Summary
India has run multiple Government-Funded Health Insurance schemes (GFHIS) over the past decades to ensure affordable healthcare. We assessed GFHIS evolution with a special focus on two national schemes - Rashtriya Swasthya Bima Yojana (RSBY) and Pradhan Mantri Jan Arogya Yojana (PMJAY). RSBY suffered from a static financial coverage cap, low enrollment, inequitable service supply, utilization, etc. PMJAY expanded coverage and mitigated some of RSBY's drawbacks. Investigating equity in PMJAY's supply and utilization across geography, sex, age, social groups, and healthcare sectors depicts several systemic skews. Kerala and Himachal Pradesh with low poverty and disease burden use more services. Males are more likely to seek care under PMJAY than females. Mid-age population (19–50 years) is a common group availing services. Scheduled Caste and Scheduled Tribe people have low service utilization. Most hospitals providing services are private. Such inequities can lead the most vulnerable populations further into deprivation due to healthcare inaccessibility.
Keywords: Government Funded Health Insurance, Universal Health Coverage, Pradhan Mantri Jan Aarogya Yojna, Rashtriya Swasthya Bima Yojna, Health Equity, Ayushman Bharat Yojana
Introduction
In 2019, 193 countries including India unanimously affirmed their strong political commitment to universal health coverage (UHC) in a high-level meeting conducted by the United Nations.1,2 UHC means that all individuals receive quality health services without suffering financial hardship.2 Achieving UHC is, therefore, subject to a geographically and financially accessible, and culturally appropriate health system with adequate and quality human resources and infrastructure. According to the 75th round (2017–18) of the National Sample Survey, 12% Indians have unmet health needs.3 Inability to afford healthcare i.e. financial inaccessibility is one of the factors responsible for the unmet needs and, therefore, is a hindrance to UHC in India.3
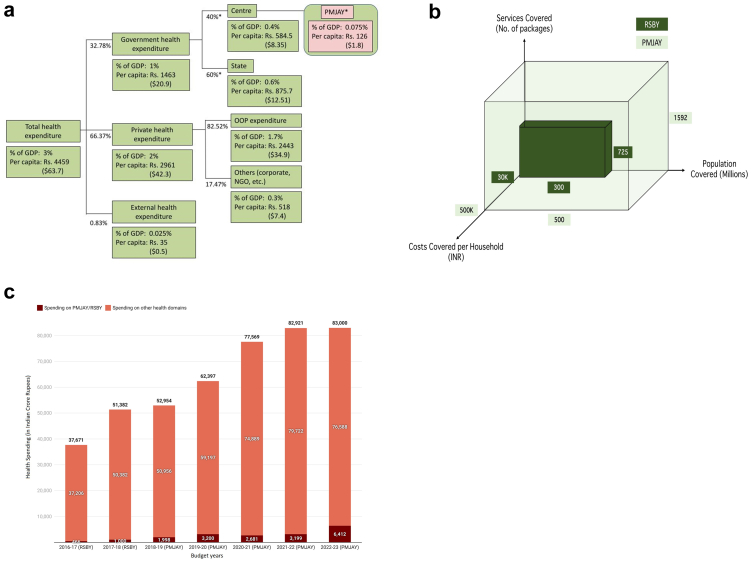
India's healthcare is financed by multiple sources - domestic government sources, private sources, and external/global sources (Fig. 1a). Out-of-pocket expenditure (OOPE), a major source of health financing in the country, contributes to 54.7% of total health expenditure.4 High OOPE has several disadvantages. First, financial shock due to OOPE can push people into poverty and can force them to cut down subsistence costs (food and clothing).5 Second, OOPE contributes to low health service utilization rates as people may avoid using unaffordable services.5 Third, OOPE is an inequitable and regressive health expenditure method as everyone pays the same fee for the service regardless of differences in paying ability. Hence, the felt burden of OOPE is greater on people in lower wealth quintiles than those in the upper wealth quintiles.6 In India, in 2018, 16.51% people faced catastrophic health expenses i.e. CHE (at a 10% threshold level), and 3.3% people were pushed into poverty due to OOPE on health.7,8
Fig. 1.
Financing of health system and GFHIS in India. (a) Sources of healthcare financing in India, (b) Universal health coverage (UHC) Cubes: RSBY vs PMJAY, (c) Central Government spending on PMJAY/RSBY scheme and other health domains (in crore Indian Rupees). GDP: Gross Domestic Product, PMJAY: Pradhan Mantri Jan Arogya Yojana, RSBY: Rashtriya Swasthya Bima Yojana, OOP: Out-of-pocket, NGO: non-government organization. In figure (a), values for various sources of health expenditure were taken from World Bank 2019 and ∗ indicates authors' calculation. GDP of India was Rs. 198 lakh crore and the population was 136 crore in 2019 @ 1$ = Rs. 70.4. External health expenditure is the share of total health expenditure funded from outside the country (foreign source). In figure (c) values of central government spending is taken from Union Budget of India. For year, 2021-22 spending values indicate budget estimates, for 2020-21 spending values indicate revised estimates, and for the rest of the years spending values indicate actual spending.
Among several, one way to reduce OOPE is by increasing government health expenditure (GHE). The government spends on infrastructure, human resources, and service delivery at public hospitals, vertical health programs, and government-funded health insurance schemes (GFHIS). The current review focuses exclusively on GFHIS due to three reasons. First, the share of GFHIS and other forms of health insurance schemes in the overall health financing has increased several folds in India.9 Second, there is limited literature on how multiple GFHIS have operated and evolved, especially the recent Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) or PMJAY. Third, PMJAY is high on India's health policy and political agenda. Under GFHIS, healthcare costs are subsidized or paid for entirely by the government. Ideally, GFHIS should provide financial protection to the entire population. However, there is a huge economic divide in India with around 10.01% of people still living under the international poverty line of $2.15 per day.10 The vulnerable population groups e.g. Scheduled Castes, Other Backward Classes, Islamic population, and families with children and elderly have higher cases of CHE.7 Also, the incidence of impoverishing health expenditure (IHE) is higher in rural areas and poorer states compared to urban areas and richer states.7 Therefore, the government prioritizes the protection of people with low household incomes and at risk of impoverishment by covering their healthcare expenditures. Details about the differences in demography and geography of India are given in Panel 1. Recently, in 2018, India launched one of the biggest GFHIS, PMJAY, to protect its vulnerable populations.22 This scheme does not ensure UHC but protects the most vulnerable people from financial hardships encouraging them to seek healthcare which is a step toward UHC.23
Panel 1. Geography, demography, social structure and development of India.
India is the world's most populated lower-middle-income country located in South Asia. As of 2022, India has 28 states and 8 union territories comprising 766 districts. There are well-documented developmental and healthcare inequities across states. For example, states such as Uttar Pradesh, Madhya Pradesh, and Chhattisgarh are comparable to the sub-Saharan African nation, Djibouti and the north African nation, Sudan with regards to life expectancy while others such as Delhi and Kerala see life expectancy as high as Vietnam.11 States are divided into smaller units called districts. Aspirational districts are the 117 districts that have been identified as facing critical developmental challenges and are targeted for rapid transformation and investments.
As per World Bank, the GDP per capita of India in 2021 is US$2277.12 However, there is massive economic inequality in the country with the top 10% holding 57% of the national income while the bottom 50% sharing just 13%.13 Based on 2012 Reserve Bank of India estimates, 270 million people (21.92%) are below the poverty line with the number being as low as 5% for Goa while as high as 40% for Chhattisgarh.
In 2018–20, the sex ratio at birth is 907 females per 1000 males, and this has improved over the past two decades. Kerala has the highest sex ratio (974) while Uttarakhand (844) has the lowest.14 The median age of Indians in 2022 is 28.7 years with 63.6% of the population belonging to 15–64 years.15 As per World Bank estimates, the average life expectancy of Indians in 2020 is 70 years and has increased by seven years in the last two decades.16 The literacy rate of India in 2017–18 is 73.2% with Mizoram (98%) having the highest and Andhra Pradesh having the lowest rate (61%). The adult female literacy rate (64.6%) is lower than the male literacy (81.5%).17 The labour force participation rates are 25.1% and 57.5% for females and males as per the Periodic Labour Force Survey of 2020–21.18
The 2011 Census noted that 79.8% of the population are Hindu, 14.2% are Muslim, 2.3% are Christian, 1.7% are Sikh, 0.7% are Buddhist, and 0.4% are Jain.19 The Indian population is classified into several social groups or castes. As per the socio-economic and caste census 2011, 19.7% of people in India belong to Scheduled Castes (SCs), 8.5% to Scheduled Tribes (STs), 41.1% to Other Backward Castes (OBCs), and 30.8% to forward castes.20 Religion and caste are major social determinants of health in India. For example, in 2016, the life expectancy at birth is noted to be highest among Christians (68.1 years) followed by Muslims (66), and Hindus (65). Life expectancy at birth of SCs is 63.1 years, STs is 64.0 years, OBCs is 65.1 years, and forward class is 68.0 years.21
In this paper, we aim to
-
1)
investigate the journey of GFHIS and Social Health Insurance Schemes (SHIS) of independent India.
