Abstract
Background:
Dissociative and posttraumatic stress disorder (PTSD) symptoms are common co-occurring responses to psychological trauma. Yet, these two groups of symptoms appear to be related to diverging patterns of physiological response. To date, few studies have examined how specific dissociative symptoms, namely, depersonalization and derealization, relate to skin conductance response (SCR), a marker of autonomic function, within the context of PTSD symptoms. We examined associations among depersonalization, derealization, and SCR during two conditions – resting control and breath-focused mindfulness – in the context of current PTSD symptoms.
Methods:
Sixty-eight trauma-exposed women (82.4% Black; Mage=42.5, SDage=12.1) were recruited from the community for a breath-focused mindfulness study. SCR data were collected during alternating resting control and breath-focused mindfulness conditions. Moderation analyses were conducted to examine relationships among dissociative symptoms, SCR, and PTSD for these different conditions.
Results:
Moderation analyses revealed that depersonalization was linked to lower SCR during resting control, B=.0005, SE=.0002, p=.006, in participants low-to-moderate PTSD symptoms; however, depersonalization was associated with higher SCR during breath-focused mindfulness, B = −.0006, SE = .0003, p = .029, in individuals with similar levels of PTSD symptoms. No significant interaction between derealization and PTSD symptoms on SCR was observed.
Conclusions:
Depersonalization symptoms may associate with physiological withdrawal during rest, but greater physiological arousal during effortful emotion regulation in individuals with low- to moderate levels of PTSD, which has significant implications for barriers to treatment engagement as well as treatment selection in this population.
Keywords: dissociation, depersonalization, derealization, posttraumatic stress disorder, skin conductance, trauma exposure
Exposure to psychological trauma increases risk for multiple adverse physical and mental health outcomes (Fonkoue et al., 2020; Fusco et al., 2021), including symptoms of posttraumatic stress disorder (PTSD). PTSD is a psychiatric disorder characterized by marked distress and functional impairment resulting from exposure to a traumatic event, trauma-related avoidance, intrusive/re-experiencing symptoms, hyperarousal and physiological reactivity, and negative alterations in cognition and mood.3 Another type of trauma response that often co-occurs with symptoms of PTSD is dissociation, a transdiagnostic phenomenon that involves disruptions in the integration of consciousness, memory, identity, emotion, perception, and body awareness (American Psychiatric Association, 2013). Dissociation is most likely to occur in the context of acute life-threatening events or chronic, repeated traumas, especially those in which escape may be impossible or highly risky, such as repeated childhood sexual abuse (Bailey & Brand, 2017). Other factors that increase risk for dissociative responses include traumas involving betrayal, higher PTSD severity, and female sex (Platt & Freyd, 2015; Wolf, Lunney, et al., 2012; Wolf, Miller, et al., 2012).
Both dissociative and PTSD symptoms often arise in highly trauma-exposed populations (Schimmenti, 2018), leading to the inclusion of a dissociative subtype of PTSD in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The dissociative subtype of PTSD is characterized by symptoms of depersonalization (i.e., experiences of feeling detached from the self, as if one were an outside observer of one’s mental processes or body) or derealization (i.e., experiences of unreality of the outside world or surroundings) in addition to traditional PTSD diagnostic criteria (American Psychiatric Association, 2013; Choi et al., 2017). Dissociation has been likened to a “freeze response,” manifesting as tonic immobility, heightened parasympathetic tone, lower emotional reactivity, and pain sensitivity/analgesia (Kozlowska et al., 2015). These manifestations of dissociation are adaptive, as pain tolerance, emotional numbing, motor paralysis, and language loss can have functional value in inescapable, life-threatening situations (Schauer & Elbert, 2010; Williamson et al., 2015).
Despite its short-term value, dissociation that persists beyond immediate threat is often accompanied by a complex, and sometimes treatment-resistant, clinical presentation. Specifically, dissociative symptoms that occur in the absence of stress or on an involuntary basis are related to greater severity, chronicity, and comorbidity of psychiatric disorders (Lebois et al., 2022; Semiz et al., 2014). Dissociative symptoms may also act as a major barrier to psychotherapeutic treatment, particularly, first-line trauma treatments (Boyer et al., 2022; M. Price et al., 2014; Spitzer et al., 2007), given that disconnecting from the present moment precludes sufficient engagement with traumatic memories or processing related negative emotions (Frewen & Lanius, 2006; Lanius et al., 2010). Exposure-based psychotherapies require a subjective psychological and physiological distress level within a certain therapeutic window. Thus, dissociative symptoms can hinder treatment effectiveness and symptom reduction when they prevent an individual from experiencing trauma-related emotions.
At the physiological level, a pattern of autonomic nervous system (ANS) dysfunction is apparent among those with dissociative symptoms and disorders (Boulet et al., 2022; D’Andrea et al., 2013). The ANS has two branches, the parasympathetic and sympathetic nervous systems, which maintain homeostasis and allow adaptive adjustment to internal and external stimuli (Jänig, 2022). Trauma exposure disrupts the rhythmic balance between the parasympathetic and sympathetic branches (Schauer & Elbert, 2010), contributing to emotional under-modulation (i.e., PTSD symptoms of intrusions and hyperarousal), emotional over-modulation (i.e., dissociation), or both (Lanius et al., 2010). Overall, psychophysiological data suggest that traditional PTSD symptoms are associated with heightened physiological reactivity (Morris & Rao, 2013; Orr et al., 2002), while dissociative symptoms are associated with a blunted autonomic response (Sack et al., 2012).
One method frequently used to examine autonomic functioning is electrodermal activity (EDA), a marker of physiological arousal that reflects changes in sweat gland activity. Prior studies have shown that PTSD symptoms are associated with greater baseline, or resting, skin conductance levels (SCL; Orr et al., 2000) and increased skin conductance response (SCR) to a trauma interview (Grasser et al., 2022; Hinrichs et al., 2017) and aversive imagery (McTeague et al., 2010), whereas those with dissociative symptoms exhibit lower SCL (Sierra et al., 2002) and attenuated SCR to startling sounds (D’Andrea et al., 2013; Ebner-Priemer et al., 2005; Herrero et al., 2020). Further, in the only study of SCR in a sample of trauma-exposed individuals with both PTSD and dissociative symptoms, higher dissociation was related to lower SCR during a fear potentiated startle paradigm (Seligowski et al., 2019). However, a recent systematic review did not find a clear trend in the relationship between trauma-related dissociation and ANS activation during a range of tasks (Beutler et al., 2022). Taken together, PTSD symptoms that are present, but remain unaccounted for, in conjunction with study-specific differences in tasks and procedures, may contribute to inconsistent findings regarding the association between dissociative symptoms and SCR.
