Abstract
Orogastric (OG) and nasogastric (NG) tubes have been reported to delay breastfeeding initiation and affect respiratory function. However, the effects of feeding tubes on sucking pressure have not been well studied. Fourteen preterm infants were enrolled in this study, and their sucking pressures during bottle feeding with an OG tube, NG tube, and without any tube were measured. Sucking pressure significantly increased after changing the OG tube to an NG tube (p = 0.044). However, sucking pressure showed no significant differences after changing the feeding method from an NG tube to oral intake. Thus, NG tubes are superior to OG tubes in terms of sucking pressure.
Keywords: Sucking Pressure, Feeding tube, Preterm infant, Swallowing function
INTRODUCTION
The coordination of sucking, swallowing, and respiration is important for oral feeding, especially in infants (1). However, preterm and low-birthweight infants often have difficulty with oral intake immediately after birth due to immaturity and/or respiratory distress syndromes (2). Although these infants gradually mature through enteral nutrition (3), their sucking ability remains insufficient due to poor neurologic (4) and cardiorespiratory functions (5). At present, these infants receive two types of tube feeding, orogastric (OG) tube feeding and nasogastric (NG) tube feeding (6), in combination until they mature. These infants practice oral feeding while relying on tube feeding until they can obtain adequate nutrition through oral intake.
The use of NG tubes has been reported to cause increased nasal and airway resistance during respiration (7), a reduction in the oxygen saturation (8), and delayed initiation of oral intake (9). On the other hand, OG tubes have been reported to increase the incidence of vagal reflexes and bradycardia (2, 6) and affect palate growth (10). Conversely, several studies have reported no significant differences in weight gain and episodes of apnea and bradycardia between NG and OG tubes (11). As such, evidence for the influence of feeding tubes is insufficient, and the choice of a feeding tube is currently based on the infant’s respiratory status and method of respiratory support (6) and the guidelines of the individual institutions.
Although several studies (3, 12–14) have used sucking pressure to assess infant oral feeding, no study has examined the influence of OG and NG tubes on sucking pressure. Therefore, in this study, we examined the effect of NG and OG tubes on oral feeding by measuring the sucking pressure to provide additional evidence for selecting the appropriate type of feeding tube for immature infants.
MATERIALS AND METHODS
Participants
We recruited infants during insertion of OG or NG tubes in the Neonatal Intensive Care Unit (NICU) or Growing Care Unit (GCU) of the Comprehensive Perinatal Maternal and Child Medical Center at Hyogo Prefectural Kobe Children’s Hospital between April 2019 and November 2020. The infants included in this study were born at 34 weeks of gestation and had no congenital abnormalities in the oral cavity, nasal cavity, larynx, esophagus, stomach, or intestines, heart disease requiring surgery, chromosomal abnormalities, or obvious brain dysfunction. Laryngoscopic examination was performed as needed to examine abnormalities of the nasal cavity and laryngopharynx, such as layngomalacia. Oxygen saturation was monitored if required, but no abnormal changes were observed in any of the participants. Since preterm infants and low-birth-weight infants often require nasal continuous positive airway pressure (NCPAP) or high-flow nasal cannula (HFNC) due to severe respiratory conditions, a feeding tube could not be inserted through the nose in these circumstances. Therefore, the hospital policy was to start tube feeding with an OG tube, which was changed to an NG tube as soon as the infant’s respiratory condition improved. This protocol was approved by the Ethics Committee of Hyogo Prefectural Kobe Children’s Hospital (R2–10), and written informed consent was obtained from the parents of all the participants.
