Goal:
The COVID-19 pandemic has left a significant impact on hospitals' operations, expenses, and revenues. However, little is known about the pandemic's financial impact on rural and urban hospitals. Our main objective was to analyze how hospital profitability changed during the first year of the pandemic. We specifically studied the association between COVID-19 infections and hospitalizations and county-level variables with operating margins (OMs) and total margins (TMs).
Methods:
We obtained data from Medicare Cost Reports, the American Hospital Association Annual Survey Database, and the Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry (CDC/ATSDR) for 2012–2020. Our final dataset consisted of an unbalanced panel with 17,510 observations for urban hospitals and 17,876 observations for rural hospitals. We estimated separate hospital fixed-effects models for urban and rural hospitals' OMs and TMs. The fixed-effects models controlled for time-invariant differences across hospitals.
Principal Findings:
In our review of the early impact of the COVID-19 pandemic on rural and urban hospitals' profits as well as trends in OMs and TMs from 2012 to 2020, we found that OMs were inversely related to the duration of hospitals' exposure to infections in urban and rural locations. In contrast, TMs and hospitals' exposures had a positive relationship. Government relief funds, a source of nonoperating revenue, apparently allowed most hospitals to avoid financial distress from the pandemic. We also found a positive relationship between the magnitude of weekly adult hospitalizations and OMs in urban and rural hospitals. Size, participation in group purchasing organizations (GPOs), and occupancy rates were positively related to OMs, with size and participation in GPOs relating to scale economies and occupancy rates reflecting capital efficiencies.
Practical Applications:
Hospitals' OMs have been declining since 2014. The pandemic made this decline worse, especially for rural hospitals. Federal relief funds, along with investment income, helped hospitals remain financially solvent during the pandemic. However, investment income and temporary federal aid are insufficient to sustain financial well-being. Executives need to explore cost-saving opportunities such as joining a GPO. Small rural hospitals with low occupancy and low community COVID-19 hospitalization rates have been particularly vulnerable to the financial impact of the pandemic. Although federal relief funds have limited hospital financial distress induced by the pandemic, we maintain that the funds should have been more effectively targeted, as the mean TM increased to its highest level in a decade. The disparate results of our analysis of OMs and TMs illustrate the utility of using multiple measures of profitability.
INTRODUCTION
During the height of the COVID-19 pandemic in 2020–2021, the world experienced a magnitude of societal and economic impact unprecedented in recent history. Previous pandemics and outbreaks resulted in significant financial losses for hospitals (Matheny et al., 2007). During the COVID-19 pandemic, however, hospitals were forced to (1) meet the complex and resource-intensive needs of hospitalized COVID-19 patients while providing routine care to non-COVID patients, (2) handle staffing shortages, (3) address widened disparities in outcomes and access, and (4) deal with financial struggles caused by the increased expenses and reduced utilization of non-COVID services (Grimm, 2021).
The pandemic has exposed hospitals to a plethora of challenges at the clinical, operational, and financial levels. The American Hospital Association (2022) estimated that drug expenses increased by 36.9% and medical supply expenses by 20.6% from prepandemic times. The high cost and shortages of medical supplies, coupled with unprecedented inflation, have led to higher hospital expenses. Moreover, the pandemic has forced hospitals to invest extra resources in training hospital staff on new protocols, securing a large volume of personal protective equipment, and expanding or reconfiguring their medical and intensive care units to accommodate the surge of COVID-19 patients (Anoushiravani et al., 2020). In addition to increased spending on training, supplies, and space reconfiguration, hospitals have been burdened by labor expenses that worsened during the pandemic as managers called on contract labor to meet the demand surge. A recent report estimates that labor expenses increased by 37% per patient from 2019 to March 2022 primarily because of a significant increase in contract labor expenses (Kaufman Hall, 2022).
The pandemic's impact on revenues has been significant, too. At the pandemic's peak, hospitals canceled not only elective surgeries but also cancer screenings, outpatient specialist visits, and even primary care visits (Barnett et al., 2020). Moreover, hospital admissions declined drastically at the start of the pandemic mainly because hospitals restricted the number of elective surgeries and nonemergency medical services (Birkmeyer et al., 2020). Hospital admissions from acute medical illnesses for non-COVID-19 patients also dropped (Birkmeyer et al., 2020). The cancelation of elective procedures threatened hospital solvency, given that those admissions make up almost one third of inpatient revenues—orthopedic and cardiac procedures specifically are primary revenue sources for hospitals (Khullar et al., 2020; Weiss et al., 2014). The financial impact of postponements and cancelations was significant: Nonelective care declined by almost 50% during the first year of the pandemic (Cutler et al., 2020).
Some counterforces may have mitigated the impact of the pandemic on hospitals. These included broadening reimbursement for telehealth, expanding the scope of tasks completed by nonphysician providers, and relaxing rules to allow physicians and nurses to practice in multiple states (Cutler et al., 2020). Moreover, Congress dedicated a total of $178 billion to hospitals and other healthcare organizations with its Coronavirus Aid, Relief, and Economic Security (CARES) Act, Paycheck Protection Program and Health Care Enhancement Act, and Consolidated Appropriations Act (Office of Inspector General, 2022). These funds compensated hospitals for their financial losses and ensured that pandemic-related services were available. Also, Medicare suspended its 2% payment sequestration, given that value-based purchasing indicators would have been hard to interpret during a public health emergency that lasted for multiple months (Binkowski et al., 2021).