-
2)
critically analyze various aspects of equity for PMJAY's implementation and utilization in the early years (2018–2022).
-
3)
study the implications of expanding PMJAY to include universal population coverage.
India's journey towards UHC through GFHIS
India's ambition towards UHC dates back to 1946, even before its independence from the colonial British government when the Bhore Committee report noted that “… the present medical service should be free to all without distinction and that the contribution from those who can afford to pay should be through the channel of general and local taxation”.24 The Committee acknowledged that a central health insurance fund could be a useful interim future step.24 In 1948, an employer-mandated SHIS - Employees' State Insurance Scheme (ESIS) was instituted to provide health insurance to organized sector workers with the aspiration that economic growth will absorb more people into the organized sector expanding ESIS.25 The Central Government Health Scheme (1954) selectively insured central government employees.26
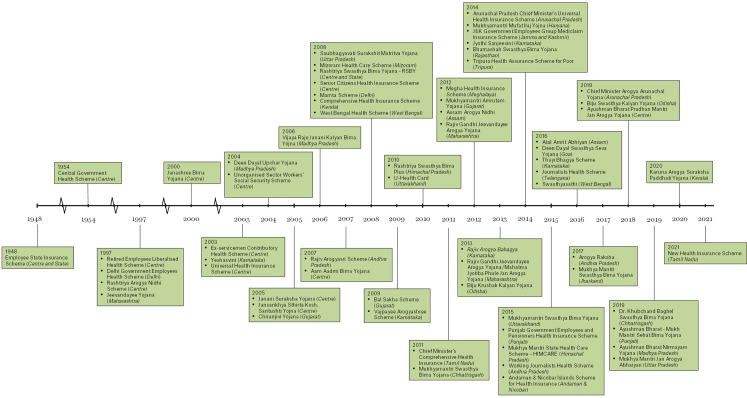
The 1983 National Health Policy (NHP) reinstated India's commitment to “health for all by 2000” and suggested the adoption of state-wise GFHIS.27 Contrary to this recommendation, several national insurance schemes for organized sector workers were launched in the next decade.25 Poor people from the unorganized sector were insured for the first time by Rashtriya Aarogya Nidhi Scheme in 1997 which covered services availed for life-threatening diseases at government hospitals.25 In the same year, the first state GFHIS - Jeevandayee Yojana, was launched in Maharashtra which covered health services in government and select private hospitals for the BPL population.28 This model was later adopted by several states and the Centre (Fig. 2).29 It is important to note that the launch of several state-level GFHIS followed the wave of privatization in the healthcare sector in the 1990s.30 During this period, government investments in the health sector also declined leading to a rise in inadequacies in the public health system.30 As a result, more people started accessing private hospitals that used a fee-for-service model. To protect the population from the risk of financial shock at private hospitals, GFHIS were launched.
Fig. 2.
Timeline of social health insurance and government-funded health insurance schemes in independent India (1947 to 2022). Aam Admi Bima Yojana and Janashree Bima Yojana merged into one scheme on January 01, 2013 and renamed as Aam Admi Bima Yojana.
Taking a different turn than its previous iteration, the NHP 2002 proposed a national GFHIS for the poor delivered through the public and private sectors and suggested district-level pilots to delineate the scheme's administration and logistics.31 In 2003, the Universal Health Insurance Scheme (UHIS), the first national GFHIS of India, was announced by the Ministry of Finance.26 While the scheme was initially launched as “a health insurance scheme for all”, a year later, it was restructured to “only for BPL population”.26 Due to a lack of sufficient coverage, the scheme failed to take off. After UHIS, the government tried to ensure health security for poor people through the Unorganised Sector Workers' Social Security Scheme in 2004.32 The scheme was discontinued at the pilot stage.
Consequently, RSBY was launched in 2008 by the Labour Ministry.33 One major driver for RSBY was the failure of expansion of ESIS as the proportion of organized workers in India's total workforce had not crossed 8% by 2008.25 ESIS also underperformed on both supply-side and demand-side evident by the declining availability of beds, hospitalization rates, and outpatient visits.34 RSBY insured secondary and tertiary-level services availed at public and contracted private hospitals for the BPL population. Details about RSBY are given in Panel 2. In 2012, the High-level Expert Group (HLEG) report on UHC in India proposed that GFHIS should cover all primary and specific secondary- and tertiary-level services including free in- and out-patient care at all public and contracted-in private healthcare facilities for all Indians, regardless of economic class.54 The recommendation resonates with WHO's financial risk protection model ensuring universality.55 Thailand, for instance, has witnessed reduced financial hardships and health outcome benefits by implementing such a model.55 However, in 2017, the new NHP recommended an insurance scheme aligning with existing RSBY excluding primary care services and focusing only on vulnerable populations rather than universal coverage.56 Consequentially, PMJAY, the world's largest GFHIS was launched in 2018. The difference in population, service and cost coverage between RSBY and PMJAY can be seen as a UHC cube in Fig. 1b.
Panel 2. Rashtriya Swasthya Bima Yojana (RSBY).
Scheme objectives and details: RSBY scheme was launched by the Ministry of Labour and Employment in 2008 with two main objectives - First, to reduce the CHE and IHE and improve the population's health-seeking behaviour.35 Second, to overcome supply-side shortages by involving private health providers.35 The scheme provided a cover of Rs. 30,000 per five-member household for secondary and tertiary-level health services to about 30 crore BPL beneficiaries.36 Pre-existing conditions were covered but outpatient and drug costs were excluded.37 The Rs. 30,000 cap was considered sufficient as the average hospitalization cost in 2004–05 was Rs. 9000. It was fiscally manageable and had good staying power with insurance companies.38 The scheme was funded by the central and state governments and beneficiaries paid an annual registration fee of Rs. 30 per household.39
Scheme's successes: RSBY achieved high enrolment rates in comparison to health insurance schemes of countries like Georgia, Mexico, and Vietnam, probably due to the implementation of electronic enrollment records and smart cards.40,41 It received recognition for its cashless, paperless, and portable health service transactions.35 After its implementation, an increase in health service utilization was noted, primarily in private hospitals.42,43 An internal evaluation of the scheme indicated high beneficiary satisfaction rates (90%).35 The number of days lost due to illness decreased by 20.8% on account of RSBY.41
Scheme's Shortcomings: The framing of RSBY under the purview of the Ministry of Labour led to its development being largely disconnected from global health issues like UHC and Millennium Development Goals.36 Another shortcoming of the scheme's design was that in several states, RSBY and state-level GFHIS coexisted but worked independently, resulting in fragmented risk pools.44 Although overall enrolment was higher than the neighboring nations, only 57% of eligible families were enrolled under the scheme by the end of 2016.37,45 Inadequate outreach by enrolment agencies, the inability of beneficiaries to obtain BPL cards, and the lack of participation of some districts were responsible for incomplete enrollment.45,46 Enrollment was inequitable with people from remote rural areas, poorer districts, tribal communities, and female-headed households largely contributing to lower enrollment.47 Districts with more households in the third and fourth wealth quintiles were more likely to participate in RSBY.40 The distribution of private empanelled hospitals was skewed towards urban and richer districts.48 Complaints of poor quality or denial to provide care to RSBY beneficiaries were reported.49 Lack of transparency and access to data, information, and grievance redressal mechanisms were also highlighted.50,51
The utilization of RSBY was associated with a 30% increased likelihood of incurring OOPE.45 Reasons for increased OOPE included the low RSBY cap leading to utilization of hospital services exceeding it and deficits in the public health system necessitating seeking care from private providers.45,52,53 Between 2004 and 2014, the hospitalization cost increased by 10.1% in rural areas and 10.7% in urban areas with the average cost of hospitalization in 2014 being Rs. 14,935 and Rs. 24,435 per household, respectively. However, the RSBY cap amount remained static.38 Additionally, the scheme did not pay outpatient costs which constituted 63.5% of all OOPE on health.38 There was no decrease in CHE among the enrolled households.45 In fact, a significant increase in the incidence of health expenditure-induced poverty was observed.52 Thus, there was a need for a new GFHIS that transformed the shortcomings of RSBY by introducing changes including (1) Aligning the financial protection scheme with broader concepts of UHC and Sustainable Development Goal 3 (SDG-3) (2) Investing in awareness and enrollment through local bodies, especially for the most vulnerable population (3) Incentivizing private hospital establishments in poorly served areas and the simultaneous strengthening of the public health system (4) A higher dynamic cap of cost coverage that incorporates the market inflation (5) Inclusion of outpatient services in the coverage (6) Focus on monitoring, data transparency, and sharing.