Measurement of Sucking Pressure and Intake Amount During Bottle Feeding
An artificial nipple (SofTouch™ Peristaltic PLUS SSS size; Pigeon Co. Ltd., Tokyo, Japan), which is routinely used in nurseries, was used in this study. A silicone tube with an outer diameter of 2 mm and an inner diameter of 1 mm was attached 1 mm from the nipple hole at the tip of the artificial nipple, and a semiconductor pressure transducer PMS-5M-2™ (JTEKT Co. Ltd., Tokyo, Japan) was connected to the end of the tube (Figure 1). The pressures were amplified with an AA6210 amplifier (JTEKT Co. Ltd., Tokyo, Japan) and recorded using a data logger (GL240; Graphtec Co. Ltd., Yokohama, Japan) (Figure 2). Sucking pressure was measured for 5 min after the start of feeding. Among the waveforms measured for 5 min, continuous waveforms of −10 mmHg or less for 10 s without a pause of >2 s were selected for analysis (Figure 3).
Figure 1.
Structure of the Artificial Nipple
Figure 2.
Measurement of Sucking Pressure in Bottle Feeding.
AN: Artificial nipple (SofTouch™ Peristaltic PLUS SSS size; Pigeon Co. Ltd., Tokyo, Japan)
PT: Semiconductor pressure transducer PMS-5M-2™ (JTEKT Co. Ltd., Tokyo, Japan)
AA: AA6210 amplifier (JTEKT Co. Ltd., Tokyo, Japan)
GL: Data logger GL240 (Graphtec Co. Ltd., Yokohama, Japan)
Blue arrows: Silicone tube placed on the artificial nipple
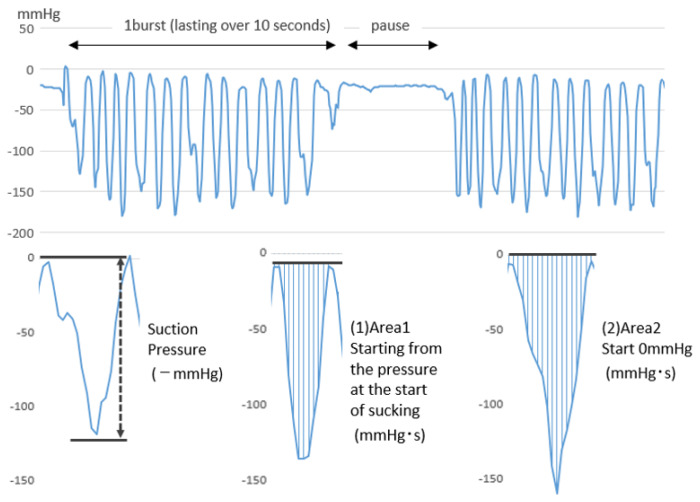
Figure 3.
Pressure waveform for sucking pressure measurements.
Sucking Pressure: From the start of sucking to the bottom of the negative pressure waveform
Area 1: Total negative pressure (time integral of negative pressure) every 0.05 s from the beginning to the end of the sucking waveform, starting from the pressure at the beginning of the sucking waveform and ending at the pressure at the end of the sucking waveform [mmHg × 0.05 s]
Area 2: From the beginning to the end of the sucking sip waveform, the negative pressure (time integration of negative pressure) was added up every 0.05 seconds, starting at 0 mmHg [mmHg × 0.05 s]
The intake amount was measured for 5 min during measurement of the sucking pressure. In our experience, preterm and low-birth-weight infants find it difficult to continuously suck for more than 5 min. Moreover, they occasionally take a break from sucking even within 5 min. Thus, we set the observation period to 5 min and selected continuous waveforms of −10 mmHg or less for 10 s or more without a pause of more than 2 s for the analysis.
The sucking pressure during bottle feeding was measured at the time of changing the feeding method [1] from the OG tube to the NG tube (pre: during insertion of the OG tube, post: during insertion of the NG tube) and [2] from the NG tube to oral feeding (pre: during insertion of the NG tube, post: after tube removal). To eliminate the influence of maturation, the sucking pressure measurements were obtained within 24 h before and after the change in feeding method ([1] from the OG tube to the NG tube and [2] from the NG tube to oral feeding). In addition, to eliminate the influence of changes in the feeding method, the sucking pressure was measured for more than 2 h after the change. Injections and eye examinations were avoided within 30 minutes immediately before measurement, and the infant was allowed to rest.