Financial well-being is critical for both for-profit (FP) and not-for-profit (NFP) hospitals (Rosko et al., 2018) and has an impact on patient experience and the quality of care (Akinleye et al., 2019). Hospitals in recent years relied significantly on outpatient services and elective surgeries to boost revenues. For example, the aggregate outpatient share of total hospital revenue grew from 28% in 1994 to 48% in 2018 (Gerhardt & Arora, 2020). Therefore, there is a legitimate concern that hospitals might feel the pandemic's impact well past the COVID-19 public health emergency. Hospital CEOs of FP hospital systems in August 2022 reported a drop in net income from the same quarter in 2021; unlike what they initially expected, hospitals did not witness a boost in volume driven by pent-up care delayed by the pandemic (HealthcareDive, 2022).
In this article, we present our analysis of how the pandemic affected hospitals' profitability. We specifically compare the financial effects of the pandemic on rural and urban hospitals. There is a vast difference between rural and urban hospitals in terms of the populations they serve, the services they offer, Medicare reimbursement, and other challenges to operations and revenues. This is reflected in the high rate of closure of rural hospitals since 2013, which has been driven mainly by the lack of financial viability of some hospitals (Kaufman et al., 2020). We also describe hospital- and county-level variables and their impact on the profitability of rural and urban hospitals during the first year of the pandemic.
METHODS
Data and Sample
We relied on two sources for COVID-19 data. First was the county-level cumulative COVID-19 case rate from the New York Times COVID-19 database. We used information from the first day a county recorded COVID-19 cases to calculate the percentage of a hospital's fiscal year that fell during the pandemic. The second source of data was the hospital-level number of adults admitted with a diagnosis of COVID-19 provided by the U.S. Department of Health and Human Services.
We obtained information about margins from Medicare Cost Reports. Other hospital-level variables were obtained from the American Hospital Association Annual Survey Database. We obtained the Social Vulnerability Index (SVI) from the Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry (CDC/ATSDR). All data covered 2012–2020 except for the SVI, which was only available for 2010, 2014, 2016, and 2018. For the years in which updated SVIs were not available, we used the data from the most recent year.
The data sources were merged to construct the final analytical file consisting of 4,062 general acute hospitals, of which 2,022 were urban hospitals and 2,040 were rural hospitals. About 3% of the observations could not be used because data were missing or reported for less than 360 days. This resulted in a 9-year, unbalanced panel with 17,510 observations for urban hospitals and 17,876 observations for rural hospitals.
Dependent Variables
We used two measures of profitability as independent variables. We defined total margin (TM) as total income divided by revenue and operating margin (OM) as net patient income divided by net patient revenue. The latter measures profitability from business operations and is a more sensitive measure of payment policies' impact and operational efficiencies. The former includes nonoperating sources of income such as investments, philanthropy, and government appropriations (including federal COVID-19 relief payments) and is a better measure of hospitals' solvency (Rosko et al., 2020). Investment income is typically the largest source of nonoperating income for NFP hospitals, accounting for 43% of nonoperating income (Bai et al., 2020). The profit margin variables were winsorized at the 1st and 99th percentiles of the original distribution to prevent unrealistically large or small outliers from biasing our results.
Our conceptual model based financial performance on the hospital's exposure to COVID-19 and the intensity of the exposure, and a set of hospital- and county-level variables likely to affect a hospital's financial performance. The control variables were based on a recent review of the literature (Rosko et al., 2020), which found that hospital profitability is related to government policy, hospital characteristics, patient characteristics, and environmental characteristics.
Independent Variables
The primary independent variables of interest were two COVID-19-related independent variables: (1) the percentage of a hospital's fiscal year that occurred during the pandemic in its area and (2) adult COVID-19 hospitalizations per week. The former measured the exposure to COVID-19 while the latter measured the intensity of the exposure. All hospitals had exposure during their 2020 fiscal year. Depending on the start and end dates of a hospital's fiscal year and the first day when COVID-19 started in the county that the hospital was located, some hospitals might also have had exposure during their 2019 fiscal year.
At the hospital level, we included standard control variables. These included binary variables (i.e., 0/1) for size (i.e., small with fewer than 100 beds, medium with 100–400 beds, large with more than 400 beds), ownership (NFP, FP, local government hospitals), and whether they were an academic medical center (AMC), other teaching hospital (defined as having more than one resident or intern), multihospital system member, critical access hospital (CAH), or fully integrated with physicians (i.e., physicians under the foundation, integrated salary, or equity model). Further, we considered whether they participated in a group purchasing agreement, were located in a state that had expanded Medicaid eligibility after the passage of the Affordable Care Act, or provided transplant services or telehealth services. We also included continuous variables for Medicare's share of admissions, the share of Medicaid admissions, labor intensity (the number of full-time equivalent total personnel divided by the adjusted patient days), and the occupancy rate (calculated as the average daily census divided by the number of beds).
At the market level, we included a Herfindahl–Hirschman Index (the sum of the squared hospital market shares in the county) to control for the level of market competition. To control for social determinants of health, we used the CDC's SVI, which grouped 15 indicators into 4 themes and ranked counties on those themes and an overall SVI score. The four themes were: socioeconomic status (Theme 1), household composition and disability (Theme 2), minority status and language (Theme 3), and housing type and transportation (Theme 4). This article represents the themes by percentiles, with higher values indicating greater vulnerability.