Thus, the journey of health-related financial risk protection in India started with protecting organized workers through SHIS. The protection expanded to include financially disadvantaged people in the unorganized sector through the advent of GFHIS. The policies have evolved over the decades and the current scheme (PMJAY) insures socially backward classes beyond BPL populations. Across schemes, the service providers have expanded from the public sector to now include non-profit and for-profit private providers. However, all schemes have largely covered secondary and tertiary-level services, neglecting primary care.
Pradhan Mantri Jan Arogya Yojana
We used an equity-based framework for evaluating publicly funded health insurance programmes proposed by Nandi and Schneider for PMJAY's assessment.49
Policy process and political context
The Bharatiya Janata Party (BJP) came to power in the 2014 general election and Shri Narendra Modi was sworn in as the Prime Minister of India. Providing affordable, accessible, and quality healthcare services was a part of BJP's 2014 election manifesto.57 As a step towards satisfying the party's health-related agenda, a new national health policy draft was released in 2017. NHP 2017 provided several recommendations on the structure and implementation of GFHIS. These recommendations and limitations of the existing RSBY created an opportunity for a new GFHIS. In response to this, PMJAY was announced in February 2018 Union Budget and launched in September 2018 by the Ministry of Health and Family Welfare (MoHFW), Government of India.58,59 The launch came just before the 2019 general elections where the ruling party was running for a second term and made healthcare an election agenda item for the first time in Indian politics.60 This was most likely in response to the known insight on healthcare inaccessibility being the second most important concern among Indian voters after better employment opportunities.61 The rise in interest in GFHIS can also be partly attributed to the global movement toward UHC and India's ambition to demonstrate its commitment to protecting the health of its people in the global community.
Goal, design, targets and implementation of PMJAY
The five-year vision of the scheme is achieving SDG 3.8 i.e. ensuring financial protection against CHE and access to affordable and quality healthcare for all.62 The scheme provides a cover of Rs. 500,000 per household for secondary and tertiary-level health services to about 50 crore beneficiaries belonging to the bottom 40% of the population.23 Currently, PMJAY beneficiaries can avail health services included in 920 health packages that consist of 1670 procedures across 24 specialties.63 The beneficiaries can utilize strategically purchased services from both public and empanelled private hospitals. As of July 2021, approximately 23,000 hospitals were empanelled under PMJAY.64 Households eligible under PMJAY are identified by applying specific ‘Deprivation and Occupational criteria’ to the Socio-Economic Caste Census 2011 (SECC 2011).65 Additionally, RSBY beneficiaries are also covered irrespective of their SECC status. SECC deprivation criteria are more inclusive than RSBY's economic criteria as they consider parameters like caste, residence, and occupation in addition to income for beneficiary identification. However, the SECC-based criteria also have drawbacks that are detailed in Supplement Text S1.
PMJAY has a hierarchical implementation model with the National Health Authority (NHA) as the apex body responsible for its execution through State Health Agencies (SHAs).23 Each participating state has one SHA that empanels public and private hospitals under its jurisdiction. SHAs have autonomy to extend PMJAY's coverage to non-SECC beneficiaries, and modify treatment package rates.66 Each SHA can choose between three modes of implementation - a) Insurance model - SHA selects an insurance company to manage PMJAY, b) Trust model - The state government directly pays compensation to the providers without the intermediation of an insurance company, c) Mixed/Hybrid model - Both state and insurance company manage claim settlements.23 Below SHA, a District Implementation Unit (DIU) is established to support the implementation in every district.62 States can decide whether or not to participate in PMJAY. States can also continue with their existing GFHIS with varying degrees of collaboration with PMJAY (e.g. Andhra Pradesh, Karnataka, Kerala, Madhya Pradesh (MP), Meghalaya, Punjab, Rajasthan, Tamil Nadu (TN), and Telangana).67 PMJAY states which previously did not have state-GFHIS are called greenfield states while states which previously had GFHIS scheme are called brownfield states (Supplement Table S1).68 As of April 2022, PMJAY has been implemented in 33 states and union territories (UTs) except in Delhi, West Bengal, and Odisha.67
PMJAY does not have fixed targets for the annual volume or value of hospitalizations to be covered as it operates on beneficiary demand for health services.64 Concerning the impact on CHE reduction, the proportion of SECC-eligible households spending 25% of household consumption on health-related expenditure (or CHE-25) is expected to fall from 16% to 10% if the PMJAY expansion is equivalent to brownfield states’ GFHIS.69 If PMJAY take-up occurs at par with the better-performing states this reduction is expected to be from 16% to 1%.69 The overall progress of the PMJAY from 2018 to 2022 can be seen in Supplement Table S2.
Since the scheme is in its early stage, details of ground-level implementation experiences and challenges are limited. However, a cross-sectional study in Uttar Pradesh (UP) indicated that a majority of hospitals (93.5%) were satisfied with the empanelment process.70 Satisfaction concerning packages was low (35.5%). Overall, PMJAY was perceived to be inferior to private insurance by 77.4% of providers due to poor grievance redressal mechanisms, claim processing delays, and lower health packages rate which has resulted in disinterest in implementing scheme and sometime suspension of implemented scheme.70, 71 Insurance agencies also concurred that premium rates quoted are low (about ten times lower than the market prices).71
Financing PMJAY Scheme
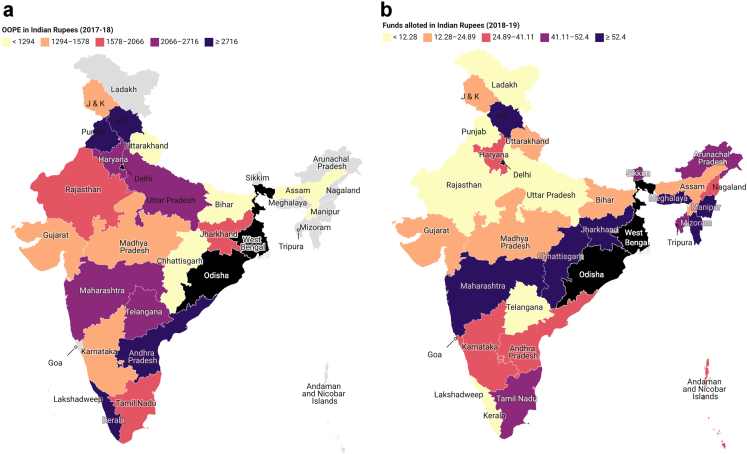
PMJAY is entirely funded by state and central government in a predetermined ratio as specified by the Ministry of Finance.64 The central government allocated 1.8% of GDP to health in the 2022-23 budget. Approximately 7.5% of this fund, amounting to Rs. 6412 crores is dedicated to PMJAY. The 15th Finance Commission estimated that to provide services to the bottom 40% of the population, costs (including Centre and State budgets) of PMJAY for 2019 could range from Rs. 28,000 - Rs. 74,000 crores.72, 73 However, funds allocated to PMJAY in 2019 were substantially less than the estimated costs (88.5%–95.5% lower). The per-capita expenditure on the scheme was much lower than the average national per-capita OOPE incurred (Fig. 1a). Additionally, there are concerns that PMJAY is diverting funds from other health budget sections including non-communicable diseases, communicable diseases, and family welfare.74 This is because the GHE has not increased parallelly to the funds allocated to PMJAY. For example, in 2019–20, while the overall health budget increased by 16.3% compared to the previous budget, the funds allocated to PMJAY increased by 166% (Fig. 1c).74 There is also the issue of inequitable allotment of funds to states as shown in Fig. 3. Thus, PMJAY's budget allotment needs to increase to the estimates provided by the 15th Finance Commission Report. Additionally, the scheme's budgetary requirements should be assessed regularly based on the expenses incurred, existing deficits, and stakeholders' feedback.
