010; 304(1):43–44. [DOI] [PubMed] [Google Scholar]
- 50. Venema TA, Kroese FM, De Ridder DTD. I’m still standing: a longitudinal study on the effect of a default nudge. Psychol Health. 2018; 33(5):669–681. [DOI] [PubMed] [Google Scholar]
- 51.Friis R, Skov LR, Olsen A, et al. Comparison of three nudge interventions (priming, default option, and perceived variety) to promote vegetable consumption in a self-service buffet setting. PLoS One. 2017; 12(5):e0176028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Jachimowicz JM, Duncan S, Weber EU, Johnson EJ. When and why defaults influence decisions: a meta-analysis of default effects. Behav Public Policy 2019; 87:1–28. [Google Scholar]
- 53. Lindenberg S, Papies, E.K. Two kinds of nudging and the power of cues: shifting salience of alternatives and shifting salience of goals. Int Rev Environ Res Econ. 2019;13(3-4):229–63. [Google Scholar]
- 54. Suri G, Sheppes G, Gross JJ. The role of action readiness in motivated behavior. J Exp Psychol Gen. 2015; 144(6):1105–1113. [DOI] [PubMed] [Google Scholar]
- 55. Suri G, Gross JJ, McClelland JL. Value-based decision making: an interactive activation perspective. Psychol Rev. 2020; 127(2):153–185. [DOI] [PubMed] [Google Scholar]
- 56. Higgins ET. Knowledge activation: accessibility, applicability, and salience. In: Higgins E, Kruglanksi, AW, eds. Social Psychology: Handbook of Basic Principles. New York: Guilford; 1996. p. 133–68. [Google Scholar]
- 57. Suri G, Gross JJ. The role of attention in motivated behavior. J Exp Psychol Gen. 2015; 144(4):864–872. [DOI] [PubMed] [Google Scholar]
- 58. Privitera GJ, Zuraikat FM. Proximity of foods in a competitive food environment influences consumption of a low calorie and a high calorie food. Appetite. 2014; 76:175–179. [DOI] [PubMed] [Google Scholar]
- 59. Kroese FM, Marchiori DR, de Ridder DTD. Nudging healthy food choices: a field experiment at the train station. 2016; 38(2):e133–e1e7. [DOI] [PubMed] [Google Scholar]
- 60. Maas J, de Ridder DTD. de Vet E, de Wit JBF. Do distant foods decrease intake? The effect of food accessibility on consumption. Psychol Health. 2012; 27(sup2):59–73. [DOI] [PubMed] [Google Scholar]
- 61.Bucher T, Collins C, Rollo ME, et al. Nudging consumers towards healthier choices: a systematic review of positional influences on food choice. Br J Nutr. 2016; 115(12):2252–2263. [DOI] [PubMed] [Google Scholar]
- 62. Hollands GJ, Shemilt I, Marteau TM, Jebb SA, et al. Portion, package or tableware size for changing selection and consumption of food, alcohol and tobacco. Cochrane Database Syst Rev. 2015; 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Knowles DB, Aldrovandi S. Exploring the underpinning mechanisms of the proximity effect within a competitive food environment. Appetite. 2019; 134:94–102. [DOI] [PubMed] [Google Scholar]
- 64. Hunter JA, Hollands G, Couturier D-L, Marteau TM. Effect of snack-food proximity on intake in general population samples with higher and lower cognitive resource. Appetite. 2018; 121:337–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Garnett EE, Marteau T, Sandbrook C, Pilling MA, Balmford A. Order of meals at the counter and distance between options affect student cafeteria vegetarian sales. Nature Food. 2020; 1(8):485–488. [DOI] [PubMed] [Google Scholar]
- 66. Young LR, Nestle M. The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health. 2002; 92:246–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Zlatevska ND, Holden SS. Sizing up the effect of portion size on consumption: a meta-analytic review. J Marketing. 2014; 78:140–154. [Google Scholar]
- 68. Tversky A, Kahneman, D. Judgment under uncertainty. Heuristics and biases. Science. 1974:1124–31. [DOI] [PubMed] [Google Scholar]
- 69. Versluis I, Papies EK. The role of social norms in the portion size effect: reducing normative relevance reduces the effect of portion size on consumption decisions. Front Psychol. 2016; 7:593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Harvey H, Reissland N, Mason J. Parental reminder, recall and educational interventions to improve early childhood immunisation uptake: a systematic review and meta-analysis. Vaccine. 2015; 33(25):2862–2880. [DOI] [PubMed] [Google Scholar]