Statistical Analysis
We performed the Chow test on urban and rural hospitals to assess whether their estimated parameters were equal. The result suggested that the two types of hospitals should be analyzed separately. Therefore, we estimated separate hospital fixed-effects models for urban and rural hospitals' OMs and TMs. The fixed effects control for time-invariant differences across hospitals. We also ran the Wald test to determine whether the equal variance assumption was satisfied. The test result suggested that the assumption was violated; therefore, instead of using the standard errors when determining the significance of the independent variables, we used the robust standard errors. All variance inflation factors were less than 3.5, so multicollinearity was not a concern. All analyses were performed using Stata (Version 16.0).
RESULTS
Univariate Results
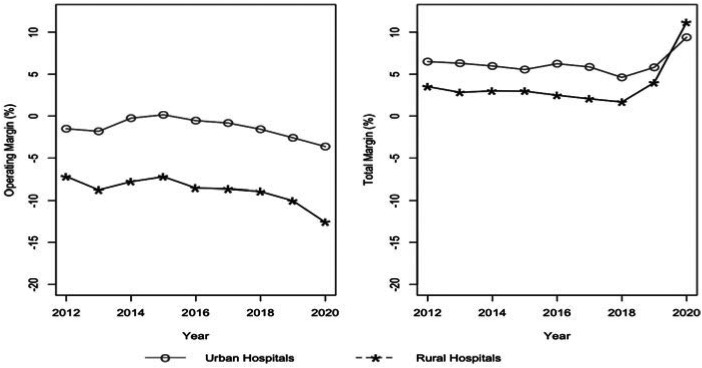
We compared OMs and TMs by year, 2012–2020, for six different characteristics of hospitals' internal and external environments. Figure 1 shows that urban hospitals had consistently higher OMs and TMs than their rural counterparts for each year of the study with one exception, 2020, when TMs increased for both. Hospitals in both types of locations have had declining OMs in recent years. A similar pattern held for TMs until 2019. We expected the pandemic would have a negative effect on operational performance. However, the increase in mean TMs in 2019 and 2020 may be due, in part, to extraordinary returns in the stock market in 2019 (Damodaran, 2022) and billions of dollars in government subsidies provided in 2020 to hospitals in response to the pandemic. Both were important sources of nonoperating revenue. Bai and colleagues (2020) and Wang and colleagues (2022) provide support for our contention.
FIGURE 1.
Operating and Total Margins of Urban and Rural Hospitals, Fiscal Years 2012–2020
Other teaching hospitals had a higher mean OM than AMCs and nonteaching hospitals during each study year. Nonteaching hospitals had the lowest OMs, with AMCs occupying a middle position. In 2020, other teaching hospitals saw an uptick in OMs, while hospitals in the other two categories suffered declines. When we analyzed TM, we found that AMCs held the top position in most years, but they were not much higher than other teaching hospitals. Nonteaching hospitals had the lowest TMs each year. Hospitals in each group experienced large gains in TM in 2020, with nonteaching hospitals showing the most significant increases.
Medium hospitals had the largest OM every year except in 2020 when large hospitals had the highest margin. The gap between these two types of hospitals has been narrowing since 2018. Small hospitals had the lowest OM every year, and the gap between them and other hospitals increased in recent years. Large hospitals had the highest TM every year, with medium hospitals in second place except in 2020 when small hospitals overtook them.
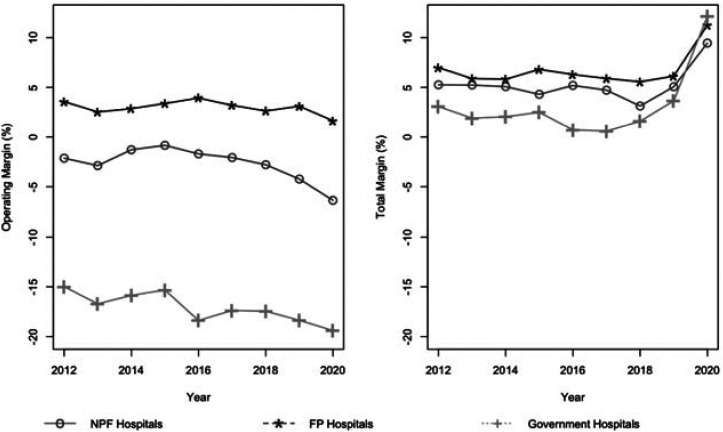
Figure 2 shows a consistently larger mean OM of FP hospitals as compared with NFP hospitals throughout the study period, with government hospitals having the lowest mean OM. Hospitals in each of these ownership groups experienced larger declines in 2020. Before 2019, the relative profitability by ownership type, when TM was examined, was the same as the order for OM. However, the mean TM increased for each type of hospital in 2019 and 2020. Government hospitals experienced the greatest increases in 2020 and had larger TMs than hospitals in the other two categories.
FIGURE 2.