Fig. 3.
State-wise per-capita out-of-pocket expenditure on health and funds allocated to PMJAY. PMJAY: Pradhan Mantri Jan Arogya Yojana, HP: Himachal Pradesh, J & K: Jammu and Kashmir. Odisha, West Bengal, and Delhi do not implement the PMJAY scheme. Values for out-of-pocket expenditure (OOPE) are for the years 2017–18 and values for funds allotted are for 2018–19. In figure (a), OOPE values were taken from National Health Accounts 2017–18. Data for the per-capita out-of-pocket expenditure was unavailable for Sikkim, Arunachal Pradesh, Nagaland, Manipur, Mizoram, Tripura, and Meghalaya. In figure (b), funds allocated for PMJAY for 2018–19 were taken from the answer to Lok Sabha 2019 starred question no. 170. States like Uttar Pradesh, Andhra Pradesh, and Kerala with higher per-capita OOPE receive lesser funds for PMJAY implementation than Tamil Nadu with lesser per-capita OOPE.
Beneficiary awareness and enrollment
PMJAY has employed several communications platforms including field drives, letters, information kiosks, print media campaigns, volunteers, websites/apps, etc.96 A 2021 national household survey showed that over 70% of households in states implementing PMJAY were aware of the scheme while only 16% were enrolled. Awareness and enrolment were higher in urban areas than in rural.64 Awareness and enrolment levels were the lowest among households in the first and second economic quintiles and increased progressively in the third, fourth, and fifth quintiles.64 State-level variations in beneficiary awareness and enrollment are detailed in Supplement Text S2.1 and Supplement Table S3. Thus, overall, the scheme is failing to target the most vulnerable population. This mistargeting can risk inequitable demand and utilization of PMJAY.
Monitoring and evaluation
NHA has created an Anti-Fraud and Abuse Control framework that acts as a guideline for fraud detection and prevention.75 The National Anti-Fraud Unit (NAFU) implements this framework with the support of State Anti-Fraud Units (SAFU).76 NAFU and SAFU monitor the utilization of services, conduct medical audits, issue anti-fraud advisory notes, and take action against fraudulent empanelled hospitals which can cause de-empanelment.75 NAFU also uses data analytic tools to detect suspicious transactions, e-cards, and entities.75 In 2020–21, 207 hospitals were de-empanelled and about 4.5 lakh fraudulent e-cards were disabled.62 NHA along with the Quality Council of India provides quality certification to the empanelled hospitals if they fulfill pre-decided standards. There are three levels of certifications - Bronze, Silver, and Gold and hospitals achieving these certifications are provided 15%, 10%, and 5% higher package rates, respectively.64
Insurer/Implementation Support Agency Monitoring & Performance Analysis Core Team (IMPACT) monitors the performance of Insurers, Implementation Support Agencies, and Third Party Administrators by measuring claim turnaround time, workforce productivity, claim rejections validity, etc.75 Central Grievance Redressal Management System (CRGMS), dedicated call centres, and grievance redressal guidelines have been established to redress grievances of beneficiaries, healthcare providers, insurers, etc.77 88% of total registered grievances had been resolved using the CRGMS.62 NHA has created a Management Information System (MIS) which includes information about state's and district's empanelment, hospital procedures, beneficiaries, etc. in the form of dashboards.75 Data from MIS has been used to remove or add new packages under the scheme by measuring utilization.78 NHA disseminates knowledge and experience regarding scheme progress through Policy Briefs and Working Papers.23 However, raw data of any monitoring methods are not available publicly. Creating channels for data sharing is crucial to ensure data transparency for all stakeholders.
Equity of supply and utilization of PMJAY
Inequities in healthcare access and population level outcomes are present across multiple intersecting dimensions including geography, sex, age, caste, religion, etc.49 These inequities are also reflected in the supply and utilization of services under PMJAY. To assess equity in PMJAY's supply side components, we measured the number and distribution of empanelled hospitals. Information about supply-side components like medical equipment, drugs, and health workforce was unavailable. To assess utilization-side components of PMJAY, we measured claim volumes, claim values, and enrollment rates.
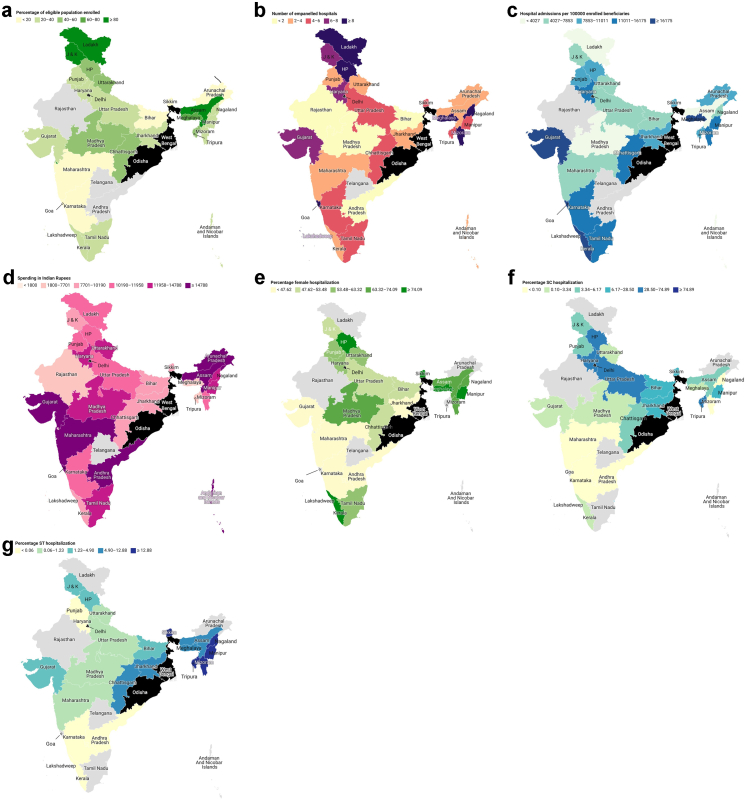
Geography
States with higher poverty headcounts and disease burdens are considered to have a higher need for PMJAY and vice versa.79 However, the utilization in terms of claim volume and value is higher in states with lesser needs e.g. Kerala and Himachal Pradesh, and lesser in states with higher needs e.g. Bihar, MP, UP, and Assam.79 This discrepancy in need vs. utilization is due to poor supply-side factors including a low number of empanelled hospitals, an inefficient beneficiary identification system, and weak health governance in states with greater poverty and disease burdens.79 A similar pattern is seen at the district level, where socio-economically backward districts (also known as aspirational districts) have lower beneficiary identification rates, total number of claims, and total claim amounts than non-aspirational districts.80 The majority of aspirational districts are located in Jharkhand, Orissa, and Chhattisgarh. The state-level variations in utilization and supply are further detailed in Fig. 4a–g and Fig. 5a and b. Additionally, specialty-wise geographical utilization and supply patterns that need attention are mentioned in Supplement Tables S4 and S5.
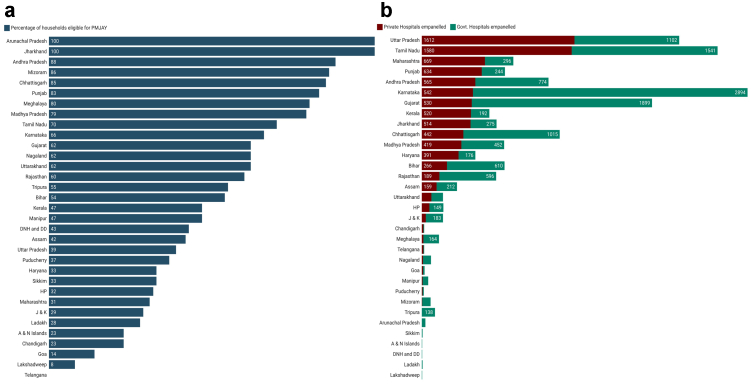
Fig. 4.