The presence of one or both of two types of dissociative symptoms, depersonalization and derealization, is used to classify the dissociative subtype of PTSD. While previous findings have linked depersonalization to reduced SCR to emotional stimuli (Dewe et al., 2016; Sierra et al., 2002, 2006), few studies have examined the relationship between depersonalization and SCR during a resting condition (Horn et al., 2020). These studies have generated mixed results, and more importantly, were conducted in samples with depersonalization disorder diagnoses and failed to account for co-occurring PTSD symptoms’ potential influence (Michal et al., 2013; Schoenberg et al., 2012). Moreover, to our knowledge, the relationship between derealization symptoms and SCR has yet to be examined in a chronically trauma-exposed sample. Because dissociative and PTSD symptoms commonly co-occur in trauma-exposed individuals, understanding the interaction of these symptoms with physiological response may permit characterization of autonomic response profiles that accompany different clinical symptom presentations. The extant literature has not explored how depersonalization and derealization relate to SCR during different conditions at various levels of PTSD symptoms. Altogether, the unique associations of depersonalization, derealization, and SCR, especially within the context of PTSD symptoms, remain unknown.
To address this gap in the literature, we examined associations between two types of dissociative symptoms – depersonalization and derealization – and SCR during two conditions – resting control and breath-focused mindfulness – in a sample of trauma-exposed women. We also examined potential interactions of dissociative symptoms with PTSD symptoms on SCR. In particular, the relationship between dissociation and SCR during breath-focused mindfulness was compared to that of SCR during resting control given deep breathing’s association with increased SCR (Blain et al., 2008). Given the dearth of literature on the associations between dissociative symptoms and SCR-rest and SCR-breath at different PTSD symptom levels, we also explored the potential moderating effects of current PTSD symptoms. Considering dissociation often manifests as blunted physiological response, we hypothesized that PTSD symptoms would moderate SCR’s associations with depersonalization and derealization during the rest and breath-focused mindfulness conditions.
Methods and Materials
Participants and Procedures
Participants were recruited as part of a breath-focused mindfulness study for trauma-exposed individuals (procedures outlined below), during which SCR data were collected. Data from 68 individuals were available for analysis. The vast majority of participants identified as Black (82.4%, n = 56) and all were female (Mage = 42.5, SDage = 12.10). Most participants reported experiencing significant economic disadvantage (63.2%, n = 43; i.e., reported a monthly household income of less than $2,000). On average, participants reported exposure to approximately 4 different trauma types (SD = 1.3). See Table 1 for sample characteristics. Participants were recruited in 2 ways: 1) from community advertisements; 2) as part of a larger, ongoing study of PTSD which recruited patients from a publicly funded healthcare system in a large southeastern city. As part of the larger study, trained interns approached patients in the medical clinics regarding potential participation. During the COVID-19 pandemic, patients admitted to the hospital were contacted via telephone and invited to participate.
Table 1.
Sample Characteristics
| Variable | % (n) |
|---|---|
| Race | |
| African American/Black | 82.4 (56) |
| Caucasian/White | 13.2 (9) |
| Multiracial | 2.9 (2) |
| Other | 1.5 (1) |
| Household Monthly Income | |
| $ 2,000 or more | 33.8 (23) |
| $ 1,000 – 1,999 | 25.0 (17) |
| $ 500 – 999 | 19.1 (13) |
| $ 0 – 249 | 14.7 (10) |
| $ 250 – 499 | 4.4 (3) |
| Missing | 2.9 (2) |
| Education | |
| Some college or technical school | 20.6 (14) |
| Graduate school | 19.1 (13) |
| College graduate | 19.1 (13) |
| 12th grade / High school graduate | 13.2 (9) |
| Less than 12th grade | 11.8 (8) |
| Technical school graduate | 8.8 (6) |
| GED | 7.4 (5) |
| Missing | 1.4 (1) |
| Relationship Status | |
| Single, never married | 54.4 (37) |
| Divorced | 22.1 (15) |
| Married | 17.6 (12) |
| Domestic partner | 2.9 (2) |
| Separated | 1.5 (1) |
| Widowed | 1.5 (1) |
| Employment Status | |
| Not employed | 57.4 (39) |
| Employed | 42.6 (29) |
| Trauma Exposure | M = 4.1 types (SD = 1.3) |
| Witnessed violence | 85.3% (58) |
| Exposure to accident, injury, or illness | 76.5% (52) |
| Experienced sexual violence | 73.5% (50) |
| Experienced childhood abuse | 69.1% (47) |
| Experienced intimate partner violence | 54.4% (37) |
| Experienced non-partner violence | 44.1% (30) |
| Age | M = 42.5 years (SD = 12.1) |
Informed consent was obtained from all study participants after the nature of procedures were explained. If eligible, participants were given information about a brief breath-focused mindfulness intervention for PTSD (Study NCT02754557). Inclusion criteria included being aged 18–65, identifying as female, the ability to provide informed consent, exposure to a criterion A traumatic event, and PTSD symptoms in the past month. Exclusion criteria included cognitive impairment, a history of neurological disorders, active psychosis, or active mania. Data collection and study procedures were approved by Emory University Institutional Review Board and the Grady Research Oversight Committee in accordance with the provisions of the Declaration of Helsinki.
Measures
Traumatic Events Inventory (TEI; Gillespie et al., 2009; Mekawi et al., 2021).
The TEI was used to assess participants’ self-reported exposure to 14 different traumatic events. Each item was rated on a binary scale (0 = No, 1 = Yes). Six trauma type variables were generated by collapsing similar traumas into broad binary categories: experiencing childhood physical and emotional abuse (two items), sexual violence (three items), witnessing violence (six items), experiencing physical assault by a non-partner (two items), experiencing intimate partner violence (two items), and exposure to a serious accident or injury (two items). For example, if a participant endorsed witnessing an attack with or without a weapon, witnessing violence between caregivers, or witnessing the murder of a family member or friend, they were coded as having witnessed violence (0 = Did not witness violence, 1 = Witnessed violence). A cumulative trauma exposure variable was generated by summing the total number of trauma types endorsed.
Modified PTSD Symptom Scale, Self-Report (MPSS-SR; Falsetti et al., 1993).
The MPSS-SR, a 17-item self-report measure, was used to assess severity of PTSD symptoms within the past two weeks. Participants responded based on a Likert scale ranging from 0 (not at all) to 3 (five or more times per week). PTSD symptoms were summed to generate a total score, with higher scores reflecting greater PTSD symptom severity. In the present study, internal consistency for MPSS total score was good (α = 0.77).
Multiscale Dissociative Inventory (Briere et al., 2005).