Operating and Total Margins of Not-For-Profit, For-Profit, and Government Hospitals, Fiscal Years 2012–2020
As we expected, hospitals in states that expanded Medicaid coverage had a larger mean OM than hospitals in other states. When mean TM was examined, the differences between these two groups of hospitals narrowed considerably, and the hospitals in Medicaid expansion states did not have a larger value each year. Consistent with expectations, the mean OM was lowest for hospitals located in areas in the third and fourth quartile of the SVI. Mean TM was not very sensitive to differences in this index.
Regression Results
Table 1 shows regression results from the OM regression equations for rural and urban hospitals. As expected, we found a negative relationship (p < .05) between the duration of a hospital's exposure (measured by the percentage of a hospital's fiscal year that fell during the pandemic in its area) to COVID-19 infections and OM in urban and rural hospitals. As noted earlier, hospitals report data using different fiscal years and the pandemic struck communities at different times in 2020. We found a positive relationship (p < .01) between the magnitude of the infections, that is, weekly adult COVID-19 hospitalizations and OM in both urban and rural hospitals.
TABLE 1. Fixed-Effect Regression Estimates, Operating Margin, Fiscal Years 2012–2020.
| Variable | Urban Hospitals | Rural Hospitals | ||||
|---|---|---|---|---|---|---|
| Coef | Robust SE | Coef | Robust SE | |||
| Percentage of FY during COVID-19 | –3.847 | 1.727 | * | –4.971 | 0.673 | ** |
| Number of adult COVID-19 hospitalizations per week | 0.008 | 0.003 | ** | 0.035 | 0.009 | ** |
| Medium size (100–400 beds) | 3.479 | 1.178 | ** | 0.441 | 1.027 | |
| Large size (>400 beds) | 8.757 | 5.949 | –1.044 | 3.587 | ||
| Small size (<100 beds)—reference | ||||||
| For-profit ownership | 3.728 | 1.529 | * | 4.222 | 1.618 | ** |
| Government ownership | –2.255 | 4.133 | 0.183 | 1.271 | ||
| Not-for-profit ownership—reference | ||||||
| Academic medical center | 1.267 | 0.593 | * | N/A | ||
| Other teaching hospital | –2.47 | 2.163 | –0.658 | 1.304 | ||
| Nonteaching hospital—reference | ||||||
| System member | 1.163 | 1.005 | 0.419 | 1.040 | ||
| Critical access hospital | 9.989 | 3.693 | ** | 5.958 | 2.357 | * |
| Fully integrated physicians | 0.666 | 0.995 | 0.376 | 0.479 | ||
| Provides transplant services | –1.749 | 1.242 | ||||
| Provides telehealth services | –0.928 | 0.692 | –1.394 | 0.547 | * | |
| Participates in group purchasing | 1.337 | 0.646 | * | 0.464 | 0.553 | |
| Medicare share of admissions | 0.003 | 0.030 | 0.051 | 0.023 | * | |
| Medicaid share of admissions | –0.123 | 0.086 | –0.012 | 0.030 | ||
| Labor intensity | 1.998 | 8.273 | –7.520 | 7.620 | ||
| Occupancy rate | 0.071 | 0.033 | * | 0.089 | 0.017 | ** |
| Herfindahl–Hirschman Index | 0.000 | 0.000 | 0.000 | 0.000 | ||
| Located in a Medicaid expansion state | 0.995 | 0.500 | * | 0.883 | 0.397 | * |
| SVI Theme 1a | 0.696 | 9.037 | 1.860 | 3.516 | ||
| SVI Theme 2 | 2.934 | 4.048 | 1.516 | 2.394 | ||
| SVI Theme 3 | 2.173 | 9.188 | –0.564 | 3.101 | ||
| SVI Theme 4 | 4.349 | 5.915 | –0.507 | 2.053 | ||
| Constant | –15.229 | 8.806 | 23.385 | 4.733 | ||
| R2 within | 0.007 | 0.016 | ||||
| R2 between | 0.022 | 0.005 | ||||
| R2 overall | 0.012 | 0.006 | ||||
Note. N/A indicates that these were omitted in the rural hospital model because few hospitals are in this category. Reference signifies the omitted reference category. Coef = Coefficient; FY = fiscal year; SVI = Social Vulnerability Index.
aThe four SVI themes are: socioeconomic status (Theme 1), household composition and disability (Theme 2), minority status and language (Theme 3), and housing type and transportation (Theme 4).
*p < .05,
**p < .01.
We obtained different results when analyzing TM (see Table 2). We found a positive relationship (p < .01) between COVID-19 exposure and TM in the urban and rural hospital analysis. The coefficient of adult weekly hospitalizations for COVID-19 was negative and significant (p < .01) in the analysis of rural hospitals but not significant in urban hospitals. We found interesting results in the estimated coefficients of the control variables.