- 71. Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Inform Assoc. 1996; 3(6):399–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. van Leeuwen L, Onrust S, van den Putte B, et al. Cue-reminders to prevent health-risk behaviors: a systematic review. Front Public Health. 2019; 7:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Duncan J, Emslie H, Williams P. Intelligence and the frontal lobe: the organization of goal-directed behavior. Cogn Psychol. 1996; 30:257–303. [DOI] [PubMed] [Google Scholar]
- 74. Papies EK, Hamstra P. Goal priming and eating behavior: enhancing self-regulation by environmental cues. Health Psychol. 2010; 29(4):384–388. [DOI] [PubMed] [Google Scholar]
- 75. Papies EK, Potjes I, Keesman M, Schwinghammer S, van Koningsbruggen GM. Using health primes to reduce unhealthy snack purchases among overweight consumers in a grocery store. Int J Obes (Lond). 2014; 38(4):597–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Versluis I, Papies EK. Eating less from bigger packs: preventing the pack size effect with diet primes. Appetite. 2016; 100:70–79. [DOI] [PubMed] [Google Scholar]
- 77.King D, Vlaev I, Everett-Thomas R, Fitzpatrick M, Darzi A, Birnbach DJ. “Priming” hand hygiene compliance in clinical environments. Health Psychology. 2016;35(1):96–101. [DOI] [PubMed]
- 78. Weingarten E, Chen Q, McAdams M, Yi J, Hepler J, Albarracin D. From primed concepts to action: a meta-analysis of the behavioral effects of incidentally presented words. Psychol Bull. 2016; 142(5):472–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Bargh JA, Gollwitzer, PM, Oettingen, G. Motivation. In: Fiske ST, Gilbert DT., Lindzay G, eds. Handbook of Social Psychology (5th ed). New York: Wiley; 2010. pp. 269–316. [Google Scholar]
- 80. Conner M, Godin G, Norman P, Sheeran P. Using the question-behavior effect to promote disease prevention behaviors: two randomized controlled trials. Health Psychol. 2011; 30(3):300–309. [DOI] [PubMed] [Google Scholar]
- 81. Godin G, Sheeran P, Conner M, Germain M. Asking questions changes behavior: mere measurement effects on frequency of blood donation. Health Psychol. 2008; 27(2):179–184. [DOI] [PubMed] [Google Scholar]
- 82. Godin G, Sheeran P, Conner M, et al. Which survey questions change behavior? Randomized controlled trial of mere measurement interventions. Health Psychol. 2010; 29(6):636–644. [DOI] [PubMed] [Google Scholar]
- 83. Hagoel L, Neter E, Stein N, Rennert G. Harnessing the Question–Behavior Effect to enhance colorectal cancer screening in an mhealth experiment. Am J Public Health. 2016; 106(11):1998–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wilding S, Conner M, Sandberg T, et al. The question-behaviour effect: a theoretical and methodological review and meta-analysis. Eur Rev Social Psychol 2016; 27:196–230. [Google Scholar]
- 85. Wood C, Conner M, Miles E, et al. The impact of asking intention or self-prediction questions on subsequent behavior: a meta-analysis. Pers Soc Psychol Rev. 2016; 20(3):245–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Gollwitzer PM. Weakness of the will: is a quick fix possible? Motivation Emotion 2014; 38(3):305–322. [Google Scholar]
- 87. Brown I, Sheeran P, Reuber M. Enhancing antiepileptic drug adherence: a randomized controlled trial. Epilepsy Behav. 2009; 16(4):634–639. [DOI] [PubMed] [Google Scholar]
- 88. Milne SO, Orbell S, Sheeran P. Combining motivational and volitional interventions to promote exercise participation: protection motivation theory and implementation intentions. Br J Health Psychol. 2002; 7(2):163–184. [DOI] [PubMed] [Google Scholar]
- 89. Martin J, Sheeran P, Slade P, Wright A, Dibble T. Durable effects of implementation intentions: reduced rates of confirmed pregnancy at 2 years. Health Psychol. 2011; 30(3):368–373. [DOI] [PubMed] [Google Scholar]
- 90. Sheeran P, Orbell S. Using implementation intentions to increase attendance for cervical cancer screening. Health Psychol. 2000; 18:283–289. [DOI] [PubMed] [Google Scholar]
- 91. Keller L, Gollwitzer, PM, Sheeran, P. Changing behavior using the model of action phases. In: Hagger MS, Cameroon LD, Hamilton K, Hankonen N, Lintunen T., eds. The Handbook of Behavior Change. New York: Cambridge University Press; 2020. pp. 77–88. [Google Scholar]