State-wise geographic variation in supply and utilization of health services under PMJAY (a) Percentage of eligible beneficiaries enrolled, (b) Empanelled hospitals per 100,000 eligible beneficiaries, (c) Hospital admission rate per 100,000 enrolled beneficiaries, (d) Per-capita expenditure on hospital admission (in Indian Rupees), (e) Percentage of female admissions in private hospitals, (f) Percentage of SC admissions in private hospitals, (g) Percentage of ST admissions in private hospitals. PMJAY: Pradhan Mantri Jan Arogya Yojana, HP: Himachal Pradesh, J & K: Jammu and Kashmir. Odisha, West Bengal, and Delhi do not implement the PMJAY scheme. In figures (a)–(d), the values of enrolled beneficiaries, empanelled hospitals, value, and volume of hospital admissions are from September 2018 to July 2021. Values of eligible beneficiaries are for the most recent year i.e. 2021. The values of enrolled beneficiaries, empanelled hospitals, value, and volume of hospital admissions were taken from the answer to Lok Sabha 2021 unstarred question no. 917. The number of eligible beneficiaries for the year 2021 was taken from the ‘state at a glance’ sheet given at www.pmjay.gov.in. Data for the number of beneficiaries enrolled was unavailable for Rajasthan and Andhra Pradesh. Data for the number of hospital admissions was unavailable for Rajasthan, Andhra Pradesh, and Telangana. Data on the value of hospital admissions was unavailable for Telangana. In figures (e)–(g), the number of private hospitalizations for females, SCs, and STs was taken from the answer to Lok Sabha 2021 unstarred question no. 3014. Total hospitalizations (public and private) were taken from the answer to Rajya Sabha session 250 question no. 2522 and Lok Sabha 2021 unstarred question no. 3014. The total number of private hospitalizations was calculated by multiplying total hospitalization with the percentage of private hospitalizations obtained from the policy brief on ‘PM-JAY: Role of Private hospitals’. Data on the percentage of Scheduled caste (SC), and Schedules tribe (ST) patient hospitalizations in private hospitals were unavailable for Ladakh, Rajasthan, Telangana, Goa, Arunachal Pradesh, and Tamil Nadu. Data on the percentage of female patient hospitalization in private hospitals was unavailable for Ladakh, Rajasthan, Telangana, Goa, Arunachal Pradesh, and Tripura.
Fig. 5.
State-wise percentage of eligible households (families) and number of private and public hospitals empanelled under PMJAY. PMJAY: Pradhan Mantri Jan Arogya Yojana, HP: Himachal Pradesh, J & K: Jammu and Kashmir, A & N Islands: Andaman and Nicobar Islands. Odisha, West Bengal, and Delhi do not implement the PMJAY scheme. Data source: In figure (a) state-wise eligible and total households for the year 2021 were taken from the ‘state at a glance’ sheet given at www.pmjay.gov.in. In figure (b) data for the number of public and private hospitals taken from the answer to Lok Sabha 2021 unstarred question no. 917.
The portability feature under PMJAY allows eligible beneficiaries to access the scheme's services in any empanelled hospital across the country irrespective of their state of residence.81 States from where beneficiaries travel to avail services are called outgoing states while states where beneficiaries avail services are called incoming states. Overall 1.4% PMJAY beneficiaries use portability.81 However, the portability rate for high-value claims (number of high-value portable claims/total high-value claims) is 2.4%, and for very-high-value claims is 5.3%.82 Beneficiaries use portability for availing tertiary health services including cardiology, cardiovascular surgery, and orthopaedics.81 Beneficiaries from MP, UP, Bihar, Jharkhand, and Haryana states account for more than 70% of outgoing portability volume and value.81 Gujarat, UP, and Maharashtra provide care to 75% of incoming portability volume and value.81 Beneficiaries in aspirational districts utilize portability benefits less often than non-aspirational district beneficiaries.80 The portability rates and major outgoing and incoming states for different specialties are detailed in Supplement Table S6.
Sex and gender
At the national level, males form the majority in most of the deprivation and occupational SECC criteria.83 Thus, overall there is a male predominance in the eligible beneficiaries implying a predictable inequality in sex-wise scheme utilization.83 Enrollment under the scheme is almost equal for males (50.8%) and females (49.2%), nationally.83 The total number (volume) and value of claims are higher for males as compared to females (51.5% and 56.4% vs 48.5% and 43.6%, respectively).83 The average per-capita claim value for males is Rs. 16,715 and for females is Rs. 13,730.83 68% of overall high-value claims (claim value > Rs. 30,000) are attributed to males.82 Of the total portability cases, 61% are male and 39% are female.81 The readmission and mortality rates are also found to be higher in male beneficiaries.84 However, sex-based utilization varies from state-to-state therefore studying local-level patterns is crucial (Supplement Text S2.2.). More male claims are seen at private hospitals and for tertiary conditions, while more female claims are seen at public hospitals and for secondary conditions.83 State-wise variations in female hospitalizations at private hospitals can be seen in Fig. 4e.
Of the top ten specialties (in terms of volume), general medicine, general surgery, oral surgery, orthopaedics, urology, cardiology, and pediatric medicine show higher utilization by males, and OBGYN, ophthalmology, and medical oncology show higher utilization by females.83,85 Out of the top 50 procedures in PMJAY, 60% of procedures are utilized more by males and 30% are utilized more by females.83 Hemodialysis, percutaneous coronary transluminal angioplasty (PTCA), myocardial infarction management, open reduction internal fixation, and inguinal hernioplasty show a utilization gap of >70% slanting towards males.83 (Note: Here, we have presented beneficiaries finding in terms of male and female. However, in PMJAY's policy briefs and working papers, sex and gender of beneficiaries have not been clearly defined.)
Age
Over half of all claims (51%) come from the 19–50 years age group.82 This could be explained by the country's demographics where this age group constitutes 47% of the total population.86 The average age of patients using PMJAY insurance is 42.2 years which is higher than the median age of the Indian population (28.7 years) but this could be due to the age-related rise in hospitalization episodes.84 High-value claims are more prevalent among under-five children and those above 50 years. This is expected as children and the elderly suffer from conditions such as congenital heart diseases, coronary artery diseases, cancers, etc. that require high-value treatment.82 Portability is high for the 24–55 years age group and low among those above 65 years indicating that older patients might avoid displacement for seeking healthcare.81 Readmissions are highest in children and lowest in the 20–25 years age group. The average age of mortality among scheme beneficiaries is 52.2 years which is much lower than the average life expectancy of 69.66 years.84 Specific age-wise utilization patterns are also seen in medical specialties within PMJAY (Supplement Table S7). Tracking these utilization patterns is important in the context of the country's evolving demographics. In the next two-three decades, India will have a greater proportion of the aging population.87 Advances in the management of communicable diseases along with an aging population will skew healthcare patient burden towards non-communicable diseases, and age-related conditions. Hence, adapting PMJAY's health package composition in a timely manner would be necessary to match the population's needs.
Caste and religion
Scheduled Caste (SC) and Scheduled Tribe (ST) groups are considered the two most vulnerable in India and are therefore eligible for PMJAY. Overall, these groups comprise approximately 28% of India's population. However, there is little information to understand the utilization. At the national level, SC and ST populations contribute to only 5% and 2% of private hospital admissions respectively, since the scheme's inception. State-level variation can be seen in Fig. 4f and g. There is no publicly available information regarding the utilization of PMJAY for other castes and religious groups. Caste and religion are important dimensions for equity in India and evaluation of utilization for these dimensions is crucial.
Public/private Sector
Beneficiaries should be able to easily access care for a range of health conditions at the cost and quality they desire. There is difference in type, quality, and cost of care in private and public hospitals making their equitable distribution and utilization necessary (see Supplement Text S3, Supplement Tables S8 and S9). However, the utilization and distribution of private and public hospitals are far from equitable (Fig. 5b). Males are more likely to use private hospitals than females. SC and ST populations are more likely to use public hospitals. At the national level, from September 2018 to February 2019, private hospitals contributed to 56% of total empanelled hospitals, 63% of total claim volume, and 75% of total claim value under PMJAY.88 However, for some states utilization of services was higher in public hospital (Supplement Table S10). More than 65% of total hospitals empanelled in Maharashtra, Haryana, Rajasthan, and Punjab are private while in North-Eastern states, Jammu and Kashmir, and Ladakh <25% are private.88 19 of the top 20 private hospitals by claim value are empanelled in just two states, Gujarat and TN.88 State-level differenced in supply and utilization of public and private hospitals are further detailed in Supplement Text S2.3. About 44% of empanelled hospitals in aspirational districts are private, compared with 49% in non-aspirational districts.80
Conclusions
India has a long history of attempting to provide UHC to its citizens using different models including free healthcare for all, subsidized healthcare, SHIS, and GFHIS. Selective protection of vulnerable populations against health shocks through GFHIS has existed in India since 2003. To date, RSBY has been the longest-running national-level GFHIS. Despite its drawbacks, RSBY was a good experiment that should have translated into a better scheme. PMJAY, a successor of RSBY, has been updated in several aspects including a larger population, services and cost coverages, awareness creation, and monitoring and evaluation. However, it still lags in some crucial domains like equity in supply and utilization, targeting vulnerable populations, including outpatient coverage, and dynamic cost coverage. The inequitable supply and utilization affect the most vulnerable groups. It risks creating a spiral where the most deprived classes can fall into further deprivation. PMJAY should work on the above-discussed shortfalls which will need an increase in supply-response in terms of healthcare infrastructure and services and an overall increment in GHE. With its population of 138 crores (approximately 18% of the global population), achieving UHC in India is crucial for achieving the global UHC targets (Panel 3).