Severity of dissociative symptoms experienced within the past month were measured via the MDI, a 30-item self-report measure with six subscales: disengagement, emotional constriction, memory disturbance, identity dissociation, depersonalization (five items; e.g., “Your body feeling like it was someone else’s”), derealization (five items; e.g., “Feeling like you were in a dream”). Item responses ranged from 1 (never) to 5 (very often). In the current study, only the depersonalization and derealization subscales were used; higher depersonalization subscale scores reflect greater depersonalization symptoms, while higher derealization subscale scores reflect greater derealization symptoms. Internal consistencies were good in the present study (depersonalization, α = 0.74; derealization, α = 0.83).
Skin Conductance Response (SCR).
At each of six intervention visits over approximately three weeks, participants were fitted with psychophysiology leads, including skin conductance, and sat in a chair in a sound-attenuated chamber in front of a computer screen and microphone. Instructions appeared on the screen that directed the participant to either rest with their eyes open (“Rest and relax”) or engage in breath-focused mindfulness (“Focus on your breath”) for one minute per condition, for a total of ten minutes (i.e., five blocks per condition); conditions were randomized for each participant.
SCR was recorded with the Biopac MP150 system for Windows (Biopac systems, INC., Aero Camino, CA, USA). EDA was sampled at 1,000 Hz and amplified using the respective modules of the Biopac system. Disposable electrodes from Biopac (EL-507) pre-coated with isotonic lotion were placed on the palm of the hand. For the purpose of this study, we examined SCR during the resting control and breath-focused mindfulness conditions for the first study session, using an average SCR value from each condition’s five blocks. SCR data were Winsorized (i.e., data outside the Tukey Hinges of 1.5 times the interquartile range from the 25th and 75th percentiles were rescaled to the last good value within the Tukey Hinges) and entered into group analyses.
Data Analyses
Participants completed measures of interest (i.e., MPSS, MDI, SCL) between August 2015 and July 2021. There were no missing data on any variables of interest. Analyses were conducted using SPSS version 28. Descriptive statistics were generated. We examined the associations between two SCR conditions – resting control (i.e., SCR-rest) and breath-focused mindfulness (i.e., SCR-breath) – and various demographic variables connected to SCR in previous studies. Pearson’s correlations were conducted to assess bivariate associations among depersonalization, derealization, SCR-rest, and SCR-breath. To address our hypothesis, we conducted four moderation models using Hayes’ PROCESS Macro (Model 1). PTSD symptoms served as the moderator in each model; low, moderate, and severe groups reflect values at −1 SD, mean, and +1 SD. In the first model, depersonalization was entered as the predictor, and SCR-rest was entered as the outcome. In the second model, derealization was entered as the predictor, and SCR-rest was entered as the outcome. In each model, continuous variables were mean centered. The third moderation model included depersonalization as the predictor and SCR-breath as the outcome, and the fourth included derealization as the predictor and SCR-breath as the outcome. Bonferroni correction was applied to correct for error associated with multiple comparisons across moderation analyses, leaving the threshold for statistical significance at p≤.0125.
Results
Table 2 details bivariate associations between dissociative symptoms, PTSD and SCR for both conditions. Neither PTSD symptoms overall, r = −.07, p = .60, nor individual symptom clusters (re-experiencing, r = −.04, p = .73; avoidance/numbing, r = −.03, p = .83; hyperarousal, r = −.10, p = .44; anhedonia, r = −.10, p = .42) were related to SCR-rest at the bivariate level. Similarly, overall PTSD symptoms, r = −.10, p = .40, and individual symptom clusters (re-experiencing, r = −.03, p = .83; avoidance/numbing, r = −.14, p = .24; hyperarousal, r = −.05, p = .68; anhedonia, r = −.15, p = .23) were not associated with SCR-breath at the bivariate level. Because SCR was not related to age (rest, r = .01, p = .92; breath, r = −.18, p = .13), race (rest, r = −.07, p = .57; breath, r = .07, p = .60), income (rest, r = −.09, p = .50; breath, r = −.07, p = .56), nor education level (rest, r = −.05, p = .68; breath, r = −.08, p = .53), these variables were not included in further analyses as covariates. Greater depersonalization was related to lower SCR-rest, r = −.26, p = .03 but not lower SCR-breath, r = .22, p = .08. Greater derealization was not associated with lower SCR-rest, r = −.13, p = .31, nor SCR-breath, r = .11, p = .36.
Table 2.
Descriptive Statistics (n = 68) and Bivariate Correlations with Confidence Intervals
| Variable | Min-Max | M | SD | 2. | 3. | 4. | 5 |
|---|---|---|---|---|---|---|---|
| 1. Depersonalization | 5.00 – 24.00 | 8.03 | 3.81 | .72*** | −.26* | .22 | .37** |
| [.57−.81] | [−.47--.02] | [−.03−.43] | [.14−.56] | ||||
| 2. Derealization | 5.00 – 25.00 | 9.81 | 4.21 | -- | −.13 | .11 | .18 |
| [−.35−.12] | [−.13−.34] | [−.06−.40] | |||||
| 3. SCR-Rest | −.25 − .16 | −.0012 | .05 | -- | -- | −.64*** | −.07 |
| [−.76--.47] | [−.30−.18] | ||||||
| 4. SCR-Breath | −.30 − .45 | 0.146 | .08 | -- | -- | -- | −.10 |
| [−.33−.14] | |||||||
| 4. PTSD symptoms | 7.00 – 50.00 | 27.49 | 8.58 | -- | -- | -- | -- |
Note: SCR = skin conductance response; bracketed values represent 95% Confidence Intervals [lower CI - upper CI];
p < .05
p < .01
p < .001
In line with our hypothesis, the first moderation model revealed depersonalization and PTSD symptoms significantly interacted to predict SCR-rest, B = .0005, SE = .0002, p = .006. A significant negative association between depersonalization and SCR-rest was apparent for those with low, t = −3.62, p < .001, LLCI = −.0152, ULCI = −.0044, and moderate, t = −3.31, p = .002, LLCI = −.0095, ULCI = −.0024, PTSD symptom levels, but this relationship was not present for those with high PTSD symptom levels, t = −1.01, p = .32, LLCI = −.0050, ULCI = .0016 (See Figure 1). The model accounted for 17.4% of the variance in SCR-rest. Results held when controlling for race (White vs. Black), B = .0005, SE = .0002, p = .007. In the second moderation model, however, a significant interaction between derealization and PTSD symptoms on SCR-rest was not found, B = .0001, SE = .0001, p = .68.
Figure 1.