- 92. Webb TL, Sheeran P. Mechanisms of implementation intention effects: the role of goal intentions, self-efficacy, and accessibility of plan components. Br J Soc Psychol. 2008; 47(Pt 3):373–395. [DOI] [PubMed] [Google Scholar]
- 93. Webb TL, Sheeran P. How do implementation intentions promote goal attainment? A test of component processes. J Exp Social Psych. 2007; 43(2):295–302. [Google Scholar]
- 94. Webb TL, Sheeran P. Identifying good opportunities to act: implementation intentions and cue discrimination. Eur Social Psychol. 2004; 34(4):407–419. [Google Scholar]
- 95. Custers R, Aarts H. Goal-discrepant situations prime goal-directed actions if goals are temporarily or chronically accessible. Pers Soc Psychol Bull. 2007; 33(5):623–633. [DOI] [PubMed] [Google Scholar]
- 96. Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: the role of message framing. Psychol Bull. 1997; 121(1):3–19. [DOI] [PubMed] [Google Scholar]
- 97. Updegraff JA, Rothman AJ. Health message framing: moderators, mediators, and mysteries. Social Personality Psychol Compass. 7(9):668–79. [Google Scholar]
- 98. Iyengar SS. Is Anyone Responsible?: How Television Frames Political Issues. Chicago, CA: University of Chicago Press; 1991. [Google Scholar]
- 99. Ellis EM, Elwyn G, Nelson WL, Scalia P, Kobrin SC, Ferrer RA. Interventions to engage affective forecasting in health-related decision making: a meta-analysis. Ann Behav Med. 2018; 52(2):157–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Abraham C, Sheeran P. Deciding to exercise: the role of anticipated regret. Br J Health Psychol. 2004; 9(2):269–278. [DOI] [PubMed] [Google Scholar]
- 101. Wood W, Runger D. Psychology of Habit. Annu Rev Psychol. 2016; 67:289–314. [DOI] [PubMed] [Google Scholar]
- 102. Neal DT, Wood W, Labrecque JS, Lally P. How do habits guide behavior? Perceived and actual triggers of habits in daily life. J Exp Social Psychol 2012; 48(2):492–498. [Google Scholar]
- 103. Lally P, Chipperfield A, Wardle J. Healthy habits: efficacy of simple advice on weight control based on a habit-formation model. Int J Obes (Lond). 2008; 32(4):700–707. [DOI] [PubMed] [Google Scholar]
- 104. Kaushal N, Rhodes RE, Spence JC, Meldrum JT. Increasing physical activity through principles of habit formation in new gym members: a randomized controlled trial. Ann Behav Med. 2017; 51(4):578–586. [DOI] [PubMed] [Google Scholar]
- 105. Rothman AJ, Gollwitzer PM, Grant AM, Neal DT, Sheeran P, Wood W. Hale and hearty policies: how psychological science can create and maintain healthy habits. Perspect Psychol Sci 2015; 10(6):701–705. [DOI] [PubMed] [Google Scholar]
- 106. Harris JL, Bargh JA, Brownell KD. Priming effects of television food advertising on eating behavior. Health Psychol. 2009; 28(4):404–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Roehrich L, Goldman MS. Implicit priming of alcohol expectancy memory processes and subsequent drinking behavior. Exp Clin Psychopharmacol. 1995; 3(4):402. [Google Scholar]
- 108. Rivis A, Sheeran P. Automatic risk behavior: direct effects of binge drinker stereotypes on drinking behavior. Health Psychol. 2013; 32(5):571–580. [DOI] [PubMed] [Google Scholar]
- 109. Harris JL, Pierce M, Bargh JA. Priming effect of antismoking PSAs on smoking behaviour: a pilot study. Tob Control. 2014; 23(4):285–290. [DOI] [PubMed] [Google Scholar]
- 110. He Y, Shang C, Huang J, Cheng K-W, Chaloupka FJ. Global evidence on the effect of point-of-sale display bans on smoking prevalence. Tob Control. 2018; 27:98–104. [DOI] [PubMed] [Google Scholar]
- 111. Palmedo PC, Dorfman L, Garza S, Murphy E, Freudenberg N. Countermarketing alcohol and unhealthy food: an effective strategy for preventing noncommunicable diseases? Lessons from Tobacco. Annu Rev Public Health. 2017; 38:119–144. [DOI] [PubMed] [Google Scholar]
- 112. Bryan CJ, Yeager DS, Hinojosa CP, et al. Harnessing adolescent values to motivate healthier eating. Proc Natl Acad Sci USA. 2016; 113(39):10830–10835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Gollwitzer PM, Sheeran P, Trotschel R, Webb TL. Self-regulation of priming effects on behavior. Psychol Sci. 2011; 22(7):901–907. [DOI] [PubMed] [Google Scholar]
- 114. Webb TL, Sheeran, P., Gollwitzer, PM, Trötschel, R. Strategic control over the unhelpful effects of primed social categories and goals. Zeitschrift für Psychologie. 2012;220(3). [Google Scholar]