During bottle feeding, the investigator held the infant in a semi-upright supine position. The infant was allowed to rest when oxygen desaturation or bradycardia occurred during sucking (3). The pre- and post-sucking pressures were measured using the same milk under the same respiratory conditions.
Sucking Pressure, Area, and Intake Ratios
For evaluation of the sucking pressure, the mean sucking pressure (mmHg) was calculated, and the mean sucking pressure after a change in the feeding method was divided by the mean sucking pressure before the change in the feeding method to obtain the sucking pressure ratio (Figure 3). The mean area was calculated under two conditions: Area 1, calculation starting from the pressure at the start of sucking (mmHg · s), and Area 2, calculation starting from 0 mmHg (mmHg · s). The mean area after the change in the feeding method was divided by the mean area before the change in the feeding method to obtain the area ratio. The intake ratio was calculated by dividing the intake (mL) after the change in the feeding method by the intake (mL) before the change in feeding method (Figure 3).
Areas 1 and 2 were determined by integration of the sucking waveform from the start to the end of each sucking. In Area 1, the baseline pressure was determined as the pressure at the beginning of sucking; in Area 2, the baseline pressure was determined to be 0 mmHg (atmospheric pressure). Although the differences between the two methods were considered to be small, we performed evaluations using both methods, since no standard evaluation method has been established to date.
Sub-analysis
The infants were subclassified by birth weight into low birth weight (LBW: less than 2500 g), very low birth weight (VLBW: less than 1500 g), and extremely low birth weight (ELBW: less than 1000 g) groups. To more precisely analyze the influence of the feeding method on immature infants, we sub-analyzed the sucking pressure of ELBW infants, and separately analyzed the mean sucking pressure, Area 1, Area 2, and bottle-feeding intake before and after changing the feeding method for infants weighing less than 1000 g and those weighing 1000 g or more.
Statistical Analyses
A paired t-test was used for statistical analysis of the sucking pressure ratio, area ratio, and intake ratio before and after changing the feeding method. EZR v1.54 (64-bit) was used for the calculations (15). Statistical significance was set at P < 0.05.
Disclosure Statement
The authors have no conflicts of interest to disclose concerning this study. The equipment used for the measurement of sucking pressure in this study (artificial nipple, silicone tubing, pressure transducer, amplifier, and data logger) was provided by Pigeon Co. Ltd. (Tokyo, Japan).
RESULTS
Fourteen preterm infants (7 each in the OG-to-NG and NG-to-oral feeding groups) participated in this study. In the OG-to-NG group, the average gestational age (GA) was 26.5 ± 1.5 weeks, and the average birth weight was 993 ± 252 g. On the day of changing the feeding method from the OG tube to the NG tube, postnatal age (PNA) was 69.2 ± 17.5 days, modified postconceptional age (PCA) was 36.9 ± 1.3 weeks, and weight was 2128 ± 267 g (Table I). In the NG-to-oral feeding group, the average GA was 26.8 ± 3.6 weeks, and the average weight was 938 ± 325 g at birth. On the day of changing the feeding method from the NG tube change to oral feeding, the PNA was 78.1 ± 20.5 days, PCA was 38.7 ± 2.1 weeks, and weight was 2271 ± 275 g (Table I).
Table I.