TABLE 2. Fixed-Effect Regression Estimates, Total Margin, Fiscal Years 2012–2020.
| Variable | Urban Hospitals | Rural Hospitals | ||||
|---|---|---|---|---|---|---|
| Coef | Robust SE | Coef | Robust SE | |||
| Percentage of FY during COVID-19 | 4.059 | 0.704 | ** | 11.310 | 0.740 | ** |
| Number of adult COVID-19 hospitalizations per week | 0.004 | 0.002 | –0.024 | 0.008 | ** | |
| Medium size (100–400 beds) | 2.564 | 1.170 | * | 1.206 | 0.929 | |
| Large size (>400 beds) | 4.284 | 2.114 | * | 0.416 | 2.025 | |
| Small size (<100 beds)—reference | ||||||
| For-profit ownership | 4.726 | 1.903 | * | 2.704 | 1.517 | |
| Government ownership | 0.833 | 2.308 | 0.383 | 1.095 | ||
| Not-for-profit—reference | ||||||
| Academic medical center | 1.085 | 0.506 | * | N/A | 1.269 | |
| Other teaching hospital | –0.703 | 1.113 | –1.889 | |||
| Nonteaching hospital—reference | ||||||
| System member | 0.492 | 0.713 | 1.014 | 1.034 | ||
| Critical access hospital | 12.919 | 3.592 | ** | 4.837 | 1.774 | ** |
| Fully integrated physicians | 0.876 | 0.423 | * | –0.039 | 0.510 | |
| Provides transplant services | –1.159 | 1.467 | N/A | |||
| Provides telehealth services | –0.055 | 0.363 | 0.258 | 0.571 | ||
| Participates in group purchasing | 0.377 | 0.513 | –0.079 | 0.619 | ||
| Medicare share of admissions | –0.016 | 0.023 | 0.034 | 0.021 | ||
| Medicaid share of admissions | –0.026 | 0.041 | 0.020 | 0.028 | ||
| Labor intensity | 14.618 | 5.607 | ** | 9.458 | 6.822 | |
| Occupancy rate | 0.052 | 0.030 | 0.034 | 0.016 | * | |
| Herfindahl–Hirschman Index | 0.000 | 0.000 | 0.000 | 0.000 | ||
| Located in a Medicaid expansion state | –0.764 | 0.302 | * | 0.217 | 0.357 | |
| SVI Theme 1a | 11.609 | 8.300 | 2.600 | 3.813 | ||
| SVI Theme 2 | 1.416 | 3.716 | 0.493 | 1.806 | ||
| SVI Theme 3 | 3.290 | 7.238 | 2.859 | 3.244 | ||
| SVI Theme 4 | –2.440 | 5.506 | 0.081 | 1.815 | ||
| Constant | –8.150 | 7.930 | 10.032 | 4.973 | ||
| R2 within | 0.013 | 0.047 | ||||
| R2 between | 0.001 | 0.001 | ||||
| R2 overall | 0.001 | 0.018 | ||||
Note. N/A indicates that these were omitted in the rural hospital model because few hospitals are in this category. Reference signifies the omitted reference category. Coef = Coefficient; FY = fiscal year; SVI = Social Vulnerability Index.
aThe four SVI themes are: socioeconomic status (Theme 1), household composition and disability (Theme 2), minority status and language (Theme 3), and housing type and transportation (Theme 4).
*p < .05,
**p < .01.
Regarding OM results, the coefficient of the Medicaid expansion and CAH variables was positive (p < .05) for both rural and urban hospitals. The positive coefficient of the binary variable, indicating whether a hospital is in a state with Medicaid expansion, suggests that increased Medicaid eligibility is associated with better operating performance. The positive coefficient of the binary variable, indicating whether a hospital is a CAH, suggests that cost-based Medicare payments are associated with higher profits.
We also found that the coefficient of medium size was positive and significant for urban hospitals only. Large size was not significant in either urban or rural locations. The positive estimate suggests that scale economies, up to certain limits, support profits in urban hospitals. Rural hospitals tend to be much smaller than their urban counterparts—too small to reap any scale benefits. The coefficient of AMC was positive and significant (p < .05) in urban hospitals in the OM equation. Occupancy rate had a positive association (p < .05) with OM in urban and rural hospitals. This suggests that greater capital efficiency is positively associated with OM. FP ownership had a positive coefficient (p < .05) in both equations, a result consistent with property rights theory (Mutter & Rosko, 2007). Participation in a group purchasing program, which confers some scale efficiencies, had a positive coefficient in urban hospitals but not in rural hospitals. Telehealth capability had a negative coefficient (p < .05) in rural hospitals but was not significant (p > .10) in urban facilities. The share of admissions paid by Medicare had a positive relationship (p < .05) in rural hospitals only.
Some independent variables were associated with the TM the same way as they were associated with the OM: Medium hospitals, AMCs, FP hospitals, and CAHs had significantly higher TM (p < .05), and the higher occupancy rate was associated with higher TM (p < .05).
Other variables had different results from those obtained in the OM equation. Large size was associated (p < .05) with higher TMs in urban hospitals compared to small hospitals, but not a significant predictor of OM. Larger hospitals have higher profiles and may be able to attract more donations. Similarly, size might affect the ability to obtain more government appropriations because larger hospitals may be able to hire people who specialize in grant writing. Labor intensity was positively correlated with TM (p < .01) for urban hospitals, but not a significant predictor for the OM of either urban or rural hospitals. Extra staff can provide more amenities, and this might be associated with better patient experiences and more donations. Finally, contrary to our expectations and our univariate analysis, location in a state that expanded Medicaid was negatively associated (p < .05) with the TM of urban hospitals.
DISCUSSION
Financial well-being is crucial for hospitals to meet growing demands associated with labor shortages, outdated facilities, technological and clinical innovations, demand surges, and the operational and clinical implications of the healthcare sector's shift toward value-based purchasing. We examined how hospitals' financial performance changed during the first year of the COVID-19 pandemic and identified hospital- and county-level variables associated with better OMs and TMs.