- 115. Oettingen G. Future thought and behaviour change. Eur Rev Social Psychol. 2012; 23(1):1–63. [Google Scholar]
- 116. Cross A, Sheffield D. Mental contrasting for health behaviour change: a systematic review and meta-analysis of effects and moderator variables. Health Psychol Rev. 2019; 13(2):209–225. [DOI] [PubMed] [Google Scholar]
- 117. Sheeran P, Harris P, Vaughan J, Oettingen G, Gollwitzer PM. Gone exercising: mental contrasting promotes physical activity among overweight, middle-aged, low-SES fishermen. Health Psychol. 2013; 32(7):802–809. [DOI] [PubMed] [Google Scholar]
- 118. Oettingen G, Reininger KM. The power of prospection: mental contrasting and behavior change. Social Personality Psychol Compass 2016; 10(11):591–604. [Google Scholar]
- 119. Sheeran P, Webb TL, Gollwitzer PM. The interplay between goal intentions and implementation intentions. Pers Soc Psychol Bull. 2005; 31(1):87–98. [DOI] [PubMed] [Google Scholar]
- 120. Sunstein CR. Nudges that fail. Behav Public Policy. 2017; 1(1):4–25. [Google Scholar]
- 121. Rothman AJ, Sheeran P. The Operating Conditions framework: integrating mechanisms and moderators in health behavior interventions. Health Psychol. 2021; 40(12):845–857. [DOI] [PubMed] [Google Scholar]
- 122. Jolink TA, Fendinger NJ, Alvarez GM, Feldman MJ, Gaudier-Diaz MM, Muscatell KA. Inflammatory reactivity to the influenza vaccine is associated with changes in automatic social behavior. Brain Behav Immun. 2022; 99:339–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Loersch CP, Payne BK. The situated inference model: an integrative account of the effects of primes on perception, behavior, and motivation. Perspect Psychol Sci. 2011; 6:234–252. [DOI] [PubMed] [Google Scholar]
- 124. Hall PA, Zehr CE, Ng M, Zanna MP. Implementation intentions for physical activity in supportive and unsupportive environmental conditions: an experimental examination of intention–behavior consistency. J Exp Social Psychol. 2012; 48(1):432–436. [Google Scholar]
- 125. Toli A, Webb TL, Hardy GE. Does forming implementation intentions help people with mental health problems to achieve goals? A meta-analysis of experimental studies with clinical and analogue samples. Br J Clin Psychol. 2016; 55(1):69–90. [DOI] [PubMed] [Google Scholar]
- 126. Bryan CJ, Tipton E, Yeager DS. Behavioural science is unlikely to change the world without a heterogeneity revolution. Nat Hum Behav. 2021; 5(8):980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. MacDonald TK, Fong G, Zanna MP, Martineau AM. Alcohol myopia and condom use: can alcohol intoxication be associated with more prudent behavior? J Personality Social Psychol. 2000;78(4):605–19. [DOI] [PubMed] [Google Scholar]
- 128. Shah J, Friedman R, Kruglanski A. Forgetting all else: on the antecedents and consequences of goal shielding. J Pers Soc Psychol. 2002; 83(6):1261–1280. [PubMed] [Google Scholar]
- 129. Eddington KM, Dolcos F, McLean AN, Krishnan KR, Cabeza R, Strauman TJ. Neural correlates of idiographic goal priming in depression: goal-specific dysfunctions in the orbitofrontal cortex. Social Cognitive Affective Neurosci. 2009; 4(3):238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Strauman T. Self-regulation and psychopathology: toward an integrative translational research paradigm. Annu Rev Clin Psychol. 2017; 13:497–523. [DOI] [PubMed] [Google Scholar]
- 131. Nieuwenhuis S, Broerse A, Nielen MM, de Jong R. A goal activation approach to the study of executive function: an application to antisaccade tasks. Brain Cogn. 2004; 56(2):198–214. [DOI] [PubMed] [Google Scholar]
- 132. Quinn ME, Stanton CH, Slavich GM, Joormann J. Executive control, cytokine reactivity to social stress, and depressive symptoms: testing the social signal transduction theory of depression. Stress. 2020; 23(1):60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Funder DC, Ozer DJ. Evaluating effect sizes in psychological research: sense and nonsense. Adv Methods Practices Psychol Sci 2019; 2(2):156–168. [Google Scholar]
- 134. de Ridder D, Kroese F, van Gestel L. Nudgeability: mapping conditions of susceptibility to nudge influence. Perspective Psychol Sci 2022; 17(2):346–359. [DOI] [PMC free article] [PubMed] [Google Scholar]