Search strategy and selection criteria.
PMJAY's official policy documents including policy briefs, working papers, annual reports, state-at-a-glance reports, and state profile reports were retrieved from www.pmjay.gov.in. Additionally, we searched PubMed with the search terms “Pradhan Mantri Jan Arogya Yojana” and “Rashtriya Swasthya Bima Yojana” until April 2021 to fetch relevant research articles. Further relevant literature was obtained by snowballing the references of included materials. While we relied on database searches, it is important to note that this was not a systematic or scoping review. Rather, our goal was to retrieve literature relevant to the study themes and aims listed.
Panel 3. The case for expanding PMJAY to universal population coverage.
GFHIS can be implemented in one of two ways: a) universal population coverage for priority health services and b) selective ‘vulnerable’ population coverage for comprehensive services. WHO and the United Nations have recommended a universal population coverage model for priority services.89,90 Countries like Chile, Brazil, Mexico, Turkey, Thailand, and China have improved health outcomes and bettered financial protection for their population by implementing the recommended model.54 Indonesia, Vietnam, Philippines, Ghana, Zambia, Cambodia, and India provide financial risk protection to a selective population with a target of progressive population coverage expansion.54 The majority of these countries suffer from stagnant population coverage and scheme outputs and poor quality care to the insured population.54 For example, the average annual decline of OOPE at the end of a decade after the implementation of health insurance schemes in India (selective vulnerable population coverage) and Thailand (universal population coverage) was 2% and 6.1%, respectively (Supplement Fig. S1). However, it is noteworthy that Thailand used 70% of its GHE towards its GFHIS known as Universal Coverage Scheme while this proportion for India is only 1%.91,92
India's PMJAY is based on selective coverage of deprived people for comprehensive health conditions. One of the drawbacks of such a model is that a part of the population, also known as the “missing middle”, is not protected from health-related financial shocks.93 The organized and affluent class of India is covered by SHIS (e.g. ESIS or CGHS) or private health insurance. The vulnerable section is covered by PMJAY and state schemes. As per the National Sample Survey 75th round, around 50% of the population positioned between the deprived and affluent sections are devoid of any financial health protection.54,93 These missing middles largely consist of the self-employed class in rural areas, and several organized and unorganized occupations in urban areas.93 Previous evidence shows that this class does not voluntarily buy insurance unless heavily subsidized.94 Incremental inclusion of this class into GFHIS is also difficult due to minimal political incentives. In fact, in a recent Lok Sabha discussion, the MoHFW clarified that there is no plan as of now to expand PMJAY to other economic classes.95 The second drawback is that the selective scheme implementation for the bottom 40% is unfounded and unjustifiable for India because a much larger section of the Indian population is vulnerable to catastrophic or impoverishing health shocks. The difference in monthly mean per capita household consumption between the 40th and 80th percentiles of the welfare distribution is just Rs. 1000, which is far less than a hospital bill.96 Thus, a far larger share of India's population needs health insurance coverage. This is why the goal needs to be universality. Third, the implementation of such a scheme is often found to be economically inefficient as fragmented systems have higher administration costs.54 Lastly, as noted in the Equity of supply and utilization of PMJAY section such models tend to promote inequity across several dimensions.
Implementing a universal health protection scheme in India needs a thorough look into the economic implications of the scheme which is out of the scope of this discussion. It will require further government investments both at the state and central levels given the current minimal investments. However, it will also offer protection from inefficient administrative spending on fragmented population coverage. Additionally, there is ample evidence of enhanced financial protection and health outcomes in neighbouring countries after implementing universal health protection schemes.
Contributors
SD: Sweta Dubey, SwD: Swasti Deshpande, LK: Lokesh Krishna, SZ: Siddhesh Zadey
Study concept and design: SZ, SD
Acquisition, analysis, or interpretation of data: SD, SZ
Drafting of the manuscript: SD, SZ, SwD, LK
Literature review: SD, SwD, LK
Critical revision of the manuscript for important intellectual content: SD, SZ, SwD, LK
Statistical analysis: SZ, SD
Obtained study funding: Not applicable
Administrative, technical, or material support: SZ
Study supervision: SZ
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
All authors declare no competing interests.
Acknowledgments
The authors acknowledge Dr. Jeel Vasa and Dr. Rachit Sekhrajka for their constructive feedback and assistance.
Funding: None
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2023.100180.
Appendix A. Supplementary data
References
- 1.United Nations, Political declaration of the high-level meeting on universal health coverage: “universal health coverage: moving together to build a healthier world”. published online September 2019. https://www.un.org/pga/73/wp-content/uploads/sites/53/2019/07/FINAL-draft-UHC-Political-Declaration.pdf. Accessed April 27, 2022.
- 2.Universal health coverage overview. 2021. https://www.worldbank.org/en/topic/universalhealthcoverage#1 published online May 19.
- 3.Mahapatro S.R., James K.S., Mishra U.S. Intersection of class, caste, gender and unmet healthcare needs in India: implications for health policy. Health Policy OPEN. 2021;2 doi: 10.1016/j.hpopen.2021.100040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Bank Out-of-pocket expenditure (% of current health expenditure) - India | Data. 2022. https://data.worldbank.org/indicator/SH.XPD.OOPC.CH.ZS?locations=IN&name_desc=true published online Jan 30.
- 5.Sangar S., Dutt V., Thakur R. Burden of out-of-pocket health expenditure and its impoverishment impact in India: evidence from National Sample Survey. Asian Public Policy. 2019;1–18 [Google Scholar]
- 6.Baji P., Pavlova M., Gulácsi L., Groot W. Changes in equity in out-of-pocket payments during the period of health care reforms: evidence from Hungary. Int J Equity Health. 2012;11:36. doi: 10.1186/1475-9276-11-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sriram S., Albadrani M. A study of catastrophic health expenditures in India - evidence from nationally representative survey data: 2014-2018. F1000Res. 2022;11:141. doi: 10.12688/f1000research.75808.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohanty S.K., Dwivedi L.K. Addressing data and methodological limitations in estimating catastrophic health spending and impoverishment in India, 2004-18. Int J Equity Health. 2021;20:85. doi: 10.1186/s12939-021-01421-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Healthcare System in India. Healthcare India - IBEF. 2022. https://www.ibef.org/industry/healthcare-india [Google Scholar]
- 10.World Bank . Poverty & equity data portal. 2023. https://povertydata.worldbank.org/poverty/country/IND [Google Scholar]
- 11.Khandelwal V. Picture this: if Indian states were countries – life expectancy - CEDA. 2021. https://ceda.ashoka.edu.in/picture-this-if-indian-states-were-countries-life-expectancy/ published online Oct 1.
- 12.GDP per capita (current US$) - India | Data. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=IN. Accessed October 9, 2022.
- 13.JC A . The Economic Times; 2021. World Inequality Report 2022: India amongst the most unequal countries in the world, says report - the Economic Times. published online Dec 9. [Google Scholar]
- 14.ORGI . Office of the Registrar General & Census Commissioner; India: 2020. India - sample registration system (SRS)-STATISTICAL report; p. 2022. (ORGI) [Google Scholar]
- 15.Median age - The World Factbook. https://www.cia.gov/the-world-factbook/field/median-age/country-comparison. Accessed October 10, 2022.