According to our findings, hospitals in the United States have experienced declining OMs since 2014. Surprisingly, TMs have increased from 2018 to 2020. While on average, FP hospitals have had higher OMs than NFP and government hospitals, all hospitals, regardless of ownership, experienced a decline in their OMs in 2020 during the height of the pandemic.
One of the key takeaways from our analysis is that rural and urban hospitals alike had higher margins if COVID-19 hospitalizations were higher in the counties they served. Moreover, hospitals with higher occupancy rates experienced higher OMs. After the pandemic struck in March 2019, many hospitals ceased elective and outpatient department services for several months. It appears that hospitals that were able to fill their empty beds with COVID-19 patients were able to improve their OMs.
Regardless of actual COVID-19 hospitalizations, hospitals across the United States had to prepare for a possible pandemic-related surge in demand and thus incur additional expenses to buy needed personal protective equipment and ventilators and to train staff on new pandemic-related protocols, among other expenses. Therefore, hospitals incurred additional expenses that could only be offset if counter-balanced by increased utilization of inpatient services. Hospitals with low rates of COVID-19 hospitalizations in the county might have incurred the cost but did not gain the needed revenues. Moreover, hospitals with higher occupancy rates had higher OMs regardless of location. Occupancy rate not only reflects the utilization of hospital inpatient services and thus revenues, but it also reflects how effective a hospital's strategies were in gaining market share, perceptions of patients and physicians in the community, and the availability of services, technology, and trained staff (Langland-Orban et al., 1996).
The finding that group purchasing organizations (GPOs) are associated with higher OMs is not surprising. Hospitals that rely on GPOs tend to be more efficient; however, there is limited evidence that the reliance results in higher profitability (Lee et al., 2021). GPOs function as intermediaries by giving hospitals access to thousands of cataloged products from various manufacturers (Bruhn et al., 2018). They leverage their purchasing power to acquire supplies and devices from manufacturers at lower prices (Bruhn et al., 2018). Therefore, most hospitals use a GPO to scan thousands of cataloged products, purchase supplies, and receive training on the use of the supplies, all while benefiting from the discounted rates GPOs offer. Given the supply chain challenges that hospitals faced during the pandemic, it is likely that GPOs played a role in minimizing the impact supply shortages had on hospital operations and spending.
Interestingly, our findings show that rural hospitals with telehealth capabilities had lower OMs. This finding should be interpreted with caution. While telehealth technology, in theory, should enable hospitals to provide certain services remotely, there is a wide range of capabilities associated with telehealth. Unfortunately, the telehealth variable in our model indicates only whether the hospital has the technology without going into specifics. It does not offer data on which capabilities are available and used by the hospital. Therefore, while a rural hospital might have telehealth services, the literature indicates that rural hospitals with telehealth technology are less likely than urban hospitals to have the capabilities to enable robust patient engagement (Chen et al., 2021). Another explanation could be the high cost of telehealth technology, which in the short-term increases hospital expenses and consequently reduces profits. This is especially important if the demand for telehealth services in rural areas is not strong enough to offset the costs of providing those services.
TM is affected by the same factors that influence OM plus those (e.g., investment income, government appropriations) that influence nonoperating revenues and expenses. Unlike the experience with OMs, mean hospital TMs increased in 2019 and 2020 for all the hospital categories we tracked. The improvement in TM in 2019 was influenced by an unusually robust stock market (the Standard & Poor's 500 index increased by more than 30% over the previous year). Undoubtedly, the 2020 TM increase was influenced by the substantial COVID-19 aid packages authorized by the federal government, which amounted to $178 billion (Office of Inspector General, 2022). The funds received by hospitals during the public health emergency likely contributed to the sharp drop in the number of hospital closures in 2020 (25) and 2021 (11) compared to 2019 (46) (Binkowski et al., 2021).
The estimate for percent fiscal year during COVID-19 is positive (p < .05) in both the urban and rural TM equations. This suggests that hospitals with reporting periods covering a longer COVID-19 outbreak might have had more time to obtain government pandemic relief funds. Given the magnitude of the health emergency, the federal government needed to provide swift fiscal relief as expenses soared and revenues plummeted. However, the relief funding likely was either too much or not effectively deployed. Our analysis shows that the mean TM increased dramatically in 2020 to a level not achieved earlier in this study's time period. Anecdotal evidence suggests that some hospitals received excess funding. For example, the Mayo Health System gave back $156 million in federal funds (Rau & Spolar, 2021). Recognizing its mistake, in September 2020, the U.S. Department of Health and Human Services restricted relief payments to hospitals with 3% or lower profit margins.
We found that AMCs and larger hospitals tended to have larger TMs than other types of hospitals. These hospitals are more likely to have specialized staff to seek and obtain government funds. MACPAC (2021) estimates that only 73% of hospitals received Provider Relief Funds in 2020. MACPAC notes that the application process was burdensome, especially for small providers with few administrative staff. We recommend that future relief funding applications be simplified.
Our findings indicate that rural hospitals (particularly CAHs) had substantial increases in average TM during the pandemic period. Given their precarious financial position before the pandemic (see Figure 1), it is understandable that these types of hospitals would be targeted for extra relief funds (MACPAC, 2021).