Characteristics of preterm infants in the two groups at birth and at tube change
| Birth | Tube change | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| GA (wk) | Weight (g) | PNA (day) | PCA (wk) | Weight (g) | Tube size | Milk | Respiration | ||
| OG→NG | 1 | 30 | 1372 | 45 | 37 | 2424 | 5Fr | breast | RA |
| 2 | 27 | 902 | 77 | 38 | 2200 | 5Fr | breast | RA | |
| 3 | 25 | 656 | 100 | 39 | 2245 | 5Fr | breast | HFNC6L | |
| 4 | 26 | 1008 | 73 | 36 | 2150 | 5Fr | breast | RA | |
| 5 | 27 | 1110 | 64 | 36 | 2217 | 5Fr | breast | HFNC6L | |
| 6 | 29 | 1172 | 55 | 37 | 2090 | 5Fr | breast | RA | |
| 7 | 25 | 728 | 71 | 35 | 1570 | 5Fr | breast | RA | |
| NG→OFF | 1 | 31 | 1564 | 48 | 38 | 2420 | 5Fr | breast | RA |
| 2 | 26 | 656 | 101 | 41 | 2790 | 5Fr | breast | RA | |
| 3 | 25 | 746 | 94 | 39 | 2010 | 5Fr | breast | RA | |
| 4 | 26 | 896 | 75 | 37 | 2086 | 5Fr | formula | RA | |
| 5 | 34 | 1074 | 54 | 42 | 2110 | 5Fr | breast | RA | |
| 6 | 24 | 620 | 93 | 37 | 2114 | 5Fr | breast | RA | |
| 7 | 26 | 1008 | 82 | 37 | 2365 | 5Fr | breast | RA | |
GA, gestational age; PNA, postnatal age; PCA, postconceptional age; OG, orogastric tube; NG, nasogastric tube; OFF, oral feeding; RA, room air; HFNC6L, high-flow nasal cannula at 6 L/min.
The mean sucking pressures, Area 1, Area 2, and bottle-feeding intake before and after changing the feeding methods are summarized in Table II. The sucking pressure, Area 1, Area 2, and intake ratios are summarized in Table III. As shown in Table II, the sucking pressure significantly increased after changing the feeding method from the OG tube to the NG tube (p = 0.044). Although the analyses did not show statistical significance, Area 1 (p = 0.066), Area 2 (p = 0.078), and intake (p = 0.091) also tended to increase after changing the feeding method from the OG to the NG. On the other hand, no significant differences were observed in the sucking pressure, Area 1, Area 2, and intake ratios before and after changing the feeding method from the NG tube to oral intake.
Table II.
Bottle-feeding values before (pre) and after (post) changing the feeding methods
| Pre | Post | Ratio (post/pre) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sucking pressure* | Area 1* | Area 2* | Intake | Sucking pressure* | Area 1* | Area 2* | Intake | Sucking pressure | Area 1 | Area 2 | Intake | ||
| OG→NG | 1 | −88.83 | −28.07 | −43.56 | 10.00 | −120.88 | −47.75 | −51.90 | 17.00 | 1.36 | 1.70 | 1.19 | 1.70 |
| 2 | −60.07 | −18.69 | −18.70 | 7.00 | −109.18 | −40.30 | −40.27 | 9.00 | 1.82 | 2.16 | 2.15 | 1.29 | |
| 3 | −105.74 | −23.25 | −22.36 | 14.00 | −122.14 | −49.64 | −52.19 | 19.00 | 1.16 | 2.14 | 2.33 | 1.36 | |
| 4 | −34.21 | −9.36 | −10.02 | 5.00 | −130.64 | −75.68 | −69.66 | 18.00 | 3.82 | 8.09 | 6.95 | 3.60 | |
| 5 | −96.46 | −22.63 | −24.45 | 12.00 | −110.08 | −54.45 | −54.33 | 14.00 | 1.14 | 2.41 | 2.22 | 1.17 | |
| 6 | −77.67 | −31.74 | −33.54 | 12.00 | −162.61 | −73.71 | −71.24 | 19.00 | 2.09 | 2.32 | 2.12 | 1.58 | |
| 7 | −64.50 | −22.42 | −31.48 | 8.00 | −119.12 | −39.81 | −37.01 | 8.00 | 1.85 | 1.78 | 1.18 | 1.00 | |
| NG→OFF | 1 | −142.55 | −52.08 | −59.08 | 21.00 | −159.96 | −53.22 | −58.83 | 27.00 | 1.12 | 1.02 | 1.00 | 1.29 |
| 2 | −106.60 | −42.42 | −37.78 | 20.00 | −106.23 | −40.67 | −38.18 | 17.00 | 1.00 | 0.96 | 1.01 | 0.85 | |
| 3 | −54.54 | −16.40 | −23.38 | 3.00 | −82.43 | −28.66 | −27.56 | 8.00 | 1.51 | 1.75 | 1.18 | 2.67 | |
| 4 | −83.48 | −24.13 | −30.18 | 15.00 | −81.33 | −21.55 | −27.42 | 10.00 | 0.97 | 0.89 | 0.91 | 0.67 | |
| 5 | −123.28 | −42.05 | −41.76 | 12.00 | −112.50 | −38.87 | −39.36 | 9.00 | 0.91 | 0.92 | 0.94 | 0.75 | |
| 6 | −144.59 | −56.60 | −57.87 | 22.00 | −128.65 | −51.16 | −50.81 | 19.00 | 0.89 | 0.90 | 0.88 | 0.86 | |
| 7 | −138.72 | −72.58 | −71.84 | 23.00 | −140.26 | −69.00 | −69.69 | 21.00 | 1.01 | 0.95 | 0.97 | 0.91 | |
OG, orogastric tube; NG, nasogastric tube; OFF, oral feeding.