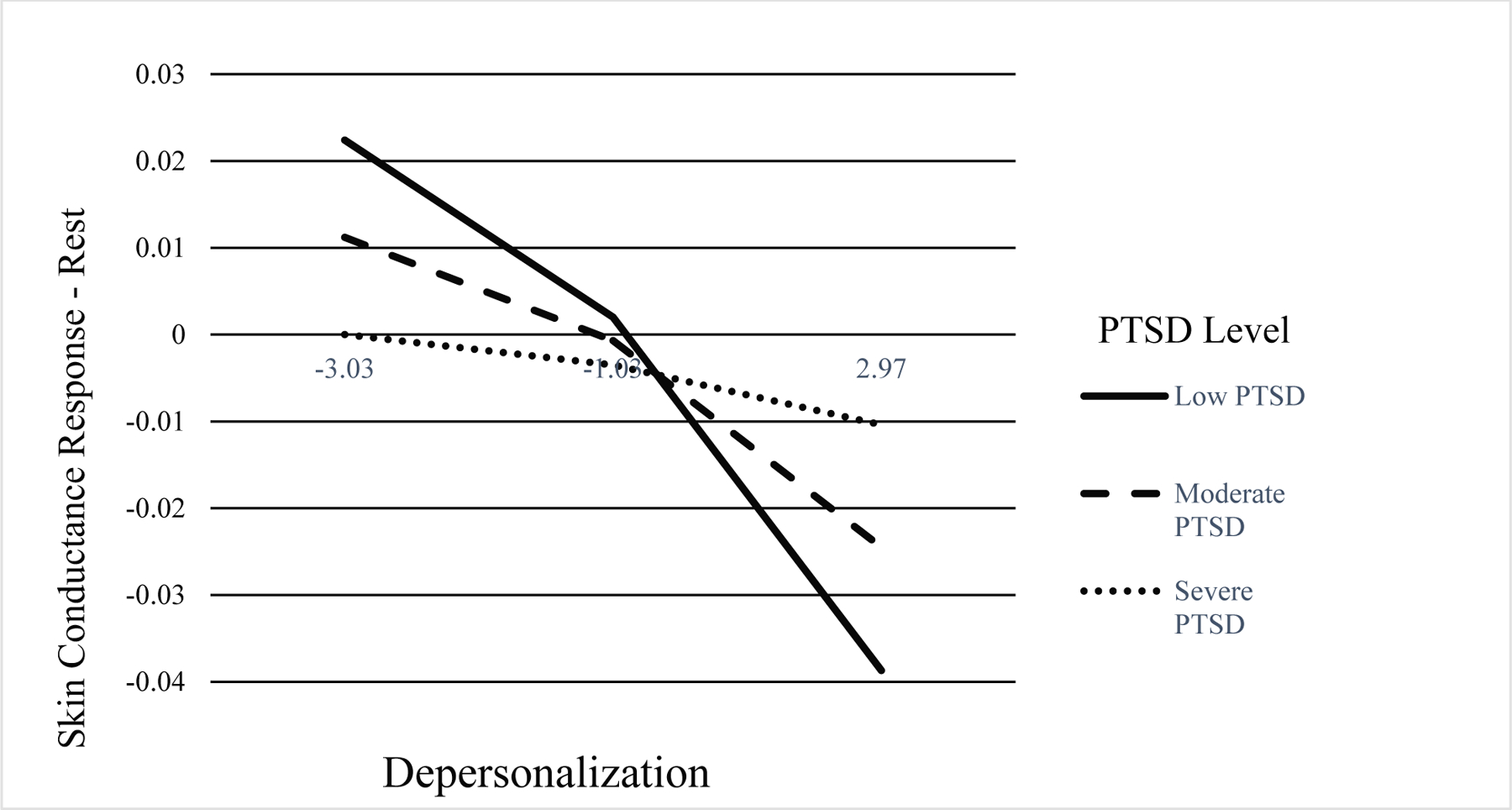
Depersonalization by PTSD Symptom Level Interaction
Note. PTSD symptom level groups = Low (−1 SD), Moderate (Mean), and Severe (+1 SD)
The third moderation model indicated depersonalization and PTSD symptoms interacted to predict SCR-breath, B = −.0006, SE = .0003, p = .03, accounting for 15.0% of the variance. There was a significant positive relationship between depersonalization and SCR-breath for participants with low, t = 3.17, p = .002, LLCI = .0054, ULCI = .0237, and moderate, t = 3.12, p = .003, LLCI = .0033, ULCI = .0150, PTSD symptom levels. This relationship was not observed among those with high PTSD symptom levels, t = 1.35, p = .18, LLCI = −.0018, ULCI = .0094 (See Figure 2). Findings were unchanged when controlling for race (White vs. Black), B = −.0005, SE = .0003, p = .03. For the fourth moderation model, similar to the findings with derealization for the resting control condition, a significant interaction between derealization and PTSD symptoms on SCR-breath was not found, B = −.0001, SE = .0002, p = .59.
Figure 2.
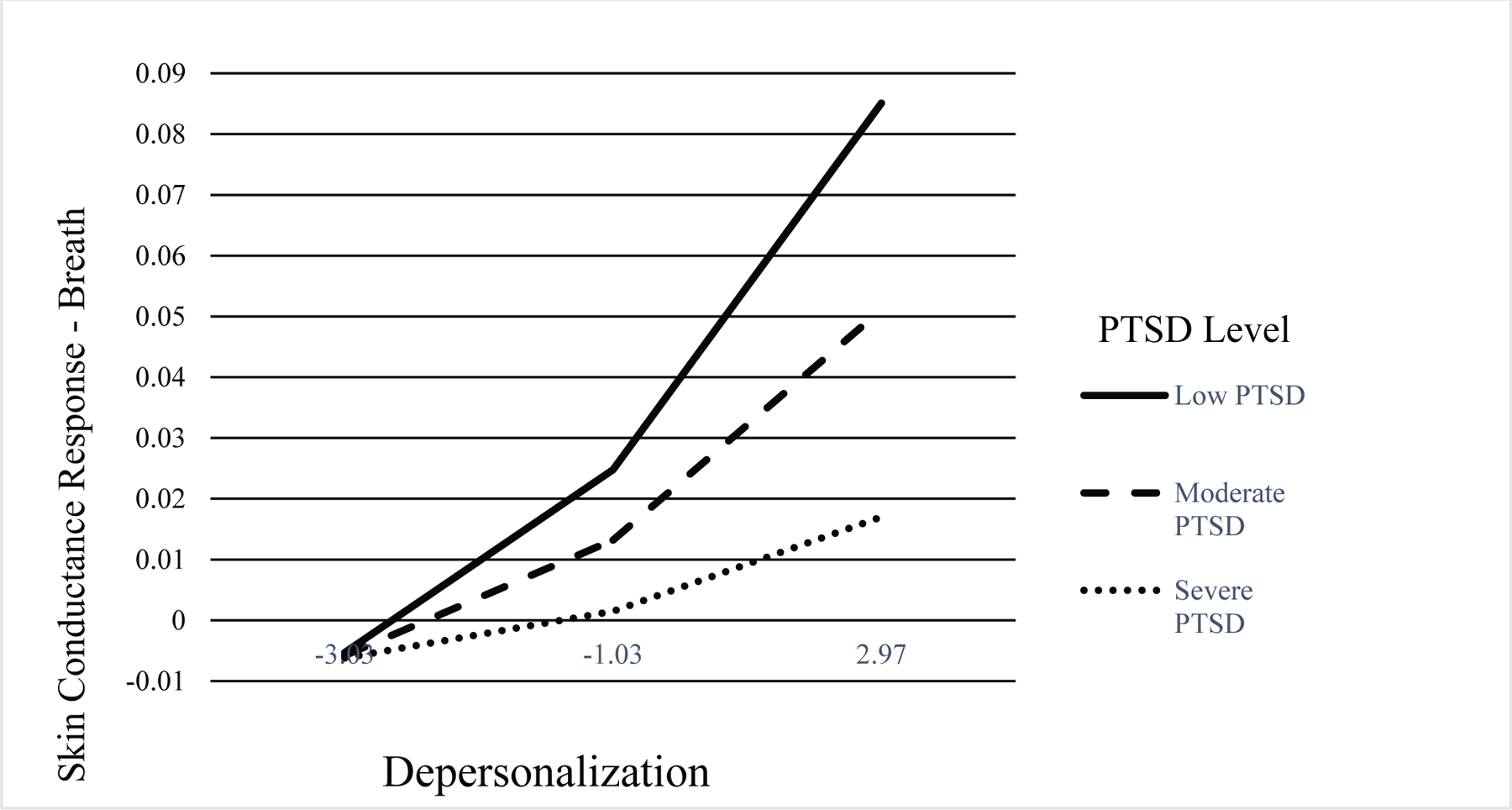
Depersonalization by PTSD Symptom Level Interaction
Note. PTSD symptom level groups = Low (−1 SD), Moderate (Mean), and Severe (+1 SD)
Discussion
The present study is the first to examine SCR in relation to two facets of dissociation used to define the dissociative subtype of PTSD – depersonalization and derealization – in a trauma-exposed, female, predominantly Black sample. Specifically, the associations between dissociative symptoms and SCR during two conditions – resting control and breath-focused mindfulness – were examined in the context of concurrent PTSD symptoms. Depersonalization, but not derealization, was negatively associated with SCR during the resting control condition but positively associated with SCR during the breath condition at low and moderate PTSD symptom levels. Overall, results suggest different types of dissociative symptoms have unique autonomic signatures in the context of PTSD symptoms.
Higher depersonalization was associated with relatively lower SCR during the resting control condition. In line with prior research indicating that repeated, inescapable or early-onset traumas contribute to diminished SCR (D’Andrea et al., 2013; Quevedo et al., 2010), chronic trauma exposure may have contributed to participants with depersonalization symptoms exhibiting lower resting SCR. Indeed, the larger parent study has documented high rates of trauma exposure characterized by multiple trauma types and chronic stressors (i.e., poverty, racism) in the current population (Gillespie et al., 2009). However, this same pattern was not found for derealization symptoms, suggesting feelings of disconnection from self but not surroundings are related to reduced SCR during the resting control condition. Current results are consistent with previous findings indicating depersonalization and derealization are associated with unique patterns of autonomic withdrawal or suppression. For example, in a recent study examining autonomic arousal in response to simulated body-threats, increased depersonalization was associated with suppression of SCR related to threat to self, while increased derealization was associated with suppression of SCR related to threat to others (Dewe et al., 2018). Future studies should consider the potential roles of trauma-type and self-referential processing in the associations among depersonalization, PTSD symptoms, and SCR.