It is important to emphasize that the disparate results for OM and TM suggest that the strong TM in 2020 might be a short-term mirage associated with strong stock market returns, which influenced investment income and donations, and generous—but temporary—government relief payments. A report by Kaufman Hall (2022) projected hospital OMs in 2022 to fall 37% relative to pre-pandemic levels. Flicek (2022) points out that hospitals ranging from small CAHs to members of large systems faced a looming financial crisis as financial subsidies began to dry up. Letting hospital solvency rest on this shaky foundation is not wise; the government should reexamine its payment policies.
Study Limitations
We note that Medicare Cost Reports have known limitations with item nonresponse and data quality (Blavin & Ramos, 2021). While we based our study on the most recent Medicare Cost Reports, some hospitals had fiscal years that did not span the entire first year of the pandemic. The COVID-19 exposure variable compensated for this limitation. Moreover, although we controlled for hospital-level variables, we might not have included a few variables because the data were not available. Another limitation is our inability to control for leadership variables due to data limitations. For example, leadership tenure and experience are likely to affect a hospital's ability to manage resources, expenditures, and revenues during a crisis.
CONCLUSION
The COVID-19 pandemic has threatened the healthcare system at multiple levels, from patient care to staff well-being and retention—even to hospital financial solvency. Hospitals' OMs have been declining since 2014, and the pandemic has worsened this decline. While TMs have not suffered, hospital executives and policymakers should be alarmed by the declining OMs. The OM is an indicator of the viability of hospitals as a business model because it excludes donations and investment income and reflects the difference between operating revenues and expenses.
Moreover, some preliminary analyses have found that pandemic relief payments may have been less than equitable. According to Schwartz and Damico (2020), hospitals with the lowest share of private insurance revenue received less than half as much funding for each hospital bed compared to the hospitals with the greatest share of revenue from private insurance. Grogan et al. (2021) conclude, “In terms of distributional equity, the allocation of Provider Relief Funds to address the COVID-19 crisis can only bluntly be described as unsanitized and unfair” (p. 808).
This study only captures the early impact of the pandemic and should be followed up as more data are available and experience is gained. Moreover, future pandemics are inevitable. The federal government needs to sufficiently invest in the U.S. public health system to lessen the pressure on hospitals.
We also recommend that future research should examine the impact of the distribution of COVID-19 funds on hospital financial performance and consider the demographics of hospitals' service areas.
Footnotes
The authors declare no conflicts of interest.
Contributor Information
Kate Li, Email: kjli@suffolk.edu.
Mona Al-Amin, Email: malamin@suffolk.edu, Sawyer Business School, Suffolk University, Boston, Massachusetts.
Michael D. Rosko, Email: m_rosko@hotmail.com, School of Business Administration, Widener University, Chester, Pennsylvania.
REFERENCES
- Akinleye D. D., McNutt L.-A., Lazariu V., McLaughlin C. C. (2019). Correlation between hospital finances and quality and safety of patient care. PLoS One, 14(8), e0219124. 10.1371/journal.pone.0219124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Hospital Association. (2022, April). Massive growth in expenses & rising inflation fuel financial challenges for America's hospitals & health systems [Report]. https://www.aha.org/guidesreports/2022-04-22-massive-growth-expenses-and-rising-inflation-fuel-continued-financial
- Anoushiravani A. A., O'Connor C. M., DiCaprio M. R., Iorio R. (2020). Economic impacts of the COVID-19 crisis: An orthopaedic perspective. Journal of Bone and Joint Surgery, 102(11), 937–941. 10.2106/JBJS.20.00557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai G., Yehia F., Chen W., Anderson G. F. (2020). Investment income of US nonprofit hospitals in 2017. Journal of General Internal Medicine, 35(9), 2818–2820. 10.1007/s11606-020-05929-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett M. L., Mehrotra A., Landon B. E. (2020, April 29). COVID-19 and the upcoming financial crisis in health care. NEJM Catalyst, 1(2). https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0153 [Google Scholar]
- Binkowski A., Stensland J., Zabinski D., Tabor L., O'Donnell B. (2021). Assessing payment adequacy and updating payments: Hospital inpatient and outpatient services. https://www.medpac.gov/wp-content/uploads/2021/09/Hospital-update-MedPAC-Dec-2021.pdf
- Birkmeyer J. D., Barnato A., Birkmeyer N., Bessler R., Skinner J. (2020). The impact of the COVID-19 pandemic on hospital admissions in the United States: Study examines trends in US hospital admissions during the COVID-19 pandemic. Health Affairs (Millwood), 39(11), 2010–2017. 10.1377/hlthaff.2020.00980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blavin F., Ramos C. (2021). Study examines Medicaid expansion effects on hospital finances and implications for hospitals facing COVID-19 challenges. Health Affairs (Millwood), 40(1), 82–90. 10.1377/hlthaff.2020.00502 [DOI] [PubMed] [Google Scholar]