- 16.Life expectancy at birth, total (years) - India | Data. 2022. https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=IN [Google Scholar]
- 17.Chandra T. 2019. Literacy in India: the gender and age dimension. ORF Issue Brief No 322. published online Oct 31. [Google Scholar]
- 18.Periodic Labour Force Survey (PLFS) – Quarterly Bulletin [April – June 2022]. 2022; published online Aug. https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1855783. Accessed October 9, 2022.
- 19.Census of India . 2011. Religion data - population of Hindu/Muslim/Sikh/christian - census 2011 India.https://www.census2011.co.in/religion.php [Google Scholar]
- 20.SECC Socio Economic and Caste Census (SECC) 2011. https://secc.gov.in/
- 21.Kumari M., Mohanty S.K. Caste, religion and regional differentials in life expectancy at birth in India: cross-sectional estimates from recent National Family Health Survey. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2019-035392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Health Authority, India Ayushman Bharat pradhan Mantri jan Arogya yojana homepage. 2021. https://pmjay.gov.in/ Ayushman Bharat Website Homepage. published online Feb 8.
- 23.National Health Authority, India About pradhan Mantri jan Arogya yojana (PM-JAY) 2021. https://pmjay.gov.in/about/pmjay About Pradhan Mantri Jan Arogya Yojana. published online Feb 8.
- 24.Bhore committee National health portal of India. 1946. https://www.nhp.gov.in/bhore-committee-1946_pg
- 25.Patnaik I., Roy S., Shah A. National Institute of Public Finance and Policy New Delhi; 2018. The rise of government-funded health insurance in India.https://www.nipfp.org.in/media/medialibrary/2018/05/WP_231.pdf [Google Scholar]
- 26.National Health Portal of India National health insurance schemes. 2015. https://www.nhp.gov.inhttps://www.nhp.gov.in/national-health-insurance-schemes_pg#Aam%20Aadmi%20Bima%20Yojana(AABY published online April 4.
- 27.Ministry of Health and Family Welfare . Government of India; 1983. National health policy.https://www.nhp.gov.in/sites/default/files/pdf/nhp_1983.pdf [Google Scholar]
- 28.Wikipedia Mahatma jyotiba phule jan Arogya yojana. 2021. https://en.wikipedia.orghttps://en.wikipedia.org/wiki/Mahatma_Jyotiba_Phule_Jan_Arogya_Yojana published online Sept 11.
- 29.Hooda S.K. Penetration and coverage of government-funded health insurance schemes in India. Clin Epidemiol Glob Health. 2020;8:1017–1033. [Google Scholar]
- 30.Duggal R. CEHAT (Center for Enquiry into Health and Allied Themes); Mumbai, India: 2001. Evolution of health policy in India.https://www.cehat.org/uploads/files/a147.pdf [Google Scholar]
- 31.Health and Family Welfare M . Government of India; 2002. National health policy. [Google Scholar]
- 32.National Health Profile (NHP) of India- 2017. 2022. https://www.cbhidghs.nic.in/index1.php?lang=1&level=2&sublinkid=87&lid=1137 [Google Scholar]
- 33.National Portal of India Rashtriya swasthya bima yojana. 2016. https://www.india.gov.in/spotlight/rashtriya-swasthya-bima-yojana published online June 4.
- 34.Prasad S., Ghosh I. Dvara Research; 2022. Employee state insurance scheme - performance and potential pathways for reform. [Google Scholar]
- 35.van Langenhove T., De L. International Labour Office; 2015. RSBY: extending social health protection to vulnerable population by using new technologies. [Google Scholar]
- 36.Shroff Z.C., Roberts M.J., Reich M.R. Agenda setting and policy adoption of India's national health insurance scheme:rashtriya swasthya bima yojana. Health Systems Reform. 2015;1:107–118. doi: 10.1080/23288604.2015.1034310. [DOI] [PubMed] [Google Scholar]
- 37.Malhi R., Goel D., Gambhir R.S., Brar P., Behal D., Bhardwaj A. Rashtriya swasthya bima yojana (RSBY) and outpatient coverage. J Family Med Prim Care. 2020;9:459–464. doi: 10.4103/jfmpc.jfmpc_959_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salve P., Yadavar S. Why rashtriya swasthya bima yojana has failed India’s poor; 2017. Business Standard News. https://www.business-standard.com/article/economy-policy/why-rashtriya-swasthya-bima-yojana-has-failed-india-s-poor-117101700115_1.html published online October 19.
- 39.Dutta S., Sarkar S. Ideas for India; 2022. How RSBY impacted healthcare utilisation and spending.https://www.ideasforindia.in/topics/human-development/how-rsby-impacted-healthcare-utilisation-and-spending.html published online March 31. [Google Scholar]
- 40.Nandi A., Ashok A., Laxminarayan R. The socioeconomic and institutional determinants of participation in India's health insurance scheme for the poor. PLoS One. 2013;8 doi: 10.1371/journal.pone.0066296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morton M., Nagpal S., Sadanandan R., Bauhoff S. India's largest hospital insurance program faces challenges in using claims data to measure quality. Health Aff. 2016;35:1792–1799. doi: 10.1377/hlthaff.2016.0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Krishnaswamy K. World Bank Group; 2012. The impact of RSBY on hospital utilization and out-of-pocket health expenditure.https://www.researchgate.net/publication/280484982_The_impact_of_RSBY_on_Hospital_Utilization_and_Out-of-pocket_Health_Expenditure [Google Scholar]
- 43.Azam M. Does social health insurance reduce financial burden? Panel data evidence from India. World Dev. 2018;102:1–17. [Google Scholar]
- 44.Giedion U., Alfonso E.A., Díaz Y. World Bank; 2013. The impact of universal coverage schemes in the developing world: a review of the existing evidence. [Google Scholar]
- 45.Karan A., Yip W., Mahal A. Extending health insurance to the poor in India: an impact evaluation of Rashtriya Swasthya Bima Yojana on out of pocket spending for healthcare. Soc Sci Med. 2017;181:83–92. doi: 10.1016/j.socscimed.2017.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Prinja S., Chauhan A.S., Karan A., Kaur G., Kumar R. Impact of publicly financed health insurance schemes on healthcare utilization and financial risk protection in India: a systematic review. PLoS One. 2017;12 doi: 10.1371/journal.pone.0170996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Devadasan N., Seshadri T., Trivedi M., Criel B. Promoting universal financial protection: evidence from the rashtriya swasthya bima yojana (RSBY) in Gujarat, India. Health Res Policy Syst. 2013;11:29. doi: 10.1186/1478-4505-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nandi S., Schneider H., Garg S. Assessing geographical inequity in availability of hospital services under the state-funded universal health insurance scheme in Chhattisgarh state, India, using a composite vulnerability index. Glob Health Action. 2018;11 doi: 10.1080/16549716.2018.1541220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nandi S., Schneider H. Using an equity-based framework for evaluating publicly funded health insurance programmes as an instrument of UHC in Chhattisgarh State, India. Health Res Policy Syst. 2020;18:50. doi: 10.1186/s12961-020-00555-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thakur H. Study of awareness, enrollment, and utilization of rashtriya swasthya bima yojana (national health insurance scheme) in Maharashtra, India. Front Public Health. 2015;3:282. doi: 10.3389/fpubh.2015.00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Narayana D. Review of the rashtriya swasthya bima yojana. Econ Polit Wkly. 2017;45 https://www.epw.in/journal/2010/29/commentary/review-rashtriya-swasthya-bima-yojana.html [Google Scholar]
- 52.Sinha R.K. Impact of publicly financed health insurance scheme (rashtriya swasthya bima yojana) from equity and efficiency perspectives. Vikalpa. 2018;43:191–206. [Google Scholar]
- 53.Maurya D., Ramesh M. Program design, implementation and performance: the case of social health insurance in India. Health Econ Policy Law. 2018:1–22. doi: 10.1017/S1744133118000257. [DOI] [PubMed] [Google Scholar]
- 54.Reddy K.S., Sethi N.K., Chatterjee M., et al. Planning Commission of India; New Delhi: 2011. High level Expert group report on universal health coverage for India.https://nhm.gov.in/images/pdf/publication/Planning_Commission/rep_uhc0812.pdf [Google Scholar]
- 55.Nicholson D., Yates R., Warburton W., Fontana G. World Innovation Summit for Health; 2015. Delivering universal health coverage: a guide for policymakers.https://www.imperial.ac.uk/media/imperial-college/institute-of-global-health-innovation/public/Universal-health-coverage.pdf [Google Scholar]
- 56.Ministry of Health and Family Welfare . Government of India; 2017. National health policy.https://www.nhp.gov.in/nhpfiles/national_health_policy_2017.pdf [Google Scholar]
- 57.Bhartiya Janta Party . 2014. Bharatiya janata party: ek Bharat - shreshtha Bharat - 2014 election manifesto. [Google Scholar]
- 58.Ayushman Bharat Yojana - Wikipedia. published online March 23. https://en.wikipedia.org/wiki/Ayushman_Bharat_Yojana. Accessed October 7, 2022.