Depersonalization and PTSD symptoms interacted to predict SCR during the resting control condition; more specifically, the negative relationship between depersonalization and SCR was apparent for those with low and average levels of PTSD symptoms but not for those with high levels of PTSD symptoms. Perhaps, greater depersonalization symptoms serve to suppress the increased physiological arousal that often characterizes severe PTSD. This is evidenced by our finding that participants with high levels of PTSD symptoms alone had relatively high SCR during the resting control condition, and therefore greater levels of physiological activation even at rest, when compared to those with higher depersonalization symptoms. Contrarily, individuals who self-reported higher levels of depersonalization symptoms and low PTSD symptoms had the lowest SCR during the resting control condition, pointing to less sympathetic activation; this physiological blunting may be due to the presence of depersonalization symptoms in conjunction with an absence of PTSD symptoms or having few PTSD symptoms that fall within a single cluster.
When engaging in breath-focused mindfulness, however, a different pattern of associations emerged; depersonalization symptoms were associated with relatively higher SCR in participants with low- to moderate PTSD symptoms. Results indicate that engaging in an effortful emotion regulation strategy, such as breath-focused mindfulness, may be linked to increased physiological arousal in trauma-exposed individuals with a tendency to experience depersonalization. It is possible that emotion regulation in the form of breath-focused mindfulness is particularly difficult (Luberto et al., 2020) for those who tend to detach from their bodies. This could serve as a treatment barrier or lead to increased treatment attrition, particularly among treatments that require emotion regulation in the context of highly arousing information, such as recollection of trauma memories in exposure-based therapies. Alternatively, this higher SCR may represent a correction from blunted sympathetic tone to a normative baseline because mindful attention to breath contributes to an increased ability to orient to the present moment. Because a present-orientation is a common goal of mindfulness-based interventions, these strategies may help prepare highly dissociative individuals for trauma-focused treatments. Indeed, prior literature has shown that highly dissociative trauma-exposed individuals are more likely to drop out or show treatment non-response (or minimal response), potentially due to the fact that their arousal levels may not be within the “therapeutic window” for such exposure-based treatments (Frewen & Lanius, 2006; Lanius et al., 2010). Findings suggest that highly dissociative, depersonalizing individuals may require additional support (e.g., emotion awareness/skills training) to experience the optimal level of physiological arousal to successfully engage in these treatments.
It is important to note that our study sample primarily consisted of Black women with few socioeconomic resources and histories of chronic trauma exposure. Notably, several variables that are indicative of structural inequity, including age, race, income, and education level, were not related to SCL in the current sample. Given participants’ intersecting vulnerabilities, however, many have likely experienced various forms of individual discrimination and systematic marginalization, including racial trauma and gendered racism (Comas-Díaz et al., 2019; Moody & Lewis, 2019). For People of Color, racism can be a chronic, inescapable stressor with adverse physiological consequences, including increased (Karmali et al., 2017) or blunted skin conductance (Harnett et al., 2023) and reduced heart rate variability (Hill et al., 2017). Because Black Americans experience racism more frequently than any other racial group (Anderson & Stevenson, 2019), the potential role of experiences of racism and other forms of discrimination in the associations between dissociative and PTSD symptoms and SCR need to be explored among Black women.