Sucking pressure values are expressed in mmHg; Area 1, 2 are expressed in mmHg · s; and intake is expressed in mL.
Values are expressed as means.
Table III.
Characteristics of ratio (post/pre)
| OG→NG | Ratio (post/pre) | p value |
|---|---|---|
| Sucking Pressure | 1.89 ± 0.93 | 0.044 |
| Area 1 | 2.94 ± 2.28 | 0.066 |
| Area 2 | 2.59 ± 1.98 | 0.078 |
| Intake | 1.67 ± 0.88 | 0.091 |
|
| ||
| NG→OFF | Ratio (post/pre) | p value |
|
| ||
| Sucking Pressure | 1.06 ± 0.21 | 0.487 |
| Area 1 | 1.06 ± 0.31 | 0.640 |
| Area 2 | 0.98 ± 0.10 | 0.673 |
| Intake | 1.14 ± 0.70 | 0.610 |
OG, orogastric tube; NG, nasogastric tube; OFF, oral feeding.
Values are expressed as mean ± standard error of the mean.
The results of the analysis of the two groups based on body weight are shown in Table IV, which presents the sucking pressure, Area 1, Area 2, and intake ratios for these two groups of infants. Although significant differences were observed only in Area 1 on changing from the OG tube to the NG tube in infants weighing less than 1000 g, sucking pressure, Area 1, Area 2, and intake tended to increase after changing the feeding method from the OG tube to the NG tube in both groups. In contrast, no significant differences were observed in the sucking pressure, Area 1, Area 2, and intake before and after changing the feeding method from the NG tube to oral intake in both groups.
Table IV.
Characteristics of ratio (post/pre)
| Birth weight <1000 g group | ||
|---|---|---|
| OG→NG (n = 3) | Ratio (post/pre) | p value |
| Sucking pressure | 1.61 ± 0.39 | 0.115 |
| Area 1 | 2.02 ± 0.21 | 0.014 |
| Area 2 | 1.89 ± 0.62 | 0.132 |
| Intake | 1.21 ± 0.19 | 0.188 |
|
| ||
| NG→OFF (n = 4) | Ratio (post/pre) | p value |
|
| ||
| Sucking pressure | 1.09 ± 0.28 | 0.558 |
| Area 1 | 1.13 ± 0.42 | 0.587 |
| Area 2 | 0.99 ± 0.14 | 0.935 |
| Intake | 1.26 ± 0.94 | 0.616 |
|
| ||
| Birth weight ≥1000 g group | ||
|
| ||
| OG→NG (n = 4) | Ratio (post/pre) | p value |
|
| ||
| Sucking pressure | 2.10 ± 1.21 | 0.167 |
| Area 1 | 3.63 ± 2.99 | 0.177 |
| Area 2 | 3.12 ± 2.60 | 0.200 |
| Intake | 2.01 ± 1.08 | 0.158 |
|
| ||
| NG→OFF (n = 3) | Ratio (post/pre) | p value |
|
| ||
| Sucking pressure | 1.02 ± 0.10 | 0.823 |
| Area 1 | 0.97 ± 0.05 | 0.361 |
| Area 2 | 0.97 ± 0.03 | 0.186 |
| Intake | 0.98 ± 0.27 | 0.924 |
OG, orogastric tube; NG, nasogastric tube; OFF, oral feeding.