- 59.Pawar DrBP. Lok Sabha India; 2022. Ayushman bharat–pradhan Mantri jan Aarogya Yojana- loksabha question. [Google Scholar]
- 60.Chalkidou K., Jain N., Cluzeau F., Glassman A. Modicare post-election: recommendations to enhance the impact of public health insurance on UHC goals in India | center for global development | ideas to action. 2019. https://www.cgdev.org/publication/modicare-post-election-recommendations-enhance-impact-public-health-insurance-uhc-goals published online May 11.
- 61.Association for Democratic Reforms . 2018. ADR's mid-term survey report - all India (Jan ’17 – Apr ’17) [Google Scholar]
- 62.National Health Authority . National Health Authority; 2022. Ayushman bharat pradhan mantri jan arogya yojana - annual report 2020-21. [Google Scholar]
- 63.National Health Authority . Ministry of Health and Family Welfare; 2021. National health benefit package 2.2: user guidelines.https://nha.gov.in/img/resources/HBP-2.2-manual.pdf [Google Scholar]
- 64.Press Information Bureau India Ayushman Bharat pradhan Mantri jan Arogya yojana (AB-PMJAY) 2021. https://www.pib.gov.in/PressReleasePage.aspx?PRID=1738169 published online July 23.
- 65.National Health Authority . National Health Authority; 2018. Beneficiary identification guidelines ayushman Bharat – pradhan Mantri jan Arogya Yojana (AB PM-JAY) [Google Scholar]
- 66.Press Information Bureau Implementation of PMJAY. 2019. https://pib.gov.in/Pressreleaseshare.aspx?PRID=1562704 published online Feb 5.
- 67.National Health Authority. PMJAY- implementing states. https://pmjay.gov.in/states/states-glance. Accessed June 23, 2022.
- 68.Sharma S., Singh A., Gupta DrA., Pandey A., Kamat S., Kumar A. KPGM and ASSOCHAM; 2019. Ayushman Bharat— a big leap towards universal health coverage in India. [Google Scholar]
- 69.Gruber DrJ., Sachdeva S., Aggarwal DrV., Agrawal DrR., Patil P., Jay P.M.- National Health Authority; 2022. Impact on in-patient out-of-pocket expenditures. [Google Scholar]
- 70.Verma N., Bano T., Chopra H., Singh G., Mittal C. Implementation challenges of pradhan Mantri jan Arogya yojana: a cross- sectional study in Meerut, Uttar Pradesh. Indian J Community Health. 2022;34:330–333. [Google Scholar]
- 71.Bhasin S. The Tribune; 2021. Non-payment of claims: private hospitals in Punjab suspend ayushman Bharat scheme : the tribune India. published online Oct 24. [Google Scholar]
- 72.Gupta I., Chowdhury S., Ramandeep, Roy A. Institute of Economic Growth (IEG); Delhi: 2019. Ayushman Bharat costs and finances of PMJAY. [Google Scholar]
- 73.Kumar A. PRS Legislative Research; 2021. Demand for grants 2021-22 analysis: health and family welfare. [Google Scholar]
- 74.Sharma N.C. Health budget focuses only on Ayushman Bharat, other schemes ignored. Mint. 2019 published online Feb. [Google Scholar]
- 75.National Health Authority . National Health Authority; 2019. Ayushman Bharat pradhan mantri jan arogya yojana - annual report 2018-19. [Google Scholar]
- 76.National Health Authority, India. About National health authority. https://pmjay.gov.in/about/nha. Accessed June 23, 2022.
- 77.Gautam P. National Health Authority; India: 2021. PMJAY grievance redressal guidelines. [Google Scholar]
- 78.NHA NHA insights training module. 2020. https://insights.pmjay.gov.in/Insights%20Dashboard%20Training%20Module.pdf published online Sept.
- 79.Smith O., Dong D., Chhabra S. National Health Authority; 2019. PM-JAY across India's states: need and Utilization. [Google Scholar]
- 80.Smith O., Dong D., Chhabra S. National Health Authority; 2019. PM-JAY and India's aspirational districts. [Google Scholar]
- 81.Arora A., Bhutani P., Chhabra S., Smith O. National Health Authority; 2020. PM-JAY without borders: analysis of portability services.https://pmjay.gov.in/sites/default/files/2020-02/Policy%20Brief%205_Analysis%20of%20Portability%20Services.pdf [Google Scholar]
- 82.Dong D., Naib P., Smith O., Chhabra S. National Health Authority; 2019. Raising the bar: analysis of PM-JAY high-value claims.https://www.pmjay.gov.in/sites/default/files/2019-10/Policy%20Brief_Raising%20the%20Bar_High%20Value%20Claims_10-10-19_WB.pdf [Google Scholar]
- 83.Kaur S., Jain N., Kumar S. National Health Authority; 2021. Addressing gender issues under ayushman Bharat pradhan Mantri jan ArogyaYojana (AB PM-JAY) in India- implications for equity.https://pmjay.gov.in/sites/default/files/2020-03/Working%20paper.pdf [Google Scholar]
- 84.Mohpal A., Smith O., Chhabra S. National Health Authority; 2020. Quality of care in PM-JAY: a first look at unplanned readmissions and mortality.https://pmjay.gov.in/sites/default/files/2020-06/Policy-Brief-7_PMJAY-Readmissions_30-05-20_NHA.pdf [Google Scholar]
- 85.Sehgal P.K., Chandrashekhar S., Naib P. National Health Authority; 2021. Trends in cardiac care utilisation under ayushman Bharat pradhan Mantri jan Arogya yojana (PM-JAY)https://pmjay.gov.in/sites/default/files/2021-06/Analysis-of-Cardiac-Packages-Utilization-Under-PMJAY_Final.pdf [Google Scholar]
- 86.Institute for Health Metrics and Evaluation Population forecasting. 2017. https://vizhub.healthdata.org/population-forecast/
- 87.Statista India - median age of the population 1950-2050. 2022. https://www.statista.com/statistics/254469/median-age-of-the-population-in-india/
- 88.Dong D., Sehgal P., Chhabra S., Naib P., Smith O., Jay P.M.- National Health Authority; 2020. The Role of private hospitals.https://pmjay.gov.in/sites/default/files/2020-11/Policy_Brief_9_Private_PM-JAY_201123_WB_NHA_R.pdf [Google Scholar]
- 89.WHO . World Health Organization; 2014. Making fair choices on the path to universal health coverage: final report of the WHO consultative group on equity and universal health coverage.https://apps.who.int/iris/handle/10665/112671 [Google Scholar]
- 90.Sustainable Development Solutions Network (SDSN) United Nations; 2014. Health in framework of sustainable development. [Google Scholar]
- 91.Tangcharoensathien V., Thammatach-Aree J., Witthayapipopsakul W., Viriyathorn S., Kulthanmanusorn A., Patcharanarumol W. Political economy of Thailand's tax-financed universal coverage scheme. Bull World Health Organ. 2020;98:140–145. doi: 10.2471/BLT.19.239343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jongudomsuk P., Srithamrongsawat S., Patcharanarumol W. World Health Organization; 2015. The kingdom of Thailand health system review. [Google Scholar]
- 93.Sarwal R., Kumar A. 2021. Health insurance for India's missing middle. published online Oct 27. [DOI] [Google Scholar]
- 94.Chuma J., Mulupi S., McIntyre D. RESYST); 2013. Providing financial protection and funding health service benefits for the informal sector: evidence from Sub-Saharan Africa. Resilient and responsive health system. [Google Scholar]
- 95.Choubey A.K. Government of India; Lok Sabha: 2020. Expansion of PMJAY scheme.http://164.100.24.220/loksabhaquestions/annex/174/AU2081.pdf [Google Scholar]
- 96.Bhatnagar A., Chhabra S., Manchanda N., Smith O., Jay Awareness P.M.- National Health Authority; 2022. Enrolment and targeting: evidence from a national household survey. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.