Several limitations should be considered when drawing conclusions. Findings should be interpreted in light of the study’s cross-sectional methodology and reliance on clinician-administered self-report measures. In addition, all of the present sample reported female sex, meaning male and intersex individuals were not represented, pointing to an important area of future research. Despite limitations, this study has several strengths, including a racially diverse, community-based sample. Namely, our sample primarily consisted of Black women with limited socioeconomic resources, which represents a strength given the paucity of research on mindfulness in diverse communities. Further, P eople of C olor, particularly Black individuals, historically have been excluded from psychophysiological studies of psychiatric disorders (J. L. Price et al., 2022). Our use of validated dissociative and PTSD symptom measures, as opposed to diagnoses, also represents a strength in that it provides a naturalistic view of the population.
Altogether, we found that depersonalization can manifest in different autonomic responses at resting control versus emotion regulation in the context of low-to-moderate PTSD symptomology, pointing to important implications for research and clinical practice. First, findings highlight the importance of accounting for potential PTSD symptoms and study conditions (i.e., resting control, breath-focused mindfulness) when examining the relationship between depersonalization and SCR. In line with previous research (D’Andrea et al., 2013), our results suggest that, at rest, depersonalization symptoms contribute to a responding pattern that more closely reflects physiological withdrawal or blunted reactivity, perhaps to allow disconnection from the self in response to internal or external trauma-related stimuli or preemptively dissociate to avoid anticipated stimuli; however, this pattern is reversed during breath-focused mindfulness. As such, highly dissociative individuals may need additional support to successfully engage in emotion regulation interventions, from mindfulness to exposure-based treatments.
Second, another important area of future work concerns the associations between other types of dissociative symptoms, such as emotional constriction or identity disturbances, in relation to SCR in the context of PTSD symptoms. In addition, further studies should consider how depersonalization interacts with other trauma responses to influence autonomic regulation in highly trauma-exposed populations. Additional inquiry into depersonalization’s associations with other markers of autonomic dysfunction, including heart rate variability and pupil diameter, in the context of PTSD symptomology is necessary to obtain a more comprehensive understanding of the impact of co-occurring depersonalization and PTSD symptoms on autonomic regulation.
Lastly, it is critical to assess dissociation throughout treatment to streamline trauma-focused intervention and enhance overall functioning (Boyer et al., 2022). Without routine assessment, clinicians often remain unaware of the potential impact of dissociative symptoms on patients’ treatment engagement and PTSD symptom reduction, whereas knowledge of baseline dissociative symptoms can enhance clinicians’ understanding of patient progress. Moreover, clinicians who regularly monitor patients’ dissociation levels can develop informed treatment plans that address dissociative symptoms prior to beginning exposure-based PTSD treatments and adapt these plans accordingly (Lanius et al., 2012).
Supplementary Material
Highlights.
Depersonalization and PTSD symptoms interacted to predict skin conductance response.
Depersonalization can manifest in different autonomic responses.
It is critical to assess dissociation throughout treatment to better understand presentation.
Acknowledgment
This work was supported by National Institutes of Mental Health (MH101380 to NF), the National Center for Complementary and Integrative Health (AT011267 to NF and GJS), the Emory Medical Care Foundation and Emory University Research Council, the American Psychological Association, Society for Clinical Neuropsychology. We wish to thank Allen Graham, Rebecca Hinrichs, and Angelo Brown, as well as members of the Fani laboratory and Grady Trauma Project for their assistance with data collection. We thank all of our participants for their time and involvement in this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: None.
Conflict of Interest
None of the authors (ECL, AG, DLLB, AT, AP, GJS, NF) report financial disclosures or conflicts of interest.
Contributor Information
Emma C. Lathan, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA.
Alfonsina Guelfo, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA.
Dominique L. La Barrie, Department of Psychology, University of Georgia, Athens, GA.
Andrew Teer, Home Base, a Red Sox Foundation and Massachusetts General Hospital Program, Massachusetts General Hospital, Charlestown, MA, Department of Psychiatry, Harvard Medical School, Cambridge, MA.
Abigail Powers, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA.
Greg Siegle, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA.
Negar Fani, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA.
Data Availability Statement:
The data and materials that support the results or analyses presented in this study will be made available via email to the corresponding author, EL (emma.catherine.lathan-powell@emory.edu), upon reasonable request.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Anderson RE, & Stevenson HC (2019). RECASTing racial stress and trauma: Theorizing the healing potential of racial socialization in families. American Psychologist, 74(1), 63–75. 10.1037/amp0000392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey TD, & Brand BL (2017). Traumatic dissociation: Theory, research, and treatment. Clinical Psychology: Science and Practice, 24(2), 170–185. 10.1111/cpsp.12195 [DOI] [Google Scholar]
- Beutler S, Mertens YL, Ladner L, Schellong J, Croy I, & Daniels JK (2022). Trauma-related dissociation and the autonomic nervous system: A systematic literature review of psychophysiological correlates of dissociative experiencing in PTSD patients. European Journal of Psychotraumatology, 13(2), 2132599. 10.1080/20008066.2022.2132599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blain S, Mihailidis A, & Chau T (2008). Assessing the potential of electrodermal activity as an alternative access pathway. Medical Engineering & Physics, 30(4), 498–505. 10.1016/j.medengphy.2007.05.015 [DOI] [PubMed] [Google Scholar]
- Boulet C, Lopez-Castroman J, Mouchabac S, Olié E, Courtet P, Thouvenot E, Abbar M, & Conejero I (2022). Stress response in dissociation and conversion disorders: A systematic review. Neuroscience & Biobehavioral Reviews, 132, 957–967. 10.1016/j.neubiorev.2021.10.049 [DOI] [PubMed] [Google Scholar]