- Bruhn W. E., Fracica E. A., Makary M. A. (2018). Group purchasing organizations, health care costs, and drug shortages. JAMA, 320(18), 1859–1860. 10.1001/jama.2018.13604 [DOI] [PubMed] [Google Scholar]
- Chen J., Amaize A., Barath D. (2021). Evaluating telehealth adoption and related barriers among hospitals located in rural and urban areas. Journal of Rural Health, 37(4), 801–811. 10.1111/jrh.12534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D. M., Nikpay S., Huckman R. S. (2020). The business of medicine in the era of COVID-19. JAMA, 323(20), 2003–2004. 10.1001/jama.2020.7242 [DOI] [PubMed] [Google Scholar]
- Flicek G. (2022). Analysis: 88% of large health systems are losing money in 2022 [Blog]. https://www.ascendient.com/insights/blog/healthcare-financial-planning-88-of-large-health-systems-are-losing-money-in-2022/
- Gerhardt W., Arora A. (2020). Hospital revenue trends: Outpatient, home, virtual, and other care settings are becoming more common. https://www2.deloitte.com/us/en/insights/industry/health-care/outpatient-virtual-health-care-trends.html
- Grimm C. A. (2021, March). Hospitals reported that the COVID-19 pandemic has significantly strained health care delivery. U.S. Department of Health and Human Services. https://oig.hhs.gov/oei/reports/OEI-09-21-00140.asp [Google Scholar]
- Grogan C. M., Lin Y. -A., Gusmano M. K. (2021). Unsanitized and unfair: How COVID-19 bailout funds refuel inequity in the US health care system. Journal of Health Politics, Policy and Law, 46(5), 785–809. 10.1215/03616878-9155977 [DOI] [PubMed] [Google Scholar]
- HealthcareDive. (2022). Volumes, net income down at for-profit hospitals in Q2 [News release]. https://www.healthcaredive.com/news/for-profit-hospitals-second-quarter-income-volumes-down/628679/
- Kaufman B. G., Whitaker R., Pink G., Holmes G. M. (2020). Half of rural residents at high risk of serious illness due to COVID-19, creating stress on rural hospitals. Journal of Rural Health, 36(4), 584–590. 10.1111/jrh.12481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman Hall. (2022, May 11). Reliance on contract labor during pandemic means higher hospital expenses [News release]. https://www.kaufmanhall.com/news/reliance-contract-labor-during-pandemic-means-higher-hospital-expenses
- Khullar D., Bond A. M., Schpero W. L. (2020). COVID-19 and the financial health of US hospitals. JAMA, 323(21), 2127–2128. 10.1001/jama.2020.6269 [DOI] [PubMed] [Google Scholar]
- Langland-Orban B., Gapenski L. C., Vogel W. B. (1996). Differences in characteristics of hospitals with sustained high and sustained low profitability. Journal of Healthcare Management, 41(3), 385–399. [PubMed] [Google Scholar]
- Lee C. C., Langdo J., Hwang D., Marques V., Hwang P. (2021). Impacts of distributors and group purchasing organizations on hospital efficiency and profitability: A bilateral data envelopment analysis model. International Transactions in Operational Research, 30(1), 476–502. 10.1111/itor.12957 [DOI] [Google Scholar]
- MACPAC. (2021, February). COVID relief funding for Medicaid providers [Issue brief]. https://www.macpac.gov/wp-content/uploads/ 2021/02/COVID-Relief-Funding-for-Medicaid-Providers.pdf
- Matheny J., Toner E., Waldhorn R. (2007). Financial effects of an influenza pandemic on US hospitals. Journal of Health Care Finance, 34(1), 58–63. [PubMed] [Google Scholar]
- Mutter R. L., Rosko M. D. (2007). The impact of ownership on the cost-efficiency of US hospitals. Advances in Health Economics and Health Services Research, 18, 113–138. 10.1016/S0731-2199(07)00007-6 [DOI] [PubMed] [Google Scholar]
- Office of Inspector General. (2022). Hospital's compliance with the provider relief fund balance billing requirement for out-of- network patients. Retrieved August 15, 2022, from https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000647.asp#:∼:text=The%20Coronavirus%20Aid%2C%20Relief%2C%20and,and%20other%20health%20care%20providers
- Rau J., Spolar C. (2021, April 1). Some of America's wealthiest hospital systems ended up even richer, thanks to federal bailouts. Washington Post. https://www.washingtonpost.com/us-policy/2021/04/01/hospital-systems-cares-act-bailout/
- Rosko M., Al-Amin M., Tavakoli M. (2020). Efficiency and profitability in US not-for-profit hospitals. International Journal of Health Economics and Management, 20(4), 359–379. https://link.springer.com/article/10.1007/s10754-020-09284-0 https://doi.org/10.1007/s10754-020-09284-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosko M., Goddard J., Al-Amin M., Tavakoli M. (2018). Predictors of hospital profitability: A panel study including the early years of the ACA. Journal of Health Care Finance, 44(3), 359–379. http://www.healthfinancejournal.com/index.php/johcf/article/download/148/152 [Google Scholar]
- Schwartz K., Damico A. (2020, May 13). Distribution of CARES Act funding among providers. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/issue-brief/distribution-of-cares-act-funding-among-hospitals/ [Google Scholar]
- Wang Y., Witman A. E., Cho D. D., Watson E. D. (2022, September). Financial outcomes associated with the COVID-19 pandemic in California hospitals. JAMA Health Forum, 3(9), e223056. 10.1001/jamahealthforum.2022.3056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss A. J., Elixhauser A., Andrews R. M. (2014, February). Characteristics of operating room procedures in US hospitals, 2011 [Statistical brief 170]. Agency for Healthcare Research and Quality. https://hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.jsp [PubMed] [Google Scholar]