Values are expressed as mean ± standard error of the mean. P < 0.05 was considered to indicate significance.
DISCUSSION
Although the coordination of sucking, swallowing, and respiration is known to be important for safe feeding (1), no previous study has investigated the effects of tube feeding on sucking in preterm infants. In this study, we evaluated the effects of OG and NG tubes on sucking to provide evidence for the choice between these feeding tubes in preterm infants. In the OG-to-NG group, we found a significant difference in sucking pressure between OG (pre) and NG (post). In contrast, in the NG-to-oral feeding group, the sucking pressure showed no significant difference. Similar results were obtained when infants weighing less than 1000 g and those weighing more than 1000 g were analyzed separately. These results suggest that the OG tube may affect sucking function, but the NG tube may not. The most likely reason for the significant difference between OG (pre) and NG (post) is that the OG tube in the mouth created a gap between the lips and the artificial nipple and did not allow sufficient negative pressure. These results suggest that even babies with sufficient sucking ability may not suck enough milk, leading to underestimation of their sucking ability. Therefore, we suggest that the NG tube should be selected for tube feeding because of the possibility that the OG tube may affect the infant’s sucking function. However, since neonates generally breathe through the nasal cavity instead of the oral cavity, OG tubes are often used as the first choice, especially in premature infants, as shown in this study. Even in cases where an OG tube is first selected, we recommend changing it to the NG tube immediately after resolution of the initial indication for selecting the OG tube. Since the NG tube had no effect on sucking, we recommend maintaining the NG tube in place and continuing oral feeding practice until sufficient oral feeding is possible.
Several studies have reported no significant differences between NG and OG tube feeding in terms of weight gain and episodes of apnea and bradycardia. While the present study highlighted the superiority of NG tube feeding from the viewpoint of sucking pressure, various factors should be considered when choosing between NG and OG tubes.
This study had several limitations. The first limitation is that the sucking function includes both suction and compression (14, 16). However, we did not assess compression in the present study. Nevertheless, OG tubes may also inhibit swallowing and tongue movement. Thus, the anatomical differences between placement of OG and NG tubes may negatively influence the sucking ability even in terms of compression. As a second limitation, we used two methods for measurement of the areas, but neither method showed significant differences. As for the intake, one study reported that 80% of infants drink within 10 min of starting bottle feeding (17). Thus, we may need to consider extending the measurement time. A third limitation is the lack of direct comparisons between OG tube feeding and oral feeding. In OG tube feeding, the gap between the lips and restriction of tongue movement affects the sucking pressure. Thus, the effect of the gap between the lips and restriction of tongue movement by OG on sucking should be evaluated by directly comparing OG tube feeding with oral feeding. However, none of the infants transitioned directly from the OG tube to oral feeding in this study, in accordance with the hospital policy. A final limitation is the small number of participants in this study. Initially, we planned to conduct the study with a larger number of participants. However, owing to the spread of coronavirus disease 2019 (COVID-19), we were not allowed to continue this study by the authorities. Thus, we will restart this study to draw a more definitive conclusion after the COVID-19 pandemic.
CONCLUSION
Immature infants practice oral feeding while relying on tube feeding until they can obtain adequate nutrition through oral intake. However, the effects of feeding tubes on sucking pressure have not been well studied. Thus, we examined the effect of NG and OG tubes on oral feeding. This study showed that NG tubes are superior to OG tubes in terms of sucking pressure.
ACKNOWLEDGMENTS
The authors sincerely thank Ms. Takae Nagai and Mr. Satoru Saito of Pigeon Co. Ltd. for the bottle pressure measuring device and their technical support. The authors have no financial information to disclose regarding this study.