- Boyer SM, Caplan JE, & Edwards LK (2022). Trauma-Related Dissociation and the Dissociative Disorders: Delaware Journal of Public Health, 8(2), 78–84. 10.32481/djph.2022.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J, Weathers FW, & Runtz M (2005). Is dissociation a multidimensional construct? Data from the Multiscale Dissociation Inventory. Journal of Traumatic Stress, 18(3), 221–231. 10.1002/jts.20024 [DOI] [PubMed] [Google Scholar]
- Choi KR, Seng JS, Briggs EC, Munro-Kramer ML, Graham-Bermann SA, Lee RC, & Ford JD (2017). The Dissociative Subtype of Posttraumatic Stress Disorder (PTSD) Among Adolescents: Co-Occurring PTSD, Depersonalization/Derealization, and Other Dissociation Symptoms. Journal of the American Academy of Child & Adolescent Psychiatry, 56(12), 1062–1072. 10.1016/j.jaac.2017.09.425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comas-Díaz L, Hall GN, & Neville HA (2019). Racial trauma: Theory, research, and healing: Introduction to the special issue. American Psychologist, 74(1), 1–5. 10.1037/amp0000442 [DOI] [PubMed] [Google Scholar]
- D’Andrea W, Pole N, DePierro J, Freed S, & Wallace DB (2013). Heterogeneity of defensive responses after exposure to trauma: Blunted autonomic reactivity in response to startling sounds. International Journal of Psychophysiology, 90(1), 80–89. 10.1016/j.ijpsycho.2013.07.008 [DOI] [PubMed] [Google Scholar]
- Dewe H, Watson DG, & Braithwaite JJ (2016). Uncomfortably numb: New evidence for suppressed emotional reactivity in response to body-threats in those predisposed to sub-clinical dissociative experiences. Cognitive Neuropsychiatry, 21(5), 377–401. 10.1080/13546805.2016.1212703 [DOI] [PubMed] [Google Scholar]
- Dewe H, Watson DG, Kessler K, & Braithwaite JJ (2018). The depersonalized brain: New evidence supporting a distinction between depersonalization and derealization from discrete patterns of autonomic suppression observed in a non-clinical sample. Consciousness and Cognition, 63, 29–46. 10.1016/j.concog.2018.06.008 [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Badeck S, Beckmann C, Wagner A, Feige B, Weiss I, Lieb K, & Bohus M (2005). Affective dysregulation and dissociative experience in female patients with borderline personality disorder: A startle response study. Journal of Psychiatric Research, 39(1), 85–92. 10.1016/j.jpsychires.2004.05.001 [DOI] [PubMed] [Google Scholar]
- Falsetti SA, Resnick HS, Resick PA, & Kilpatrick D (1993). The Modified PTSD Symptom Scale: A brief self-report measure of posttraumatic stress disorder 16, 161–162. [Google Scholar]
- Fonkoue IT, Marvar PJ, Norrholm S, Li Y, Kankam ML, Jones TN, Vemulapalli M, Rothbaum B, Bremner JD, Le N-A, & Park J (2020). Symptom severity impacts sympathetic dysregulation and inflammation in post-traumatic stress disorder (PTSD). Brain, Behavior, and Immunity, 83, 260–269. 10.1016/j.bbi.2019.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, & Lanius RA (2006). Neurobiology of Dissociation: Unity and Disunity in Mind–Body–Brain. Psychiatric Clinics of North America, 29(1), 113–128. 10.1016/j.psc.2005.10.016 [DOI] [PubMed] [Google Scholar]
- Fusco RA, Yuan Y, Lee H, & Newhill CE (2021). Trauma, Sleep and Mental Health Problems in Low-Income Young Adults. International Journal of Environmental Research and Public Health, 18(3), 1145. 10.3390/ijerph18031145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, Weiss T, Schwartz AC, Cubells JF, & Ressler KJ (2009). Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry, 31(6), 505–514. 10.1016/j.genhosppsych.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnett NG, Fani N, Carter S, Sanchez LD, Rowland GE, Davie WM, Guzman C, Lebois LAM, Ely TD, van Rooij SJH, Seligowski AV, Winters S, Grasser LR, Musey PI, Seamon MJ, House SL, Beaudoin FL, An X, Zeng D, … Ressler KJ (2023). Structural inequities contribute to racial/ethnic differences in neurophysiological tone, but not threat reactivity, after trauma exposure. Molecular Psychiatry 10.1038/s41380-023-01971-x [DOI] [PMC free article] [PubMed]
- Herrero H, Tarrada A, Haffen E, Mignot T, Sense C, Schwan R, EL-Hage W, Maillard L, & Hingray C (2020). Skin conductance response and emotional response in women with psychogenic non-epileptic seizures. Seizure, 81, 123–131. 10.1016/j.seizure.2020.07.028 [DOI] [PubMed] [Google Scholar]
- Hill LK, Hoggard LS, Richmond AS, Gray DL, Williams DP, & Thayer JF (2017). Examining the association between perceived discrimination and heart rate variability in African Americans. Cultural Diversity and Ethnic Minority Psychology, 23(1), 5–14. 10.1037/cdp0000076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinrichs R, Michopoulos V, Winters S, Rothbaum AO, Rothbaum BO, Ressler KJ, & Jovanovic T (2017). Mobile assessment of heightened skin conductance in posttraumatic stress disorder: H INRICHS ET AL . Depression and Anxiety, 34(6), 502–507. 10.1002/da.22610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn M, Fovet T, Vaiva G, Thomas P, Amad A, & D’Hondt F (2020). Emotional response in depersonalization: A systematic review of electrodermal activity studies. Journal of Affective Disorders, 276, 877–882. 10.1016/j.jad.2020.07.064 [DOI] [PubMed] [Google Scholar]
- Jänig W (2022). The Integrative Action of the Autonomic Nervous System: Neurobiology of Homeostasis (2nd ed.). Cambridge University Press. 10.1017/9781108778411 [DOI] [Google Scholar]
- Karmali F, Kawakami K, & Page-Gould E (2017). He said what? Physiological and cognitive responses to imagining and witnessing outgroup racism. Journal of Experimental Psychology: General, 146(8), 1073–1085. 10.1037/xge0000304 [DOI] [PubMed] [Google Scholar]
- Kozlowska K, Walker P, McLean L, & Carrive P (2015). Fear and the Defense Cascade: Clinical Implications and Management. Harvard Review of Psychiatry, 23(4), 263–287. 10.1097/HRP.0000000000000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanius RA, Brand B, Vermetten E, Frewen PA, & Spiegel D (2012). THE DISSOCIATIVE SUBTYPE OF POSTTRAUMATIC STRESS DISORDER: RATIONALE, CLINICAL AND NEUROBIOLOGICAL EVIDENCE, AND IMPLICATIONS: Dissociative Subtype of PTSD. Depression and Anxiety, 29(8), 701–708. 10.1002/da.21889 [DOI] [PubMed] [Google Scholar]
- Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, & Spiegel D (2010). Emotion Modulation in PTSD: Clinical and Neurobiological Evidence for a Dissociative Subtype. American Journal of Psychiatry, 167(6), 640–647. 10.1176/appi.ajp.2009.09081168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebois LAM, Harnett NG, van Rooij SJH, Ely TD, Jovanovic T, Bruce SE, House SL, Ravichandran C, Dumornay NM, Finegold KE, Hill SB, Merker JB, Phillips KA, Beaudoin FL, An X, Neylan TC, Clifford GD, Linnstaedt SD, Germine LT, … Ressler KJ (2022). Persistent Dissociation and Its Neural Correlates in Predicting Outcomes After Trauma Exposure. American Journal of Psychiatry, 179(9), 661–672. 10.1176/appi.ajp.21090911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luberto CM, Hall DL, Park ER, Haramati A, & Cotton S (2020). A Perspective on the Similarities and Differences Between Mindfulness and Relaxation. Global Advances in Health and Medicine, 9, 216495612090559. 10.1177/2164956120905597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTeague LM, Lang PJ, Laplante M-C, Cuthbert BN, Shumen JR, & Bradley MM (2010). Aversive Imagery in Posttraumatic Stress Disorder: Trauma Recurrence, Comorbidity, and Physiological Reactivity. Biological Psychiatry, 67(4), 346–356. 10.1016/j.biopsych.2009.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekawi Y, Kuzyk E, Dixon HD, McKenna B, Camacho L, de Andino AM, Stevens J, Michopolous V, & Powers A (2021). Characterizing Typologies of Polytraumatization: A Replication and Extension Study Examining Internalizing and Externalizing Psychopathology in an Urban Population. Clinical Psychological Science, 9(6), 1144–1163. 10.1177/21677026211000723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michal M, Koechel A, Canterino M, Adler J, Reiner I, Vossel G, Beutel ME, & Gamer M (2013). Depersonalization Disorder: Disconnection of Cognitive Evaluation from Autonomic Responses to Emotional Stimuli. PLoS ONE, 8(9), e74331. 10.1371/journal.pone.0074331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moody AT, & Lewis JA (2019). Gendered Racial Microaggressions and Traumatic Stress Symptoms Among Black Women. Psychology of Women Quarterly, 43(2), 201–214. 10.1177/0361684319828288 [DOI] [Google Scholar]
- Morris MC, & Rao U (2013). Psychobiology of PTSD in the acute aftermath of trauma: Integrating research on coping, HPA function and sympathetic nervous system activity. Asian Journal of Psychiatry, 6(1), 3–21. 10.1016/j.ajp.2012.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr SP, Metzger LJ, Lasko NB, Macklin ML, Peri T, & Pitman RK (2000). De novo conditioning in trauma-exposed individuals with and without posttraumatic stress disorder. Journal of Abnormal Psychology, 109(2), 290–298. 10.1037/0021-843X.109.2.290 [DOI] [PubMed] [Google Scholar]
- Orr SP, Metzger LJ, & Pitman RK (2002). Psychophysiology of post-traumatic stress disorder. Psychiatric Clinics of North America, 25(2), 271–293. 10.1016/S0193-953X(01)00007-7 [DOI] [PubMed] [Google Scholar]
- Platt MG, & Freyd JJ (2015). Betray my trust, shame on me: Shame, dissociation, fear, and betrayal trauma. Psychological Trauma: Theory, Research, Practice, and Policy, 7(4), 398–404. 10.1037/tra0000022 [DOI] [PubMed] [Google Scholar]
- Price JL, Bruce MA, & Adinoff B (2022). Addressing Structural Racism in Psychiatry With Steps to Improve Psychophysiologic Research. JAMA Psychiatry, 79(1), 70. 10.1001/jamapsychiatry.2021.2663 [DOI] [PubMed] [Google Scholar]
- Price M, Kearns M, Houry D, & Rothbaum BO (2014). Emergency department predictors of posttraumatic stress reduction for trauma-exposed individuals with and without an early intervention. Journal of Consulting and Clinical Psychology, 82(2), 336–341. 10.1037/a0035537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quevedo K, Smith T, Donzella B, Schunk E, & Gunnar M (2010). The startle response: Developmental effects and a paradigm for children and adults. Developmental Psychobiology, 52(1), 78–89. 10.1002/dev.20415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sack M, Cillien M, & Hopper JW (2012). Acute dissociation and cardiac reactivity to script-driven imagery in trauma-related disorders. European Journal of Psychotraumatology, 3(1), 17419. 10.3402/ejpt.v3i0.17419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer M, & Elbert T (2010). Dissociation Following Traumatic Stress: Etiology and Treatment. Zeitschrift für Psychologie / Journal of Psychology, 218(2), 109–127. 10.1027/0044-3409/a000018 [DOI] [Google Scholar]
- Schimmenti A (2018). The trauma factor: Examining the relationships among different types of trauma, dissociation, and psychopathology. Journal of Trauma & Dissociation, 19(5), 552–571. 10.1080/15299732.2017.1402400 [DOI] [PubMed] [Google Scholar]
- Schoenberg PLA, Sierra M, & David AS (2012). Psychophysiological Investigations in Depersonalization Disorder and Effects of Electrodermal Biofeedback. Journal of Trauma & Dissociation, 13(3), 311–329. 10.1080/15299732.2011.606742 [DOI] [PubMed] [Google Scholar]
- Seligowski AV, Lebois LAM, Hill SB, Kahhale I, Wolff JD, Jovanovic T, Winternitz SR, Kaufman ML, & Ressler KJ (2019). Autonomic responses to fear conditioning among women with PTSD and dissociation. Depression and Anxiety, 36(7), 625–634. 10.1002/da.22903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semiz UB, Inanc L, & Bezgin CH (2014). Are trauma and dissociation related to treatment resistance in patients with obsessive–compulsive disorder? Social Psychiatry and Psychiatric Epidemiology, 49(8), 1287–1296. 10.1007/s00127-013-0787-7 [DOI] [PubMed] [Google Scholar]
- Sierra M, Senior C, Dalton J, McDonough M, Bond A, Phillips ML, O’Dwyer AM, & David AS (2002). Autonomic Response in Depersonalization Disorder. Archives of General Psychiatry, 59(9), 833. 10.1001/archpsyc.59.9.833 [DOI] [PubMed] [Google Scholar]
- Sierra M, Senior C, Phillips ML, & David AS (2006). Autonomic response in the perception of disgust and happiness in depersonalization disorder. Psychiatry Research, 145(2–3), 225–231. 10.1016/j.psychres.2005.05.022 [DOI] [PubMed] [Google Scholar]
- Spitzer C, Barnow S, Freyberger HJ, & Joergen Grabe H (2007). Dissociation Predicts Symptom-Related Treatment Outcome in Short-Term Inpatient Psychotherapy. Australian & New Zealand Journal of Psychiatry, 41(8), 682–687. 10.1080/00048670701449146 [DOI] [PubMed] [Google Scholar]
- Williamson JB, Porges EC, Lamb DG, & Porges SW (2015). Maladaptive autonomic regulation in PTSD accelerates physiological aging. Frontiers in Psychology, 5. 10.3389/fpsyg.2014.01571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Lunney CA, Miller MW, Resick PA, Friedman MJ, & Schnurr PP (2012). THE DISSOCIATIVE SUBTYPE OF PTSD: A REPLICATION AND EXTENSION: Research Article: The Dissociative Subtype of PTSD. Depression and Anxiety, 29(8), 679–688. 10.1002/da.21946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Reardon AF, Ryabchenko KA, Castillo D, & Freund R (2012). A Latent Class Analysis of Dissociation and Posttraumatic Stress Disorder: Evidence for a Dissociative Subtype. Archives of General Psychiatry, 69(7). 10.1001/archgenpsychiatry.2011.1574 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data and materials that support the results or analyses presented in this study will be made available via email to the corresponding author, EL (emma.catherine.lathan-powell@emory.edu), upon reasonable request.