REFERENCES
- 1.Martin-Harris B. Clinical implications of respiratory-swallowing interactions. Curr Opin Otolaryngol Head Neck Surg. 2008;16(3):194–9. doi: 10.1097/MOO.0b013e3282febd4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watson J, McGuire W. Nasal versus oral route for placing feeding tubes in preterm or low birth weight infants. Cochrane Database Syst Rev. 2013;(2):CD003952. doi: 10.1002/14651858.CD003952.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mizuno K, Ueda A. The maturation and coordination of sucking, swallowing, and respiration in preterm infants. J Pediatr. 2003;142(1):36–40. doi: 10.1067/mpd.2003.mpd0312. [DOI] [PubMed] [Google Scholar]
- 4.Casaer P, Daniels H, Devlieger H, De Cock P, Eggermont E. Feeding behaviour in preterm neonates. Early Hum Dev. 1982;7(4):331–46. doi: 10.1016/0378-3782(82)90035-4. [DOI] [PubMed] [Google Scholar]
- 5.Daniels H, Devlieger H, Casaer P, Ramaekers V, Van den Broeck J, Eggermont E. Feeding, behavioural state and cardiorespiratory control. Acta Paediatr Scand. 1988;77(3):369–73. doi: 10.1111/j.1651-2227.1988.tb10662.x. [DOI] [PubMed] [Google Scholar]
- 6.Wallace T, Steward D. Gastric tube use and care in the NICU. Newborn Infant Nurs Rev. 2014;14(3):103–8. [Google Scholar]
- 7.Stocks J. Effect of nasogastric tubes on nasal resistance during infancy. Arch Dis Child. 1980;55(1):17–21. doi: 10.1136/adc.55.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daga SR, Lunkad NG, Daga AS, Ahuja VK. Orogastric versus nasogastric feeding of newborn babies. Trop Doct. 1999;29(4):242–3. doi: 10.1177/004947559902900417. [DOI] [PubMed] [Google Scholar]
- 9.Shiao SY, Youngblut JM, Anderson GC, DiFiore JM, Martin RJ. Nasogastric tube placement: effects on breathing and sucking in very-low-birth-weight infants. Nurs Res. 1995;44(2):82–8. [PubMed] [Google Scholar]
- 10.Arens R, Reichman B. Grooved palate associated with prolonged use of orogastric feeding tubes in premature infants. J Oral Maxillofac Surg. 1992;50(1):64–5. doi: 10.1016/0278-2391(92)90199-a. [DOI] [PubMed] [Google Scholar]
- 11.Bohnhorst B, Cech K, Peter C, Doerdelmann M. Oral versus nasal route for placing feeding tubes: no effect on hypoxemia and bradycardia in infants with apnea of prematurity. Neonatology. 2010;98(2):143–9. doi: 10.1159/000279617. [DOI] [PubMed] [Google Scholar]
- 12.Amaizu N, Shulman R, Schanler R, Lau C. Maturation of oral feeding skills in preterm infants. Acta Paediatr. 2008;97(1):61–7. doi: 10.1111/j.1651-2227.2007.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boiron M, Da Nobrega L, Roux S, Henrot A, Saliba E. Effects of oral stimulation and oral support on non-nutritive sucking and feeding performance in preterm infants. Dev Med Child Neurol. 2007;49(6):439–44. doi: 10.1111/j.1469-8749.2007.00439.x. [DOI] [PubMed] [Google Scholar]
- 14.Lau C, Alagugurusamy R, Schanler RJ, Smith EO, Shulman RJ. Characterization of the developmental stages of sucking in preterm infants during bottle feeding. Acta Paediatr. 2000;89(7):846–52. [PubMed] [Google Scholar]
- 15.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mizuno K, Ueda A. Neonatal feeding performance as a predictor of neurodevelopmental outcome at 18 months. Dev Med Child Neurol. 2005;47(5):299–304. doi: 10.1017/s0012162205000587. [DOI] [PubMed] [Google Scholar]
- 17.Lucas A, Lucas PJ, Baum JD. Differences in the pattern of milk intake between breast and bottle fed infants. Early Hum Dev. 1981;5(2):195–9. doi: 10.1016/0378-3782(81)90052-9. [DOI] [PubMed] [Google Scholar]